Immunity and infection
IntroductionThe development of an infectious disease in an individual involves complex interactions between the microbe and the host. The key events during infection include:
entry of the microbe
invasion and colonization of host tissues
evasion of host immunity
tissue injury or functional impairment
Microbes produce disease by:
directly killing the host cells they infect, or
liberating toxins that can cause tissue damage and functional derangements in neighboring or distant cells and tissues that are not infected, or
stimulating immune responses that injure both the infected tissues and normal tissues.
General Features of Immune Responses to Microbes
Defense against microbes is mediated by the effector mechanisms of innate and adaptive immunity.The immune system responds in specialized and distinct ways to different types of microbes to most effectively combat these infectious agents.
The survival and pathogenicity of microbes in a host are critically influenced by the ability of the microbes to evade or resist the effector mechanisms of immunity.
The extracellular bacteria
Extracellular bacteria defined as the bacteria that capable to replicate outside the host cells, e.g. in blood, connective tissue, airway/gastrointestinal tractThe bacteria may either
1) induce inflammation or
2) produce toxins that destruct the body tissue
E.g. of toxin: Endotoxin of gram-negative or lipopolysaccharide (LPS).
Innate immunity to extracellular bacteria
Principles:Complement activation
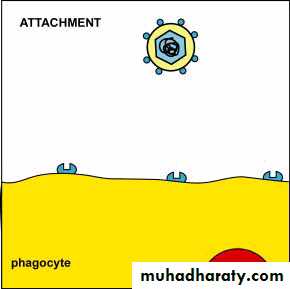
Activation of phagocytes and inflammatory responseNonspecific immune system
The complement systemThe complement system is a primary mediator of the humoral immune response that enables the body to produce an inflammatory response, lyse foreign cells, and increase phagocytosis.
The complement system, consists of a group of proteins that normally are present in the circulation as functionally inactive precursors. These proteins make up 10% to 15% of the plasma protein fraction.
For a complement reaction to occur, the complement components must be activated in the proper sequence.
Uncontrolled activation of the complement system is prevented by inhibitor proteins.
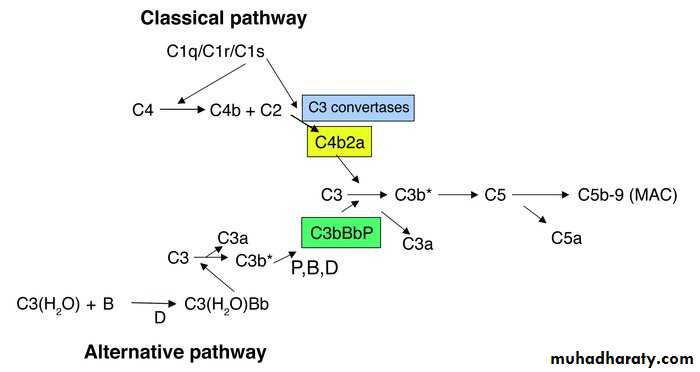
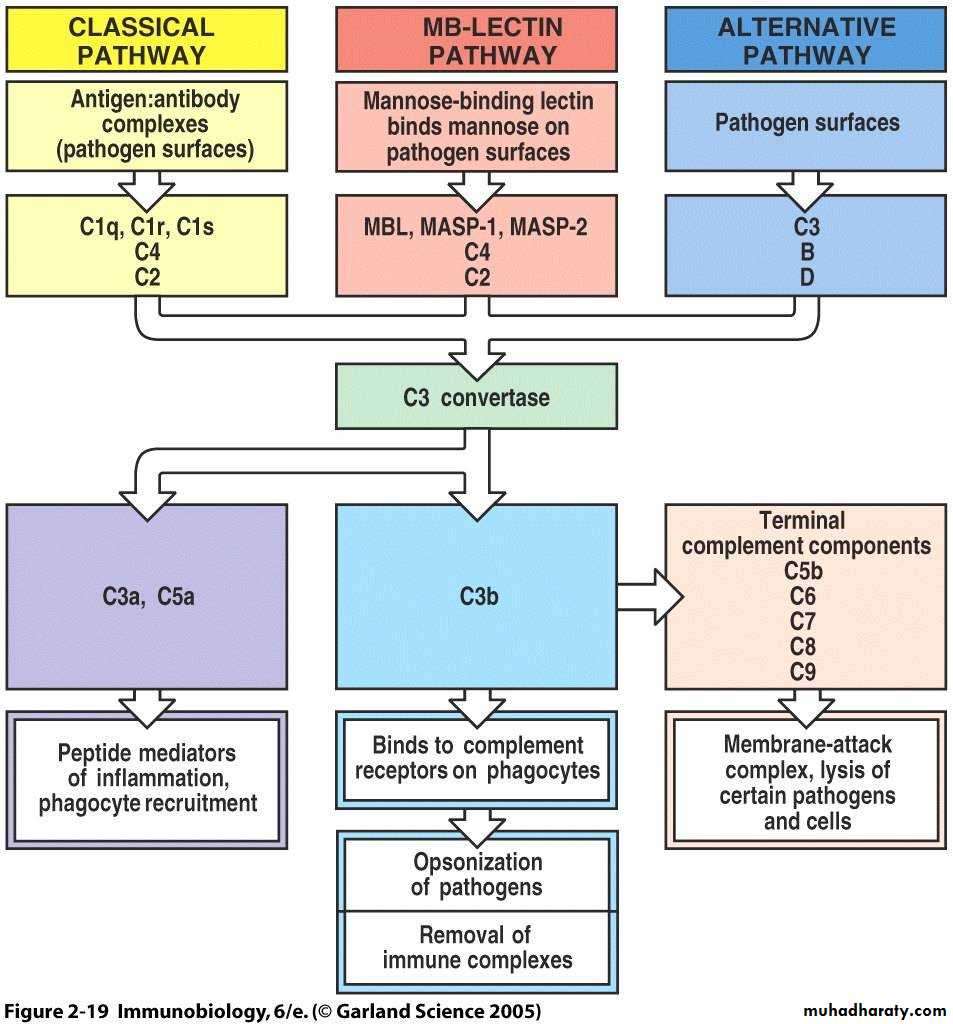
Complement activation
The classic pathway of complement activation is initiated by
antibody bound to antigens on the surface of microbes.
The alternate and the lectin pathways do not use antibodies and are part of the innate immune defenses.
The alternate pathway of complement activation is initiated by the interaction with certain polysaccharide molecules characteristic of bacterial surfaces.
The lectin-mediated pathway is initiated following the binding of a mannose-binding protein to mannose-containing molecules commonly present on the surface of bacteria and yeast.
The activation of the three pathways produces similar effects on C3 and subsequent complement proteins.
Complement activation
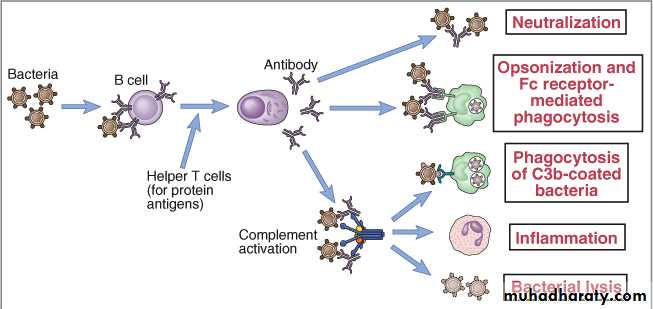
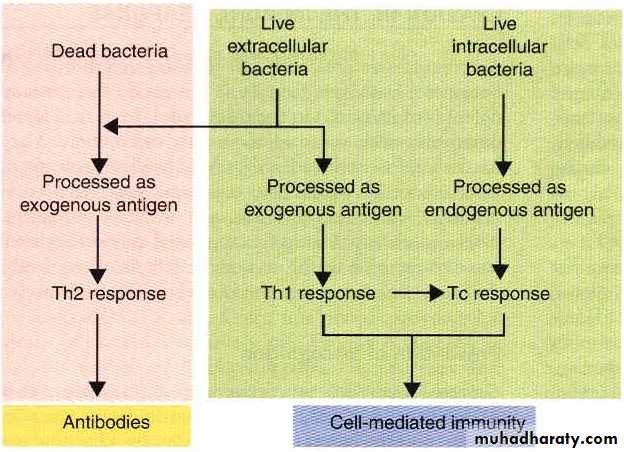
Classic PathwayAdaptive immunity to extracellular bacteria
Humoral immunity: block infection, eliminate microbes and neutralize toxins
The B-cell response to antigens has two stages:
Primary immune response:
When B cells first encounter an antigen, the antigen attaches to a receptor, stimulating the B cells.
Some B cells change into memory cells, which remember that specific antigen, and others change into plasma cells. Helper T cells help B cells in this process.
Plasma cells produce antibodies that are specific to the antigen that stimulated their production. After the first encounter with an antigen, production of enough of the specific antibody takes several days. Thus, the primary immune response is slow.
Secondary immune response
Whenever B cells encounter the antigen again, memory B cells very rapidly recognize the antigen, multiply, change into plasma cells, and produce antibodies. This response is quick and very effective.Primary and secondary phases of the humoralimmune response to the same antigen.
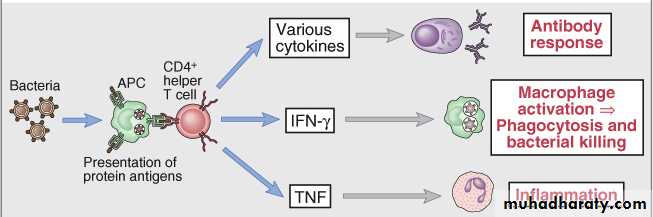
Humoral ImmunityCellular Immunity
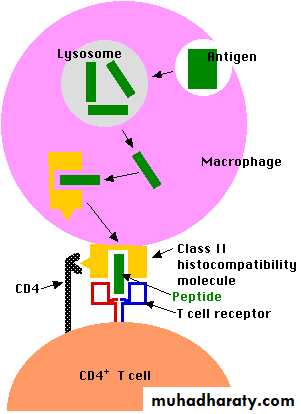
• D4+ produces cytokines that induce local inflammation and activate phagocytic function and microbicidal activities of Macrophages and Neutrophiles
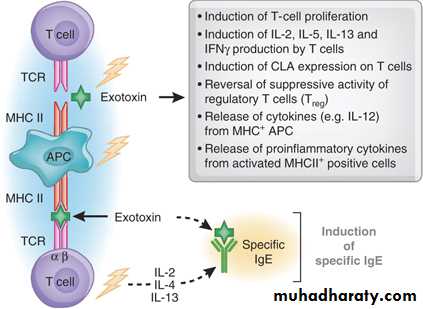
Polyclonal activation of T cells by bacterial superantigens
Extracellular bacteria evasion
A mechanism used by bacteria to evade humoral immunity.Genetic variation of surface antigen (E. coli, N. gonorrhoeae, S. typhimurium)
Resistance to phagocytes (Pneumococcus)Destruction to ROS? (Catalase producing Staphylococci)
??Immunity to
Intracellular BacteriaIntracellular bacteria
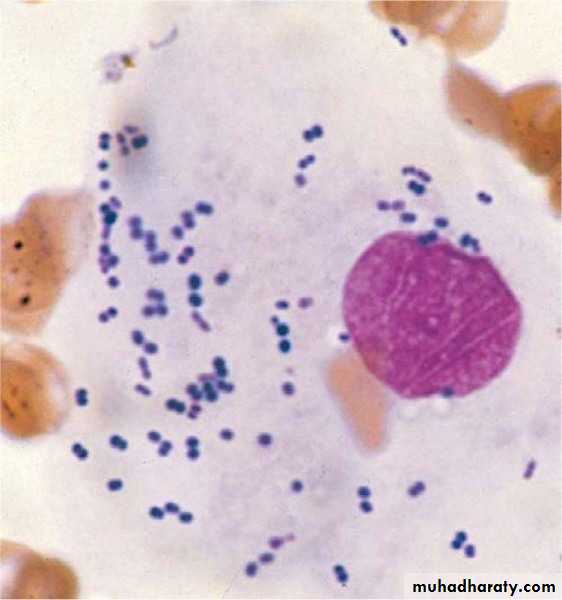
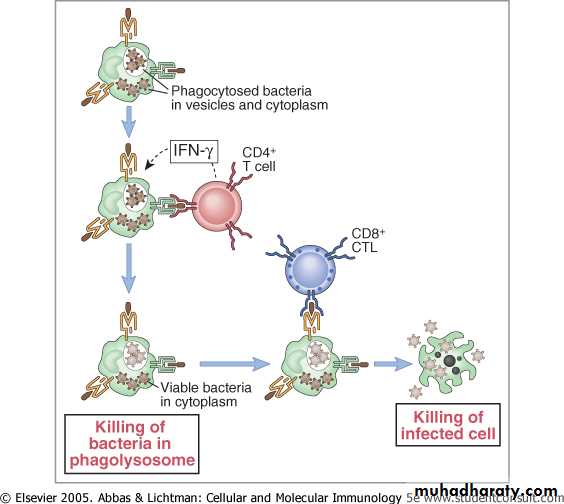
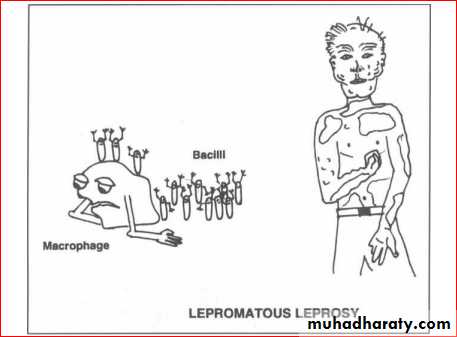
A characteristic of facultative intracellular bacteria is their ability to survive even replicate within phagocytes.
Requires cell-mediated immunity
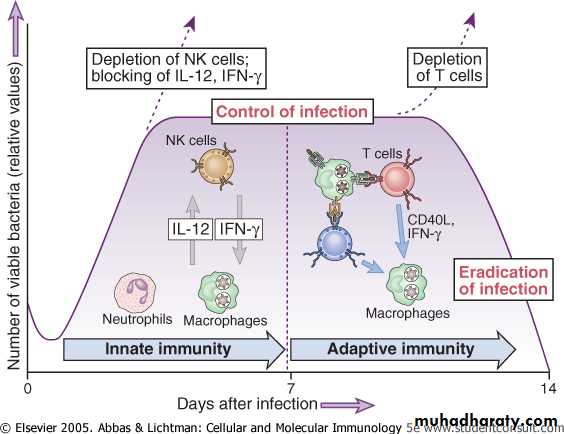
Innate and Adaptive ImmunityThe innate immune response to intracellular bacteria consists mainly of phagocytes and NK (natural killer) cells.
The major adaptive-protective immune response against intracellular bacteria is cell-mediated immunity .
The macrophage activation in response to intracellular microbes is capable of causing tissue injury.
Mechanisms of Immune Evasion by Bacteria
Inhibition of phagolysosome formation (Mycobacterium tuberculosis, Legionella pneumophila)Inactivating reactive oxygen and nitrogen intermediates Mycobacterium leprae
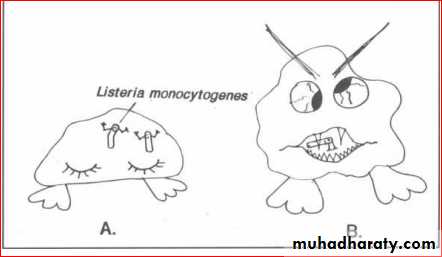
Disruption of phagosome membrane, escape into cytoplasm Listeria monocytogenes (hemolysin protein)
Intracellular bacteria
MicrobeHuman Diseases
Pathogenicity
Mycobacteria species
Tuberculosis, Leprosy
Macrophage activation, granulomatous inflammation, tissue destruction
Listeria monocytogenes
Listeriosis
Listeriolysin damages cell membrane
Legionella pneumophila
Legionnaires’ disease
Cytotoxin lyses cells
Immunity to Intracellular Bacteria
The type of immune response stimulated by bacteria depends on whether the bacteria are live or dead and whether they grow inside or outside cells.
IFN-γ
IL-2
Viruses
Obligatory intercellular pathogens that replicate within cells.Use the nucleic acid and protein synthetic machineries of the host cell.
Infect a variety of cell populations by utilizing normal cell surface molecules as receptors to enter cell.Innate Immune Response to Viruses
Viral infection directly stimulates the production of interferons (INF).Interferons are antiviral proteins, or glycoproteins produced by several types of cells in response to viral infection.
INFα by leucocytes
INFβ by fibroblast
INFγ by natural killers (NK) cells
Natural killer (NK) cells lyse a wide variety of virally infected cells.
Specific Immune Response to Viruses
Mediated by a combination of humoral and cell mediated immune mechanisms.Humoral mediated immune response.
Antibodies specific for viral surface antigens are often crucial in containing the spread of a virus during acute infection and in protecting against re-infection.
Specific antibodies are important in defense against viruses early in the course of infection and in defense against cytopathic ??? viruses that are liberated from lysed infected cells.
Opsonization
• Opsonizing antibodies may enhance phagocytic clearance of viral particles.
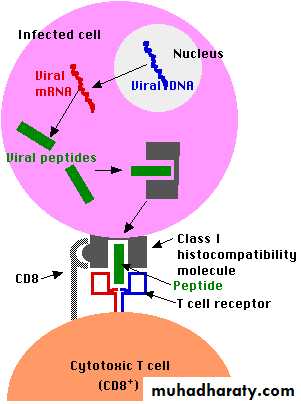
Specific Immune Response to VirusesCell-mediated immune responses.
Most important in host defense, once a viral infection is established.
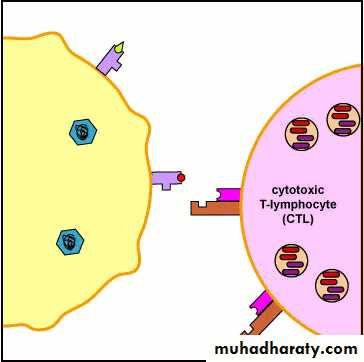
CD8+ Tc cells (Cytotoxic T lymphocytes; CTLs) and CD4+ helper T lymphocytes are the main components of cell mediated antiviral defense.CD8+ T and CD4+ T
CTL activating macrophage function
Tissue Injury
In some cases, infections with non-cytopathic viruses, CTLs may be responsible for tissue damage to the host.Evasion of Immune Mechanisms by Viruses
Viruses have evolved numerous mechanisms for evading host immunity.A number of viruses have strategies to evade complement-mediated destruction.
Evasion of Immune Mechanisms by VirusesViruses can also escape immune attack by changing their antigens.
A large number of viruses evade the immune response by causing generalized immunosuppression.
Parasites
In infectious disease terminology, “ parasitic infection” refers to infection with animal parasites, such as protozoa, helminthes, and ectoparasites.
Humans are only part of the complex life cycle of parasites.
Innate Immunity Parasites• Protozoa and helminthic parasites that enter the blood stream or tissue are often able to survive and replicate because they are resistant to host innate immune responses.
• Parasites in humane host are usually resistant to complement.
• Macrophages can phagocytose protozoa, but the tegument of helminthic parasites makes them resistant to the cytocidal effects of both neutrophils and macrophages.
Specific Immunity to Parasites
Different parasites elicit quite distinct specific immune responses.Cell-mediated immunity is the principal defense against protozoa that survive within macrophages.
Protozoa that replicate inside cells and lyse host cells stimulate specific CTL responses, similar to cytopathic viruses.
IgE antibodies and eosinophils mediate defense against many helminthic infections.
Evasion of Immune Mechanisms by Parasites
Evolutionary adaptations give parasites their ability to evade and resist immune responses.Some parasites survive and replicate inside cells.
Others develop cysts that are resistant to immune responses.
Antigen masking is an effective form of immune response evasion by some parasites.
Parasites can develop a tegument that is resistant to damage by antibodies and complement or CTLs.
Some parasites have mechanisms for surface antigen variation