1
Fifth stage
Dermatology
Lec-21
.د
عمر
18/4/2016
Urticaria
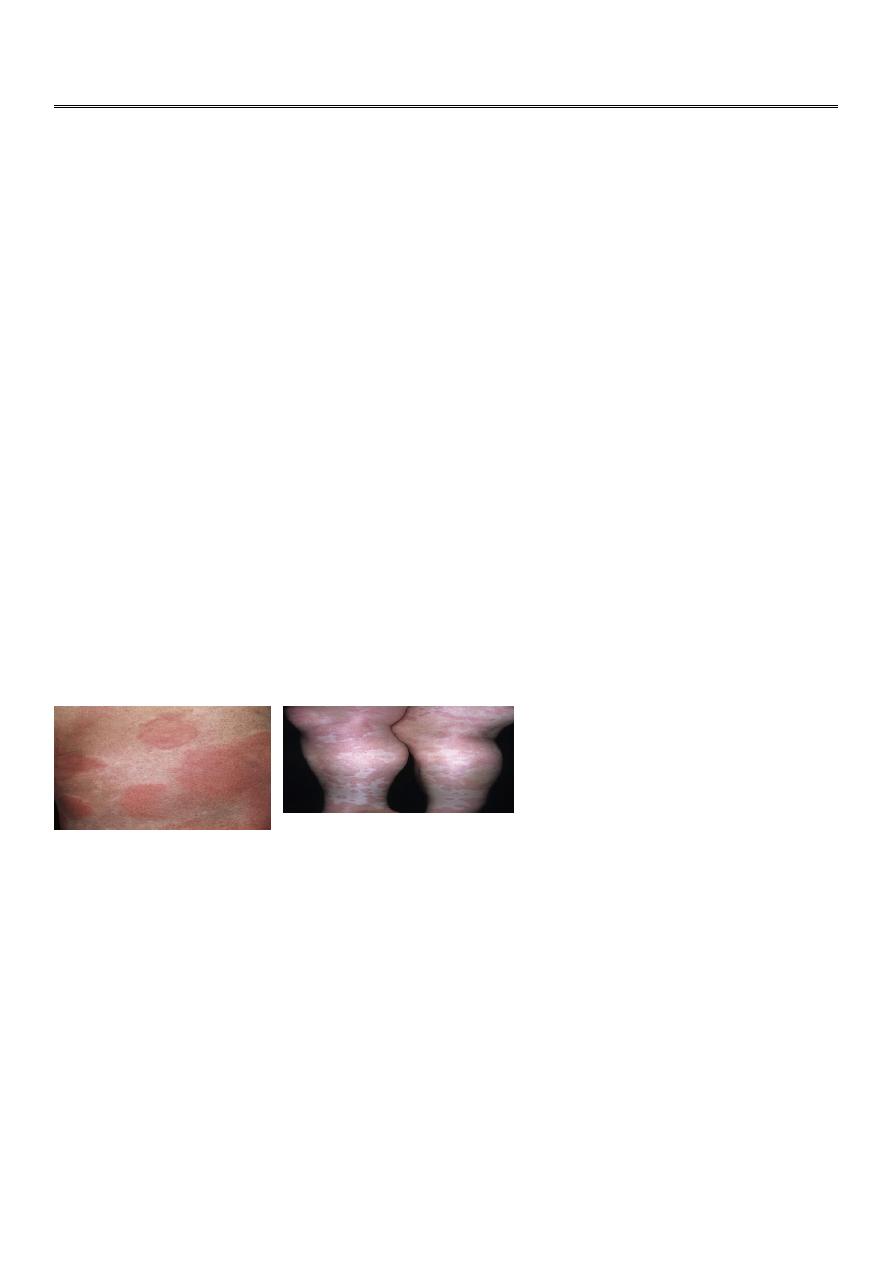
Urticaria: also referred to as hives or wheals, is a common and distinctive reaction pattern.
Hives may occur at any age
20% of the population will have at least one episode.
Urticaria is classified as: acute(less6wk) or chronic(more 6wk).
Angioedema frequently occurs with acute urticaria, which is more common in children and
young adults. while Chronic urticaria is more common in middle-aged women and
commonly accompanies angioedema.The cause of acute urticaria is known in many cases.
While The cause of chronic urticaria is determined in less than 5% to 20% of cases.
The evolution of urticaria is a
dynamic
process = new lesions evolve as old ones resolve.
Hives result from localized capillary vasodilation, followed by transudation of protein-rich
fluid into the surrounding tissue; they resolve when the fluid is slowly reabsorbed.The
edema in urticaria is found in the superficial dermis. while Lesions of angioedema are less
well demarcated and the edema is found in the deep dermis or subcutaneous/submucosal
locations.
(itchy ,red,temporary edematous papule or plaque)
Clinical Classification of Urticaria/Angioedema:
مهم
1. Ordinary urticaria (recurrent or episodic urticaria not in the categories
2. Physical urticaria (defined by the triggering stimulus):
Adrenergic urticaria
Aquagenic urticaria
Cholinergic urticaria
Cold urticaria
Delayed pressure urticaria
Dermographism

2
Exercise-induced anaphylaxis
Localized heat urticaria
Solar urticaria
Vibratory angioedema
3. Contact urticaria (induced by biologic or chemical skin contact)
4. Urticarial vasculitis (defined by vasculitis as shown by skin biopsy)
5. Angioedema (without wheals)
Duration of hives???
PATHOPHYSIOLOGY: Histamine is the most important mediator of urticaria.Histamine is
produced and stored in mast cells. A variety of immunologic, nonimmunologic, physical,
and chemical stimuli cause histamine release which causes localized capillary
vasodilatation, which allows vascular fluid to leak between the cells through the vessel wall,
contributing to tissue edema and wheal formation.
The “triple response” of Lewis???
Flush:capillary dilatation
Flare:arteriolar dilatation
Weal:exudation,edema
Blood vessels contain two (and possibly more) receptors for histamine. The two most
studied are H1 and H2.
ACUTE URTICARIA :
If the urticaria has been present for( less than 6 weeks), it is considered acute.
ETIOLOGY:مثال( مهمة+مسا)
1. IgE-MEDIATED REACTIONS : Circulating antigens such as foods, drugs, insect stings,
natural rubber latex or inhalants interact with cell membrane–bound IgE to release
histamine.
2. COMPLEMENT-MEDIATED, OR IMMUNE-COMPLEX-MEDIATED, ACUTE URTICARIA :
Administration of whole blood, plasma, immunoglobulins, and drugs or by insect stings.
3.NONIMMUNOLOGIC RELEASE OF HISTAMINE: Acetylcholine, opiates, polymyxin B, and
strawberries, aspirin/NSAIDs.
3
CHRONIC URTICARIA (
الفرق عنacute)
1.Patients who have a history of hives lasting for( 6 weeks or more) are classified as having
chronic urticaria (CU).
2.The Etiology is often unclear.
3.The morphology is similar to that of acute urticaria but lesions are slightly deeper.
4.CU is more common in middle-aged women and is infrequent in children.
Individual lesions remain for less than 24 hours but the diasease continues for weeks,
months, or yearsl
مهم اكثر من
6
اسابيع
5.Angioedema occurs in 50% of cases and rarely affects the larynx.
6.About 70% of patients with CU have physical urticarias. Aspirin/NSAIDs, penicillin, ACEIs,
opiates, alcohol, fever, and stress exacerbate CU.CU also results from the cutaneous mast
cell release of histamine.Over 30% of CU patients have autoimmune phenomena: positive
autologous serum skin tests, antibodies to the alpha subunit of the basophil IgE receptor
and to IgE, and thyroid autoimmunity.There is a significant association between chronic
urticaria and autoimmune thyroid disease. Most patients are women. Most patients are
asymptomatic and have thyroid function that is normal or only slightly abnormal.
Evaluation and management of acute & chronic urticarial:
1.History and physical examination
2.Lab. Tests: Allergen testing
3.Rx [1st (Antihistamines), 2nd (oral steroids) and 3rd (IV Ig) line agents]
Other measures
PHYSICAL URTICARIAS
Physical urticarias are induced by physical and external stimuli.They typically affect young
adults.
More than one type of physical urticaria can occur in an individual.
Provocative testing confirms the diagnosis.Most physical urticaria forms persist for about 3
to 5 years or longer.
Duration of individual lesions?
4
Dermographism
(Most frequent) Stroking the skin, toweling, clothing.
Starts in minutes, lasting 2-3 hours.
Clinically: irregular pruritic wheals. No systemic symptoms
Testing (Darier’s sign)
Rx : anti histamine
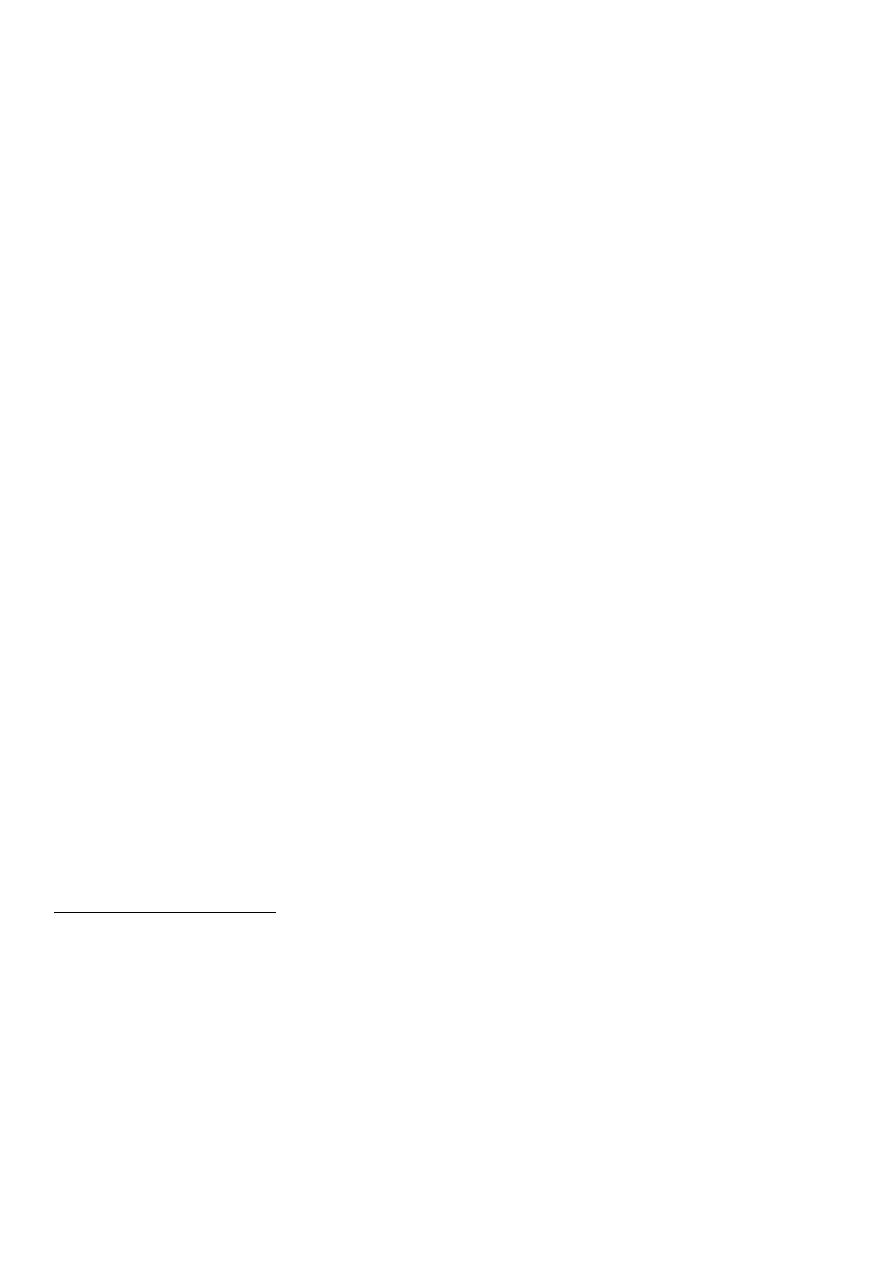
Delayed pressure urticaria
(Frequent) Prolonged pressure (belt, bra, manual work, standing, sitting on a hard surface).
Starts within 3-12 hrs. lasting 4-36 hrs.
Clinically: diffuse tender swelling. Flu-like symptoms
Testing? Pressure challenge test
Rx : oral steroids
Cholinergic urticaria
(Very frequent) General overheating of body
Starts in 2-20 minutes, lasting ½ - 2 hour.
Clinically: tiny papular pruritic wheals. Anaphylaxis and angioedema may occur.
Testing: exercising.
Rx:anti histamine like danazole
ANGIOEDEMA
Angioedema AE (angioneurotic edema) is a hive-like swelling caused by increased vascular
permeability in the subcutaneous tissue of the skin and mucosa and the submucosal layers
of the respiratory and GI tracts.
Hives and angioedema commonly occur simultaneously.
Syndromes of Angioedema: (
اسبابAE)
Idiopathic recurrent AE
Allergic (IgE-mediated) angioedema
5
Medication-induced (e.g., ACE inhibitors)
HAE (hereditary angioedema):
1. Type I: deficiency of C1 INH protein
2. Type II: dysfunctional C1 INH protein
3. Type III: coagulation factor XII gene mutation
AAE (acquired angioedema):
1. Type I: associated with lymphoproliferative diseases
2. Type II: autoimmune (anti–C1 INH antibody)
Episodic angioedema with eosinophilia (Gleich’s syndrome)
Thyroid autoimmune disease–associated AE
Hereditary angioedema : Type 1 is the most common and results from a lack of functional
C1 esterase inhibitor causing plasma kallikrein activation, which leads to the production of
the vasoactive peptide
bradykinin
. Transmitted as an autosomal dominant trait.The
disease affects between 1 in 10,000 and 1 in 50,000 persons.
The disease begins in late childhood or early adolescence.
Many have ancestors and family members who died suddenly from
asphyxia
.
Mortality rate can reach up to 30%.Patients live in constant dread of life-threatening
laryngeal obstruction which occurs in about 65% of cases.Minor trauma, mental stress, and
other unknown triggering factors lead to the release of vasoactive peptides that produce
episodic swelling.
Histamine has
no role
in this type.
Clinical presentation? Swelling hands &face ,colicky abd. Pain(acute abd)
Young age, fhx of death+ ,not respond to anti histamine,no urticarial only edema
Investigations
C1 INH (quantity and function) low, C4 low
C1q normal , 24 hr urine histamine normal , tryptase normal.
Treatment:
Acute attacks (C1 INH conc., danazol, tranexamic acid, FFP)
Prophylaxis (danazol, tranexamic acid)
