Restrictive lung disease
Lecture fourRestrictive Lung Disease
Mostly cause is unknownEqual decline in FEV1 & FVC
Diffuse Interstitial Disease
Spectrum of diseases that involves pulmonary connective tissue .Many of the diseases have a similar clinical picture and an unknown etiology
Present with dyspnea, tachypnea, crackles, cyanosis, and wheezing. Pulmonary function tests show decreased diffusing capacity, lung capacity, and compliance
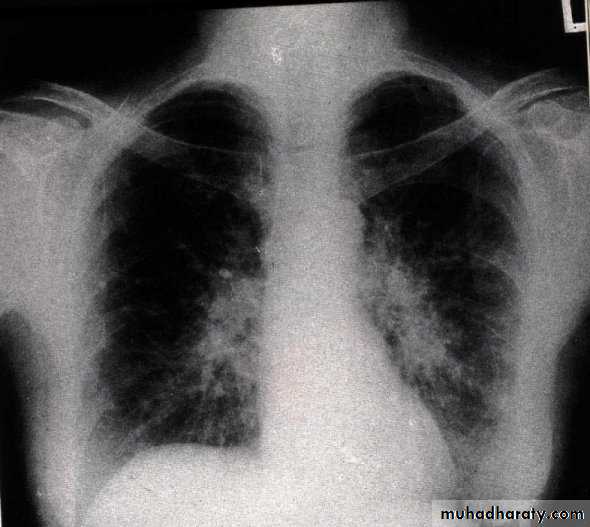
Chest x-ray shows irregular lines or a ground glass appearance
Eventual pulmonary hypertension, cor pulmonale, and honeycomb lung occur.
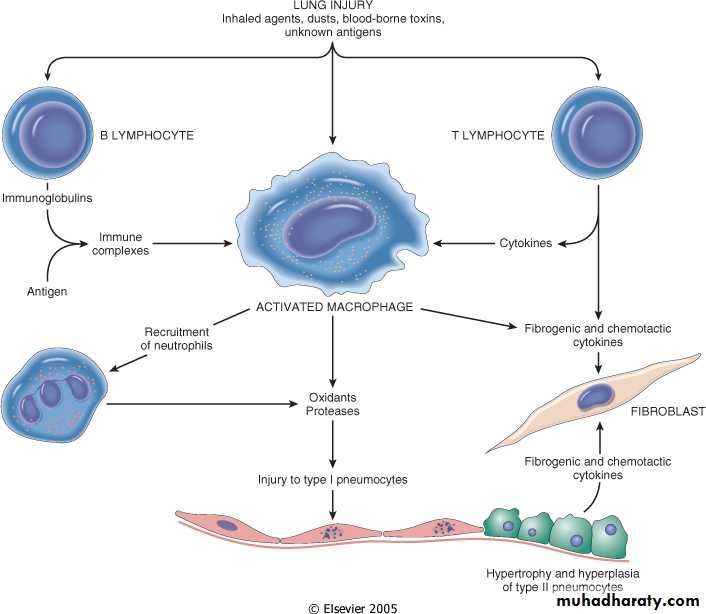
Pathogenesis: thought to be inflammatory
Frequency: pneumoconiosis (25%), sarcoidosis (20%), idiopathic pulmonary fibrosis (15%), and collagen vascular disease (10%)
Idiopathic Pulmonary Fibrosis
Fibrosing disease of unknown causeDiagnosis is based on constellation of factors: clinical presentation, radiology, and pathology
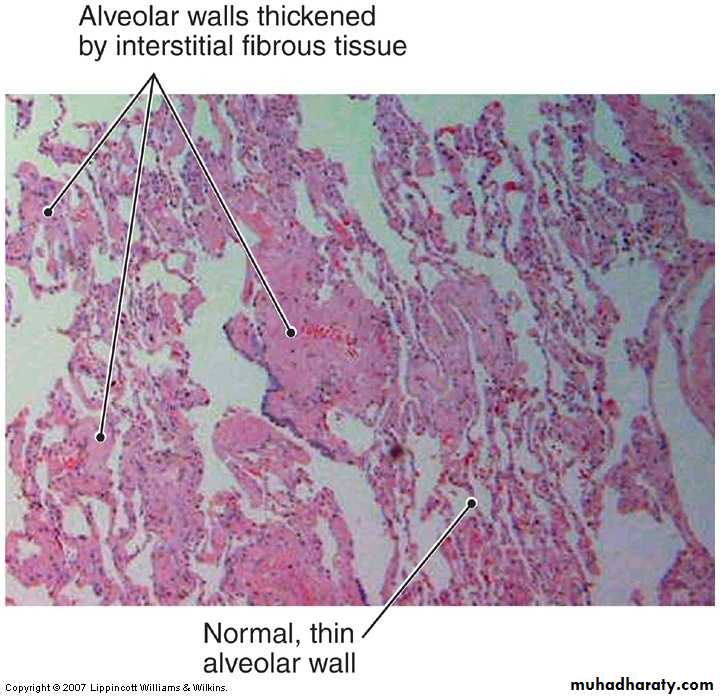
Thought to be caused by repeated bouts of alveolitis with fibroblastic healing
The pathologic correlate is usual interstitial pneumonia (UIP)
Clinical course :- Patients usually present between 40 and 70 years of age with a dry, relentless cough.
Progresses to dyspnea, cyanosis, and heart and lung failure
Patients usually die within three years of diagnosis
Lung transplant is the only effective treatment
Idiopathic Pulmonary Fibrosis/ Usual Interstitial Pneumonia
Cryptogenic Organizing Pneumonia
Consists of loose connective tissue plugs in the acini and terminal bronchioles. No evidence of interstitial fibrosisFormerly known as bronchiolitis obliterans with organizing pneumonia
Most patients have a spontaneous regression, and require months of steroid treatment
Similar histologic and clinical patterns can occur in the presence of other insults.
Collagen Vascular Disease
Many different collagen vascular diseases affect the lung architecture
lupus, scleroderma, rheumatoid arthritis, and mixed connective tissue disease are some examples
Lung involvement is highly variable between diseases and between individual cases of each disease
Pattern of involvement is also highly variable
has four different patterns of lung involvement ranging from chronic pleuritis to fibrosis to pulmonary hypertension.
Pneumoconiosis
Pneumoconiosis
Non-neoplastic lung disease caused by a wide variety of particulates, vapors, and fumes.Originally documented as exposures in the workplace, but is now extending to exposures in the population from ambient air exposure
Effects can vary widely from patient to patient and depend largely on the agent the person was exposed to and the degree of exposure
Pneumoconiosis Pathogenesis
In general, development and extent of disease depends on four variables:Amount of agent in the lungs- depends on concentration of exposure, duration of exposure and clearance mechanisms
Size and shape , Solubility and toxicity of particles- smaller particles rest in terminal airways and alveoli causing more damage
Additional effects of other irritants- e.g. smoking and asbestos exposure
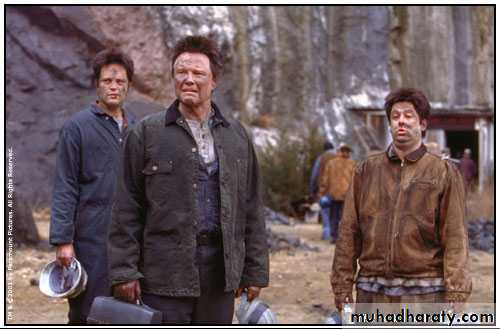
Coal Workers’ Pneumoconiosis (CWP)
Results from exposure to coal dust
Response to exposure varies greatly from person to person. Most are asymptomatic.
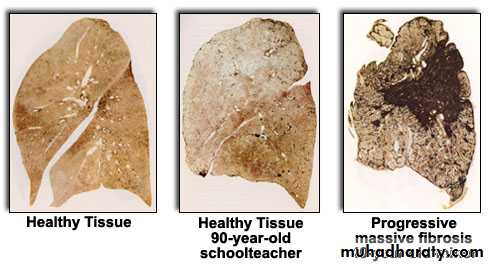
The range of host responses varies from asymptomatic anthracosis to simple CWP to complicated CWP, or progressive massive fibrosis. Complicated CWP is the only one of clinical concern
Coal Induced Pulmonary Lesions
Anthracosis- has no deleterious effect on patients. Manifests as black carbon streaks in lymphatics and nodes. Carbon is also ingested by macrophages. Present in majority of autopsies, because it is also seen in people that smoke or live in urban areasSimple CWP- characterized by coal macules and nodules. They are primarily located near bronchioles in the lower lung lobes. Rarely can lead to centilobular emphysema
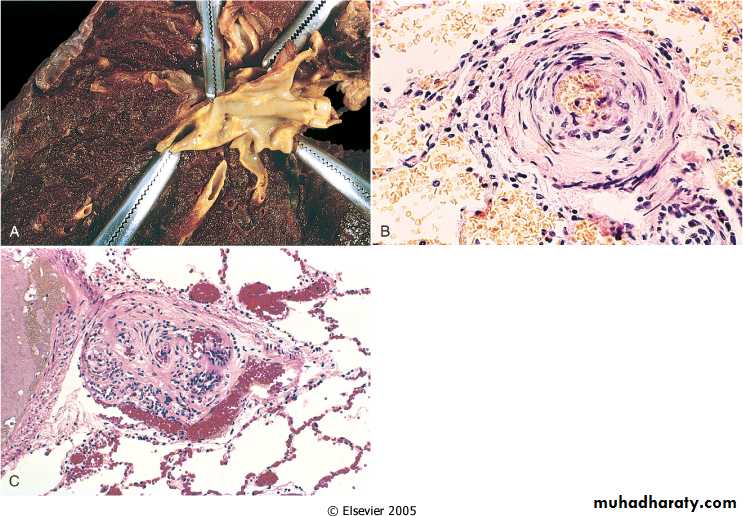
Complicated CWP (Progressive massive fibrosis)- is a progression from sCWP and takes years to develop. Consists of multiple confluent large black fibrotic scars (“black lung”). Terminal progression leads to pulmonary hypertension and corpulmonale, along with respiratory failure
Gross of “Black Lung”
Silicosis and Asbestosis
Also forms of pneumoconiosisSilicosis- most prevalent occupational disease. Caused by inhalation of silica. Progression is similar to that of CWP.
Silicosis also causes active secretion of inflammatory mediators by macrophages
Carries an increased risk of tuberculosis
Also causes PMF similar to other pneumoconiosis
Exposure to large concentrations of silica can lead to acute disease
Silicosis and Asbestosis
Asbestos- crystalline fibers of silicates that form sheets. Used widely in insulation and heat resistant products
Asbestos exposure is linked to fibrous plaques, pleural effusions, interstitial fibrosis, lung cancer, mesothelioma.
Characteristic that sets asbestos apart is its ability to induce neoplasm formation. Also acts in synergy with other carcinogens
about 5x risk of lung cancer in asbestos workers; about 55x risk of lung cancer in asbestos workers that smoke. Also, and about 1000x risk of mesothelioma in asbestos workers.
Asbestos reaches deep into the lung parenchyma and can reach the parietal surface forming collagenous plaques
Treatment Induced Pulmonary Disease
Drugs have been known to produce a wide range of pulmonary side effects from bronchospasm to ARDS to fibrosis.Bleomycin and amiodarone- fibrosis and pneumonitis
Aspirin and beta blockers- bronchospasm
Dozens of drugs- allergic hypersensitivity
Radiation causes a wide range of pulmonary complications. Pneumonitis and subsequent fibrosis are well documented effects.
Acutely the patient has fever and dyspnea
Some patients do not resolve and progress to fibrosis
Sarcoidosis
A systemic disease that has been known to affect almost any organ in the bodyCharacterized by non-caseating granulomas
Presents most often with bilateral hilar lymphadenopathy, fever, fatigue, and SOB
Also presents with ocular and skin lesions
Most prevalent in African American blacks, women, and people from the Southeast
Etiology is unknown. Thought to be a T cell hyperresponse to an unknown antigen.
Genetic factors are implicated- clustering in families and races.
Effects of Sarcoidosis
Pulmonary- grossly normal, but microscopically there are diffuse granulomas. Fibrosis and amyloid deposition occur. Pulmonary hypertension and cor pulmonale ensue
Systemic effects-
eye- iritis, corneal opacities, glaucoma, vision loss
Skin- very common, nodules or erythematous plaques
Oral cavity- similar plaques and nodules of the skin
Muscle- weakness, tenderness, fatigue
Spleen, bone marrow- diffuse replacement with granulomas
Sarcoidosis
Hypersensitivity Pneumonitis
Hypersensitivity pneumonitis- an immunologically mediated interstitial lung disorder caused by prolonged exposure to an offending environmental agentThe agent is normally organic and related to occupations or hobbies:
Bird fancier’s lung
Farmer’s lung
Patients present with fever, dyspnea, cough, often associated with exposure to antigen.
Represents a hypersensitivity reaction involving alveoli, not bronchioles. Removal of the offending antigen is essential to prevent terminal fibrosis
Pathogenesis of hypersensitivity pneumonitis involves immune complex formation and delayed hypersensitivity
Smoking Related Interstitial Disease
Desquamative Interstitial Pneumonia (DIP)- collection of macrophages with brown pigment in the airspaces. Not squamous cells. Thickened septa lined by reactive pneumocytes.
Presents in 40’s and 50’s with cough, dyspnea, clubbing
All patients are smokers
Steroid therapy and smoking cessation is curative
Respiratory Bronchiolitis- similar collection of macrophages as seen in DIP, but macrophages are located in the bronchioles.
“Respiratory bronchiolitis-associated interstitial lung disease”- given to those with significant symptoms, or radiologic abnormalities
Mild dyspnea, cough in smokers around 40-60
Smoking cessation is curative
Vascular lung disease
Pulmonary EmbolismCommon. Causes almost 50,000 deaths/yr
Blood clots that occlude the pulmonary artery
Vast majority are from lower extremities
Risk factors- Virchow’s triad- stasis, hypercoaguable states, injury
Burn, trauma, cancer, and immobile patients
Presenting symptoms
Effects depend on size of occulsion
Respiratory compromise is frequent
Sudden death due to saddle embolus or critical compromise of respiratory function
Pulmonary Hypertension
Normal pressure within the pulmonary artery vasculature is 13-17 mmHg. Elevation of this normal pressure to approximately 25 mmHg and over is pulmonary hypertensionCan be primary or secondary. Most disease is secondary to abnormalities that increases pulmonary artery blood flow or pressure:
Chronic obstructive or restrictive lung disease
Congenital or acquired heart disease- e.g. mitral stenosis
Recurrent thromboembolism
Autoimmune disorders- e.g. scleroderma directly involves pulmonary vasculature causing sclerosis
Pulmonary Hypertension
Histologic morphologyMedial hypertrophy, intimal fibrosis, stenosis
Extreme cases-plexogenic pulmonary arteriopathy