1
Overview of viral infections
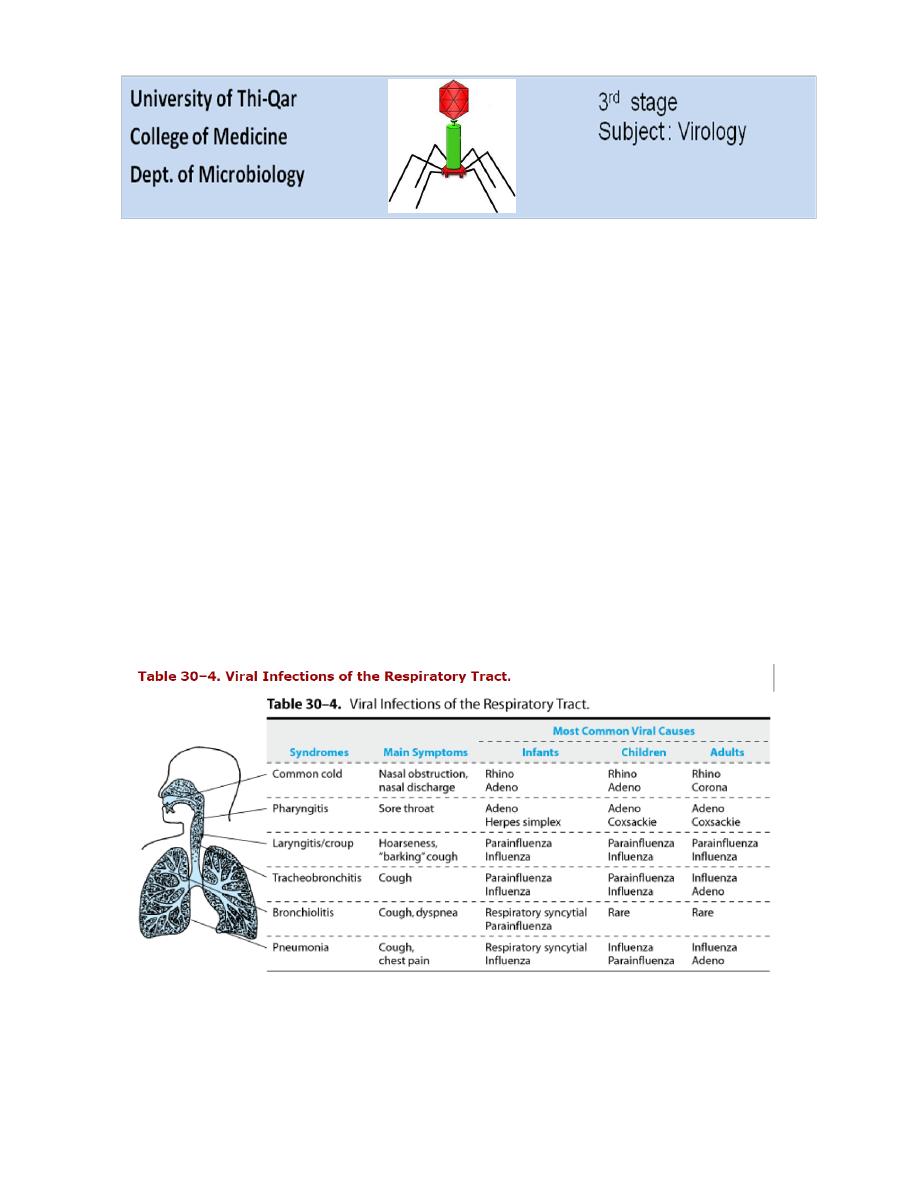
Acute Viral Respiratory Infections
Many types of viruses gain access to the human body via the respiratory tract, primarily
in the form of aerosolized droplets or saliva. This is the most frequent means of viral
entry into the host. Successful infection occurs despite normal host protective
mechanisms, including the mucus covering most surfaces, ciliary action, collections of
lymphoid cells, alveolar macrophages, and secretory IgA. Many infections remain
localized in the respiratory tract, although some viruses produce their characteristic
disease symptoms following systemic spread (eg, chickenpox, measles, rubella).
Disease symptoms exhibited by the host depend on whether the infection is concentrated
in the upper or lower respiratory tract. Although definitive diagnosis requires isolation of
the virus, identification of viral gene sequences, or demonstration of a rise in antibody
titer, the specific viral disease can frequently be deduced by considering the major
symptoms, the patient's age, the time of year, and any pattern of illness in the community.
The most severe illness is usually seen in infants infected with certain paramyxoviruses
and in elderly or chronically ill adults infected with influenza virus.

2
Overview of Viral Infections of the Gastrointestinal Tract (GIT)
Many viruses initiate infection via the alimentary tract. A few agents, such as herpes
simplex virus and Epstein-Barr virus, probably infect cells in the mouth. Viruses are
exposed in the intestinal tract to harsh elements involved in the digestion of food—acid,
bile salts (detergents), and proteolytic enzymes. Consequently, viruses able to initiate
infection by this route are all acid- and bile salts-resistant. There may also be virus-
specific secretory IgA and nonspecific inhibitors of viral replication to overcome.
Acute gastroenteritis is the designation for short-term gastrointestinal disease with
symptoms ranging from mild, watery diarrhea to severe febrile illness characterized by
vomiting, diarrhea, and prostration. Rotaviruses, Norwalk viruses, and caliciviruses are
major causes of gastroenteritis. Infants and children are affected most often.
Some viruses that produce enteric infections utilize host proteases to facilitate infection.
In general, proteolytic digestion alters the viral capsid by partial cleavage of a viral
surface protein that then facilitates a specific event such as virus attachment or membrane
fusion.
Enteroviruses, coronaviruses, and adenoviruses also infect the gastrointestinal tract, but
those infections are often asymptomatic. Some enteroviruses, notably polioviruses, and
hepatitis A virus are important causes of systemic disease but do not produce intestinal
symptoms.
Overview of Viral Skin Infections
The skin is a tough and impermeable barrier to the entry of viruses. However, a few
viruses are able to breach this barrier and initiate infection of the host. Some obtain entry
through small abrasions of the skin (poxviruses, papillomaviruses, herpes simplex
viruses), others are introduced by the bite of arthropod vectors (arboviruses) or infected
vertebrate hosts (rabies virus, herpes B virus), and still others are injected during blood
transfusions or other manipulations involving contaminated needles, such as acupuncture
and tattooing (hepatitis B virus, HIV).
A few agents remain localized and produce lesions at the site of entry (papillomaviruses);
most spread to other sites. The epidermal layer is devoid of blood vessels and nerve
fibers, so viruses that infect epidermal cells tend to stay localized. Viruses that are
introduced deeper into the dermis have access to blood vessels, lymphatics, dendritic
cells, and macrophages and usually spread and cause systemic infections.
Many of the generalized skin rashes associated with viral infections develop because
virus spreads to the skin via the bloodstream following replication at some other site.
Such infections originate by another route (eg, measles virus infections occur via the
respiratory tract), and the skin becomes infected from below.

3
Lesions in skin rashes are designated as macules, papules, vesicles, or pustules. Macules,
which are caused by local dilation of dermal blood vessels, progress to papules if edema
and cellular infiltration are present in the area. Vesicles occur if the epidermis is
involved, and they become pustules if an inflammatory reaction delivers
polymorphonuclear leukocytes to the lesion. Ulceration and scabbing follow.
Hemorrhagic and petechial rashes occur when there is more severe involvement of the
dermal vessels.
Skin lesions frequently play no role in viral transmission. Infectious virus is not shed
from the maculopapular rash of measles or from rashes associated with arbovirus
infections. In contrast, skin lesions are important in the spread of poxviruses and herpes
simplex viruses. Infectious virus particles are present in high titers in the fluid of these
vesiculopustular rashes, and they are able to initiate infection by direct contact with other
hosts. However, even in these instances, it is believed that virions in oropharyngeal
secretions may be more important to disease transmission than the skin lesions.
Overview of Viral Infections of the Central Nervous System
Invasion of the central nervous system by viruses is always a serious matter. Viruses can
gain access to the brain by two routes: by the bloodstream (hematogenous spread) and by
peripheral nerve fibers (neuronal spread). Access from the blood may occur by growth
through the endothelium of small cerebral vessels, by passive transport across the
vascular endothelium, by passage through the choroid plexus to the cerebrospinal fluid,
or by transport within infected monocytes, leukocytes, or lymphocytes. Once the blood-
brain barrier is breached, more extensive spread throughout the brain and spinal cord is
possible. There tends to be a correlation between the level of viremia achieved by a
blood-borne neurotropic virus and its neuroinvasiveness.
The other pathway to the central nervous system is via peripheral nerves. Virions can be
taken up at sensory nerve or motor endings and be moved within axons, through
endoneural spaces, or by Schwann cell infections. Herpesviruses travel in axons to be
delivered to dorsal root ganglia neurons.
The routes of spread are not mutually exclusive, and a virus may utilize more than one
method. Many viruses, including herpes-, toga-, flavi-, entero-, rhabdo-, paramyxo-, and
bunyaviruses, can infect the central nervous system and cause meningitis, encephalitis, or
both. Encephalitis caused by herpes simplex virus is the most common cause of sporadic
encephalitis in humans.
Pathologic reactions to cytocidal viral infections of the central nervous system include
necrosis, inflammation, and phagocytosis by glial cells. The cause of symptoms in some
other central nervous system infections, such as rabies, is unclear. The postinfectious
encephalitis that occurs after measles infections (about one per 1000 cases) and more
rarely after rubella infections is characterized by demyelination without neuronal
degeneration and is probably an autoimmune disease.
4
There are several rare neurodegenerative disorders, called slow virus infections that are
uniformly fatal. Features of these infections include a long incubation period (months to
years) followed by the onset of clinical illness and progressive deterioration, resulting in
death in weeks to months; usually only the central nervous system is involved. Some
slow virus infections, such as progressive multifocal leukoencephalopathy (JC
polyomavirus) and subacute sclerosing panencephalitis (measles virus), are caused by
typical viruses. In contrast, the subacute spongiform encephalopathies, typified by
scrapie, are caused by unconventional agents called prions. In those infections,
characteristic neuropathologic changes occur, but no inflammatory or immune response
is elicited.
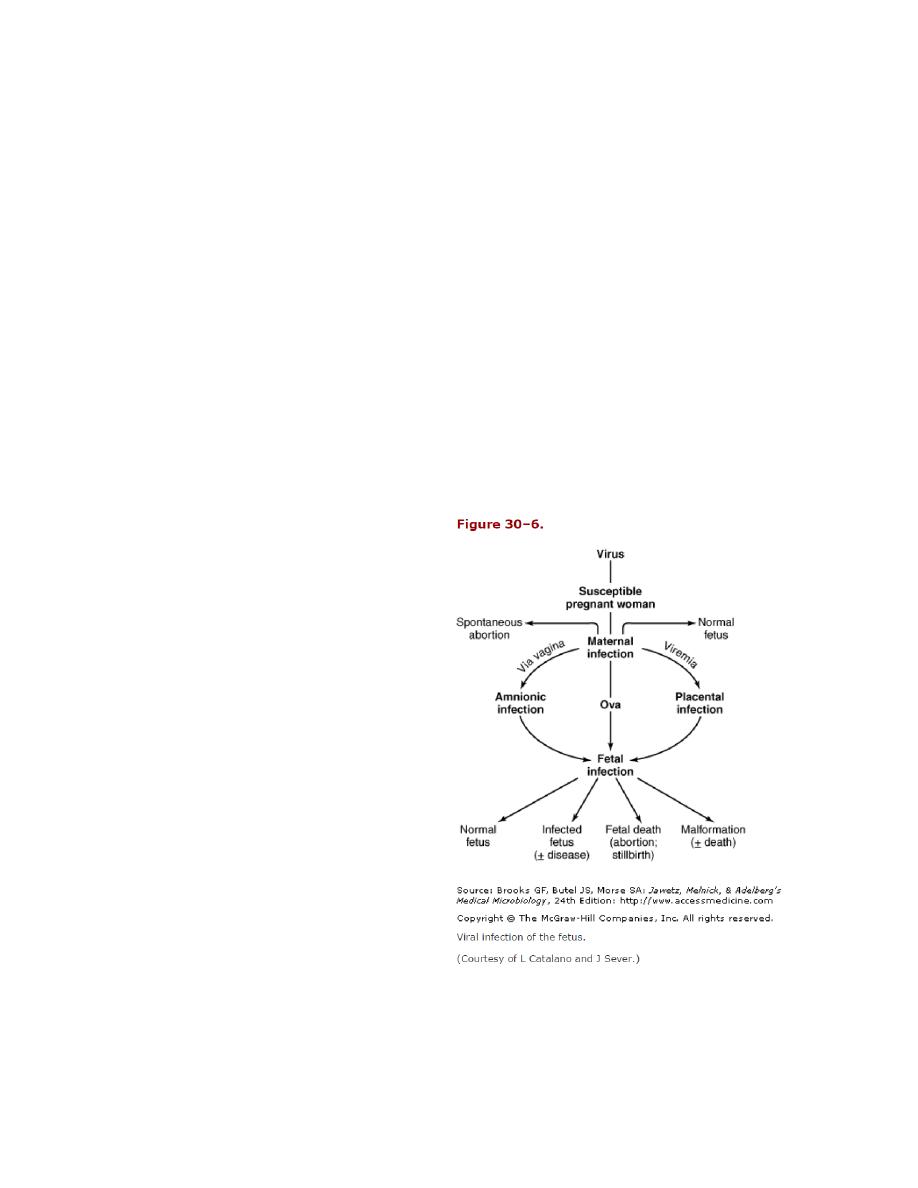
Overview of Congenital Viral Infections
Few viruses produce disease in the human fetus. Most maternal viral infections do not
result in viremia and fetal involvement. However, if the virus crosses the placenta and
infection occurs in utero, serious damage may be done to the fetus.
Three principals involved in the production of congenital defects are:
(1) The ability of the virus to infect the
pregnant woman and be transmitted to
the fetus;
(2) The stage of gestation at which
infection occurs;
(3) The ability of the virus to cause
damage to the fetus directly, by infection
of the fetus, or indirectly, by infection of
the mother resulting in an altered fetal
environment (eg, fever). The sequence of
events that may occur prior to and
following viral invasion of the fetus is
shown in Figure 30–6.
Rubella virus and cytomegalovirus are
presently the primary agents responsible
for congenital defects in humans.
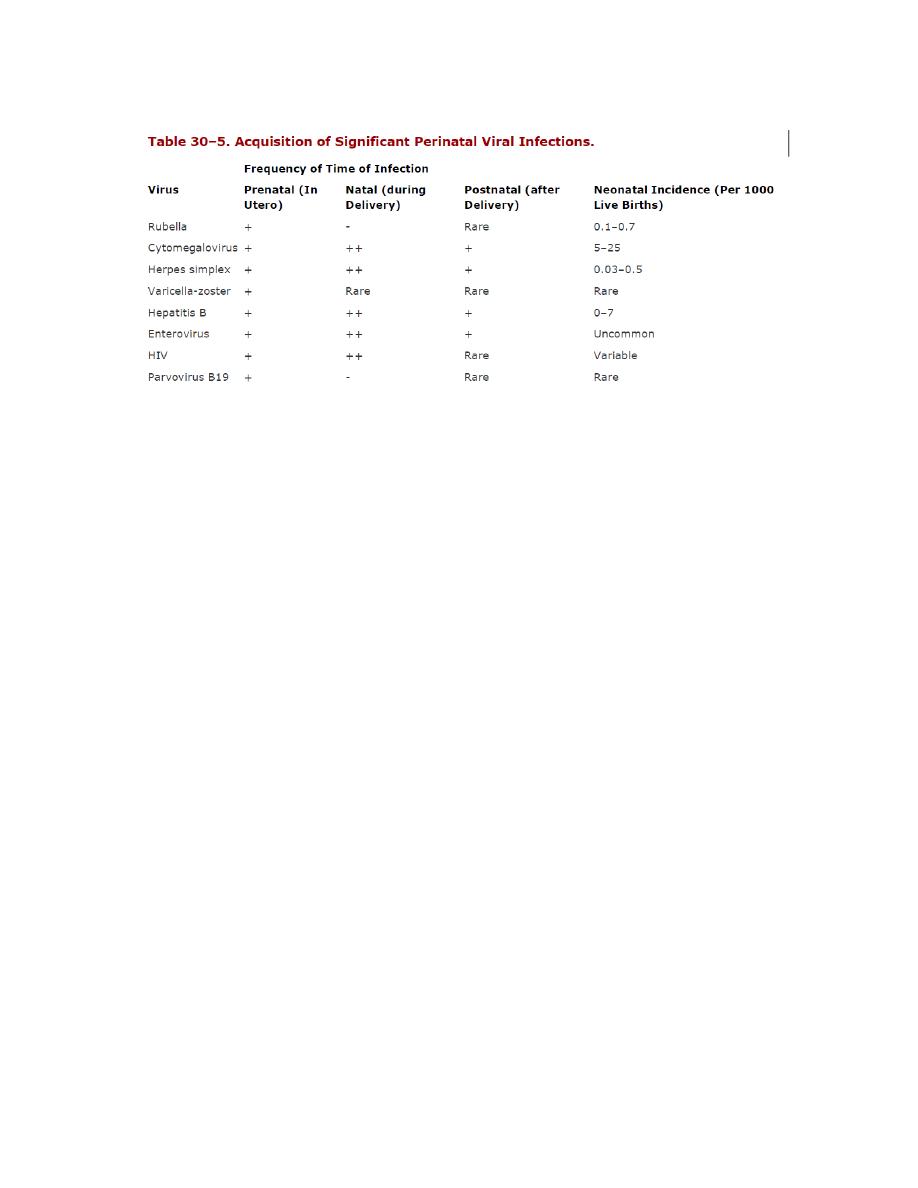
Congenital infections can also occur with
herpes simplex, varicella-zoster, hepatitis
B, measles, and mumps virus and with
HIV, parvovirus, and some enteroviruses (Table 30–5).
5
In utero infections may result in fetal death, premature birth, intrauterine growth
retardation, or persistent postnatal infection. Developmental malformations, including
congenital heart defects, cataracts, deafness, microcephaly, and limb hypoplasia, may
result. Fetal tissue is rapidly proliferating. Viral infection and multiplication may destroy
cells or alter cell function. Lytic viruses, such as herpes simplex, may result in fetal
death. Less cytolytic viruses, such as rubella, may slow the rate of cell division. If this
occurs during a critical phase in organ development, structural defects and congenital
anomalies may result.
Many of the same viruses can produce serious disease in newborns (Table 30–5). Such
infections may be contracted from the mother during delivery (natal) from contaminated
genital secretions, stool, or blood. Less commonly, infections may be acquired during the
first few weeks after birth (postnatal) from maternal sources, family members, hospital
personnel, or blood transfusions.
Effect of Host Age
Host age is an important factor in viral pathogenicity. More severe disease is often
produced in newborns. In addition to maturation of the immune response with age, there
seem to be age-related changes in the susceptibility of certain cell types to viral infection.
Viral infections usually can occur in all age groups but may have their major impact at
different times of life. Examples include rubella, which is highly serious during gestation;
while rotavirus is mostly serious for infants; and St. Louis encephalitis is more serious in
the elderly people.
