Periodontal therapy
Gingival Surgical ProcedureGingival Surgical Procedure
They are periodontal pocket reduction surgery limited to the gingival tissue only and not involving the underlying osseous structures, without use flap surgery.They include:
A)gingival currettage
B)gingivectomy
Gingival curretage
Scrapping of the gingival wall of a periodontal pocket to remove diseased soft tissue.It is of 2 types
Gingival curretage (lateral to pocket wall).
Subgingival curretage (apical to Attached epith. down to osseous crest).
Some degree of curretage is accomplished during scaling and root planning (Inadverted curretage).
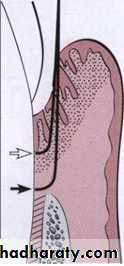
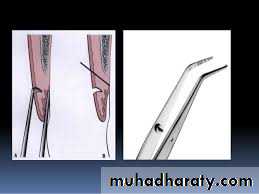
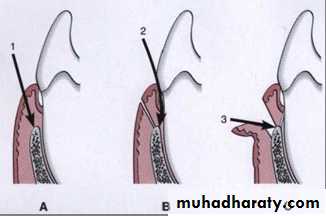
Extent of gingival curettage (white arrow) and subgingival
curettage (black arrow)
Periodontal pocket wall component
Granulation tissue (fibroblastic and angioblastic prolifiration)Chronic inflammation
Pieces of dislodgement calculus
Bacterial colonies
Epithelium lining (act as barrier for new fiber attachment)
Indications
Indications for curettage are very limited. It can be used after scaling and root planing for the following purposes:.• Curettage can be performed as part of new attachment attempts in moderately deep intrabony pockets located in accessible areas in wich closed surgery is indicated.
• Curettage can be done as a non definitive procedure to reduce inflammation prior to pocket elimination using other methods or in patients in whom more aggressive surgical techniques are contraindicated. It should be understood that in these patients.
Indication
3)Curettage is also frequently performed on recall visits as a method of maintenance treatment for areas of recurrent inflammation and pocket depth, particularly where pocket reduction surgery has previously been performed.Procedure:
it should always be preceded by scaling and root planing.The use of local infiltrative anesthesia for this procedure is optional.
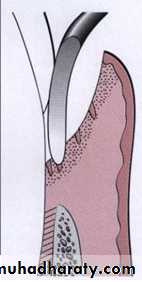
The curette is selected so that the cutting edge will be against the tissue (e.g., the Gracey No. 13-14 is used for mesial surfaces and the Gracey No. 11-12 for distal surfaces).
The instrument is inserted so as to engage the inner lining of the pocket wall and is carried along the soft tissue, usually in a horizontal Stroke.
The curette is then placed under the cut edge of junctional epithelium to undermine it.
The area is flushed to remove debris.
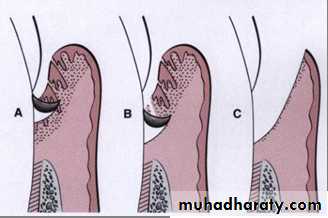
Subgingival curettage. A, Elimination of pocket lining. B, Elimination of junctional epithelium and granulation tissue. C, Procedure completed.
Other Techniques
Other techniques for gingival curettage includethe excisional new attachment procedure
ultrasonic curettage
the use of caustic drugs
Excisional New A ttachment Procedure (E N A P )
It is difinitive subgingival curretage procedure performed with a knife.• After adequate anesthesia, an internal bevel incision
is made from the margin of the free gingiva apically
to a point below the bottom of the pocket.
The incision is carried interproximally on both the facial and the lingual sides, attempting to retain as much interproximal tissue as possible.
Excisional New A ttachment Procedure (E N A P )
2. Remove the excised tissue with a curette, and care-
fully root plane all exposed cementum to a smooth,
hard consistency. Preserve all connective tissue fibers
that remain attached to the root surface.
3. Approximate the wound edges; if they do not meet passively, recontour the bone until good adaptation of the wound edges is achieved. Place sutures and a periodontal dressing.
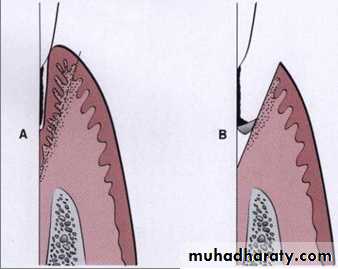
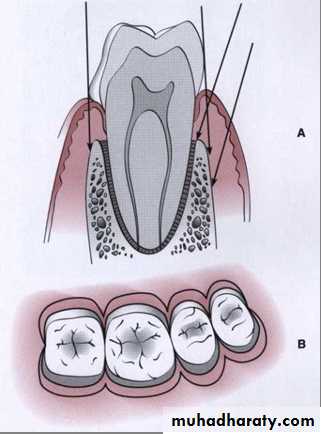
Excisional new attachment procedure. A, Internal bevel incision to point below bottom of pocket. B, After excision of tissue, scaling and root planing are performed.
Ultrasonic Curettage.
The use of ultrasonic devices has been recommended for gingival curettage.Ultrasound is effective for debriding the epithelial lining of periodontal pockets.
The gingiva can be made more rigid for ultrasonic curettage by injecting anesthetic solution directly into it.
Caustic Drugs
Since early in the development of periodontal procedures, the use of caustic drugs has been recommended to induce a chemical curettage of the lateral wall of the pocket or even the selective elimination of the epithelium.Drugs such as sodium sulfide, alkaline sodium hypochlorite solution and phenol have been proposed and then discarded after studies showed their ineffectiveness.
The extent of tissue destruction with these drugs cannot be controlled and they may increase rather than reduce the amount of tissue to be removed by enzymes and phagocytes.
Gingivectomy
means excision of the gingiva.by removing pocket wall so provide visibility and accessibility for complete calculus removal.
Types of gingivectomy:
• Surgical gingivectomy
• Electrical gingivectomy
• Laser gingivectomy
• Chemical gingivectomy
Indication
Elimination of suprabony pockets, regardless of their depth, if the pocket wall is fibrous and firmElimination of gingival enlargements.
Elimination of suprabony periodontal abscesses'
Contraindications
• The need for bone surgery or examination of the bone shape and morphology.• Situations in which the bottom of the pocket is apical to the mucogingival junction
• Esthetic considerations, particularly in the anterior maxilla.
Surgical Gingivectoy
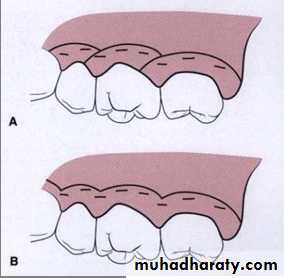
Step 1: The pockets on each surface are explored with a periodontal probe and marked with a pocket marker. Each pocket is marked in several areas to outline its course on each surface.Step 2: Periodontal knives (Kirkland knives) are used for incisions on the facial and lingual surfaces and those distal to the terminal tooth in the arch. Orban periodontal knives are used for supplemental interdental incisions.
The incision should be beveled at approximately 45 degrees to the tooth surface. Failure to bevel leaves may lead to recurrence of pockets.
Discontinuous or continuous incisions may be used is started apical to the points marking the course of the pockets and is directed coronally to a point between the base of the pocket and the crest of the bone. Exposure of bone is undesirable.
If it occurs, should adequately covered by the periodontal pack
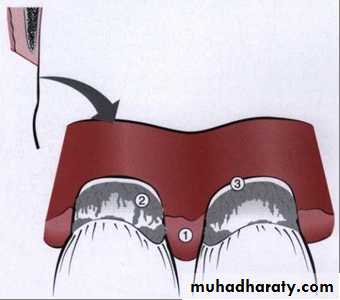
Step 3: Remove the excised pocket wall, clean the area. Field of operation immediately after removing pocket wall:
1, Granulation tissue
2, calculus and other root deposits
3, clear space where bottom of the pocket was attached.
Step 4: Carefully curette out the granulation tissue and remove any calculus and necrotic cementum so as to leave a smooth and clean surface.
Step 5: Cover the area with a surgical pack.
Gingivoplasty
Gingivoplasty is a reshaping of the gingivato create physiologic gingival contours indicated to
Shelf like interdental papillae caused by acute necrotizing ulcerative gingivitis
Gingival clefts and craters
gingival enlargement
The Periodontal Flap
periodontal flap is a section of gingiva and/ormucosa surgically separated from the underlying tissues to provide visibility of and access to the
bone and root surface
Classification Of Flaps
Periodontal flaps can be classified based on the following:Bone exposure after flap reflection
Placement of the flap after surgery
Management of the papilla
Based on bone exposure after flap reflection
The flaps are classified :
• full thickness (mucoperiosteal) which is indicated when resective osseous surgery is contemplated.
• partial thickness (mucosal) is indicated when the flap is to be positioned apically or when the operator does not desire to expose bone.
Based on flap placement after surgery
flaps are classified as1) nondisplaced flaps, when the flap is returned and sutured in its original position
2) displaced flaps that are placed apically, coronally, or laterally to their original position.
Based on management of the papilla
• conventional flap (papilla is split beneath the contact point of the two approximating teeth). The conventional flap is used when1) the interdental spaces are too narrow
2) when the flap is to be displaced
Conventional flaps include
the modified Widman flap
the undisplaced flap
the apically displaced flap
the flap for regenerative procedures.
2. papilla preservation flaps(incorporates the entire papilla in one of the flaps and a horizontal incision at the base of the papilla leaving it connected)
Incision
Horizontal Incisionsthe internal bevel incision which starts with bevel incision
crevicular incision
• interdental incision
internal bevel incision accomplishes three important objectives:
1) it removes the pocket lining2) it conserves the relatively un involved outer surface of the gingiva
3) it produces a sharp, thin flap margin for adaptation to the bone-tooth junction.
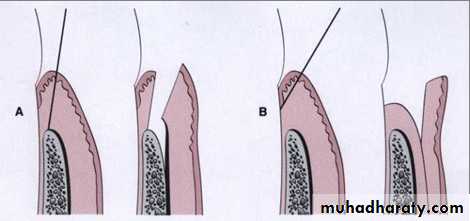
A. The internal bevel incision can be made at varying locations and angles according to the different anatomic and pocket situations.
B. An occlusal view of the different locations
Where the internal bevel incision can be made.
Note the scalloped
Shape of the incisions.
crevicular incision
is made from the base of the pocket to the crest of the bone
interdental incision
Vertical Incisions
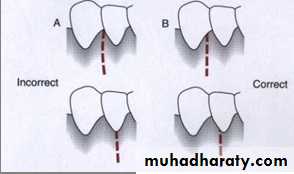
Vertical or oblique releasing incisions can be used on one or both ends of the horizontal incision , depending on the design and purpose of the flap .Vertical incisions must extend beyond the mucogingival line, reaching the alveolar mucosa, to allow for the release of the flap to be displaced. In general, vertical incisions in the lingual and palatal areas are avoided .
Incorrect (A) and correct (B) locations of a vertical incision. This incision should be made at the line angles to prevent splitting of a papilla or incising directly over a radicular surface.