NEONATAL JAUNDICE
Hyperbilirubinemia is common, affects 60% of term babies and 80% of preterm babies and, in most cases it is benign problem in neonates.It is either:
-Indirect (unconjugated) which is the most common and it is either.physiologic (benign non pathologic).
.Hemolytic (pathologic), it carry a risk of CNS damage known as
kernicterus when bilirubin exceed certain limit.
.Breast Milk jaundice (benign).
-Direct hyperbilirubinemia: this is when the direct bilirubin is more
than 2mg/dl, no risk of kernicterus, caused by:Common causes:-
- biliary atresia.- idiopathic neonatal hepatitis.
Less common causes as:-
cystic fibrosis, galactosemia, Wilson disease, tyrosinemia,
fructosemia, alpha 1 antitrypsin deficiency, TORCH infection,
choledochal cyst, total parenteral nutrition.
Physiologic Jaundice:
To say it is physiologic jaundice, the following criteria must be found:- It starts during the 2nd or the 3rd day of life.
- The peak of jaundice in full term baby is at the 2nd to 4th day
of life, while in preterm baby it peaks at 5th to 7th day of life.
- Decline to below 2mg/dl by the 7th day of life in term & by
the 10th day in preterm baby.
- Jaundice disappear completely within 2 weeks of life.
- The raise in the bilirubin is less than 5 mg/dl/24 hours.
- The peak level of bilirubin is less than 12mg/dl, although
10% of these babies having higher bilirubin level as in babies
of diabetic mothers, prematurity, polycythemia, vit k
administration, male sex, Down syndrome, cephalhematoma,
cutaneous bruising, oxytocin during labor, dehydration and
calory deprivation, delay bowel motion.
Why physiologic jaundice occur:
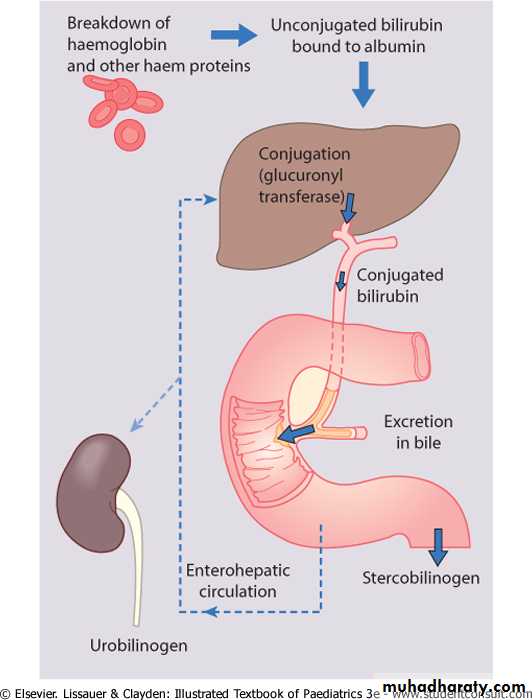
-There is marked physiological release of haemoglobin
from the breakdown of red cells because of the high Hbconcentration at birth.
-The red cell life span of newborn infants (70-90 days) is
markedly shorter than that of adults (120 days).
-Hepatic bilirubin metabolism is slow during the first few days of life.
Pathologic Jaundice (hemolytic):
The criteria of this jaundice are:- It starts during the 1st 24 hr of life.
- The rise in serum bilirubin is more than 5mg/dl/24 hr.- The serum bilirubin is higher than 12mg/dl.
- Jaundice persist for more than 2 weeks.
- May be positive family history of hemolytic disease, pallor,
hepatosplenomegaly, signs of kernecterus.
- Lab. findings may show evidence of Rh or ABO incompatability
low hemoglobin, reticulocytosis, and may be a positive
Coombs test.
Breast Milk Jaundice:
An estimated of 2% of breast fed term infants develops an
elevated level of uncongugated bilirubin after the7th day of lifereaching maximal concentrations as high as 10-30mg per dl during
the 2nd & 3rd week.If breast feeding continued the
hyperbilirubinemia gradually decreases & then may persist for
3-10 weeks at lower levels. These infants show no signs of illness
and kernicterus is very rarely reported.
Kernicterus:
Is a neurologic syndrome results from a deposition ofunconjugated bilirubin in the brain cells particularly in the basal
ganglia, hippocumpus,and cerebellum. Lipid soluble indirect
bilirubin may cross the blood brain barrier and enter the brain
by diffusion.
Clinical Features:
signs & symptoms of kernicterus usually appear in the 1st week of life although kernicterus can occur at any time during the neonatal period.The early signs may be subtle & indistinguishable from sepsis,
asphyxia, hypoglycemia or intracranial hemorrhage which are:-Lethargy, poor feeding & absence Moro reflex are common initial
signs.
In advanced cases there is irritability, increased muscle tone causing
the baby to lie with an arched back (opisthotonos),twitching, seizures,high pitched cry, bulging fontanel, coma with the infant stiffly
extended his arms with inward rotation.
Many infants who progress to these severe neurologic signs die, the
survivors are usually seriously damaged and may appear to recover &after 2-3 months they show few abnormalities.
Later in the 1st year of life opisthotonos, muscular rigidity,
irregular movements, and convulsions tends to recur.In the 2nd year opisthotonos & convulsions abate,but irregular
involuntary movements, muscular rigidity or in some infantshypotonia increase gradually.
By 3 years of age the syndrome is completely developed
consisting of bilateral chorioathetosis with involuntary muscle spasm,seizures, mental deficiency, dysarthric speech, high frequency hearing loss,squints, and defective upward movement of the eyes.
In mildly affected infants, the syndrome may be characterized only by mild to moderate neuromuscular incoordination, partial deafness, or minimal brain dysfunction.
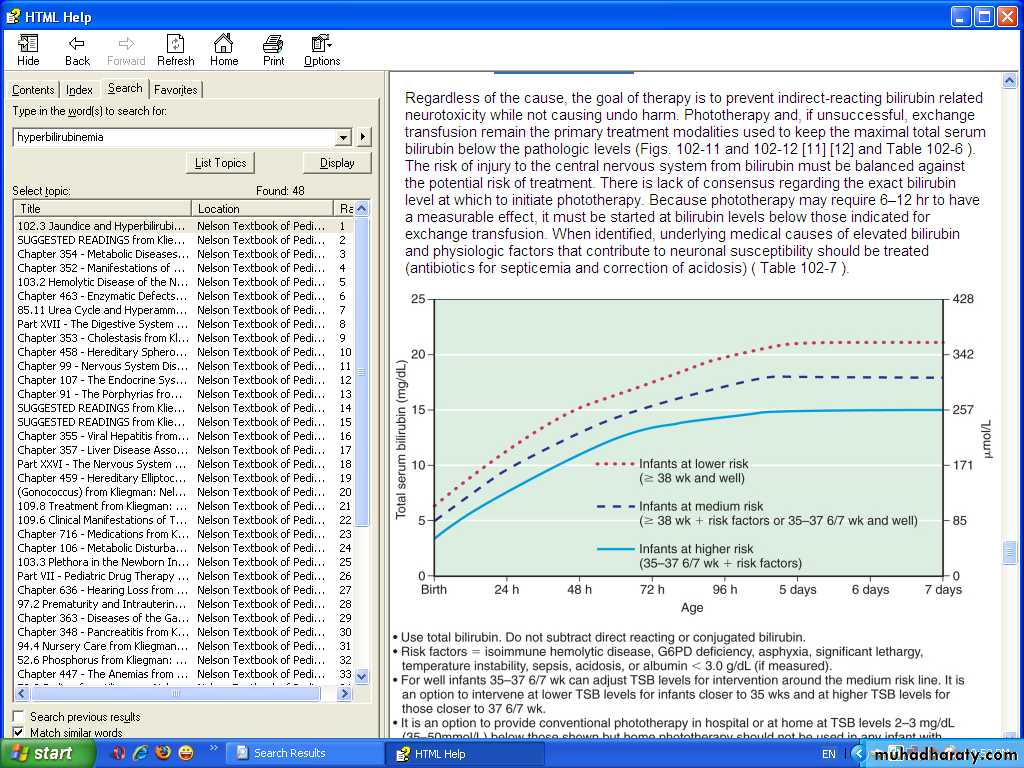
Treatment of hyperbilirubinemia:
Either there is no need for treatment especially if there is nohemolysis, full term baby, healthy active & the jaundice is not
deep with criteria of physiologic jaundice.
2. Phototherapy
3. Exchange transfusion.
4. Intravenous immunoglobulin: for ABO and Rh incompatability
in a dose of 0.5-1 grams/kg/dose repeated every 12 hours.Phototherapy:-
Clinical jaundice & indirect hyperbilirubinemia reduced onexposure to a high intensity of light in a wave length of
420-470nm. Bilirubin in the skin absorbs light energy which by
photoisomerization converts the toxic unconjugated bilirubin to
a product which can be excreted in bile without the need for
conjugation, also phototherapy converts uncojugated bilirubin to
lumirubin which excreted in urine by the kidney.
Prophylactic phototherapy in VLBW infants may prevents
hyperbilirubinemia & may reduce the need for exchange
transfusion.
Monitoring should continue for at least 24 hrs after cessation of
phototherapy in infants with hemolytic disease that unexpectedrise of bilirubin sometimes occur & require further treatment.
Skin color can not be relied on for evaluation of the effectiveness of
phototherapy that the skin of babies exposed to light may appear
without jaundice in the presence of marked hyperbilirubinemia.
The infants eyes should be closed & adequately covered to prevent
exposure to light. Body temp also should be monitored.Complications of phototherapy:
1. loose stool.
2. Erythematous macular rashes.
3. Overheating.
4. Dehydration.
5. Bronze baby syndrome when there is direct
hyperbilirubinemia.
6. Eye injury and nasal obstruction.
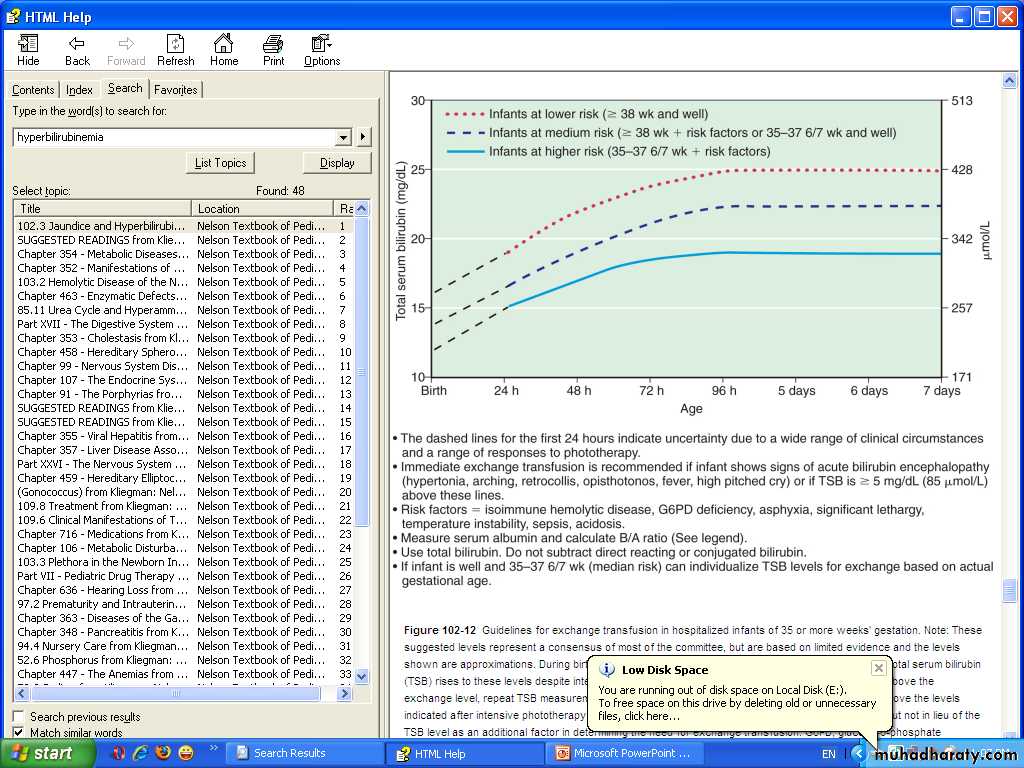
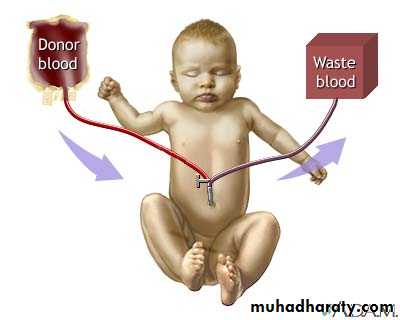
Exchange transfusion:-
It is used to remove bilirubin from the circulation when phototherapyfails, is especially used for infants with increased in bilirubin production
from immune mediated hemolysis because the circulating antibodies
and the sensitized RBCs are also removed.
Functions of exchange transfusion:-
- Clear excess bilirubin.- Correct the anemia without causing circulatory overload.
- Removes maternal antibodies.
- Removes sensitized RBCs.
Procedure of Exchange Transfusion:
Volume of blood needed is double the blood volume of the baby, so itwill be the boy weight multiplied by 170ml (as the blood volume of the newborn is 85ml/Kg body weight.
The procedure involves placement of a central catheter into the umbilical vein, then alternatively remove then give 15-20ml of blood in
a repeated way until completing the required amount of blood.
After the procedure serum bilirubin falls to approximately 1/2 of the pre exchange value, then increase to approximately 2/3 of that level as the extravascular & vascular bilirubin reequilibirate.
Complications of Exchange Transfusion:-
- blood born infection.thrombocytopenia.
-metabolic acidosis.
-volume overload.
- coagulopathy.
- graft versus host disease.
- necrotizing enterocolitis.
- portal vein thrombosis and portal hypertension years later.
- electrolytes disturbance.
- hypoglycemia, hypocalcemia.
- cardiac arrhythmias.
- sudden death.