2nd part
Adaptive or acquired immunityDone by Dr. Zubaida Najat
The immune system andthe oral cavity
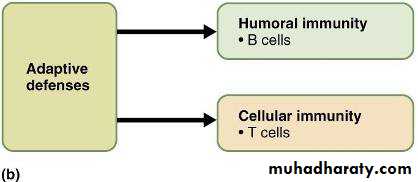
Adaptive Immune System –IntroductionAdaptive: responds to specific foreign substances
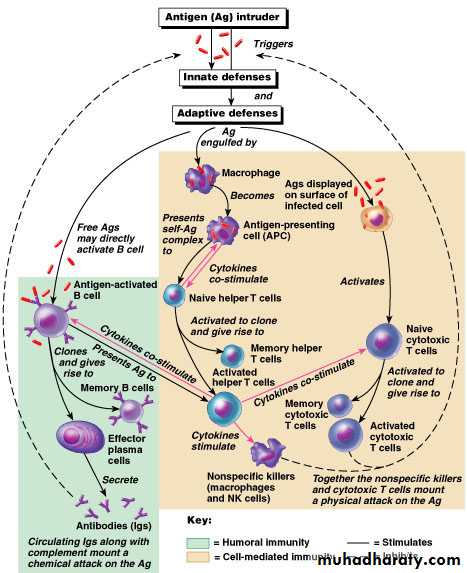
Innate & adaptive mechanisms work together
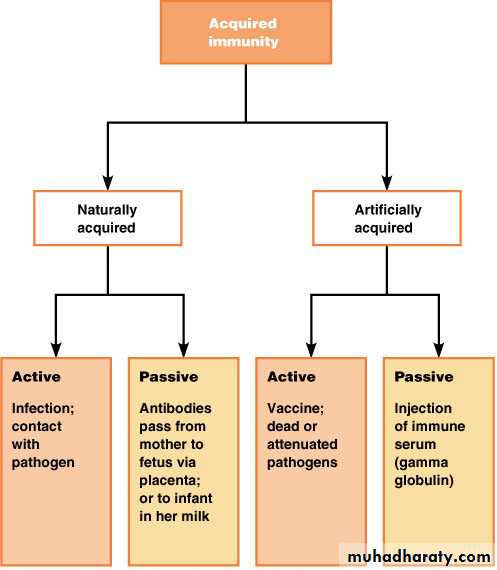
Types of Acquired Immunity
Figure 21.11Types of Acquired Immunity
1- Passive acquired immunity includes
a- Naturally passive acquired immunity
antibodies are pass through placenta of fetusb- Artificially passive acquired immunity:The injection of alredy prepared antibodies such as gamma globulin
2- Active immunity
a- Natural active acquired immunityFollowing clinical or subclinical infections
b-Artificial active acquired immunity:-[[[[[Following vaccination with live or killed infectious agents or their products
Adaptive Immune System: Cells
LymphocytesT-cells
B-cells
Antigen Presenting Cells (APCs)
Acquired immunity is triggered in vertebrates when a pathogen evades the innate immune system and
(1) generates a threshold level of antigen and
(2) generates "stranger" or "danger" signals activating dendritic cells
The major functions of the acquired immune system include:
Recognition of specific "non-self" antigens in the presence of "self", during the process of antigen presentation.
Generation of responses that are tailored to maximally eliminate specific pathogens or pathogen-infected cells systemic action .
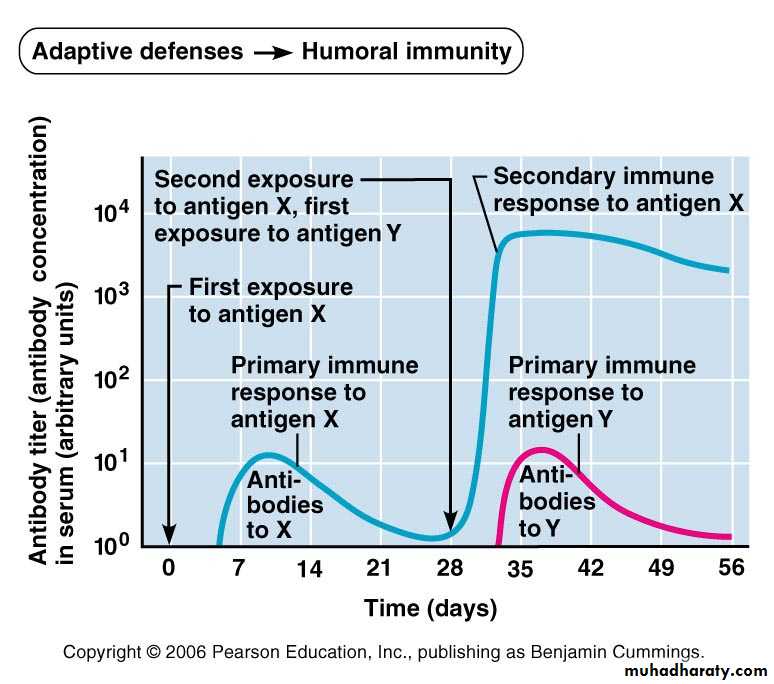
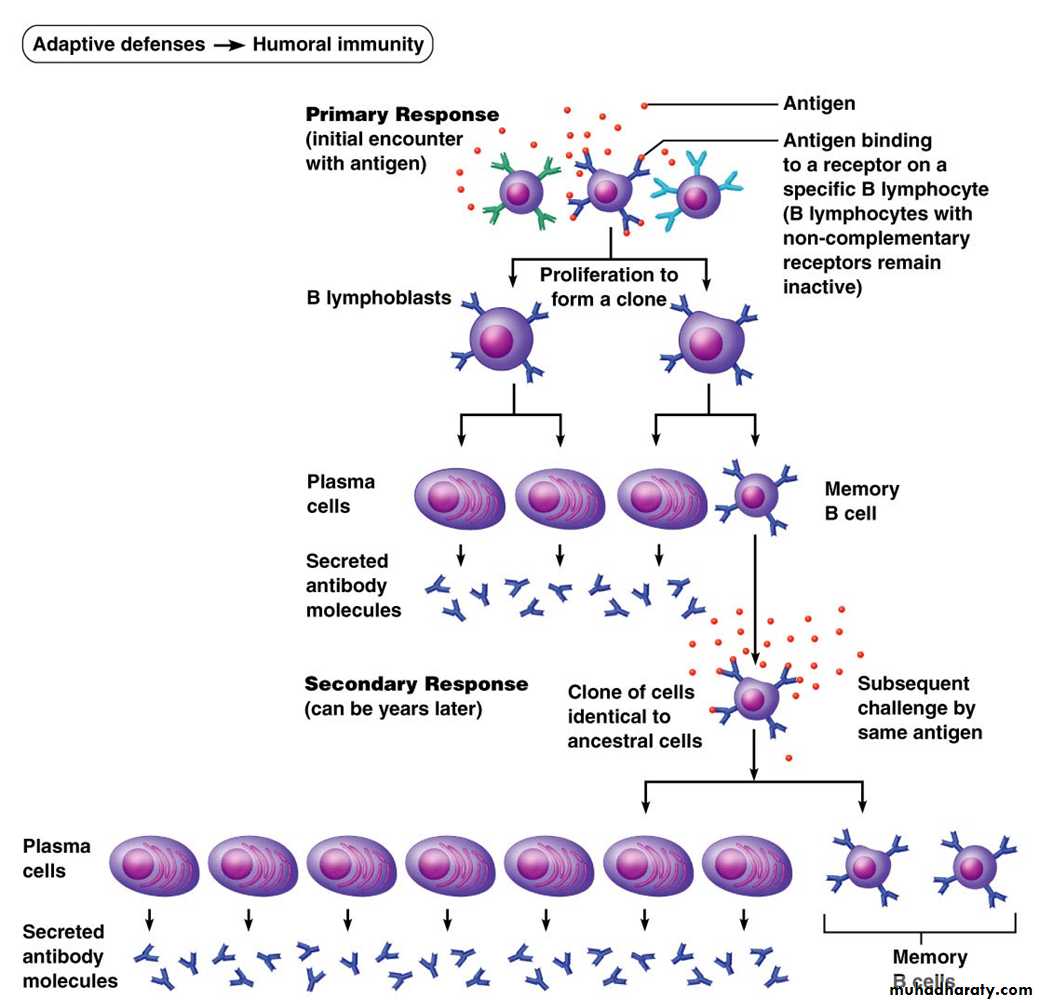
Development of immunological memory, in which pathogens are "remembered" through memory B cells and memory T cells.
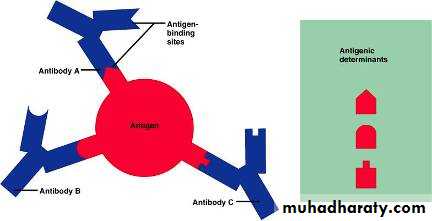
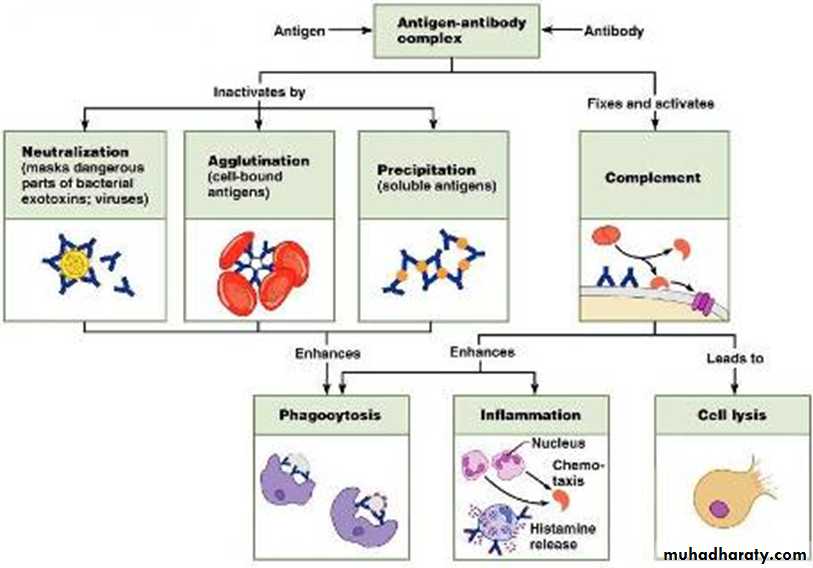
Antibody Targets & Functions
Immune complex formation = antigen-antibody binding.All the following events are initiated by antigen-antibody binding.
Complement fixation:Neutralization:
Agglutination:
Precipitation:
Inflammation & phagocytosis prompted by debris
Adaptive, Humoral Immunity
Antigen – “any substance when introduced into the body stimulates the production of an antibody”Bacteria, fungus, parasite
Viral particles
Other foreign material
Pathogen – an Antigen which causes disease
Adaptive, Humoral Immunity
Complete antigens (proteins, nucleic acids, lipids, polysaccharides):
Immunogenicity: the ability to stimulate specific lymphocytes & specific antibodies
Reactivity: the ability to react with activated lymphocytes & antibodies
Hapten (an incomplete antigen): a smaller molecule that is not immunogenic until attached to proteins
Adaptive, Humoral Immunity
Antigenic determinants: sites on an antigenic molecule that are immunogenicEpitope
Major Histocompatibility Complex (MHC): cell surface glycoproteins associated with self recognition
Humoral Immunity
Active humoral immunity:B-cells encounter & respond to antigen to produce an antibody
Passive humoral immunity:
Introduced “non-native” antibodyAntibodies
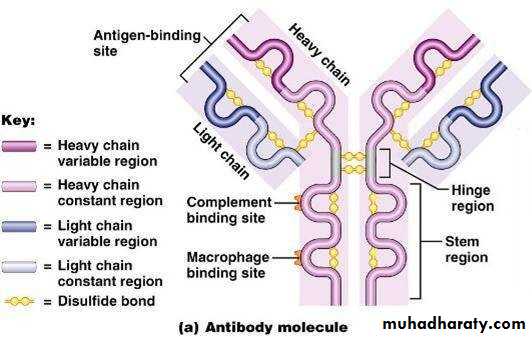
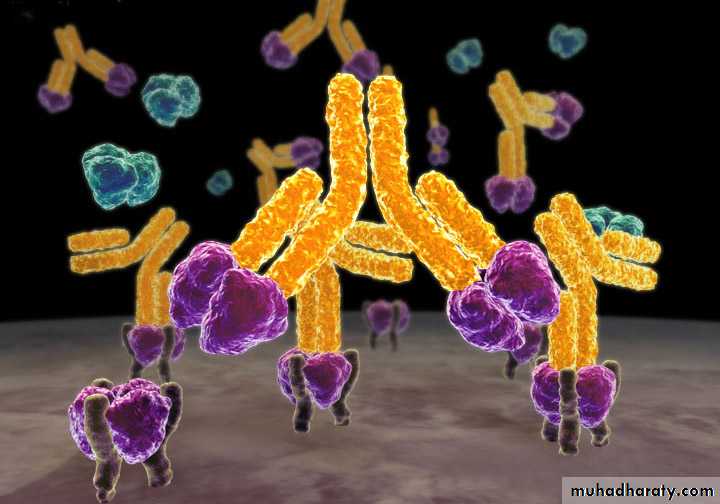
Antibody – “a Y-shaped protein, found on the surface of B-Cells or free in the blood, that neutralize antigen by binding specifically to it”
Also known as an Immunoglobulin
Constant (C) region defines antibody class
determines chemical & cellular interactionsdetermines how class functions to eliminate antigens
Humoral Mediated Immunity
B-CellT-Cell
CytokinesPlasma Cell
AntibodiesImmunoglobulins & gamma globulins
Structure
variable
hypervariable
constant
Figure 21.13a
Antibody Classes
Antibody Classes: IgM, IgG, IgA, IgD, IgE (Ig = immunoglobulin)Antibody Classes
IgM: occurs as a monomer & a pentamerOccurs on the B-cell surface (Monomer).
The Ig of early primary plasma cell response, circulating antibody; a potent agglutinator. Complement binding (Pentamer).Antibody Classes
IgE: the Ig associated with allergies.Stem binds to mast cells & basophils.
Receptor binding results in histamine release & inflammation.
Found mostly in mucosa of respiratory & GI tract (Monomer).
Antibody Classes
IgG: the most abundant circulating Ig. The dominant circulating Ig of the primary & the secondary response. Crosses the placenta. Complement binding (Monomer).IgA: the Ig of secretions. Helps prevent antigen penetration of membranes (Dimer).
IgD: the Ig of B-cell activation. Found on B-cell surface (Monomer).
Adaptive Immune System: Cells
Immunocompetence: as T- or B-cells mature they become immunocompetent, they display receptors on their cell membrane for a specific antigen.All of the receptors on one cell are identical; immunity depends upon genetic coding for appropriate receptors.
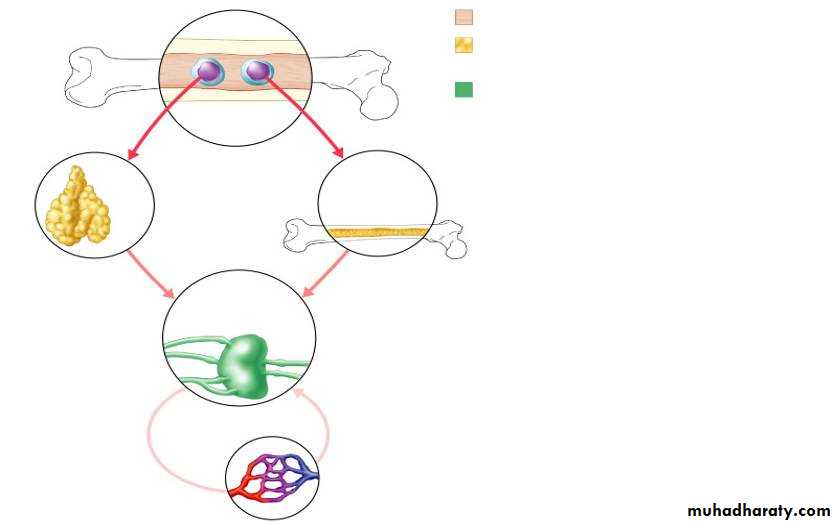
Red bone marrow
12
3
Immunocompetent, but still naive, lymphocyte migrates via blood
Mature (antigen-activated) immunocompetent lymphocytes circulate continuously in the bloodstream & lymph & throughout the lymphoid organs of the body.
Key:
= Site of lymphocyte origin• = Site of development of immunocompetence as B or T cells; primary lymphoid organs
• = Site of antigen challenge & final differentiation to activated B & T cells
Immature lymphocytes
Circulation in blood
1
1
Lymphocytes destined to become T cells migrate to the thymus & develop immunocompetence there. B cells develop immunocompetence in red bone marrow.
Thymus
Bonemarrow
Lymph nodes, spleen, & other lymphoid tissues
2
2
After leaving the thymus or bone marrow as naive immunocompetent cells, lymphocytes “seed” the lymph nodes, spleen, & other lymphoid tissues where the antigen challenge occurs.
3
3
Activated immunocompetent B & T cells recirculate in blood & lymph
Immunocompetent B or T cells
Figure 21.8
Adaptive Immune System: Cells
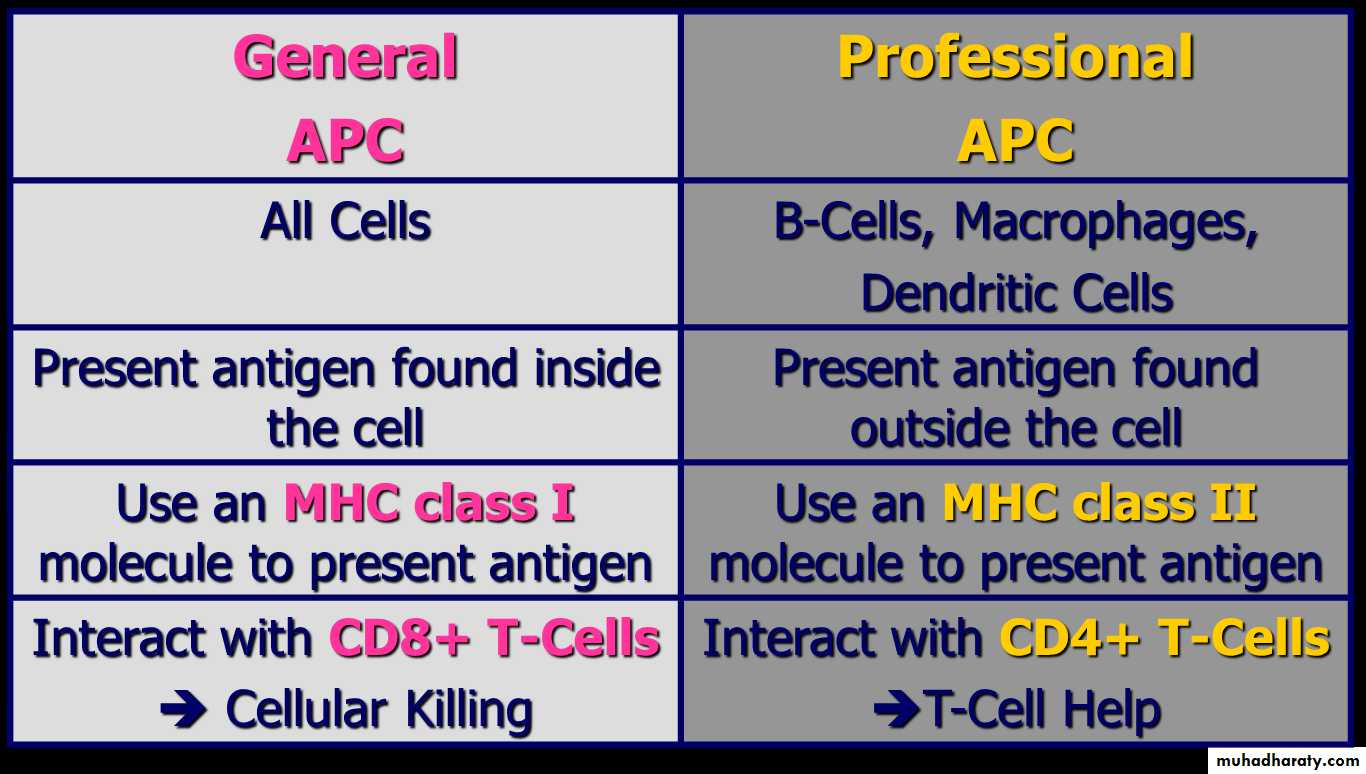
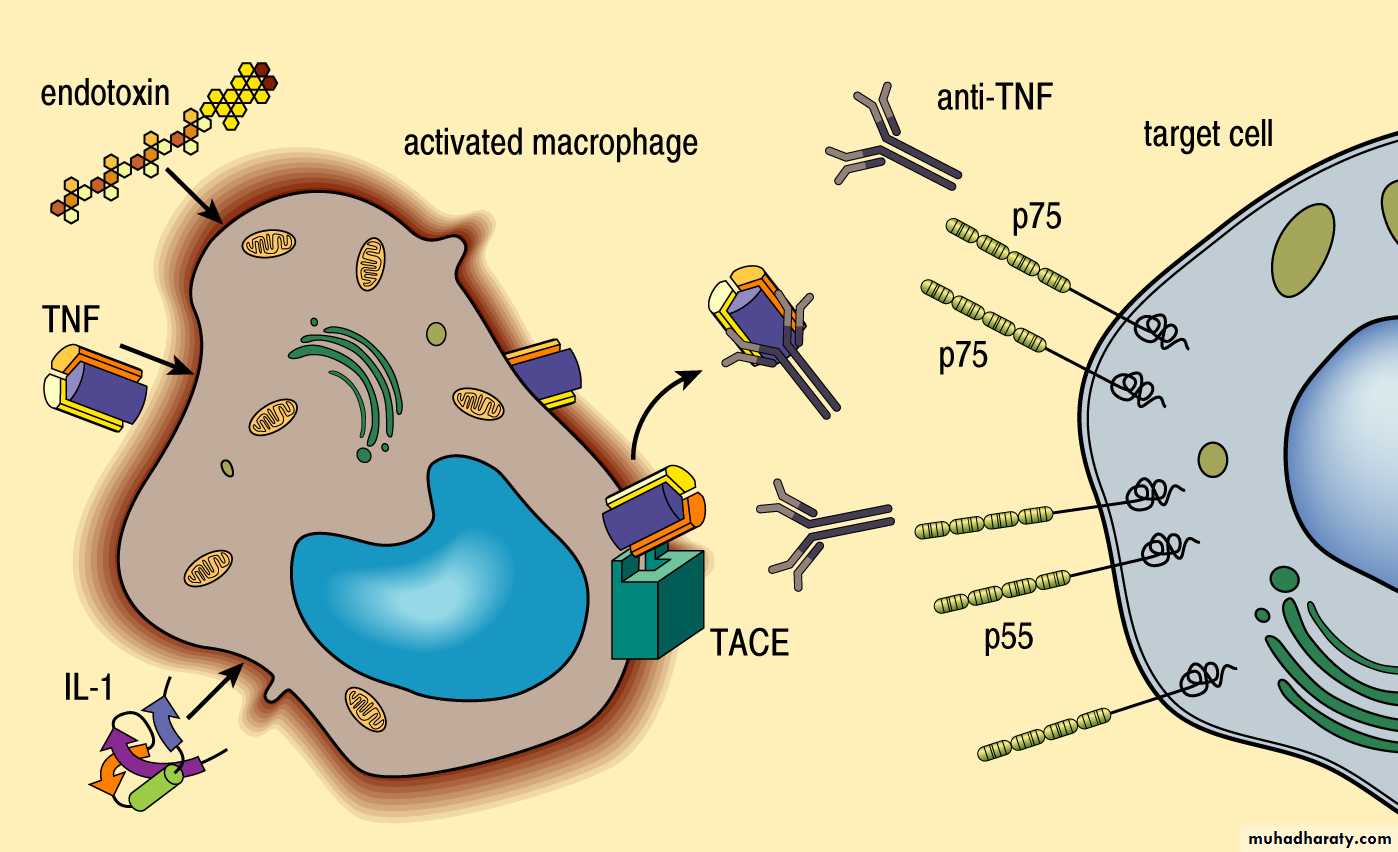
Antigen Presenting Cells (APCs)
APCs ingest foreign material, then present antigenic fragments on their cell surface where they are recognized by T-cells
APCs: Macrophages & B lymphocytes
Interactions between APCs & lymphocytes & lymphocyte-lymphocyte interactions are critical to immune response
Adaptive, Humoral response
Humoral response (clonal selection)Figure 21.14
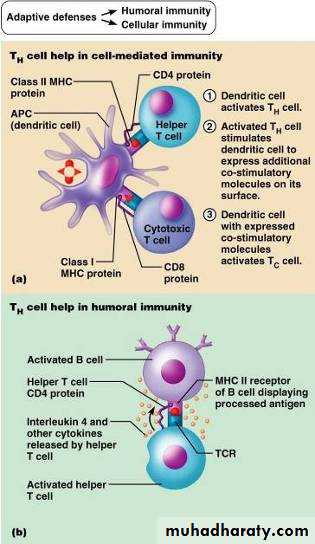
Cellular Immunity
TcellCD4& CD8
Adaptive Immune System: Cells
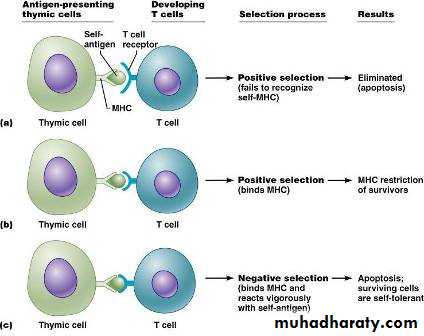
Lymphocytes: initially uncommittedT-cells: are sorted in the Thymus
Positive selection: recognize MHC survive
Negative selection: react against to self-antigens on MHC killed
2% of initial T-cell precursors
T-cells manage the immune response
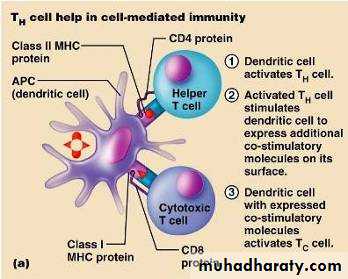
Cell Mediated Immune Response
T-cell activation: involves recognition of PM surface antigens onlyAntigen is combined with MHC & displayed on PM
T-cell receptors: bind to the MHC & are stimulated by the associated antigen
The addition of a co-stimulator (cytokines, interleukins, etc) prompts the T-cell to form a clone
Helper T Cells (TH)
Figure 21.17aProfessional APCsCD4+ Th1-Cells
MacrophageProtein
CD4+ Th1-Cell
IFN-gamma
TNF-alpha
IL-2
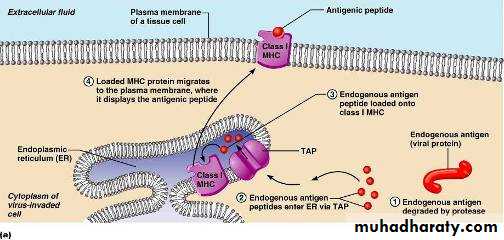
Cell Mediated: MHC
MHC occurs as two classesMHC I on virtually all tissue cells
MHC II only on PM some immune system cells
Cell Mediated: MHC display properties
MHC I on virtually all tissue cellsDisplay only proteins produced inside the cell
Endogenous antigens = foreign proteins produced by the cell (viral / cancer)
Stimulate the CD8* cell population
form cytotoxic T-cells (Killer T, TC)
*formerly T8 cells
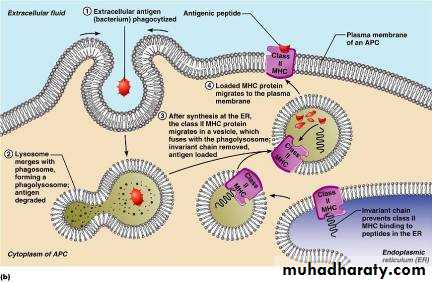
Cell Mediated: MHC display properties
MHC II found only on PM of B-cells, some T-cells & APCsDisplay proteins derived from a phagocytized target
Exogenous antigen: foreign protein from outside the cell – presented to PM surface
Stimulates the CD4* cell population
form Helper T-cells (TH)
Figure 21.16b
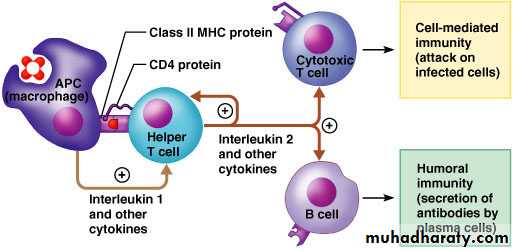
Cell Mediated: T-cell rolesHelper T-cells (TH) stimulate B-cells & other T-cells to proliferate
Figure 21.18
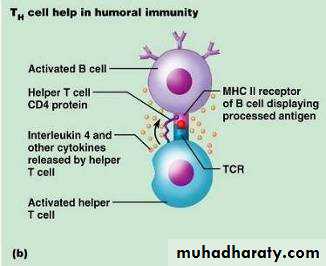
Cell Mediated: T-cell rolesActivated TH cells interact with B-cells displaying antigen & produce cytokines that prompt the B-cell to mature & form antibody
Cell Mediated: T-cell roles
TH cells also produce cytokines that promote TC cellsTH cells recruit other WBCs & amplify innate defenses (inflammatory)
Subpopulations of TH cells specialize in specific sets of activationsCell Mediated: T-cell roles
Cytotoxic T-cells (TC, Killer T): directly attack & kill cells with specific antigenActivated TC cells are co-stimulated by TH cells
Cell Mediated: T-cell roles
TC mechanism (Cytotoxic T-cells, Killer T)TC binds to cell & releases perforin & granzymes
In the presence of Ca2+ perforin forms pores in target cell PM
Granzymes enter through pores & degrade cellular contents
TC then detaches & moves on
Macrophages clean up
Cell Mediated: T-cell roles
Other T-cells*Regulatory T-cells (TReg): release inhibitory cytokines that suppress B-cell & T-cell activity
Help to prevent autoimmune events
*formerly Suppressor T (TS)
Gamma Delta T-cells (Tgd): live in the intestine. Function in surveillance & are triggered much like NK cells