• These may result from:
• Excessive immune responses (hypersensitivity reactions)• Unwanted or inappropriate immunes response ( Autoimmune diseases )
• Inadequate immune responses (immunodeficiency disease
DISORDERS OF THE IMMUNE SYSTEM
Hypersensitivity Reactions
The purpose of the immune response is to protect against invasion by foreign organisms,but they often lead to host tissue damage. An exaggerated immune response that results in
tissue injury is broadly referred to as a hypersensitivity reaction.
Classification:
a. According to Gell and Comb’s classification, hypersensitivity reactions can be divided
into four types (type I, II, III, and IV) depending on the mechanism of immune recognition
involved and on the inflammatory mediator system recruited.
b. Types – I, II, and III reactions are dependent on the interaction of specific antibodies with
the given antigen, whereas, in type IV reactions recognition is achieved by antigen
receptors on T-cells.
a. Type 1 hypersensitivity (IgE) anaphylactic type
may be defined as a rapidly developing immunologic reaction occurring within minutes after the combination of Ag with Ab (IgE) bond to mast cells or basophiles in individuals previously sensitized to the Ag .
Example of diseases
Local reactionAtopic dermatitis ( acute eczema )
Allergic rhinitis (Hay fever) often associated with
Atopic conjunctivitis
Extrinsic allergic asthma
Food allergy
Systemic reaction
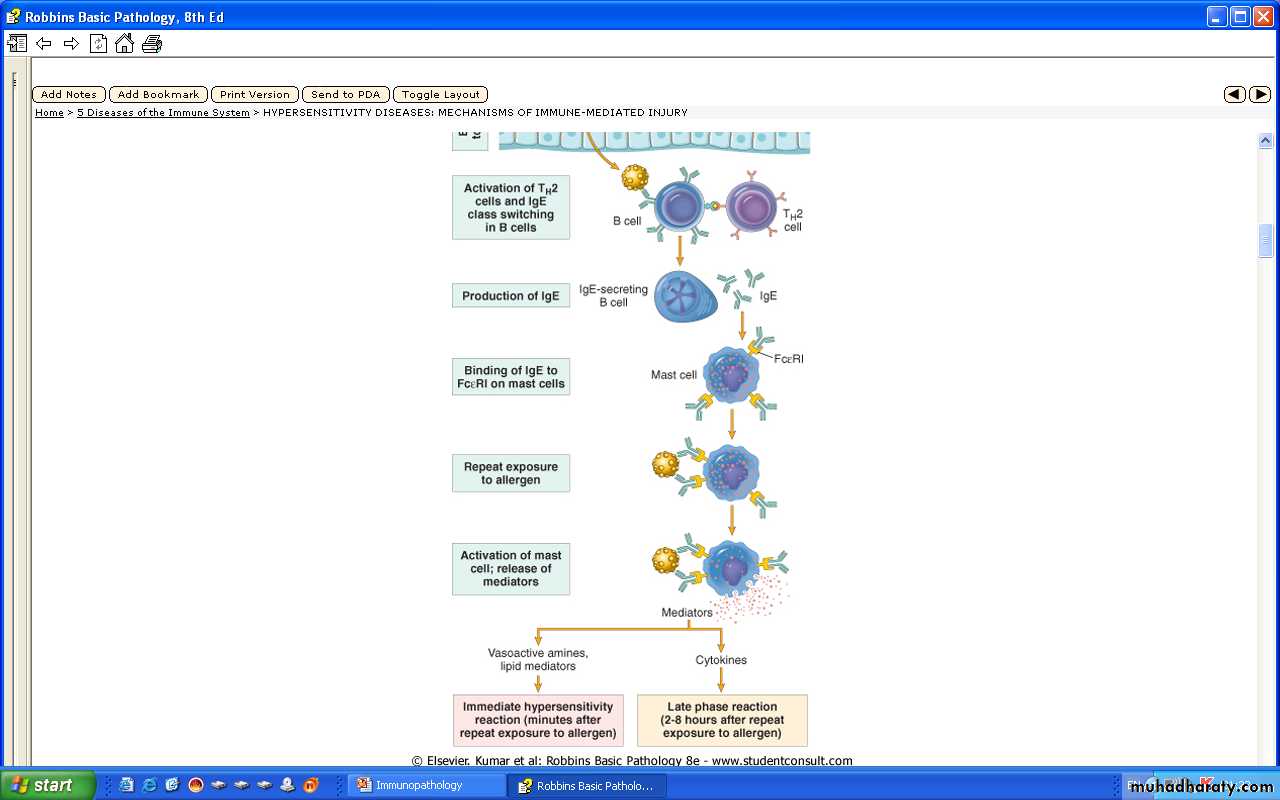
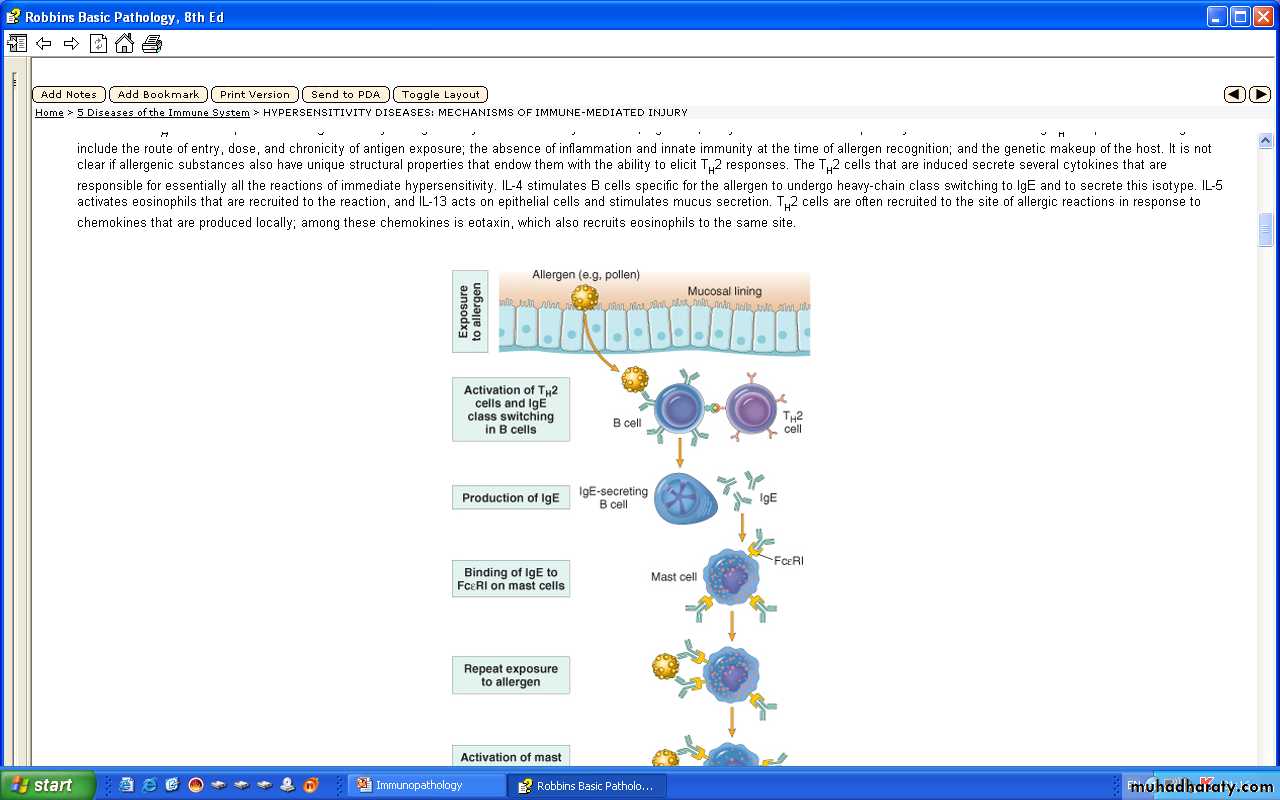
Systemic anaphylaxis e,g, Penicillin, bee venomSequence of events in immediate (type 1) hypersensitivity Immediate hypersensitivity reactions are - initiated by the introduction of an allergen, - which stimulates TH2 responses & IgE production. - IgE binds to Fc receptors on mast cells, -& exposure to the allergen --activates the mast cells to secrete the mediators that are responsible for the pathologic manifestations of immediate hypersensitivity
Ag.
TH2
IgE
B-cell
Epithelium
APC
TCR
IL-4
IL-4,5eosinophil
IgE-A.b.Release
Granules
Activation
Mast cell
Rexposure1°&2°
MediatorsCross linking
Initial
Phase
Late
Phase
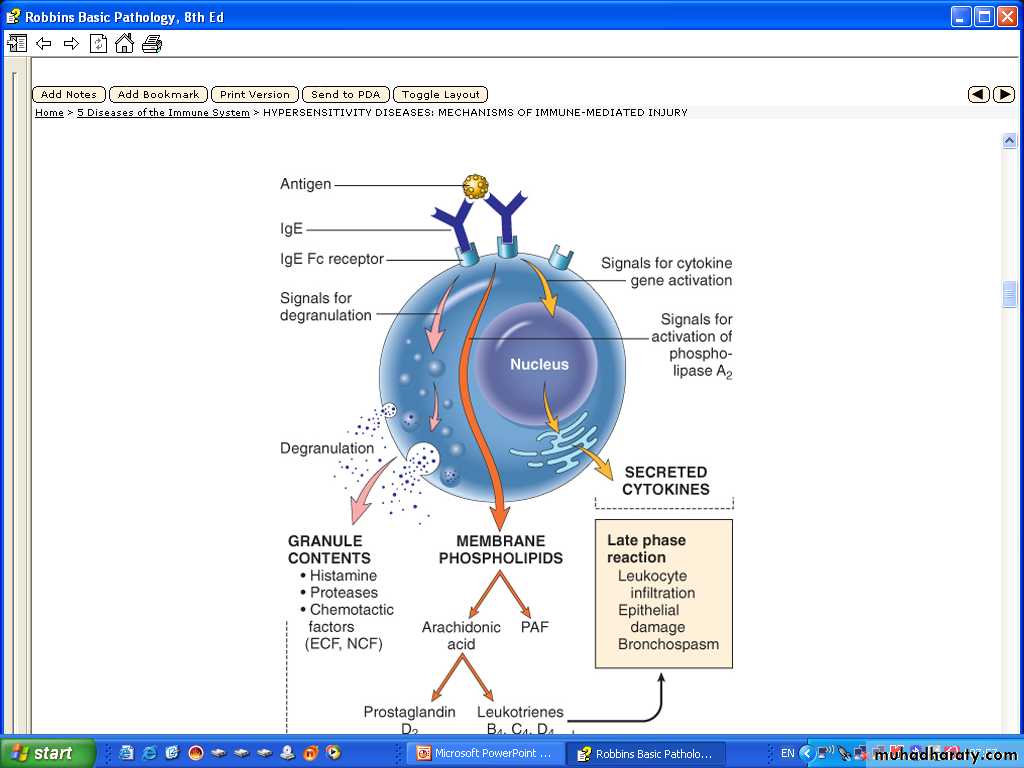
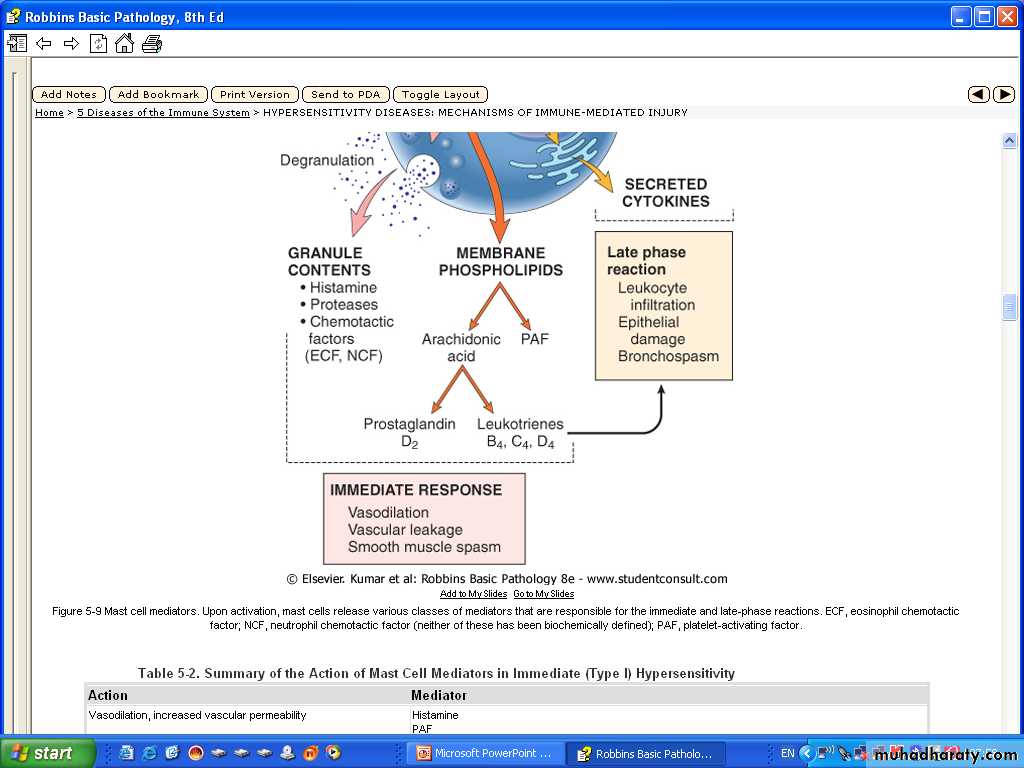
1- Vasoactive amine released from granule stores :e,g, Histamine, 2-Newly synthesized lipid mediators e.g, Prostaglandins & Leukotrienes3- Cytokines these are important for the late phase e.g. TNF & Chemokines for leukocytes ,IL-4 & IL-5
Thus, type I reactions have two well-defined phases.
a. Initial phase (response):Characterized by vasodilatation, vascular leakage, and depending on the
location, smooth muscle spasm or glandular secretions.
b. Late phase
As it is manifested for example in allergic rhinitis and bronchial asthma, more
intense infiltration of eosinophiles, neutrophiles, basophilic, monocytes and CD4 + T
cells are encountered and so does tissue destruction (epithelial mucosal
cells).
Mast cells and basophiles are central to the development of Type I reaction.
Mast cells are bone marrow driven cells widely distributed in tissues around
blood vessels, and sub epithelial sites where type I reaction occurs.
Antibody-Mediated Diseases(Type II Hypersensitivity)
Antibody-mediated (type II) hypersensitivity disorders are caused by antibodies directed against target antigens on the surface of cells or other tissue components.
The antigens may be normal molecules intrinsic to cell membranes or extracellular matrix, or they may be adsorbed exogenous antigens (e.g., a drug metabolite).
Antibody-mediated abnormalities are the underlying cause of many human diseases
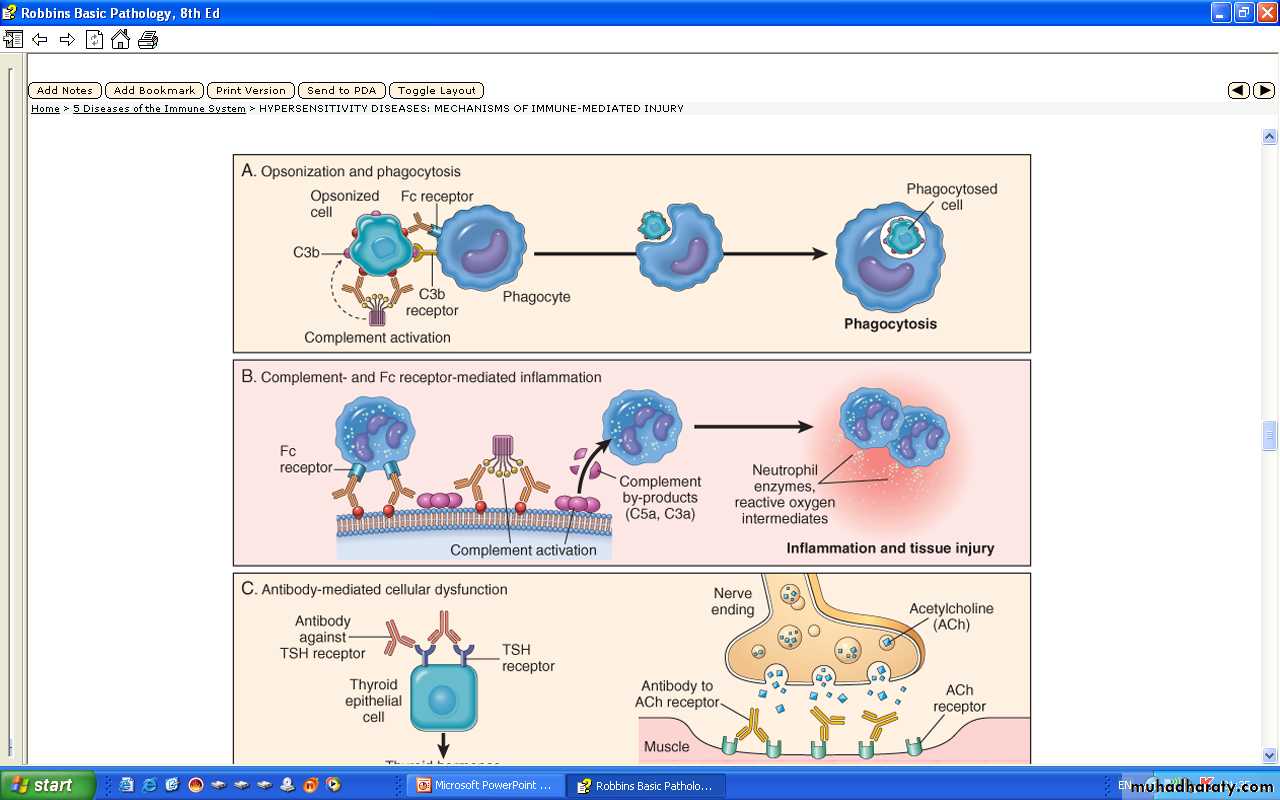
Antibodies cause disease by targeting cells for phagocytosis, by activating the complement system, and by interfering with normal cellular functions
The antibodies that are responsible are typically high-affinity antibodies capable of activating complement and binding to the Fc receptors of phagocytes
.
Three different antibody-dependent mechanisms are involved in this type of reaction
(i) Complement-dependent reaction
i. Direct lysis:
a) It is effected by complements activation, formation of membrane attack complex (C5 –9)
. This membrane attack complex then disrupts cell membrane integrity by drilling a
Hole.
b) Opsoinization: By C3b, fragment of the complement to the cell surface enhances
Phagcytosis
Examples include red blood cells, leukocytes and platelets disorders: Transfusion reaction;
haemolytic anemia; A; Thrombocytopenia; Certain drug reaction
b. Type II hypersensitivity (ab-dependent)
1` complement dependent reactions
Target
cell
A.B. (IgG,IgM)
A.g.
complementC3b-
opsonizationMembrane
attackcomplex
Lysis
Drilling holesOpsonic adhesion
& phagocytosis
Antibody-Mediated Diseases (Type II Hypersensitivity
Opsonization and phagocytosis. ( ADCC) When circulating cells, such as erythrocytes or platelets, are coated (opsonized) with autoantibodies, with or without complement proteins, the cells become targets for phagocytosis by neutrophils and macrophages .
These phagocytes express receptors for the Fc tails of IgG antibodies and for breakdown products of the C3 complement protein, and use these receptors to bind and ingest opsonized particles. Opsonized cells are usually eliminated in the spleen, and this is why splenectomy is of some benefit in autoimmune thrombocytopenia and hemolytic anemia.