lect-5 PROF.DR.Al-JANABI
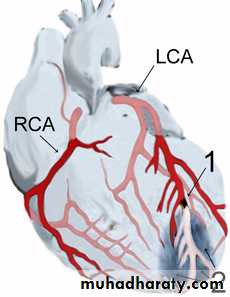
Acute Myocardial Infarction(AMI)Refers to myocardial cell death& necrosis due to acute&critical interruption of blood supply commonly caused by sudden thrombotic occlussion of an atheromatous coronary artery(See diagram→infarcted apical(2) area due distal occlusion of LAD(1).
Pathology of AMI&it's sequelae:I.primary pathology is ruptured atheromatous plaque→occlusive thrombus formation→total or subtotal obstruction of CA→ischaemic myocardial necrosis. II.Consequences of CA occlusion: 1.sudden severe&irreversible→ischemia→ myocardial injury→electrical instability→ ventricular arrhythmias.infact ventricular fibrillation(VF) is main cause of sudden cardiac death(SCD) in patients with AMI before arrival to hospital. 2.Cell death&myocardial necrosis occur within 6-8hrs then healing by fibrosis&scar formation within 4-6 weeks. 3.Mechanical sequeale: -Infarct segment→poor&incoordinate myocardial contraction→ LV-systolic dysfunction,heart failure(HF)&even cardiogenic shock in large MI. --Myocardial rupture at infarct site→either ventricular septal defect( VSD),mitral regurgitation(MR) due to ruptured papillary muscle or rupture of free LV wall→massive haemopericardium →fatal cardiac temponade. -Ischemic damage of conducting tissue →conduction disorders like various bradycardias ,AV block or bundle branch block. -The weak&yielding scar at site of infarct→ →akinetic or dyskinetic area or true LV aneurysm. –The thin ,weak infarct region→LV remodeling(change of size ,shape&function)as this thin area can not withstand pressure& volume load of LV causing the LV to dilate,hypertrophies& become more spherical rather than ellepticl→LV systolic dysfunction&Late HF. 4.Inflammatory i.e acute pericarditis. 5.Thrombotic i.e mural thrombus at infarct site →systemic thromboemboli.
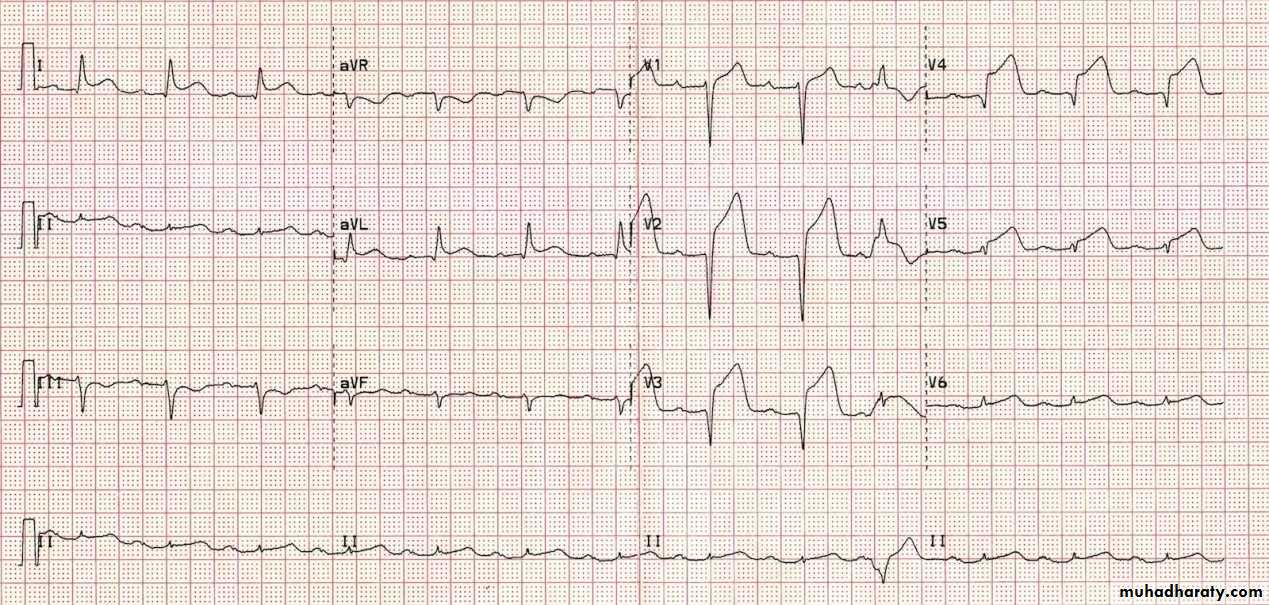
RFs of AMI: 1. Age 2. Sex: At any given age men are more at risk than women 3.DM.4.HTN. 5.Dyslipidemia( particularly high low-density lipoprotein, low high-density lipoprotein and high triglycerides 6.Tobacco smoking, including secondhand smoke 7.FH of IHD; particularly if one has a first-degree relative (father, brother, mother, sister) who suffered a 'premature' myocardial infarction (defined as occurring at or younger than age 55 years (men) or 65 (women). 8.Obesity.9.Psychosocial factors including, low socio-economic status, social isolation, negative emotions and stress increase the risk of myocardial infarction and are associated with worse outcomes after myocardial infarction. 10.Alcohol — Studies show that prolonged exposure to high quantities of alcohol can increase the risk of heart attack. 11. Oral contraceptive pill – combined oral contraceptive pills modestly increased risk of MI, esp.in presence of other risk factors. Clinical features:AMI often presents with severe retrosternal chest pain,often lasts>30min.&may lasts hours,unrelieved by rest or GTN&is associated with visceral symptoms(nausea& vomiting)&diaphoresis due to activation of autonomic nervous system(ANS).Sometimes,AMI painless esp.elderly,diabetics or people with high pain threshold&may present by sudden cardiac death,due unwittnessed VF. Signs:none in small MI.but patient may be restless&anxious due to distressing&frightening chest pain.Sympathetic nervous system(SNS)→transient pallor,sweat, cold peripheries,sinus tachycardia&↑BP but parasympathetic(PNS) activation,(often with inferior MI)→transient sinus bradycardia&even drop of BP but bradycardia&even AV blocks often due to nodal ischemia. Rapid pulse&persistent sinus tachycardia may reflect left ventricular systolic dysfunction(LVSD) or HF due to large MI which may→ cardiogenic shock. -Apex often quiet,difficult to feel.Diffuse precordial systolic pulsation may be felt due to dyskinetic protrusion of infracted area during systole.Heart sounds may be quiet&S3,S4 may be heard.Apical systolic murmur due ischemic papillary dysfunction→MR. but loud pansystolic murmur at apex indicate ruptured papillary m&at left sterna edge(LSE) indicates perforated interventricular septum( IVS) Pulmonary basal crackles indicate left ventricular failure( LVF). .Dx of AMI: WHO recommends presence of two of following THREE criteria:1.Ischemic type chest pain or discomfort.2.Serial ECG changes consitent with MI.3.Rise&rise of serum markers. The ECG changes of ST-seg.elevation MI: 1.STseg.↑,convex up- wards.2.T-wave inversion.3.Abnormal Q-wave.
.
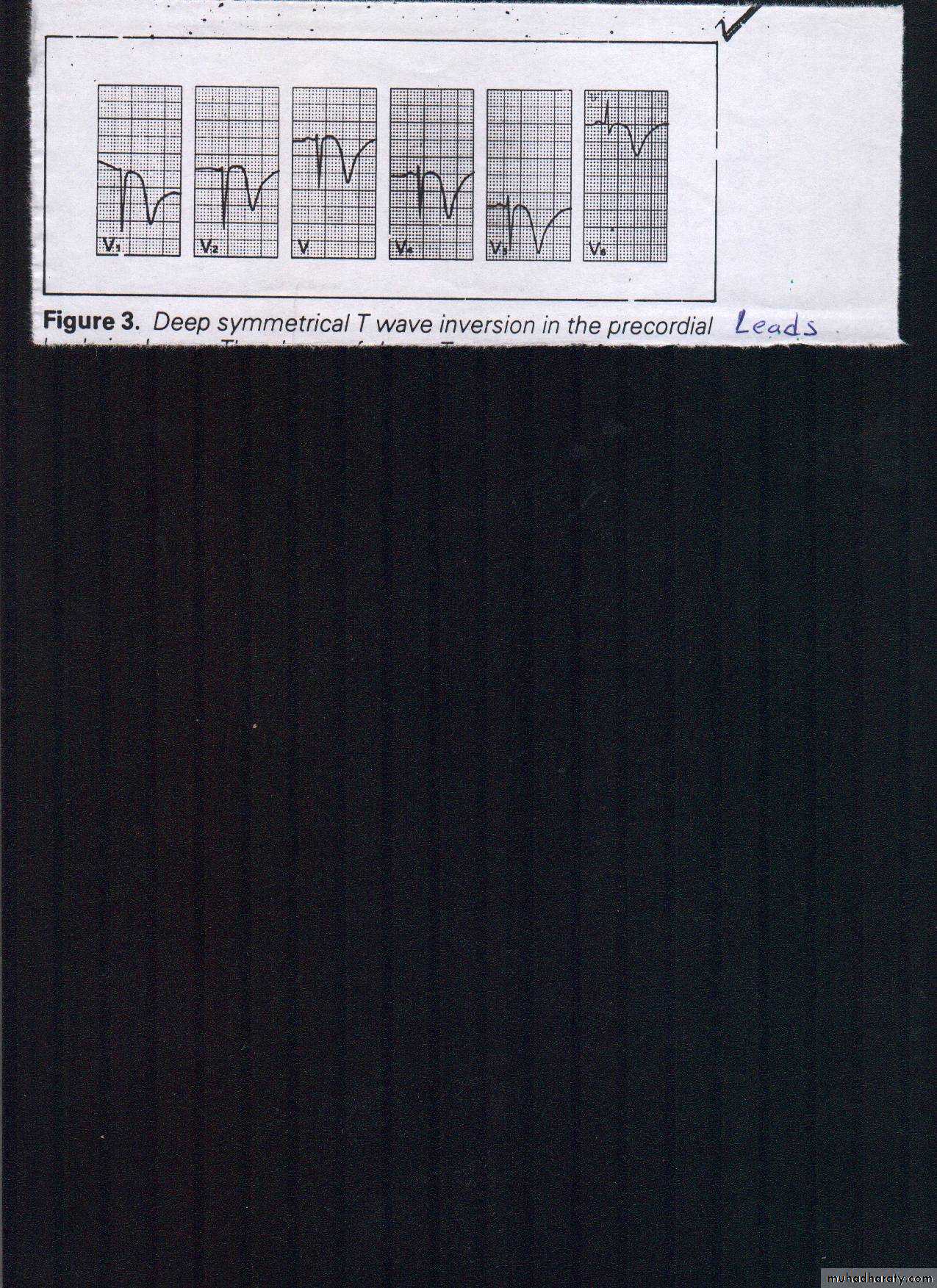
AMI classified based on ECGinto: 1.ST seg.Elevation Myocardial Infarction(STEMI)(formerly called transmural or Q-wave infarction).2.Non ST seg.Elevation Myocardial Infarction(NSTEMI) (formerly called subendocardial or nonQ-wave infarct.(see ECG→only"deep symmetrical T-wave inversion")
II.Site of Infarction.1.Ant.MI:Changes seen in one or more ofthe leads recording from ant.wall of LV(V1---V6&I- aVL. 2.Inferior MI (II III aVF) 3.Posterior MI. As the posterior myocardium is not directly visualised by the standard 12-lead ECG,so suspected by reciprocal changes of post.STEMI seen in the anteroseptal leads V1-3(Horizontal ST depression,Tall R waves, Upright T waves& Dominant R wave (R/S ratio > 1) in V2).Dx confirmed by post.leads→changes of post.STEMI. 3.Serum markers:They're intracellular enzymes&proteins released into blood following myocardial cell necrosis1.Cardiac troponins ,T&I(cTnT&cTnI).-Cardiac specific proteins,sensitive,rise early(2-4hrs)&peak in- 1-2/7&last long1-2/52.2.Other enzymes(CPK, AST,ALT&LDH);Non specific&now abandoned. Other investigations: 1.Echocardiogram.Infarcted area look akinetic&can detect RVI,VSDorMR&toasses LV function.2.IFDx remains doubted 99Tclabelled pyrophosphate scan→hot area if +Ve&Th201 scan→cold area if +ve 3.Blood tests(FBS&lipid profile
Complications of AMI:early&late A.Early:I.Arrhythmias & Conduction disorders :Very common(95%)include:-VEs;often benign but may compex -VT:More serious as it may degenerate into VF&cause haemodynaemic compromise. Atrial fibrillation(AF)&atrial flutter(AFL); reflect LVdysfunction due to large MI&poor prognostic indicator. Supraventricular tachycardia(SVT)not infrequent.less serious than ventricular tachycardia(VT). Sinus tachycardia.Common but persistent STC is poor prognostic factor. Sinus bradycardia:common with inferiorMI due nodal ischemia.AV-block:All degrees of AV-block can benign but 2nd&3rd degree types are benign if they cmplicate inferior MI but prognostically bad if complicate ant.MI.
II.Mechanical complications.1.CHF:commonly due to large infarct or right ventricular infarction(RVI) detected by right-sided leads. 2,Cardiogenic shock:Often caused by massive myocardial damage. III,others*:Acute pericartditis→sharp pain& friction rub.
B.Late complications of AMI :1.Late CHF: Causes:*LV-remodeling prevented by ACEIs *LV aneurysm.2.Recurrent ventricular arrhythmias (VTorVF).seious,due re-entry&definitive R/ by ICD.3.Dressler's syndrome. Late pericarditis &often with pleuritis&fever.
Management of STEMI: Early&Late. 1.Early management 1.First aid Rx:1.obtain 12-leads ECG for Dx.2.Insert IV canula. 3.Antiplatelets in loading doses (chewable aspirine 300mg&oral clopedogril 150mg). 4.Pain relief by IV opiate&IV antiemetic.5.High flow O2. 6.Rapid transfer to CCU for monitoring.2.Urgent PCI if available is better than thrombo- lytic therapy to occluded artery. 3.Thrombolytic therapy if PCI not available or failed. Thrombolytic agents (streptokinase or tPA)given to all pts with STEMI&within 1st 2 hrs.3.parenteral heparin to support reperfusion therapy. 4.Adminstration of drugs that improve survival&reduce adverse outcomes of MI.*Antiplatelet therapy:1.Apirine for life. &Clopidogril for 2/52*β-blockers:metoprolol 50mg twice daily is given within 1st 24hrs .*ACEIs like captopril for all pts. with STEMI to counteract LV remodeling .5.Prohibit NSAIDs in all pts.with STEMI as they↑ mortality,Reinfarction,HTN,HF&myocardial rupture.
Longterm management: LINES:I.secondary prevention measures:1.continue drugs improving longterm prognos(ACEIs,β-blockers&aspirine).2.R/of modifiable RFs(smoking,lipids etc.). 3.continue prohibiting use of NSAIDS in pts.with STEMI. II.Rehabilitation by encourage programmed exercise(walking, cycling&gardening)&House work for women.Return to normal daily life regarding to work.driving or sex life in 6-8/52. Prognosis of AMI::depends on state of LV function,residual ischemia&propensity to late ventricular arrhythmias; so poor prognostic parameters are:*Clinical parameters( Presistent sinus tachycardia,AFor flutter,CHF,postinfarct angina,late ventricular arrhythmias&AV block *lab.parameters;ECG→ant.MI&bundle branch block. CxR:Cardiomegaly or frank pulmonary odema. Echo:Significantly ↓EF. Poor Ex.test:Impaired performance or marked ECG changes on low workload).*Others like continuing stress&social isolation.