PHARMACOLOGY
Dr. Husam Aldeen Salim AlnajarAtropine
Characteristics of AtropineSource
Atropa belladonna
Chemical nature
An alkaloid
ANTIMUSCARINIC AGENTS
BELLADONNAALKALOIDS
• ATROPINE
• SCOPOLAMINE
TX: USED WHEN A REDUCTION OF PARASYMATHETIC
TONE IS DESIRABLE
• PREOP TO REDUCE SALIVATIONS / BRONCHIAL SECRETIONS
• REDUCE INTESTINAL MOTILITY
• TREAT OVERACTIVE BLADDER
• OPHTHALMOLOGICAL EXAMINATIONS
• PREVENTING MOTION SICKNESS
• TREAT ASTHMA
• TREAT POISONING BY AChE INHIBITOR
Effect Of Atropine in Relation to Dosage ...
DOSE EFFECT
0.5 mg Slight decline in heart rate
Some dryness of mouth
Inhibition of sweating
DOSE EFFECT
1.0 mg Definit dryness of mouthThirst
Inreased heart rate, sometimes preceded by slowing
Mild dilatation of pupil
DOSE EFFECT
2.0 mg Rapid heart ratePalpitation
Marked dryness of mouth
Dilated pupils
Some blurring of near vision
DOSE EFFECT
5.0 mg All the previous symptoms are markedDifficulty in speaking and swallowing Restlessness and fatigue
Headache
Dry hot skin
Difficulty in micturition
Reduced intestinal peristalsis
DOSE EFFECT
10 mg Previous symtoms are more marked
and more Pulse, rapid and weak
Iris practically obliterated
Vision very blurred
Skin flushed, hot, dry, and scarlet
Ataxia
Restlessness and excitement
Hallucinations and delirium
Coma
ATROPINE: OVERVIEW OF TOXIC ACTIONS
DRY AS A BONE HOT AS A PISTOL
RED AS A BEET
BLIND AS A BAT
MAD AS A HATTER
Therapeutic Uses of Antimuscarinic Agents
Cardiovascular System - atropine is generally used for the following casesSinus or nodal bradycardia in cases of excessive vagal tone associated with myocardial infarct
Hyperactive carotid sinus (syncope and severe bradycardia)
Second degree heart blockGastrointestinal Tract
Peptic ulcersM1 muscarinic receptor antagonists such as pirenzepine and telenzepine are used
Spasticity of the g.i. tract
Excessive salivation associated with heavy metal poisoning and parkinsonism
Production of partial blockade of salivation in patients unable to swallowUrinary Bladder
Reverse spasm of the ureteral smooth muscle (renal colic)Increase bladder capacity in cases of enuresis
Reduce urinary frequency in cases of hypertonic bladderCentral Nervous System
Parkinson’s disease
Motion sickness
Anesthesia, to inhibit salivation
Prevent vagal reflexes induced by surgical manipulation of organs
Posioning by inhibitors of acetylcholinesterase
Mushroom poisoning due to muscarine
In conjunction with inhibitors of acetylcholinesterase when they are used to promote recovery from neuromuscular blockade after surgery
Prevent vagal reflexes induced by surgical manipulation of visceral organs
Drugs of Other Classes With Antimuscarinic Activity
Tricyclic antidepressantsImipramine
Amitriptyline
Protriptyline
Phenothiazine Antipsychotic Agents
Chlorpromazine & Thioridazine
H1 Histamine receptor blocking agents
Diphenhydramine
Promethazine
Chlorpheniramine
Cyproheptadine
Contraindications to the Use of Antimuscarinic Agents
Narrow angle glaucomaHypertrophy of the prostate gland
Atony of the bladder
Atony of the G.I. Tract
NE
1, 2, 1
Adrenergic Receptors
ACh
ACh
ACh
CNS
C
T
L
S
SM
ACh
ACh
N
N
ACh
M
ACh
CNS
C
T
L
S
SM
ACh
N
ACh
NE
N
N
ACh
M
ACh
CNS
C
T
L
S
SM
ACh
NE
N
ACh
NE
N
1
21
N
ACh
M
ACh
CNS
C
T
L
S
SM
ACh
NE
N
ACh
NE
N
ACh
EPI
N
1
2
1
N
ACh
M
ACh
CNS
C
T
L
S
ACh
NE
SM
N
NE
EPI
1, 2, 1, 2
1, 2, 1
Adrenergic Receptors
Differences between autonomic and somatic nervesAutonomic:
- Synapses located in ganglions outside cerebrospinal axis- Extensive peripheral plexuses
- Postganglionic nerves are not myelinated
- Some level of spontaneous activity without intact innervation
Somatic:
- Innervates all organs/glands except skeletal muscle
- Innervates only skeletal muscle
- Synapses within CNS
- Does not form peripheral plexuses
- myelinated
- Denervation results in paralysis, atrophy
Differences between functions of the
parasympathetic and sympathetic nervous system
Parasympathetic:
- Bradycardia- Salivation increased
- Vasodilator predominance
- Blood pressure reduced
Sympathetic:
- Conservation of energy
- Urine output increased
- Respiration reduced
- GI motility and secretions increased
- Renal blood flow increased
- Expenditure of energy
- Tachycardia
- Vasoconstrictor predominance
- Blood pressure increased
- Renal blood flow decreased
- Salivation reduced
- Urine output decreased
- Respiration increased
- GI motility and secretions reduced
• SITE EFFECT
•
•
•
•
•
EFFECTS OF STIMULATING MUSCARINIC RECEPTORS (SLUDE)
BRONCHOSPASM
BRADYCARDIA
VASODILATION
MIOSIS
INCREASED URINATION
INCREASED GI MOTILITY
INCREASED SALIVATION
INCREASED TEARS
LACRIMAL GLANDS
SALIVARY GLANDS
GI TRACT
BLADDER
IRIS
AIRWAYS
VASCULATURE
HEART
SWEAT GLANDS
INCREASED SWEATNG
1, 2
vasoconstriction
TPR
contractile force
heart rate
1
2
vasodilation,TPR
EFFECTS OF STIMULATING ADRENERGIC RECEPTORS
• SITE EFFECT•
•
•
•
•
•
EFFECTS OF STIMULATING ADRENERGIC RECEPTORS
BRONCHORELAXATION (2)
TACHYCARDIA (1)
VASODILATION
MYDRIASIS (2)
DECREASED URINATION (2)
DECREASED GI MOTILITY (2)GI TRACT
BLADDERIRIS
AIRWAYS
VASCULATURE
HEART
(2)
VASOCONSTRICTION
(1, 2)
UTERUS
RELAXATION (2)
Dual Innervation
Predominant ToneExceptions -
Primarily parasympathetic NS
blood vessels
(only sympathetic)
Exceptions -
blood vessels (sympathetic)
- sweat glands (sympathetic
cholinergic)
Predominate Autonomic Tone
Arterioles Sympathetic (adrenergic)Veins Sympathetic (adrenergic)
Heart Parasympathetic (cholinergic)
Iris Parasympathetic (cholinergic)Ciliary muscle Parasympathetic (cholinergic)
GI tract Parasympathetic (cholinergic)
Urinary bladder Parasympathetic (cholinergic)
Salivary glands Parasympathetic (cholinergic)
Sweat glands Sympathetic (cholinergic)
Site
Predominate Tone
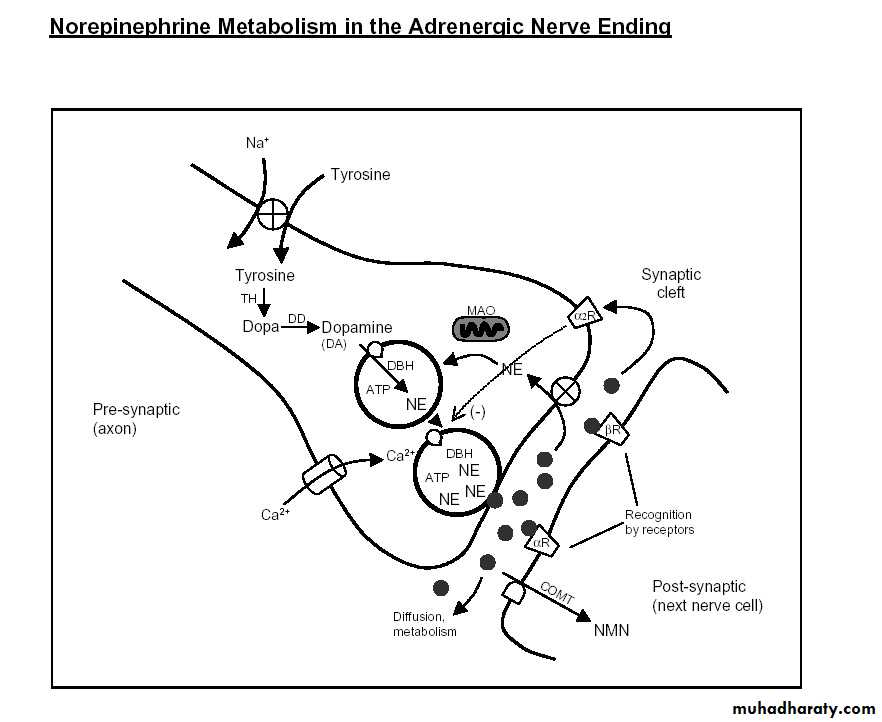
PRESYNAPTIC
POSTSYNAPTICNE
Re-uptake 1
Metabolic RemovalAction
/
ReceptorBinding
NE synthesis
NE
COMT
MAO
Re-uptake 2
(-)
NE - predominately removed from synapse via re-uptake 1
21, 2
vasoconstrictionTPR
contractile force
heart rate
1
2
vasodilation,TPR
renin release
MIXED ADRENERGIC AGONISTS
NorepinephrineEpinephrine
1, 2, 1, 2
1, 2, 1
Dopamine
DA, 1, 1
MIXED ADRENERGIC AGONISTS
Norepinephrine (1, 2, 1)Epinephrine (1, 2, 1, 2)
Dopamine (DA, 1, 1)
Tx: ● Asthma (but there are better drugs)
Tx: ● CHF
● Anaphylactic shock,
● Cardiogenic shock
● Prolong action of local anesthetics
● Topical hemostatic agent
ALPHA AGONISTS
- Phenylephrine (1)
- Oxymetazoline (1 and 2 in periphery)
- Ephedrine/Pseudoephedrine (1)
- Clonidine (2, Tx site of action is CNS)
- Methoxamine (1)
- Tetrahydrozoline (1)
- Naphazoline (1)
BETA AGONISTS
• Non-selective 1/2• Isoproterenol
• Selective 1
• Dobutamine
Selective 2
Albuterol
Terbutaline
Isoetharine
Metaproterenol
Bitolterol
Ritodrine
ACh
NE
N
1
2
1
N
ACh
M
ACh
CNS
C
T
L
S
ACh
NE
SM
N
Adrenergic Antagonists
EPI
N
ACh
X
X
X
ALPHA ANTAGONISTS
- Phentolamine- Prazosin
- Terazosin (water soluble)
- Phenoxybenzamine
Used in pts with pheochromocytoma
Nonselective 1 and 2 receptor antagonists
Selective 1 receptor antagonists
Used Tx as antihypertensive agents
NE
Re-uptake 1
Vasoconstriction1
Phentolamine - 1 and 2 blockade Prozosin - 1 blockadeNE
(-)
Effects of Alpha-Receptor Blockade on
Vascular Smooth Muscle Tone2
VSMCVasodilation
Vasodilation
● Non-selective 1, 2
BETA ANTAGONISTS
● ‘Cardio’- Selective 1
Propranolol
Nadolol
Timolol
Pindolol
Carteolol
Intrinsic
Sympathomimetic
Activity
Atenolol
Metropolol
Esmolol
Acebutolol (ISA)
● Non-selective
1, 2, 1
Labetalol
CarvedilolINDIRECT ACTING ADRENERGIC
AGONISTSTyramine (dietary substance)
Cocaine
Tricyclic AntidepressantsUptake Blockers
PRESYNAPTIC
POSTSYNAPTIC
NE
Re-uptake 1
Action /
ReceptorBinding
NE
Cocaine
PRESYNAPTICPOSTSYNAPTIC
Re-uptake 1
Action /
Receptor
Binding
NE
Cocaine
NEX
cocaine
Guanethadine
Inhibits NE release, also causes NE depletion, and can damage NE neuronsNeuronal Blockers
Reserpine
Depletes NE stores by inhibiting vesicular uptake of NE, NE then metabolized by intra-neuronal MAO
Pargyline
Monoamine Oxidase (MAO) InhibitorsTranylcypromine
Tyramine (or other drugs that promote NE release) may cause markedly increased blood pressure in patients taking MAO inhibitors