pg.
1
Fifth stage
Dermatology
Lec-3
.د
منار
3/11/2016
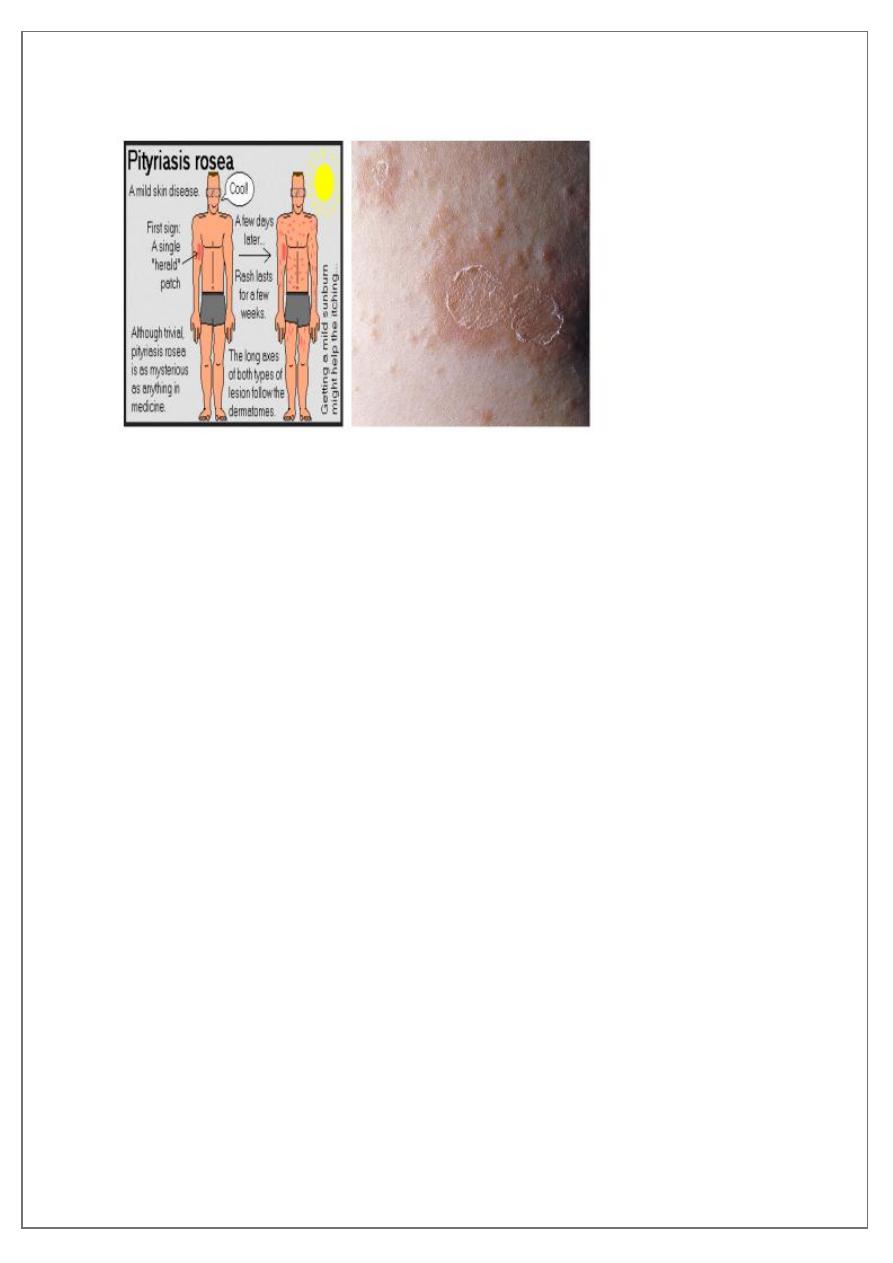
PITYRIASIS ROSEA
Other Papulosequamous Disease:
• Pityriasis Rosea
• Lichen Planus
Pityriasis rosea (PR)
is a common, benign, usually asymptomatic, distinctive, self-limiting skin eruption
There is some evidence that human herpesvirus 6 (HHV-6) and 7 (HHV-7) may be
involved.
More than 75% of cases occur between 10 and 35 years of age with an age range
of 4 months to 78 years.
Recurrence rate is about 2%.
The incidence is higher during winter time.
Upper respiratory tract infection occurs before the eruption in about 70% of cases.
CLINICAL MANIFESTATIONS
• Typically, the herald patch, a single 2- to 10-cm round-to-oval lesion, abruptly appears
in 17% of patients. May occur anywhere, but is most frequently located on the trunk
or proximal extremities.
• Within a few days to several weeks the disease enters the eruptive phase and reach its
maximum in 1 to 2 weeks.
• Lesions are typically limited to the trunk (lower trunk) and proximal extremities, but
any area could be affected.
• Individual lesions are salmon pink in whites and hyperpigmented in blacks.
• Typically 1- to 2-cm oval plaques appear, a fine, wrinkled, tissue-like scale remains
attached within the border of the plaque, giving the characteristic ring of scale, called
collarette scale.
• The long axis of the oval plaques is oriented along skin lines.
• Numerous lesions on the back, oriented along skin lines, give the appearance of
“Christmas-tree distribution.”
• Remits spontaneously in 6 weeks
• 50% itching
pg.
2
Differential diagnosis
1. Secondary syphilis
2. Guttate psoriasis
3. Viral exanthems
4. Tinea corporis
5. Nummular eczema
6. Drug eruptions
Management of PR
• The disease is benign and self-limited and can resolve spontaneously within 6 weeks
• Oral erythromycin 250 mg 4 times daily for 2 weeks.
• Topical steroids
• Oral antihistamines may be used as needed for itching.
• Uvb phototherapy five times per week for 2 weeks.
• Oral acyclovir (800 mg five times daily for 1 week)??
pg.
3
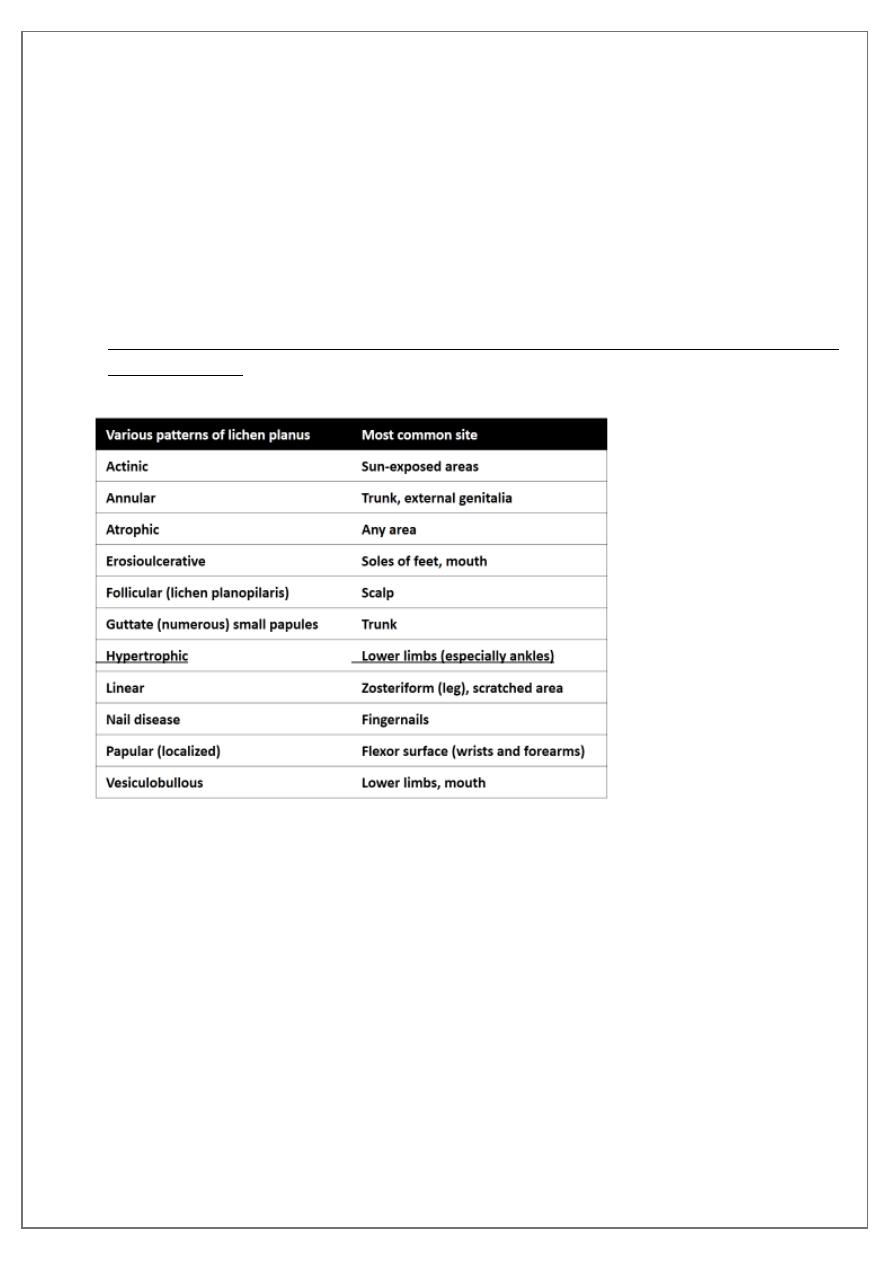
Lichen planus (LP)
• Lichen planus (LP) is an inflammatory cutaneous , mucous membrane , hair and nail
diseas
• Etiology : immunological mechanism mediate its development
• The mean age of onset is 40 years
• it is rare in children younger than 5 years.
• The main eruption clears within 1 year in about 70% of patients, but 50% of eruptions
recur.
• Approximately 10% of patients have a positive family history.
• Cutaneous and oral LP may be associated with hepatitis C virus (HCV)-related, chronic,
active hepatitis.
Eruptions from drugs (e.g., gold, chloroquine, methyldopa, penicillamine)
chemical exposure (film processing), bacterial infections (secondary syphilis)
post–bone marrow transplants (graft-versus-host reaction) that have a similar
appearance are referred to as lichenoid.
pg.
4
Description
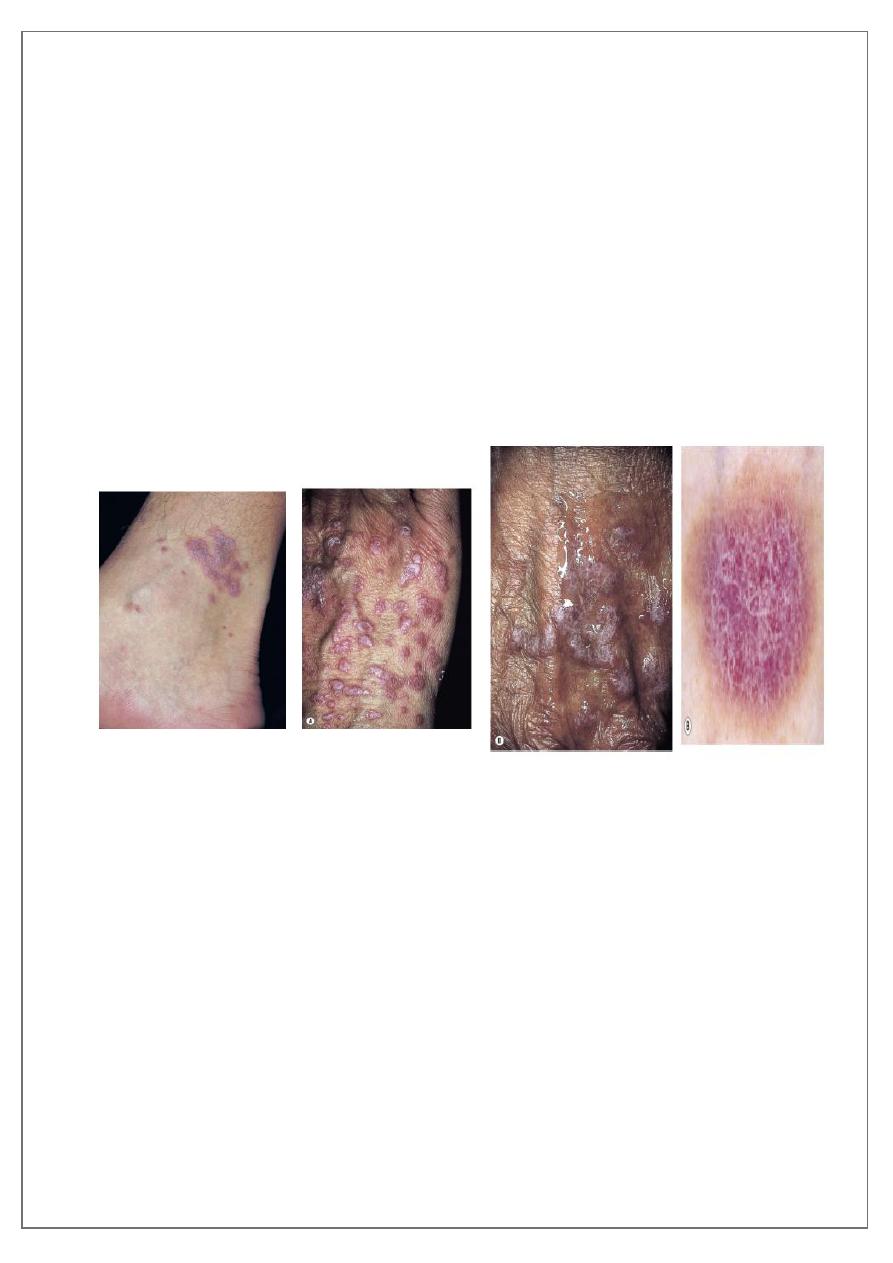
• The five (ps) rule of lichen planus:
Pruritic, plane (flat-topped), polygonal, purple papules.
• Close inspection of the surface shows a lacy, reticular pattern of crisscrossed, whitish
lines (wickham’s striae) that can be accentuated by a drop of immersion oil.
• Symmetrical
• Papules aggregate into different patterns, they may also koebnerize.
• Itching is variable; 20% of patients with LP do not itch.
• Itch does not necessarily correlate with disease severity.
• Flexural distribution on wrists and forearms, the legs immediately above the ankles
and the lumbar region.
• Many patients have persistent post inflammatory hyperpigmentation many years after
the rash has cleared.
Treatment
For Cutaneous Lichen Planus
• Topical steroids
• Intralesional steroids
• Systemic steroids
• Acitretin
• Azathioprine
• Cyclosporine
• Antihistamines
• Tacrolimus ointment: Ulcerative lichen planus of the sole may respond to topical
tacrolimus 0.1% ointment.
• Light therapy
• PUVA (psoralen + UVA light) and broadband and narrow-band UVB therapy.
pg.
5
THERAPY FOR MUCOUS MEMBRANE LICHEN PLANUS
• The course of oral and vaginal lichen planus can extend for years.
• Consider a biopsy to establish the diagnosis.
• Most patients are asymptomatic (non-erosive type) and do not need treatment.
• Tacrolimus ointment and pimecrolimus cream.
• Corticosteroids (topical, systemic and intralesional)
• Dapsone
• Hydroxychloroquine
• Azathioprine
• Mycophenolate mofetil
Hydroxychloroquine
Azathioprine
Mycophenolate mofetil
