
1
Fifth stage
Pediatric
Lec-5
د.ندى العلي
21/12/2016
Urinary Tract Infections
Objectives
1-What are the risk factors of U.T.I. in children
2-What are the the signs and symptoms in different age group
3-How you diagnose
4-treatment and complication
5-Prevention-
EPIDEMIOLOGY
Approximately 8% of girls and 2% of boys have a UTI by 11 years of age. In infants,
boys are affected more than five times as often as girls.
After 12 months of age, UTI in healthy children usually is seen in girls.
A short urethra predisposes girls to UTI. Uncircumcised male infants are at 5- to 12-
fold increased risk for UTI compared with circumcised male infants.
Obstruction to urine flow and urinary stasis is the major risk factor and may result
from anatomic abnormalities, nephrolithiasis, renal tumor, indwelling urinary
catheter, ureteropelvic junction obstruction, megaureter, extrinsic compression, and
pregnancy.
Vesicoureteral reflux, whether primary (70% of cases) or secondary to urinary tract
obstruction, predisposes to chronic infection and renal scarring. Scarring also may
develop in the absence of reflux
The urinary tract and urine are normally sterile. Escherichia coli, ascending from
bowel flora, accounts for 90% of first infections and 75% of recurrent infections.
CLINICAL MANIFESTATIONS
The symptoms and signs of UTI vary markedly with age. Few have high positive
predictive values in neonates, with failure to thrive, feeding problems, and fever the
most consistent symptoms. Direct hyperbilirubinemia may develop secondary to
gram-negative endotoxin.
Infants 1 month to 2 years old may present with feeding problems, failure to thrive,
diarrhea, vomiting

2
At 2 years of age, children begin to show the classic signs of UTI such as urgency,
dysuria, frequency, and abdominal or back pain. The presence of UTI should be
suspected in all infants and young children with unexplained fever and in patients of
all ages with fever and congenital anomalies of the urinary tract.
LABORATORY AND IMAGING STUDIES
Urine obtained by midstream, (for older children and adolescents) is considered
significant i.e the patient considered to have u.t.i.with bacterial growth of a single
organism of more than 100,000 colony-forming units/unit or if there is10,000&the the
child is symptomatic
In infants(not trained)the use of adhesive sterile collecting bag can be useful if
negative to exclude infection or if positive100,000 in symptomatic with positive urine
culture if any of these criteria not met then confirmation by catheterized sample
In infants(not trained)the use of adhesive sterile collecting bag can be useful if
negative to exclude infection or if positive100,000 in symptomatic with positive urine
culture if any of these criteria not met then confirmation by catheterized sample
Urine obtained by catheterization is considered significant with bacterial growth of
more than 10,000 CFU/mL. Urine obtained by suprapubic aspiration is considered
significant with any bacterial growth .
Suprapubic percutaneous aspiration of the bladder may be performed in young
infants if they have not voided for 1 to 3 hours. Perineal bags for urine collection are
prone to contamination and are not recommended for urine collection for culture.
The diagnosis of UTI requires a culture of the urine. Urine samples for urinalysis
should be examined promptly (within 20 minutes) or refrigerated until cultured
Urinalysis showing pyuria (leukocyturia of >5 white blood cells suggests infection
The presence of numerous motile bacteria in freshly voided, uncentrifuged urine from
symptomatic infants and children has a 94% correlation with a positive culture )
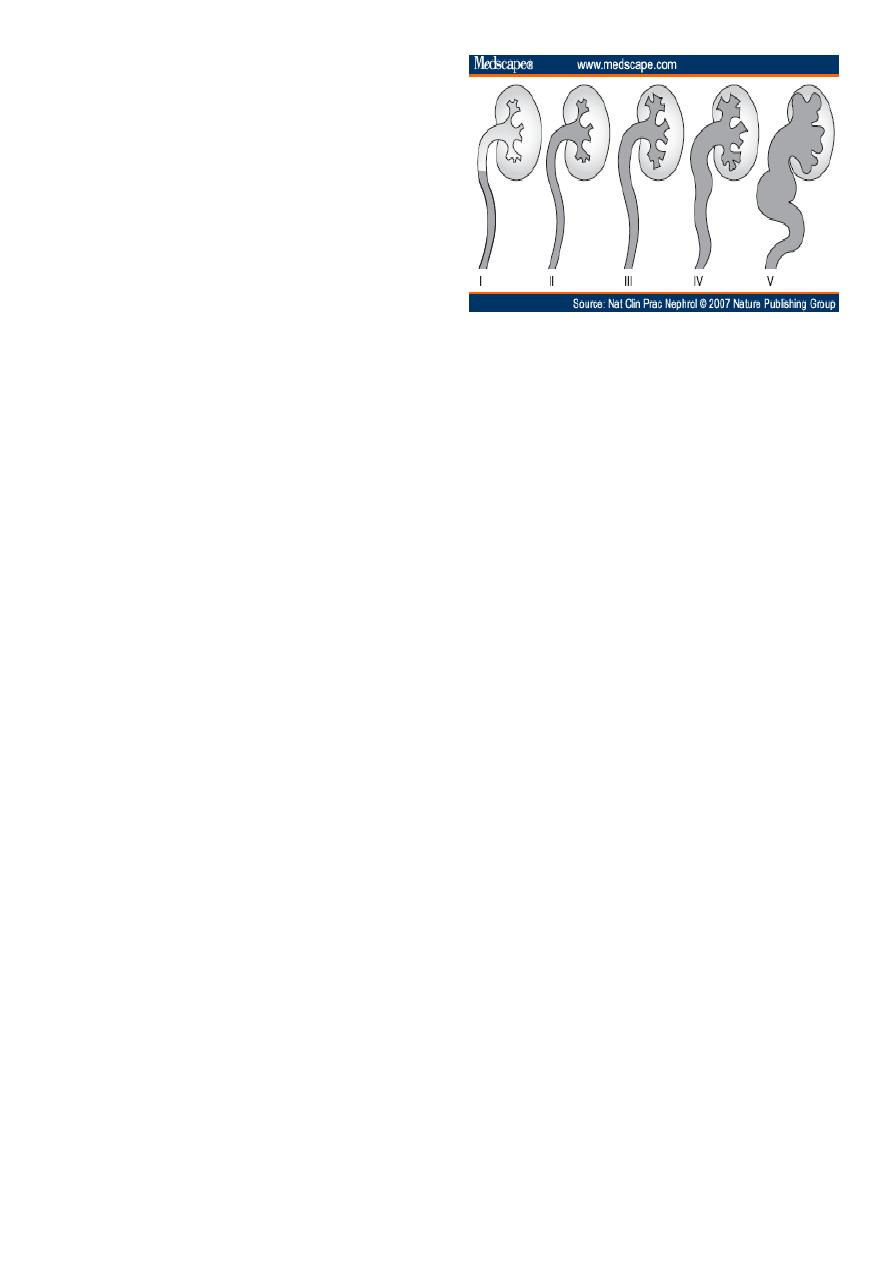
VCUG is done after3weeks&is the best imaging study for determining the presence or
absence of vesicoureteral reflux, which is ranked from grade I (ureter only) to grade V
(complete gross dilation of the ureter and obliteration of caliceal and pelvic anatomy)
Ultrasound which done in the acute illness provides limited information about renal
scarring and is performed to exclude an anatomic abnormality
renal nucleotide scans, and computed tomography (CT) or magnetic resonance
imaging (MRI) can be used for anatomic and functional assessment of the urinary A
technetium-99m DMSA scan can identify acute pyelonephritis and is most useful to
define renal scarring as a late effect of UTI. tract
3
Grades of reflux
Grade1 reflux into non dilated ureter
Grade2 reflux into upper collecting with
out dilatation
Grade3 reflux into dilated ureter and or
blunting collecting system
Grade4 reflux into grossly dilated ureter
Grade5 massive reflux with tortuosity
and loss of impression
DIFFERENTIAL DIAGNOSIS
The manifestations of UTI overlap with signs of sepsis seen in young infants and with
enteritis, appendicitis, mesenteric lymphadenitis, and pneumonia in older children.
Dysuria may indicate pinworm infection, hypersensitivity to soaps or detergents,
vaginitis, or sexual abuse and infection
Localization of a UTI is important because upper UTI is associated more frequently
with bacteremia and with anatomic abnormalities than is cystitis.
The clinical manifestations of UTI do not reliably distinguish the site of infection in
neonates, infants, and toddlers. Fever and abdominal pain may occur with either
lower or upper UTI, although high fever, costovertebral tenderness, high erythrocyte
sedimentation rate (ESR), leukocytosis, and bacteremia each suggest upper tract
involvement. Indirect findings such as WBC casts, inability to concentrate urine
maximally, presence of antibody-coated bacteria detected by immunofluorescence,
are of limited value in localizing the site of the UTI to the upper tract. DMSA scan is
sensitive for detecting acute pyelonephritis.
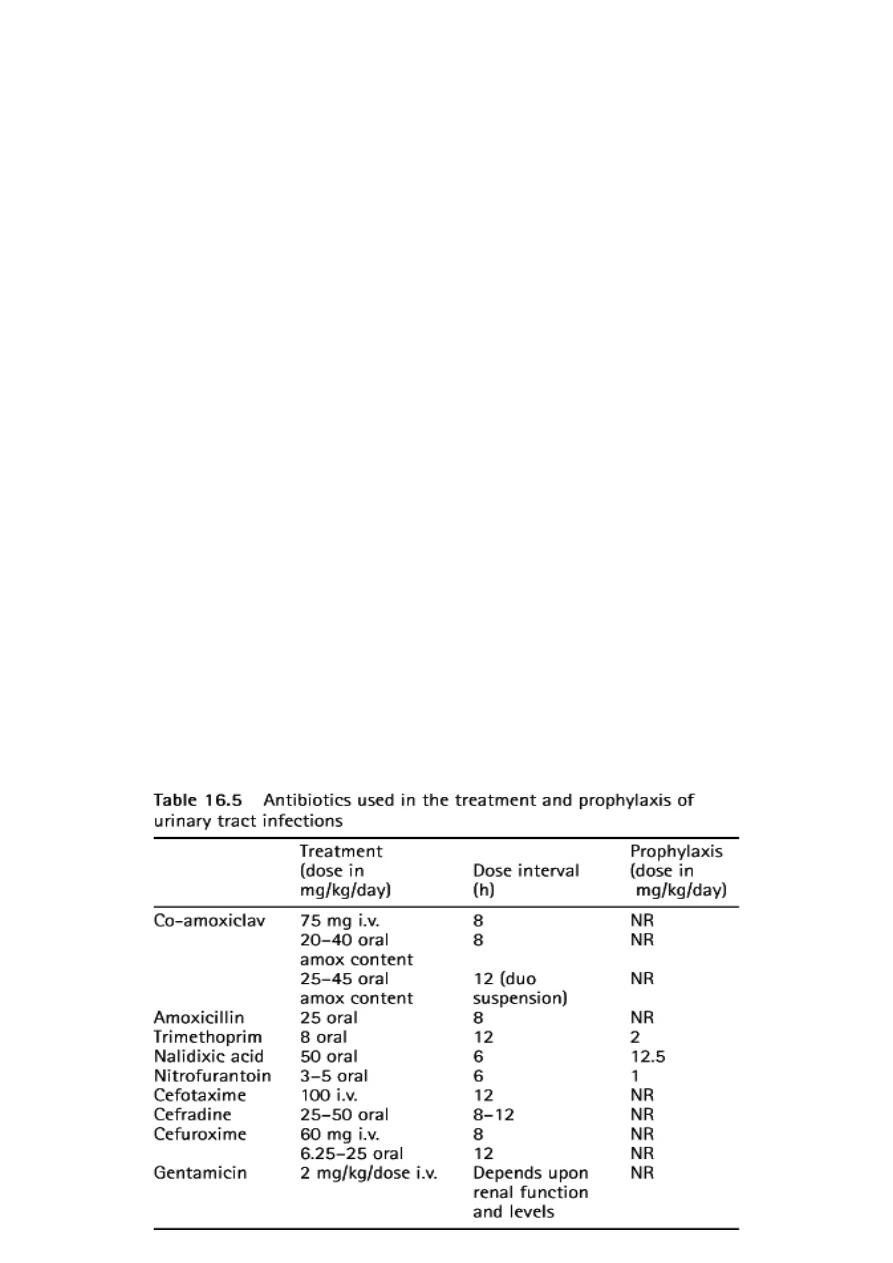
TREATMENT
Neonates with UTI are treated for 14 days with parenteral antibiotics because of the
higher rate of bacteremia.
Older children with acute cystitis are treated for 7 to 14 days with an oral antibiotic
Increasing bactearial resistance has limited the usefulness of some antibiotics such as
amoxicillin.
Oral third-generation cephalosporins such as cefixime and cefpodoxime are effective
Children with high fever or other manifestations of acute pyelonephritis often are
hospitalized for initial treatment with parenteral antibiotics as cefotaxime and
gentamicin or another aminoglycosid. Then after initial improvement therapy can be
continued orally for a total of 14 days

4
The degree of toxicity, dehydration, and ability to retain oral intake of fluids should be
assessed carefully.
Restoring or maintaining adequate hydration, including correction of electrolyte
abnormalities that are often associated with vomiting or poor oral intake, is
important.
Infants and children who do not show the expected clinical response within 2 days of
starting antimicrobial therapy should be re-evaluated, have another urine specimen
obtained for culture, and undergo ultrasound
COMPLICATIONS AND PROGNOSIS
Bacteremia occurs in 2% to 5% of episodes of pyelonephritis and is more likely in
infants than in older children. Focal renal abscesses are an uncommon complication
The relapse rate of UTI is approximately 25% to 40% Most relapses occur within 2 to 3
weeks of treatment. Follow-up urine cultures should be obtained 1 to 2 weeks after
completing therapy to document sterility of the urine
Prophylactic antibiotics should be administered until the VCUG has been completed
and the presence of reflux is known. TMP-SMZ (2 mg/kg TMP, 10 mg/kg SMZ) and
nitrofurantoin (1 to 2 mg/kg) given once daily at bedtime are recommended as
prophylactic agents, which, in contrast to amoxicillin and cephalosporins, are
associated with low rates of developing antibiotic resistance.
Clinical follow-up for at least 2 to 3 years is prudent, with repeat urine culture as
indicated.
Some experts recommend that follow-up urine cultures after recurrent cystitis or
pyelonephritis are obtained monthly for 3 months, at 3-month intervals for 6 months,
then yearly for 2 to 3 years.
Grade 1 to 3 reflux resolves at a rate of about 13% per year and is treated medically,
Grade 4 to 5 reflux resolves at a rate of about 5% per year and its treated surgically.
Bilateral reflux resolves more slowly than unilateral reflux
PREVENTION
Primary prevention is achieved by promoting good perineal hygiene and managing
underlying risk factors for UTI, such as chronic constipation, encopresis, and daytime
and nighttime urinary incontinence.
Secondary prevention of UTI with antibiotic prophylaxis given once daily is directed
toward preventing recurrent infections, although the impact of secondary prophylaxis
to prevent renal scarring is unknown
5
Prevention of urinary tract infections
Instruction to mothers:
Avoid constipation.
If your child has any problems with WORMS let the doctor know.
WIPING should be done in a front to back direction.
It is better to take a shower rather than a bath. Always avoid irritating soaps and
bubble baths. CLEANLINESS is very important to help prevent infection.
EMPTYING THE BLADDER PROPERLY IS VERY IMPORTANT.
Always encourage your child to DRINK as much as possible during the day, and to
EMPTY THE BLADDER PROPERLY LAST THING AT NIGHT.
CORRECT UNDERWEAR. Avoid tight underpants or pantyhose. They prevent air from
circulating freely and encourage the warm, moist environment which favors infection.
When taking antibiotics the full course must be taken at the time required.
Any PROBLEMS such as burning when passing water, going to the toilet often, or
blood in the water SHOULD BE REPORTED to the doctor.
When to Hospitalize
Treatment of suspected pyelonephritis in an infant younger than 3 months of age or
patients who have clinical urosepsis
Patients who have clinical pyelonephritis whose symptoms worsen despite 24 hours
of appropriate antibiotics
or those not significantly improved within 48 to 72 hours
For initiation of parenteral therapy if home treatment compliance is in question
