1
Lecture 02 Pathology D. Rasha
CARDIOVASCULAR SYSTEM
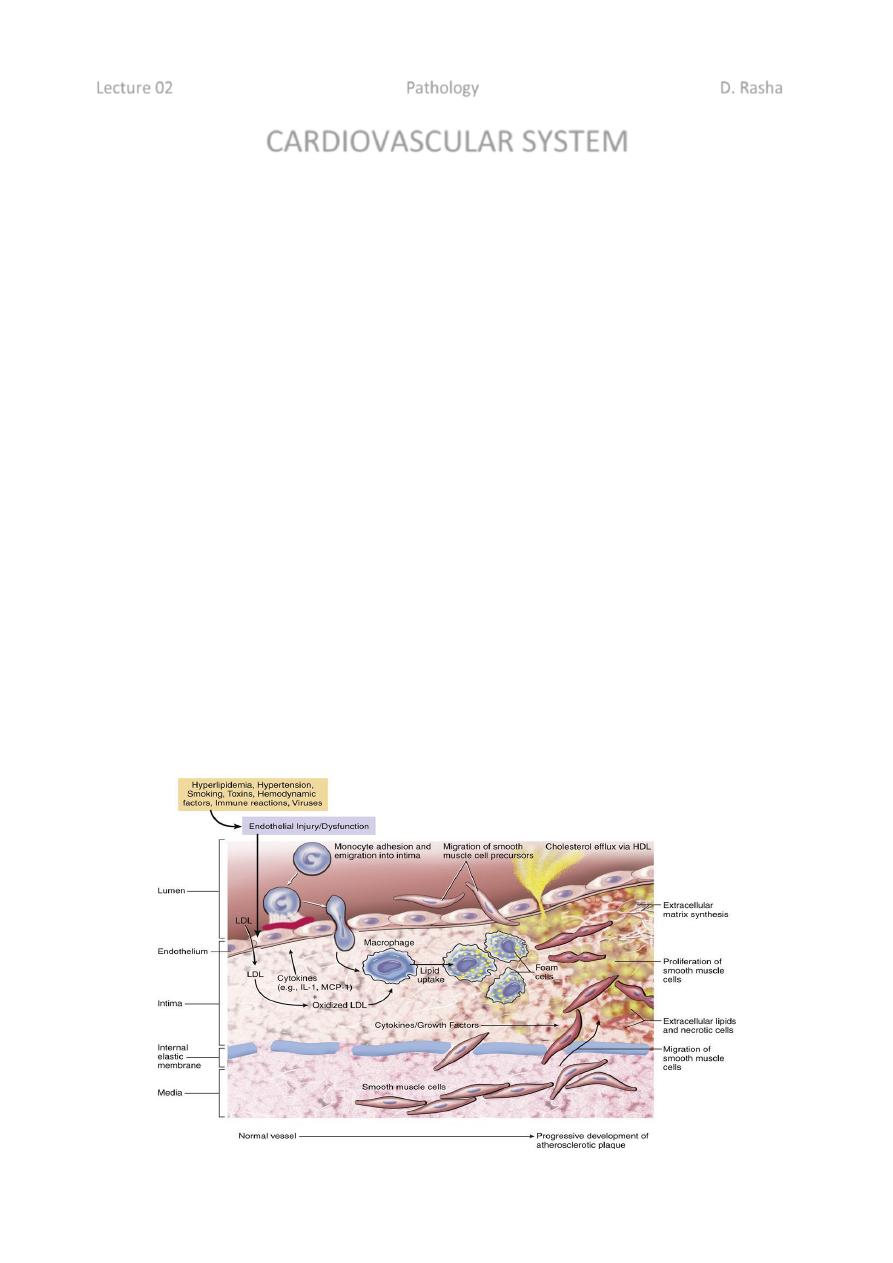
Pathogenesis:-
These are a number of hypotheses for pathogenesis of atherosclerosis, the most
important one is response- to- injury hypothesis which begins by chronic endothelial
injury from hyperlipidemia, HT, cigarette smoking, immune reaction, haemodynamic
factors, toxins and viruses, these factors cause increased endothelial permeability to:-
1- Lipoproteins especially LDL or modified LDL.
2- Circulating monocytes, leukocytes, T-lymphocytes and SMCs of intimal or
medial origin.
The monocytes after endothelial injury adhere and migrate between ECs to localized
subendothelially they transformed into macrophages and engulf the lipoproteins to
become foam cells, macrophages also proliferate in the intima. If injury continue,
platelets also adhere to the endothelium. SMCs some of medial origin also migrate in the
intima and take present lipids to transform into foam cells, the accumulation of these
foamy cells appear macroscopically as fatty streaks, the SMCs also synthesize collagen,
elastin and glycoproteins to form mature fibrofatty atheroma.
Thrombosis is a complication of late-stage atherosclerosis and organization of thrombi
may contribute to plaque formation, platelets generally do not adhere to the arterial wall
without severe injury of endothelial cells, Where the foam macrophages and SMCs died
the released extracellular lipid and cellular debris which surrounded by SMCs.
2
Morphology:-
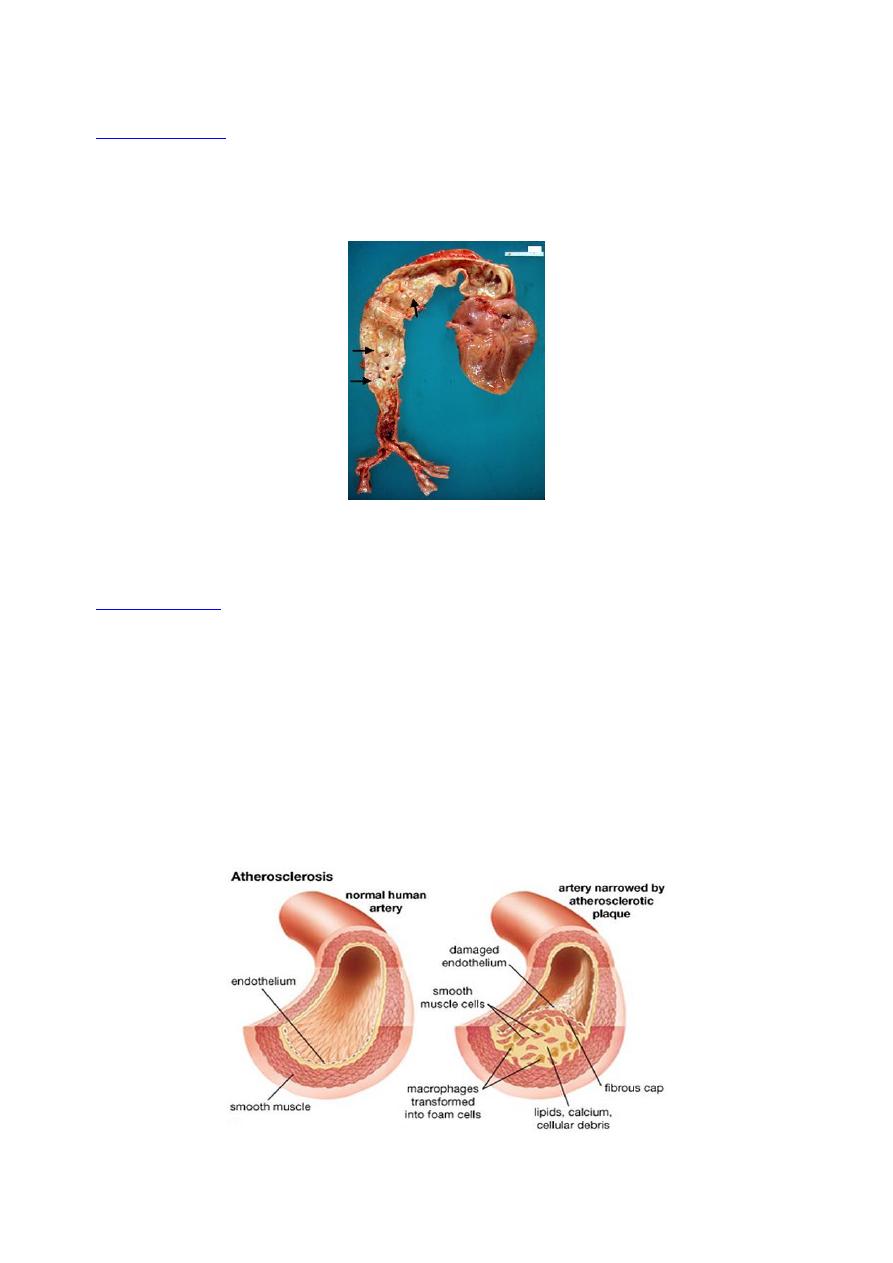
Macroscopically:-
The atheroma of aorta and large arteries occur in childhood as fatty
streaks in the 1
st
years of life, these begin as 1 mm, soft yellow intimal discolorations (fatty
dots) that progressively enlarge by becoming thicker and slightly elevated while they
elongate with long axis to produce fatty streaks 1-3 mm wide and 1-5 cm length.
The atheroma plaque appearance depending on the content of lipid, so it may be bright
yellow if lipid content more, or grey if fibrous tissue more.
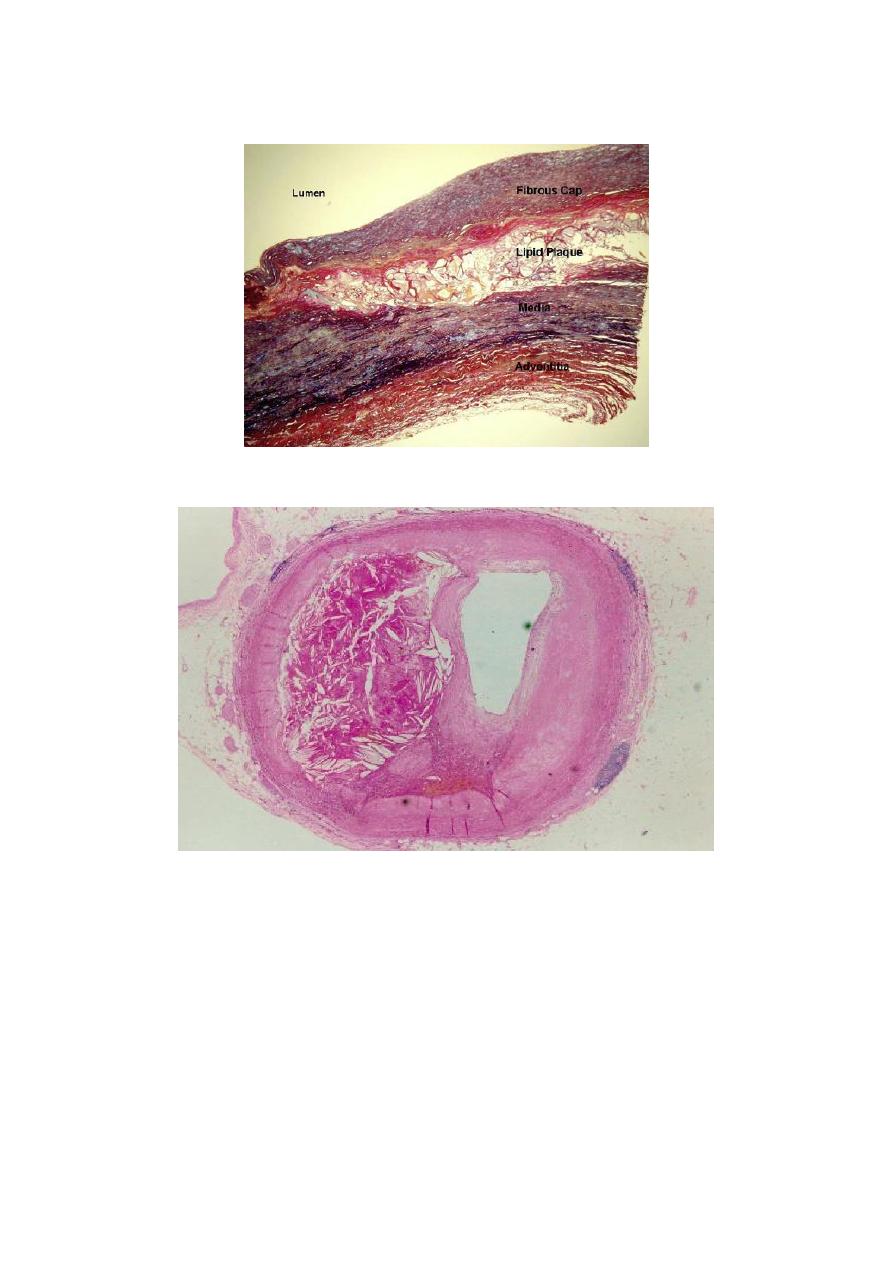
Microscopically:-
The plaques have essentially 3 components:-
1- Cells including vascular SMCs, blood derived monocytes/macrophages and
scattering of lymhpcytes.
2- Connective tissue fibers and matrix.
3- Lipids.
Some plaques contain relatively small amounts of lipids and are composing almost
entirely of connective tissue cells from fibrous plaque.
The extracellular lipid core composed of cholesterol (which forms needle-like crystals).
3
Some plaques contain relatively small amounts of lipids and are composing almost
entirely of connective tissue cells from fibrous plaque.
The extracellular lipid core composed of cholesterol (which forms needle-like crystals).
Plaques may develop 4 complications, these are:-
Ulceration
,
thrombosis
and
intraplaque hemorrhage
have serious consequences in
smaller vessels such as those of heart and brain and may cause
total occlusion
. In larger
vessels e.g. aorta, such complication have little effect on the luminal diameter by damage
the underlying media may cause atherosclerotic aneurysm as in distal aorta below renal
arteries.
4
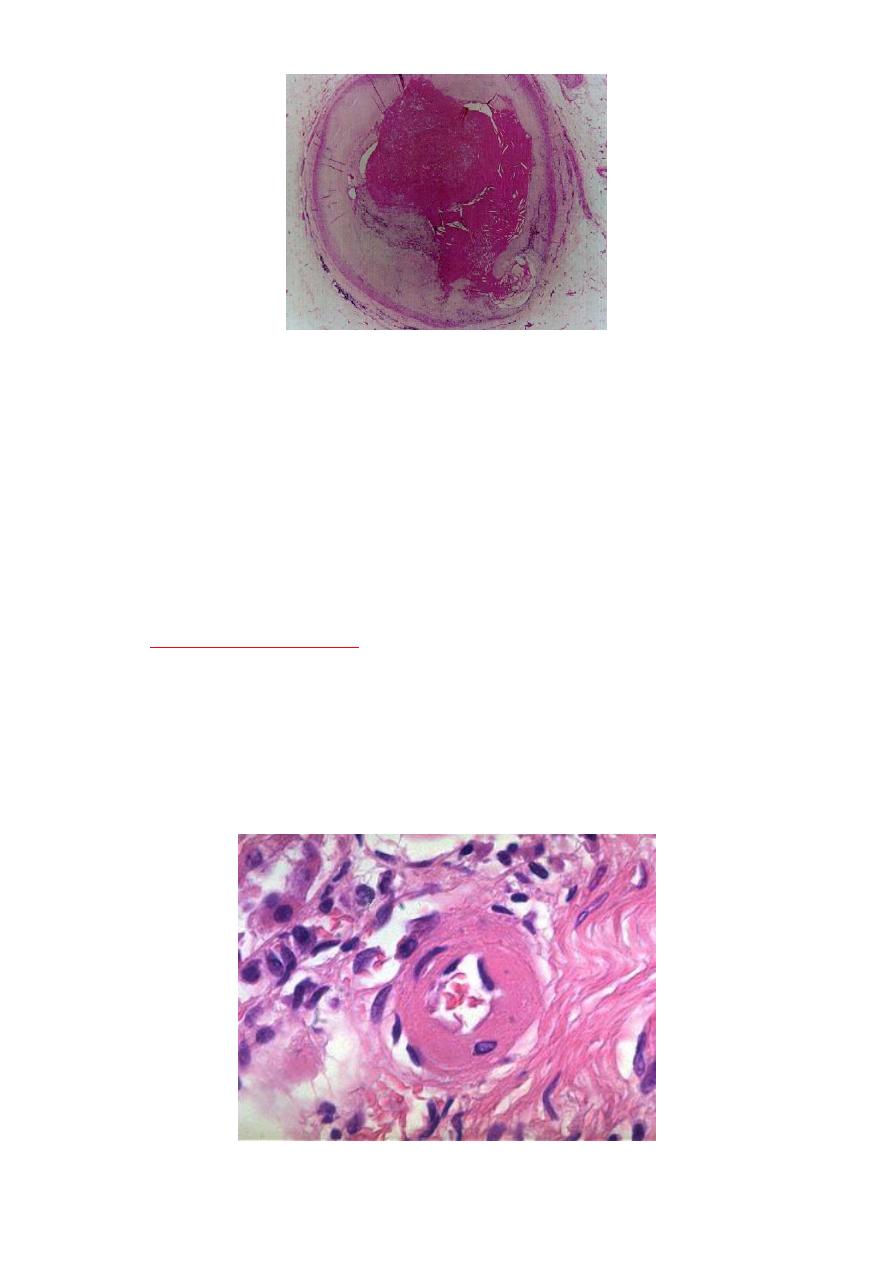
Hypertension and hypertensive vascular disease:-
Hypertension is associated with both functional and pathologic alteration , it's a common
disease and important risk factor in ischemic heart disease, CVA and congestive heart
failure.
Vascular pathology in hypertension:-
Hypertension is associated with 2 forms of small blood vessels disease:
1- Hyaline arteriolosclerosis.
2- Hyperplastic arteriolosclerosis.
Hyaline arteriolosclerosis:-
Seen in elderly patients who are hypertensive, diabetic and even normotensive but it's
more generalized and severe in hypertensive patients, the wall is consisting of
homogenous, pink, hyaline thickening of the walls of arterioles with narrowing of the
lumen.
5
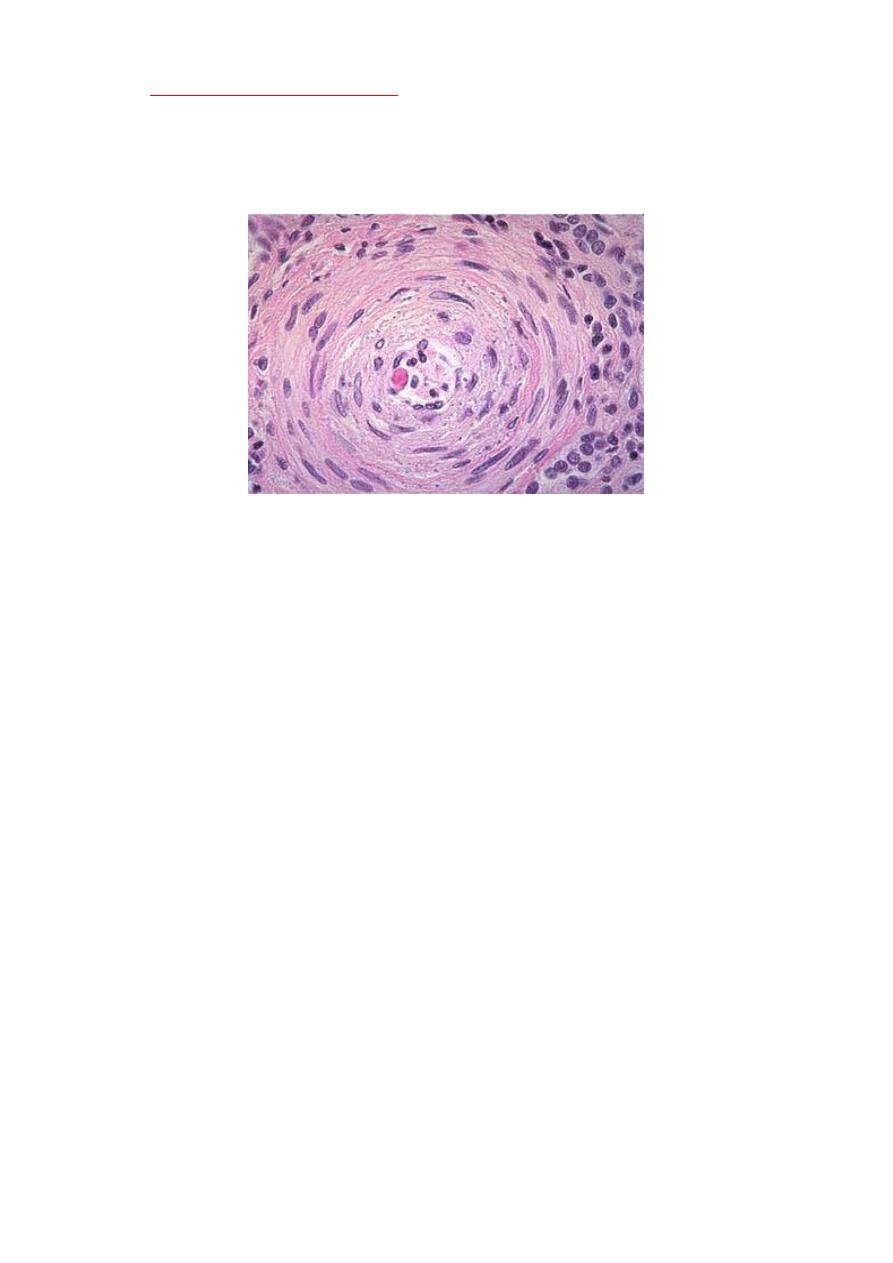
Hyperplastic arteriolosclerosis:-
This type occur in acute or severe elevations of blood pressure, this type seen in light
microscope by its concentric laminated, onion like, thickening of the lumen, there is
hypertrophy and hyperplasia of vascular SMCs and thickening of basement membrane.
Vasculitis:-
The term vasculitis is applied to any inflammatory involvement of an artery, vein
or venule, it's caused by infection, irradiation, mechanical trauma and arthus
reaction.
But systemic necrotizing vasculitis which induced by immune complexes, these
complexes found accumulate in vessel walls by deposition from circulation, by in
situ formation or by combination of these mechanism.
The classification of systemic vasculitis depend on the size of the involved blood
vessels, the anatomic site, the histologic characteristics of the lesion and the
clinical manifestations.
So the most common types of vasculitis.
1- Polyarteritis nodosa (PAN).
It's a disease of medium-sized to small arteries that's characterized by transmural
acute necrotizing inflammation of these vessels, any organ or tissue of the body
may be affected except lungs and aorta with its primary branches.
The clinical signs and symptoms are varied according to vascular involvement, as
malaise, fever, weakness and weight loss, but renal involvement is one of the
prominent manifestations, it's a major cause of hypertension and even death.
Clinical diagnosis depend on biopsy of suspected areas of involvement especially
kidney and skeletal muscles.
6
2- Wegener's granulomatosis:-
It's a disease of small to mdedium-sized arteries, the type of vasculiltis is necrotizing or
granulomatous, predominantly in the lungs but possibly else where.
This vasculitis is one of triad of Wegnere's granulomatosis which characterized by:
1. Necrotizing granuloma of upper or lower respiratory tract or both.
2. Vasculitis.
3. Necrotizing, often crescentric glomerulonephritis.
So that the clinical signs and symptoms very similar to PAN but the lung is involved.
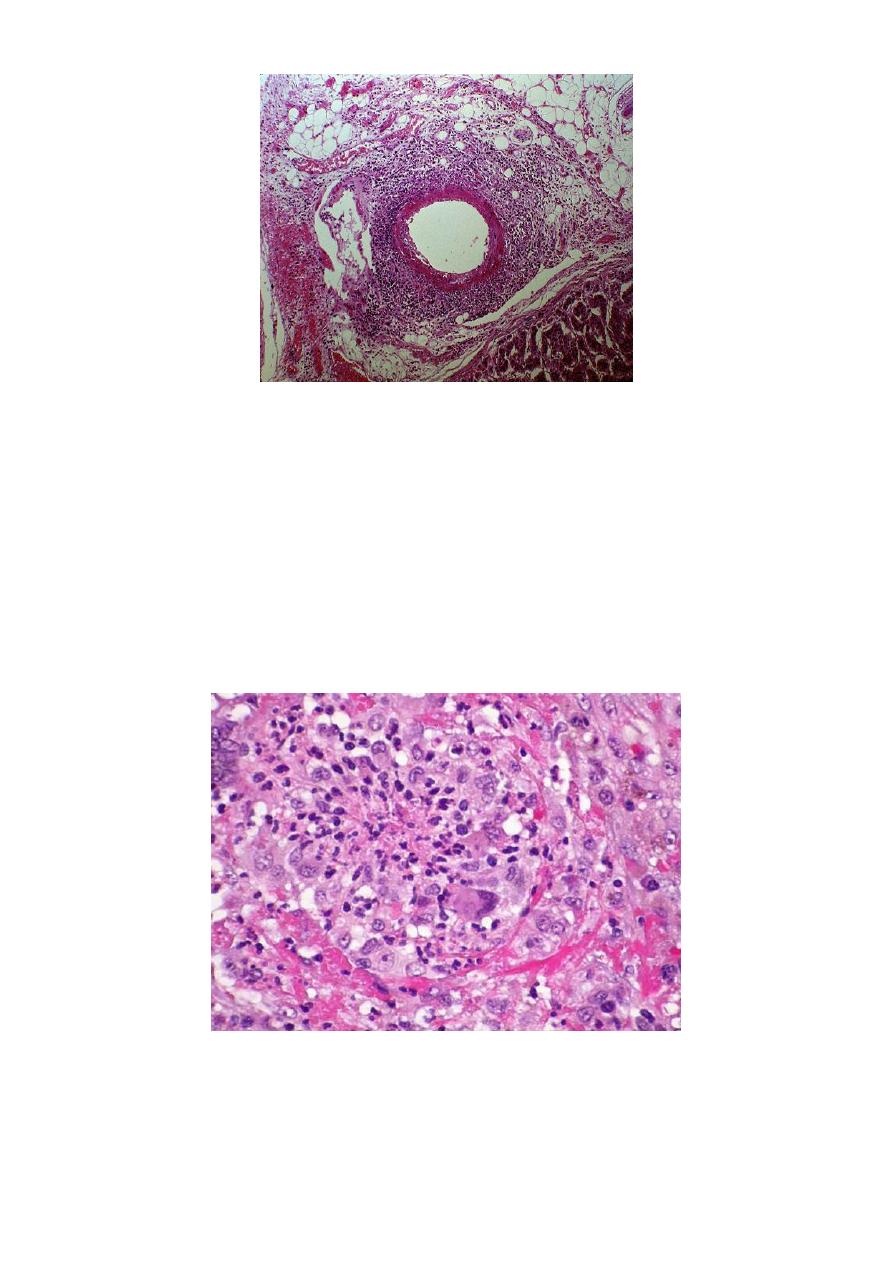
3- Microscopic polyangitis:-
This type of necrotizing vasculitis generally affects smaller vessels than PAN
(arterioles, capillaries and venules).

7
It's usually wide spread but especially the skin, necrotizing glomerulonephritis
and pulmonary capillaries are common.
So that clinical presentation includes:-
o Hemoptysis, hematuria, proteinuria, muscle pain or weakness and
palpable purpura.
4- Temporal( giant cell, cranial ) arteritis
It's segmental acute and chronic (most often granulomatous) vasculitis involve
larger arteries in the head especially the branches of the carotid artery as
temporal artery and ophthalmic artery, so it will cause unilateral or rarely
bilateral blindness, it's never involve the arteries of heart and lungs.
Clinical signs and symptoms characterized by facial pain, headache, which's
severe, sometimes unilateral, and often most intense along the course of the
superficial temporal artery, the vessel may be nodular and painful to palpation.
5- Kawasaki's disease:-
It's usually occur in small and medium-sized arteries, which occur in skin, ocular,
oral mucosa and coronary artery, it characterized by occurance as acute febrile
illness of infancy and early childhood, the disease is self limiting but the most
important complication, when involve coronary artery with formation of
aneurysm, thrombosis and death from M.I in 0.5 to 1% of cases.
The etiology supposed that in genetically susceptible persons with viral infection
there's activation of T-cells and macrophages and formation of autoantibodies to
endothelial and smooth muscle cells leading to acute vasculitis.
6- Thromboangitis obliterans (Buerger's disease):-
It's a disease of medium-sized and small arteries and veins which is characterized
as a remitting, relapsing, inflammatory disorder lead to thrombosis of extrimiteis
and secondary extension to adjacent veins and nerves.
It's usually occur in male cigarette smokers which will cause vascular insufficiency
and gangrene.
Its etiology occur from direct endothelial toxicity of tobacco or in indirect
immunologic reaction in predisposed persons.
The wall of involved blood vessel usually acute and chronic inflamed
accompanied by thrombosis, the thrombosis characteristically contain small
microabscesses.
