1
Fifth stage
Pediatric
Lec-9
د.اثل
01/00/2016
HEMORRHAGIC DISEASE OF THE NEWBORN
• A moderate decrease in factors II, VII, IX, and X normally occurs in all newborn infants
by 48-72 hr after birth, with a gradual return to birth levels by 7-10 days of age.
• This transient deficiency of vitamin K–dependent factors is probably caused by lack of
free vitamin K from the mother and absence of the bacterial intestinal flora normally
responsible for the synthesis of vitamin K.
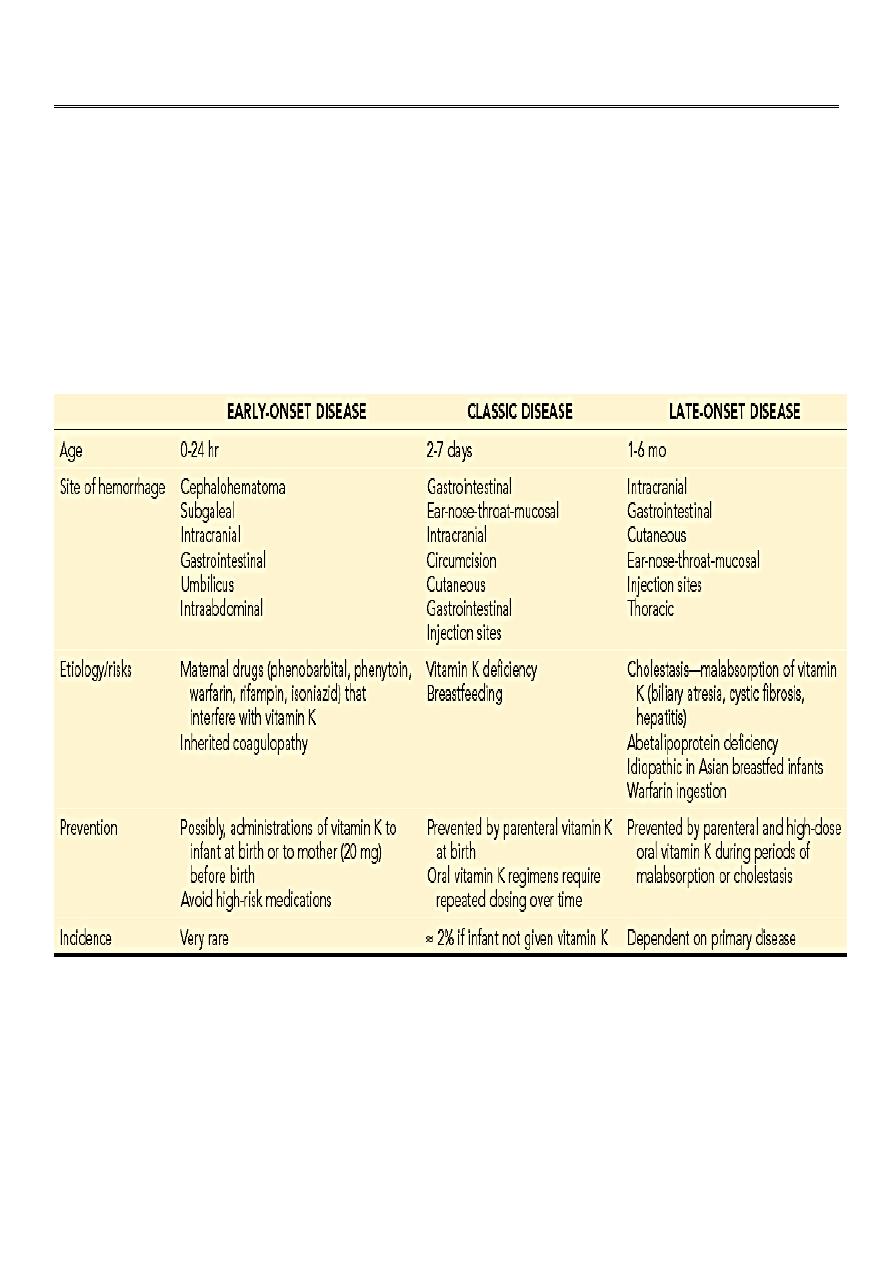
Types of Hemorrhagic Disease Of The newborn
Lab. Investigation
• The prothrombin time, blood coagulation time, and partial thromboplastin time are
prolonged.
• Levels of prothrombin (II) and factors VII, IX, and X are decreased.
2
Prevention & Treatment
• Intramuscular administration of 1 mg of vitamin K at the time of birth prevents the
decrease in vitamin K–dependent factors in fullterm infants.
• The disease may be effectively treated with a slow intravenous infusion of 1-5 mg of
vitamin K1, with improvement in coagulation defects and cessation of bleeding noted
within a few hours.
• Serious bleeding, particularly in premature infants or those with liver disease, may
require a transfusion of fresh-frozen plasma or whole blood. The mortality rate is low
in treated patients.
DDx
• Congenital defects in blood coagulation.
• DIC
• Swallowed blood syndrome
3
Fifth stage
Pediatric
Lec-11
د.اثل
01/10/2016
Neonatal Seizures
About 2–4/1000 live births suffers of seizure disorder. Usually occur 12–48hr after
delivery.
Can be generalized or focal, and tonic, clonic, or myoclonic.
Subtle seizure patterns (lip-smacking, limb-cycling, eye deviation, apnoea, etc.) can
be difficult to identify or differentiate from other benign conditions that may mimic
seizures as:
• Startle or Moro reflexe.
• Normal jittery movements (fine, fast limb movements that are abated by
holding affected limb).
• Sleep myoclonus (REM movements).
ETIOLOGY
Brain injury:
• HIE.
• Intracranial haemorrhage.
• Cerebral infarction (ischaemic or haemorrhagic).
• Cerebral oedema.
• Birth trauma.
CNS infection:
• Meningitis (e.g. GBS, coliforms).
• Encephalitis (e.g. HSV, CMV).
Cerebral malformations.
Kernicterus.
Metabolic:
• Hypoglycaemia.
• Hypo- or hypernatraemia.
• Hypocalcaemia, hypomagnesia.
• Pyridoxine dependent seizures.

4
Neonatal withdrawal from maternal medication or substance abuse.
Rare syndromes:
• Benign familial neonatal seizures (autosomal dominant).
• Early myoclonic encephalopathy.
Idiopathic: with improved access to neuroimaging, fewer infants are being
categorized as ‘idiopathic’ seizures. Neonatal stroke is increasingly recognized
TREATMENT
• Immediate ABC: maintain airway, give O2, insert IV canula.
• Indication anticonvulsants:
>3seizures/hr
single seizure lasting >3–5min particularly if evidence of cardio-respiratory
compromise.
• First-line anticonvulsant:
IV phenobarbital 20-40mg/kg bolus
Maintenance dose 5mg/kg/day.
• Then treat the underlying cause.
