HISTORY TAKING & PHYSICAL EXAMINATION
Dr.Bilal Jamal KamalMB ChB
FIBMS
MRCP(UK)
Part2
HITORY TAKING
Tips for effective conversations:1. Choose a quiet & private space
2. Speak clearly & audibly
3. Ask open questions to start with
4. Don’t interrupt your patient
5. Try & appear unharried
6. Use silence to encourage explanations
7. Do not use jargon or emotive words
8.Clarify & summarize what you understand
9. Acknowledge emotions
10. Seek ideas, concerns & expectations
History taking usually takes 15 min, but for students, it may take upto 30 min.
Arrange seating in a non-confrontational way.
Look for non-verbal cues e.g. distress & mood.
Active listening:
Hear your patients story, ask open questions to start with, e.g. What has brought you along to see me today?
Active listening means encouraging the patient to talk by looking interested, making encouraging comments.
Closed questions, e.g. Have you had cough today? Seek specific information as part of a systemic enquiry. They invite yes or no answers. Both types of questions have their places.
• Demographic data: name, age, gender, address, marital status, date of addmission
• Chief complain• History of present illness;
• Characteristic of pain (SOCRATES)
• Site, somatic is well localized, visceral is diffuse
• Onset, speed of onset & any associated circumstances
• Character, sharp, dull, burning, stabbing
• Radiation
Associated symptoms
Timing (duration, course, pattern)Exacerbating & relieving factors
Severity
Past history:
Have you had any serious illness that brought you to see doctor?
Have you had any operations?Have you attended any hospital clinics?
Drug history
Ask about prescribed drugs, OTC, herbal, traditional.Ask about compliance,adherance,dosage,regimen,duration.
DRUG ALLERGIES
Family history:Diseases run in the family??
Social history:
Helps you to understand the context of the patients life & possible relevant factors.Lifestyle: exercise, diet, travel history, sexual history, smooking, alcohol, non-prescribed drugs
Occupation
House
Leisure activities
Systemic enquiry
Cardiovascular system: chest pain,breathlessness
Palpitation,leg swelling
Respiratory: cough,dyspnea,sputum,blood in sputum, chest pain
GIT: mouth, difficulty in swelling,nausea,vomitin
Blood in vomiting,heartburn,bowel motion
Genitourinary: Dysurea,blood in urine,
Frequency, libido
CNS: headache,fits,weakness,visual diturbance
Memory change
Endocrine: heat & cold intolerance, sweating
Musculoskeletal: joint pain, stiffness, mobility
Women: menstrual history
PHYSICAL EXAMINATION
Privacy is essential when you examine a patientTalk quietly but ensure good communication
The room should be warm and well lit
Subtle abnormalities of complexion such as mild jaundice are easier to detect in natural light
cannot lie flat.
Seek permission and sensitively, but adequately, expose the areas of the body to be examined; cover the rest of the patient with a blanket or sheet to ensure that he or she does not become cold. Avoid unnecessary exposure and embarrassment
The sequence of examination is:
Inspection
Palpation
Percussion
Auscultation
Introduce yourself to the patient (Handshake & first impressions)
History taking from the patientDifferential diagnosis
Examine the patient(General & systemic)Confirm or refute your diagnosis
First Impressions:The physical examination starts as soon as you see the patient. Assess patients’ general demeanour and external appearance, and watch how they rise from their chair and walk into the room.
The handshake:
Introduce yourself and shake hands. This may provide diagnostic clues . Greet your patient in a friendly but professional manner. Note if his right hand works; in patients with a right hemiparesis you may need to shake his left hand. Avoid too firm a grip, particularly in patients with arthritis.
Facial expression and general demeanour:
Actively recognise the features of anxiety, fear, anger.
Clothing:
Clothing gives clues about personality, state of mind and social circumstances. Young people wearing dirty clothes may have problems with alcohol or drug addiction.
Complexion:
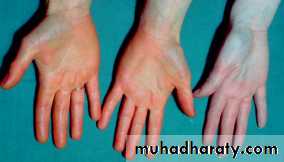
Facial colour depends on oxyhaemoglobin, reduced haemoglobin, melanin and carotene. Unusual skin colours are due to abnormal pigments.Haemoglobin: Untanned European skin is pink due to the red pigment oxyhaemoglobin in the superficial capillary–venous plexuses. A pale complexion may be misleading(because it can be caused by vasoconstriction during faint or fear) but can suggest anaemia. The pallor of anaemia is best seen in the mucous membranes of the conjunctivae, lips and tongue and in the nail beds. Facial plethora is caused by raised haemoglobin concentration with elevated haematocrit (polycythaemia).
Cyanosis:
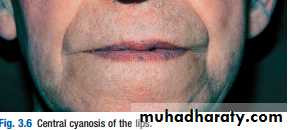
Cyanosis is a blue discoloration of the skin and mucous membranes that occurs when the absolute concentration of deoxygenated haemoglobin is increased.Central cyanosis
Central cyanosis of the lips.This is seen at the lips and tongue . It corresponds to an arterial oxygen saturation (SpO2) of <90% and usually indicates underlying cardiac or pulmonary ot due to increment of deoxygenated Hb > 5 g/dl
Peripheral cyanosis
This occurs in the hands, feet or ears, usually when they are cold. In healthy people it occurs in cold conditions when prolonged peripheral capillary flow allows greater oxygen extraction and hence increased levels of deoxyhaemoglobin. In combination with central cyanosis, it is most often seen with poor peripheral circulation due to shock, heart failure.Melanin
Causes of abnormal melanin productionSkin colour is greatly influenced by the deposition of melanin.Vitiligo:
This chronic condition produces bilateral symmetrical depigmentation, commonly of the face, neck and extensor aspects of the limbs, resulting in irregular pale patches of skin.
Albinism:
This is an inherited disorder in which patients have little or no melanin in their skin or hair
Overproduction of melanin
This can be due to excess of the pituitary hormone, adrenocorticotrophic hormone, as in adrenal insufficiency
Pregnancy and oral contraceptives
These may produce chloasma (blotchy pigmentation of the face)Carotene: Hypercarotenaemia occurs in people who eat large amounts of raw carrots and tomatoes, and in hypothyroidism. A yellowish discoloration is seen on the face, palms and soles, but not the sclerae, and this distinguishes it from jaundice
Bilirubin: Jaundice is detectable when serum bilirubin concentration is elevated and the sclerae, mucous membranes and skin become yellow.
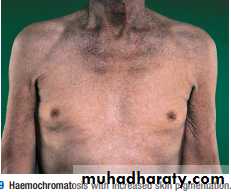
Iron: Haemochromatosis increases skin pigmentation due to iron deposition and increased melanin production
m
The Hands:
Examination sequence:■ Inspect the dorsal and then palmar aspects of both hands.
■ Note changes in the:
■ skin
■ nails
■ soft tissues (evidence of muscle wasting)
■ tendons
■joints.
■ Feel the temperature.
Abnormal findings :
DeformityColour
Temperature
Skin
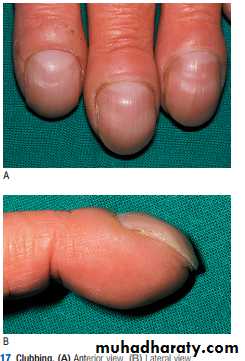
Finger clubbing Clubbing: is painless soft-tissue swelling of the terminal phalanges. The enlargement increases convexity of the nail with loss of nail fold angle.
Cause of finger clubbing:
Lung diseses: abscess, bronchiectasis, fibrosis
Heart diseases: cyanotic congenital heart disease, Infective endocarditis
GIT: Cirrhosis , IBD, Celiac disease
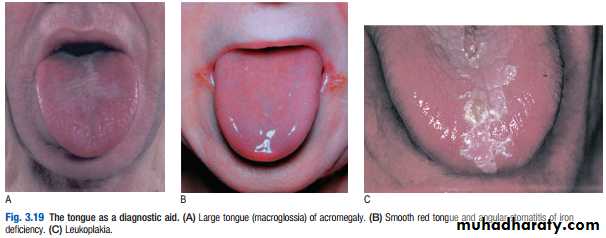
THE TONGUE:
Examination sequence :Ask the patient to put out his tongue.
Look at the size, shape, movements, colour and surface
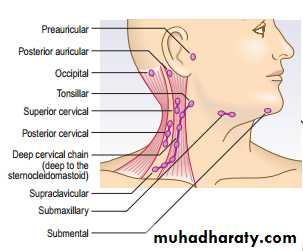
THE LYMPH NODES :
Lymph nodes may be palpable in normal people, especially in the submandibular, axilla and groin regions . Distinguish between normal and pathological nodes. Pathological lymphadenopathy may be local or generalised, and is of diagnostic and prognostic significance in the staging of lymphoproliferative and other malignancies.