
1
Clinical urology
stage
th
6
/
th
5
2016 / 2017
Dr. Mohammed fawzi
Assi.Prof
Ninavah college of medicine

2
Anatomy :
the kidney extend from L1-L3
kidney and ureter is retroperitoneal
uretropelvic junction{UPJ} :between the ureter and the kidney [ if
obstructed will cause UPJ obstruction and hydronephrosis]
uretrovasical junction : between the ureter and bladder{ if dilated will
cause uretrovasical reflux}
the the urethra is 2 part :
1. posterior urethra : prostatic – membranous
2. anterior urethra : bulbar – perenial
the epithelial lining the urinary system is transitional cell
the kidney is consist of cortex and medulla ( the thickness of cortex
reflect the function …much thickness more function )
the pelvic and ureter and bladder is low pressure system to alow the
urine to descent into the bladder .the urine is descent by gravity and
peristalsis of the ureter( if the pressure increase inside the bladder or
ureter this will prevent the urine from descend and cause hydronephrosis
and gradually renal failure )
the capacity of the bladder is 350-500 ml
investigation in urology
1.
general urine examination
we see :the color -pus cell - cast - RBC
the food and drug (rifampicin-flagel ) may change the
color of the urine
2. us :
advanteges : a. simple b.not coasty
disadvanteges : cant see the function of the kidney .cant see the
most of the ureter …
3.
KUB
:
{ kidney. Ureter. Bladder}
It is a plane X-ray taken from the level of L1 to bladder
In the KUB we can see :
bone

3
Soft tissue shadow like …. liver. Kidney.psoas muscle
Radio opaque shadow …..stone ( normal KUB doesn't mean
absent of stone . it may be radiolucent)
Gas appear as a black
4. IVU:
is to confirm the diagnosis
IVU is for functional and anatomical
We must do an KUB before the IVU
Contraindication is sensitivity and RF
If we want to exam the renal function we
must do urea and createnin .but if we want
to exan a single kidney function we must do
a IVU and renal isotop scan
5. CT scan :
it will show anatomy .it is the definitive diagnosis .but have a
high radiation
6. Redionucli study :
for the function of the kidney
7. MRI :
give anatomy and pic .no radiation
8. MRU:
for patient with sensitivity to IVU
9. MCUJ :(
macturating cystourethrogram
)
for diagnosis of uretro
vesical reflux
10.
RETROGRADE
urethrograph :
for the diagnosis of urethral
problem
Stone
Type of stone :
1) Ca oxalate is the commonest
2) Ammonium magnesium & phosphate (staghorn stone)
3) Uric acid stone
4) Cestein stone
4
AMP stone
تتجمع
في
الوسط
القاعدي
Uric acid stone
تتجمع
في
الوسط
الحامضي
Anuria :patient have no urine output, the most common
cause is ureteric obstruction by stone in a patient have only
one kidney ,rarely obstruction in both ureter ,its emergency
.we should put a foley catheter in the bladder to exclude
acute retention of urine where the bladder is full while it is
empty in case of unuria ,also we should send for renal
function test (urea and creatinine) to see the state of the
patient because unurea usually lead to renal failure if not
treated rapidly
Treatment
Insertion of nephrostomy tube (open or percutaneous ),or
we insert double j stent we should put an nephrostomy(
urinary diversion) and check the renal function test to know
the severity of the case
Acute retention of urine
no urine with full bladder usually due to obstruction in the
bladder or urethra .it is diagnosed clinically . and it resolved
by butting a foley catheter
Acute retention of urine ---- foley catheter
Anuria ---- nephrostomy
Pyelonephritis
1 .pain 2. Fever 3. Rigor 4. Tenderness 5.pyuria 6.may
associated with vomiting
It is usually occur unilateral and with D.M
If the U.S is normal – use simple antibiotic
If U.S show complication ( stone . hydronephrosis ):
1.hospital admition . parenteral antibiotic until fever is gone we
change to oral antibiotic for 10-14 day
2 .I.V fluid

5
Cystitis
1. Frequency
2. Dysuria
3. Nocturia
4. Urgency
5. Pus +RBCs in urine
6. Low grade fever
7. Suprapubic pain or discomfort
Diagnosis,
Clinically and GUE
Treatment by antibiotic for 3 –5 days
Renal tumor
Benign ( rare )
Malignant
Presentation -
1. nowadays 50 % discovered accidentally in early stage
2. Trade ( pain - hematuria - mass )
Hematuria is painless ( any patient with painless hematuria we
must suspect renal and bladder tumor )
3. Paraneoplastic syndrome: hypercalemia - anemia - abnormal
liver function test - fever - hypertension - elevated ESR
Investigation
1. GUE 2. US 3. CT-scan ( for staging )
# For grading ( histopathology )

6
# CT of the brain and lung ( if there is any symptom of
metastesis )
# ESR - - Calecium - liver function test for follow up
If it still elevated after nephrectomy, we think about metastasis
Treatment of renal tumor
1. localized tumor (t1,t2,t3 ) ,do radical neprectomy
2. partial nephrectomy done for small tumor ,less than 7 cm
or when the tumor ocure in apatient with single kidney
3. metastasis use immune therapy ( interferon & IL )
( chemotherapy and radiotherapy are not effective )
Prognosis of renal tumors : there is possibility of recurrence so follow
up should be continuous up to 2-3 years. The smaller the tumors at
time of diagnosis the more good prognosis
If after 5 year there is no recurrence we can say it is cured
Pyonephrosis
is an infection in an obstructed hydronephrotic kidney ,its
emergency ,if not treated within days lead to destruction of the
kidney
7
Hydronephrosis
+
fever = pyonephrosis
Dx: 1- GUE ,ULS , CT SCAN ,Tapping for confirmation
Treatment , by emergency drainage of the kidney by doubl j stent or
nephrostomy tube insertion WITH ATIBIOTIC
Simple renal cyst
Dx: 1. U/S is enough 2. CT scan for confirm diagnosis
Rx:
1.asymptomatic : reassurance
2.if it is large enough to cause pressure symptoms (hydronephrosis,renal
pain ) do murcipulization by open or laparoscopy
Bladder outlet obstruction
Symptom ( lower urinary tract symptom )
( Frequency – dysuria – nucturia – hesitancy – terminal drippling –
intermittency – urgency )
D.DX. (
BPH – ca prostate –urethral stone – neurogenic blader –
urethral stricture )
urinary retention
( acute – chronic – acute on chronic )
chronic : if the residual volume is 500 and more ( normal 0 ) and it
may lead to renal failure
increase frequency – decrease volume of urine that urinate - increase
residual volume – may cause reflux – bilateral hydronephrosis – renal
failure
acute retention : sudden in ability to void with pain
8
precipitation : cold weather – delay the act of micturition – stress
– diuresis - anticholinergic drugs
Contraindicated drug to use is : anticholinergic – decongestant
with epinephrine )
Presentation : pain – desire to void
Rx : foley catheter : if fail supra pubic catheter , if not available
suprapubic aspiration by needle
Acute on chronic : sudden retention of urine in patient who is
already have chronic retention
We can know that it is chronic if :
1. amount of urine collected in the bag by foley catheter is more
than 1000 and its painless
2. by US
3. by percussion ( it will be tender in acute and not tenderness in
chronic )
To differentiate BPH from neurogenic bladder 0r CVA or
disc prolapse ( in these cases there will be an associatiated
neurological symptom )
From Urethral stricture ( the catheter cant be inserted )
BPH
( BENIGN PROSTATIC HYPERATROPHY )
Dx
:
1. GUE ( to exclude cystitis )
2. P.S.A
3. US ( kidney – bladder – prostate ,post voiding residual
volume
4. P.R
5. bladder examination

9
6. nervous system examination ( if we suspect neurogenic
bladder )
urodynamic study ( if we suspect neurogenic bladder )
Causes of BPH
1) aging
2) androgenic effect ( testesteron )
Method of treatment :
1) conservative ( for mild cases )
عدم شرب أي شي ليال
–
عدم التعرض للبرد
–
عدم استعمال أي شي يضعف المثانيه
2) medical ( if the symptom progress )
A) Anti androgen ( 5 alph reductase inhibitor ) . it need 6
month to work .so we give alfa- blocker until it work
S.E: loss of lipido – impotence
B) ( a-blocker ) cause relaxation of smooth muscle of the
prostate
S.E : hypotension – syncope –retrograde ejaculation
3) surgery : indication
Sever symptom
No benefit of medical treatment
Appearance of complication ( stone – repeated
hematuria –repeated UTI – R.F – acute or chronic
retention)
1. TURP ( trans urethral resection of prostate )
Complication ( bleeding during and after
operation – )
Post TURP syndrome : due to use of water
during operation – the water wil be absorped –

10
cause - delusional hyponatremia and brain
oedema leading to confusion and even comma
Dx of post TURP syndrome is by measuring
serum NA level
Rx : use of hypertonic saline
To avoid TURP SYNDROM we should use
normal saline instead of water during operation
with bipolar resectoscope
After TURP we insert a 3 ways foley catheter
o
1
st
way for irrigation ( to avoid clot formation in
the bladder )
o
2
nd
way for evacuation of urine
o
3
rd
line for the balloon inflation
2. Open prostatectomy
Open trans vesical prostatectomy ( by supra vesical
incision )
3. Minimal invasive ( if the patient are not compatible
with the surgery
Trans urethral microwave therapy – trans urethral
needle ablation – balloon dilatation – stent application
Complication of TURP and open prostatectomy
o
Early
– bleeding ( during and post operative ),
Clot retention which if occur treated by cystoscopy
and evacuation of clot by ellik evacuator
o
Late
Urethral stricture – recurrence – impotence –
retrograde ejaculation – incontinence,
Open prostatectomy have a complication of wound
like wound infection in addition to a previous
complication
11
AFTER SURGERY WE SEND THE SPECIMEN FOR THE
LAB FOR CITOLOGICAL EXAMINATION TO EXCLUDE
MALIGNANCY
foley's catheter
األلوان تكون حسب الحجم
It should not stay more than three (3) week and
Replaced
Indication
1. For treatment of acute or chronic retention
2. Irrigation
3. Calculate urine volume
4. After operation for the urethra . bladder or open
prostatectomy ,TURP,TURBT
5. For diagnostic purpose as in
Micturiting cystourethrographe ,Retrograde urthrography
6. For intravesical chemotherapy
Complication
Infection
Stone formation
Injury to the urethra and urethral stricture
In ability to remove it
We must sure that the ballone is reached the bladder before we
inflate it > and we deflate it before remove it
Vesico uretral reflux
Presentation: Repeated UTI IN INFANT AND CHILDREN
Diagnosis : mucturating cystourethrographe ( MCUG )
Grade 1 …. Urine reach the ureter
Grade 2 ….. urine reach the kidney but no dilatation
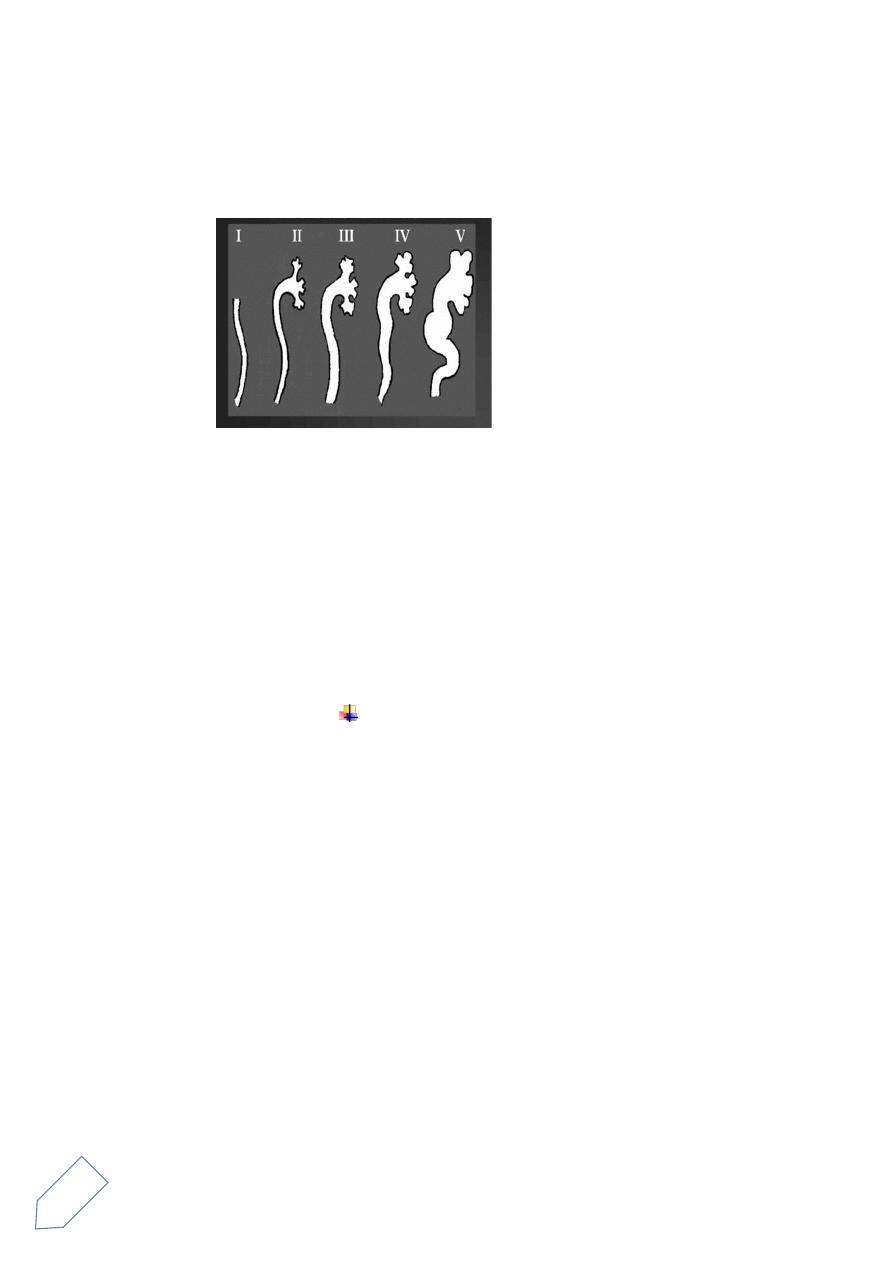
12
Grade 3 ….. urine reach the kidney with mild dilatation
Grade 4….. urine reach the kidney with sever dilatation
Grade 5…. The urine reach the kidney with sever dilatation and tortuosity
of the ureter
Treatment :
o
Grade ( 1- 2 ) : prophylactic antibiotic ( 1/3 of the
dose of the UTI – trimethoprim at night )
o
Grade ( 3- 4 -5 ) : 1. surgery ( reimplantation of the
ureter )
2 . Subtrigonal injection of
special substance ( tephlon like ) causing obstruction
Contra indication of the IVU
1. Allergy to the dye
2. Renal failure
3. Diabetic patient using Glucophage ( must stop it because
2 weeks )
Congenital anomalies ( general feature to all )
1. They are asymptomatic
2. Accidental diagnosed
3. If symptom will present it mainly due to (hydronephrosis –
repeated infection – stone )
Investigation : the best is IVU for all of them
Treatment : reassurance – treatment of complication ( UTI .
stone .
13
Differential diagnosis for absent of the kidney in KUB
1. Agenesis
2. Non functioning kidney
3. Nephrectomy
4. Ectopic kidney
Urethral stricture
Causes : 1 . congenital
2. inflammatory(gonorrhea)
3. traumatic ( external – iatrogenic )
Presentation :
1. Obstructive symptom : gradual weak stream of urine
2. Acute retention of urine
Diagnosis :
1. Urethrographic
2. Urethroscope
3. U.S
Treatment :
1. Dilatation by metallic dilator ( may recure so need repeated
dilatation)
2. Urethrotomy by endoscopic laser or knife
3. Urethroplasty ( cut of the stricture )
Congenital PUJ obstruction
Presentation
According to the severity
1. May discovered accidentally
2. A mild case may present at any age
14
3. It could be very sever that cause sever
hydronephrosis ( and nephrectomy done in early
life)
4. Pain after drinking a large amount of water or
using diuretics (details crisis)
5. Repeated infection
6. If it is bilateral and severe form it may cause renal
failure
Complication :
1. Repeated UTI and stone
2. If bilateral it will cause renal failure
3. If unilateral it will cause destruction of the kidney
Diagnosis :
1. Renal isotope ( with diuretic or diuretic renogram )
2. IVU (dilated pelvis and usually upper ureter not
seen)
TREATMENT
In mild case reassurance and follow up
Indication of surgery
Repeated pain and infection
Progressive hydronephrosis and deterioration of
renal function
Renal stone formation
Types of surgery
Pyeloplasty ( open and laparoscopic)
15
Endoscopic pyelotomy through ureteroscope
or nehroscope
Testicular swelling
painful
(acute)
torsion of the testes
torsion of testicularand epidedymal appendages
strangulated inguinal hernia
epidydemitis(acute)
fourneirs gangrene of scrotal wall
varicosity could be (dull aching pain long duration Or painless)
trauma
10 percent of testicular tumor
Investigation
o Send for US immediately
o Doppler US especially useful in :
1.torsion (check vascularity)
2. varicosity
painless
tumor
hydrocele
epidydemal cyst
spermatocele
Torsion of testis
نفكر بيهاًامئاد مزلا(
)
Testicular torsion
occur in adolescent(mainly) but any age can be affected, neonatal
torsion
if missed for 12 h lead to loss of the testes as a result of ischemia
sudden sever attack of pain
radiate to the lower abd. With vomiting

16
awake him from sleep at mid night
swelling start with 1_2 hr
usually unilateral
O/E: swelling , red ,tender , higher in position (abnormal lying)
DDx:
o epidydemitis(associated with fever)
o sometimes UTI
o torsion of appendages
*to differentiate between (epidydemitis and torsion ) we do perhens
sign
If we lift the testis pain increase in torsion and decrease in epidydemitis
Dx : Doppler US is diagnostic
Management:
--early stage manual detortion if possible
--Exploration when ever you suspect it if the testes still viable
Orcheopexy done, The other side should also be fixed by orcheopexy
also
If the testes is "gangrene" ..orcheoctomy and orcheopexy for the other
Hydrocele
Abnormal accumilation of fluid within tunica vaginalis around the testis
primary : without cause , gradual , young adult
Symptoms : heaviness , mild pain
Secondary
Causes : tumors , trauma , epidimytis , post operative

17
Congenital hydrocele (communicating)
Continue with peritoneum by patent processus vaginalis
Appear after birth
•
Rx
: of congenital hydrocele
Wait until 1yr if remain …..do surgery by ligation of the patent procassus
vaginalis
Diagnosis of hydrocele :
Ultrasound for diagnosis and exclusion of important secondary
cause like testicular tumor
DDx : hernia
o To differentiate it from hernia :
In hernia cough reflex is +ve . in hydrocele is - ve
In hernia we cant get above it. In hydrocele we can
translumination: -ve in the hernia . +ve in the
hydrocele
Treatment of hydrocele
o mild …. Follow up
o indication for surgery :distressing the patient or large
size…..hydrocelectomy
o if old pt. cant tolerate anesthesia ….aspiration
complication of aspiration
1.infection (pyocele)
2.recurrence
3. injury to vessels (heamatocele)
DDx of absent testis
1 . agenesis
2 . ectopic
3 . orcheoctomy
4. retractile testis
5 . undesending testis
18
Undesending testis
Due to arrest of the testis on its normal descending pathway
intra. Abd.
superfascial inguinal testis
canalucular
Dx : US ….CT
The most accurate is laparoscopy in intra. Abd.
Rx : orcheopexy should be done before 1yr age
Problems of undescending testis
1. liable for trauma
2. liable for torsion
3. liable for tumor
4. infertility
5. usually associated with hernia and other congenital anomalies
The indication of circumcision
1.relegiuos
2.repeated UTI
3.ca of prepuse
4.phemosis and paraphymosis (in paraphymosis need emergency
cercumcession)
Complication of circumcision
1.bleeding (suture the art.)
2.injury (cut the glans with prepuce)
If we use cautery obliterate the art. And causing gangrene of the penis
3. Infection
19
PHYMOSIS
narrowing of the prepuse opening, so its occur in
uncircumcised child
treatment is circumcision
PARAPHYMOSIS
retraction of the prepuse behind the glance(so occur in
uncircumcised child also) causing cut of blood supply to the
glance and gangrene of the glance , so its emergency
condition
MEATAL STENOSIS
narrowing of the the meatus in the glance ,its usually occur in
circumcised child causing severe narrowing or urinary stream
Treatment by enlargement of the meatus by dilatation or
meatotomy
Varicocele
Abnormal dilatation of pampiniform plexus of the testis
Cause:
Malfunction of the valves mainly the left side
o
Varicocele cause local elevation of temperature that lead to
infertility
Presentation
o
incidentally
finding during examination of the testis
o
mild pain
o
infertility
when u examine the pt. U should examine him in 2 position
(standing and setting )
Valsalva manuver During examination it appear as a sac of
worm
Investigation
:
o
u.s , doppler u.s
Indication of surgery :
1.
PAIN
20
2.
testicular atrophy
3.
infertility
4.
young unmarried
treatment
---varicocelectomy by surgery (inguinal or
subinguinal approach), or by laparoscopy ,
Hydronephrosis
is aseptic dilatation of pelvicalecial system (no infection. no
fever)
hydronephrosis will cause pressure on the cortex and cause
gradual atrophy of the cortex and decrease in thr renal function
(thinning of the cortex ---less function )
in hydeonephrosis
if the cause is from the ureter –unilateral hydronephrosis
if the cause in the bladder and urethra –bilateral hydronephrosis
Normal renal calyces shape is cup .. This mean normal cortical
thickness so normal function .. While clubbing shaped calyces mean
hydronephrosis ,thinned cortex so Decrease renal function
Causes :
o Obstructive(intramural ,mural and extramural) usually the cause
can be diagnosed by ULS,IVU AND CT SCAN
o refluxive ( vesicouretral reflux )
In child with hydronephrosis you should exclude reflex by MCUG
Pregnancy also cause hydronephrosis
most common cause of hydreonephrosis is
obstruction by calculi (stone)
Renal stone

21
Radioopaqe like calecium stone ,and radiolucent like uric acid which
occure in acidic urine
Staghorn stone which is called also infectious stone usually occur in
alkaline urine
Diagnosis bu ULS ,IVU AND CT Scan
Treatment of renal stone
1—conservative and follow up in stone less than 5 mm, this
includepain killer , antibiotic for infection and drink plenty of water
2— flexable ureteroscopy with lasser
3—ESWL ,for stone less than 2 C
m
Contraindication of ESWL:
It cause bleeding so it contraindicated in patient with bleeding
tendency
If we have obstruction distally
pregnancy
4 – PCNL for stone more than 2 cm ,staghorn stone ,and stone in the
lower renal calyces
5—open surgery ,if all the previous options is not suitable or not
available ,this include puelolithotomy,nephrolithotomy or parial
nephrectomy, and even nephrectomy in non functioning kidney
6— chemical dissolution of stone ,especially in uric acid stone by
alkalization of urine by potassium citrate
URETERIC STONE TREATMENT OPTIONS
1—conservative ,like that of renal stone conservative treatment ,in
addition we can add alpha blocker (tamsulusin) which can aid the
passage of the stone ,this patient should be followed up ,if not respond
change to intervention options
indication of intervention
Single kidney
Fail of medical treatment
Hydronephrosis

22
2—ESWL for stone less than 1 cm
3—ureteroscope the most widely used options nowadays
4—open surgery (ureterolithotomy)
2. Surgery : indication
Single kidney
Fail of medical treatment
Hydronephrosis
Vesical stone
It may be primary like in poor children, or secondary to bladder outlet
obstruction(like BPH ) ,and also in neurogenic bladder
diagnosis usually by ULS AND KUB
either by open surgery when the stone is large
or by endoscopic lithotripsy
when the stone is associated with BPH ,both conditions should be
treated at the same time
DOUBLE J STENT
Indications
1. to bypass ureteric obstruction
2. after ureteroscopic manipulation (like after removal of ureteric
stone)
3. after ureteric surgery like pyeloplasty for PUJ obstruction, end to
end anastomosis of ureter like in ureteric injury and after
reimplantation of ureter for vesicoureteral reflux
4. after ureteric injury
5. before difficult pelvic surgery like hysterectomy or colectomy to
avoid ureteric injury during surgery
6. before ESWL for renal stone in a single kidney
7. pregnancy with hydronephrosis
the hydronephrosis may be normal or pathological and we cant do
any investigation to confirm it because all test is contraindicated in
pregnancy . so we put the double J to be save until delivery
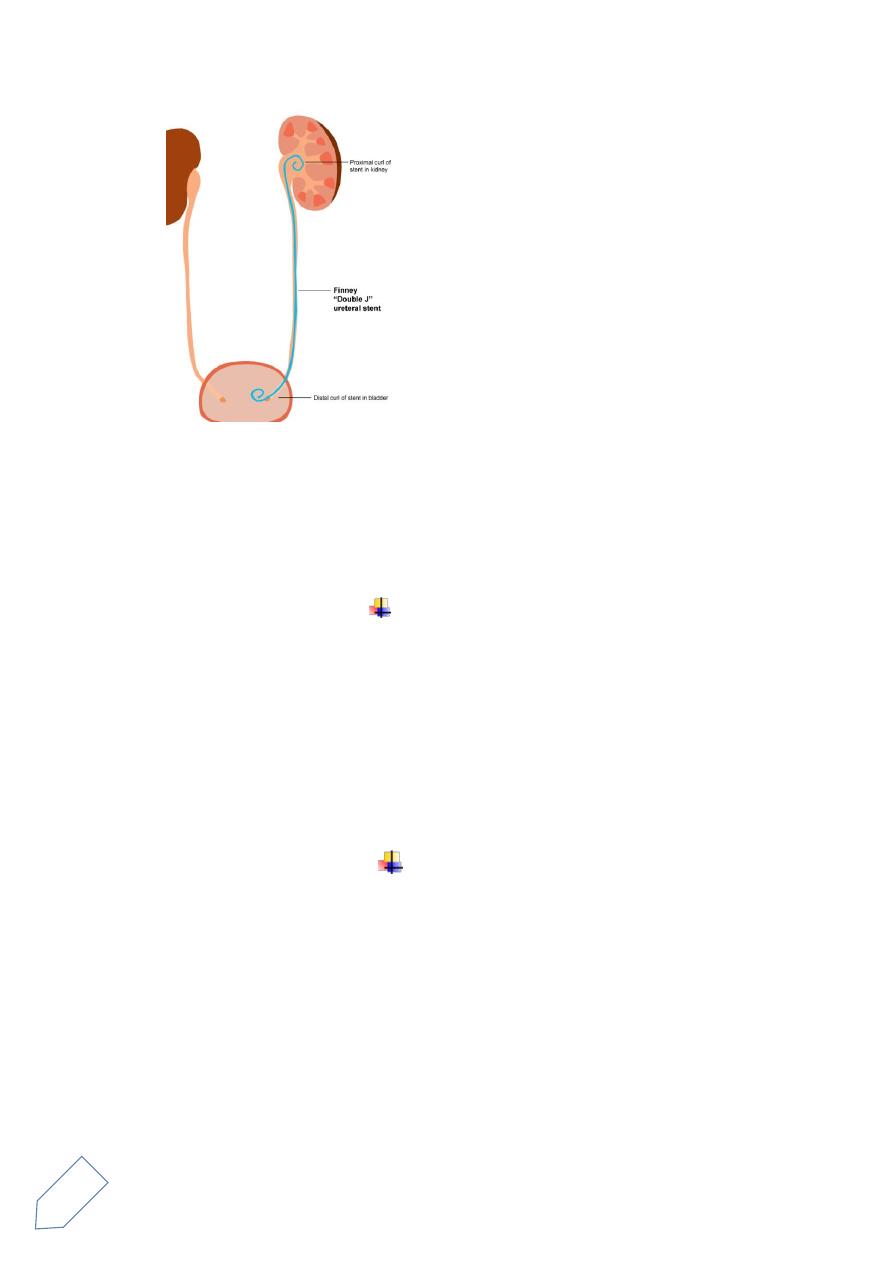
23
Complication
UTI, dysuria, ,frequency ,dislodgment of stent ,ureteric injury during
insertion of the stent incrustations on the stent and difficulty in
removing it when the stent stay for long duration
NEPHRECTOMY
simple nephrectomy ,removal of the kidney alone ,usually non
functioning kidney due to benign conditions (less than 15
percent function by isotope renal scanning)
like in hydronephrosis ,renal stone ,renal hypoplasia
radical nephrectomy ,removal of the kidney with surrounding
fat and gerota facia, this is usually done for renal cell carcinoma
bladder tumor
mostly its transitional cell carcinoma
smoking is important predisposing factor
recurrent painless hematuria is the most common presentation
DIAGNOSIS
ULS , AND CT SCANN FOR STSSGING OF THE TUMOR
DIFINIT DIAGNOSIS IS BY CYSTOSCOPY AND BIOBSY
TREATMENT
SUPERFACIAL BT (TA,T1)
24
Transurethral resection of the bladder tumor TUR BT ,with follow up
by cystoscopy every 3 months to detect any recurrence
If the tumor is large or multiple or high grade or recurrent or
involvement of lamina propria or the presence of carcinoma insitu
with bladder tumor this patient need intravasical chemotherapy
course (weekly for 6 weeks) in addition to TURBT and follow up
DEEP BT (T2---T4) (tumor with muscle invasion)
RADICAL CYSTECTOMY WITH URINARY DIVERSION
PROSTATIC CARCINOMA
localized carcinoma treated by radical prostatectomy
metastatic tumor(which is most commonly to the bone) treated
by hormonal therapy by bilateral orchectomy or by antiandrogin
therapy
