1
Dermatology sessions
Description of any skin lesion:
Site of the lesion (part of the body)
hand, face, leg, scalp, etc.
Number of lesion
single, multiple, and write the exact number if you can.
Arrangement of the multiple lesions
discrete, coalesce, grouped, linear, circular.
Distribution of the lesions:
o On extensor surface: elbow, knee, sacral region.
o On flexor surface: axilla, groin, sub-mammary, umbilicus.
o On distal site: on fingers called acral.
o Central site: like chickenpox.
o Sun exposed area: face, hand, neck, upper chest.
o Localized: unilateral or follow dermatome.
o Generalized: or called universal.
Type of lesion primary or secondary lesion.
Size of the lesion from mm to cm.
Color of the lesion silvery, erythematous, pink.
Shape of the lesion irregular, circular, flat, elevated.
Border of lesion like active border in some lesion.
Margin of the lesion well defined (psoriasis), ill defined (dermatitis).
Types of lesion:
Primary skin lesions:
Macule
A localized area of color or textural change in the skin.
Papule
A solid elevation of skin <5 mm in diameter.
Plaque
A palpable elevation of skin >2 cm diameter and <5 mm in height.
Vesicle
A clear, fluid-filled blister <5 mm in diameter.
Bulla
A fluid-filled blister >5 mm in diameter.
Pustule
A visible collection of pus in a blister.
Abscess
A localized collection of pus.
Wheal
A transitory, compressible papule or plaque of dermal edema, red or white,
indicating urticarial.
Angioedema a diffuse swelling of edema that extend to the subcutaneous tissue.
Nodule
A solid elevation of skin >5 mm in diameter.
Papilloma
A nipple-like projection from the surface of the skin.
Purpura
Extravasation of blood resulting in redness of skin or mucous membranes.
Ecchymosis
A macular red or purple haemorrhage, >2 mm in diameter, in skin or
mucous membrane.
2
Hematoma: a swelling form gross bleeding.
Burrow
A tunnel in epidermis caused by a parasite, e.g. Acarus in scabies.
Comedo
A plug of sebum and keratin wedged in a dilated pilosebaceous orifice on
the face.
Telangiectasia
Dilated dermal blood vessels resulting in a visible lesion.
Secondary skin lesions:
Scale
Accumulation of easily detached fragments of thickened keratin.
Crust
Dried exudate, e.g. serum, blood or pus, on the skin surface.
Ulcer
A circumscribed area of skin loss extending into the dermis.
Excoriation
A superficial abrasion, often linear, due to scratching.
Erosion
A superficial break in the epidermis, not extending into dermis, heals
without scarring.
Fissure
A linear split in epidermis, often just extending into dermis.
Sinus
a cavity or channel that permit the escape of pus or fluid.
Scar
Replacement of normal tissue by fibrous connective tissue at the site of an
injury.
Atrophy
Loss of epidermis, dermis or both, thin, translucent and wrinkled skin,
visible blood vessels.
Stria
Atrophic linear band in skin, white, pink or purple, from connective tissue
changes.
Other skin lesions:
Callus
Local hyperplasia of horny layer on palm or sole, due to pressure.
Cyst
A nodule consisting of an epithelial-lined cavity filled with fluid or semisolid
material.
Erythema
Redness of the skin due to vascular dilatation.
Freckle
A macular area showing increased pigment formation by melanocytes.
Lichenification
Chronic thickening of skin with increased skin markings, from rubbing
or scratching.
Milium
A small white cyst that contains keratin.
Petechia
A haemorrhagic punctate spot 1–2 mm in diameter.
See photos @ WWW.muhadharaty.com/lecture/3472
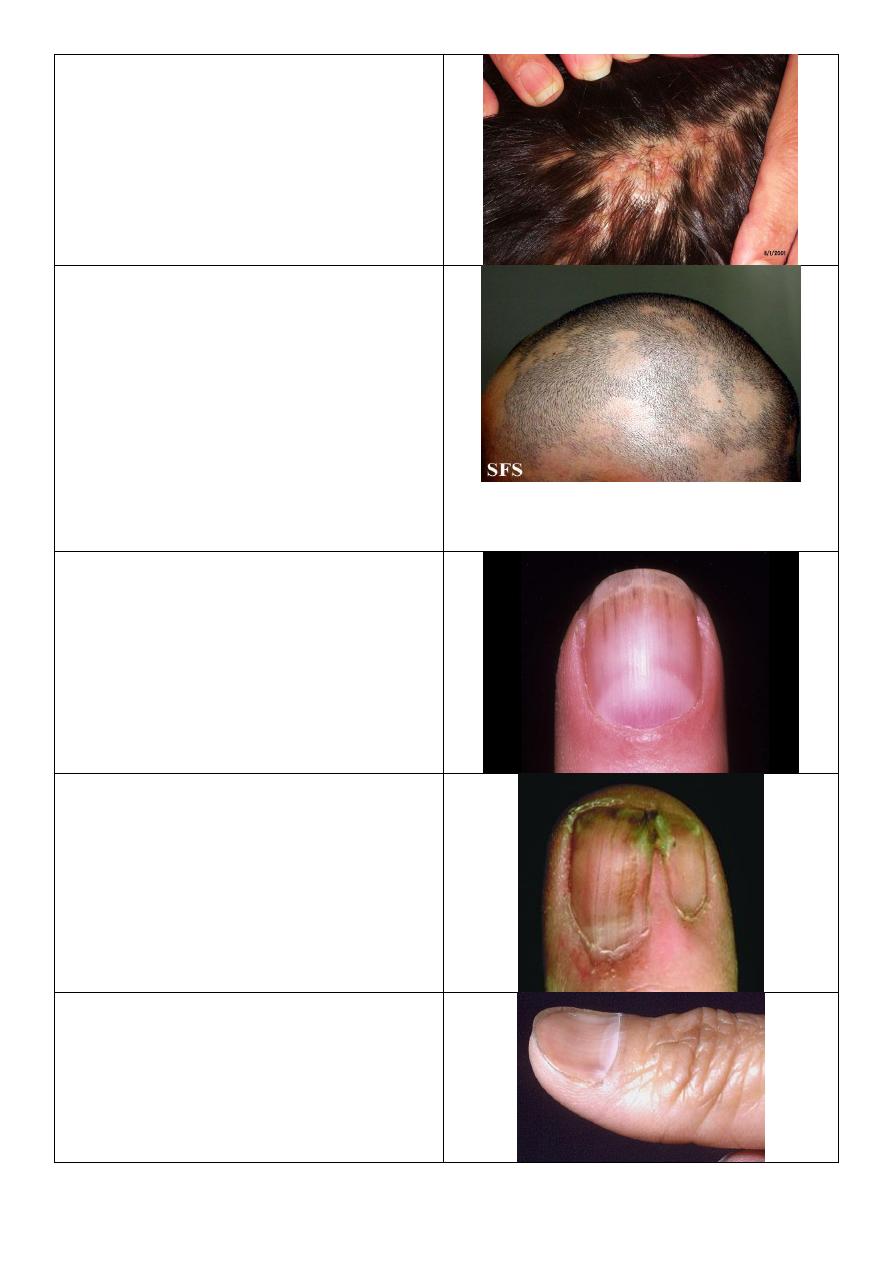
Hair loss:
Localized:
o Scarring Lichen planus, discoid lupus.
o Non scarring trachiotillamonia,
alopecia areata.
Diffuse:
o Scarring radiotherapy, burn, trauma.
o Non scarring cytotoxic drugs.
Causes:
Normal hair + abnormal skin Psoriasis,
seborrheic dermatitis.
Normal skin + abnormal hair (loss)
trachiotillomonia, alopecia areata, traction
alopecia.
Skin and hair are abnormal tenia capitis.
3
Photos form doctor:
Description
Photo
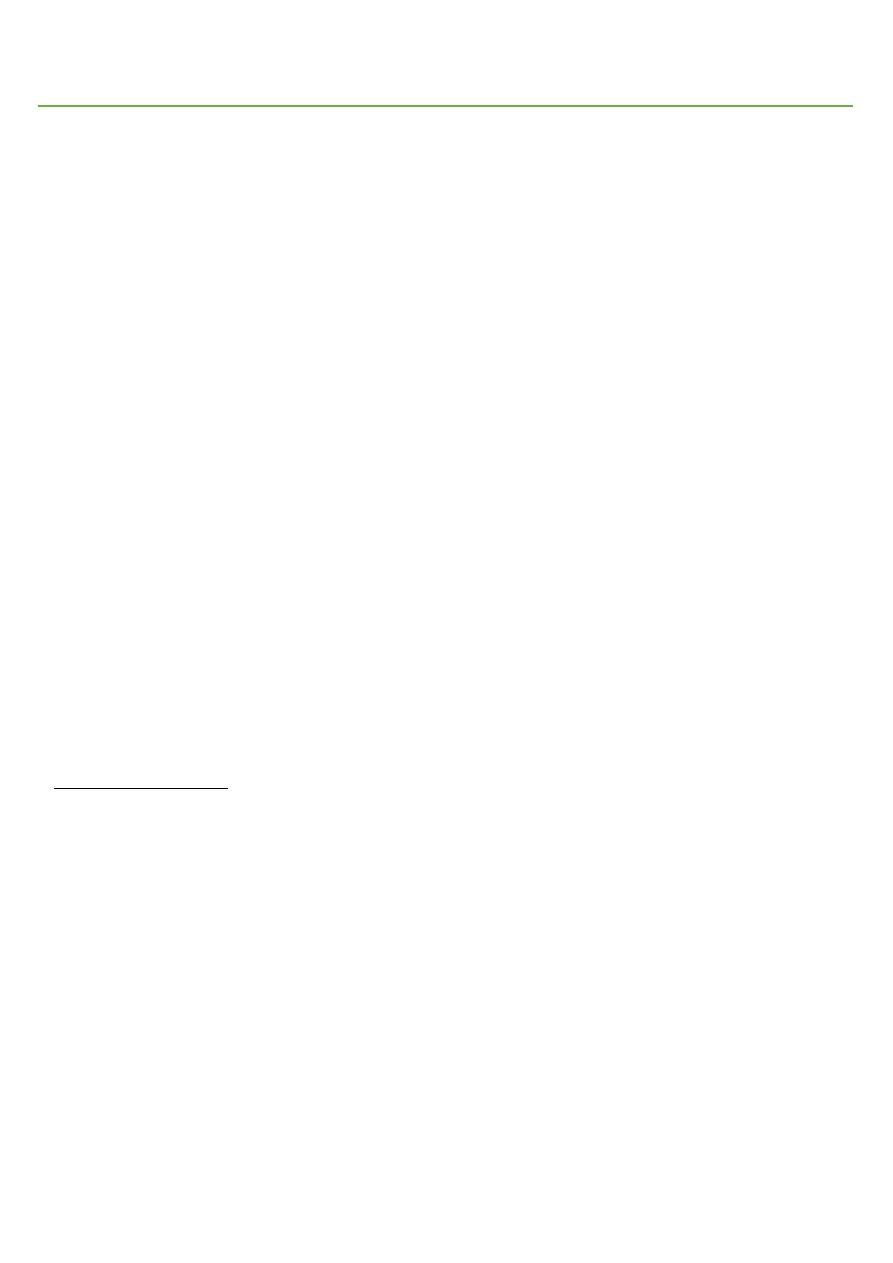
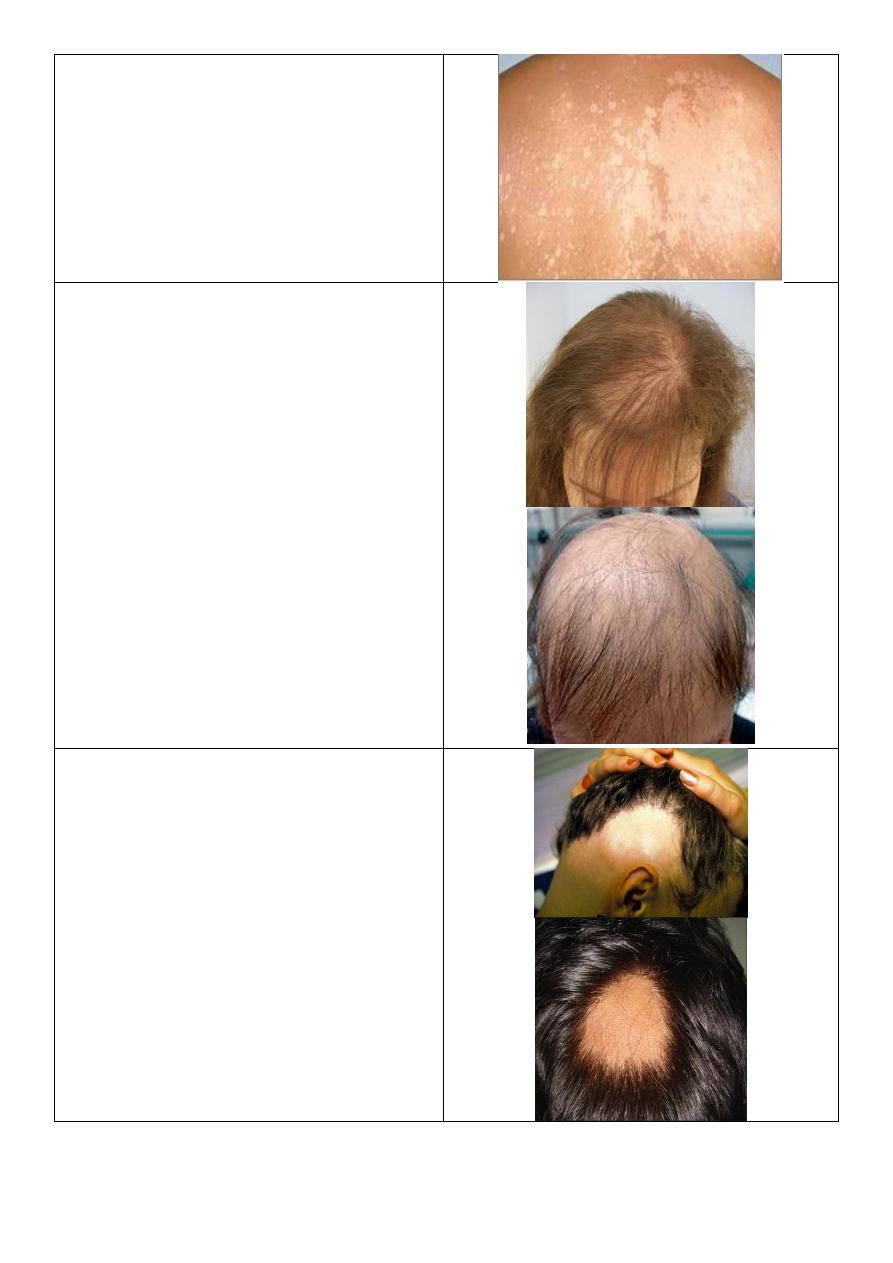
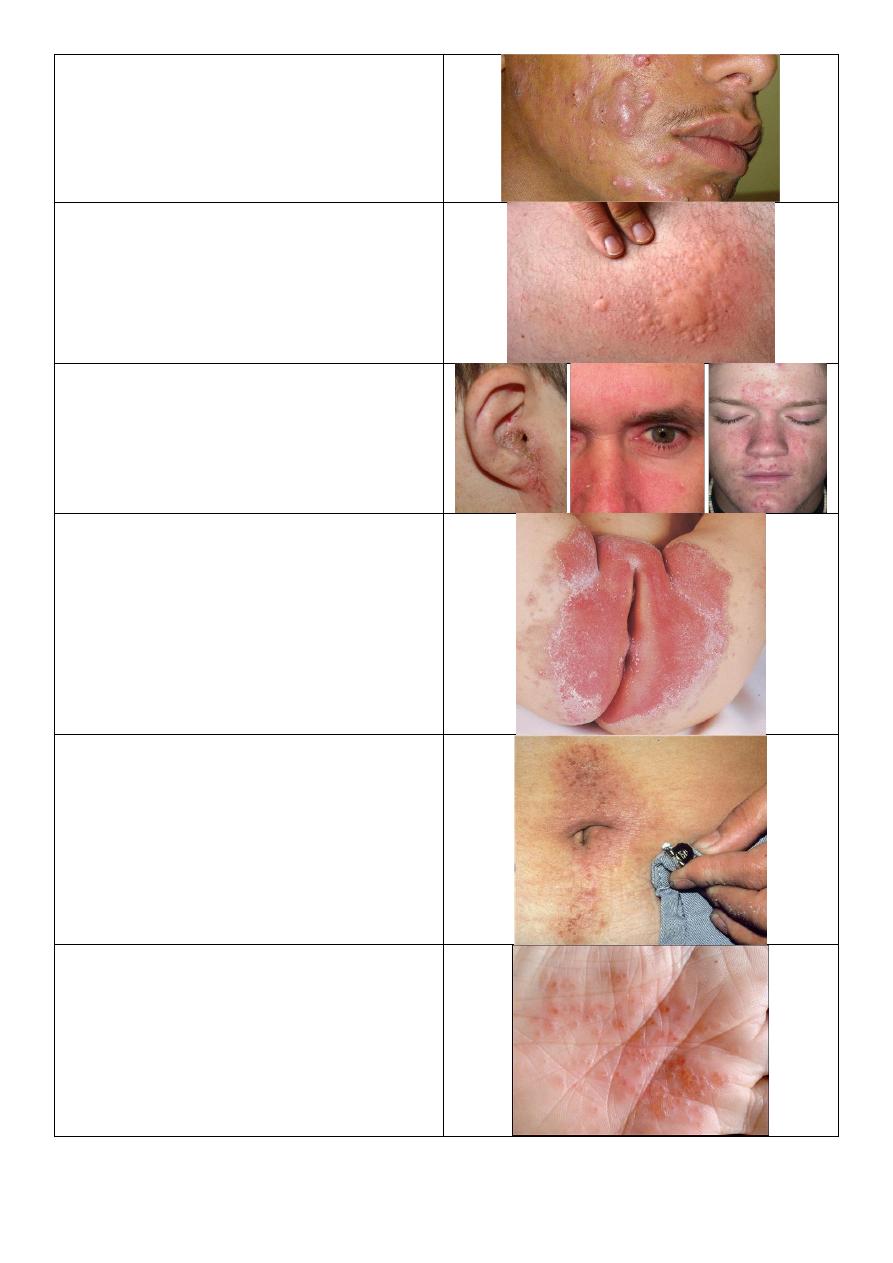
Psoriasis:
o Site: extensor part of elbow.
o Number: single.
o Type: primary (plaque) and secondary
(scale).
o Shape: oval and flat elevation.
o Size: few cm in diameter.
o Color: erythematous (red) plaques and
silvery and heavy scales.
o Margin: well defined.
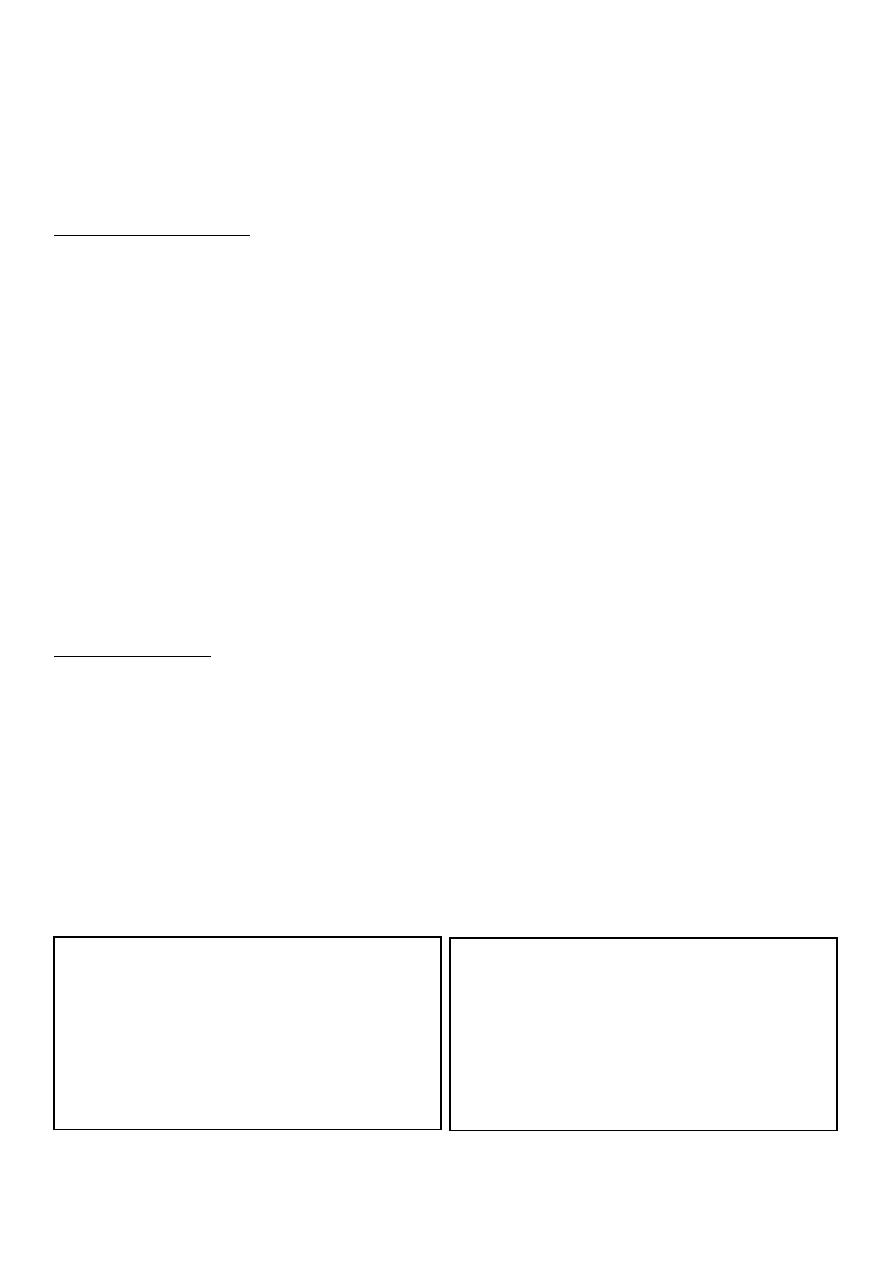
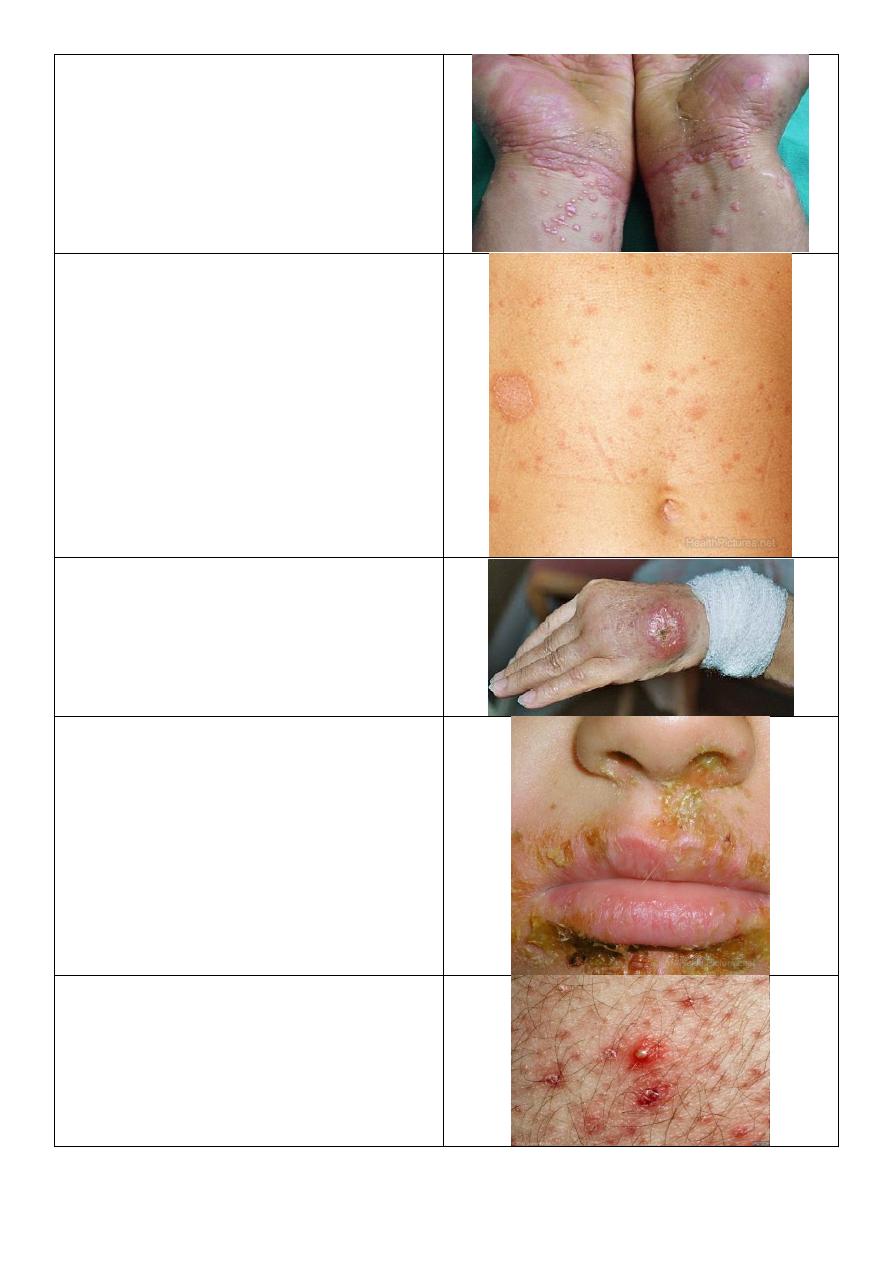
Nail changes in psoriasis:
o All nails are affected.
o Nail pitting.
o "End on" view Separation of nail
from nail bed called onycholysis,
thickening of nail, subangular
hyperkeratosis.
o "Above" view yellow color.
o "Lateral" view see the shape,
convexity, concavity of nail.
Note:
Nail changes in psoriasis occur before or
during or after the psoriasis, but it not
occur in all patients.
It may lead to psoriatic arthritis:
seronegative and DIPs affected.
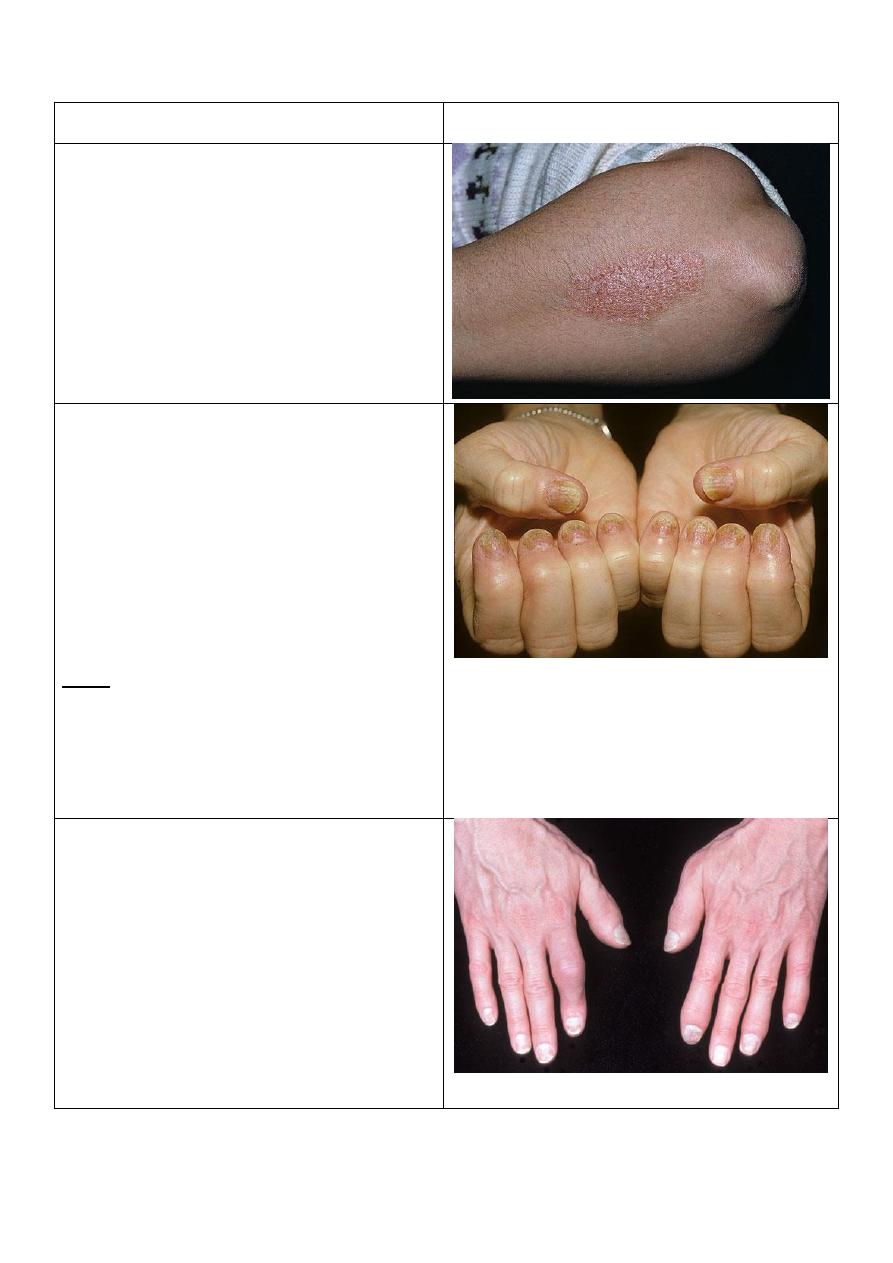
Psoriatic arthritis:
o The DIPs are affected.
o This is the typical picture.
o Sometimes the DIPs are not affected.
o Patterns of psoriatic arthritis:
1. Oligoarticular assymmetric arthritis.
2. Polyarticular symmetric arthritis (RA-like).
3. DIP joint predominant.
4. Destructive polyarthritis (arthiritis
mutilans).
5. Ankylosing spodylitis and sacroiliitis.
4
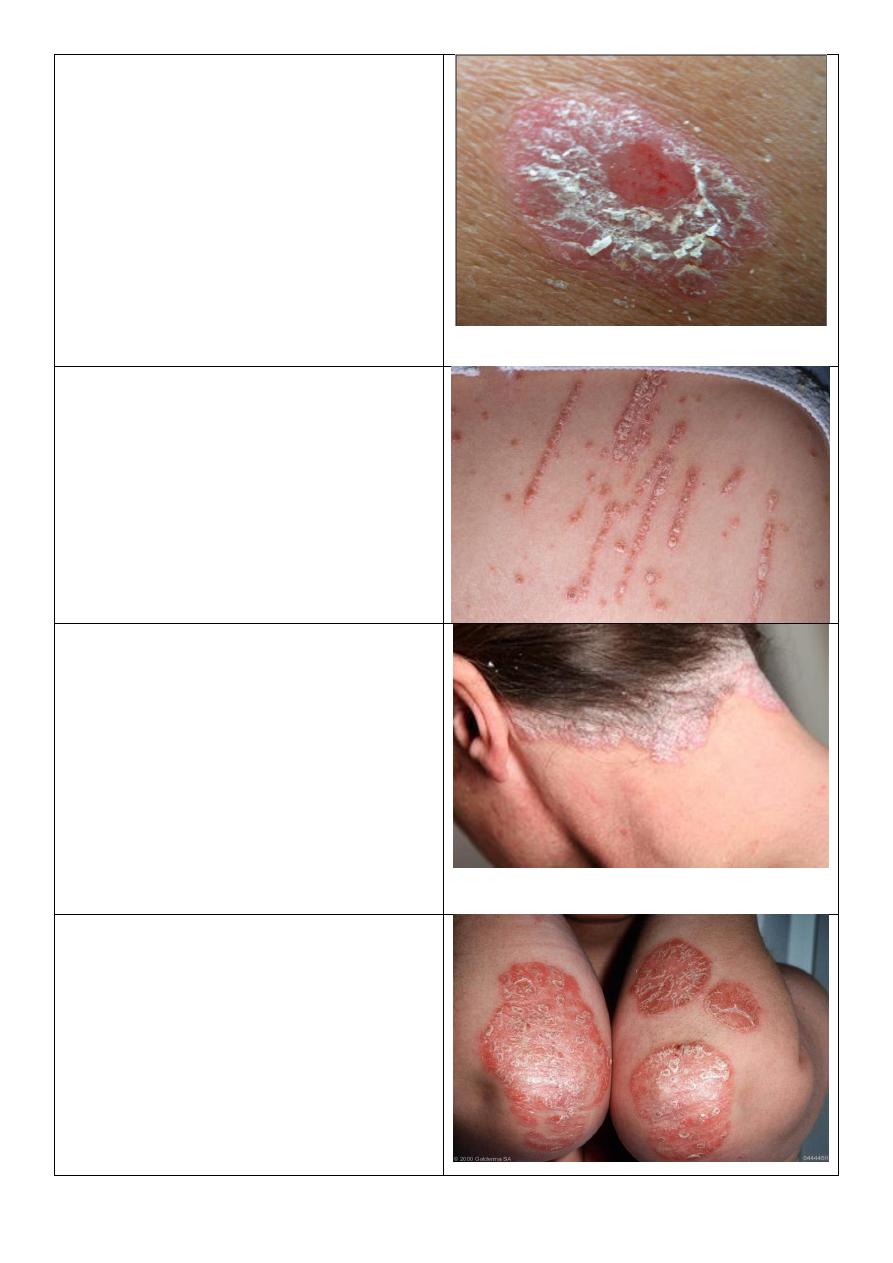
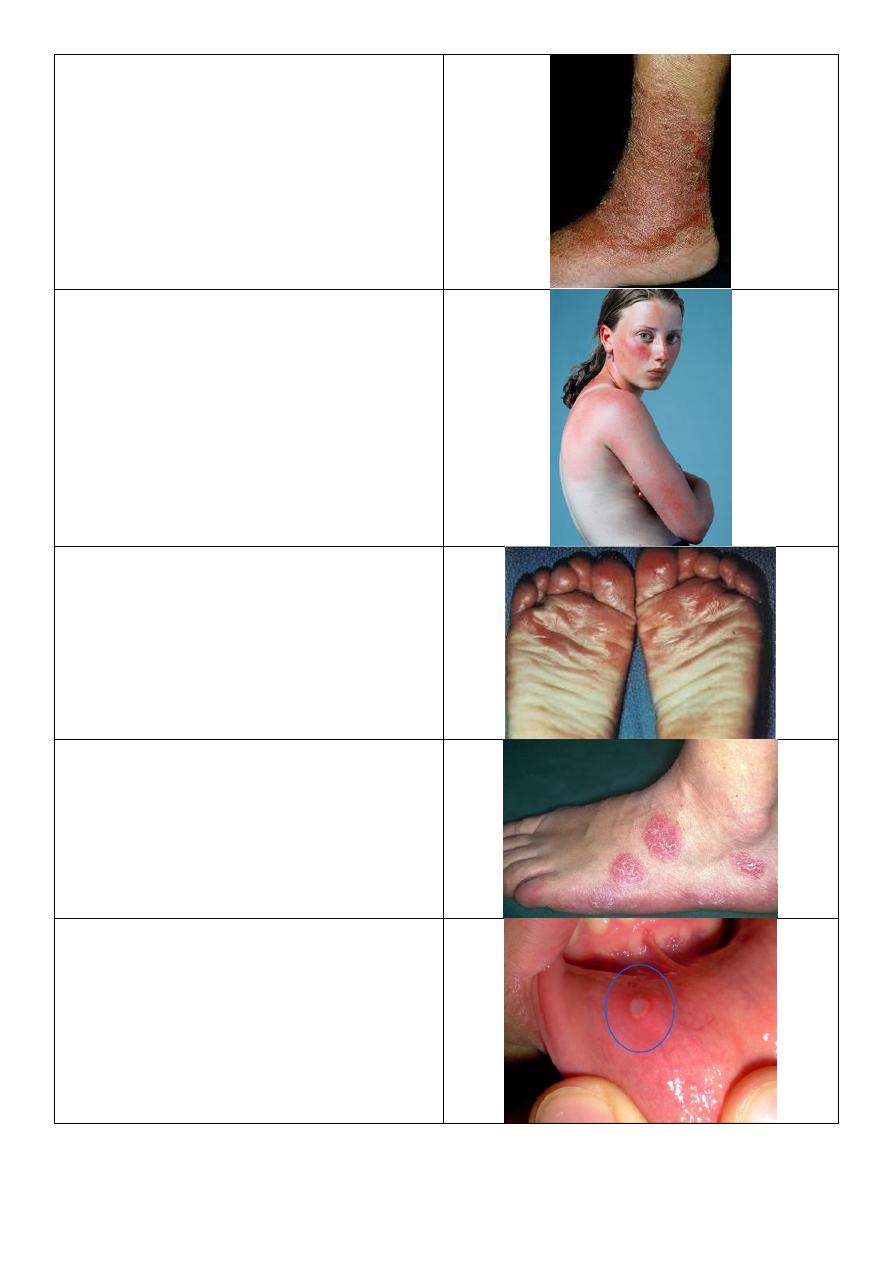
Psoriasis:
o Number: single.
o Type: primary lesion then the patient
scratch it lead to bleeding (Auspitz sign)
o Shape: oval.
o Size: few cm in diameter.
o Color: pink primary lesion, and white
scales.
o Margin: well defined.
o There are pin-point bleeding Auspitz
sign.
o This not occur in eczema.
Koebner phenomenon:
o Lines of scratching.
o Occur in psoriasis, warts, vitiligo.
o koebner phenomenon spread of a
disease in uninvolved skin by trauma.
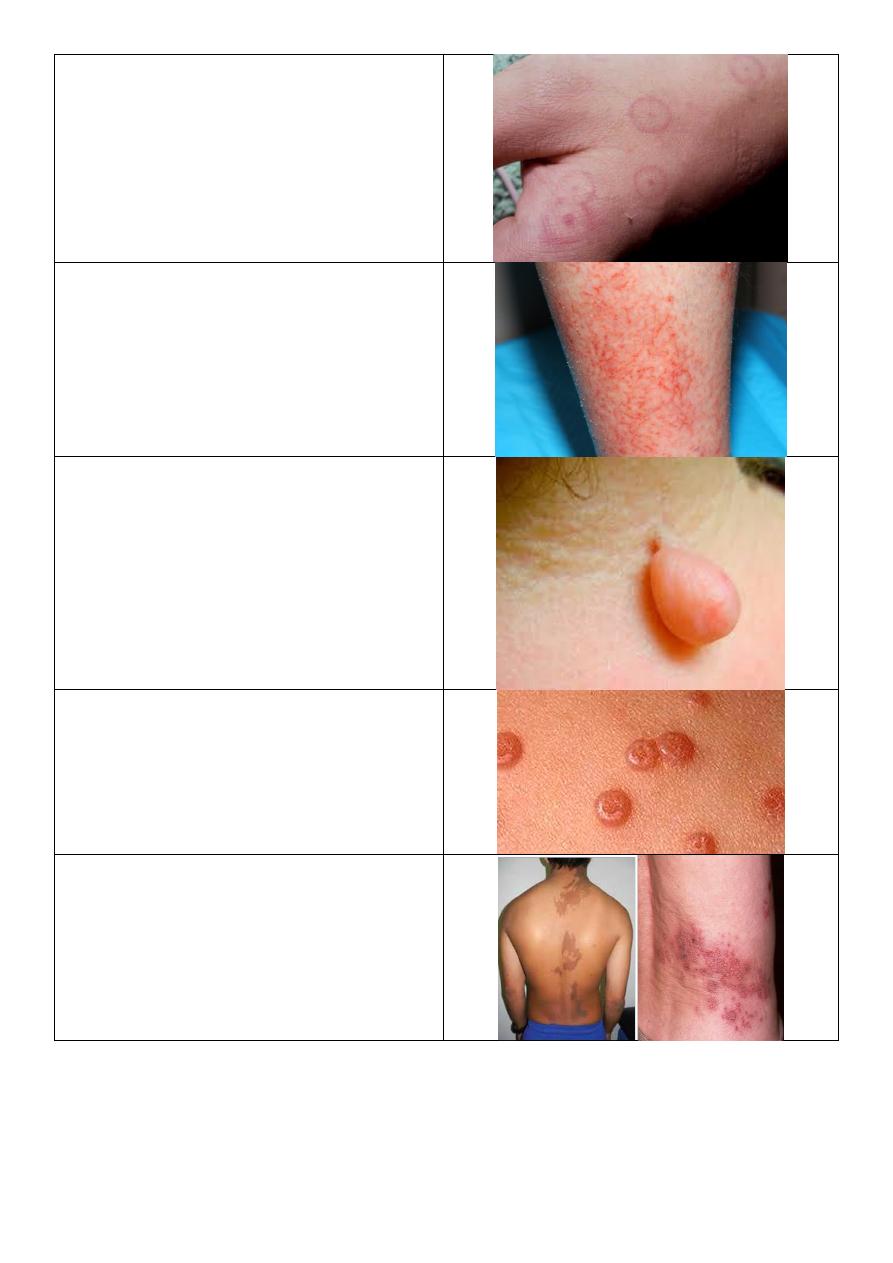
Prosiasis:
o Site: scalp.
o Color: Silvery.
o Lesion: heavy scaly scalp.
o Occur in: psoriasis and seborrheic
dermatitis.
o Differences:
Seborrheic: yellowish greasy scales.
Psoriasis: powdery dry silvery scales.
Seborrheic: Stop at hair line.
Psoriasis: extend beyond hair line.
Chronic plaque psoriasis:
o Distribution: on extensor surface
elbow, knee, sacral region.
o Lesion: plaques.
o Covered by scales thick, white,
powdery.
o Color: erythematous.
o Margin: well defined.
o Scratching lead to Auspitz sign.
5
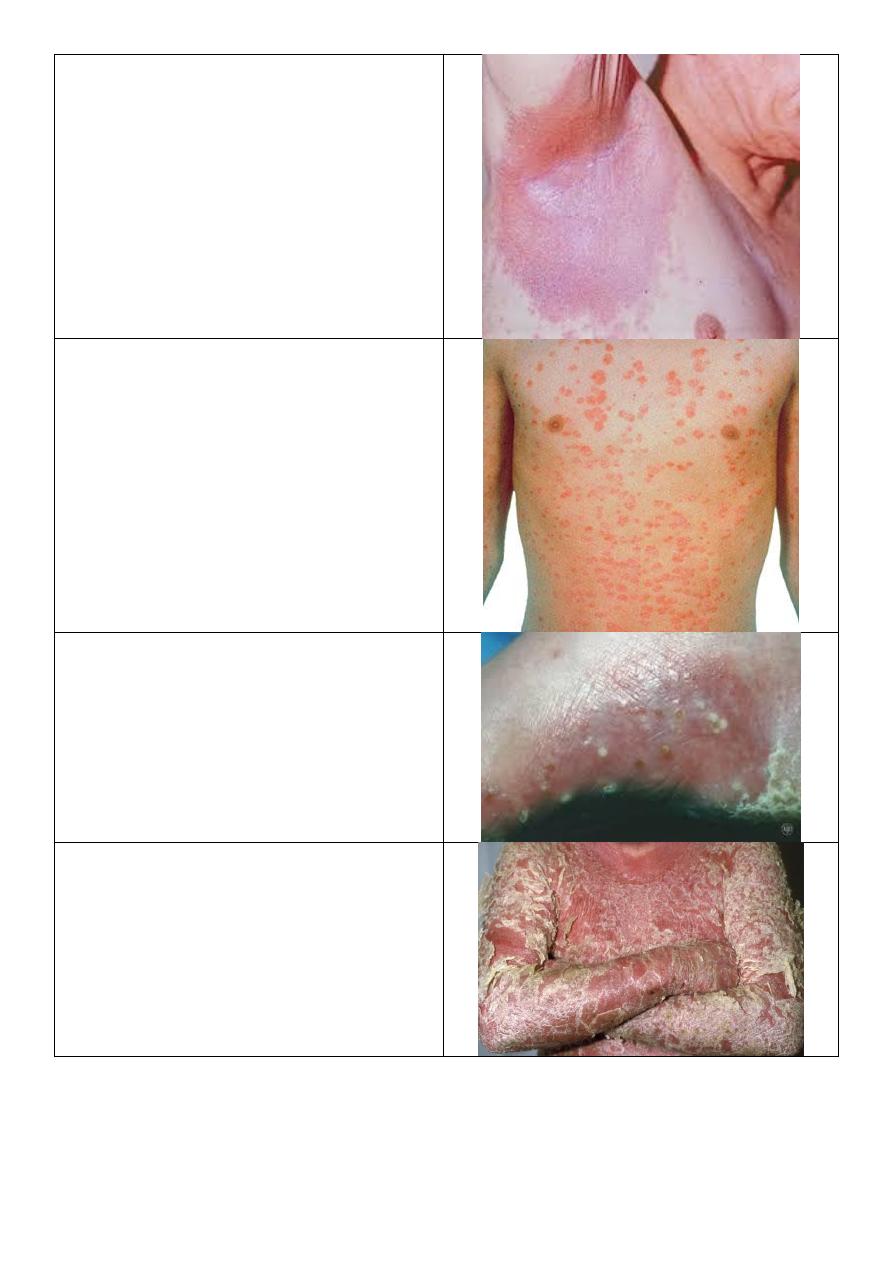
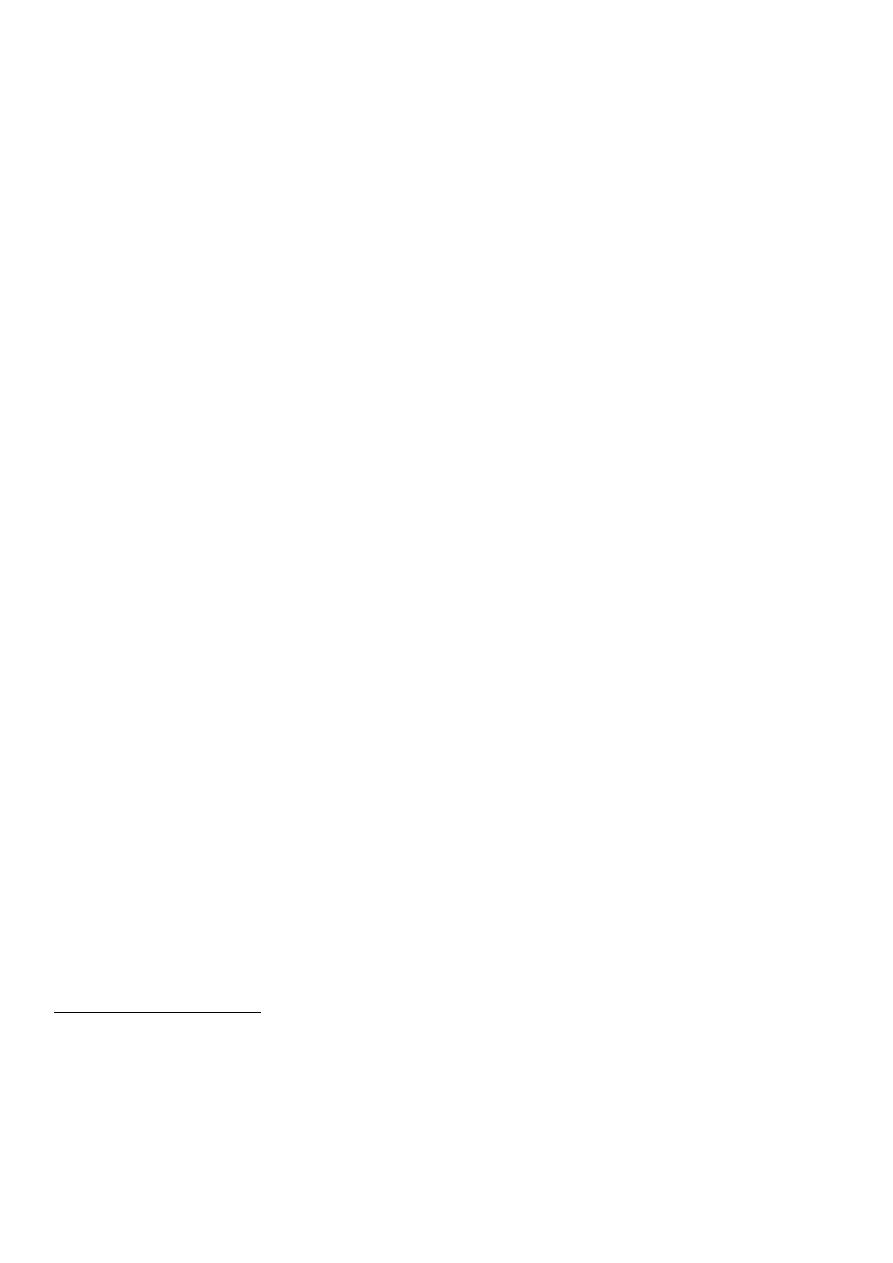
Flexor psoriasis:
o In axilla, groin, sub-mammary,
umbilicus.
o No scales because it is wet area.
Guttate psoriasis:
Tear drop lesions.
Occur in young children.
Pustular psoriasis:
Localized or generalized.
Erythrodermal psoriasis:
Red or erythematous exfoliation.
6
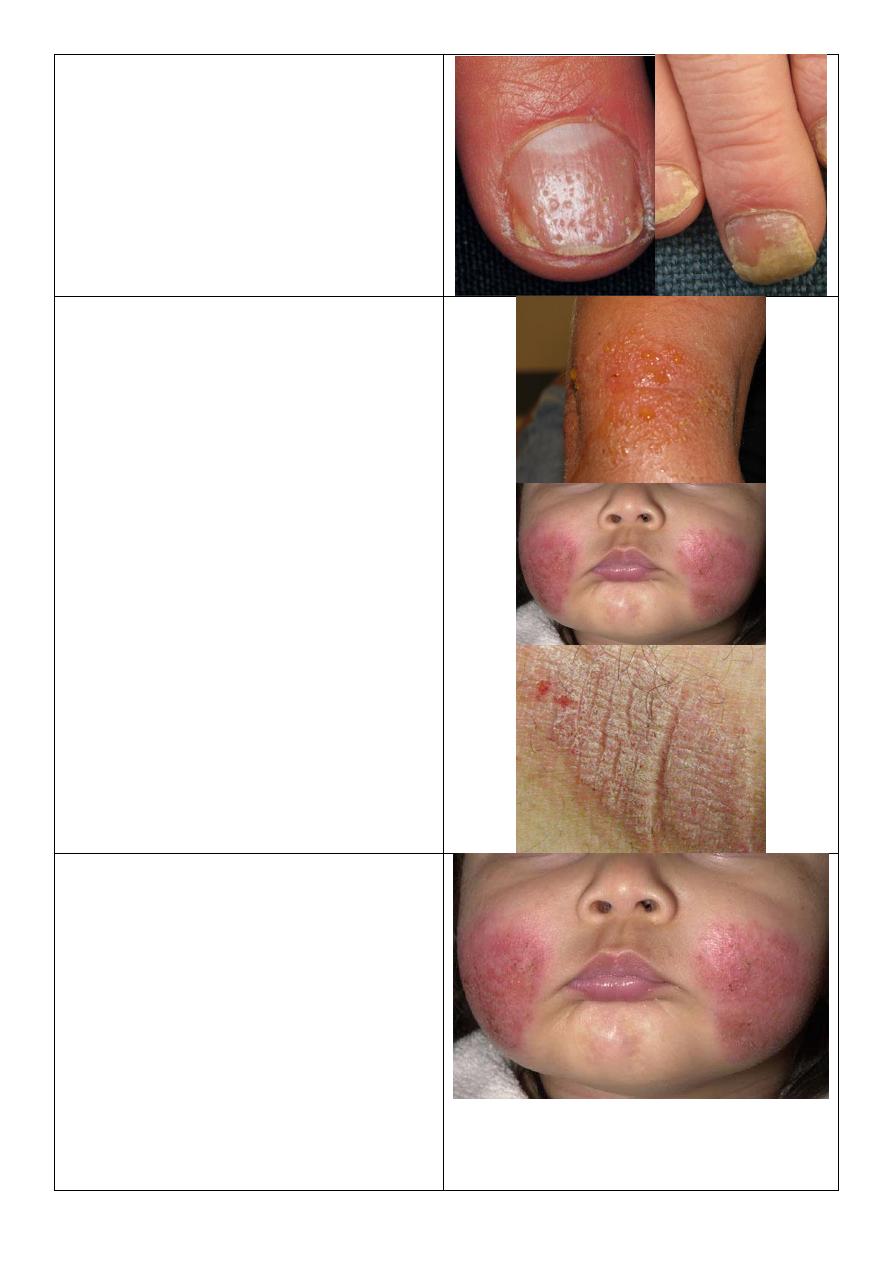
Psoriasis of nail:
o Pitting.
o Nail separation.
o Yellow discoloration.
Stages of eczema (dermatitis):
Acute stage:
o Ill defined.
o Small multiple vesicles.
o Oozing serious fluid.
Subacute stage:
o Erythematous plaque with ill-defined
border
Chronic stage:
o Ill defined.
o Lignification: thickening of skin +
exaggeration of skin marks.
Types of dermatitis Atopic dermatitis,
Seborrheic dermatitis, Stasis dermatitis, Contact
dermatitis.
Atopic dermatitis:
o Major criteria of atopic dermatitis:
1- Severe itching.
2- Typical lesion + predilection
according to age.
3- Positive personal or family history of
other atopic diseases like asthma.
4- Chronic relapsing.
o Predilection:
Infant: in cheek.
Little older: cheek, elbow, knee.
Adult: generalized.
o Prognosis: 2/3 improve – 1/3 persist.
7
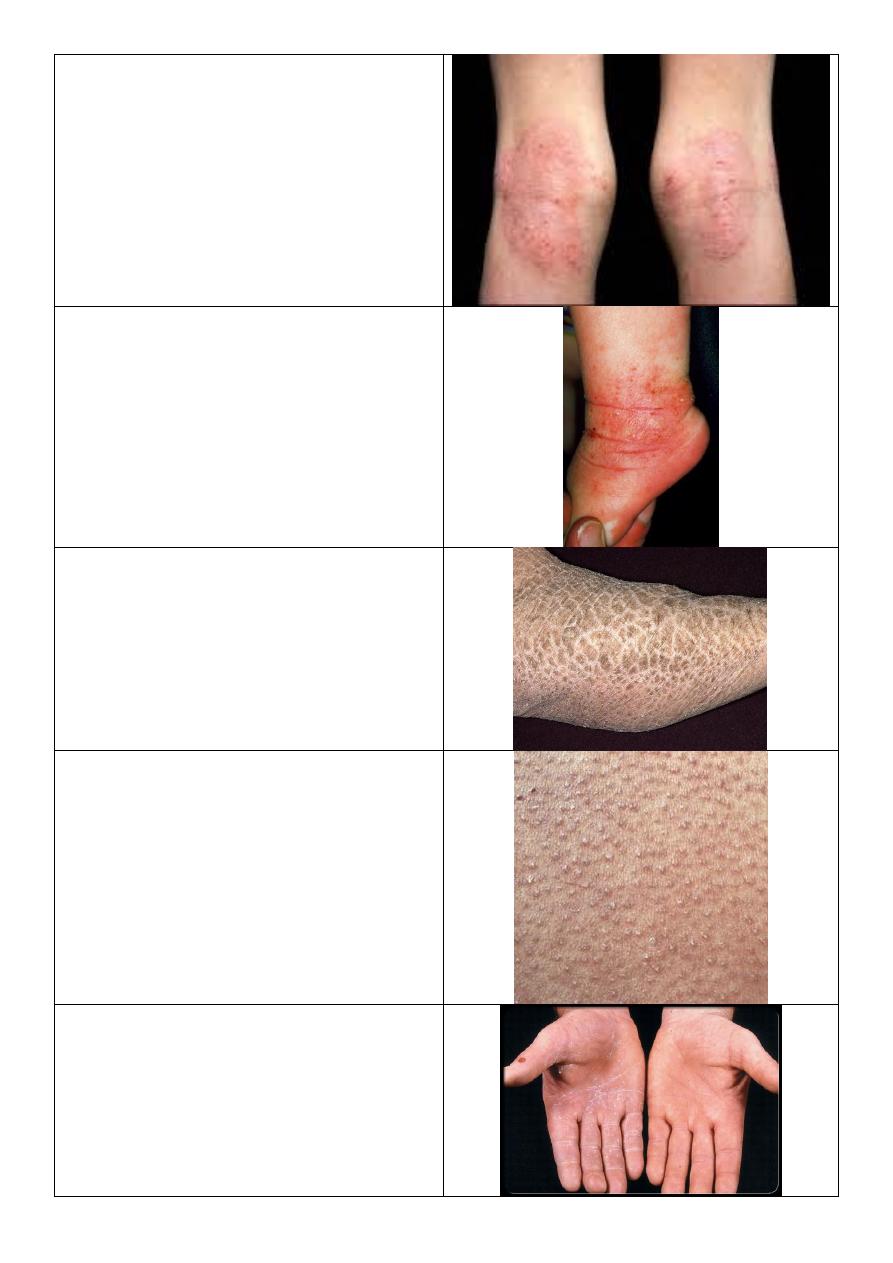
Atopic dermatitis:
o Severe itching.
o Childhood stage.
o In popliteal fossa and antecubital fossa.
o Lignification
Dermatitis:
o Severe itching.
o Infant age.
o
Occur in ankle, elbow, wrist.
Ichthyosis vulgaris:
Dry polygonal scales.
Keratosis pilaris:
o Keratosis = thickening.
o Pilaris = related to hair.
o Tiny thickening (keratosis) at hair
follicles.
o
Occur in shoulder, upper thigh, buttock.
Name the condition? Atopic patient.
Tinea manuum:
o Unilateral (right hand).
o Scales concentrating in hand creases.
o Investigation: KOH.
o The cause is outside the body like fungal
infection,, because it is unilateral.
8
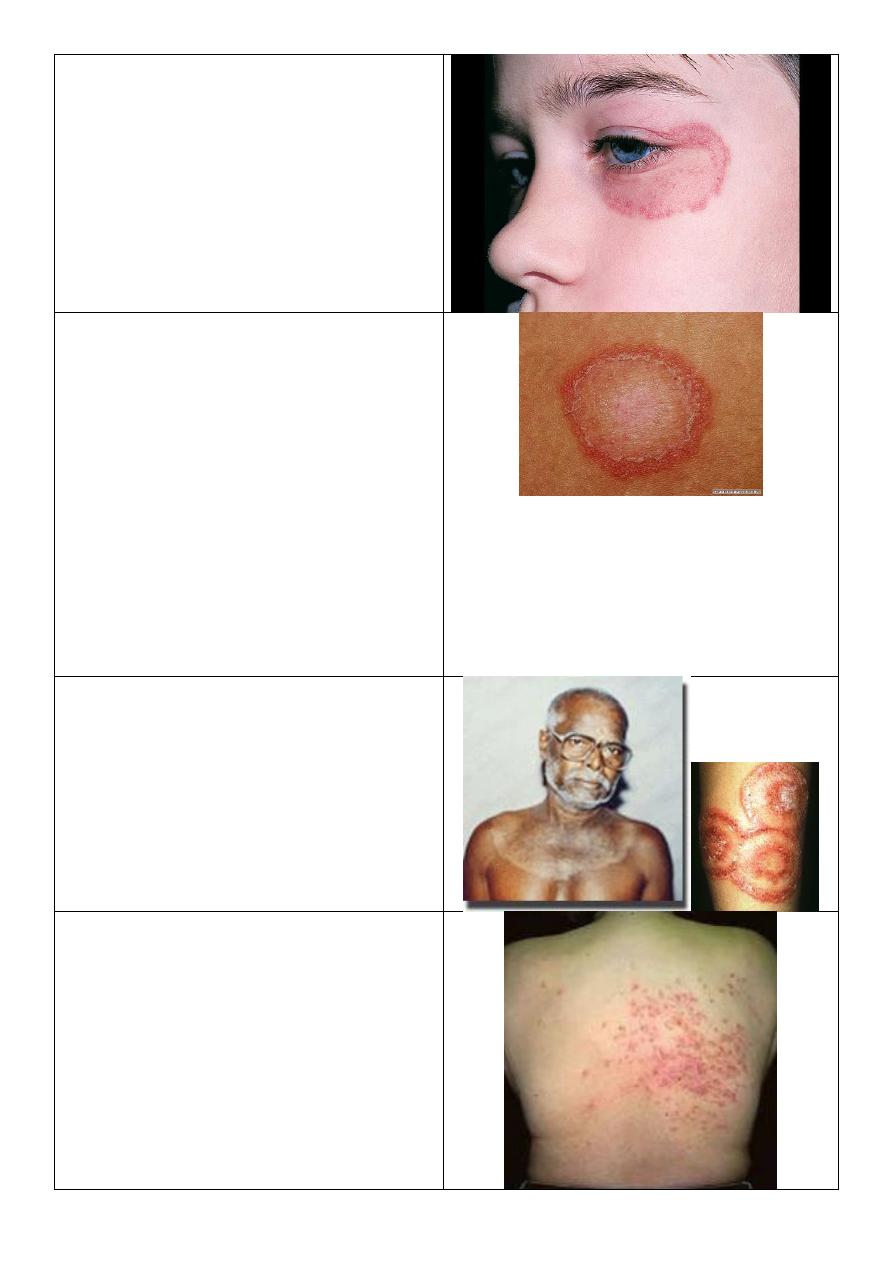
Tinea fasciae or corporis:
o Unilateral lesion (affecting the left eye).
o Erythematous plaque – well demarcated
o Active border with relatively central
healing.
o Due to localized problem from outside
like infection (fungal).
Active border in tenia:
o Round plaque.
o The border is more red and more scaly
and more elevated than the center.
o There is active border and relatively
healed center.
o The cause is dermatophyte it will eat
the keratin around it then eat the
surrounding keratin then extend and
eat more keratin so the lesion increase
in size.
o This is called tenia or ring worm.
o The tenia is named according to the site
of the lesion.
Tinea corporis:
o Has active border.
o Large size.
o Hand polycyclic lesion called
Tinea circinata
Tenia incognito:
o Due to steroid therapy (because it looks
like eczema).
o Unclear picture.
o The disease not treated by the steroids.
o Action of steroids anti-inflammatory,
vasoconstriction, anti-proliferative.
o Steroid facies
bright red, atrophy of
skin, appearance of hair, acne, very thin
skin.
9
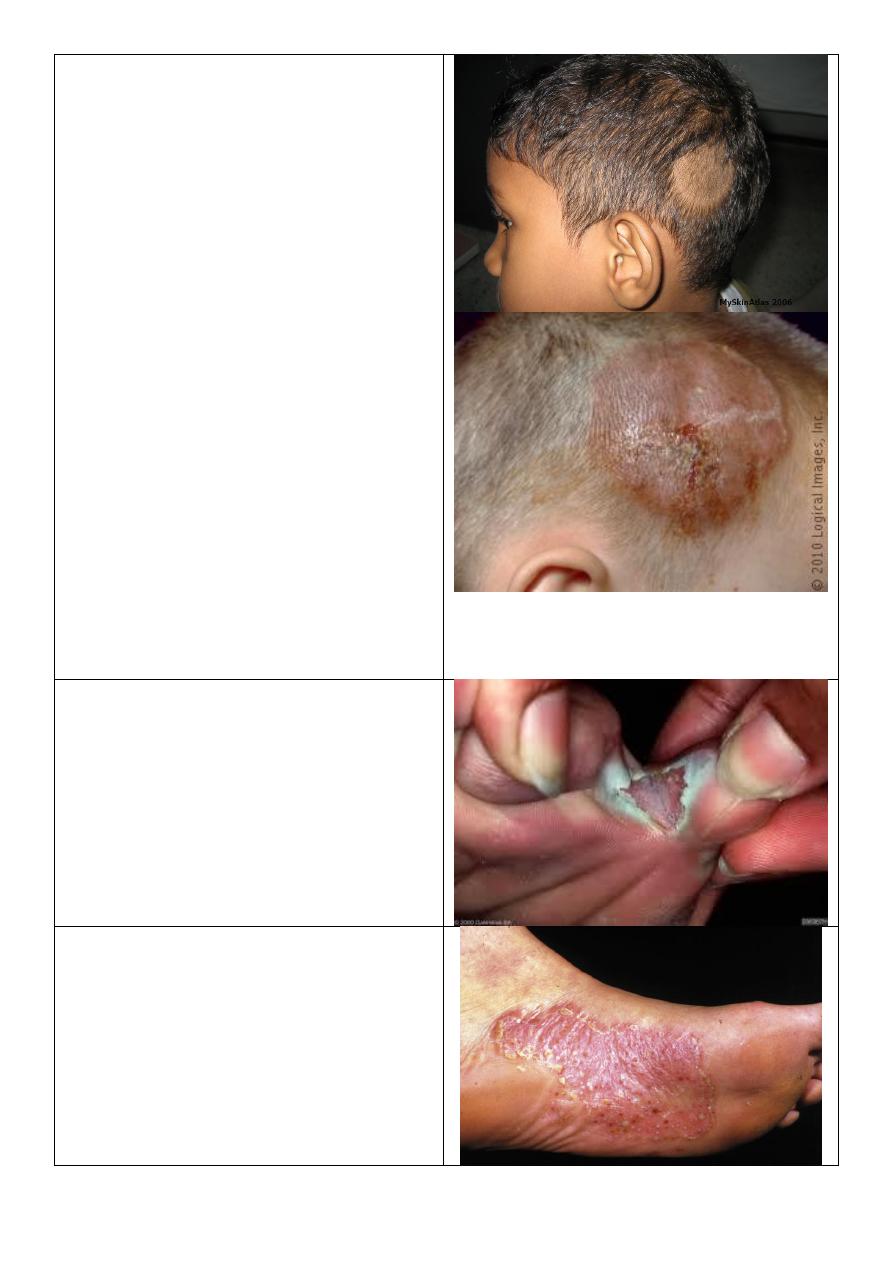
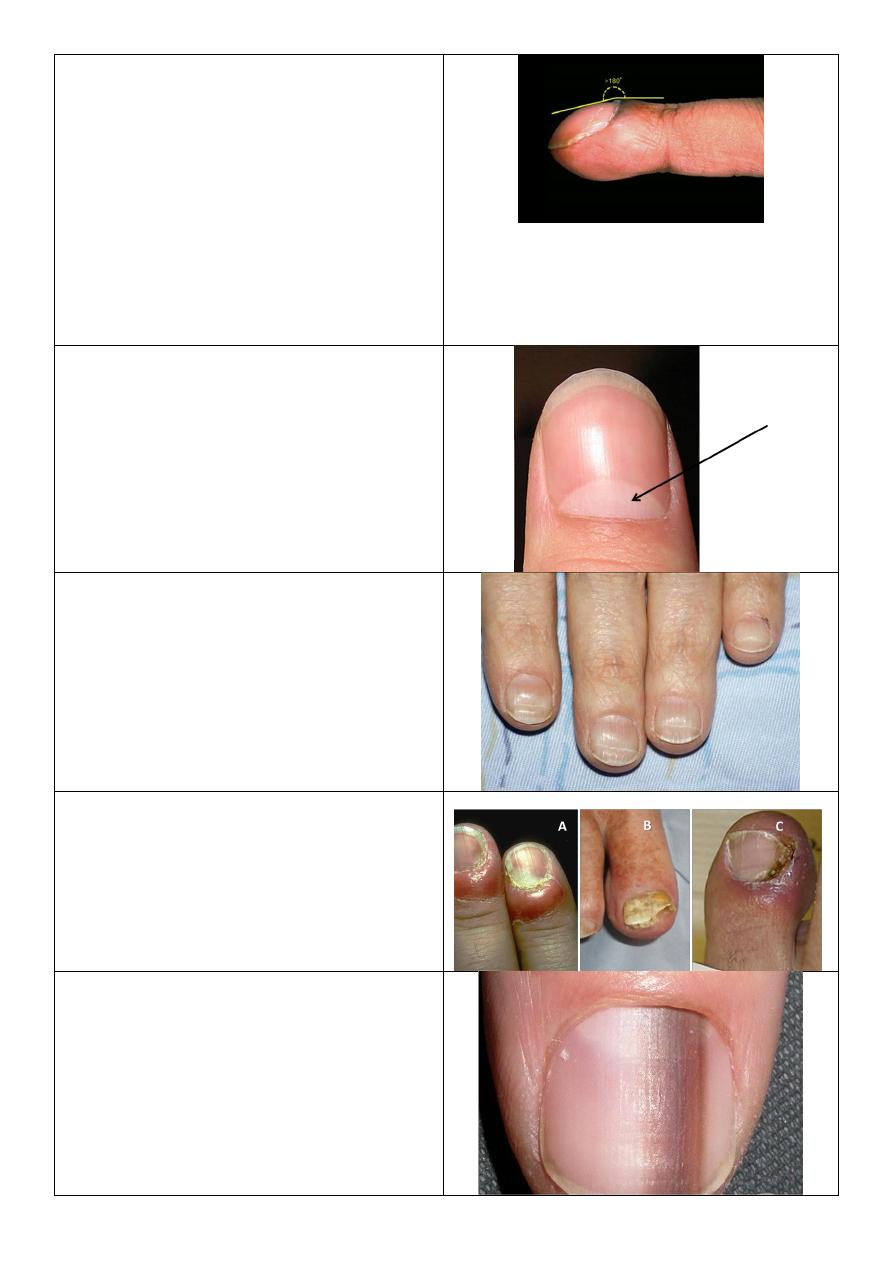
Tenia capitis:
o School age child.
o There is localized area of hair loss.
o No complete devoid of hair and there is
scanty hair in the area.
o Broken hair.
o Early destructible hair.
o Lusterless hair.
o Scalp scaly, inflammatory.
Alopecia areata:
o Round patch.
o Completely devoid of hair.
o Normal skin of scalp.
o School age child and other ages.
Causes of hair loss:
o Generalized.
o Localized:
Tenia capitis.
Alopecia areata.
Male pattern.
Burn of hair.
Trichotellomania (psychological).
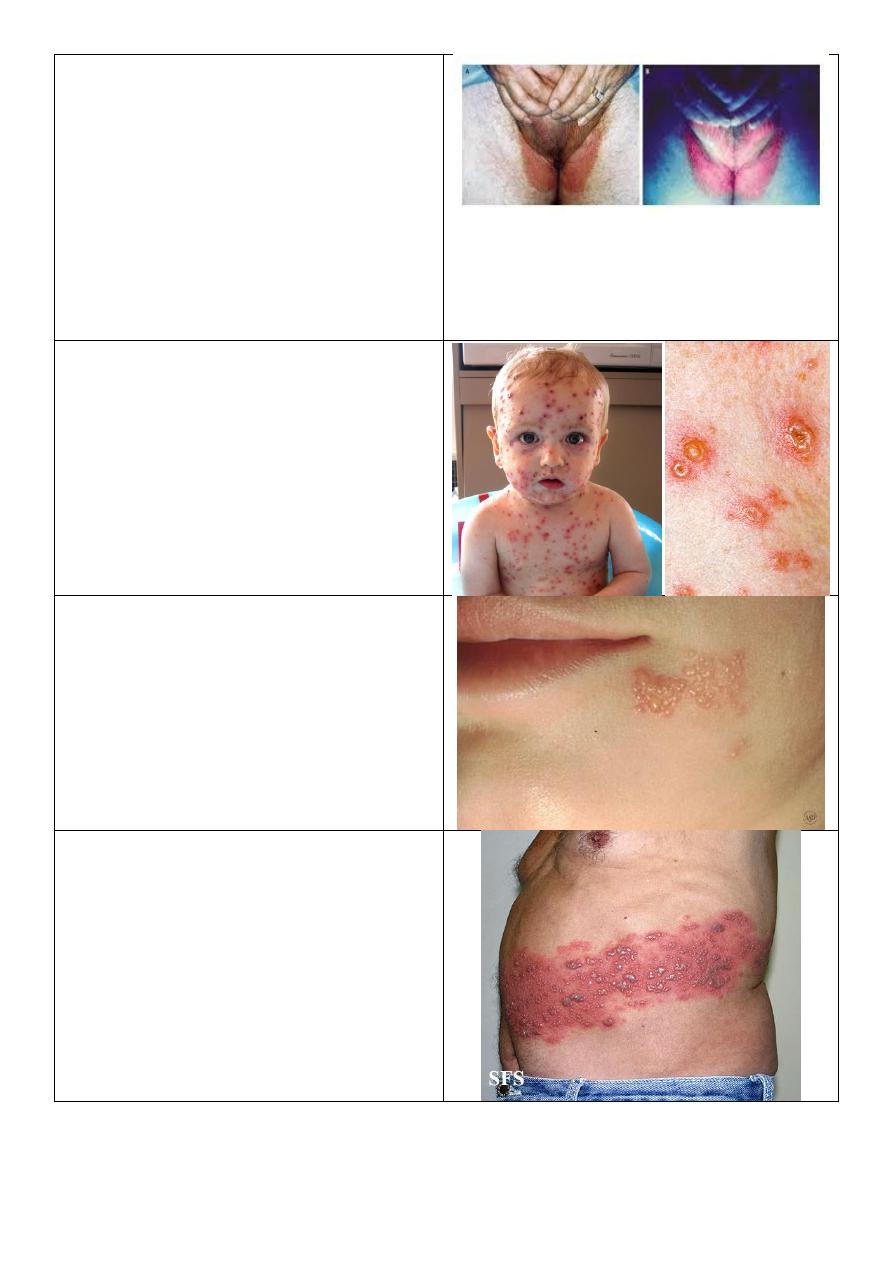
Athletes foot (tinea pedis):
o Erythematous, eroded.
o Exfoliation.
o Affect webspace.
o Mall odor due to superadded bacteria.
Tinea pedis:
o Vesico bullous.
o DDx: pustular psoriasis.

10
Tenia pedis:
o Scaly type.
o Affect whole sole then dorsum then
nails.
Tinea cruris:
o Old name: eczema marginatium.
o In upper inner thigh.
o Genitalia is free.
o Active border.
o Not symmetrical.
o Red brown color.
o Dry area.
Candidiasis:
o Folded area.
o Bright red.
o Macerated skin.
o Genitalia affected.
o Stellate lesion (lesions away from the
main lesion).
o Obese patient, Diabetic, Extreme age.
o Other endocrine diseases.
Tinea cruris:
o Dry.
o Red brown.
o Upper inner thigh.
o Active border.
o Genitalia free.
11
Erythrasma:
o It is bacterial infection.
o Brown color.
o Pink color under wood light.
DDx of lesion in thigh:
o Psoriasis.
o Eczema.
o Candidiasis.
o Erythrasma.
o Tenia cruris.
Chicken pox:
o Multiple and discrete.
o Pleomorphic (papule, vesicles, crust)
different stages at same time.
o Vesicles erythematous ground.
Herpes simplex:
o Multiple grouped vesicles.
o Erythematous base.
o At angle of mouth.
o History: only few days.
o Associated with tingling sensation.
Varicella zoster:
o One dermatome.
o Middle age or elderly.
o Pain could be post herpetic
neuralgia.
12
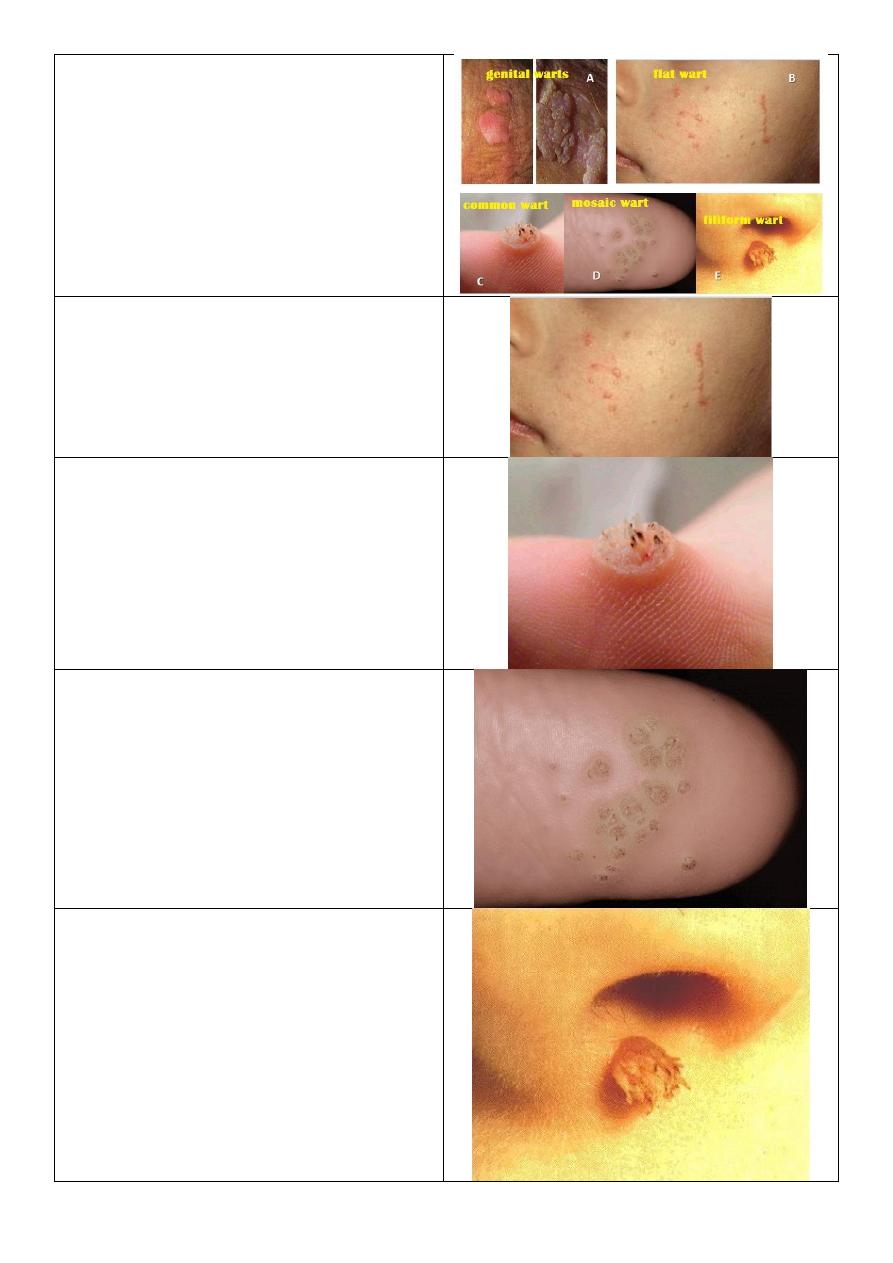
Warts
Plane warts:
o Strict to the surface.
Verruca vulgaris:
o Type of warts.
o Pale or skin color.
o Single papule.
o Well defined.
o Elevated.
o Rough surface.
Warts
Filiform wart:
o Finger like, filiform.
o Condylomata lata
affect genitalia
.
13
Wart:
o Painful in lateral site.
o Rough surface.
o With black dots.
o Interruption of skin marks.
o Multiple.
o Scratching
lead to bleeding.
o Affect sole of foot.
Corn:
o Painful in center.
o Apex in center.
o Smooth surface.
o Continuation of skin marks.
o Scratching lead to arrangement.
o Few.
o Over bone prominence.
o Affect sole of foot.
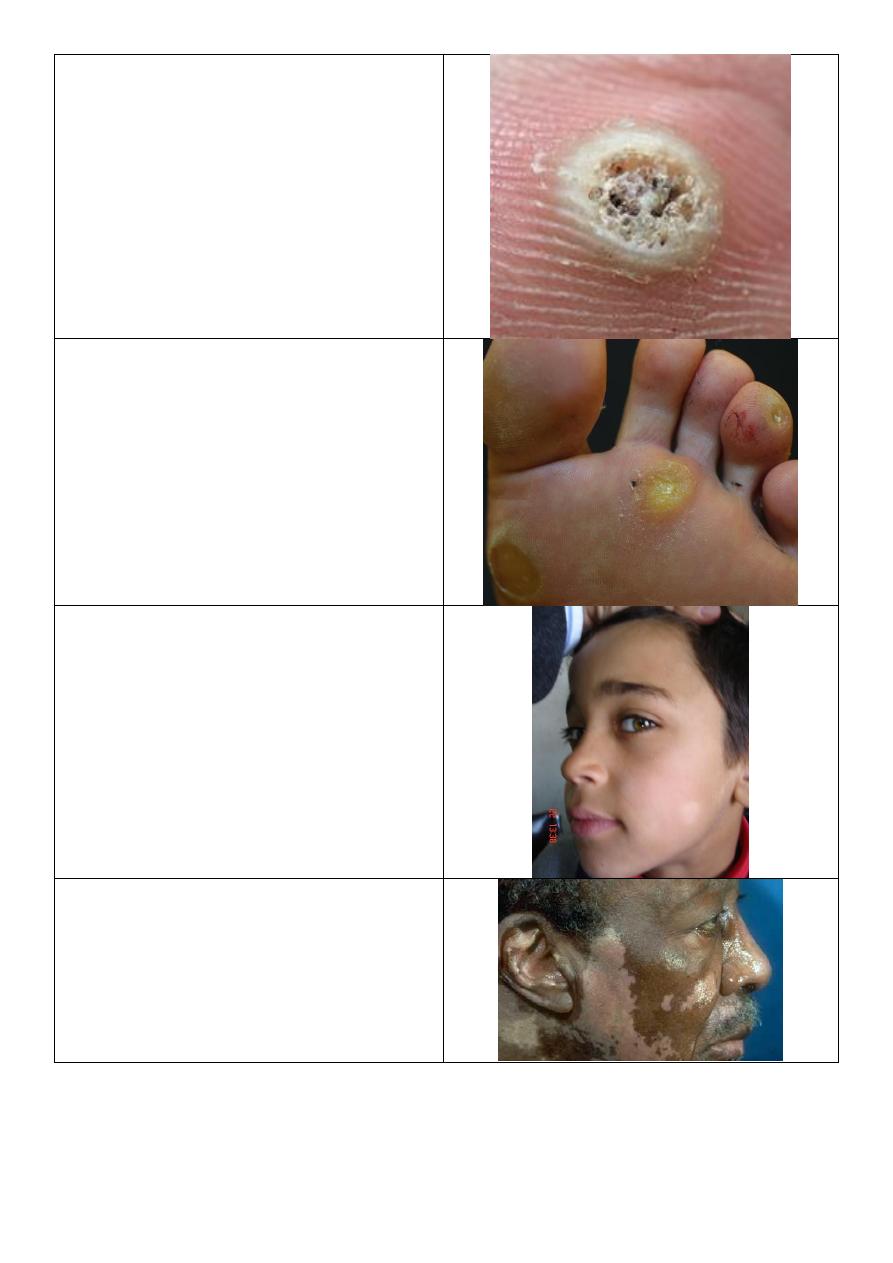
Pityriasis alba:
o Ill defined.
o Hypo pigmented.
o Scaly.
o Mainly in face then extremities.
Vitiligo:
o Well defined.
o Hypo pigmented.
o Not scaly.
o Everywhere.
14
Tenia versicolor:
o Well defined.
o Hypo pigmented.
o Scaly.
o Mainly in the trunk and neck.
o Wood light and KOH exam.
Generalized hair loss:
Hair:
o Anagene (active growing) black pulp.
o Telogene (resting stage) white pulp
of hair.
Telogene effluvium: ---------------------->
o Surgery derived infection.
o Chronic problem.
Anagene effluvium: -------------------------->
o Cytotoxic drug.
o Transient problem.
Scalp hair:
o 3 years anagene.
o 3 weeks transient.
o 3 months telogene.
Localized hair loss:
Both:
o Alopecia areata.
o Round, complete hair lose.
o Normal scalp.
Upper:
o Bad prognosis because affect hair lines
and lead to generalized alopecia.
Lower:
o Better prognosis.
o Self-limited.
15
Cicatrical hair loss:
o Ill-defined bizarre shape of hair loss.
o Scalp: erythematous, crust, scar
formation.
Alopecia areata:
o Multiple.
o May lead to genralized alopecia
o Bad prognostic sign include:
1.more than half of scalp affected
2.patient present from childhood
3.associatd with +family hx
4.associated with other autoimmune
disease or down syndrome
5.if patient present with hair loss
around scalp margin.
Splinter hemorrhage:
o Bacterial endocarditis.
Pterygium of nail:
o Splitting of nail.
o Growth of proximal nail fold.
o It is lichen planus.
Koilonychia:
o Increased concavity.
o Occur due to IDA.
16
Clubbing of nail
o Lovibond angle.
o Causes of clubbing:
Pulmonary diseases: lung cancer,
cystic fibrosis.
Cardiac: cyanotic CHD.
GIT: inflammatory bowel disease,
liver cirrhosis.
Skin condition – malignancy –
acromegaly – thyroid acropachy –
pregnancy.
Nail matrix (form doctor) nail lunula
(from internet)
o Make the nail grow forward not
upward.
o It disappear in 4
th
and 5
th
nail in most
people.
Beau's line of nail:
o Groove of nails in same area.
o Nail growth arrest due to systemic
insult.
o Benefit: calculate the time of onset of
the disease.
Infection of nail and nail fold:
o A: candidiasis: for months or years.
o B: fungal (onychomosis): distal part of
the nail, nail separate from nail bed,
destruction, lower infection of nail.
o C: bacterial: severe pain, red, hot.
Melanonychia
o It is longitudinal Melanonychia.
o We should exclude malignant
melanoma.
17
Lichen planus:
o Multiple, purple, plateform, pruritus,
papule.
o Shiny color, fine scales.
Pityriasis rosea:
o Eruption.
o Affect trunk and upper thigh and upper
arm.
o Oval shape.
o DDx: psoriasis.
Cutaneous leishmaniasis:
o Painless.
o Chronic.
o Large nodule.
Impetigo:
o Erythema.
o Golden yellow crust.
o Young age.
o Staphylococcus.
Folliculitis:
o Painful lesion.
o Affect hair follicles.
o Most common cause is staph. Aureus.
18
Cystic acne:
o Complications: Psychological and social
morbidity, permanent scarring, post
inflammatory hyperpigmentation, gram
negative folliculitis.
Urticaria
Seborrheic dermatitis:
o Area of predilection (center of body)
ear, glabella, napkin area, eye brows.
Napkin dermatitis:
o Use zinc oxide ointment.
o Education of parents.
o Cleaning and changing diaper.
o Keep the area dry.
Contact dermatitis:
o Not touch the cause of rash.
o Wash skin with mild cool water and
soap.
o Use hydrocortisone cream.
Secondary Syphilis:
o Deeply seated vesiculation in palm.
19
Stasis dermatitis:
o Management: use compression stocking
to improve the edema and venous
insufficiency.
Photosensitivity:
o Sunburn.
o Destitution: sun exposed areas.
Juvenile planter dermatitis:
o Eczematous lesion in forefoot of baby.
o Main cause is friction with stocking.
Discoid lesion
Aphthous ulcer
20
Erythema multiform
Dermatitis crculi:
o Patient advised to use lubricant
ointment with corticosteroids.
Pedunculated skin tag:
o Smooth appearance raised from skin
surface on a fleshy stalk.
Molluscum contagiosum:
o Multiple small pearly dome shaped
papules with central umbilication.
Unilateral dermatomal:
o Picture on left unilateral destitution.
o Picture on right dermatomal
distribution.

21
Questions from lectures:
Q: Define psoriasis?
Psoriasis is a genetic, immune-mediated skin and/or joint inflammatory disease in which
intralesional inflammation stimulates basal keratinocytes to hyperproliferate.
Q: Which drugs are contraindicated in psoriasis?
Lithium
Antimalarial agents
Beta blocking agents
Systemic steroids
Interferon
Q: What are the comorbidities associated with psoriasis?
Patients with psoriasis are at a higher risk for the following comorbidities than is the
general population:
1. Crohn’s dis. and UC (3.8 to 7.5 times); families with MS.
2. Cardiovascular disease
3. Metabolic syndrome???
4. Lymphoma (1.5 to 3 fold); non-melanoma skin cancer (250 PUVAs – 14 fold SCC)
5. Depression/suicide
6. Psychological/sexual dysfunction
7. Smoking
8. Alcohol
9. Obesity
10. Quality of life
Q: What are the clinical patterns of psoriasis?
A. Variations in the morphology of psoriasis:
Chronic plaque psoriasis ((commonest type))
Guttate psoriasis

22
Pustular psoriasis
Erythrodermic psoriasis
Light-sensitive psoriasis
HIV-induced psoriasis
Keratoderma blennorrhagicum (Reiter syndrome)
B. Variations in the location of psoriasis:
Scalp psoriasis
Psoriasis of the palms and soles
Pustular psoriasis of the palms and soles
Pustular psoriasis of the digits
Psoriasis inversus
Psoriasis of the penis and Reiter syndrome
Nail psoriasis
Psoriatic arthritis
Q: What is the primary lesion in psoriasis?
Well demarcated, bright red, scaly, plaques.
Q: What are the precipitating factors of Erythrodermic psoriasis?
The administration of systemic corticosteroids.
The excessive use of topical steroids.
Use of tar and anthralin on acutely inflamed plaques.
Abrupt discontinuation of systemic therapy.
Phototherapy complications.
Severe emotional stress.
Infection.
Q: What are the nail changes in psoriasis?
Onycholysis separation of the nail plate from the nail bed.
Subungual hyperkeratosis
Pitting
Oil spot sign
Nail dystrophy

23
Q: Write short notes about treatment of psoriasis:
If the affected body surface area below 20% use topical treatment like topical
steroids, pentocam, topical vitamin D3 analogue (Calcipotriene), Lubricants or lotions.
If the affected body surface area above 20% use systemic treatment like
Methotrexate, Acitretin, Cyclosporine, light therapy (lead to immunosuppression)
PUVA, UVB, UVA1.
You can use biological dugs infliximab, rituximab.
Also you can use immunosuppressive drugs (methotrexate).
Q: What are the drugs used in treatment of psoriatic arthritis?
Non-steroidal anti-inflammatory drugs
Intra-articular steroid injections
Methotrexate
Biologics
Cyclosporine
PUVA
Q: What is the active border of fungal infection?
One very characteristic pattern of inflammation is the active border of infection.
The highest numbers of hyphae are located in the active border, so samples are taken
from here.
Typically the active border is scaly, red, and slightly elevated.
Vesicles appear at the active border when inflammation is intense.
This pattern is present in all locations except the palms and soles.
Q: Enumerate the types of tenia pedis and discus the most common one?
The classic “ringworm” pattern
Interdigital tinea pedis (toe web infection)
Chronic scaly infection of the plantar surface
Acute vesicular tinea pedis
The most common types Interdigital tinea pedis (toe web infection)
The web between the fourth and fifth toes is most commonly involved.
Tight-fitting shoes are a predisposing factor.
The toe web can become dry, scaly, and fissured or white, macerated, and wet.
The bacterial flora is unchanged in the dry scaly pattern.

24
The macerated pattern occurs from an interaction of bacteria and fungus.
Extension out of the web space onto the sole or dorsum of the foot is common.
Q: Write short notes about treatment of tenia pedis?
Terbinafine 1% cream twice daily for 1 week in the interdigital type.
Econazole is excellent in the macerated interdigital TP.
Recurrence is prevented by wearing wider shoes and expanding the web space with a
small strand of lamb’s wool. Powders(not necessarily medicated) absorb moisture.
Oral terbinafine 250 mg daily for 2 weeks in the hyperkeratotic type and other types of
TP.
Acute vesicular tinea pedis responds to wet compresses, oral antifungal and oral
antibiotics.
Id reaction requires wet dressings, group V topical steroids, and occasionally systemic
steroids.
Q: Write about Tinea incognito?
Fungal infections treated with topical steroids often lose some (or sometimes all) of
their characteristics.
Tinea of the hand, body, face and groin are often misdiagnosed as eczema and treated
with topical steroids.
Topical steroids reduce inflammation giving false impression of improvement.
In the mean time, the fungus flourishes. Why?
Treatment is stopped, the rash returns, but by this time it has changed. How?
Intensity of itching is variable.
Hyphae are easily seen with KOH exam. several days after stopping the use of steroids
when scaling reappears.
Q: What are the clinical infection patterns of tenia of the scalp?
Noninflammatory grey patch pattern
Noninflammatory black dot pattern
Inflammatory tinea capitis (kerion)
Seborrheic dermatitis type
Pustular type
Q: Write about Tinea Versicolor?
Lesions begin as multiple small, circular macules of various colors (pink, white, or
brown) that enlarge radially.
25
A spectrum of clinical presentations and colors:
o Red to fawn-colored macules, patches, or follicular papules
o Hypopigmented lesions.
o Tan to dark brown macules and patches.
DDx: Vitiligo, pityriasis alba, seborrheic dermatitis, secondary syphilis, and pityriasis
rosea.
Investigations
o Scraping & KOH.
o Wood’s light examination.
Treatment
o Topical treatment.
o Ketoconazole shampoo.
o Selenium sulfide suspension.
o Terbinafine spray.
o Other topical antifungals.
o Oral itraconazole and fluconazole.
Q: Write about viral warts?
Caused by human papilloma virus
Main types, common, plane and plantar
Very common
Disappear spontaneously eventually
If treatment is needed, options include:
Salicylic acid topically – needs daily treatment and can take months
Cryotherapy
Imiquimod cream
Note description = nodule, well circumscribed, round or oval shape, rough surface, dry,
cracked, black dots (thrombosed vessels).
Q: Write about shingles and post herpetic neuralgia?
Herpes Zoster (Shingles)
Caused by reactivation of the chickenpox virus which has lain dormant in the dorsal
root or cranial nerve ganglia
Rash is preceded by a prodromal phase of up to 5 days of tingling or pain
Then develop painful grouped vesicles/pustules on a red base in a dermatomal
distribution.
Most common in thoracic and trigeminal areas

26
Lesions become purulent, then crusted
Healing takes place in 3-4 weeks
Shingles treatment
Aciclovir 800mg 5 times daily, for 7 days
Rest, analgesia usually gabapentine.
Post-herpetic Neuralgia
Pain lasting longer than 3 months after the rash.
The followings are risk factors for developing post-herpetic neuralgia?
A: Older age
B: More severe pain during the eruption
C: Severely inflamed rash
D: Prodromal pain in dermatome
Q: Write about Herpes Simplex Virus?
A highly contagious infection spread by direct contact
Primary infection is usually asymptomatic.
Recuurent infection presents as acute, painful gingivo-stomatitis with multiple small
intra/perioral ulcers (but any site could be affected).
Associated with fever, malaise and lymphadenopathy.
Clinically: Grouped umbilicated vesicles/pustules on erythematous base.
Treatment: Topical aciclovir 200mg 5 times daily for 5 days
Q: Write about Impetigo?
A highly infectious skin disease, which commonly occurs in children.
The causative organism is usually Staphylococcus Aureus (>90% cases1), but less often
can be strep pyogenes.
Begins as a vesicle, which may enlarge into a bulla.
Weeping, exudative area with characteristic honey coloured or golden, gummy crusts,
which leave denuded red areas when removed.
May present as macules, vesicles, bullae or pustules
Bullae are more prominent in staphylococcal infection and in infants
Impetigo
Treatment:
Mild localised cases - use topical antibiotic Polyfax
Widespread or more severe infections – use systemic antibiotics, such as
flucloxacillin (or erythromycin if penicillin allergic)
27
Q: Write about Folliculitis?
Inflammation of the hair follicle.
Presents as itchy or tender papules and pustules at the follicular openings.
Complications include abscess formation and cavernous sinus thrombosis if upper lip,
nose or eye affected.
Most common cause is Staph Aureus.
Other organisms to consider include:
Gram negative bacteria – usually in patients with acne who are on broad spec
antibiotics
Pseudomonas (“Hot tub folliculitis”)
Yeasts (candida and pityrosporum)
Folliculitis treatment:
Topical antiseptics such as Chlorhexidine
Topical antibiotics, such as Fusidic acid or Mupirocin
More resistant cases may need oral antibioics such as Flucloxacillin
Hot tub folliculitis – ciprofloxacin2
Gram negative – trimethoprim
Q: What are the signs and symptoms of scabies in adults and infants?
In adults:
Rash present for 4 to 8 weeks has suddenly become worse.
Generalized, severe itching
Nocturnal itching
Pinpoint erosions and crusts on the buttocks
Vesicles in the finger webs
Diffuse eruption sparing the face
Nodules on the penis and scrotum
Patient becomes better, then worse, after treatment with topical steroids.
Rash is present in several members of the same family.
In infants:
Widespread involvement usually due to misdiagnosis and Rx.
Sometimes the face and scalp are affected.
Vesicles are common on the palms and soles (characteristic).
Secondary eczematization and impetiginization are common.
Burrows are difficult to find.
Nodules may be seen in the axillae and diaper area.
28
Q: How you treat scabies?
1- Permethrin (cream)
Is the drug of choice for the treatment of scabies in children and adults of all ages
including pregnant and lactating women.
Two applications 1 week apart, apply from head/neck to toe and wash after 8-12 hours
(for permethrin and lindane).
2- Lindane (cream, shampoo, and lotion)
3- BENZYL BENZOATE
4- CROTAMITON
5- SULFUR
The pharmacist mixes 5% to 10% precipitated sulfur in petrolatum.
The compound is applied to the entire body below the neck once each day for 3 days
and the patient is instructed to bathe 24 hours after each application.
These preparations are messy, have an unpleasant odor, stain, and cause dryness.
Sulfur in petrolatum is thought to be safe for infants <2 months old and pregnant and
nursing women.
6- Ivermectin
Q: Write short notes about Nits?
The female lays approximately six eggs, or nits, each day for up to 1 month, and then
dies.
Nits are 0.8 mm long and are firmly cemented to the bases of hair shafts close to the
skin to acquire adequate heat for incubation.
Nits are very difficult to remove from the hair shafts.
Q: How you treat pediculosis?
Permethrin (1% and 5%) is the most effective treatment. It paralyzes the nerves that allow
the lice to breathe.
Remains active for 2 weeks.
Only apply to dry hair.
It is insecticidal and ovicidal.
Two applications (10 min. each) one week apart.
Permethrin has a clinical efficacy of 95%.
Lindane and pyrethrin have cure rates less than 90%.
29
Malathion
Ivermectin
Co-trimoxazole (480mg twice daily for 3 days), and repeated after 1 week.
Shaving the head
Nit removal (Combing)
Fomite control
Eye infestation: Baby shampoo or Vaseline; Ivermectin.
Q: Management of leishmaniasis?
History:
History of travel (or living) to an endemic area in the previous weeks or months.
History of insect (sandfly) bites in the previous weeks or months.
History of high-risk activities such as sleeping outdoors.
Non-healing chronic nodular, violaceous ulcer for 4–6 weeks or longer.
Examination:
Chronic nodules – dusky red in color – ulcerated or crusted – non-healing – on exposed
body parts.
Investigations:
Demonstration of amastigotes in Giemsa-stained smears from infected skin by direct
microscopy.
Demonstration of intracellular amastigotes in the dermis of H & E skin sections.
Growth of promastigotes in Nicolle–Novy–MacNeal (NNN) culture medium from
lesional specimens
Demonstration of leishmanial DNA by PCR.
Treatment:
Try topical treatment methods for simple sores.
Reserve the systemic use of pentavalent antimonials for problematic sores: these
include:
1.Sores where scarring would be disabling or severely disfiguring.
2.Sores that will not heal easily (on shin or over a joint).
3.Sores involving mucosa or cartilage.
Weekly intralesional sodium stibogluconate PLUS daily oral itraconazole 100 mg (or
allopurinol) for 6 to 8 weeks.
IM sodium stibogluconate in a single daily dose of 20 mg/kg for 15–21 days.

30
Severe scarring may require plastic repair.
After healing, patients are normally immune to reinfection with the same species.
Q: Write about pathogenesis of acne?
Increased sebum production (androgens)
Abnormal keratosis (androgens)
bacterial proliferation (Propionibacterium acnes)
inflammation
Q: Enumerate the clinical manifestations of acne?
Closed comedone (whitehead)
Open comedone (blackhead)
Papules
Pustules (pimples)
Cysts and nodules
Q: Write about classification of acne?
Comedonal acne: Only comedons
Mild acne: Less than 20 pustules.
Moderate to severe acne: More than 20 pustules
Q: Write about treatment of acne and side effects?
Antibiotics: Topical (clindamycin and erythromycin) and systemic antibiotics used in
the treatment of acne vulgaris are directed at Propionibacterium acnes.
Minocycline, Doxycycline (50 t0 200 mg / day for 3 months), Tetracycline, Lymecycline
Retinoids: These agents decrease the cohesiveness of abnormal hyperproliferative
keratinocytes.
Isotretinoin (systemic) 0.5 - 1 mg per kg over 4 to 6 months
Tretinoin (topical) cream (0.025%, 0.05%, 0.1%)
Side effects:
Mucocutaneous: dry lips, facial dermatitis, dry nose, dry skin, pruritis, conjunctivitis,
hair loss, impetiginization.
Arthralgia and myalgia and headache.
Depression and mood swing.
Impaired night vision.
