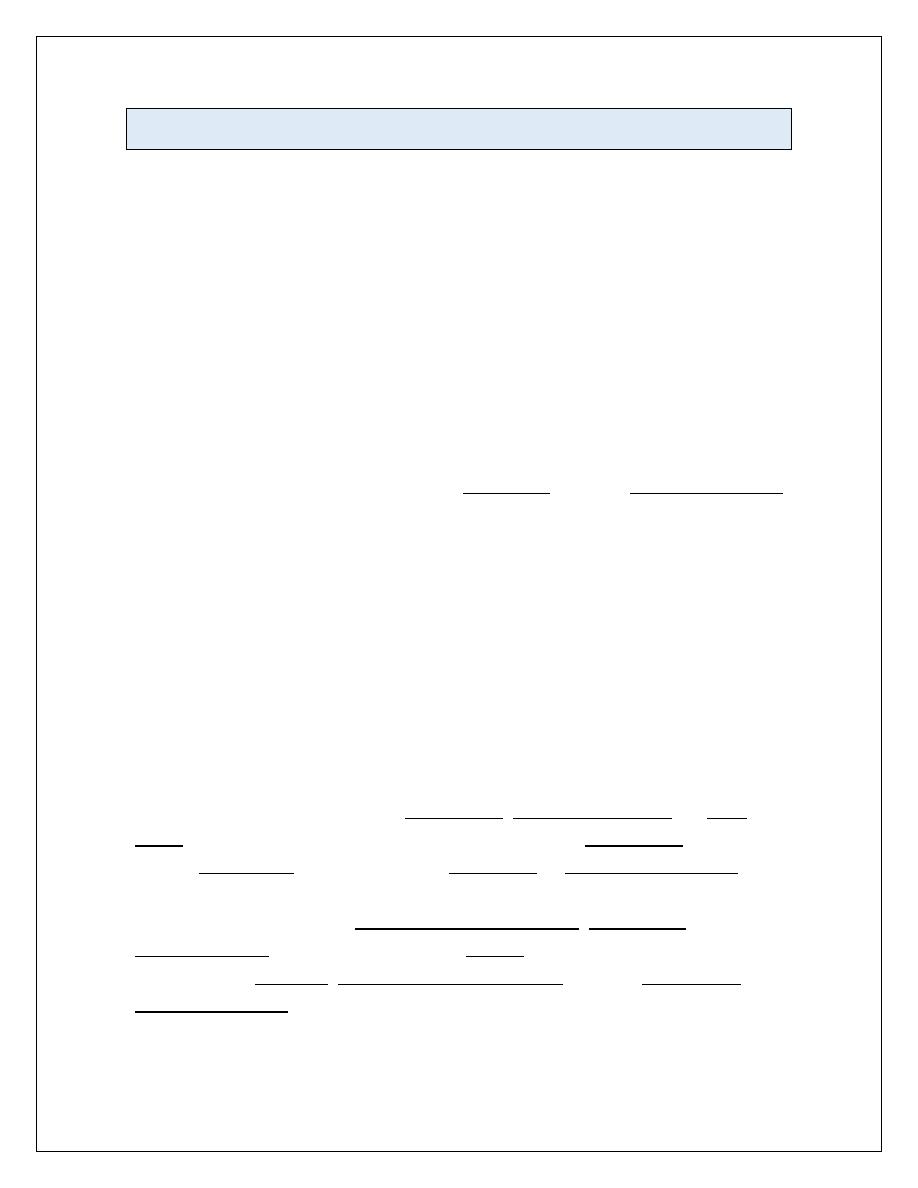
Tumours of the oesophagus
Benign tumours
This is usually asymptomatic but may cause bleeding or dysphagia.
Carcinoma of the oesophagus
Squamous oesophageal cancer is relatively rare in Caucasians but is more
common in Iran, parts of Africa and China.
Squamous cancer can occur in any part of the oesophagus, and almost all
tumours in the upper oesophagus are squamous cancers. Adenocarcinomas
typically arise in the lower third of the oesophagus from Barrett’s
oesophagus or from the cardia of the stomach.
The incidence is increasing; this is possibly because of the high prevalence
of gastro-oesophageal reflux and Barrett’s oesophagus in Western
populations.
Despite modern treatment, the overall 5-year survival of patients
presenting with oesophageal cancer is only 13%.
Clinical features
Most patients have a history of progressive, painless dysphagia for solid
foods. Others present acutely because of food bolus obstruction. In late
stages, weight loss is often extreme; chest pain or hoarseness suggests
mediastinal invasion. Fistulation between the oesophagus and the trachea
or bronchial tree leads to coughing after swallowing, pneumonia and
pleural effusion. Physical signs may be absent but, even at initial
presentation, cachexia, cervical lymphadenopathy or other evidence of
metastatic spread is common.
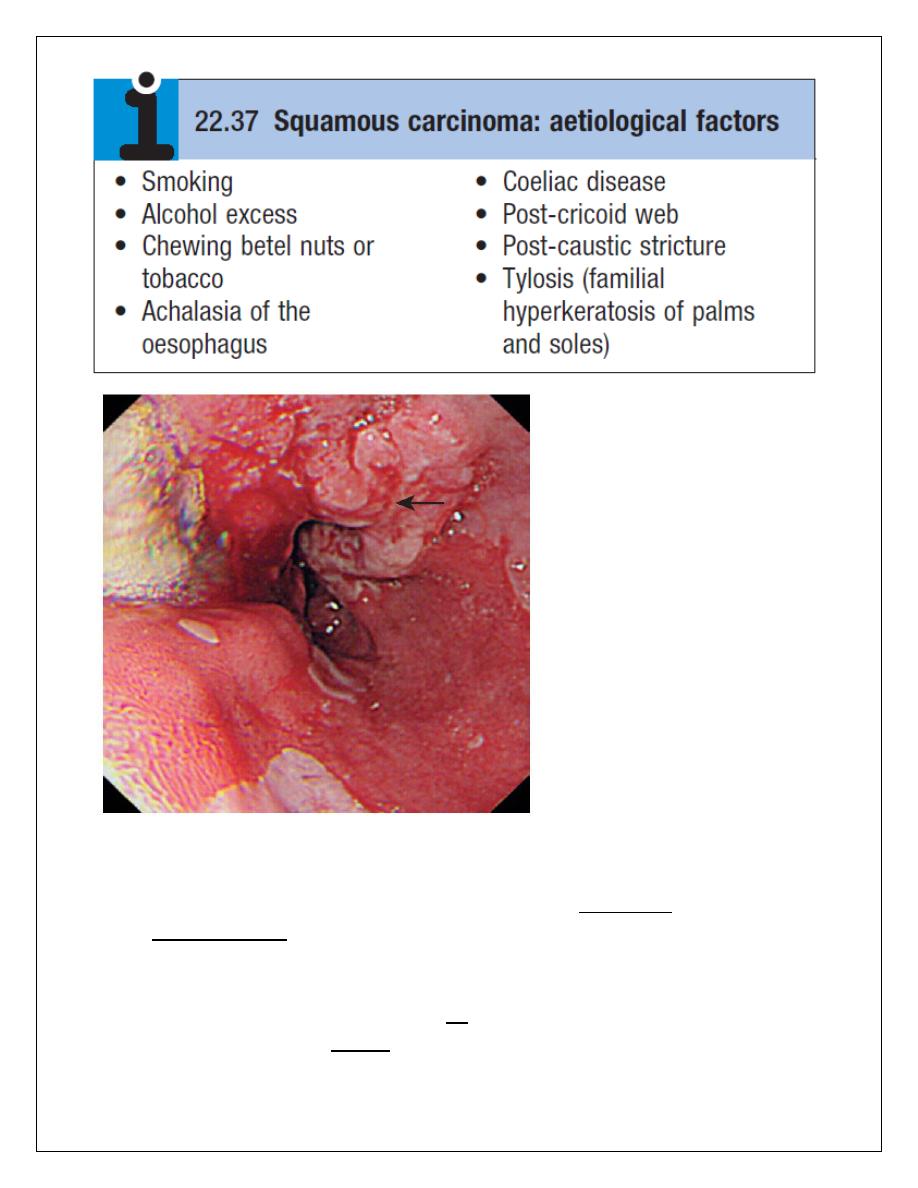
Investigations
The investigation of choice is upper gastrointestinal endoscopy with biopsy.
A barium swallow demonstrates the site and length of the stricture but
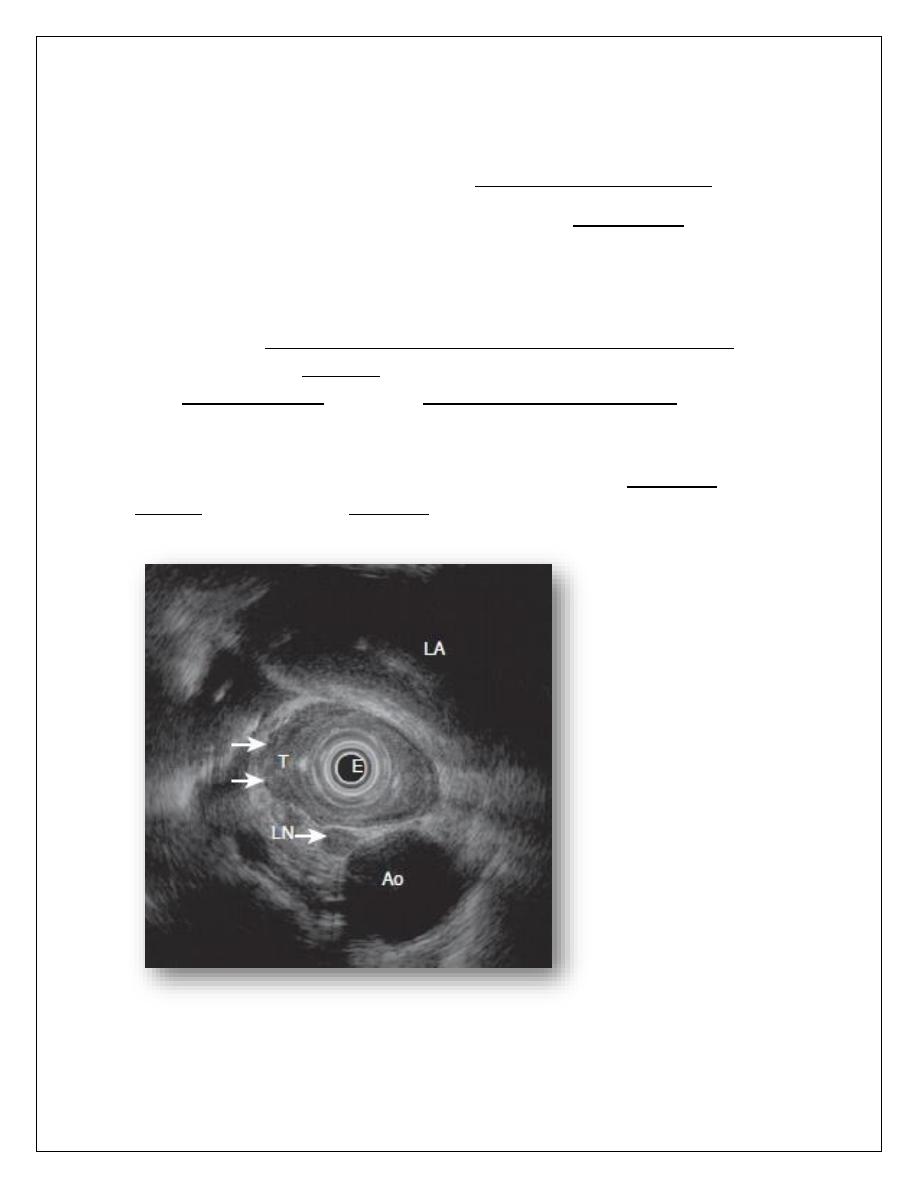
adds little useful information. Once a diagnosis has been made,
investigations should be performed to stage the tumour and define
operability. Thoracic and abdominal CT, often combined with positron
emission tomography (CT-PET), should be carried out to identify metastatic
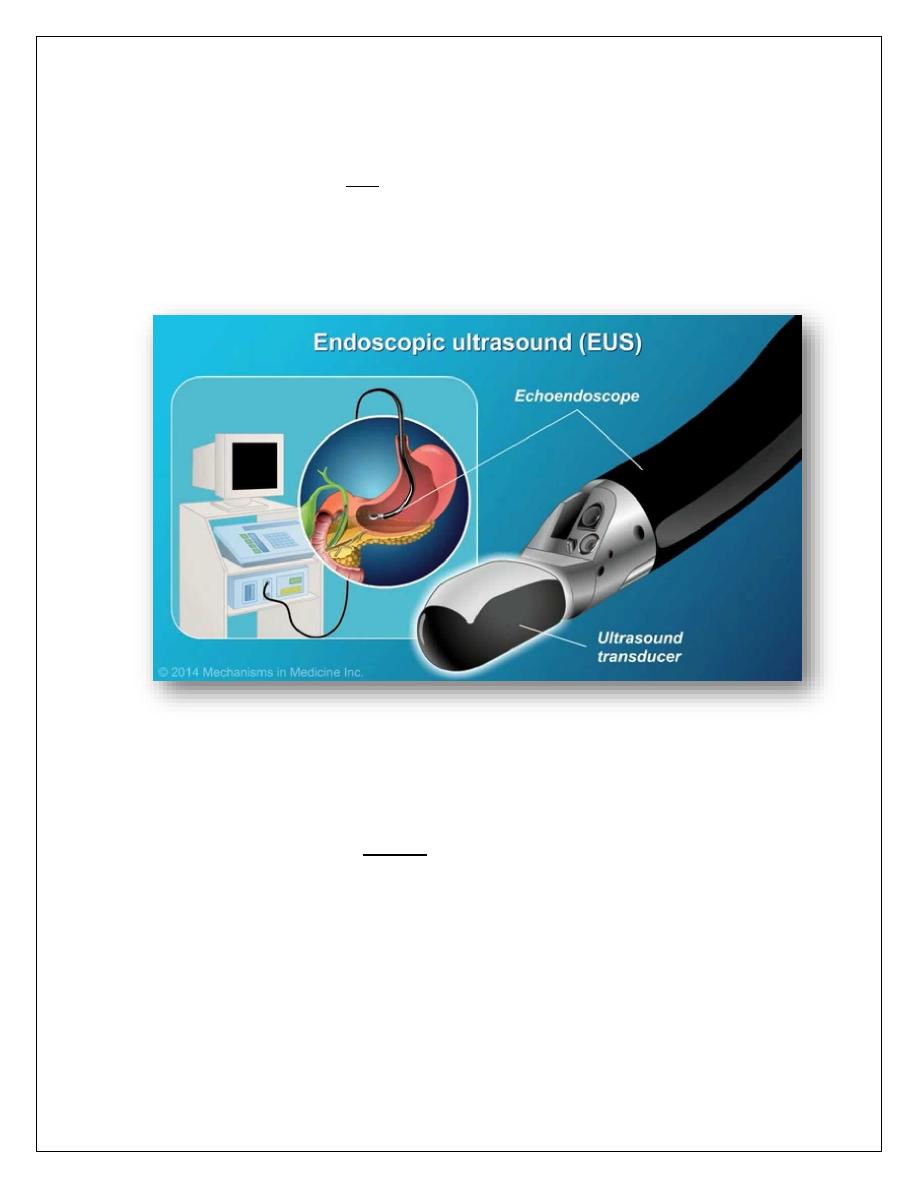
spread and local invasion. Invasion of the aorta, major airways or coeliac
axis usually precludes surgery, but patients with resectable disease on
imaging should undergo EUS to determine the depth of penetration of the
tumour into the oesophageal wall and to detect locoregional lymph node
involvement. These investigations will define the TNM stage of the disease.
Management
The treatment of choice is surgery if the patient presents at a point at
which resection is possible. Patients with tumours that have extended
beyond the wall of the oesophagus (T3) or which have lymph node
involvement (N1) have a 5-year survival of around 10%. However, this
figure improves significantly if the tumour is confined to the oesophageal
wall and there is no spread to lymph nodes.
Overall survival following ‘potentially curative’ surgery (all macroscopic
tumour removed) is about 30% at 5 years, but recent studies have
suggested that this can be improved by neoadjuvant chemotherapy.
Although squamous carcinomas are radiosensitive, radiotherapy alone is
associated with a 5-year survival of only 5%, but combined
chemoradiotherapy for these tumours can achieve 5-year survival rates of
25–30%.
Approximately 70% of patients have extensive disease at presentation; in
these, treatment is palliative and should focus on relief of dysphagia and
pain. Endoscopic laser therapy or self-expanding metallic stents can be
used to improve swallowing. Palliative radiotherapy may induce shrinkage
of both squamous cancers and adenocarcinomas but symptomatic
response may be slow. Quality of life can be improved by nutritional
support and appropriate analgesia.
