ISHIK UNIVERSITYFACULTY OF DENTISTRY
Oral PharmacologyFall 2016
Dr. Esra Tariq Bayrakdar
Pharmacist (M.Sc.)Routes of Drug Administration
oral (P.O)sublingual (SL)
rectal
application to other epithelial surfaces (e.g. skin, cornea, vagina and nasal mucosa)
inhalation
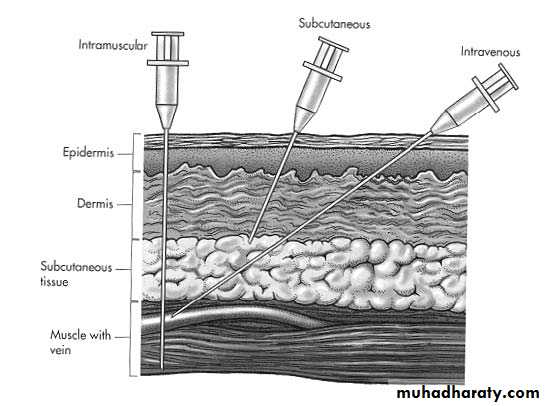
injection
subcutaneous (SC)
intramuscular (IM)
intravenous (IV)
intrathecal
intravitreal
Routes of Drug Administration
Local Routes
The dosage forms applied locally to theskin are powders, paste, lotions, ointments,creams, plasters and jellies. They are used for their antiseptic, antipruritic, analgesic,local anaesthetic and other related effects.
The absorption of drug through the skin is proportional to the surface area covered and to their lipid solubility.
The dermis layer is freely permeable to many fluids. Inflammatory and other related conditions which increase the cutaneous blood flow also enhance absorption of drugs
The topical application is also used on the mucous membranes i.e. nose, throat, eye,ear, bronchi, rectum, urethra, vagina andrectum.
In case of mouth and pharynx, the drug is used in the form of throat paints, lozenges,gargles or mouth washes.
The bronchial mucosa and lungs are treated with inhalations, aerosols (in the formof fine powder with the help of nebulizer) salbutamol (ASTHALIN) inhaler.
ADMINISTRATION BY INHALATION
Inhalation is the route used for volatile and gaseous anaesthetics ,the lung serving as the route of both administration and elimination. The rapid exchange resulting from the large surface area and blood flow makes it possible to achieve rapid adjustments of plasma concentration.Particles larger than 20 micron and the particles impact in the mouth and throat. Smaller than 0.5 micron and they aren't retained
Drugs used for their effects on the lung are also given by inhalation, usually as an aerosol.
Glucocorticoids (beclometasone dipropionate) and bronchodilators ( salbutamol are given in this way to achieve high local concentrations in the lung while minimising systemic side effects.
However, drugs given by inhalation in this way are usually partly absorbed into the circulation, and systemic side effects (tremor following salbutamol) can occur.
Chemical modification of a drug may minimise such absorption. For example, ipratropium, a muscarinic receptor antagonist
Systemic Routes- Oral Route
Enteric coated tablets: The drugs which are destroyed by the gastric juices in the stomach, arecoated with keratin, shellac and cellulose acid phosphate. These substances are not dissolved by the acid juice of the stomach, but are dissolved in the intestinal juice (alkaline) only.
Preventing gastric irritation and alteration of the drug in the stomach.
To get the desired concentration of the drug in intestine.
To delay the absorption of the drug
Time Release/Sustained Release Capsules: It is a useful solid dosage form of drug,where the particles of the drug dissolve at different time intervals.
Reduction in the frequency of admin-istration of drug
Maintenance of therapeutic effect forlonger time.
To some extent decreased incidence of undesired effects.
Appropriate for drugs with short half lives (less than 4 hours)
Sublingual Administration (SL)
The highly lipid soluble and non-irritating drugs. (nitroglycerine) in the form of tablets or pellet is placed under the tongue, where they rapidly dissolve and are absorbed quickly in the general circulation.The advantages of this routes are:
Rapid onset of action.
The degradation and metabolism of the drugs in the stomach and liver is avoided
Parenteral Route
The advantages of parenteral routes are:Rapid action of drug.
Can be employed in unconscious/uncooperative patients.
Drugs, which are modified by a limentary juices and liver can be given by this route.
Self medication is difficult.
Chances of local injury at the site of injection
Drugs, which are not absorbed in small intestine or irritate the stomach can be administered by this route.
Disadvantages are:
Less safe, more expensive.
Inconvenient (painful) for the patient
Route for administration -Time until effect-
intravenous 30-60 secondsintraosseous 30-60 seconds
endotracheal 2-3 minutes
inhalation 2-3 minutes
sublingual 3-5 minutes
intramuscular 10-20 minutes
subcutaneous 15-30 minutes
rectal 5-30 minutes
ingestion 30-90 minutes
transdermal (topical) variable (minutes to hours)
Routes of Drug AdministrationDosage Forms
Solid Dosage forms : includes capsules,granules, effervescent granules, powders,tablets, insufflations, suppositories.Semisolid/liquid dosage form : elixirs, emulsions, gels, drops, solutions, syrups, creams, enema.
Inhalation forms : aerosols,sprays.
Internal and external uses
FACTORS AFFECTING GASTROINTESTINAL ABSORPTION
gastrointestinal motility
blood flowparticle size and formulation
physicochemical factors.
PRODRUGS
Prodrugs are inactive precursors that are metabolised to active metabolites in the body.Levodopa
Valaciclovir
Zidovudine
Drug excretion: Acidification of urine decreases the effectivity of basic drugs
Changes in electrolyte and fluid balance, hypocalaemia produced by diuretics and corticosteroids increases digitals toxicity and antagonizes the antiarrhythmic activity of quinidine, phenytoin.GIT DrugsDrugs used in Constipation and Diarrhoea
Classification of Purgatives:Mild Purgatives:
• Bulk producing drugs They absorb water and increase bulk in the intestine (safest purgatives) ; Methyl cellulose 1 g (1-4 times/day)
• Stool softeners: Liquid paraffin (15 mL /day)
• Mild saline purgatives : 10 g /day
• Osmotic : Magnesium sulfate (5-15 g/day)
• Irritant Purgatives: Senna glycosides (1-2 tab /day), castor oil (15-25 mL/day), Bisacodyl (5-15mg/day)
Causes:
Environment
Emotional tension
Diseases
Adverse effects of drugs
The use of these drugs differ according to :
AgeGender
Diet and life style
Pregnancy
Drugs
Drugs used in Constipation and DiarrhoeaTherapeutic Uses
Constipation due to diminished intestinal toneDrug induced constipation
Food or drug poisining
Pateints with severe neuromuscular disease
Pateints with hepatic encephalopathy
To reduce the absorption of ammonia and toxins from colon
To clean bowel before surgery, colonoscopy, and radiological procedures
Non-Spesific Agents
Oral rehydration therapy : Glucose and electrolyte solutions is effective in majority of patients with watery dairrhoeas.
Antimotility agents: reduce peristalsis and increase tone of the rectalsphincter.
Antispasmodic drugs (atropine, oxyphenonium) are used to decrease cramps, abdominal pain anddiarrhoea associated with spasms of the intestine.
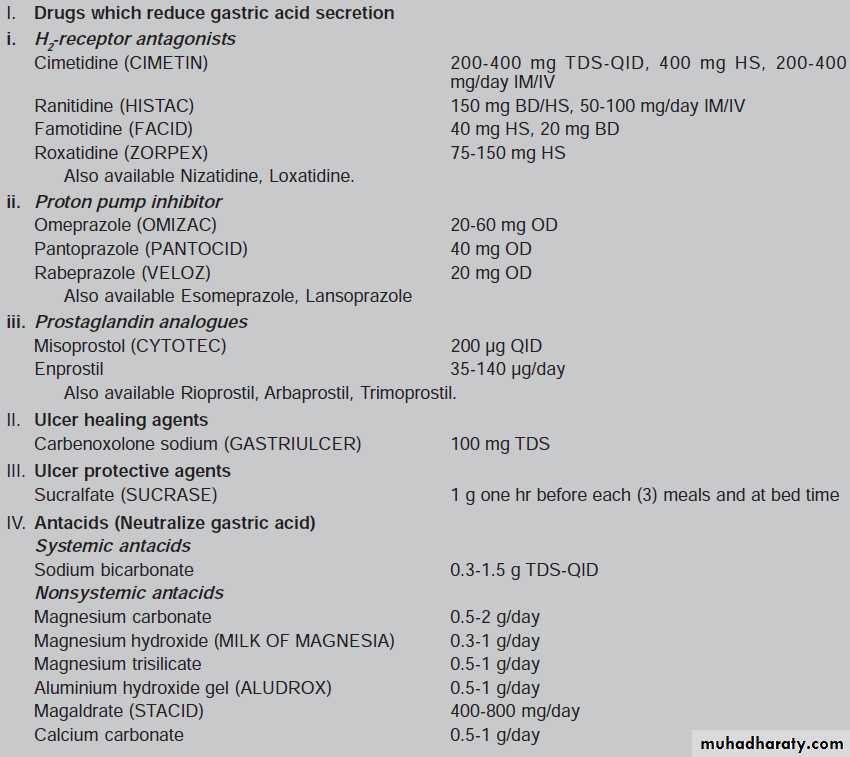
Drugs Used in Peptic Ulcer
AntiacidsAnticholinergic agents
Histamine H2 Antagonists
PPI
Drugs providing Protection to Mucosa
Anti-Helicobacter Pylori Drugs
ANTIACIDS
Non-absorbable antiacids : Al-salts (Al2(OH)3, Al-phosphate..)Magnesium salts: Mg-hydroxide, Mg-trisilicate..)
Calcium carbonate
Absorbabale antiacid : Sodium bicarbonate
They neutralize gastric hydrochloric acid and prevent activation of pepsin.
They mainly provide symptomatic relief by reducing acid irritation of ulcers and to a lessextent promote healing.ANTIACID DRUG INTERACTION
Sodium reduces antihypertensive effect of drugs
Aluminium decreases the basorption of digoxin, tetracycline, isoniazid, iron salts and prednisolone.Magnesium retards the absorption of tetracycline, digoxin and dicoumarol.
Anticholinergic Agents
M1 and M2 receptor blockers like probanthine, oxyphenium and dicyclomine.Selective M1 receptor blockers like pirenzepine and telenzepine . They have minimum effect on heart, intestine, and urinary bladder. So the adverse effects such as dryness of mouth, blurred vision and headache are less common.
They act by reducing gastric acid secretion. They also inhibit gastric motility which may be helpful in ulcer healing.
Drug interaction: Non-selective anticholinergic drugs increase the absorption of digoxin, prednisolone, and phenytoin by delaying intestinal transit time.
Histamine H2 Antagonists
Cimetidine (Low potency, short duration of action),Ranitidine(5 to 8 times more potent than cimetidine),
Famotidine (On a weight basis 20 times more potent than cimetidine and 7.5 times more potent than ranitidine in inhibiting basal and pentagastrin stimulated gastric acid secretion. It is a competitive-noncompetitive inhibitor of H2 receptors. It has a longer duration of action, It is more useful in ZE syndrome and prophylaxis of aspiration pneumonia),
Roxatidine (a potency greater than cimetidine and in the same range as Ranitidine).
They block histamine mediated acid secretion from gastric parietal cells and also reduce gastrin and cholinergic acid secretions.They reduce both quantity and concentration of acid but have no effect on mucous secretion and gastric motility.
Histamine H2 Antagonists
Uses:
Gastric and duodenal ulcers.
Gastric erosions with or without bleeding.
Reflux oesophagitis.
Stress ulcers.
Zollinger-Ellison Syndrome.
Chronic gastritis.
Histamine H2 Antagonists
Drug interactions:Cimetidine potentiates the toxicity of propranolol, diazepam, theophylline, imipramine, phenytoin, warfarin, and phenobarbitone by inhibiting hepatic microsomal oxidase enzyme.
However, in therapeutic doses newer H2 antagonists have minimal hepatic enzyme inhibiting activity.
They retard absorption ketoconazole due to reduction in gastric acidity.
Proton Pump Inhibitors
Inhibit the proton pump by inhibiting the H⁺K ⁺ -ATP ase of the gastric parietal cells.They are prodrug which are absorbed from small intestine. Their hepatic metabolite is responsible for acid reduction.
Proton Pump Inhibitors
Used to treat gastric and duodenal ulcers, not responding to H2 antagonists because its long-term use is likely to be hazardous.It is drug of choice for Zollinger-Ellison syndrome.
Reflux oesophagitis.
NSAID induced ulcerations and bleeding.
Drugs Used In Peptic Ulcer
Drugs Providing Protection To Mucosa
Sucralfate : It is an aluminium containing salt of sucrose octasulfate.It becomes highly viscous gel in acid pH of the stomach. The gel binds to proteins in the ulcer crater and forms a protective coating. Due to this, it checks the diffusion of H⁺ ions and pepsin.
It protects paietal cells by increaing endogenous PG synthesis.
It attenuates peptic activity by binding with pepsin.
It also binds with bile salts and provides an ideal physical barrier .Thus it protects ulcer site from offensive intraluminal acid.
PROSTAGLANDIN ANALOGUES
PGE2 and PGI2 are the main prostaglandins synthesized by gastric mucosa. They decrease acid secretion and improve mucosal defense mechanism by:Stimulation of synthesis and release of mucus.
Enhance bicarbonate production.
Enhancement of tight junctions of cell membrane architecture.
Inhibit gastrin production.
Stimulation of a number of cellular transport processes.
Stimulation of DNA content in damaged gastric mucosa by a process termed as cytoprotection
Misoprostol, Enprostil
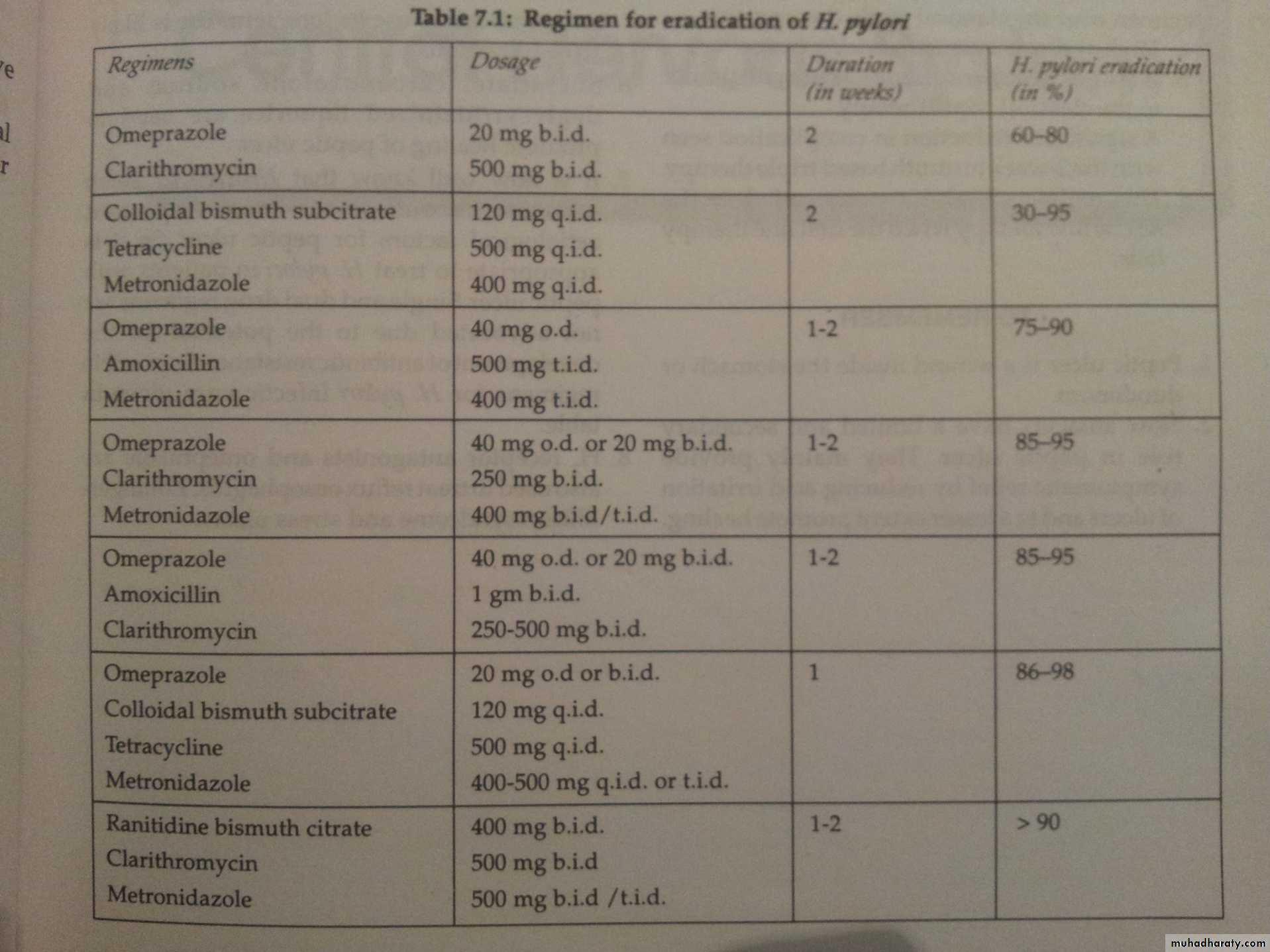
Regimen for Eradication of H. Pylori
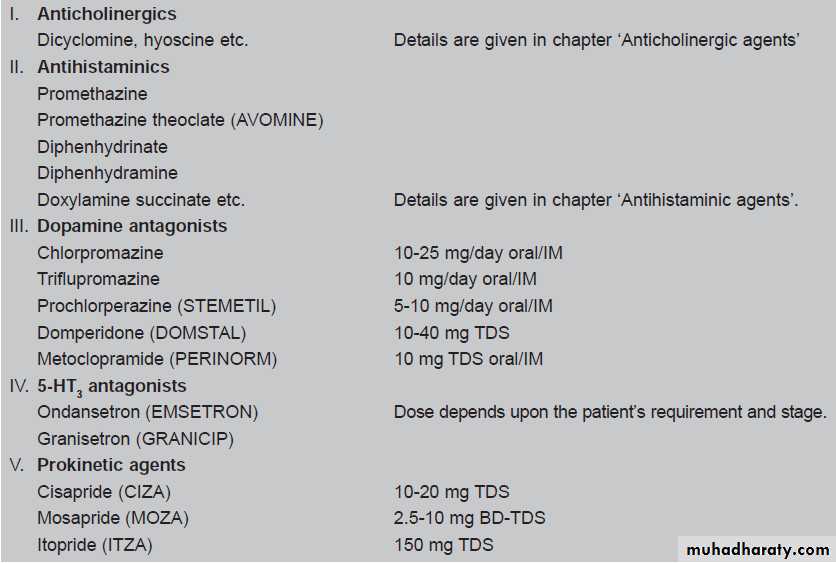
Emetics and Antiemetic Agents
Emetics: Vomiting or emesis occurs due to stimulation of vomiting/emetic centre in medulla oblongata.The chemoreceptor trigger zone (CTZ) and nucleus tractus solitarius (NTS) are relays for the afferent impulses arising from GIT, throat and other viscera.
There are different drugs e.g. morphine, digitalis glycosides, apomorphine etc. which stimulate the CTZ. While certain agents e.g. chlorpromazine and certain antihistaminics depress it.
The drugs that produce or evoke vomiting are known as emetics. The most common compounds used are apomorphine and ipecacuanha
The emetics are used mainly in poisoning when gastric lavage facilities are not available. But in certain poisoning e.g. kerosene poisoning, corrosive acid or alkali poisoning, emetics are contraindicated.
They are also not advisable in unconscious patients as they may aspirate vomitus.
The emetics are used mainly in poisoning when gastric lavage facilities are not available.
In certain poisoning e.g. kerosene poisoning, corrosive acid or alkali poisoning, emetics are contraindicated. They are also not advisable in unconscious patients as they may aspirate vomitus.
Antiemetics
These are the drugs which are used to prevent vomiting.Dopamine causes antiemetic action by blocking dopamine (D2) receptors and it also increases gastric motility
Metochlopromide is a centrally acting dopamine antagonist and acts on CTZ by blocking D2 receptors thereby preventing emesis