١
Fifth stage
Medicine
Lec-
د
.
ﺧﺎﻟد ﻧﺎﻓﻊ
8/10/2015
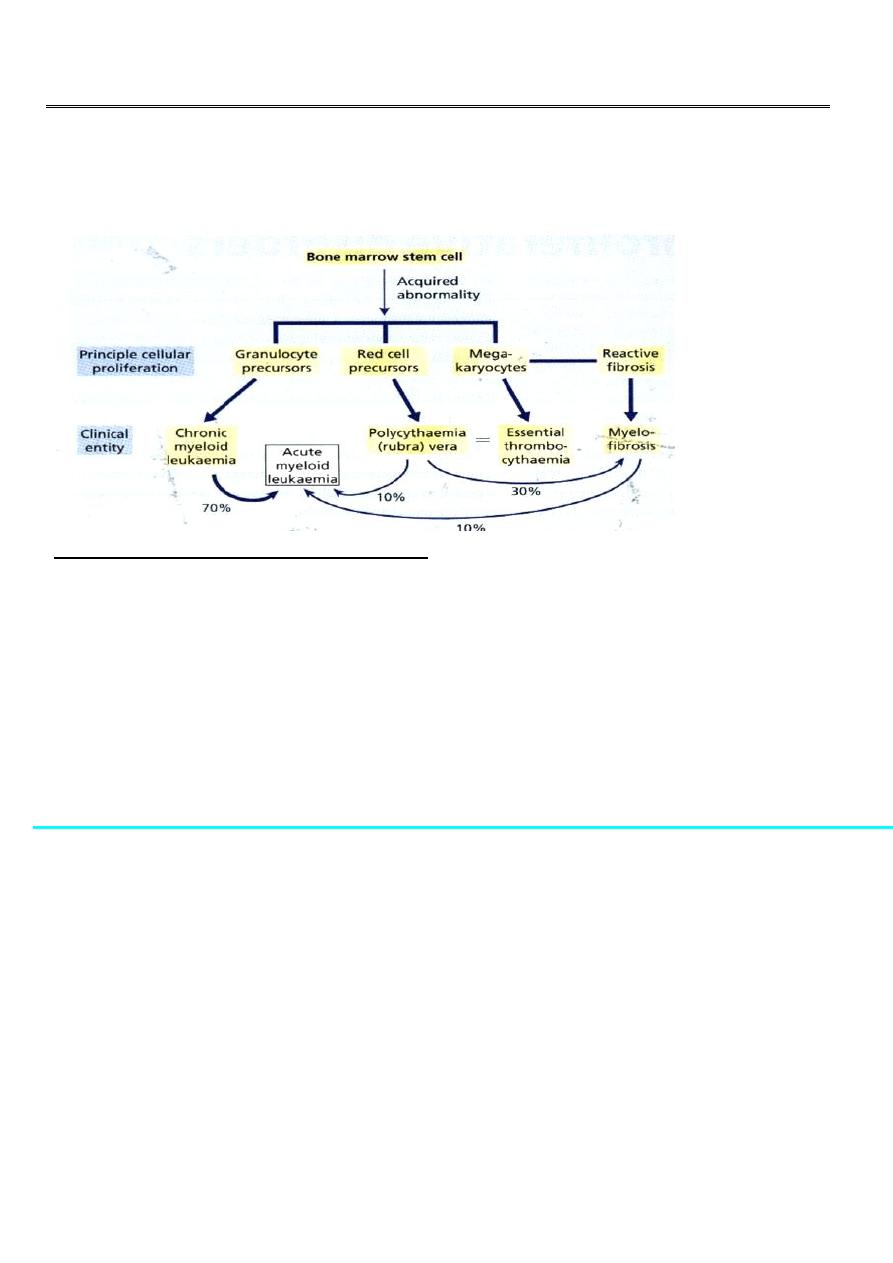
Myeloproliferative disorders
Clonal evolution
Clonal evolution & stepwise progression to fibrosis, marrow failure or acute blast phase
Chronic myelogenous leukemia(CML)
• Description : CML is a myeloproliferative disorder characterized by increased
proliferation of granulocyte, and evidence of myeloproliferation involve liver and
spleen.
• CML accounts for 20% of all leukemia affec ng pts. between 30-80 years, with a peak
incidence at 55years.
CML. Historical vs. Modern Perspective
Parameter
Historical
Modern
• Course
Fatal
Indolent
• Prognosis
Poor
Excellent
• 7-yr survival
40%
90%
• Frontline Rx
• Second line Rx
Allogeneic SCT;
IFN-
?
Imatinib
New Tyrosine Kinase Inhibitors;
allo SCT
٢
ETIOLOGY:
– Not clear
– Little evidence of genetic factors linked to the disease
– Increased incidence
• Survivors of the atomic disasters at Nagasaki & Hiroshima
• Post radiation therapy
• CML is an acquired abnormality that involves the stem cells and is characterized by
specific chromosomal abnormality (translocation) between the long arm of
chromosome 22 and 9 which is called philadelphia chromosome (ph). Approximately
95 % of pa ents with CML have this abnormality.
• The chromosome has been found in all myeloid and lymphoid cell indicating the
involvement of the pluripotential stem cell.
Leukaemogenesis:
• protein BCR–ABL, which has increased in tyrosine kinase activity
• BCR-ABL protein transform hematopoietic cells so that their growth and survival
become independent of cytokines
• It protects hematopoietic cells from programmed cell death (apoptosis)
Phases of chronic myeloid leukemia
Chronic phase Accelerated phase Blast crisis
5 years
CLINICAL FEATURES :
25% asymptoma c at me of diagnosis
Chronic Phase :
Splenomegaly in 90% of pa ents . In about 10% the enlargement is massive. Afric on rub
may be heard in cases of splenic infarction.
Hepatomegaly 50%. Lymhadenopathy is unusual.
Symptoms related to hypermetabolism
Weight loss Anorexia
Lassitude Night sweats
Stable disease, no cancer out side bone marrow or spleen,
Median dura on 3 years, range several months to > 20 years
٣
Clinical Features - cont…
• Features of anaemia
-Pallor, dyspnoea, tachycardia
• Abnormal platelet function
– Bruising, epistaxis, menorrhagia
• Hyperleukocytosis
– thrombosis
– Increased purine breakdown : gout
– Visual disturbances
– Priapism
Phases- Cont.
– Accelerated phase :
• Median dura on is 3.5 – 5 yrs before evolving to more aggressive phases
• Clinical features
– Increasing splenomegaly refractory to chemotherapy
– Increasing chemotherapy requirement
• Lab features
– Blasts>15% in blood
– Blast & promyelocyte > 30% in blood
– Basophil 20% in blood
– Thrombocytopenia
– Cytogenetic: clonal evolution
– Blastic phase :
– Resembles acute leukaemia
– Diagnosis requires > 20% blast in marrow
– 2/3 transform to myeloid blas c phase and 1/3 to lymphoid blas c phase
– Survival : 9 mos vs 3 mos (lym vs myeloid)
• LABORATORY FINDINGS
a. Complete Blood Count(CBC):
N/N anaemia.
WBC count range 9.5-600 x 10
9
/L(mean 220x 10
9
/L) .
Platelet count 162-2000 x10
9
/L(mean 445x10
9
/L)
In the blood film all stages of maturation are present from myeloblast to neutrophil,
myeloblast less than 10%.
Basophilia &oesonophils may increase as the disease progresses.

٤
• b. Bone marrow;
Hypercellular (reduced fat spaces)
Myeloid:erythroid ratio – 10:1 to 30:1 (N : 2:1)
Myelocyte predominant , blasts less 10%
Megakaryocytes increased & dysplastic
Increase re culin fibrosis in 30-40%.
*For chromosomal analysis(Ph chromosome),
*RNA analysis for BCR-ABL.
• c. other laboratory findings :
Serum B12 and transcobalamin increased
Serum uric acid increased
Lactate dehydrogenase increased
CML - principles of treatment
:
•
Relieve symptoms of hyperleukocytosis, splenomegaly and thrombocytosis
– Hydration
– Chemotherapy (busulphan, Hydoxyurea)
• Control and prolong chronic phase
– alpha interferon+chemotherapy
– imatinib mesylate
– chemotherapy (hydroxyurea)
• Eradicate malignant clone (curative)
– allogeneic transplantation
– alpha interferon ?
– ima nib mesylate/STI 571 ?(Tyrosine kinase inhibitor)
• Chemotherapy ;
Hydroxycarbamide(Hydroxyurea) 1000-1500 mg/day orally the effects should be
monitered every 2-6 weeks.
Fewer side effect
Acts by inhibiting the enzyme ribonucleotide reductase
Haematological remissions obtain in 80%.
However disease progression not altered and persistence of Ph chromosome
containing clone
٥
• 1-HSCT
Intensive chemotherapy and total body irradiation (TBI) are followed by the transplantation
of HLA matched allogeneic stem cell.
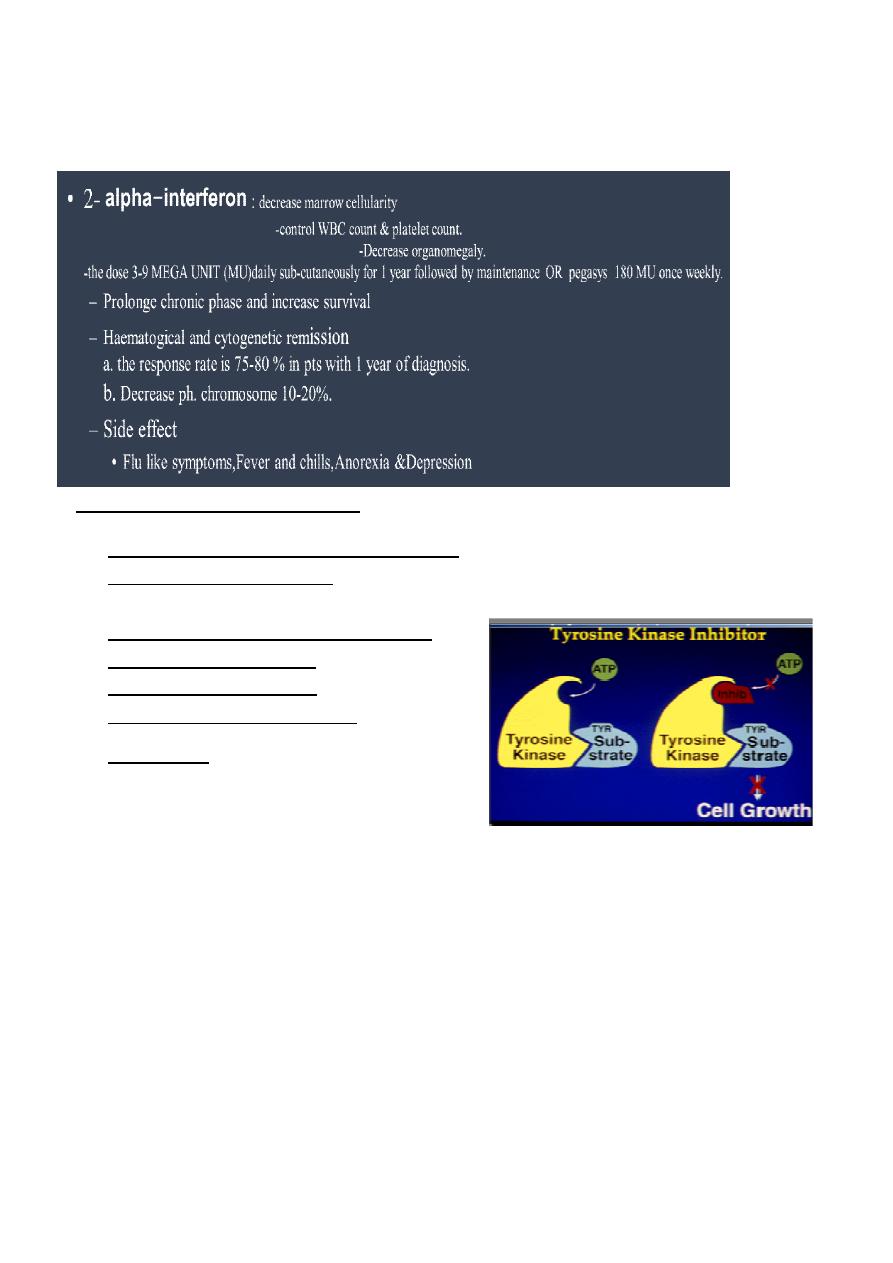
3-.Tyrosine kinase activity inhibitor
• 1- IMATINIB mesylate/ (STI 571, GLIVEC)
400 mg single dose orally.
Acts specifically by blocking the binding site for ATP in the Abl kinase.
2-NILOTINIB (TASIGNA)
3-DASATINIB (SPRYCEL)
50-70 mg once or twice daily
• 4-Ponatinib
Variants of CML :
• *Ph-negative CML BCR-ABL negative :
• About 5% of pa ents with haematologically acceptable CML lack the Ph
chromosome.
• older patient mostly male with lower platelet count and higher absolute monocyte
count.
• Respond poorly to treatment.
• Median survival less than 1 year.
• *Juvenile CML :
• Rare.
• Affec ng children <12 year-old.
• C/F – anaemia, or lymphadenopathy with hepatosplenomegaly, skin rashes.
• Lab findings – leucocytosis with variable numbers of blast in the peripheral blood.
• Marrow is hypercellular but lacks chromosomal abnormalities.
• Responds poorly to standard cytotoxic drugs.
