SUPRAVENTRICULAR' TACHYCARDIAS
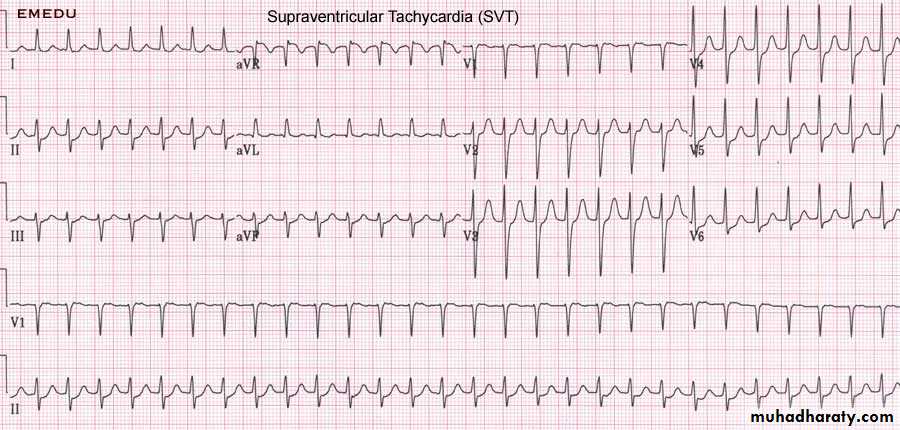
The term 'supraventricular tachycardia' (SVT) is commonly used to describe a range of regular tachycardias that have a similar appearance on an ECG. These tachycardias are usually associated with a narrow QRS complex and are characterised by a re-entry circuit or automatic focus involving the atria. The term SVT is misleading, as in many cases the ventricles also form part of the re-entry circuit, e.g. in patients with atrioventricular re-entrant tachycardia.AV NODAL RE-ENTRY TACHYCARDIA (AVNRT)
This is due to re-entry in the right atrium and AV node and produces a regular tachycardia with a rate of 140-220/min. It tends to occur in hearts that are otherwise normal, and episodes may last from a few seconds to many hours. The patient is usually aware of a fast heart beat and may feel faint or breathless. Polyuria, mainly due to the release of atrial natriuretic peptide, is sometimes a feature, and cardiac pain or heart failure may occur if there is coexisting structural heart disease.
Management
Treatment is not always necessary. However, an attack may be terminated by carotid sinus pressure or other measures that increase vagal tone (e.g. Valsalva manoeuvre , induce vomiting emersion of the head in cold water ). Intravenous adenosine or verapamil will restore sinus rhythm in most cases. Suitable alternative drugs include β-blockers, flecainide and digoxin. In an emergency when there is severe haemodynamic compromise, the tachycardia should be terminated by DC cardioversion.If attacks are frequent or otherwise disabling, prophylactic oral therapy with a β-blocker, verapamil, disopyramide or digoxin may be indicated. Catheter ablation offers a very high chance of complete cure and is usually preferable to long-term drug treatment.
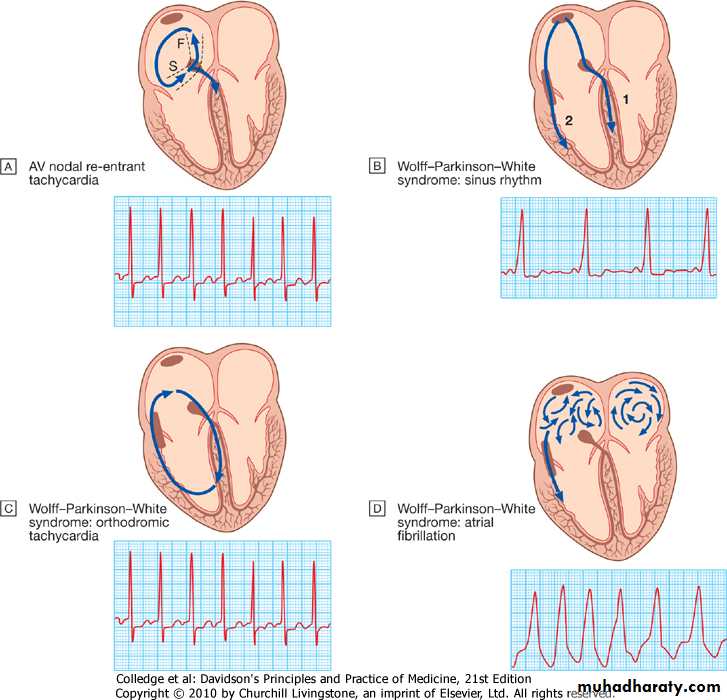
Wolff-Parkinson-White syndrome and atrioventricular re-entrant tachycardia
Sinus rhythm. In sinus rhythm the ventricles are depolarised through (1) the AV node and (2) the accessory pathway, producing an ECG with a short PR interval and broadened QRS complexes; the characteristic slurring of the upstroke of the QRS complex is known as a delta wave. The degree of pre-excitation (the proportion of activation passing down the accessory pathway) and therefore the ECG appearances may vary a lot, and at times the ECG can look normal.
2- Orthodromic tachycardia. This is the most common form of tachycardia in WPW. The re-entry circuit passes antegradely through the AV node and retrogradely through the accessory pathway. The ventricles are therefore depolarised in the normal way, producing a narrow-complex tachycardia that is indistinguishable from other forms of SVT.
3- Atrial fibrillation. In this rhythm the ventricles are largely depolarised through the accessory pathway, producing an irregular broad-complex tachycardia
Catheter ablation is first-line treatment in symptomatic patients and is nearly always curative. Prophylactic anti-arrhythmic drugs, such as flecainide, propafenone or amiodarone, can also be used. These slow the conduction rate and prolong the refractory period of the accessory pathway. Digoxin and verapamil shorten the refractory period of the accessory pathway and should be avoided.
VENTRICULAR TACHYARRHYTHMIAS
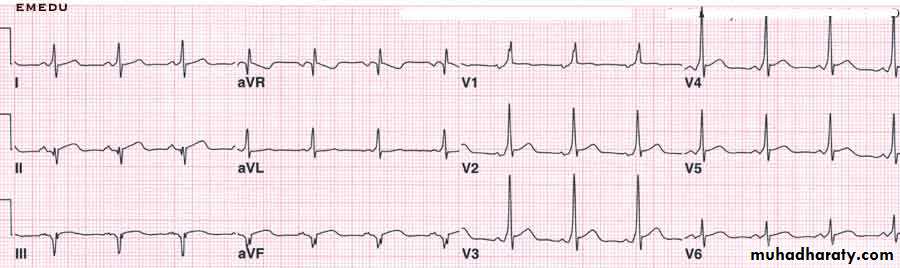
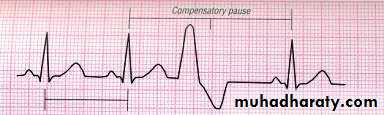
VENTRICULAR ECTOPIC BEATS (EXTRASYSTOLES, PREMATURE BEATS)The QRS complexes of ventricular ectopic beats are of abnormal morphology because the bundle branches are activated one after the other, rather than simultaneously. The ECG shows premature broad, bizarre QRS complexes which may be unifocal (identical beats arising from a single ectopic focus) or multifocal (varying morphology with multiple foci). 'Couplet' and 'triplet' are terms used to describe two or three successive ectopic beats, whereas a run of alternate sinus and ectopic beats is known as ventricular 'bigeminy'.
Patients are usually asymptomatic but may complain of an irregular heart beat, missed beats or abnormally strong beats (due to the increased output of the post-ectopic sinus beat). The significance of ventricular ectopic beats (VEBs) depends on the presence or absence of underlying heart disease.
VENTRICULAR ECTOPIC BEATS IN OTHERWISE HEALTHY SUBJECTS
VEBs are frequently found in healthy people, and their prevalence increases with age. Ectopic beats in patients with otherwise normal hearts are more prominent at rest, and disappear with exercise. Treatment is not necessary unless the patient is highly symptomatic, in which case β-blockers can be used.VEBs are sometimes a manifestation of otherwise subclinical heart disease, particularly coronary artery disease.
VENTRICULAR ECTOPIC BEATS ASSOCIATED WITH HEART DISEASE
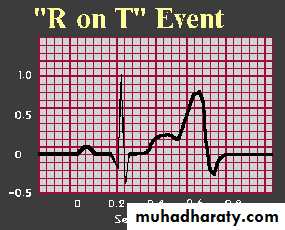
Frequent VEBs often occur during acute myocardial infarction but need no treatment. Patient with R on T or Persistent frequent (> 10 per hour) ventricular ectopic beats in patients who have survived the acute phase of myocardial infarction indicate a poor long-term outcome. Other than β-blockers, anti-arrhythmic drugs do not improve and may even worsen prognosis.VEBs are common in patients with heart failure, when they are associated with an adverse prognosis, but again the outlook is no better if they are suppressed with anti-arrhythmic drugs. Effective treatment of the heart failure may suppress the ectopic beats.
Ventricular ectopics are also a feature of digoxin toxicity, are sometimes found in mitral valve prolapse, and may occur as 'escape beats' in the presence of an underlying bradycardia. treatment should always be directed at the underlying condition.
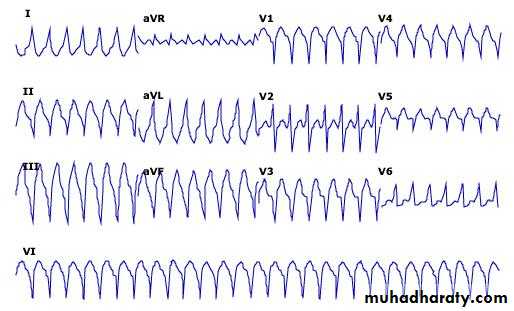
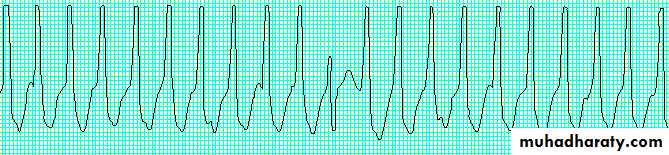
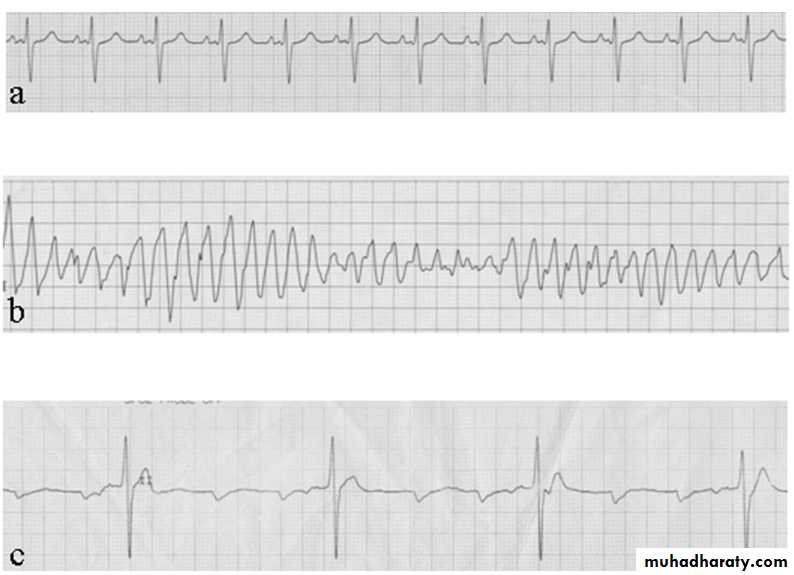
VENTRICULAR TACHYCARDIA (VT)
INCLUDEPICTURE "mk:@MSITStore:E:\\books\\davidsons-original.chm::/HTML/common/showimage.cfm@mediaisbn=9780443100574&size=thumbnails&figfile=f00574-018-f046.jpg" \* MERGEFORMATINET
FEATURES IN FAVOUR OF VENTRICULAR TACHYCARDIA IN THE DIFFERENTIAL DIAGNOSIS OF BROAD-COMPLEX TACHYCARDIA
A history of myocardial infarction
AV dissociation (pathognomonic)Capture/fusion beats (pathognomonic,)
Extreme left axis deviation
Very broad QRS complexes (> 140 ms)
No response to carotid sinus massage or i.v. adenosine
INCLUDEPICTURE "mk:@MSITStore:E:\\books\\davidsons-original.chm::/HTML/common/showimage.cfm@mediaisbn=9780443100574&size=thumbnails&figfile=f00574-018-f047.jpg" \* MERGEFORMATINET
External ECG and intracardiac or oesophageal ECG may help to establish the diagnosis. When there is doubt it is safer to manage the problem as VT, which is by far the most common cause of a broad-complex tachycardia.
The common causes of ventricular tachycardia include
*acute myocardial infarction,*cardiomyopathy
* chronic ischaemic heart disease, particularly when it is associated with a ventricular aneurysm or poor left ventricular function.
*VT occasionally occurs in patients with otherwise healthy hearts ('normal heart VT'), usually because of abnormal automaticity in the right ventricular outflow tract or one of the fascicles of the left bundle branch. In these cases the prognosis is good and catheter ablation can be curative.
Management
Prompt action to restore sinus rhythm is required and in most cases should be followed by prophylactic therapy.*DC cardioversion is the treatment of choice if systolic BP is less than 90 mmHg. If the arrhythmia is well tolerated,
*Intravenous amiodarone may be given as a bolus followed by an intravenous infusion.
*Beta-blockers are effective
*In patients at high risk of arrhythmic death (e.g. those with poor left ventricular function, or where VT is associated with haemodynamic compromise), the use of an implantable cardiac defibrillator is recommended.
*Rarely, surgery or catheter ablation can be used .
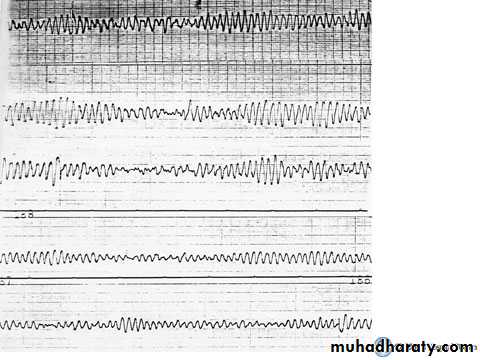
Ventricular fibrillation and pulseless ventricular tachycardia
INCLUDEPICTURE "mk:@MSITStore:E:\\books\\davidsons-original.chm::/HTML/common/showimage.cfm@mediaisbn=9780443100574&size=thumbnails&figfile=f00574-018-f030.jpg" \* MERGEFORMATINETThese are the most common and most easily treatable cardiac arrest rhythms. Ventricular fibrillation produces rapid, ineffective, uncoordinated movement of the ventricles, which therefore produce no pulse. The ECG shows chaotic, bizarre, irregular ventricular complexes. Defibrillation is the only effective treatment for these arrhythmias, and will restore cardiac output in more than 80% of patients if delivered immediately. However, the chances of a successful outcome fall by around 10% with each minute's delay, and by more if basic life support is not given .
TORSADES DE POINTES
This form of polymorphic VT is a complication of prolonged ventricular repolarisation (prolonged QT interval). The ECG shows rapid irregular complexes that oscillate from an upright to an inverted position and seem to twist around the baseline as the mean QRS axis changes. The arrhythmia is usually non-sustained and repetitive but may degenerate into ventricular fibrillation. During periods of sinus rhythm, the ECG will usually show a prolonged QT interval (> 0.42 s at a rate of 60/min).CAUSES OF LONG QT INTERVAL AND TORSADES DE POINTES
BradycardiaBradycardia compounds other factors that cause torsades de pointes
Electrolyte disturbanceHypokalaemia
HypomagnesaemiaHypocalcaemia
Drugs
Disopyramide (and other class la anti-arrhythmic drugs, p. 572)Sotalol, amiodarone (and other class III anti-arrhythmic drugs)
Amitriptyline (and other tricyclic antidepressants)
Chlorpromazine (and other phenothiazines)
Erythromycin (and other macrolides) … and many more
Congenital syndromes
Romano-Ward syndrome (autosomal dominant)Jervell and Lange-Nielson syndrome (autosomal recessive, associated with congenital deafness)
Long QT : LQT 1 , LQT 2 , LQT 3 and LQT 4
Management
*Treatment should be directed at the underlying cause.
*Intravenous magnesium (8 mmol over 15 minutes, then 72 mmol over 24 hours) should be given in all cases.
*Atrial pacing will usually suppress the arrhythmia through rate-dependent shortening of the QT interval. *Intravenous isoprenaline is a reasonable alternative to pacing but should be avoided in patients with the congenital long QT syndromes.
*Long-term therapy may not be necessary if the underlying cause can be removed.
*Beta-blockers are effective at preventing syncope in patients with congenital long QT syndrome.* Some patients, particularly those with extreme QT interval prolongation (> 500 ms) or certain high-risk genotypes should be considered for implantation of a defibrillator.
*Left stellate ganglion block may be of value in patients with resistant arrhythmias.
THE BRUGADA SYNDROME is a related genetic disorder that may present with polymorphic VT or sudden death. It is characterised by a defect in sodium channel function and an abnormal ECG (right bundle branch block and ST elevation in V1 and V2 but not usually prolongation of the QT interval).