
Genital infections in gynaecology
Dr.Alyaa A.
Al-Mallah
2016/2017
1
The vaginal epithelium is lined by stratified squamous epithelium
during the reproductive age group under the influence of oestrogen. The
pH is usually between 3.5 and 4.5 and lactobacilli are the most common
organisms present in the vagina.
Following the menopause, the influence of oestrogen is diminished
making the vaginal epithelium atrophic with a more alkaline pH of 7.0,
the lactobacillus population declines and the vagina is colonized by skin
flora.
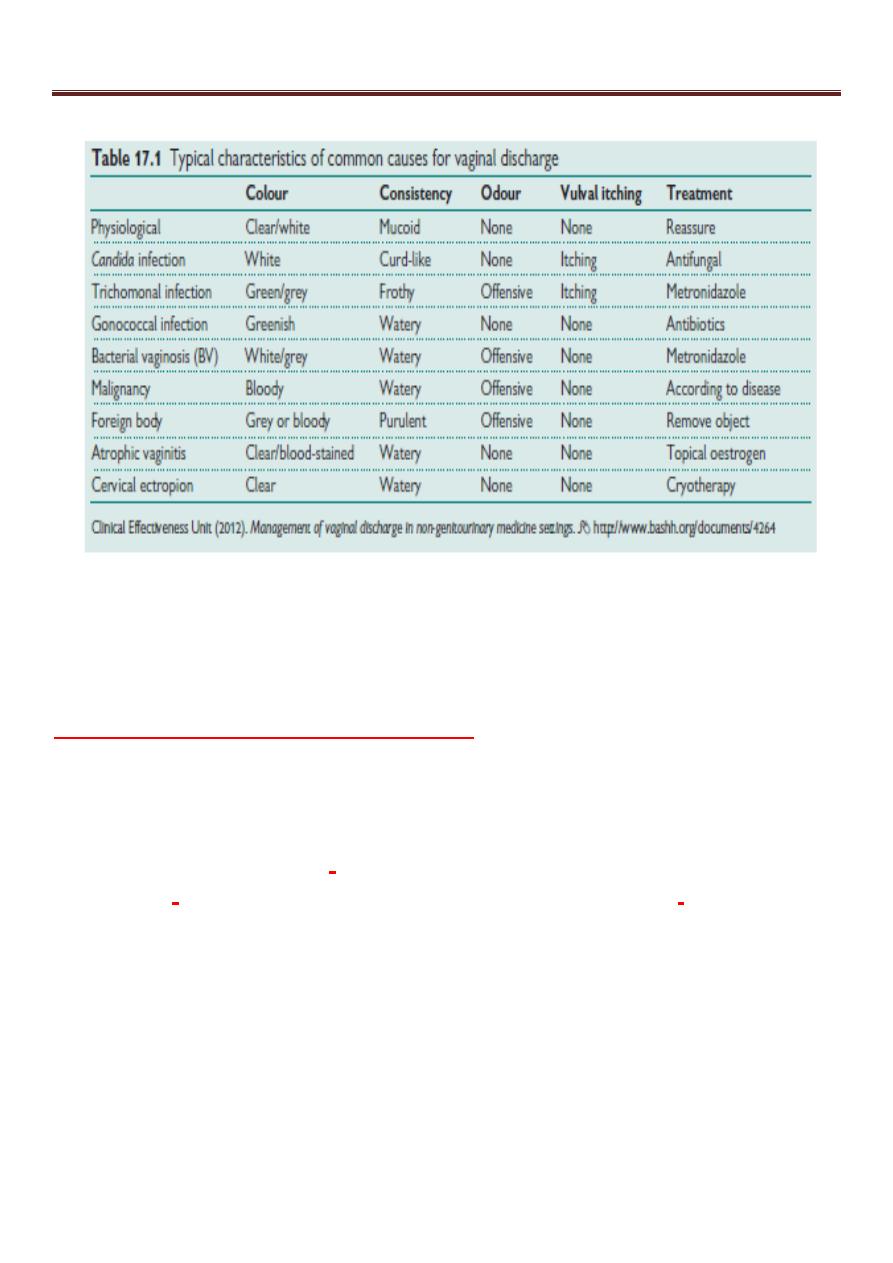
Vaginal discharge
Normal (physiological) discharge occurs in women of reproductive age
and varies with the menstrual cycle and hormonal changes.
Causes of increased vaginal discharge
Physiological
• Oestrogen related—puberty, pregnancy, COCP.
• Cycle related—maximal mid-cycle and premenstrual.
Pathological
Infection
• Non-sexually transmitted (BV, candida).
• Sexually transmitted (TV, chlamydia, gonorrhoea).
Non-infective
• Foreign body (retained tampon, condom, or post-partum swab).
• Malignancy (any part of the genital tract).
• Atrophic vaginitis (often blood-stained).
• Cervical ectropion or endocervical polyp.
• Fistulae (urinary or faecal).
Genital infections in gynaecology
2
Physiological discharge:
• Normal vaginal discharge is white, becoming yellowish on contact
with air.
• It consists of desquamated epithelial cells from the vagina and cervix,
mucus originating mainly from the cervical glands. bacteria and fluid,
which is formed as a transuedate from the vaginal wall. More than 95
per cent of the bacteria present are lactobacilli.
• The acidic pH is maintained by the lactobacilli and through the
production of lactic acid.
• It increases due to increased mucus production from the cervix in mid-
cycle, pregnancy and sometimes when women begin using a combined
oral contraceptive pill.
Lower genital tract infections:
Vulvovaginal Candidiasis ( thrush ):
Epidemiology
• It is a mycotic disease, caused by the dimorphic Yeast-like fungus
(90%Candida albicans, remainder other species,e.g. C.glabrata ).
• About 75% of women will experience at least one episode, and
10–20% are asymptomatic chronic carriers (increasing to 40% during
pregnancy).
• It is not sexually transmitted
Predisposing factors are those that alter the vaginal micro-flora and
include:
• immunosuppression
• antibiotics
• pregnancy
• diabetes mellitus
• HIV.
• Steroids.
• Vaginal douching, tight clothing.
• Combined oral contraceptive pill.

Genital infections in gynaecology
3
Diagnosis
Symptoms:
May be asymptomatic, but usually presents with:
• Vulval itching and soreness.
• Thick, curd-like, white vaginal discharge.
• Dysuria.
• Superficial dyspareunia.
Signs:
• Characteristic appearance of:
• vulval and vaginal erythema
• vulval fissuring, oedema, excoriation
• typical white plaques adherent to the vaginal wall.
•
Normal vaginal pH.
Investigations:
• Culture from HVS or LVS.
• Microscopic detection of spores and pseudohyphae on wet slides.
Complications
Unlikely to cause any significant complications unless the woman is
severely immunocompromised.
Treatment
Uncomplicated infection
• As so many women are chronic carriers, candidiasis should only be
treated if it is symptomatic.
• Azoles/imidazoles are the mainstay of the treatment. They can either
be used either as a local topical application (pessaries/creams) or oral
preparations.
•The common imidazoles are clotrimazole, econazole and miconazole.
Other antifungals, such as nystatin cream or pessary, can also be used.
•The commonly prescribed medication is clotrimazole, which can be
taken as single 500 mg pessary or a course of a 100 mg pessary over 6
days.
• Oral imidazoles, such as fluconazole, are given as a single dose at 150
mg or itraconazole 200 mg twice a day for 1 day. However, these are
contraindicated in pregnancy.
Genital infections in gynaecology
4
•There is no evidence to treat the asymptomatic male partner.
Other simple measures may help to decrease recurrent attacks, e.g.:
• Wearing cotton underwear.
• Avoiding chemical irritants, e.g. soap and bath salts.
Complicated infection
Commonly seen in acute severe infection in pregnancy, women with
diabetes mellitus or with immunosuppression conditions or therapy.
Women with complicated infection may benefit from an additional 150-
mg dose of fluconazole given 72 hours after the first dose. The
topical treatment in such cases can be extended to up to 2 weeks.
Recurrent infection
• Recurrent infection is defined as at least four episodes of infection per
year and/or a positive microscopy of moderate to heavy growth of C.
albicans.
• The principle of treatment would be an induction regimen to treat the
acute episode followed by a maintenance regimen to treat further
recurrences.
• Commonly fluconazole 150 mg is given in three doses orally every 72
hours followed by a maintenance dose of 150 mg weekly for six
months.
• Oral imidazoles cannot be used in pregnancy but a topical imidazole
can be used for 2 weeks for induction followed by a weekly dose of
Clotrimazole pessary 500 mg for possibly 6–8 weeks.
Implications in pregnancy
• It is very common in pregnancy with no apparent adverse effects.
• Topical imidazoles are not systemically absorbed and are therefore
safe at all gestations.
Trichomonas vaginalis
Epidemiology
• Trichomonas vaginalis —flagellated protozoan can cause
severe vulvovaginitis and UTI .
• Found in vaginal, urethral, and para-urethral glands.
Genital infections in gynaecology
5
• It is usually sexually transmitted and commonly recurrences occur if
the male partner is not simultaneously treated.
Signs & Symptoms
Asymptomatic in 10–50%, but may present with:
• Frothy,yellowish green, offensive smelling vaginal discharge.
• Vulval itching and soreness.
• Dysuria.
• Cervix may have a ‘strawberry’ appearance from punctate
haemorrhages (2%).
Signs and symptoms
Diagnosis
• Direct observation of the organism by a wet smear (normal saline).
(sensitivity 40–70% cases).
• Culture media are available and will diagnose up to 80% cases.
• NAATs have been developed and sensitivities and specificities
approaching 100% have been reported.
Complications
There is some evidence that trichomonal infection may enhance HIV
transmission.
Management
• Both partners should be treated and both should be screened for other
sexually transmitted infections.
• Metronidazole 2g orally in a single dose.
• Metronidazole 400mg bd for 5–7 days.
• Tinidazole in a single oral dose of 2 g is equally effective, but can cost
more
Implications in pregnancy
• Trichomonas is associated with:
• preterm delivery
• low birth weight.
• Trichomonas may be acquired perinatally, occurring in 5% of babies
born to infected mothers.

Genital infections in gynaecology
6
Bacterial vaginosis
Epidemiology
• BV is a common condition caused by an overgrowth of mixed
anaerobes, including Gardnerella vaginalis, Mycoplasma hominis,
Bacteroides spp. and Mobilincus spp., which replace the usually
dominant vaginal lactobacilli causing an increase in the vaginal pH
making it more alkaline.
• Not sexually transmitted.
• About 12% of women will experience BV at some point in their lives,
but what triggers it remains unclear.
Signs and Symptoms
• May be asymptomatic, but usually presents with a profuse, whitish
grey, offensive smelling vaginal discharge. The characteristic ‘fishy’
smell is due to the presence of amines released by bacterial proteolysis
and is often distressing to the woman.
•
More prominent during and following menstruation
Diagnosis
(Amsel criteria—3 out of 4 required for diagnosis.)
• Homogenous grey-white discharge.
• Increased vaginal pH >4.5.
• Characteristic fishy smell.
• ‘ Clue cells’ present on microscopy (squamous epithelial cells with
bacteria adherent on their walls).
Complications
Increased risk of pelvic infection after gynaecological surgery.
Treatment
May resolve spontaneously and if successfully treated has a high
recurrence rate. However, most women prefer it to be treated.
• Metronidazole 400mg orally bd for 5 days; or
• Metronidazole 2g (single dose).
• Alternatively, it can be used as a local intravaginal gel (0.75 per cent)
usually applied at night for between 5 and 7 days.

Genital infections in gynaecology
7
• Clindamycin 2% cream vaginally at night for 7 days.
Lifestyle factors—avoidance of vaginal douching/overwashing which
can destroy natural vaginal flora.
Implications in pregnancy
Associated with an increased risk of:
• Mid-trimester miscarriage.
• Preterm rupture of membranes.
• Preterm delivery.
Women with a previous history of second trimester loss or preterm
delivery should have a vaginal swab performed in early pregnancy and
if bacterial vaginosis is detected, it should be actively treated in the
early second trimester of pregnancy. Metronidazole is safe to use in
pregnancy, however, large or prolonged doses should be avoided.
Gonorrhoea
Epidemiology
• Neisseria gonorrhoeae: intracellular Gram –ve diplococcus.
• It is a STD.
• It has affinity to infect the mucous membranes of the genital tract
infecting cuboidal and columnar epithelium seen in the endocervical
and urethral mucosa. It can also infect the rectal and oropharyngeal
mucous membrane
• > 35% of strains are resistant to ciprofloxacin, 70% to tetracyclines.
• Sexually transmitted coinfection with Chlamydia and Trichomonas are
common
Signs & Symptoms
• Asymptomatic
• Increased vaginal discharge with lower abdominal/pelvic pain
• Dysuria with urethral discharge
• Proctitis with rectal bleeding, discharge and pain
• Endocervical mucopurulent discharge and contact
bleeding
• Mucopurulent urethral discharge
• Pelvic tenderness with cervical excitation.

Genital infections in gynaecology
8
Diagnosis:
• Gram staining: visualization of Gram-negative intracellular diplococci
• Culture medium using an agar medium containing antimicrobials to
reduce growth of other organisms
• Nucleic acid amplification tests (NAATs)
• Nucleic acid hybridization tests
Endocervical swabs should be taken and if symptomatic, swabs from
the rectum and pharynx should also be included.
Complications of gonococcus infection
• PID (~10% of infections result in PID).
• Bartholin’s or Skene’s abscess.
• Disseminated gonorrhoea may cause:
- fever
- pustular rash
- migratory polyarthralgia
- septic arthritis.
• Tubal infertility.
• Risk of ectopic pregnancy.
Treatment
Cephalosporins are the mainstay of treatment.
• Contact tracing and treatment of partners.
• Single oral dose of cefixime 400 mg
• Single intramuscular dose of ceftriaxone 250 mg
• Single intramuscular dose of spectinomycin 2 g
• Single oral dose of ciprofloxacin 500 mg or ofloxacin 400 mg
• Azithromycin 1 g as single dose
• Ampicillin 2 g or amoxycillin 1 g with probenecid 2 gm as a single
oral dose.
In pregnancy, it is safe to use the penicillins and cephalosporins, but
tetracycline and ciprofloxacin/ ofloxacin should be avoided.
Implications in pregnancy
• Gonorrhoea associated with:
- preterm rupture of membranes and premature delivery

Genital infections in gynaecology
9
- chorioamnionitis.
• The risks to the baby are of ophthalmia neonatarum (40–50%).
Genitourinary Chlamydia
Epidemiology
• Chlamydia trachomatis: obligate intracellular bacterium
affecting the columnar epithelium of the genital tract.
• Is the commonest bacterial sexually transmitted infection which is
commonly a symptomatic.
• Serovars D-K cause genital infections
• An important cause of tubal infertility.
SIGNS & Symptoms
Dysuria with urethral discharge, vaginal discharge and lower abdominal
pain, Mucopurulent cervical discharge ,or irregular bleeding (IMB or
PCB), but 70% of cases are asymptomatic.
Complications of Chlamydia infection
• Pelvic inflammatory disease (10–40%).
• Perihepatitis (Fitz–Hugh–Curtis syndrome).
• Reiter’s syndrome (more common in men):
• arthritis
• urethritis
• conjunctivitis.
• Tubal infertility.
• Risk of ectopic pregnancy.
Diagnosis
• Vulvovaginal or endocervical swab for nucleic acid amplification test
(NAAT). Requires specific medium.
• Real-time polymerase chain reaction.
• Endocervical, urethral, and vaginal swab for culture but are not
sensitive
• ELIZA test on endocervical smear. Old method
Screening and opportunistic testing
•
Partners of patients diagnosed or suspected with infection
•
History of chlamydia in the last year

Genital infections in gynaecology
10
•
Patients attending GUM clinics
•
Patients with two or more partners within 12 months
•
Women undergoing termination of pregnancy
•
History of other sexually transmitted infection and HIV.
Treatment
General advice
•
Avoid intercourse, before treatment of both partners is complete.
•
Use of condoms should be encouraged to prevent reinfection and other
STIs.
•
Retesting if any doubt about complete treatment. Test of cure should
be performed a minimum of 5 weeks after initiation of treatment.
•
Test of cure should be routine in pregnancy.
Antibiotic treatment
- Doxycycline 100 mg twice a day for 7 days
- Azithromycin 1 g as single dose
- Ofloxacine 400 mg daily for 7 days
-In pregnancy:
- Azithromycin 1 g as single dose
- Erythromycin 500 mg twice a day for 14 days
-Partner should be fully screened and treated
Implications in pregnancy
Association with preterm rupture of membranes and premature
delivery.The risks to the baby are of:
• Neonatal conjunctivitis (30% within the first 2wks).
• Neonatal pneumonia (15% within the first 4mths).
Genital infections in gynaecology
11
Upper genital infection
Pelvic inflammatory disease:
Definition:
PID is infection of the upper genital tract.
- Pelvic inflammatory disease is characterized by inflammation and
infection arising from the
endocervix leading to endometritis,
salpingitis,
oophoritis, pelvic peritonitis and subsequently
formation of
tubo-ovarian and pelvic abscesses.
Causes
• Most commonly caused by ascending infection from the endocervix,
but may also occur from descending infection from organs such as the
appendix.
• There are multiple causative organisms:
• 25% of cases estimated to be caused by Chlamydia trachomatis and
Neisseria gonorrhoeae

Genital infections in gynaecology
12
• anaerobes and endogenous agents, either aerobic or facultative, may be
responsible for the remainder.
Pathophysiology
• First stage of salpingitis is mucosal Inflammation with swelling,
redness and deciliation.
• Submucosal invasion with polymorph nuclear cell, mononuclear and
plasma cell.
• Inflammatory exudates fills the lumen.
• Inflammation extends to the serosal surface, and pus exudes from the
fimbriae to the ovaries and adnexia.
• Omentum usually confines the infection to the pelvis, however,
infection may cause tissue damage end with tubo-ovarian abscess .
• Subsequent scarring made the fimbrial end adherent to the tube and
sealing the end of the tubes .
• The-uterus fixed by adhesion and becomes retroverted.
• Hydrosalpinx, and if infected pyosalpinx results .
• Chlamydia and gonorrhoea can also cause perihepatitis leading to
adhesions between the liver and the peritoneal surface. This gives a
typical violin string appearance at laparoscopy and is known as the
Fitz–Hugh–Curtis syndrome.
History and examination
• A full gynaecological history including sexual history.
• An abdominal examination to elicit the site and severity of the pain.
• Speculum and vaginal examination to assess for adnexal masses,
vaginal discharge, or cervical excitation.
Risk factors for PID
• Age <25.
• Previous STIs.
• New sexual partner/multiple sexual partners.
• Uterine instrumentation such as surgical termination of pregnancy and
intrauterine contraceptive devices.
• Post-partum endometritis.
Protective factors
These include the use of barrier contraception, the
levonorgestrel (LNG)(Mirena IUS) and the COCP.

Genital infections in gynaecology
13
DIAGNOSIS:
Signs & symptoms
-PID may be relatively asymptomatic, the diagnosis only being made
retrospectively during investigation of subfertility.
-Symptoms may include some or all of the following:
• Pelvic pain (may be unilateral), constant or intermittent.
• Deep dyspareunia.
• Vaginal discharge (usually due to concurrent vaginal infection).
• Irregular and/or more painful menses.
• IMB/PCB.
• Fever (unusual in mild/chronic PID).
-Signs (at least one of which should be present when making a PID
diagnosis) are:
• Cervical motion pain (cervical excitation).
• Adnexal tenderness (commonly bilateral, but may be unilateral).
• Elevated temperature (unusual in mild/chronic infection).
Investigations
• High vaginal swab for tricomonas and vaginosis and endocervical
swab for gonorrhea and Chlamydia.
• WCC, ESR and CRP may be elevated.
• USS may be indicated if a tubo-ovarian abscess is suspected.
• Laparoscopy is the gold standard test; however, it is invasive and only
used where diagnosis is uncertain.
Complications of PID
• Tubo-ovarian abscess.
• Fitz-Hugh–Curtis syndrome.
• Recurrent PID.
• Ectopic pregnancy.
• Infertility.
Diffrential diagnosis:
• Ectopic pregnancy.
• Acute appendicitis.
• Endometriosis.
• Complicated ovarian cyst.
Genital infections in gynaecology
14
• Constipation.
Treatment
Early empirical treatment is recommended. Multiple antibiotic regimes
are required to cover all potential causative organisms.
• pregnancy test should be done in all cases to rule out ectopic
pregnancy.
• Most patients can be treated in an outpatient setting.
• Review after 72h to ensure adequate response.
• Contact tracing and treatment of partners is essential.
• Inpatient treatment may be required if symptoms are severe, fail to
respond, or abscess is suspected.
• If there is USS evidence of a tubo-ovarian abscess, drainage may be
required either by ultrasonic guided aspiration or at laparoscopy.
There are several differing antibiotic regimes that are used;
Mild/moderate infection (outpatient treatment)
• Oral ofloxacine 400mg bd + oral metronidazole 400 mg bd daily for
14 days or
• IM ceftriaxone 500 mg + oral doxycycline 100 mg bd 14 days + oral
metronidazole 400 mg bd 14 days.
Principles of inpatient treatment
•
Adequate supportive care
•
Strict watch on fluid balance
•
Parenteral antibiotics:
I.V. ceftriaxone 2g od + I.V. doxycycline 100mg bd followed by oral
doxycycline 100mg bd 14 days + oral metronidazole 400mg bd for 14
days.
•
Drainage of abscess is indicated if i.v. treatment failed after 24-48
hours & sometimes the affected tube/ovary may have to be removed. .
Signs and
symptoms
