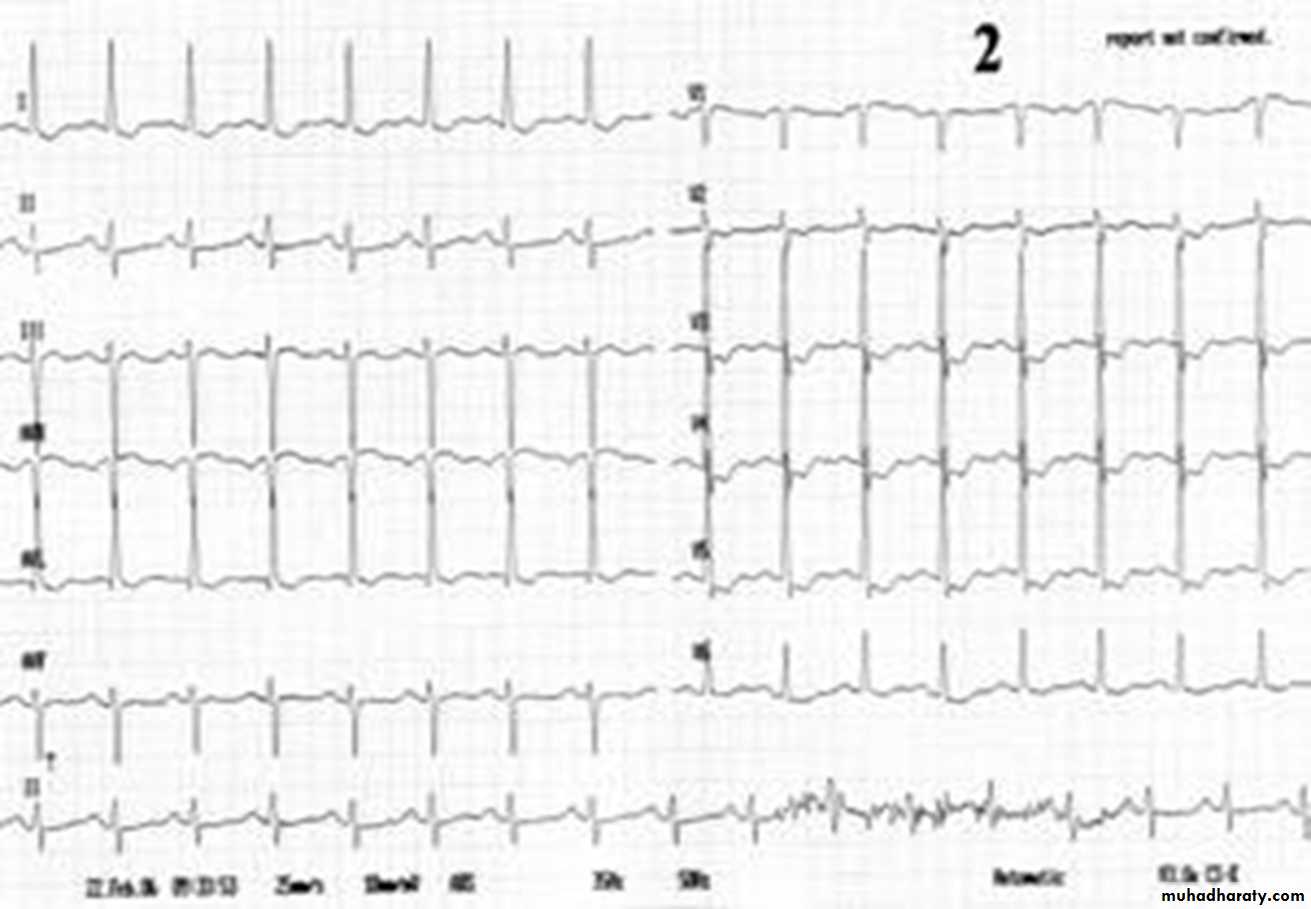
Cardio.Lect.4 1 Prof.HS Al-Janab Lab.investigations of angina: Generaltests.1.G.U.E.(glucose→DM2.BS&BU.3.Hb.→Anaemia.4.lipid profile B.Special cardiac investigations. 1CxR→*Cardiomegaly*CHF*aortic valve disease. 2.ECG. N in 50% of cases as pain-free pts,may have (N) ECG but Typical ECG changes of myocardial ischemia are (horizontal or down slopping ST↓ ≥ 1mm±T↓. Transient ST↑→prinzmetal angina Note;Typical ST seg.depression in leads V3-V6→myocardial ischemia.
3.xercise testing:- Standarized increases in external workload on the heart to provoke myocardial ischaemia by using Tradmill orBicycle ergometer with pt. monitoring for symptoms, abnormal rhythm or typical ECG changes(horizontal ST↓≥ 2mm or down slopping of seg↓.±T wave inversion&may ST-seg. However the test hase false +Ve&false –Ve &Sensitivity═70% &specificity═75% . -Contraindications of the stress test.1.Severe HTN. 2.Significant valve lesion.4.Recent AMI( < 1 week duration).5.unstable angina.6.HOCM.7.Severe HF.8.Pulmonary hypertension. 4.Echocardiography:Helps to:1.Dx as active ischemia→regional hypokinesia.—&prognosis to assess severity :by measuring LV-EF as an index of LV-systolic function&↓EF→poor prognosis. 5.Other tests:Radioisotope cardiac imaging&coronary angiography: Dx of angina:1.largely clinical&history of typical ischemic of angina is diagnostic. 2.ECG&other tests are confirming. DDx:From other causes of chest pain i.e other causes of cardiac pain or noncardiac causes like pulmonary,GIT,M/SK pains& Functional causes like Precordial catch syndrome) where Chest pain lasting only a few seconds. Treatment of angina
Goal of R/:The goals of therapy of are (1) amelioration of anginal symptoms and improved angina-free exercise capability and (2) prevention or reduction of adverse outcomes i.e subsequent AMI or ischemic sudden death(ISD). Lines of R/: I.Medical Rx. II.Interventional therapy i.e Revascularization by Percutaneous coronary intervention(PCI)&/or Coronary artery by-pass graft(CABG). Medical therapy:1.Generalmeasures. *Explanation&reassurence.Stable angina has a relatively good prognosis if treated .*Life style measures(Avoid large meal, encourage gradual&programmed exercise for at least 30min.aday walking , cycling or swimming &for some housewives house work may appropriate along with appropriate dietary measures).2.Rx of underlying cause(if any),e.g AS. 3.Rx of aggravating conditions like severe anaemia,tachycardia thyrotoxicosis, aortic stenosis, poorly controlled hypertension.) 4.RFs modification:All modifiable RFs need to be addressed& aggressively treated. Control of RFs will↓risk of MI&death in patients with angina. *Hypertension:by appropriate dugs.*Hyperlipidaemia by statins(HMG CoA reductase inhibitors)like atorvastatin. *DM:by appropriate antidiabetic measures. *Smoking:Strongly prohibited.The risk of IHD, stroke, and PVD is reduced within 1–2 years of smoking cessation&it reduces the risk of coronary artery mortality by up to 50% in 1 year &the prevalence of angina in smoking men under 60 after an initial attack was 40% less in those who had quit smoking compared to those who continued *Overwt :by wt-reduction measures. 5.Drug therapy:The antianginal drugs classified according to mode of action into SIX categories:5.1.B-blockers:Act by blocking β1- adreno- ceptors in the heart→↓HR,BP&Force of myocardial contraction thus↓ myocardial O2 demand at rest&exercise. β-blockers can be classified according to β-receptor blockade selectivity&lipidsolubility. Cardioselectives (atenolol, metoprolol& acebutolol)block cardiac β1reptors&noncardioselectives(propranolol, oxprenolol or sotalol) block cardiac β1 receptors&β2 receptors in bronchi&blood vessels like &hence can worsen asthma&PVD. Lipophilic β -blockers metabolized by liver&hence dosing is twice daily&can cross blood brain barrier&thus induce more CNS side effects .Hydrophillic like atenolol & nadolol are excreted by kidney unganged&thus given once daily). S/Es(See text):1.Cardiovascular. 2.CNS 3.Respiratory 4.Metabolic 5.Endocrinal Contraindications:1.Active asthma&COPD. 2.PVD 3.Bradycardias&AV block.4.IDDM . 5.2.Vasodllators:act as arterial& venodilators causing↑ coronary blood flow&↓pre& afterload flow;thus ↑ myocardial O2 supply&↓myocardial O2 demand through reduction of LV wall tension. They include: *Nitrates:They induce vasodilitation by stimulating the endothelium-derived relaxing factor (EDRF). devide into: -Trinitrates e.g Glyceril trinitrate(GTN) -Dinitrates e.g Isosorbide dinitrate.-Mononitrates e.g Isosorbide mononitrate.The mononitrate has better therapeutic advantages than oral dinitrate as it doesn't undergo 1stpass hepatic metabolism like oral dinitrate&thus has a more predictable&longer action&thus given once daily. S/E:1.Headache is common&can be troublesome. 2.Hypotension&even sycope.3.Tolerance:loss of effect with continuous use®imen should therefore ensure nitrate-free period thus better given not more than 2-3times daily. *Ca+2 Channel blockers:Act by blocking Ca-channels in the heart&blood vessels&their predominent action&S/Es are class-specific: I.Dihydropyridines(Nifedipine-short acting& amlodipine-long acting).They→arterial vasodilation thus↓LV afterload,thus↓myocardial O2 demand but the short acting →reflex tachycardia that offset their antianginal action hence better given combined with β-blocker. S/Es:1. Headache,facial flushing&ankle odema. 2.myocardial depression&hence are not given in left ventricular systolic dysfunction&HF except amlodipine. II.Nondihydropyridines(verapamil&diltiazem). They depress myocardium&slow down conducting tissue thus ↓ myocardial contraction&heart rate both at rest& exercise thus ↓myocardial O2 demand. S/Es:1.CVS.2.constipation (Verapamil) 3.Hepatic dysfunction.C/I:1.LV systolic dysfunction&HF. 2.Bradycardias&AV-block . *K+ Channel Activators:(Nicorandil).They have nitrate-like coronary vasodilator effect.They not only improve symptoms like nitrates but↓adverse outcomes like cardiac death, MI & unstable angina in pts. with stable angina. 5.3 If inhibitors: A new therapeutic class, HYPERLINK "http://en.wikipedia.org/wiki/Ivabradine" \o "Ivabradine" ivabradine provides pure heart rate reduction leading to major anti-ischemic and antianginal efficacy. Ivabradine acts on the If ion current, which is highly expressed in the sinoatrial nod&it is a mixed Na+–K+ inward current. S/Es 1.visual like luminous phenomena ( sensations of enhanced brightness in the visual field) but are mild, transient&reversible,blurred vision 2.cardiac like extreme bradycardia, first-degree AV block, ventricular extrasystoles, 5.4. fatty acid oxidation inhibitors e.g mildronate is a clinically used anti-ischemic drug for the treatment of angina and myocardial infarction. Mildronate; through carnitine biosynthesis inhibition ,it shifts the myocardial energy metabolism from fatty acid oxidation in ischemic tissues( highly oxygen-consuming process)to more oxygen sparing glucose oxidation under ischemic. condition Also the drug acts via stimulation of the nitric oxide production in the vascular endothelium as corononary vasodilator. 5.5 Antiplatelet agents:Aspirine given to any pt.with CAD for life unless C/I as it ↓risk of MI&premature coronary death. 5.6. Statins are the most frequently used lipid/cholesterol modifiers but a statin decreases adverse outcomes like MI,unstable angina or cardiac death in patients with stable angina with no matter the level of LDL-C, as statin has a vasculoprotective effect through stabilizing atheromatous plaques. Side effects of statins include muscle pain but though rare severe muscle damage may occur, increased risk of diabetes mellitus& abnormalities in liver enzyme . II.Revascularization: PCI:by which a critically stenosed coronary artery by balloon dilatation then a stent is deployed to prevent restenosis. &CABG:If PCI technically not feasible,failing or complicated,venous grafts used to bridge or bypassing the stenotic lesions . Patients Unstable angina pose a medical emergency as UA constitutes with AMI, the acute coronary syndrome(ACS)& treated almost similarly ;1.admission to CCU for monitoring 2.full antithrombotic measures (Antiplatelet agents Aspirine&clopedogril inaddition to heparin.to prevent thrombus formation& progression). 3.Full β-blockade with metoprolol &if no control,Ca+2 channel blocker is added.4.IV Nitrates for ongoing or recurrent pain to responding to 3 doses of sublingual GTN. 3.PCI.&/or CABG Nearly all pts.with UA considered for revascularization. Prognosis of angina:depends on functional state of LV& Extent of CAD.A. Poor prognostic factors in stable angina: 1.LV dysfunction(↓EF)& HF.2.Significant ST/T in resting ECG or at low workload in Ex.test.3.Poorly or non responsive angina despite adequate medical Rx.4.Extensive coronary artery disease (LMS or three-vessel disease). Poor prognostic factors in UA: UA is More worse than stable angina. Risk of MI is higher&sudden death occurs in 10-15% of case& it's poor prognostic factors:. 1.Clinical parameters:*Recurrent pains at rest.*LV dysfunction&HF. *Early postinfarct angina(within2/52). 2.Lab.parameters:*MarkedST/Tchanges or raised troponins > 0.2mcg/l.
-