
Kirkuk University/ College of medicine-Immunology & Microbiology department
Third year class-Medical microbiology/ Prof. Dr. Yahya G.Salman Oct.2009to2016
Lecture number one
– An introduction to medical microbiology.
Microbiology:
is a branch of biology, that concern to study the smallness, which includes the study
of microscopic living forms such as viruses, bacteria, also macroscopic forms like fungal molds
¶sitic forms.
Historical view:-
An
environment that surround human, always abound him with minute living organisms& he has
always carried them in countless billions around within his person. However, microbiology is little
more than a century old, having its origin in the work of Louis Pasteur in 1850, though that great
breakthrough was preceded by many centuries of speculation & investigation.
1- Kircher 1671 reported the presence of little worm in the blood of patients with plague& claimed
that they were responsible for the disease.
2- Antony Leeuwenhoek in 1674 was able to observe minute living creatures in rain, sea & pond
water, & in various other fluids.
3- Agostino Bassi in 1835 had described the fungus that later named Botrytis bassiana, which
caused muscardine a disease of silkworms &he had suggested that this disease was transmitted by
contact or by infection of food.
4- In 1839, Schoenleins continue the work of Agostino, so he was able to describe the fungus that
causes the human disease of favus.
5- In 1838 after the improvement of microscope design which made possible the beginning of
systematic description of microorganisms, Ehrenberg introduced such terms as bacterium, vibrio,
spirillium & spirochetes when he work on infusoria( small creatures found in infusion).
6-In 1840 Henle pointed out that a microorganism causing a disease should be present in every case
& should produce a similar disease in animals into which it was inoculated-criteria which was later
expanded into Koch postulates.
7- Rayer & Davaine in 1850 reported the presences of rod-shaped organisms in the blood of animals
that had died of anthrax. Then Davaine separately showed that this disease could be transmitted by
inoculation of blood containing such rods but not of blood from which they were absent.
8 Louis Pasteur, the French chemist, who study alcoholic fermentation, which terminate the dispute
about spontaneous generation( some animals could develop entirely from non living materials such
as Putrefying meat was believed to give rise to maggots & mud of Nile to snakes, where as corn &
linen cloth stored in a jar were product mice. Pasteur, attribute lactic & butyric acid fermentation to
bacteria.
9- Joseph Lister, a professor of surgery in Glasgow, gain benefit from the work of Pasteur on
fermentation, when he observe suppuration of wounds, so he concluded that if microorganisms
caused fermentation, they might also cause suppuration of wounds,& that in their absence wounds
might heal cleanly & without risk to the patients lives. So he introduced his antiseptic technique in
1867.
10-Great deals in medical microbiology were return to German scientist Robert Koch, who began to
follow up the work of Davaine on anthrax & he postulates the followings:
A- All microorganism must be present in every case of disease.
B- It can be isolated in pure culture.
C-Inoculation of the pure culture into animals produces the similar disease.
D- The same species of microorganism must be recovered from the diseases animals.
The methods that developed by Pasteur & Koch lead to first golden age of microbiology(1875 to
1910),when many bacterial diseases & organisms responsible for them were defined.
In the first half of the 2oth century, scientist studied the structure, physiology & genetic of microbes
in detail, which answer the link between microbial properties & disease. By the end of 20
th
century
more advances were obtained from molecular biology& genetic. The discovery of penicillin by
Fleming in 1929 & of sulfonamide by Domagk in 1935 opened the way to great developments in
chemotherapy. These gradually extended from bacterial diseases to fungal, parasite & finally viral
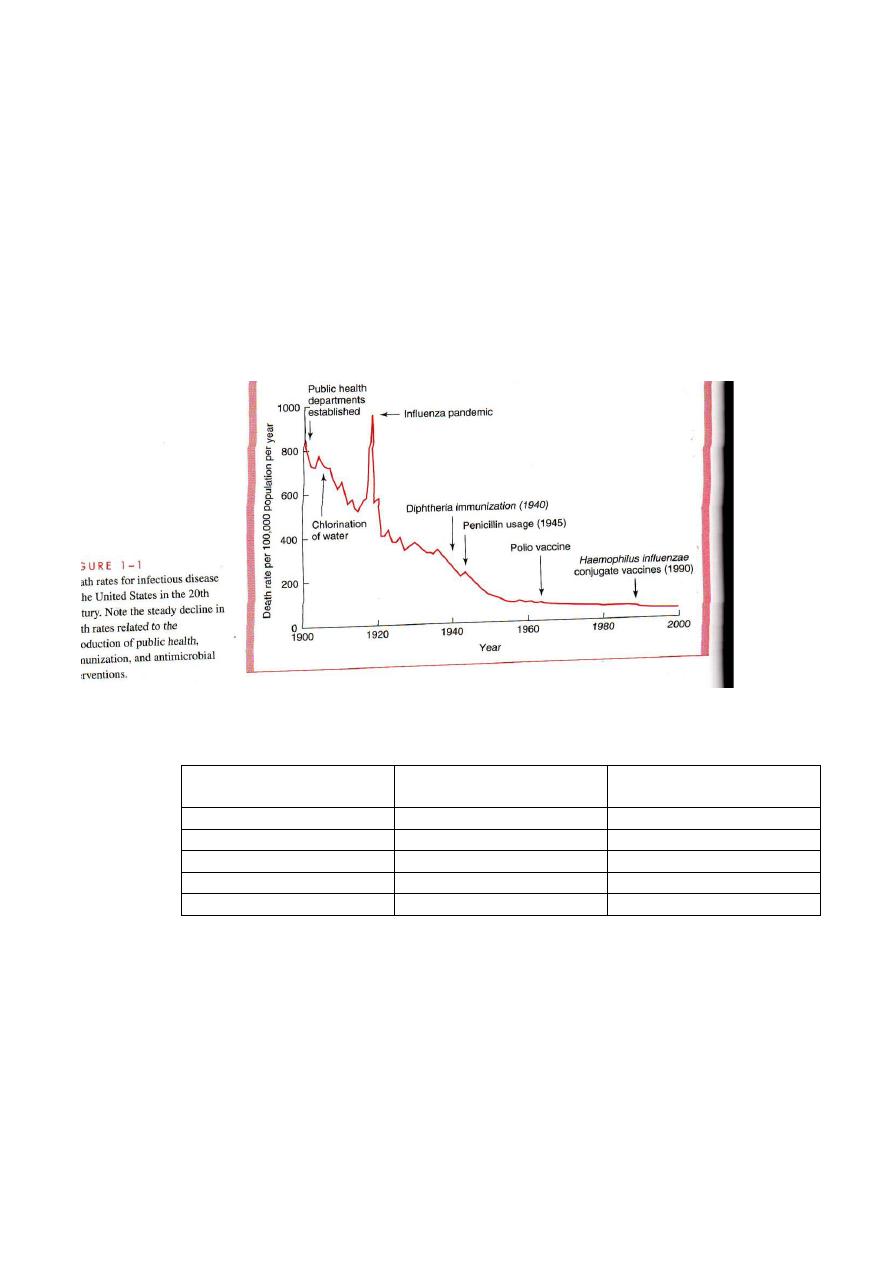
infection,& great deals in vaccinations(Diphtheria immunization in 1940,Penicillin usage in
1945,Polio vaccine in 1964 & Haemophilus influenza conjugate vaccine(1990),Treatment human
cases of anthrax by Ciprofloxacin in 2003.
Organism
s:-
Human infectious agents included five major groups of organisms:
Type of cells
Pathogenic
Microorganisms
Kingdom
Eukaryotic
Helminths
Animal
Eukaryotic
None
Plant
Eukaryotic
Protozoa&Fungi
Protista
Prokaryotic
Bacteria
Prokaryote
None cellular
Prions& Viruses
The distinction among them is based on 3 criteria:
1- Structure 2-Method of replication
3- Nature of nucleic acid.
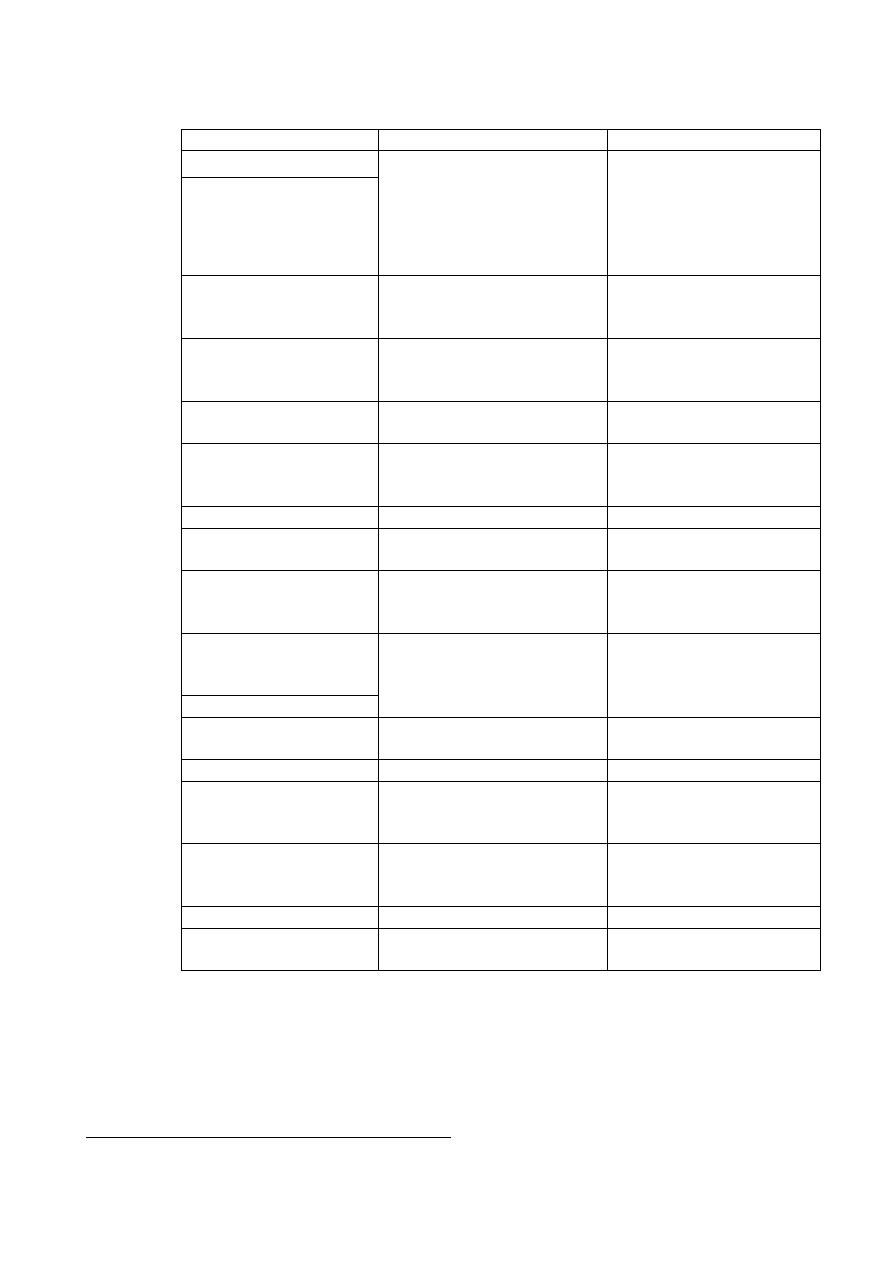
Characteristics of prokaryotic &eukaryotic cells
Eukaryotic human cells
Prokaryotic bacterial cells
Characteristic
Yes
No
DNA within nuclear
membrane
Yes
No
Mitotic division
Yes
NO
DNA associated with
histones
More than one
One
Chromosome number
Yes
No
Membrane bound
organells such as
mitochondria &lysosomes
80S
70S
Size of ribosome
No
Yes
Cell wall containing
peptidoglygan
**
*
Cytoplasmic membrane
Usually present
Absent except in
Mycoplasms
Sterols
*Contains enzymes of respiration; active secretion of enzymes; site of phospholipids& DNA
synthesis.
** Semi permeable not possessing function of prokaryotic membrane
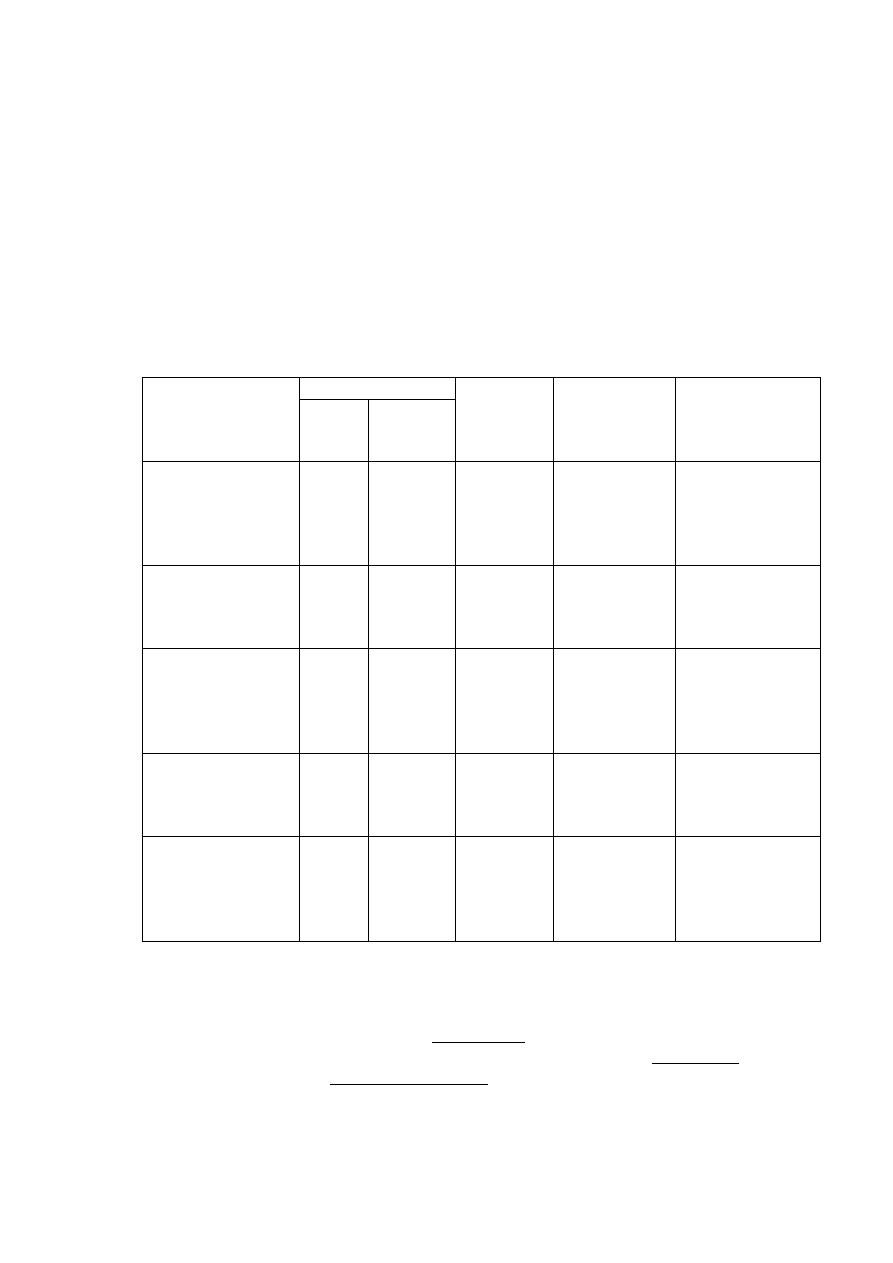
Comparison of medically important organisms
Protozoa &
helminthes
Fungi
Bacteria
Viruses
Characteristic
Yes
yes
yes
no
Cells
15 to25 for
trophozoites
3 to 10 for
yeasts
1 to 5
0.02 to 0.2
Approximately
sizeµm
Both DNA
&RNA
Both DNA
&RNA
Both DNA
&RNA
Either DNA
or RNA
Nucleic acid
Eukaryotic
Eukaryotic
prokaryotic
None
Type of nucleus
80S
80S
70S
Absent
Ribosomes
present
present
absent
Absent
mitochondria
Flexible
membrane
Rigid wall
containing
chitin
Rigid wall
containing
pepitydoglycan
*
Protein
capsid
&lipoprotein
envelope
Nature of outer
surface
Most
None
Some
None
Motility
Binary fission
Binary fission
or budding
Binary fission
No binary
fission
Method of
replication
.* Peptidoglycan is a polymer of amino acids & sugars as its unique the structural component.
.Q) What are the similarity & differences among bacteria, fungi & protozoa?
t
Bacterial structures:
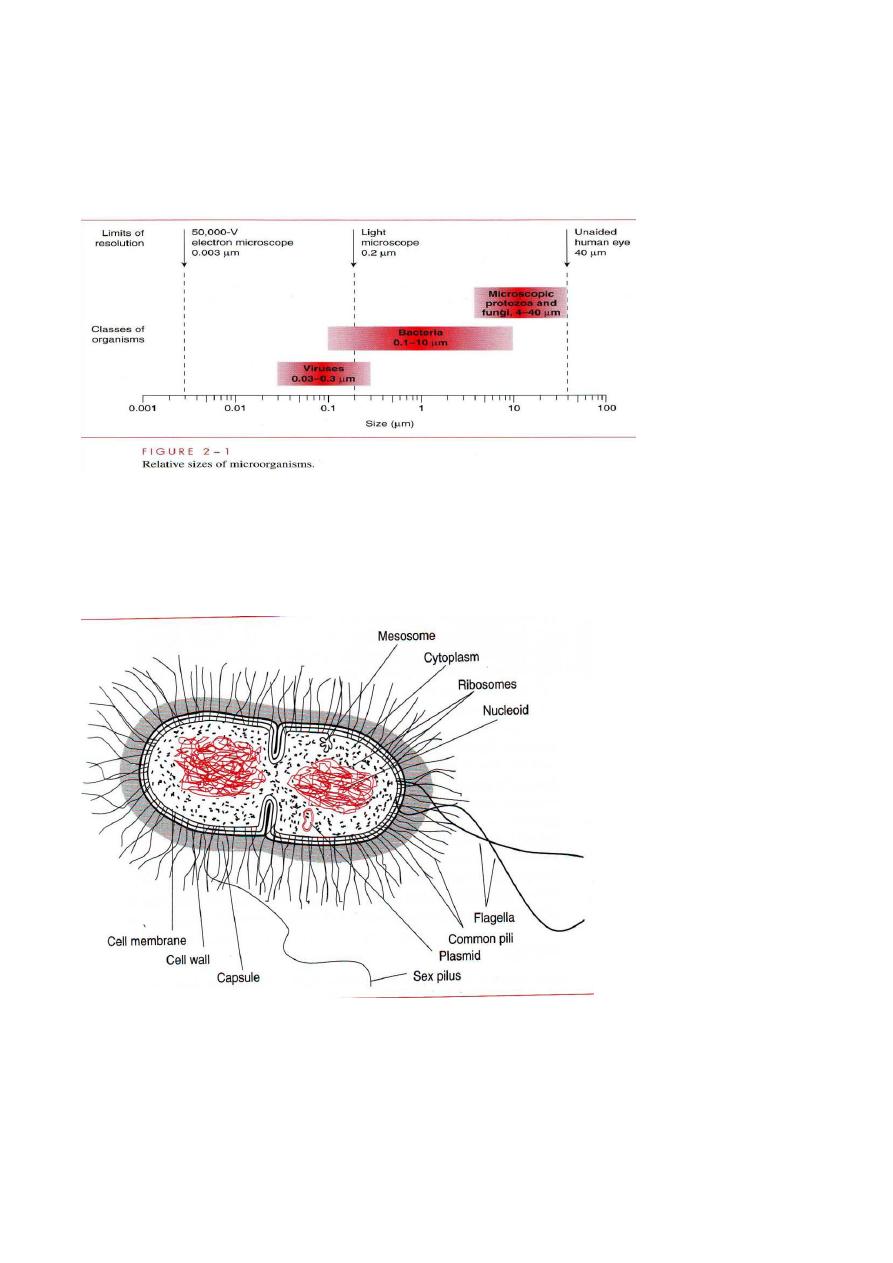
Are the smallest living cells, & some to have minimum possible size for an dependently reproducing
organism. Individual bacterial species that colonized humans range from 0.1 to 10 µm in their largest
dimension.
Bacteria are variable in shape pleomorphic, that determined by the rigid cell wall. & according to the
shape bacteria can be classified into 3 basic groups:
1-Cocci(diploid like Diplococcus species, Micrococcus ,tetrad like sarcina &Hafnia, grape like
Cluster like Staphylococci, some cocci may appears as Chain so it called streptococci (short chain,
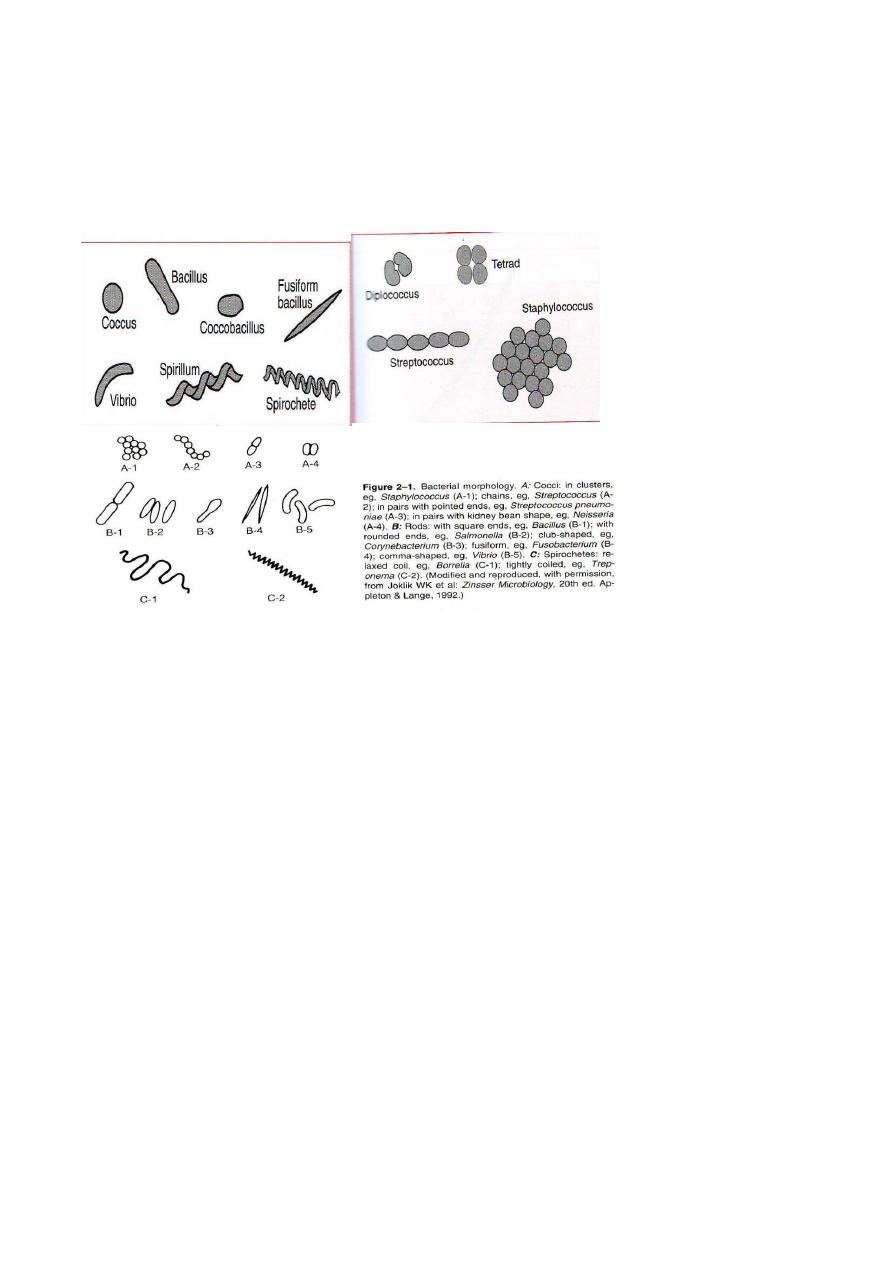
long chain) This arrangements are determined by the orientation & degree of attachment of bacteria
at the time of cell division..
2- Bacilli or rods, they appears as rounded ends like Salmonella,or club shaped like
Corynebacterium, or fusiform Like Fusibacterium & coma shaped like Vibrio.
3- Spirochetes,They appears as relaxed coil like Borrella, moderately coiled like Leptosporia &
tightly coiled like Treponema.
Cell wall:-
The main structural component of this wall is
1- Mucopeptide or peptidoglycan, which consists of chains of alternating molecules of
N-asetoglucosamine &N-asetylmuramic acid cross linked by peptide chains; it is
responsible for rigidity of cell wall. The thickness of peptidoglycan is very
important & according to it bacterial staining by gram staining divided bacteria into
gram positive (G+ve) bacteria with thick layer of peptidoglycan & gram negative
(G-ve)which posses delicate layer of it.
2- G-ve cell wall have a complex outer layer of lipopolysacharide(LPS),lipoprotein &phospholipids
,this layer can lay between outer layer & cytoplasmic membrane in G-ve bacteria so it is peri-
plasmic( the site, in some species, of enzyme like ß-lactams, that degrade penicillin & other ß-lactam
drugs like cephalosporin which inhibit its synthesis. Also this layer can called endotoxin(it is
responsible for features of disease such as fever & shock caused by these organisms), because it is
an integral part of cell wall, in contrast to exotoxins, which are freely released from bacteria.
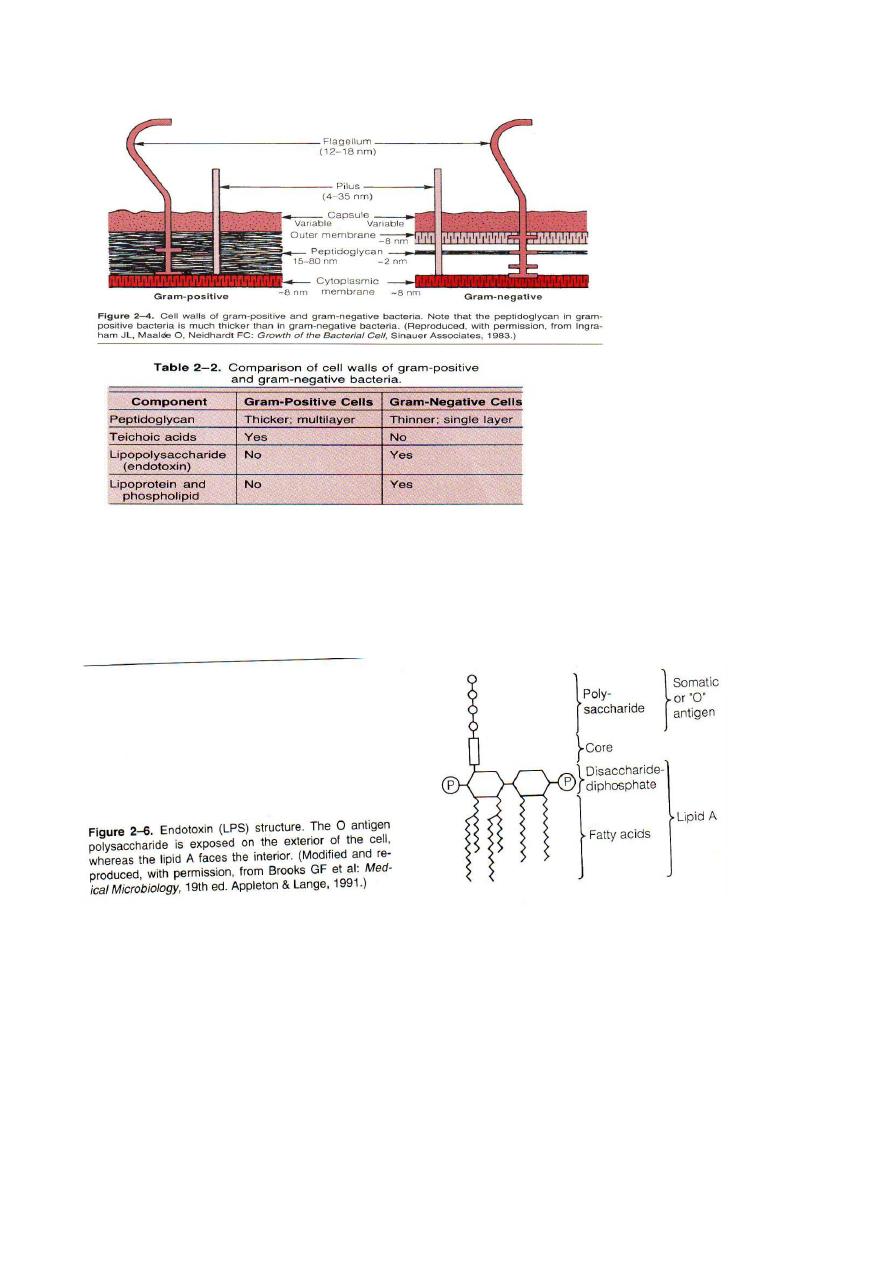
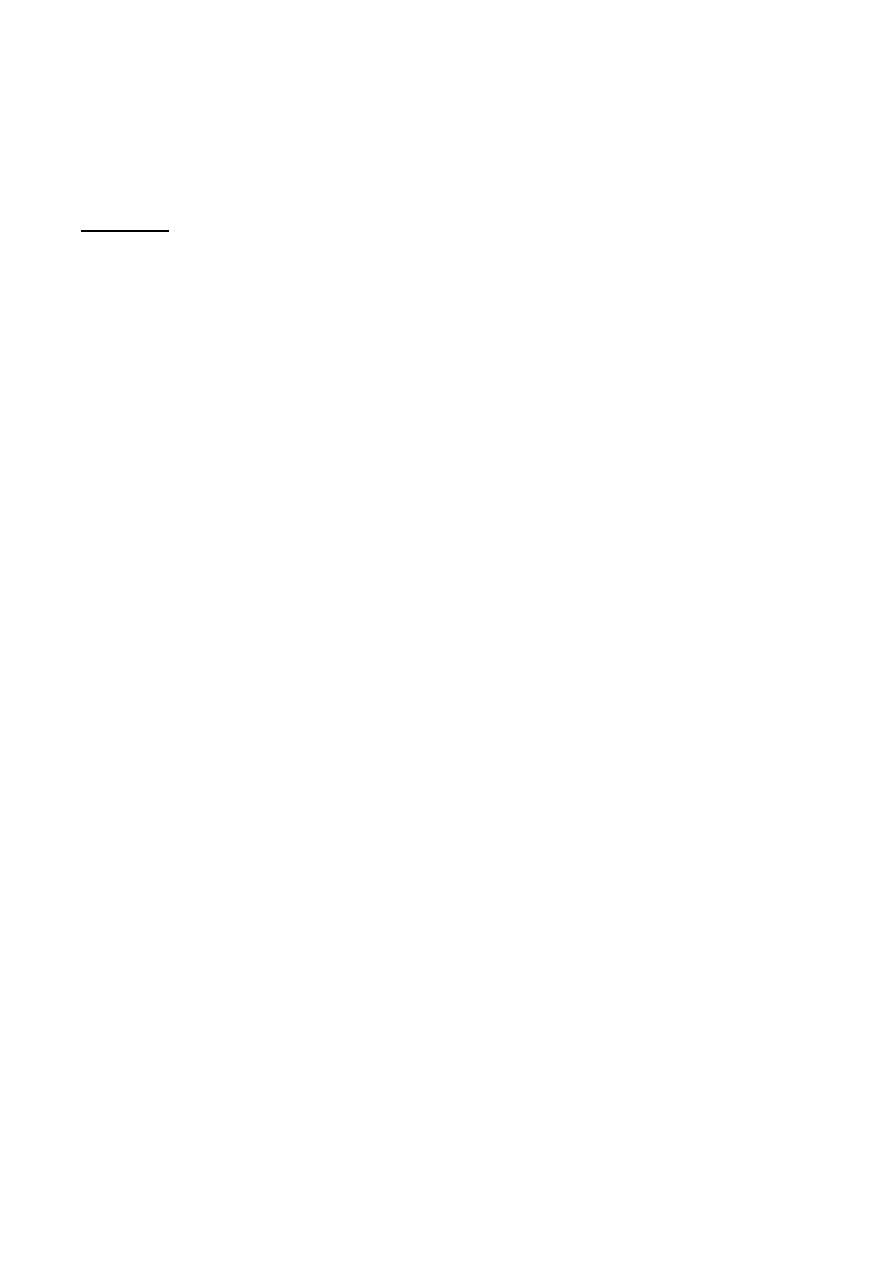
LPS is composed of the following three distinct units:
A- Lipid A, which consists of phospholipids, (responsible for toxic effects).
B- A core of polysaccharide of 5 sugars linked through keto-deoxyoculonate to
lipid A.
C-An outer polysaccharide consisting of up to 25repeating units of 3-5 sugars . This outer polymer is
important in laboratory identification of G-ve serologically (Widal test) like salmonella infection
(PUO, food poisoning ).
3- Some G+ve bacteria also have layer of techoic acid outside of peptidoglycan, whereas G-ve do
not. This layer is consisting of polymers of glycerol phosphate or ribitol phosphate .Techoic acids are
antigenic & induce antibodies that are species specific.-
Other functions of bacteria cell wall
:
1-In G-ve bacteria, it contains endotoxin, a lipopolysaccharide.
2-Its polysaccharide &proteins are antigens that are useful in laboratory identification.
3-The porin proteins play role in regulating the passage of small hydrophilic molecules into the cell,
as well as entrance of antimicrobial drugs.
** The cell wall of Mycobacterium tuberculosis can inhibit to be gram stained, the bacteria so called
acid fast bacilli (AFB), since they resist to decolorizing with acid alcohol after being stained with
strong carbol fuchsin. This property is related to the high concentration of mycolic acid in its cell
wall.
Cytoplasmic membrane:-
This layer lies inside peptidoglycan layer, this phospholipids bi-layer similar microscopically &
chemically to eukaryotic cells, but eukaryotic membranes contain sterols whereas prokaryotic
generally do not.
-
Functions:
1-Active transport of molecules into the cell .
2-It can produce energy by oxidative phosphorylation.
3-Synthesis of precursors of the cell wall .
4-Enzymes &toxin secretions.
In some the cytoplasmic membrane forms highly convoluted invaginated membranous organelle
called mesosome, which appear to be the sites of specialized metabolic activity & are prominent cell
wall synthesis &during sporulation.
By the aid of electron microscope cytoplasm of bacterium has 2 distinct areas:
An amorphous matrix that contains:
1- Ribosomes, which have had 70S size with 50S & 30S, which share in protein synthesis & it
constitute the basis of the selective action of several antibiotics that inhibit bacterial protein synthesis
but do not in human protein synthesis.
2- Granules
: they are certain types, serves as site of storage areas of nutrients
Like volutin, that serve as high energy store in the form of polymerized metaphosphate, it appears as
metachromatic granules. Since it stains red with methylene blue dye instead of blue as one would
expect .
3- Nucleoid
:- is an area in cytoplasm via which DS- DNA is located, that consist of single circular
chromosome, that has a molecular weight 200000000 &contains about 2000 genes. There is no
nuclear membrane &no mitotic apparatus.
4-Plasmids
:- are extra-chromosomal DS-DNA circular molecules That are capable of replicating
independently of the bacterial chromosome . Both Plasmids &DNA are anchored to membrane
attachment site that control their replication. Plasmids are two types:
A- Transmissible plasmids: they are usually present in 1-3 copies/cell,(MW=40 to 100 million),they
are responsible for synthesis of sex pilus & for the enzymes required for transfer.
B-Non-transmissible plasmid: Usually present in many ( 10 to 60 copies/cell),they are small(MW 3-
20 million), they do not contain transfer genes.
Functions of genes on plasmids:-
*- Antibiotic résistance, which is mediated by a variety of enzymes .
*- Resistance to heavy metals such as mercury (the active component of some antiseptics,such as
merthiolate & mercurochrome) & silver which is mediated by areductase enzyme
.*Resistance to ultra violate, which is mediated by DNA repair synthesis.
*- pili ( Fimbriae)Which mediate ther adherence of bacteria to epithelail cells and.
*-Exotoxins, including several endotoxins .
Other encoded products of plasmids are:-
A- Bactreiocins, Toxins or enzymes that are produced by certain bacteria & are lethal
for other bacteria.
B- Nitrogen fixation enzymes in Rhizobium in the root nodules of legumes.
C- Tumor caused by Agrobacterium in plants.
D- Several antibiotics produced by Streptomyces & degradative enzymes produced by Pseudomonas
& are capable of cleaning up environmental hazard such as oil spills & toxic chemical waste sites.
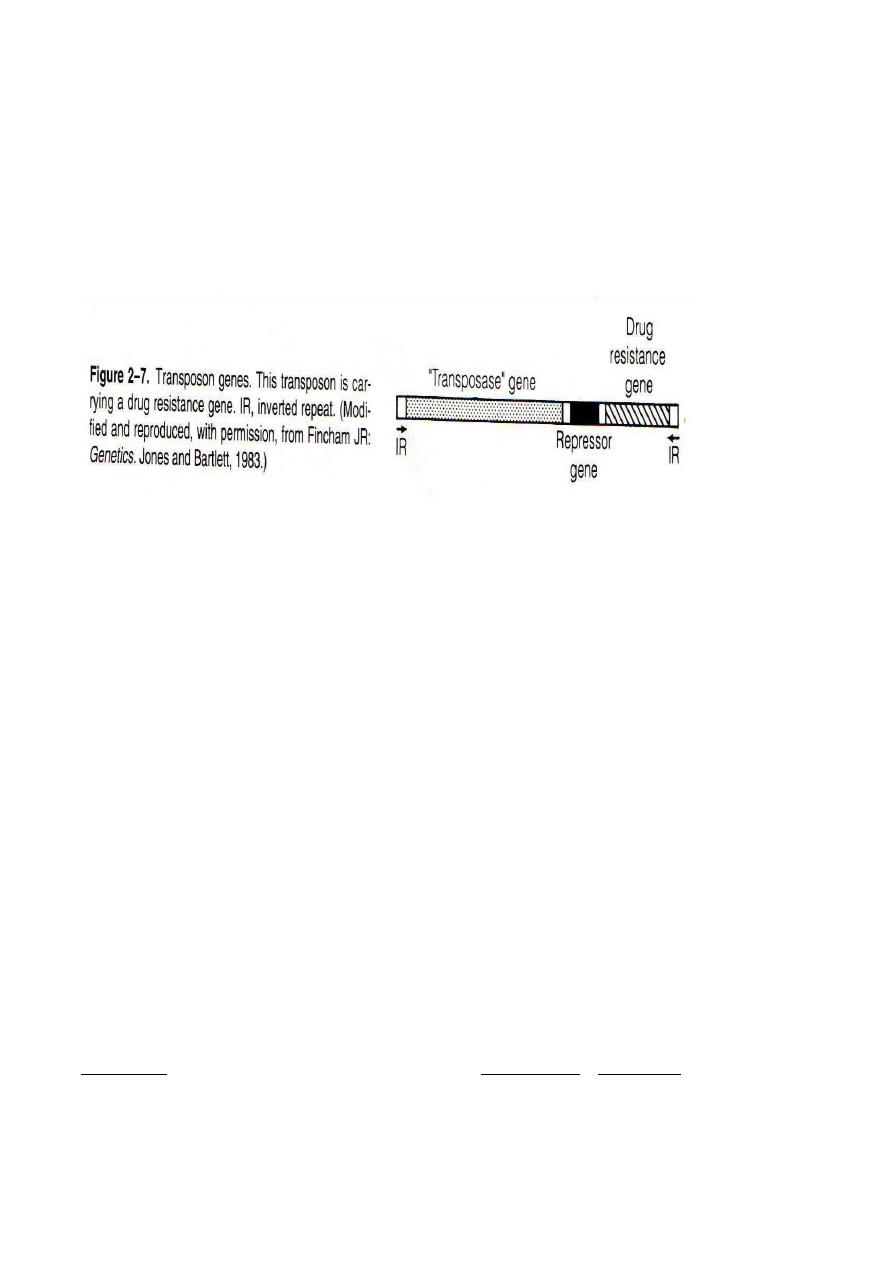
5-Transposons
( jumping genes):- are pieces of DNA that move readily from one site to another,
either within or between the DNA of bacteria ,plasmids or bacteriophages.
They can code for drug resistance enzyme, toxins & variety of metabolic enzymes, & they can cause
mutations in the gene site of integration &can be founding multiple copies at the ends of larger
transposon units.
6- Lysozyme:-
It can cleave the peptidoglycan backbone by breaking its glycosyl bonds, thereby contributing to the
natural resistance of the host to microbial infection. Lysozyme also important in regulating of
internal osmotic pressure of bacteria as the bacteria will survive as spherical form called protoplasts,
when lysozyme treated cell are in solution with the same osmotic pressure.
Specialized structures outside the cell wall:-
Capsule:-
is a protective gelatinous layer surrounding the entire bacterium, which composed of
polysaccharide, except in Bacillus anthrax, in which it composed of D- glutamic acid. Variation
in sugar component of polysaccharide composing capsule of such bacteria is useful in
identification of bacteria serologically .
Capsule importance:
1- It plays a role in the adherence of bacteria to human tissue that leads to initiation of infection.
2- It limits the ability to phagocytes to engulf the bacteria, so variant of non capsulated bacteria are
usually nonpathogenic.
3- Vaccine production from the polysaccharide of capsule, which considered as antigens that elicit
protective antibody.
4- Specific identification of an organism can be made by using antiserum against the capsular
polysaccharide (Quelling reaction, swelling of bacteria in the presence of homologous antibody).
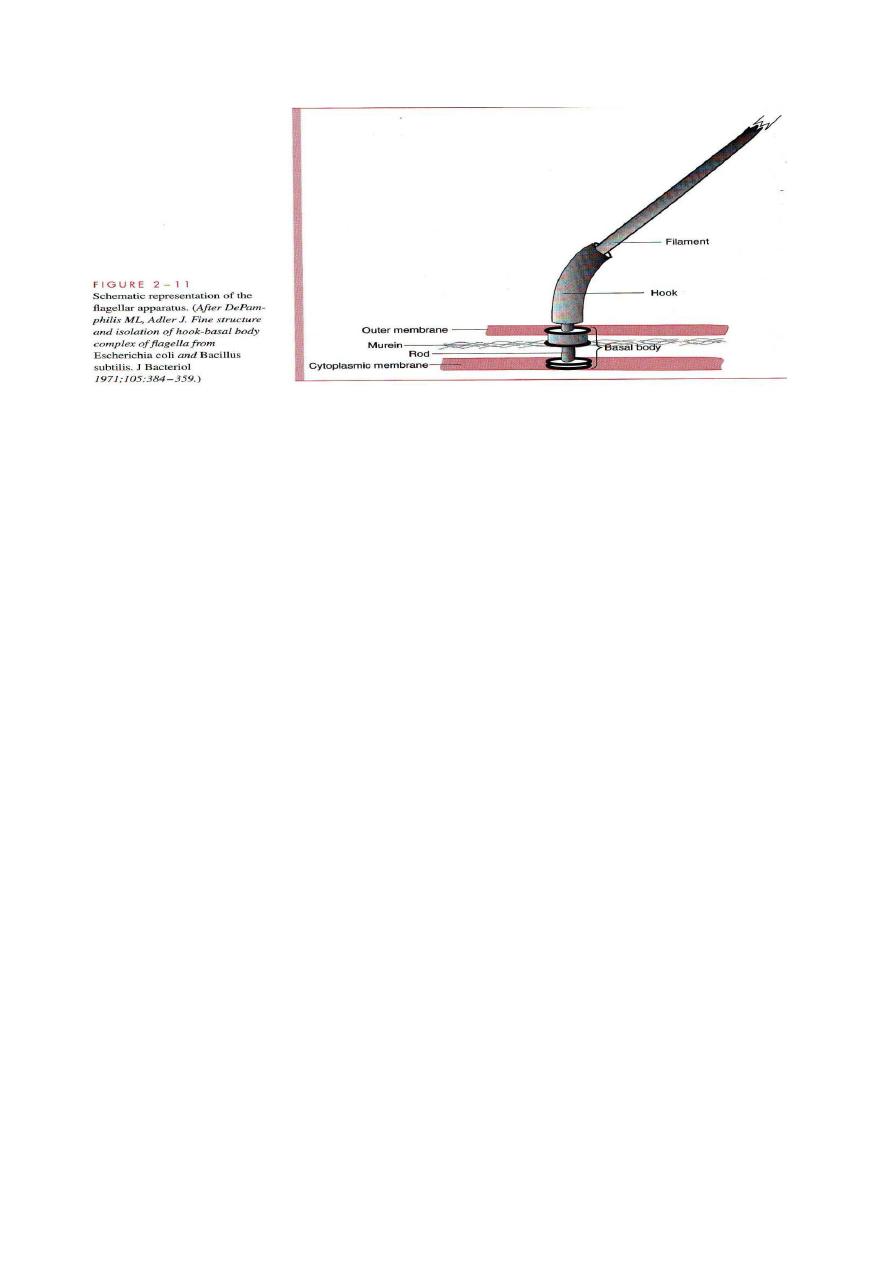
Flagella:-
Are rotating helical protein structures responsible for locomotion of bacteria, it have bushing rings
in cell envelop, Also flagella filament is composed of the protein called flagillin( used for strain
differentiation of Enterobacteriacae).The arrangement of flagellum in bacteria can be focus as
us. In addition to
monotricho
&
polytrichous
le or
from the Greek trichos= hair at one po
peritrichous
motility, flagella are important as it was chemotaxis( sensor function)that detect differences in the
concentration of the medium.
Pili:-
Is proteinous hair like projection. They are two types, common pili(or fimbriae) that have adhesive
roles specially in Neisseria gonorrhoeae. While sex pili is diagnostic of a male bacterium & is
involved in the exchange of genetic material between some G-ve bacteria, there is only on per cell.
Glycocalyx( slime layer):-
Is a polysaccharide film that cover the surface of bacteria, secreted by bacteria it self. It used to
bacterial adhere to various structures such as skin heart valves& catheters .It plays an important role
in plaque formation, the precursor of dental caries mostly caused by Streptococcus mutans.
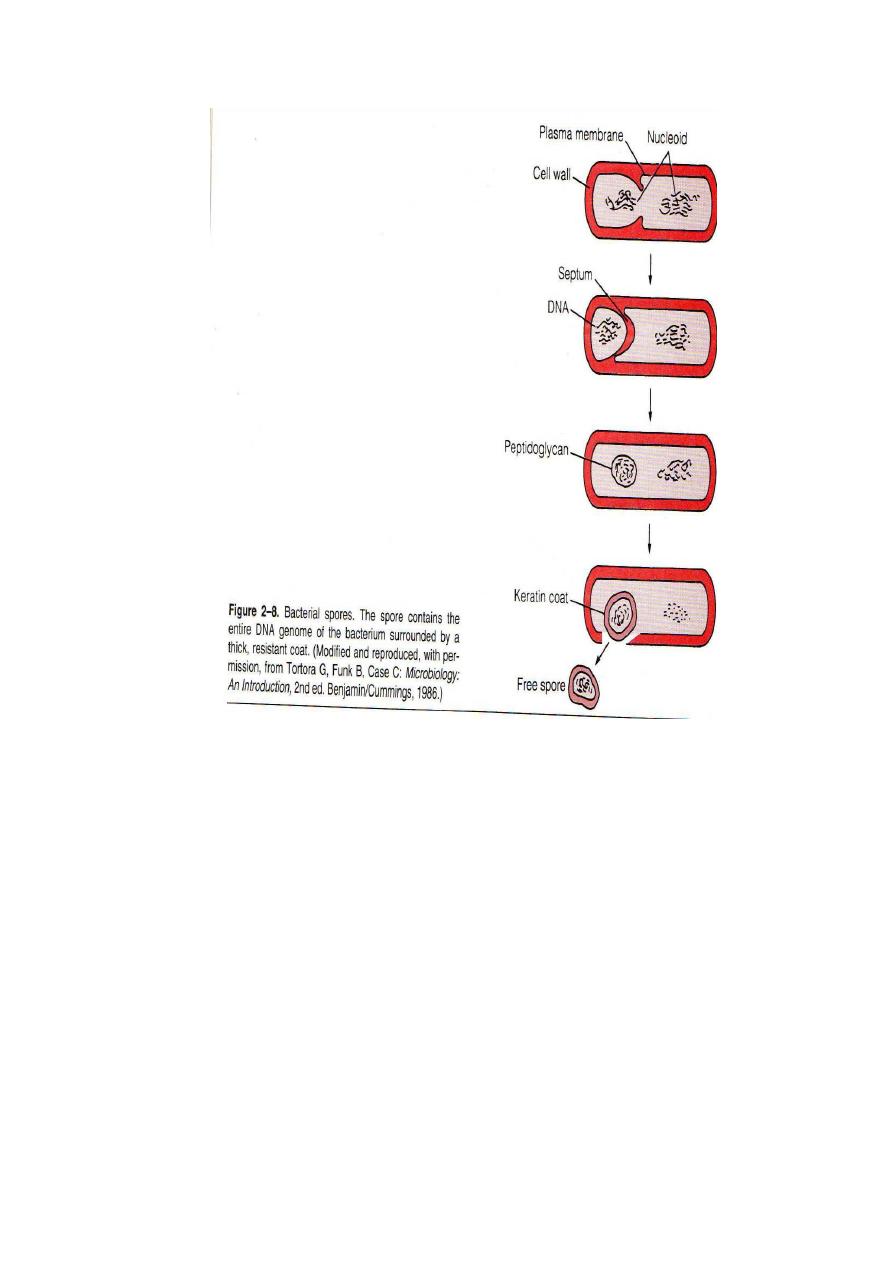
Spores:-
Endospores are small hardly quiescent form of some G+ve bacteria such as the genus Bacilli which
includes the agent of Anthrax & clostridium which involves the agent of tetanus & botulism ( food
poisoning ). In spite of germination of endospore after subsiding of adverse factor, but sporulation is
not reproductive process.
Spore of some species can withstand of Ph & temperature, thermal resistance is brought about by
lower water content & abundant mount of calcium dipicolinate. Spore membrane had role in
persisting against chemical & radiations, through special coat of peptidoglycan, which is cysteine
rich,keratine like insoluble protein.
An external layer of lipoprotein & carbohydrate layer called an exosporium.
Conclusion to bacterial structures
Function
Chemical composition
Structure
Give rigid support, protect
against osmotic pressure,
is the site of action of
penicillins&
cephalosporins& site of
degraded lysozyme
Sugar backbone with peptide
side chains that are cross
linked
Essential components
Cell wall peptidoglycan
Major surfaced antigen but
rarely used in laboratory
diagnosis
Techoic acid
Outer membrane G+ve
Toxic moiety of endotoxin
Major surface antigen used
in lab.diagnosis.
Lipid A
Polysaccharide
Outer membrane G_ve
Site of oxidative &
transport enzymes
Lipoprotein bilayer without
sterols
Cytoplasmic membrane
Protein synthesis, site of
action of
aminoglycosides&others.
RNA & protein in 50S& 30S
sununits
Ribosomes
Genetic material
DNA
Nucleoid
Participate in cell division
& secretion
Invagination of plasma
membrane
Mesosome
Contains many hydrolytic
enzymes including ß-
lactamase.
Space between plasma
membrane & outer
membrane
Periplasmic layer
Protect against
phagocytosis
Polysaccharide
Non essential
components
Capsule
Mediate adherence &
attachment to other sex.
glycoprotein
Pilus or fimbria
Motility
Protein
Flagellum
Provides resistance to
dehydration, heat &
chemicals
Keratin like coat ,dipicolinic
acid
Spore
Contains a variety of genes
for antibiotic resistance,
enzyme & toxins
DNA
Plasmid
Storage site of food
Glycogen,lipids,phospholipid
Granules
Mediate adherence to
surfaces.
polysaccharide
Glycocalyx
Bacterial processes:
Bacterial growth requires 3 complex process ( metabolisim, regulation & cell division).
Metabolism
of prokaryotic cells is more active, versatile & diverse than that of human cells..
Metabolic reactions accomplish 4 functions for growth:
.
, biosynthesis, polymerization & assembly
Fueling
Regulation
like translocation & export of protein .
Cell division:-
More genes are involved in cell division; multiple replication forks allow faster cell division than
chromosome replication. Nucleate cells are produced unless division & replication are coordinated
.Division & morphology is distorted by many antimicrobics.
Some species can divide every 20 minutes like Escherichia coli, others like Mycobacterium
tuberculosis require 24 hours, Growth rate is depend on :
Nutrient availability, PH of medium, temperature, & presence & absence of Oxygen .
*According to temperature, the best growth of bacteria is at 35 to 37 C, they called mesophiles,&
that grew at refrigerator temperature are called psychrophiles ,some bacteria can grew at above 50C
are called thermophiles.
* According to bacteria response to Oxygen, see the following table:
examples
comments
Position of
catalase&
superoxide
, dismutase
Growth response
Type of bacteria
anaerobic
aerobic
Mycobacterium
tuberculosis
Pseudomonas
aeruginosa
Bacillus subtilis
Requires
O2,can not
ferment
+
-ve
+
Aerobe(strict
aerobe)
Clostridium
botulinum
Bacteroides
melaninogenicus
Killed by
O2,fermentsin
absence of O2
-ve
+ve
-ve
Strict anaerobe
Escherichia coli
Shigella
dysenteriae
Staphylococcus
aureus
Requires with
O2,ferments
in absence of
O2
+ve
+ve
+ve
Facultative
Streptococcus
pneumoniae
Streptococcus
pyogenes
Ferments in
prescence or
absence of O2
+ ve
+ ve
+ve
Indifferent
(aerotolerant
anaerobes)
Campylobacter
jejuni
Grow best at
low O2
concentration,
can grow
without O2
(+) a
+ve
(+ve)a
Micro-aerophilic
Hydrogen ion concentration ( PH):
_ Bacteria are vary in their growing in regard of PH of culture
media, started from low PH ( 3
—4) for lactobacilli to Vibrio cholera that requires PH=8.6 .Most of
human pathogenic bacteria requires PH range of 6 to7. to slightly alkaline medium.
rom oxidation of
getting their energy f
,
chemotrophs
The majority of bacteria are
-
Source of energy:
& those
phototrophs
able to derive energy from sunlight so they called
s
chemical compounds, other
.
organotrophs
-
Chemo
of man or animal are
that parasites
Carbon dioxide (CO2)
: it is important to improve the growth of many parasitic bacteria like many
aerobes & Neisseria gonorrhoeae & for primary isolation of Brucella abortus with optimum Co2
ranges( 5 to 10 %).,Some bacteria such as Streptococcus milleri have an absolute requirement for
can be the sole
2
. Free CO
r carboxyphilic
dependent o
-
CO2
high CO2 concentration, they called
carbon of autotrophs.
Raw materials:
-Growing in simple inorganic salt is the mode of chemotrophic bacteria(called
autotrophs),while heterotrphs( using organic & inorganic substrates),like Esch.coli that grow in
solution containing glucose( carbon & energy source) & Ammonium sulphate ( nitrogen
source).while others requires vitamins ,mineral,aminoacids in addition to carbohydrate& other
requirements.
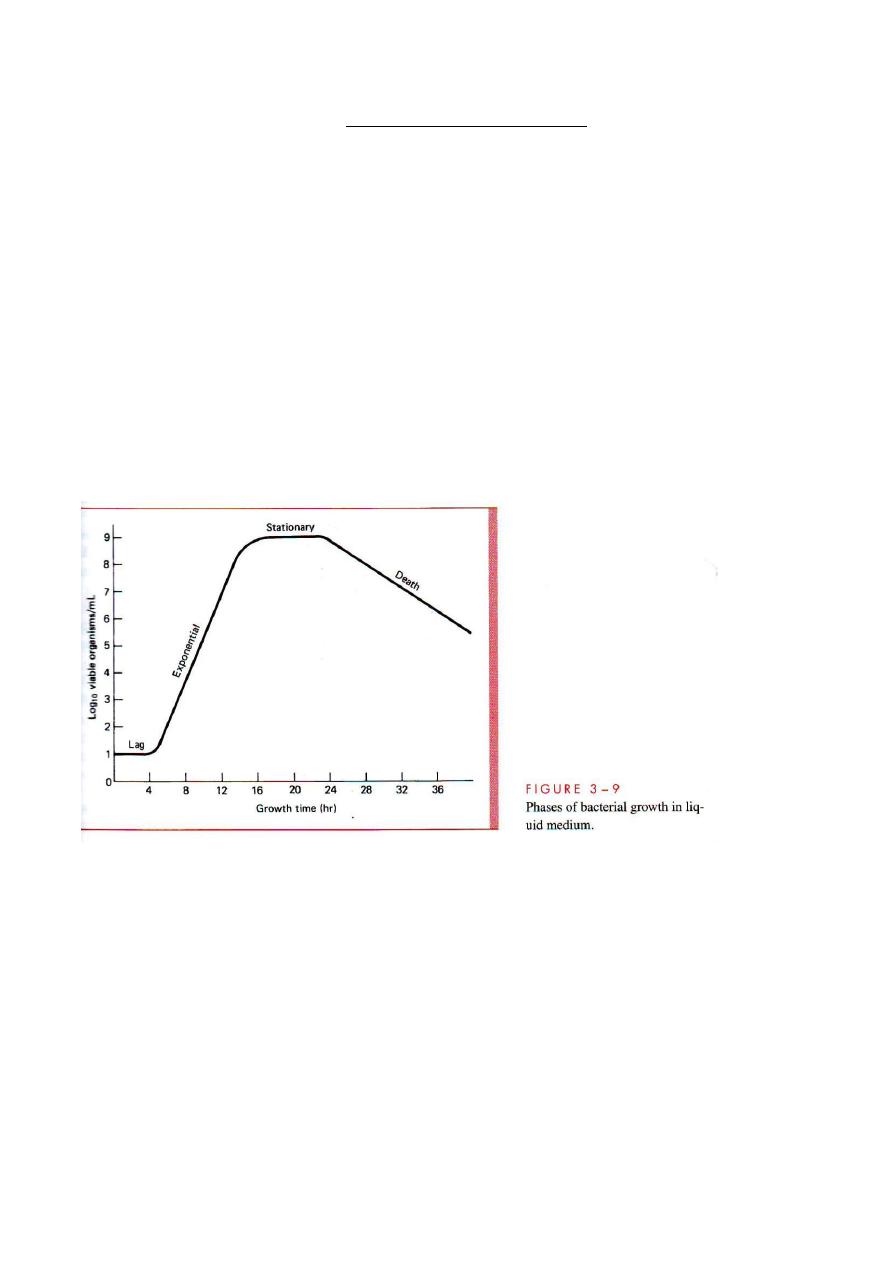
Growth cycle:-
It has 4 major phases, if a small number of bacteria are inoculated into a liquid nutrient medium, it
will reproduce by binary fission, that to be called exponential growth or( logarithmic growth), the
typical phases are:
1- lag phase, during which vigorous metabolic activity occurs, but cell do not divide, this can last for
a few minutes up to many hours.
2- Exponential (log phase) growth during which generation time is constant& reproductive capacity
enormous. it can last less than 7 hours.
3- The stationary phase occurs when nutrient depletion or toxic metabolic product lead growth to
slow until the number of cell produced balances the number of cells die, resulting in steady state.
4- Death or decline phase:- which is marked by a decline in the number of viable bacteria.
Classification of medically important bacteria:
According to nature of cell wall,( rigid, flexible, or absent) ,sub-division such as rigid thick wall can
be divided in to free living bacteria( which are capable of growing in laboratory) or non living
bacteria which are obligate intracellular(tissue or cell culture) like , Chlamydia. Also shape & type of
staining are important in classification of free living bacteria, while flexible bacteria( spirochetes)
&without cell wall( mycoplasma) form separate.
Representative diseases
genus
Characteristics
Pneumonia,pharyngitis,cellulites
Abscess of skin & other organs
Anthrax
Tetanus, gas gangrene, botulism
Diphtheria
Meningitis
Actinomycosis
Nocardiosis
Meningitis, gonorrhea
Meningitis
Whooping cough
Pneumonia
Brucellosis
Tularemia
Cellulites
Plaque
Urinary tract infection (UTI),diarrhea
UTI
Pneumonia
Pneumonia, UTI
Enterocolitis ,typhoid fever
Enterocolitis
UTI
Enterocolitis
Cholera
Pneumonia, UTI
Peritonitis
Tuberculosis, leprosy
Rocky mountain spotted fever,typhus
Fever & Q fever
Urethritis ,trachoma ,psittacosis, PID
Streptococcus
Staphylococcus
Bacillus
Clostridium
Corynebacterium
Listeria
Actinomyces
Nocardia
Neiseeria
Haemophilus
Bordetella
Legionella
Brucella
Francisella
Pasteurella
Yersinia
Escherichia
Enterobacter
Serratia
Klebsiella
Salmonella
Shigella
Proteus
Campylobacter
Vibrio
Pseudomonas
Bacteriodes
Mycobacterium
Rickettsia
Chlamydia
1-Rigid thick wall cells
A- Free living( extra-cellular
bacteria).
1Gram +ve:-
a- cocci
b- spore forming rods:
* aerobic
* Anaerobic
C- Non-spore-forming rods
* Non filamentous
*Filamentous
2- Gram
–ve
a- cocci
b- Rods:-
(I ) facultative
* straight:-
( i) respiratory organism
(ii) Zoonotic organisms
(iii)Enteric & related
organisms
* Curved
(II )- Aerobic
(III ) Anaerobic
3- Acid fast bacilli
B-Non-free living( obligate
Intracellular organisms)
Syphilis
Lyme disease
Leptospirosis
Treponema
Borrelia
Leptospira
2- Flexible, thin walled cells
spirochetes
pneumonia
Mycoplasma
Wall-less cella
Lecture Number ( 2 ): Host parasite relationships& pathogenesis.
-
The pathogen :
In medicine it can be defined as any microorganism capable for causing disease.
From mouth to anus & from head to toe, every millimetre of our cells that is exposed to the outside
world has as rich biological diversity. Most of these are not only innocucous but play a useful, if
unseen,( protection,, give us some vitamins,& nutrients & help digest food) They are necessary part
of the development pathways required for maturation of our intestinal mucosa & our innate local
immunity system.
Most of human microbes are commensal, which they eat from the same table. Some commensals
exist in mutual comfort (living together) & some commensal transient species may be opportunistic
pathogen( It refers to ability of organism to take opportunity offered to reduce host defences to cause
disease, Escherichia coli of adult is normal flora or commensal , but when induced to urinary tract it
converted to pathogenic one . opportunistic microorganisms can cause serious infections in immuno-
compromised patients
Primary pathogens:- A small group of moicroorganisms often causes infection & overt diseases in
seemingly normal individual, such as common cold virus, mumps virus, tubercle bacilli ,each
organism is adapted exclusively to humans., while Salmonella typimurium is a common cause of
food poisoning can cause disease in both humans & animals, bird & even reptile.
Features of disease may be linked to transmission, for example, coughing promotes the transmission
of the tubercle bacillus & influenza virus & diarrhea spread enteric viruses, bacteria & protozoa.
Parasite:
this term refers to animal creatures like protozoa & helminths that parasitized human &
animals, while the same term refers to the parasite relationship of bacteria to the host cell. The
presences of bacteria are detrimental to host cells.
Some bacteria pathogens are intracellular parasites like Chalmydia & Rickettsia, because they can
grow only within host cells . While other bacteria that can grow within cells, outside cells or on
bacteriological media are called facultative parasites.
-
Emergency of infectious disease:
Infectious disease have been the major causes of human morbidity & mortality, the prevalence of
infectious disease caused by microorganisms shows changes, mostly due to growing of communities
& changes in human life style, so some diseases that one third to one half human population before
700 years age, that known black death, was absent today. Some diseases such as treptonematosis,
mycobacterium infection, some parasitic & some viral infection like herpes viruses, likely afflicted
early humans because of their latency & their tendency to reactivate over long periods of time.
Poverty, with its crowding, unsanitary condition, often malnutrition, leads to an increased
susceptibility to infection & disease. War famine, civil unrest & epidemic disease lead to breakdown
in public infrastructure & the increased incidence of infectious diseases. Also animal domestication
is important, because most the infectious agents of such animal may increase the prevalence of
infectious disease
( zoonosis).
-
Types of bacterial infections:
Epidemic infection: when it occurs more frequently than usual.
Pandemic:- When the bacterial infection has a worldwide distribution.
Endemic infection: is an infection which is constantly present at low level in
a specific population.
Subclinical infection
:-Is that infection resulted in overt symptoms, it can be detected

only by demonstrating a rise in antibody titer or isolating the organism
Latent infection:-
is that state of infection can be resulted from reactivation of the
Growth of the organism &recurrence of symptoms may occur.
Chronic carrier:- In which the organism continue to grow with or without producing
symptoms in the host, the more important example is typhoid, as it acts as a
public health hazard.
Termination bacteria from the host :-
It involves an
awareness of 2 phenomena:
Normal flora & colonization.
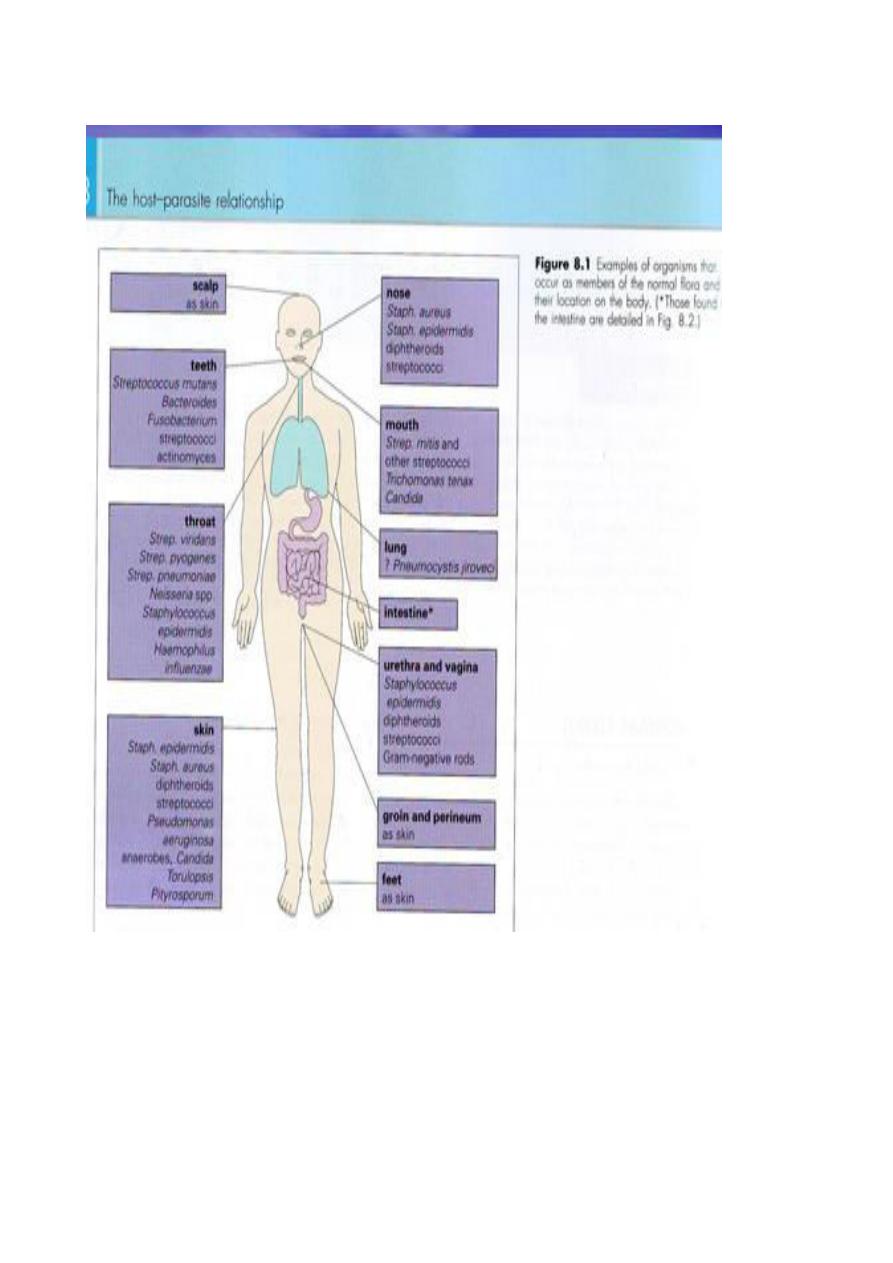
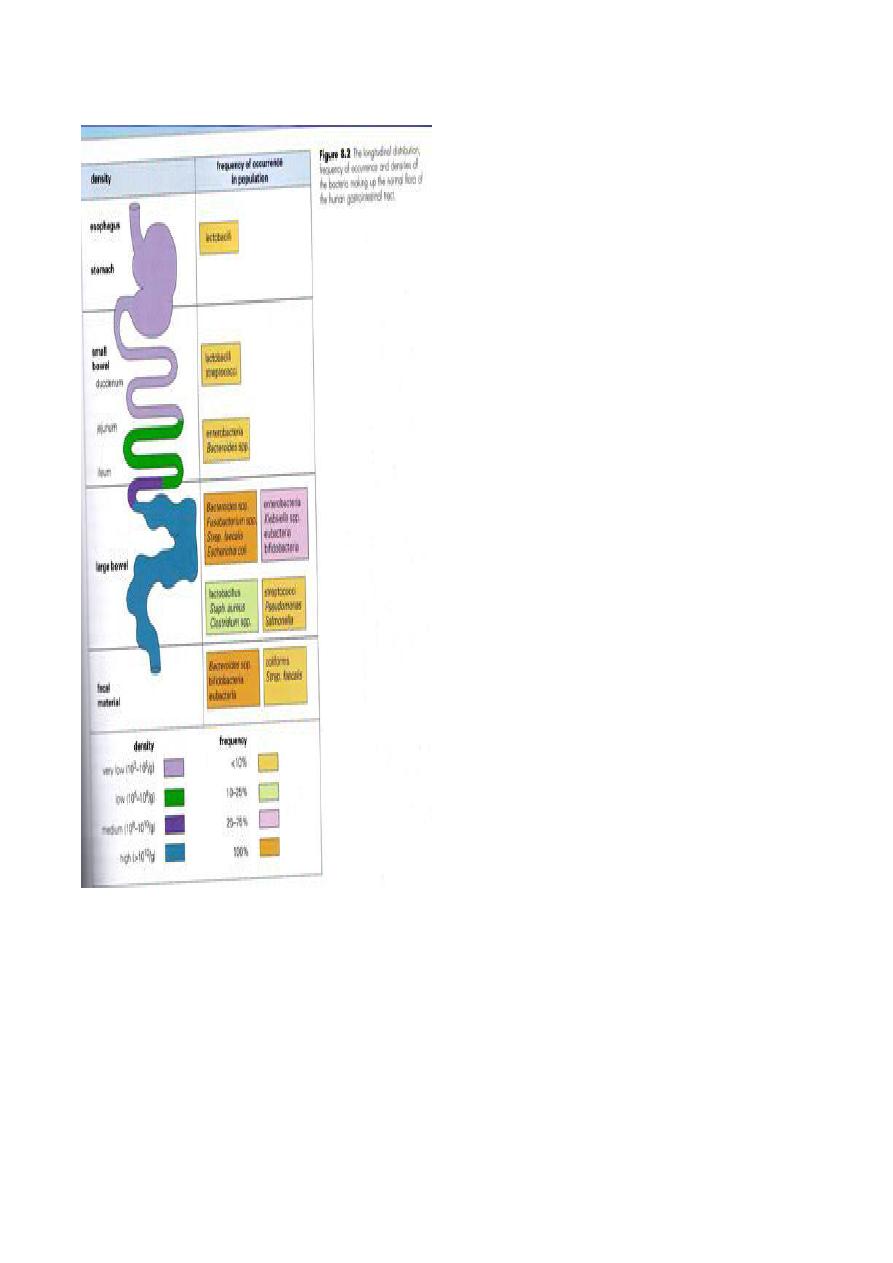
The Normal Flora:
A
A
s
s
t
t
h
h
e
e
b
b
a
a
s
s
e
e
t
t
h
h
e
e
t
t
e
e
r
r
m
m
f
f
l
l
o
o
r
r
a
a
i
i
s
s
u
u
s
s
e
e
d
d
f
f
o
o
r
r
o
o
r
r
g
g
a
a
n
n
i
i
s
s
m
m
s
s
c
c
o
o
n
n
c
c
e
e
r
r
n
n
i
i
n
n
g
g
b
b
a
a
c
c
t
t
e
e
r
r
i
i
a
a
,
,
s
s
u
u
c
c
h
h
g
g
r
r
o
o
u
u
p
p
o
o
f
f
b
b
a
a
c
c
t
t
e
e
r
r
i
i
a
a
a
a
r
r
e
e
n
n
o
o
t
t
h
h
a
a
r
r
m
m
f
f
u
u
l
l
t
t
o
o
h
h
o
o
s
s
t
t
,
,
t
t
h
h
e
e
y
y
a
a
r
r
e
e
w
w
i
i
d
d
e
e
l
l
y
y
d
d
i
i
s
s
t
t
r
r
i
i
b
b
u
u
t
t
e
e
d
d
i
i
n
n
m
m
o
o
s
s
t
t
o
o
r
r
g
g
a
a
n
n
s
s
i
i
n
n
t
t
h
h
e
e
b
b
o
o
d
d
y
y
.
.
T
T
h
h
e
e
n
n
o
o
r
r
m
m
a
a
l
l
f
f
l
l
o
o
r
r
a
a
i
i
s
s
a
a
c
c
q
q
u
u
i
i
r
r
e
e
d
d
r
r
a
a
p
p
i
i
d
d
l
l
y
y
d
d
u
u
r
r
i
i
n
n
g
g
&
&
s
s
h
h
o
o
r
r
t
t
l
l
y
y
a
a
f
f
t
t
e
e
r
r
b
b
i
i
r
r
t
t
h
h
&
&
c
c
h
h
a
a
n
n
g
g
e
e
s
s
c
c
o
o
n
n
t
t
i
i
n
n
u
u
o
o
u
u
s
s
l
l
y
y
t
t
h
h
r
r
o
o
u
u
g
g
h
h
l
l
i
i
f
f
e
e
,
,
f
f
o
o
r
r
e
e
x
x
a
a
m
m
p
p
l
l
e
e
b
b
r
r
e
e
a
a
s
s
t
t
f
f
e
e
d
d
i
i
n
n
f
f
a
a
n
n
t
t
s
s
h
h
a
a
v
v
e
e
l
l
a
a
c
c
t
t
i
i
c
c
a
a
c
c
i
i
d
d
s
s
t
t
r
r
e
e
p
p
t
t
o
o
c
c
o
o
c
c
c
c
i
i
&
&
l
l
a
a
c
c
t
t
o
o
b
b
a
a
c
c
i
i
l
l
l
l
i
i
i
i
n
n
t
t
h
h
e
e
i
i
r
r
G
G
I
I
T
T
,
,
w
w
h
h
e
e
r
r
e
e
a
a
s
s
b
b
o
o
t
t
t
t
l
l
e
e
f
f
e
e
e
e
d
d
c
c
h
h
i
i
l
l
d
d
r
r
e
e
n
n
s
s
h
h
o
o
w
w
a
a
m
m
u
u
c
c
h
h
g
g
r
r
e
e
a
a
t
t
e
e
r
r
v
v
a
a
r
r
i
i
e
e
t
t
y
y
o
o
f
f
o
o
r
r
g
g
a
a
n
n
i
i
s
s
m
m
s
s
D
D
i
i
f
f
f
f
e
e
r
r
e
e
n
n
t
t
r
r
e
e
g
g
i
i
o
o
n
n
s
s
o
o
f
f
t
t
h
h
e
e
s
s
k
k
i
i
n
n
s
s
u
u
p
p
p
p
o
o
r
r
t
t
d
d
i
i
f
f
f
f
e
e
r
r
e
e
n
n
t
t
f
f
l
l
o
o
r
r
a
a
s
s
u
u
c
c
h
h
a
a
s
s
i
i
n
n
m
m
o
o
i
i
s
s
t
t
e
e
r
r
a
a
r
r
e
e
a
a
s
s
(
(
a
a
x
x
i
i
l
l
l
l
a
a
e
e
,
,
p
p
e
e
r
r
i
i
n
n
e
e
u
u
m
m
,
,
b
b
e
e
t
t
w
w
e
e
e
e
n
n
t
t
o
o
e
e
s
s
,
,
s
s
c
c
a
a
l
l
p
p
)
)
s
s
u
u
p
p
p
p
o
o
r
r
t
t
m
m
u
u
c
c
h
h
l
l
a
a
r
r
g
g
e
e
r
r
p
p
o
o
p
p
u
u
l
l
a
a
t
t
i
i
o
o
n
n
o
o
f
f
s
s
t
t
a
a
p
p
h
h
y
y
l
l
o
o
c
c
o
o
c
c
c
c
u
u
s
s
e
e
p
p
i
i
d
d
e
e
r
r
m
m
i
i
d
d
i
i
s
s
&
&
S
S
t
t
a
a
p
p
h
h
y
y
l
l
o
o
c
c
o
o
c
c
c
c
u
u
s
s
a
a
u
u
r
r
e
e
u
u
s
s
m
m
a
a
y
y
b
b
e
e
p
p
r
r
e
e
s
s
e
e
n
n
t
t
i
i
n
n
t
t
h
h
e
e
m
m
o
o
i
i
s
s
t
t
u
u
r
r
e
e
r
r
e
e
g
g
i
i
o
o
n
n
s
s
C
C
h
h
a
a
n
n
g
g
e
e
s
s
i
i
n
n
t
t
h
h
e
e
s
s
k
k
i
i
n
n
o
o
c
c
c
c
u
u
r
r
r
r
i
i
n
n
g
g
d
d
u
u
r
r
i
i
n
n
g
g
p
p
u
u
b
b
e
e
r
r
t
t
y
y
o
o
f
f
t
t
e
e
n
n
l
l
e
e
a
a
d
d
t
t
o
o
i
i
n
n
c
c
r
r
e
e
a
a
s
s
e
e
d
d
n
n
u
u
m
m
b
b
e
e
r
r
s
s
o
o
f
f
a
a
n
n
a
a
e
e
r
r
o
o
b
b
i
i
c
c
d
d
i
i
p
p
h
h
t
t
h
h
e
e
r
r
i
i
o
o
d
d
s
s
&
&
p
p
r
r
o
o
b
b
i
i
o
o
n
n
i
i
b
b
a
a
c
c
t
t
e
e
r
r
i
i
u
u
m
m
a
a
c
c
n
n
e
e
.
.
B
B
o
o
t
t
h
h
n
n
o
o
s
s
e
e
&
&
m
m
o
o
u
u
t
t
h
h
c
c
a
a
n
n
b
b
e
e
h
h
e
e
a
a
v
v
i
i
l
l
y
y
c
c
o
o
l
l
o
o
n
n
i
i
z
z
e
e
d
d
b
b
y
y
b
b
a
a
c
c
t
t
e
e
r
r
i
i
a
a
.
.
T
T
h
h
e
e
s
s
u
u
r
r
f
f
a
a
c
c
e
e
s
s
o
o
f
f
t
t
h
h
e
e
t
t
e
e
e
e
t
t
h
h
&
&
g
g
i
i
n
n
g
g
i
i
v
v
a
a
l
l
c
c
r
r
e
e
v
v
i
i
c
c
e
e
s
s
c
c
a
a
r
r
r
r
y
y
l
l
a
a
r
r
g
g
e
e
n
n
u
u
m
m
b
b
e
e
r
r
o
o
f
f
a
a
n
n
a
a
e
e
r
r
o
o
b
b
i
i
c
c
b
b
a
a
c
c
t
t
e
e
r
r
i
i
a
a
s
s
u
u
c
c
h
h
a
a
s
s
S
S
t
t
r
r
e
e
p
p
t
t
o
o
c
c
o
o
c
c
c
c
u
u
s
s
m
m
u
u
t
t
a
a
n
n
s
s
w
w
h
h
i
i
c
c
h
h
c
c
a
a
n
n
l
l
e
e
a
a
d
d
t
t
o
o
d
d
e
e
n
n
t
t
a
a
l
l
d
d
e
e
c
c
a
a
y
y
(
(
c
c
a
a
r
r
i
i
e
e
s
s
)
)
a
a
s
s
a
a
c
c
i
i
d
d
f
f
e
e
r
r
m
m
e
e
n
n
t
t
c
c
a
a
r
r
b
b
o
o
h
h
y
y
d
d
r
r
a
a
t
t
e
e
s
s
c
c
a
a
n
n
a
a
t
t
t
t
a
a
c
c
k
k
d
d
e
e
n
n
t
t
a
a
l
l
e
e
n
n
a
a
m
m
e
e
l
l
.
.
T
T
h
h
e
e
p
p
r
r
e
e
v
v
a
a
l
l
e
e
n
n
c
c
e
e
o
o
f
f
d
d
e
e
n
n
t
t
a
a
l
l
d
d
e
e
c
c
a
a
y
y
i
i
s
s
l
l
i
i
n
n
k
k
e
e
d
d
t
t
o
o
d
d
i
i
e
e
t
t
.
.
T
T
h
h
e
e
p
p
h
h
a
a
r
r
y
y
n
n
x
x
&
&
t
t
r
r
a
a
c
c
h
h
e
e
a
a
c
c
a
a
r
r
r
r
y
y
t
t
h
h
e
e
i
i
r
r
o
o
w
w
n
n
n
n
o
o
r
r
m
m
a
a
l
l
f
f
l
l
o
o
r
r
a
a
s
s
u
u
c
c
h
h
a
a
s
s
b
b
e
e
t
t
a
a
h
h
e
e
m
m
o
o
l
l
y
y
t
t
i
i
c
c
s
s
t
t
r
r
e
e
p
p
t
t
o
o
c
c
o
o
c
c
c
c
i
i
&
&
S
S
t
t
a
a
p
p
h
h
y
y
l
l
o
o
c
c
o
o
c
c
c
c
u
u
s
s
a
a
u
u
r
r
e
e
u
u
s
s
,
,
N
N
e
e
i
i
s
s
s
s
e
e
r
r
i
i
a
a
&
&
d
d
i
i
p
p
h
h
t
t
h
h
e
e
r
r
o
o
i
i
d
d
s
s
.
.
I
I
n
n
t
t
h
h
e
e
g
g
u
u
t
t
t
t
h
h
e
e
d
d
e
e
n
n
s
s
i
i
t
t
y
y
o
o
f
f
m
m
i
i
c
c
r
r
o
o
o
o
r
r
g
g
a
a
n
n
i
i
s
s
m
m
'
'
s
s
i
i
n
n
c
c
r
r
e
e
a
a
s
s
e
e
s
s
f
f
r
r
o
o
m
m
s
s
t
t
o
o
m
m
a
a
c
c
h
h
t
t
o
o
t
t
h
h
e
e
l
l
a
a
r
r
g
g
e
e
i
i
n
n
t
t
e
e
s
s
t
t
i
i
n
n
e
e
.
.
U
U
r
r
e
e
t
t
h
h
r
r
a
a
i
i
s
s
l
l
i
i
g
g
h
h
t
t
l
l
y
y
c
c
o
o
l
l
o
o
n
n
i
i
z
z
e
e
d
d
i
i
n
n
b
b
o
o
t
t
h
h
s
s
e
e
x
x
e
e
s
s
,
,
b
b
u
u
t
t
t
t
h
h
e
e
v
v
a
a
g
g
i
i
n
n
a
a
s
s
u
u
p
p
p
p
o
o
r
r
t
t
s
s
a
a
n
n
e
e
x
x
t
t
e
e
n
n
s
s
i
i
v
v
e
e
f
f
l
l
o
o
r
r
a
a
o
o
f
f
b
b
a
a
c
c
t
t
e
e
r
r
i
i
a
a
&
&
f
f
u
u
n
n
g
g
i
i
.
.
.
.
`
`
T
T
y
y
p
p
e
e
s
s
o
o
f
f
n
n
o
o
r
r
m
m
a
a
l
l
f
f
l
l
o
o
r
r
a
a
:
:
1
1
-
-
R
R
e
e
s
s
i
i
d
d
e
e
n
n
t
t
f
f
l
l
o
o
r
r
a
a
:
:
I
I
t
t
i
i
n
n
v
v
o
o
l
l
v
v
e
e
s
s
f
f
i
i
x
x
e
e
d
d
t
t
y
y
p
p
e
e
s
s
o
o
f
f
m
m
i
i
c
c
r
r
o
o
-
-
o
o
r
r
g
g
a
a
n
n
i
i
s
s
m
m
s
s
,
,
w
w
h
h
i
i
c
c
h
h
f
f
o
o
u
u
n
n
d
d
i
i
n
n
g
g
i
i
v
v
e
e
n
n
a
a
r
r
e
e
a
a
a
a
t
t
g
g
i
i
v
v
e
e
n
n
a
a
g
g
e
e
r
r
e
e
g
g
u
u
l
l
a
a
r
r
l
l
y
y
.
.
2
2
-
-
T
T
r
r
a
a
n
n
s
s
i
i
e
e
n
n
t
t
f
f
l
l
o
o
r
r
a
a
:
:
I
I
t
t
i
i
n
n
v
v
o
o
l
l
v
v
e
e
s
s
n
n
o
o
n
n
p
p
a
a
t
t
h
h
o
o
g
g
e
e
n
n
i
i
c
c
o
o
r
r
p
p
o
o
t
t
e
e
n
n
t
t
i
i
a
a
l
l
l
l
y
y
p
p
a
a
t
t
h
h
o
o
g
g
e
e
n
n
i
i
c
c
m
m
i
i
c
c
r
r
o
o
o
o
r
r
g
g
a
a
n
n
i
i
s
s
m
m
s
s
t
t
h
h
a
a
t
t
i
i
n
n
h
h
i
i
b
b
i
i
t
t
p
p
a
a
r
r
t
t
i
i
c
c
u
u
l
l
a
a
r
r
b
b
o
o
d
d
y
y
l
l
o
o
c
c
a
a
t
t
i
i
o
o
n
n
f
f
o
o
r
r
l
l
i
i
m
m
i
i
t
t
e
e
d
d
t
t
i
i
m
m
e
e
.
.
I
I
f
f
t
t
h
h
e
e
n
n
o
o
r
r
m
m
a
a
l
l
f
f
l
l
o
o
r
r
a
a
i
i
s
s
i
i
n
n
t
t
a
a
c
c
t
t
,
,
t
t
h
h
e
e
r
r
e
e
i
i
s
s
t
t
h
h
e
e
v
v
e
e
r
r
y
y
l
l
i
i
t
t
t
t
l
l
e
e
s
s
i
i
g
g
n
n
i
i
f
f
i
i
c
c
a
a
n
n
c
c
e
e
o
o
f
f
t
t
h
h
e
e
t
t
r
r
a
a
n
n
s
s
i
i
e
e
n
n
t
t
f
f
l
l
o
o
r
r
a
a
.
.
B
B
u
u
t
t
i
i
f
f
t
t
h
h
e
e
n
n
o
o
r
r
m
m
a
a
l
l
f
f
l
l
o
o
r
r
a
a
i
i
s
s
d
d
i
i
s
s
t
t
u
u
r
r
b
b
e
e
d
d
,
,
t
t
h
h
e
e
t
t
r
r
a
a
n
n
s
s
i
i
e
e
n
n
t
t
m
m
i
i
c
c
r
r
o
o
o
o
r
r
g
g
a
a
n
n
i
i
s
s
m
m
s
s
m
m
a
a
y
y
c
c
o
o
l
l
o
o
n
n
i
i
z
z
e
e
,
,
p
p
r
r
o
o
l
l
i
i
f
f
e
e
r
r
a
a
t
t
e
e
&
&
p
p
r
r
o
o
d
d
u
u
c
c
e
e
d
d
i
i
s
s
e
e
a
a
s
s
e
e
.
.
A
A
d
d
v
v
a
a
n
n
t
t
a
a
g
g
e
e
s
s
o
o
f
f
n
n
o
o
r
r
m
m
a
a
l
l
f
f
l
l
o
o
r
r
a
a
:
:
S
S
o
o
m
m
e
e
o
o
f
f
t
t
h
h
e
e
s
s
p
p
e
e
c
c
i
i
e
e
s
s
o
o
f
f
n
n
o
o
r
r
m
m
a
a
l
l
f
f
l
l
o
o
r
r
a
a
a
a
r
r
e
e
p
p
o
o
s
s
i
i
t
t
i
i
v
v
e
e
l
l
y
y
b
b
e
e
n
n
e
e
f
f
i
i
c
c
i
i
a
a
l
l
t
t
o
o
t
t
h
h
e
e
h
h
o
o
s
s
t
t
s
s
u
u
c
c
h
h
a
a
s
s
i
i
n
n
t
t
h
h
e
e
f
f
o
o
l
l
l
l
o
o
w
w
i
i
n
n
g
g
b
b
y
y
w
w
h
h
i
i
c
c
h
h
n
n
o
o
r
r
m
m
a
a
l
l
f
f
l
l
o
o
r
r
a
a
c
c
a
a
n
n
p
p
r
r
e
e
v
v
e
e
n
n
t
t
s
s
c
c
o
o
l
l
o
o
n
n
i
i
z
z
a
a
t
t
i
i
o
o
n
n
b
b
y
y
p
p
o
o
t
t
e
e
n
n
t
t
i
i
a
a
l
l
p
p
a
a
t
t
h
h
o
o
g
g
e
e
n
n
s
s
.
.
1
1
-
-
S
S
k
k
i
i
n
n
b
b
a
a
c
c
t
t
e
e
r
r
i
i
a
a
p
p
r
r
o
o
d
d
u
u
c
c
e
e
f
f
a
a
t
t
t
t
y
y
a
a
c
c
i
i
d
d
s
s
,
,
w
w
h
h
i
i
c
c
h
h
d
d
i
i
s
s
c
c
o
o
u
u
r
r
a
a
g
g
e
e
o
o
t
t
h
h
e
e
r
r
s
s
p
p
e
e
c
c
i
i
e
e
s
s
f
f
r
r
o
o
m
m
i
i
n
n
v
v
a
a
d
d
i
i
n
n
g
g
.
.
2
2
-
-
G
G
u
u
t
t
b
b
a
a
c
c
t
t
e
e
r
r
i
i
a
a
r
r
e
e
l
l
e
e
a
a
s
s
e
e
a
a
n
n
u
u
m
m
b
b
e
e
r
r
o
o
f
f
f
f
a
a
c
c
t
t
o
o
r
r
s
s
w
w
i
i
t
t
h
h
a
a
n
n
t
t
i
i
b
b
a
a
c
c
t
t
e
e
r
r
i
i
a
a
l
l
a
a
c
c
t
t
i
i
v
v
i
i
t
t
y
y
(
(
b
b
a
a
c
c
t
t
e
e
r
r
i
i
o
o
c
c
i
i
n
n
s
s
,
,
c
c
o
o
l
l
i
i
c
c
i
i
n
n
s
s
)
)
a
a
s
s
w
w
e
e
l
l
l
l
a
a
s
s
m
m
e
e
t
t
a
a
b
b
o
o
l
l
i
i
c
c
w
w
a
a
s
s
t
t
e
e
p
p
r
r
o
o
d
d
u
u
c
c
t
t
s
s
t
t
h
h
a
a
t
t
h
h
e
e
l
l
p
p
p
p
r
r
e
e
v
v
e
e
n
n
t
t
t
t
h
h
e
e
e
e
s
s
t
t
a
a
b
b
l
l
i
i
s
s
h
h
m
m
e
e
n
n
t
t
o
o
f
f
o
o
t
t
h
h
e
e
r
r
s
s
p
p
e
e
c
c
i
i
e
e
s
s
.
.
3
3
-
-
V
V
a
a
g
g
i
i
n
n
a
a
l
l
l
l
a
a
c
c
t
t
o
o
b
b
a
a
c
c
i
i
l
l
l
l
i
i
m
m
a
a
i
i
n
n
t
t
a
a
i
i
n
n
a
a
n
n
a
a
c
c
i
i
d
d
e
e
n
n
v
v
i
i
r
r
o
o
n
n
m
m
e
e
n
n
t
t
,
,
w
w
h
h
i
i
c
c
h
h
s
s
u
u
p
p
p
p
r
r
e
e
s
s
s
s
e
e
s
s
g
g
r
r
o
o
w
w
t
t
h
h
G
G
a
a
r
r
d
d
n
n
e
e
r
r
e
e
l
l
l
l
a
a
v
v
a
a
g
g
i
i
n
n
a
a
l
l
i
i
s
s
&
&
m
m
o
o
b
b
l
l
i
i
n
n
c
c
u
u
s
s
b
b
e
e
n
n
e
e
f
f
i
i
t
t
s
s
o
o
f
f
n
n
o
o
r
r
m
m
a
a
l
l
f
f
l
l
o
o
r
r
a
a
:
:
O
O
t
t
h
h
e
e
r
r
-
-
4
4
A
A
-
-
S
S
y
y
n
n
t
t
h
h
e
e
s
s
i
i
z
z
e
e
o
o
f
f
v
v
i
i
t
t
a
a
m
m
i
i
n
n
K
K
,
,
t
t
h
h
a
a
t
t
p
p
a
a
r
r
t
t
i
i
c
c
i
i
p
p
a
a
t
t
e
e
i
i
n
n
c
c
o
o
a
a
g
g
u
u
l
l
a
a
t
t
i
i
o
o
n
n
p
p
r
r
o
o
c
c
e
e
s
s
s
s
e
e
s
s
.
.
B
B
-
-
S
S
o
o
m
m
e
e
b
b
a
a
c
c
t
t
e
e
r
r
i
i
a
a
c
c
a
a
n
n
e
e
l
l
e
e
v
v
a
a
t
t
e
e
i
i
m
m
m
m
u
u
n
n
e
e
s
s
t
t
a
a
t
t
u
u
s
s
a
a
g
g
a
a
i
i
n
n
s
s
t
t
p
p
a
a
t
t
h
h
o
o
g
g
e
e
n
n
s
s
.
.
C
C
-
-
E
E
n
n
d
d
o
o
t
t
o
o
x
x
i
i
n
n
r
r
e
e
l
l
e
e
a
a
s
s
e
e
d
d
b
b
y
y
i
i
t
t
a
a
u
u
g
g
m
m
e
e
n
n
t
t
s
s
h
h
o
o
s
s
t
t
d
d
e
e
f
f
e
e
n
n
s
s
e
e
s
s
b
b
y
y
t
t
r
r
i
i
g
g
g
g
e
e
r
r
i
i
n
n
g
g
t
t
h
h
e
e
a
a
l
l
t
t
e
e
r
r
n
n
a
a
t
t
i
i
v
v
e
e
c
c
o
o
m
m
p
p
l
l
e
e
m
m
e
e
n
n
t
t
p
p
a
a
t
t
h
h
w
w
a
a
y
y
.
.
Harmful effects of normal flora:
It converted in to opportunistic pathogens such as Candida species especially in
immunocompromised person.
It can produce disease in foreign locations with predisposing factors such as
Escherichia coli is normal flora of large in large intestine, while it will be pathogenic
if entered into urinary tract.
Production of an excessive endotoxin may cause shock.
Ubiquitous presence creates problems in establishing accurate diagnosis.
Source of infection:.
1- Human sources: either themselves may be infected or carriers._
2- Animal sources: zoonotic agents like brucellosis, leptosporiosis, rabies,
leishmaniasis.
3- Environmental source:- like inhalation of some fungi s spores such that causes mycetoma, & some
sporing bacilli of genera Bacillus & clostridium.
The source of pathogenic organisms may be either
when they come from outside the patent & in most classical infectious diseases the
:
genous
xo
E
source is exogenous. Or
type of
flora. This
the patient body, usually from his own normal
when they come from
:
Endogenous
infection is important, when trauma or lowered local or general resistance makes the patient
susceptible to attack by the resident parasites
Local resistance is lowered by impaired blood supply, & general resistance by malnutrition,
debilitating disease. such as diabetes, immunosuppressive chemotherapy or radiotherapy or even
other infections such as measles.
-
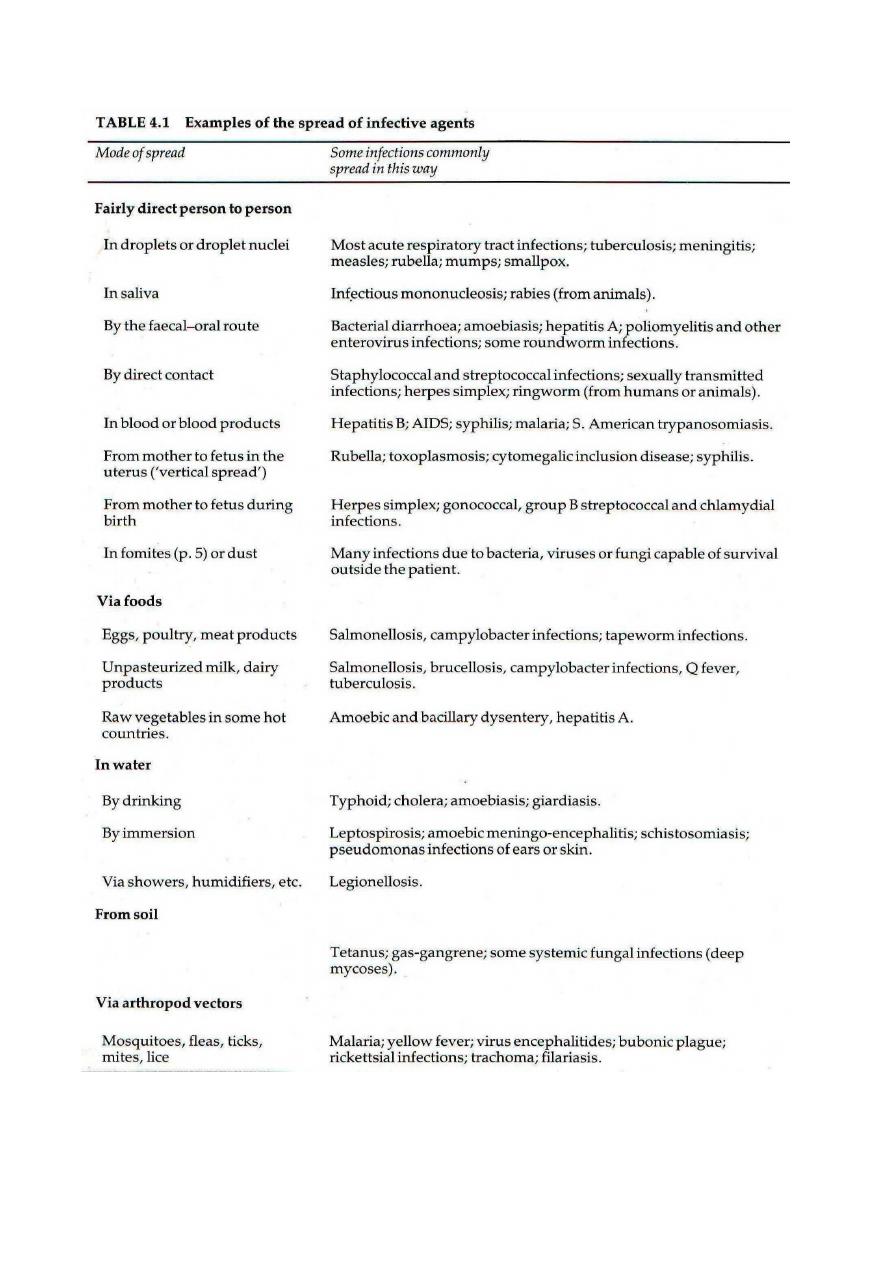
Rout of spread of infection:
BY different modes like:-
1- Contact: -
Direct: such as by kissing or sexual activity or indirect contact via fomites,
contaminated surgical instruments.
2- Inoculation:-
Like inoculation by the bite of an animal ( e.g. rabies) or of an insect vector
( e.g.malari , yellow fever, African trypanosomiasis).
3-Ingestion:- by faecal-oral route of many infectious agents .
4- Aerial spread:
Most acute respiratory infections, the common childhood infectious diseases
( Mumps, Varicella, Measles ), meningococcal meningitis & tuberculosis are
examples of infections spread through the air & acquired by inhalation.
The outcome of infection:
The factors that determine the initiation, development& outcome of infection involve a series of
complex & shifting interactions between the invading organism & the host, which can vary with
different organisms, they include the followings:-
1- The organism ability to breach host barriers & to evade destruction by innate local
& tissue host defences.
2- The organisms biochemical tactics to replicate, to spread, to established infection &
to cause disease.
3- The organism ability to transmit to a new susceptible host.
4- The body innate & adaptive immunological ability to control & to eliminate the
Invading parasite .
Despite the complexity of interaction, host specifity is also remarkable point for example Dogs do
not get measles, nor do human get canine distemper, although the causative agents are closely related
.
easured by the number of organisms
& is m
pathogenicity
is a quantitative measure of
-
Virulence:
required to cause disease. Haemophilus influenza is a common habitant of upper respiratory tract of
human, members of this species regularly cause middle ear infection & sinusitis in children &
bronchitis in smokers, but one variety of H. influenza ( those with capsule type b) can cause systemic
disease( meningitis & epiglottitis) So all H. influenza are pathogenic ,but H. influenza type b is more
virulent.
Lethal dose( LD) is the quantitative dose that to kill half the parasitized pathogen.
Infectious dose( ID) is the number of organisms needed to cause infection in half the hosts, The I.D
of an organism required to cause disease varies greatly among pathogenic bacteria, Enteric diarrhoea
can be caused by Shigella & Salmonella ,but I.D. of shigella is less than 100 organisms, while for
Salmonella is on the order of 100,000 organisms.
The infectious dose of bacteria depends primarily on the virulence factors such as :
1- Pili adherence to mucous membrane.
2- Where they produce exotoxins or endotoxins.
3- Where they poses a capsule to protect them from phagocytosis.
4- Where they can survive various non-specific host defences such as acid in
the stomach.
Virulence factors
: Toxins:-
A- Exotoxins:- they protein molecules can synthesize by number of microorganisms, they are toxic
to their host & are secreted into their environment or are found associated with the microbial surface.
Bacterial exotoxins fall into two broad classes, each of which represents a general pathogenic theme
common to many bacterial species.
A-B exotoxins , these exotoxins are divisible into two domains:
1- B subunit, which is associated with the binding specificity of the molecule( glycoprotein or
glycolipid) to the host cell.
2- A subunit : is the catalytic domain, which enzymatically attacks a susceptible hos function or
structure.
Many of the most potent A-B bacterial toxins are ADP-ribosyltranslating enzymes.
Such as:
izing apparatus of the cells.
affects the protein synthes
pseudomonas exotoxin
Diphtheria toxin,
.
toxin G2 that affect cytoskeleton
Clostridium botulinum
that affect the normal signal transduction activities of the host .
Bordetella pertussis & Vibrio cholera
The natural substrate of the toxin ADP-ribosyltransferases are Guanine nucleotide-binding protein (
G proteins), which are involved in signal transduction in eukaryotic cells..
Immunization against toxin can prevent disease.
Membrane active exotoxin like bacterial hemolysin( cytotoxins) that kill host cell by disrupting the
host cell membranes, also hemolysin may liberate necessary growth factors such as iron for the
invading microorganisms. Other examples to cytotoxins
Are RTX( repeats in toxin), that create membrane pores
& the licthinase α –toxin of Clostridium
perfringens , that disrupt the membrane of leukocytes that might otherwise destroy the organism, &
produce the necrotic environment in which it can multiply..
Differential characteristics of endotoxins & exotoxins
Exotoxins
Endotoxins
Characteristic
1- Part of G
–ve cell outer membrane yes No
2-Most from G +ve bacteria No Yes
3- Usually extra-cellular No Yes
4- Phage or plasmid coded N0 Many
5- Antigenic Weakly yes
6- Can be converted to toxoid No Many
7- Neutralized by antibody Weakly Yes
8- Different pharmacological No Yes
Specificities
9- Stable on boiling Yes No *
* Enterotoxin of Staphylococcus aureus withstands boiling.

Microbial Genetics:-
Genetics:- defines & analyzes heredity, or constancy & change in the vast array of physiologic
functions that form the properties of organisms .
Gene:-
is the unit of heredity, it’s a segment of DNA that carries in its nucleotide sequence
information for specific biochemical or physiologic property.
Traditional microbial genetics is based largely upon observation of growth.
Phenotypic variation has been observed on the bases of a gene capacity to permit growth of under
condition of selection; e.g., a bacterium containing gene that confers resistance to ampicillin can be
distinguished from a bacterium lacking the gene by its growth in the presence of antibiotics which
serves as the agent of selection.
In order to complete this process as selection it requires expression, which under appropriate
conditions can be observed at the level of phenotype.
Microbial genetics has revealed that genes consist of DNA. Subsequent of bacterial investigations
revealed the presence of restricting enzymes that cleave DNA at specific sites giving rise to DNA
restriction fragments. Also the introduction of DNA restriction fragment to plasmid (Small genetic
elements capable of independent in bacteria & yeast) allows the fragment to be amplified many time,
this process can be achieved through Polymerase chain reaction ( PCR) testing.
DNA within such regions can be placed under control of high expression bacterial promoters that
allow encoded proteins to be expressed at high level.
Therefore bacterial genetics hastened
development of genetic engineering (A technology that has introduced tremendous advance into the
field of medicine.
The structure of DNA & RNA:-
Most DNA molecules are Double strand ( DS) with complementary double bases
( A-T;G-C) that enables one strand to provide the information for copying or expression of
information in the other strand, the base pairing in double helix determine its genetic information.
The length of DNA molecule is usually expressed in 1000 base pairs ( kilo base pairs{kbp} ), DNA
molecule of small virus contain 5kbp, while Esherichia coli chromosome is about 4000 kbp, each
base pair is separated from the next about 34 angstrom ,so the length of E.coli chromosome is about
one millimetre ( mm).
RNA most frequently occurs in single strand( ss), with complementary bases (A-U ,G-C)A few
RNA molecules have been shown to function as enzymes. The most general function of RNA is
communication of DNA gene sequences in the form of messenger RNA*( mRNA) to ribosome.
Within ribosomes, which contain ribosomal RNA( rRNA) messages are translated into amino acid
structure of proteins via transfer RNA( tRNA).
RNA molecules range in size from small tRNA, which contain fewer than 100 bases to mRNA
which carry genetic messages extending to several thousand bases.
Bacterial ribosomes contain three kinds of rRNA with respective size of 120, 1500 &
2900 bases.
The need for expression of individual genes changes in response to physiologic demands,&
requirements for flexible gene expression are reflected in the rapid metabolic turnover of most
mRNA. On the other hand tRNA & rRNA which are associated with the universally required
function of protein synthesis tend to be stable.
The prokaryotic genome:-
Most prokaryotic genes are carried on the bacterial chromosome, a single circle containing about
4000 kbp of DNA. Additional genes are on plasmid that range in size from several to 100 kbp.
DNA circle that contain chromosome & plasmid, which contain genetic information necessary for
their own replication called replicons. Bacterial genes are haploid.
Plasmids carry genes associated with specialized following functions:-
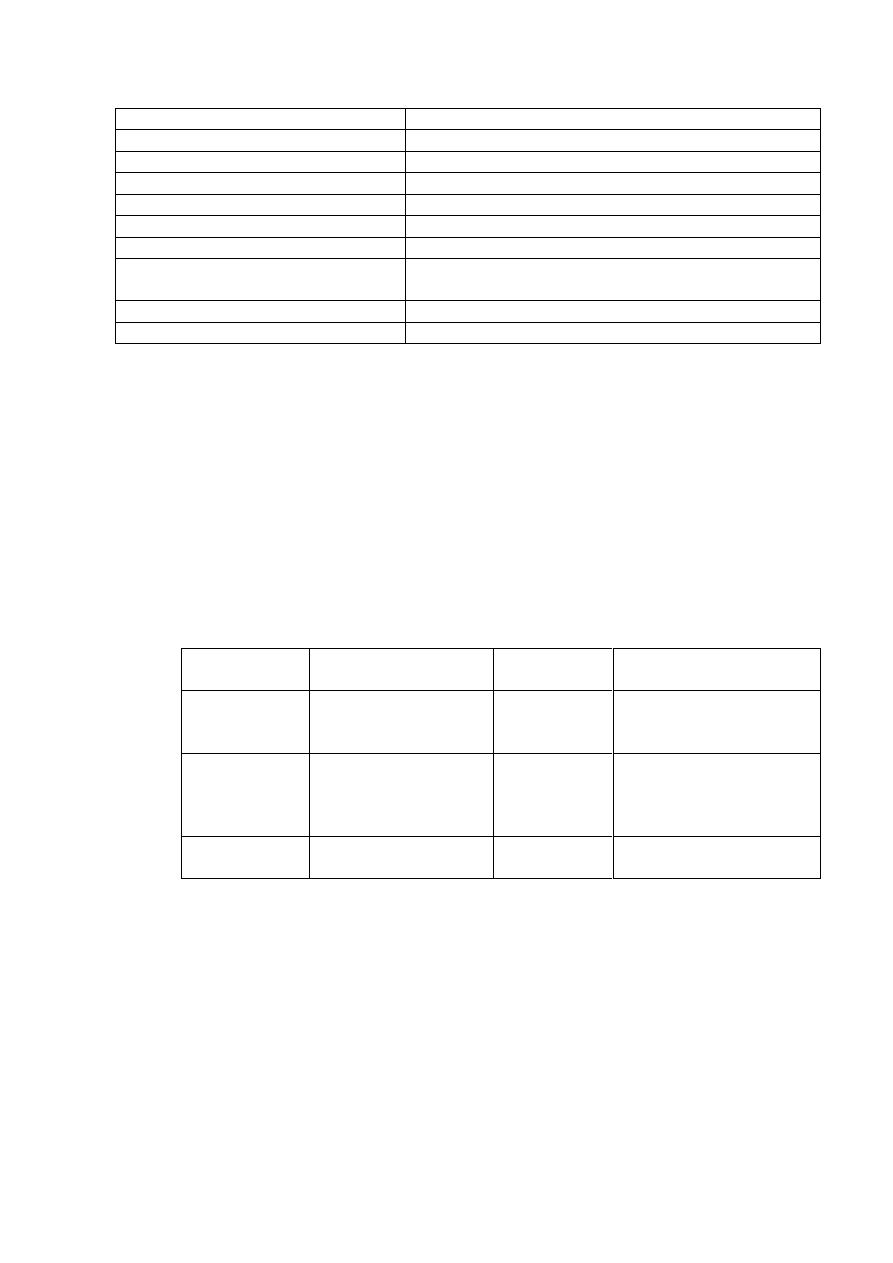
Activity
Organism
Degradation of champor, toluene, octane, salicylic acid
Pseudomonas species
∞-amylase
Bacillus stearothermophilus
Utilization of H2 as oxidizable energy source.
Algaligenes etrophus
Sucrose uptake & metabolism, citrate uptake
Escherichia coli
Nitrogen fixation
Klebsiella species
Lactose utilization, galactose phosphotransferase
system, citrate metabolism
Streptococcus ( group N)
Synthesis of photosynthetic pigment
Rhodospirillum rubrum
Nylon degradation
Flavobacterium species
Transposons
are genetic elements that contain several kbp of DNA, including the information
necessary for their migration from one gene genetic locus to another.
Simple transposons( insertion sequences) carry only this genetic information,
while complex transposon carry genes for specialized functions such as antibiotic
resistance & are close or flank to insertion sequences.
Transposon replication depends upon their replicon , so detection of genetic exploitation of
transposon is achieved by selection of specialized genetic information( normally resistance to an
antibiotic( that they carry.
Transferring of DNA between bacterial cells:-
From the medical view, the consequence of DNA transfer is that antibiotic resistance genes are
spread from one bacterium to another by the following processes:-
Conjugation, transduction & transformation .
Nature of DNA transfered
Type of cells
involved
Process
Transfer
procedure
Chromosomal or plasmid
Prokaryotic
DNA transferred from
one bacterium to
another
Conjugation
Any gene in generalized
transduction; only certain
genes in specialized
transduction
Prokaryotic
DNA transferred by
virus from one cell to
another
Transduction
Any DNA
Prokaryotic or
Eukaryotic
Purified DNA taken by
a cell
Transformation
1- Conjugation process is controlled by F(fertility ) plasmid ( F factor ) ,which carry the
genes for proteins required for conjugation. Most important protein is pillin, which form sex pilus (
conjugation tube).
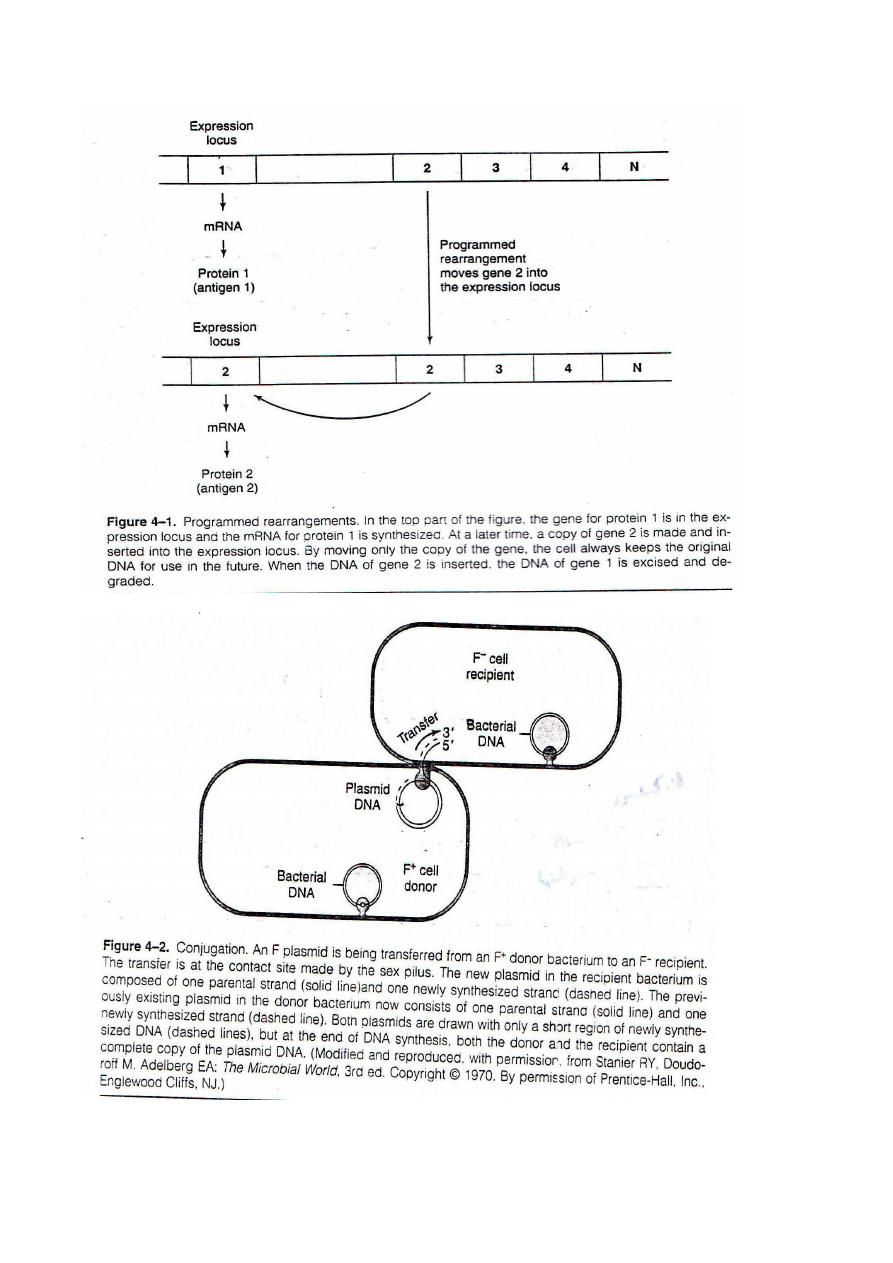
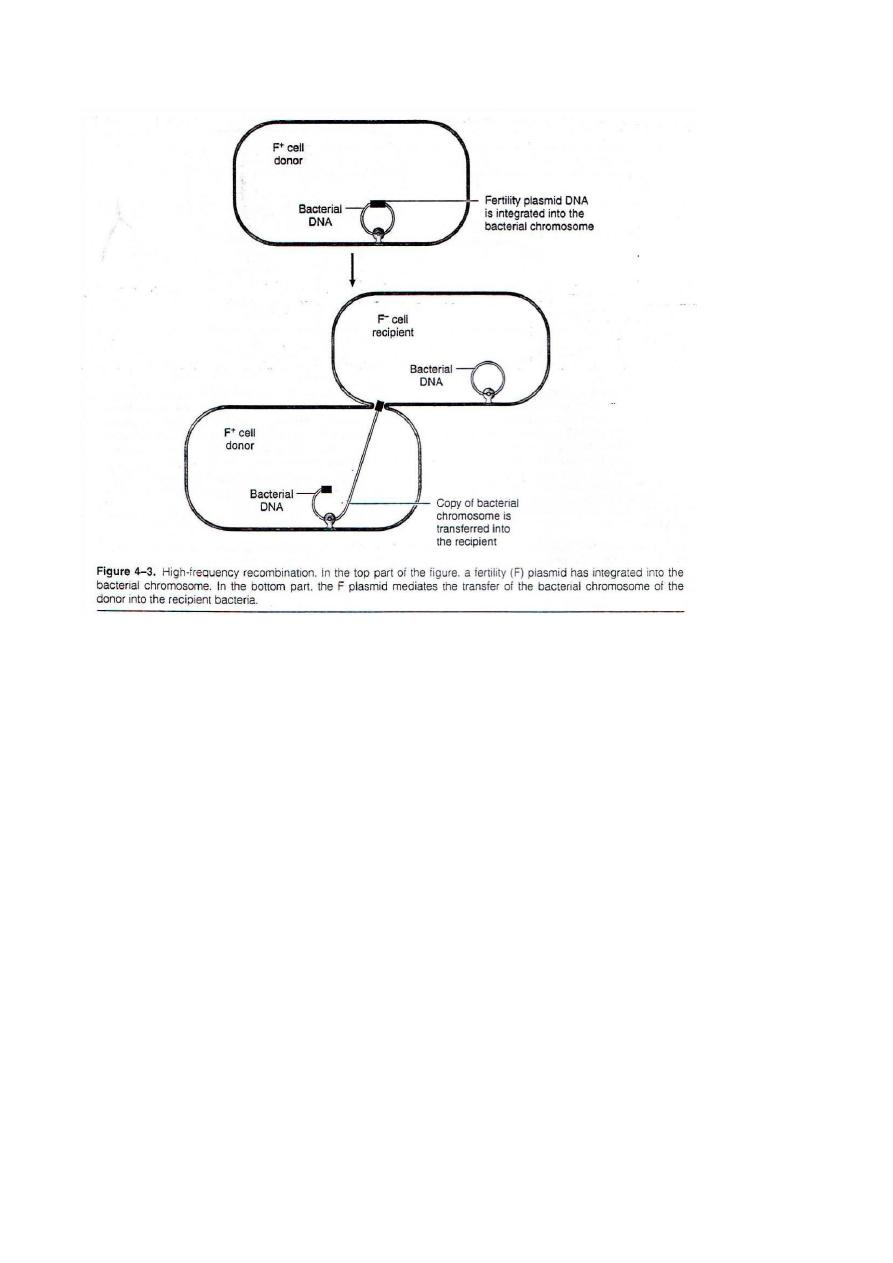
2-Transduction:-
During the growth of the virus within the cell, a piece of bacterial DNA incorporated virus particle &
is carried into recipient cell at the time of infection, within the recipient cell the phage DNA can
integrate into the cell DNA & the cell can acquire a new trait, this process called
lysogenic
conversion
. This process can change a non pathogenic organism into a pathogenic
one. Erythrogenic toxin ( Streptococcus pyogenes),Diphtheria toxin (
Corynebactreium diphtheriae) , botulinum toxin (Clostridium botulium)& Cholera
toxin ( Vibrio cholera) are encoded by bacteriophage & can be transferred by
transduction.
Transduction is two types:-
1- Generalized transduction:- occurs when the virus carries a segment from any part of the bacterial
chromosome.
2- Specialized transduction: occurs when the bacterial virus DNA that has integrated into the cell
DNA is excised & carries with it an adjacent part of the cell DNA. Since most lysogenic (temperate)
phages integrate at the specific sites in the bacterial DNA, the adjacent cellular genes that are
transduced are usually specific to that virus.
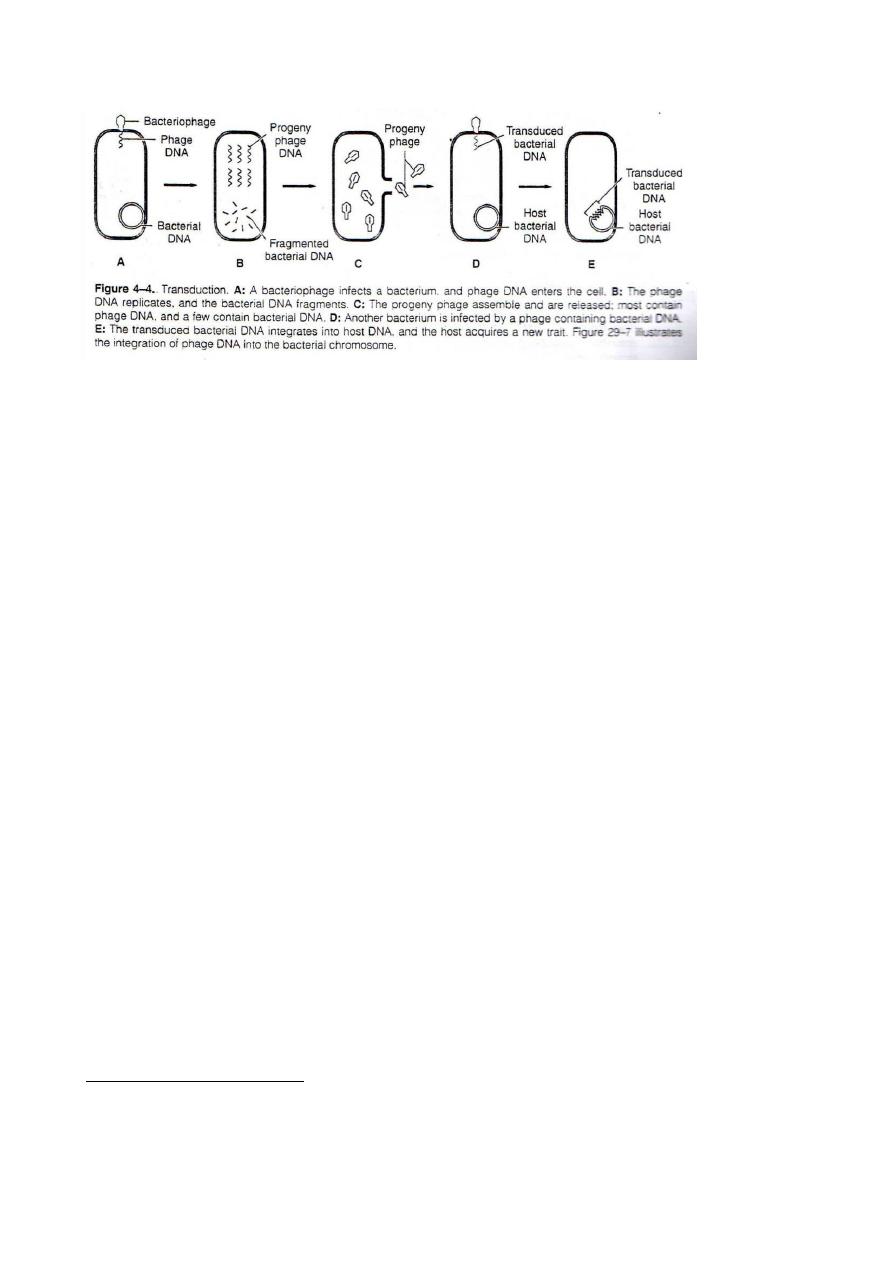
3- Transforming:-
This process is frequently used in genetic engineering ( like the extracted DNA from non-capsulated
diplococcus pneumoniae could transform non-encapsulated rough pneumococci into encapsulated
pneumococci. This phenomenon demonstrates that the transforming principle was DNA marked the
first evidence that DNA was the genetic material.
Transformation occurs :-
A- In nature, dying bacteria may release their DNA, which may be taken up by the recipient cells.
B- In the laboratory: When purified DNA is injected into the nucleus of eukaryotic cell.
DNA recombination:-
After DNA transformation by one of the three processes, which described above, it can integrate
into the host cell chromosome by recombination, which can be seen in two types:-
A- Homologous recombination: in which two pieces of DNA those have extensive homologous
regions pair up & exchange pieces by the process of breakage & reunion.
B- Non-homologous recombination: - in which little, if any homology is necessary.
In these two types different enzymes are involved (because different genetic loci govern these
processes). Although it is known that a variety of endonucleases & ligases are involved, but the
precise sequence of events is unknown
.
Epidemiology of infectious diseases:-
Communicability:-
Non-communicable infections:- Are those that are not transmitted from human to human & include:-
1- Infections derived from the patient's normal flora, such as peritonitis after rupture of appendix.
2- Infections caused by the ingestion of preformed toxin such as botulism.
3- Infections caused by certain organisms found in the environment, such as clostridial gas gangrene
4- Some zoonotic infections (diseases transmitted from animal to human) such as rabies &
brucellosis are not transmitted between man.
they do not lead to
, &
not spread from person to person
: are
infections
ble
communica
-
Non
secondary spread, but can occur as common source outbreaks.
Communicable infections: Require that an organism be able to leave the body in a form that is
directly infectious like influenza virus, or is able to become so after development in a suitable
environment.
Communicable infections can be endemic, epidemic or pandemic.
Incubation period:-
is the time between exposure to the organism & appearance of first symptoms
of the disease. It depends on the inherent infectivity, virulence & mode of multiplication of the
microorganisms, so such has short incubation period like gonorrhea & influenza ( 2 to 4 days ) ,
hepatitis B virus may vary from a fewe weeks to several months..
Some diseases have even more prolonged incubation periods because:-
1-Slow passage organism to the target organ as in rabies.
2- Slow growth of the organism as in tuberculosis.
Routes of transmission:-
In general infectious agents' transmission can be accomplished by:-
-
Vertical transmission:
-
1
Such as the ability of some micro-organisms to cross the placental barriers & infect the fetus, if the
mother is infected during pregnancy . The infant may die, or be born with the typical disease or may
suffer congenital damage, particularly if the infection occurred during first trimester of pregnancy.
Of particular concern are rubella, syphilis, toxoplasma & cytomegalovirus .
-
Horizontal transmission:
-
2
Direct or indirect from person to person . It can be seen in the followings:-
1- Respiratory spread is by aerosolization of respiratory secretions with subsequent inhalation by
others such as common cold agent & tuberculosis.
2- Salivary spread; Such as herpes simplex & infectious mononucleosis.
3- Fecal-oral spread: such as enterovirus infection (stool to hand to mouth ) or hepatitis A virus (
stool, object ,mouth) & salmonelosis , shigellosis ( stool, water or food to mouth ). Reduced gastric
hydrochloric acid facilitates enteric infections.
4- Skin to skin transfer: such as Treponema palladium, the causative agent of syphilis, group A
streptococci that cause impetigo & ring worm by dermatophyte fungi.
5- Blood borne transmission:- such as HIV, Hepatitis B & C viruses & others.
6- Eye to eye transmission:- Infections of the conjunctiva may occur in epidemic disease such as
adenovirus & haemophilus. While trachoma caused by Chlamydia is an example to endemic eye
transmission by using fomites, unsterile ophthalmologic instruments.
7- Zoonotic transmission:- from animal to human by different ways, in rabies by the bite of dog &
bite of rodent flea may produce pneumonia.
-
Epidemics:
The following quantitative measures can recognize the epidemics:-
Infectivity:-
In epidemiological terms ,equates to attack rate & is measured as the frequency with
which an infection is transmitted when there is contact between the agent & a susceptible individual.
Disease index:-
Of an infection can be expressed as the number of persons who develop the disease
divided by the total number infected.

Virulence: of
an infection can be estimated as the number of fatal or sever cases per total number of
cases.
Incidence:-
The number of new cases of a disease within a specific period.
Prevalence:- Total number of cases existing in a population at risk a point in time.
Incidence & prevalence rates are usually expressed as number of cases per 100, 1000 or 100000
population.
Sudden appearance of new agents can result in pandemic spread.
Social ecological factors determine aspects of epidemic diseases.
Nosocomial infections have role in increasing epidemic rate of such disease.
Control of epidemics:-
1- By recognition of an epidemics, identification& studied to determine rout of
transmission ( eg : food poisoning).
2- To control spread & development of further infection by following methods:
A- Blocking the route of transmission if possible.
B- Identifying & treating infected persons & carriers.
C- Raising the level of immunity in the uninfected population by immunization.
D-Selecting the chemoprophylaxis for subject or populations at particular risk of
infection.
E- Correcting & improving people conditions from different sites.
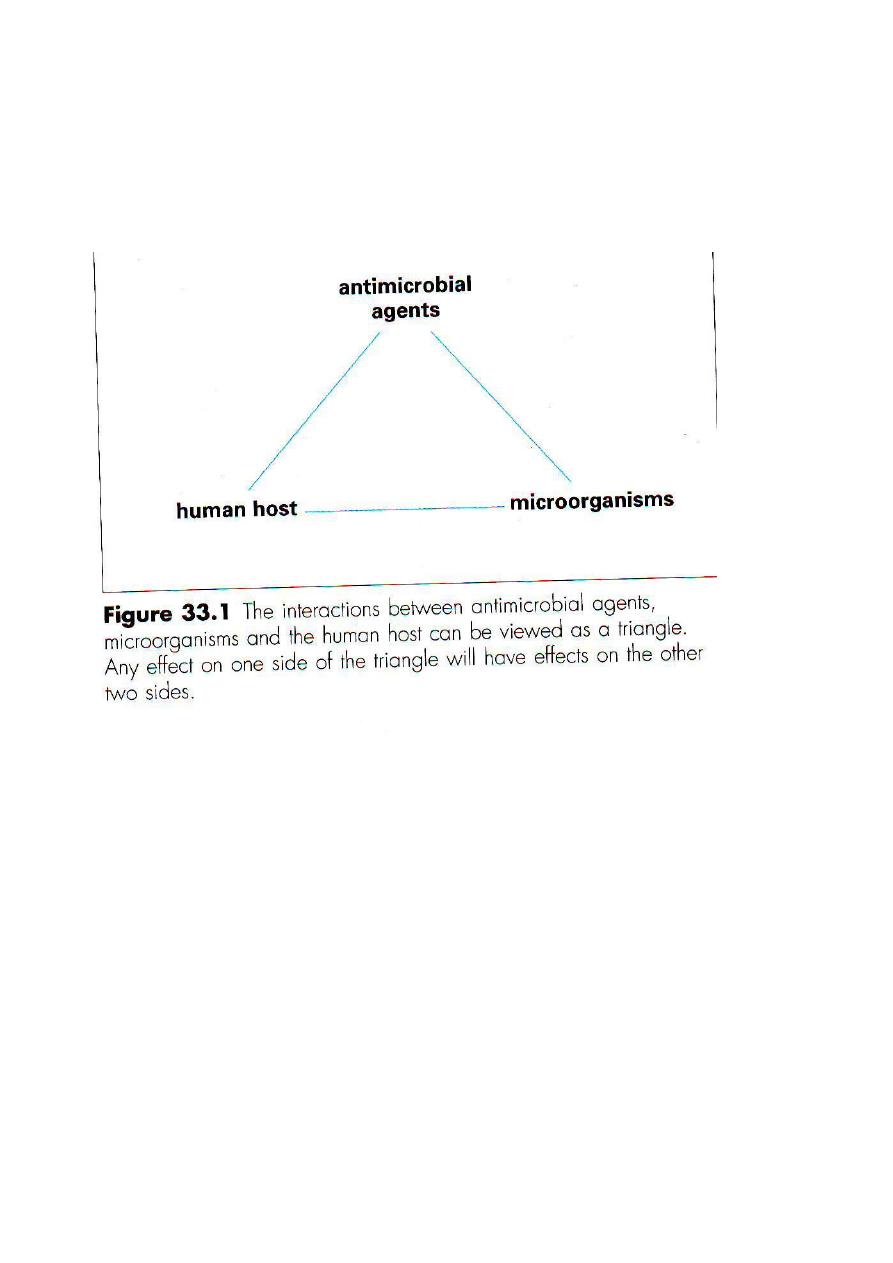
Lecture No.6 Dr. Yahya G.Salman.
Antibacterial & antiviral agents:-.
The interaction between host, microbial pathogen & antimicrobial agent can be
considered as a triangle & any alteration in one side will inevitably affect other two
sides.
Ideally, selective toxicity is based on the ability of an antimicrobial agent to attack a
target present in bacteria but not humans.
Definitions:-
Antibiotic:- Antimicrobials of microbial origin, most of which are produced by fungi,
or by bacteria of the genus Streptomysis.
Antimicrobial, antimicrobic :- Any substance with sufficient antimicrobial activity that
it can be used in treatment of infectious diseases.
Bactericidal: - An antimicrobial that not only inhibit growth but is lethal to bacteria.
Bacterostatic:- An antimicrobial that inhibits growth but does not kill the organisms.
Chemotherapeutic:- A broad term that encompasses antibiotics, antimicrobials & drug
used in the treatment of cancer.
Minimal inhibitory concentration (MIC):- The laboratory term that defines the lowest
concentration (µg/ml) able to inhibit growth of microorganism.
Resistant:- Organisms that are not inhibited by clinically achieved concentration of a
antimicrobial agent.
Susceptible:- Term applied to mocroorganisms indicating that they will be inhibited by
concentration of the antimicrobic that can be achieved clinically.
Spectrum:- An expression of the categories of microorganisms against only a few
organisms.
Narrow spectrum agent has activity against few organisms, while broad spectrum
agent has activity against organisms of diverse types ( G+ve & G
–ve bacteria).
Desired properties of a new antimicrobial agent:
Antimicrobial properties & pharmacologic properties of antibiotic for the host have to
be considered when a new design is desired.
-
Antimicrobial properties:
1- It is selective for microbial rather than mammalian targets.
2- It should have cidal activity (antibacterial &antifungal agents).
3- with slow emergency of resistance.
4- Narrow spectrum of activity.
-
ivities:
Pharmacologic act
1- Non toxic to the host.
2- Long plasma half life.( once a-day dosing).
3- Good tissue distribution including CSF.
4- Low plasma protein binding.
5- Oral & parental dosing forms.
6- No interference with other drugs.
Source of antimicrobial agents:-
1- Antibiotics are synthesized by molds or bacteria.
2- Production of quantities is by industrial fermentation.
3-Chemicals with antibacterial activity are discovered by chance as the result of
screening programs.
4- Naturally occurring antimicrobics can be chemically modified.
Classification of antibacterial agents:-
There are three ways of claasfying anitimicrobial agents:
1- According to whether they are bactericidal or bacteriostatic.
The distinction between them is blurred because some agents are capable of killing
some species, but are only bacteriostatic for others, e.g. chloramphenicol inhibits
growth of Esch. Coli, but kills Haemophilus influenzae.
2- By target sites:-
There are five main target sites for antibacterial action (mechanism of action):-
A- Inhibition of cell wall synthesis.
B- Inhibition of protein synthesis.
C- Inhibition of Nucleic acid( by inhibiting of translation & transcription).
D- Inhibition of cell membrane function.
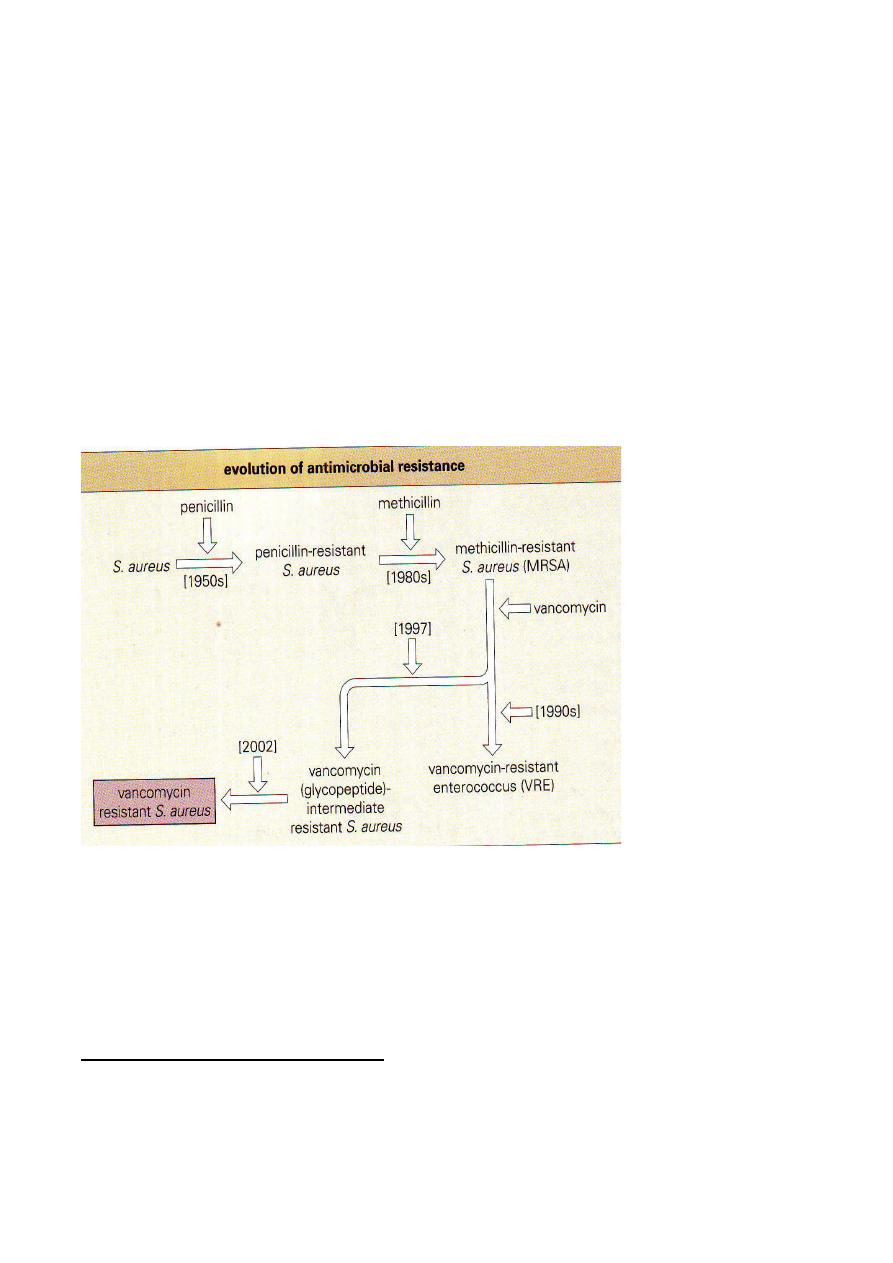
E- Inhibition of metabolic pathways.
3- Antibacterial chemical structures.
According to chemical structure alone is not of practical use, because there is such
diversity.
Combination of target sites & chemical structure provides a useful working
classification to organize antibacterial agents into specific families
Resistance to antibacterial agents:
1- Chromosomal mutation may result in resistance to a class of antimicrobial agents (
cross- resistance).
2- Genes on transmissible plasmids may result in resistance to different classes of
antimicrobial agents (Multiple resistances).
£- Resistance may be acquired from transposons & other mobile elements.
Drug inactivation:-
Enzymes that modify or destroy the antimicrobial agent involves:
1- Beta-lactamase.
2- Aminoglycosides- modifying enzymes.
3- Chloramphenicol acetyl transferases.
:
** Inhibitors of cell wall synthesis
Peptidoglycan , a vital component of the cell wall, is a compound unique to bacteria &
therefore provides an optimum target for selective toxicity. Synthesis of peptidoglycan
precursors starts in the cytoplasm; wall subunits are then transported across the

cytoplasmic membrane & finally inserted into growing peptidoglycan molecule. Cell
wall synthesis is inhibited by
A-Beta lactams drug, the largest group.
B- The glycopeptides (include vancomycin & teicoplanin that must be given by
injection for systemic infections they are active only against Gram positive organism
Also included other such as:
Bacitracin( primarily used topically) : prevents dephosphorylation of phospholipids
carrier, which prevents regeneration of carrier necessary for synthesis to continue.
Cycloserine: inhibits reactions involved in incorporation of alanine into cell wall
precursor.
Side effects:
The glycopeptides are potentially ototoxic & nephrotoxic.
Beta-lactams:-
A very large family of different group of bactericidal compounds all containing the
beta lactam ring that inhibit cell wall synthesis by binding to penicillin-binding
proteins ( PBPs).
PBPs are membrane proteins ( e.g. carboxipeptidase, transglycosylases &
transpeptidases) capable of binding to penicillin( hence the name of PBP). And are
responsible for final stages of cross-linking of the bacterial cell wall structure .
Inhibition of one or more of these essential enzymes results in an accumulation of
precursor cell wall unit, leading to activation of the cells autolytic system & cell lysis.
Members of the beta-lacta family:-
1- Penicillins: such as:
Benzylpenicillin, cloxacillin,flucloxacillin, ampicillin, amoxicillin, carbenicillin,
ticarcilin,azlocilin,mezlocilin & pipracillin.
2- Cephalosporins:- such as:
Cefalexin, cefaclor, cefadroxilm, cefuroxime, cefamandol, cefotaxime, ceftazidame,
cefepime & cefpirome.
3- Cefamycins: such as cefoxitin.
4- Carbapenems: such as imipenem.
5- Monobactams: such as aztreonam.
Also they can be classified into generation as first to fourth.
Side effects: Toxic effects of beta-lactam drugs include mild rashes & immediate
hypersensitivity reactions.
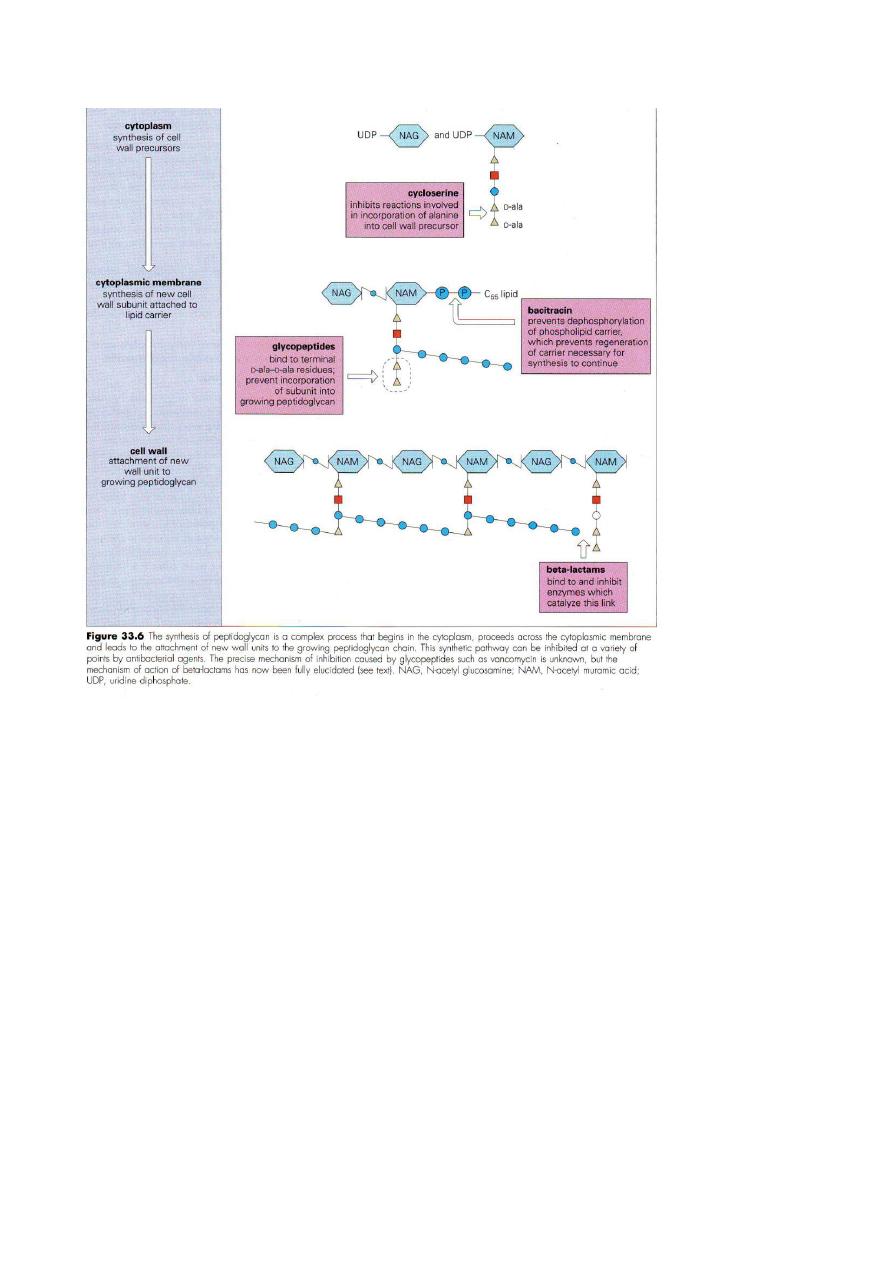
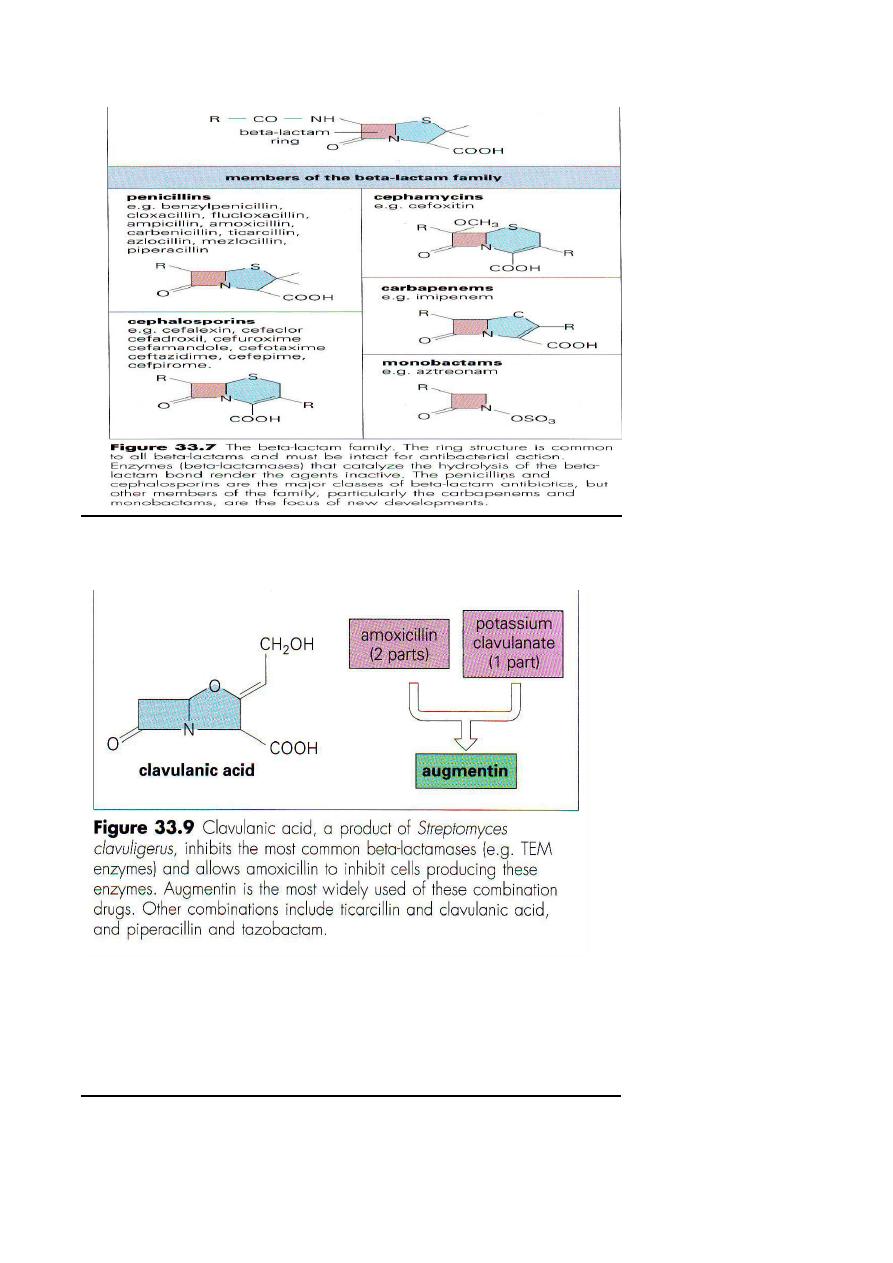
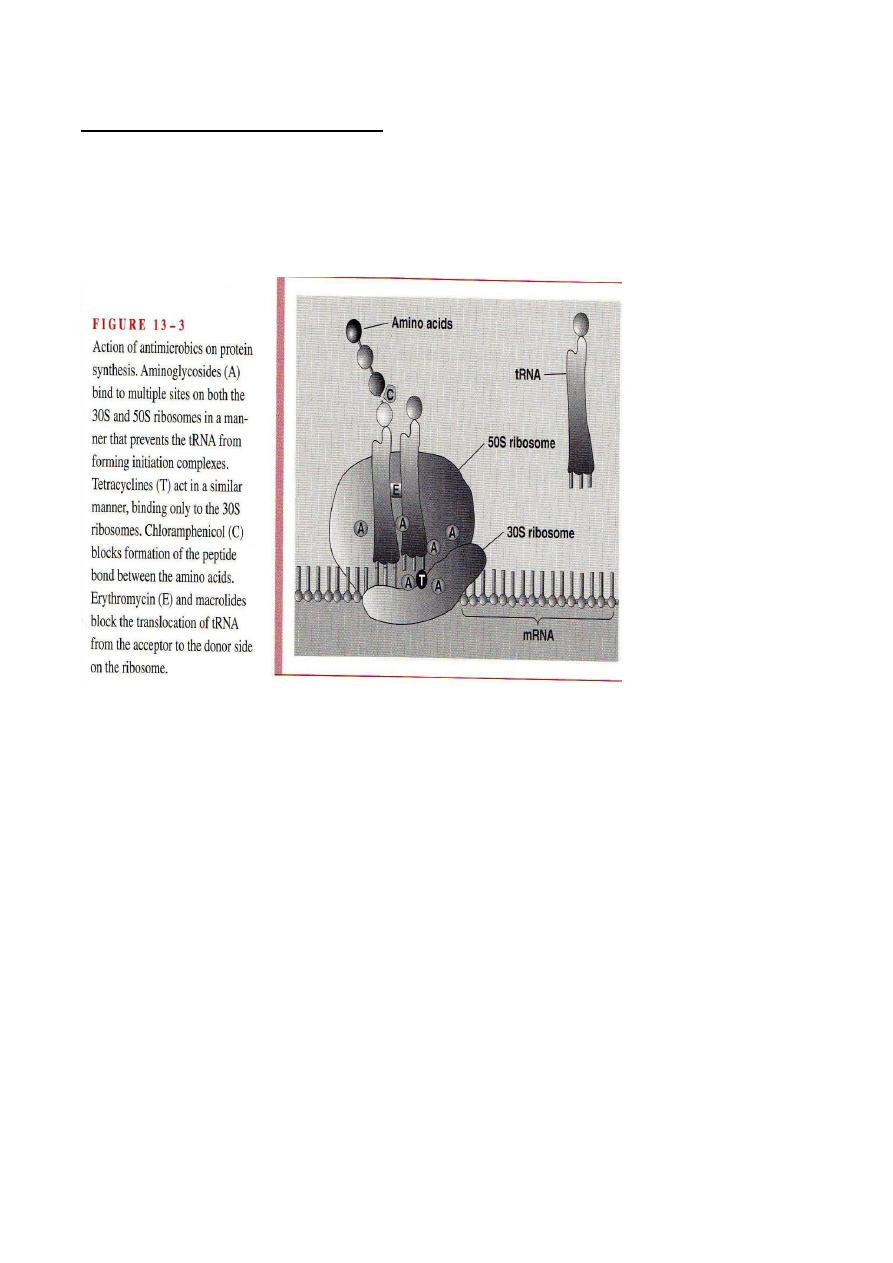
* Inhibitors of protein synthesis:
*
A member of different group of antibacterial agent act by inhibiting proteins with
specific reaction on the 30S subunit of the ribosome like aminoglycosides &
tetracyclines , also that act on the 50S subunit such as lincosamides, erythromycin,&
fusidic acid. Where they interfere with the binding of formylmethionyl= transfer
RNA( fmet-tRNA) to ribosome ,thereby preventing the formation of initiation
complexes from which protein synthesis proceeds.
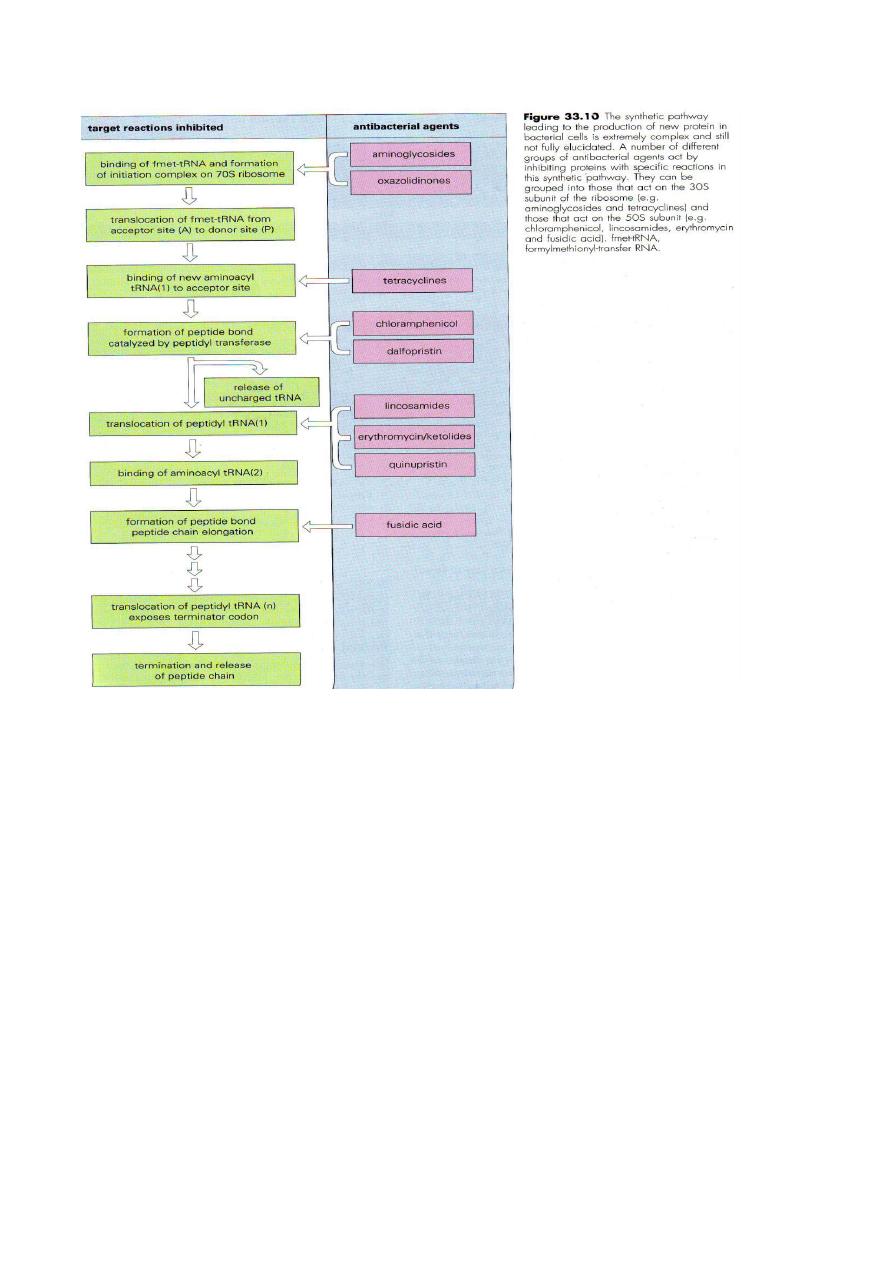
Aminoglycosides are important agents active against G-ve facultative bacteria & are
often used in combination with betalactams to broaden the spectrum to include
streptococci & some anaerobes, which are not susceptible to aminoglycosides alone.
Resistant to aminoglucosides particularly among enterobacteria & staphlylococci is
mediated by the production of aminoglycoside-modifying enzymes, which react with
groups on the aminoglycoside molecule to yield an alterd aminoglycoside product.
This competes with the unmodified aminoglycoside for uptake into the cell & binding
to the ribosome.
Aminoglycosides are used only in sever life-threatening infections such as:
a- G-ve septicaemia( including Pseudomonas ) Usually in combination with
beta-lactam.
b- Septicaemia of unknown aetiology arising forms:
Hospital acquired infection, malignancy, immunosuppressive therapy, major trauma,
major surgery or burns, intravenous catheter, urinary catheter, extremes of age.
C- Bacterial endocarditis for synergy with beta-lactam.
d- Staphylococcus aureus septicaemia in combination with beta-lactam.
e- Pylonephritis for difficult cases.
h- Post surgical abdominal sepsis in combination with anti-anaerobe therapy.

Tetracycline's:-
*Are bacteriostatic compounds that differ mainly in their pharmacological properties
rather than their in their antibacterial spectra.
*They are a family of large cyclic structures that have several sites for possible
chemical substitutions.
* Tetracyclines are active against a wide variety of bacteria such as mycoplasma,
Chlamydia & rickesttsiae, but their use is restricted due to widespread resistance.
*Tertacyclines should be avoided in pregnancy & in children less than 8 years, also
interference with bone development & brown staining of teeth occurs in fetus & in
children. Systemic administration may cause liver damage.
** Tetracyclines inhibit protein synthesis by binding to the small ribosomal subunit
in ammanar thast prevents amino-cyletransfer RNA from entering the acceptor
sites on the ribosome
Type of tetracyclines:
Tetracycline, chlortetracycline, oxytetracycline,doxycycline,minocycline &
tigecycline.
Chloramphenicol:
* It contains a nitrobenzene nucleus & prevents peptide bond synthesis, with a
bacteriostatic result.
*Chloramphenicol has affinity for the large ( 50S) ribosomal subunit where it
blocks the action of peptidyl-transferase, thereby preventing peptide bond system
synthesis.
* The drug has some inhibitory activity on human mitochondria ribosomes( which
are also 70S), which may account for some of the dose-dependent toxicity to bone
marrow. Also it is toxic to neonate( premature babies) whose liver enzyme systems
are incompletely developed, this can result in gray baby syndrome.
* Resistance to chloramphenicol is mediated in G-ve bacteria by production of a
chloramphenicol acetyl transferase enzyme, which catalyzes the addition of acetyl
groups to the chloramphenicol molecule which inactive lead to failure binding to
the ribosome target.
* Chloramphenicol has been used in treatment of bacterial meningitis (particularly
H. influenzae) since the drug achieves satisfactory concentrations in the CSF. Also
it is active against a wide variety of G+ve & G-ve bacteria( such as Salmonella ),
aerobes & anaerobes including intracellular organisms( like Chlamydia &
rickettsiae) .
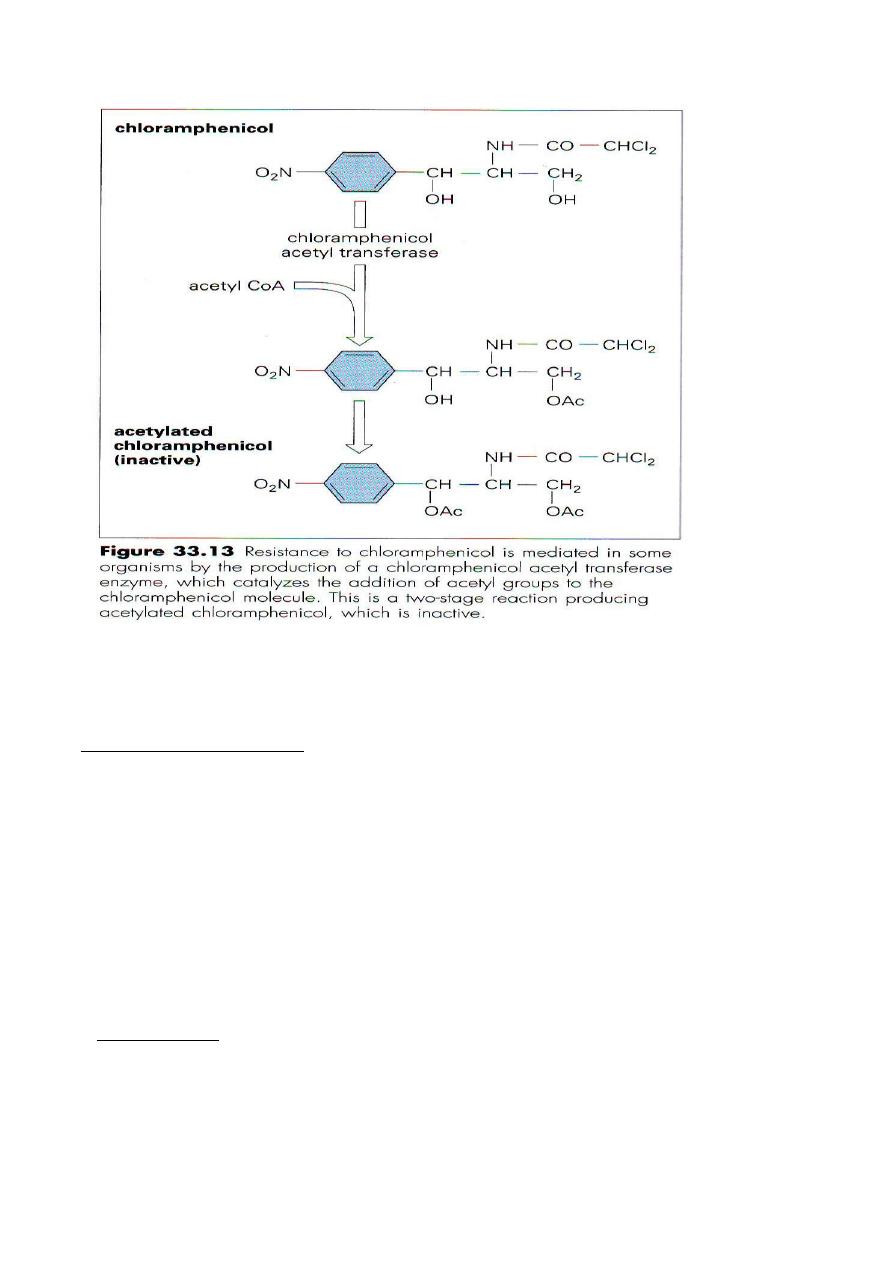
Macrolide
s, lincosamides & streptogramins:
Are 3 groups of antibacterial agents sharing overlapping binding sites on ribosomes
& resistance to macrolides confers resistance to the other 2 groups.
The clinically important drugs are :-
& bacteriostatic
that posses a macrocyclic lactone ring
Macrolides erythromycin
*
in activity. New agents involve:
Roxithromycin. Azithromycin( improved against G-ve bacteria),
clarithromycin(improved Against G+ve bacteria & Legionella sPP. &
telithromycin(also called ketolides that improved actively against respiratory
pathogens including Streptococcus pneumoniae).
** Erythromycin binds to the 23S ribosomal RNA in the 50S subunit of the
ribosome & blocks the translocation step in protein synthesis, thereby preventing
the release of tRNA after peptide bond formation.
Spiramycin is another macrolids used in the preventing of congenital
toxoplasmosis.
Lincosamides:
*
Clindamycin: is a chlorinated more active derivative of lincomycin, which inhibit
peptide bond formation in the same manner or erythromycin.
It is more active against anaerobes, both G+ve ( Clostridium sPP), G-ve (
bacteriodes). Pseudomembranous colitis caused by Cl. difficile follows treatment
with clindamycin .
Clindamycin penetration into bone makes it a valuable drug in the treatment of
osteomyelities . Clindamycin is not active against aerobic G-ve bacteria, because of
poor penetration of the outer membrane.
-
Streptogarmins:
*
Its formulation currently available as a mixture of A compound of dalfopristin &
B compound of quinupristin, that are bacteriostatic individually but synergistically
bactericidal in combination. Both compound bind to 23SRNA in the large 50S
ribosomal subunit, both compound interfere with elongation & extension of peptide
chains.
Quinupristin-dalfopristin is administrated intravenously & primarily metabolized in
the liver. This drug is active against G+ve bacteria, specially against Enterococcus
faecium but not E. faecalis.
-
Oxazolidinones:
-
*
Is a new class of synthetic bacteriostatic antimicrobial agents. Linezolid currently
available is active against a wide range of G+ve bacteria, including multi-resistant
strains. This drug inhibits protein synthesis by targeting 23S rRNA in the 50S
subunit in a manner which prevents formation of a functional 70S complex.
-
Fusidic acid:
*
Is a steroid-like compound ( bacteriostatic) that inhibits protein synthesis by
forming a stable complex with elongation factor EF-G ( the bacterial equivalent of
the human EF-2) Guanosine diphosphate & the ribosome. It is administrated orally,
IM & topically.
Fusidic acid is a treatment for staphylococcus infections, but should be used with
other anti-staphylococcal drugs to prevent emergence of resistance.
Occasionally, fusidic acid causes jaundice & gastrointestinal upset.
Inhibitors of Nucleic acid synthesis:
It occurs in different stages in nucleic acid synthesis & function, they involve:-
1- Inhibitor of DNA replication such as Quinolones.
2- Inhibitors of RNA polymerase such as refampicin.
3- Anti-metabolites inhabiting precursor synthesis such as sulfonamides,
trimethoprim.
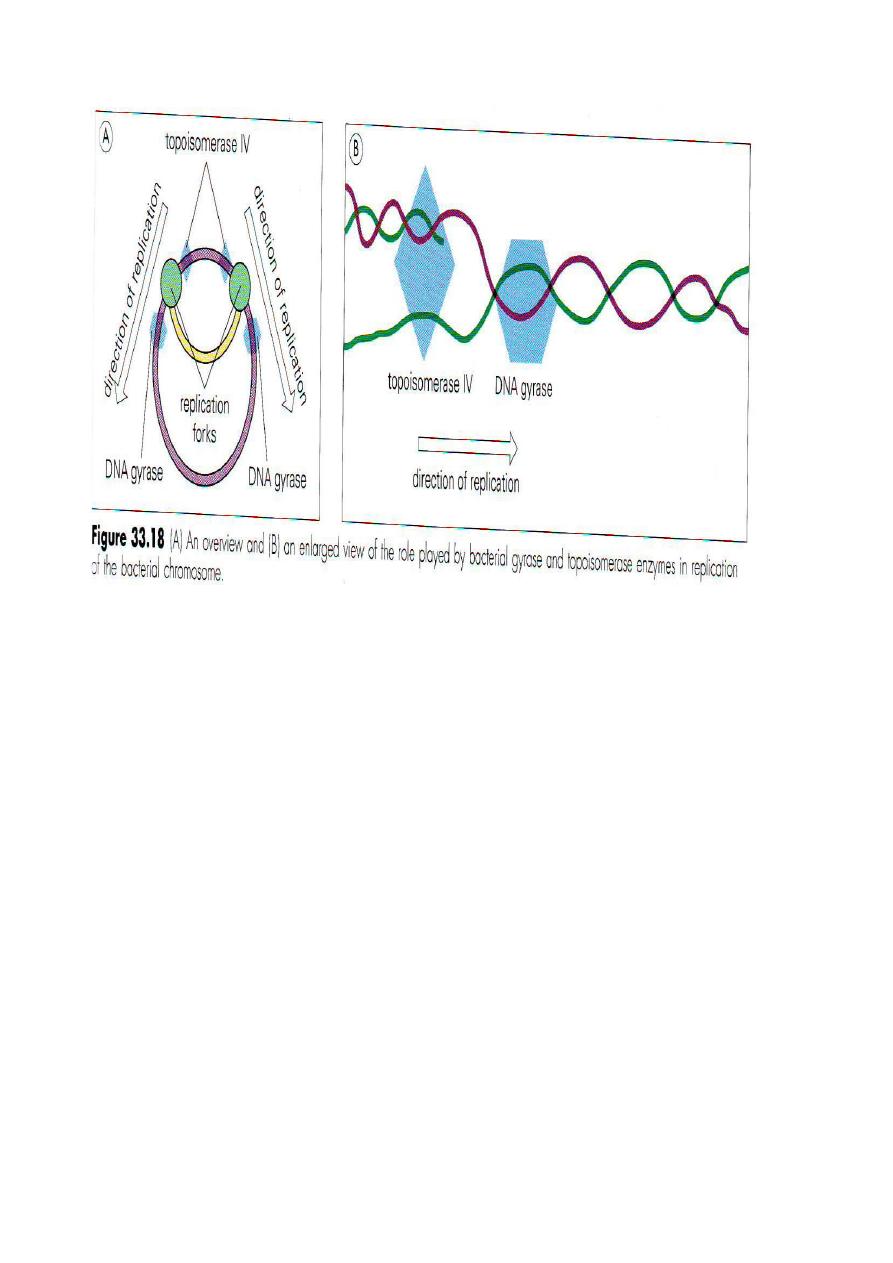
-
َ
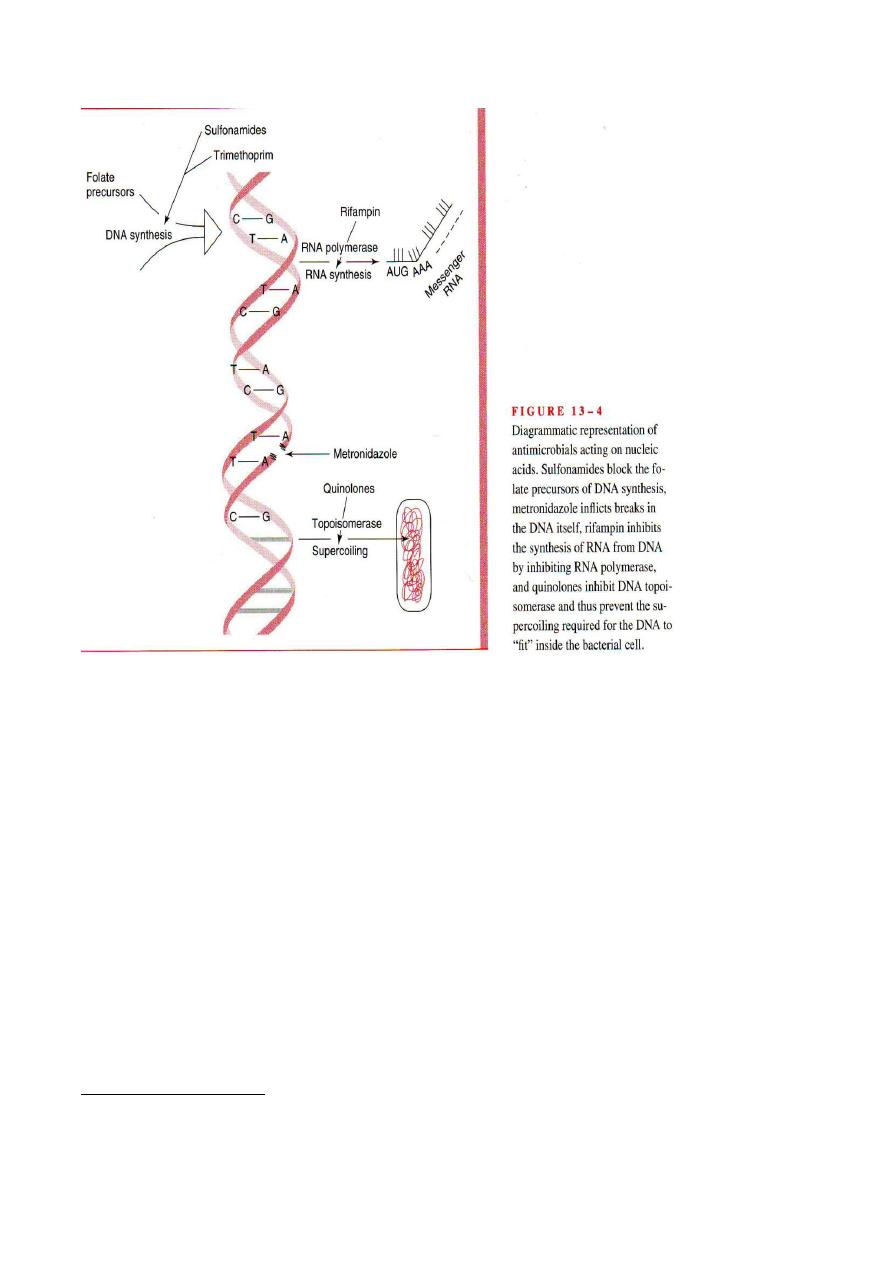
Quinolones:
Are bactericidal synthetic agents that interfere with replication of the bacterial
chromosome. Can be grouped generally into following:-
1-
First generation: Naldixic acid( common name Negram): generally active
against G-ve bacteria( excluding pseudomonas).
2
- Second generation: Ciprofloxacin,Enoxacin,tomefloxacin,Norfloxacin &
Ofloxacin.
Active against G-ve including Pseudomonas.
3
- Third generation: Levofloxacin, Gatifloxacin & moxifloxacin.
Second generation coverage but improved G+ve coverage (penicillin-sensitive &
resistant Strept.pneumoniae)& some anaerobes.
4
-Fourth generation: Trovafloxacin.
Third generation coverage, expanded activity against anaerobes .
is due to their ability to inhibit the activity of bacterial DNA
Antibacterial activity:
gyrase & topoisomerases. During replication DNAgyrase produces & removes
supercoils in DNA ahead of replication fork to maintain the proper tension required

for efficient DNA duplication. While Topoisomerase IV similarly act to remove
supercoils & to separate newly formed DNA daughter strands after replication.
Because of their safety & tolerability, quinolones are commonly used as
alternatives to beta-lactam antibiotics for treating a variety of infections.
Also are not recommended for children or pregnant or lactating women because of
possible toxic effect on cartilage development.
Refamycin:-
Refampicin is most clinically used which bind to DNA-dependent RNA
polymerase & block the synthesis of mRNA .It is used for treatment of prosthetic
valve endocarditis.
The primary use of rifampicin is in the treatment of Mycobacterial infection &
prophylaxis of contact s of meningococcal & Haemophilus meningitis.
Resistance ( in case of TB, meningitis & against staph) is provided by
chromosomal mutations that alter the RNA-polymerase target, which then has
lowered affinity for rifampicin & escapes inhibition.
Rash & jaundice are side-effects of rifampicin treatment. Also intermittent
rifampicin can lead to hypersensitivity reactions.
** Antimetabolites affecting nucleic acid synthesis:
1- Sulfonamides: are bacteriostatic compound that acts in competition with para-
aminobenzoic acid(PABA) for the active site of dihyropteroate synthetase, an
enzyme that catalazea an esse4ntial reaction in the synthetic pathways of
tetrahydrofolic acid(THFA), which is required for the synthesis of purines &
pyrimidines & therefore for nucleic acid synthesis.
Sulfonamides are useful in the treatment of urinary tract infection, but resistance is
widespread.
Sulphonamides are relatively free of toxic side-effects, but rashes & bone marrow
suppression can occur.
Sulphonamides are active against G-ve organisms (except Pseudomonas).
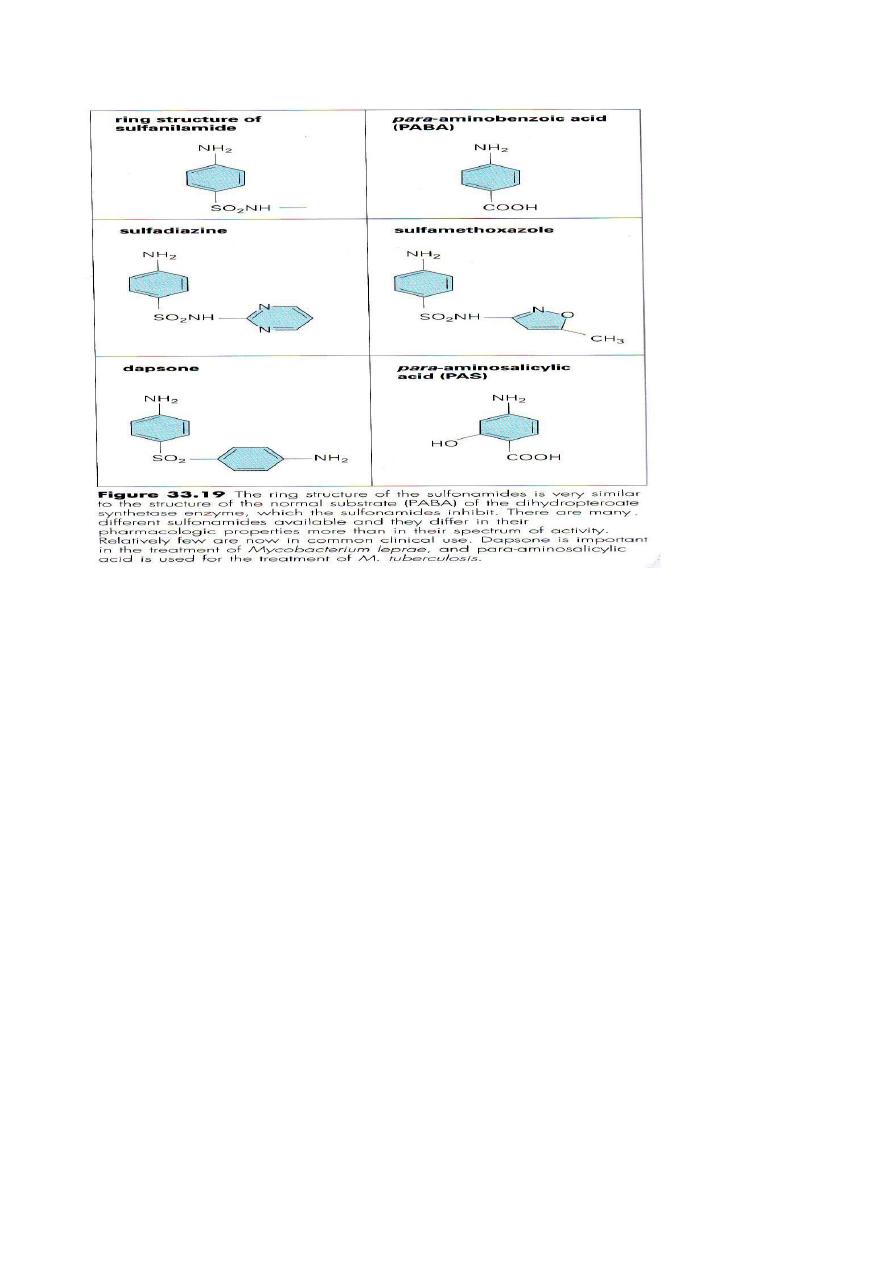
2- Trimethoprim( and Co-trimoxazole):
Trimethoprim is one of a group of pyrimidinelike molecule structure analogous in
structure to the aminohydroxypyrimidine moiety of folic acid molecule. Other
agents with similar structure & mechanism of action include antimalarial
pyrimethamine & the anti-cancer drug methotrexate.
Trimethoprime prevents THFA synthesis in late stage by inhibiting dihydrofolate
reductase. This enzyme is present in mammalian cells as well as in bacterial &
protozoan cells, selective toxicity depends upon the far greater affinity of
trimethoprim for bacterial enzyme.
Trimethoprim is often given with sulfa-methoxazole as co-trimoxazole for urinary
tract infections & against G-ve rods such as Salmonella typhi, except
Pseudomonas. Also for treatment of pneumonia caused by Pneumocystis jiroveci(
formerly P.carinii),for Nocardiosis & chancroid caused by syphilis spirochetes(
treponema)
People with AIDS seem to be more prone to the side-effects of Trimethoprine &
co-trimoxazole. Neutropenia,mausea & vomiting may occur.
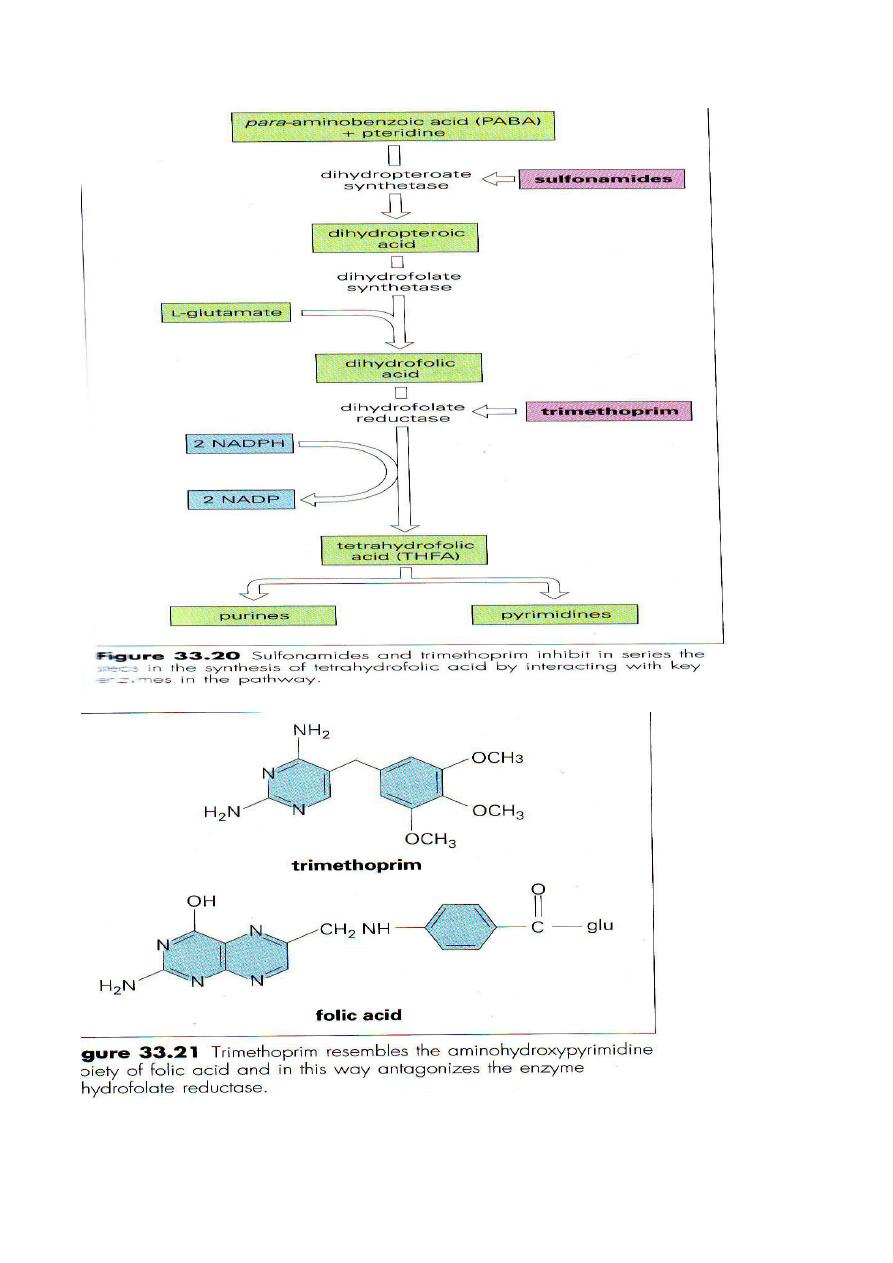
Other agents that affect DNA:

Nitriimadiazole:
Metronidazole( Flagyl) is a nitroimidazole with antiparasitic & anti bacterial
properties .
After entry into the microbial cell, the molecule is activated by reduction, & the
reduced intermediate products are responsible for antimicrobial activity, probably
through interaction with & breakage of the cells DNA. The reactive intermediates
are short lived & decomposed to non toxic inactive end products.
Metronidazole is active only against anaerobic organisms because only these can
produce the low redox potential necessary to reduce the parent drug.
Also been used as hypoxic cell sensitizer radiotherapy .
Metronidazole resistance is of increasing concern in T.vaginalis, G. lamblia &
several anaerobes & Helicobacter pylori ( Micro-aerophilic).
Rarely, metronidazole causes CNS side-effects.
** Inhibitors of cytoplasmic membrane:
The structure of cytoplasmic membranes in bacterial cells differs from that in
mammalian cells & allow the application of some selectively toxic molecules, but
these are few in number compared with those acting at other target sites.
peptides:
-
Lipo
Are new classes of membrane active antibiotics, like Daptomycin, which is
bactericidal against G+ve bacteria including vancomycin resistant E. faecalis & E.
faecium & methicillin resistant Staph.aureus & Staph epidermidis.
The compound acts in a calicium-dependent matter to insert the depolarize the
bacterial cytoplasmic membrane. This action leads to a number of consequences
including the inability to synthesizw ATP & interference with uptake of nutrients.
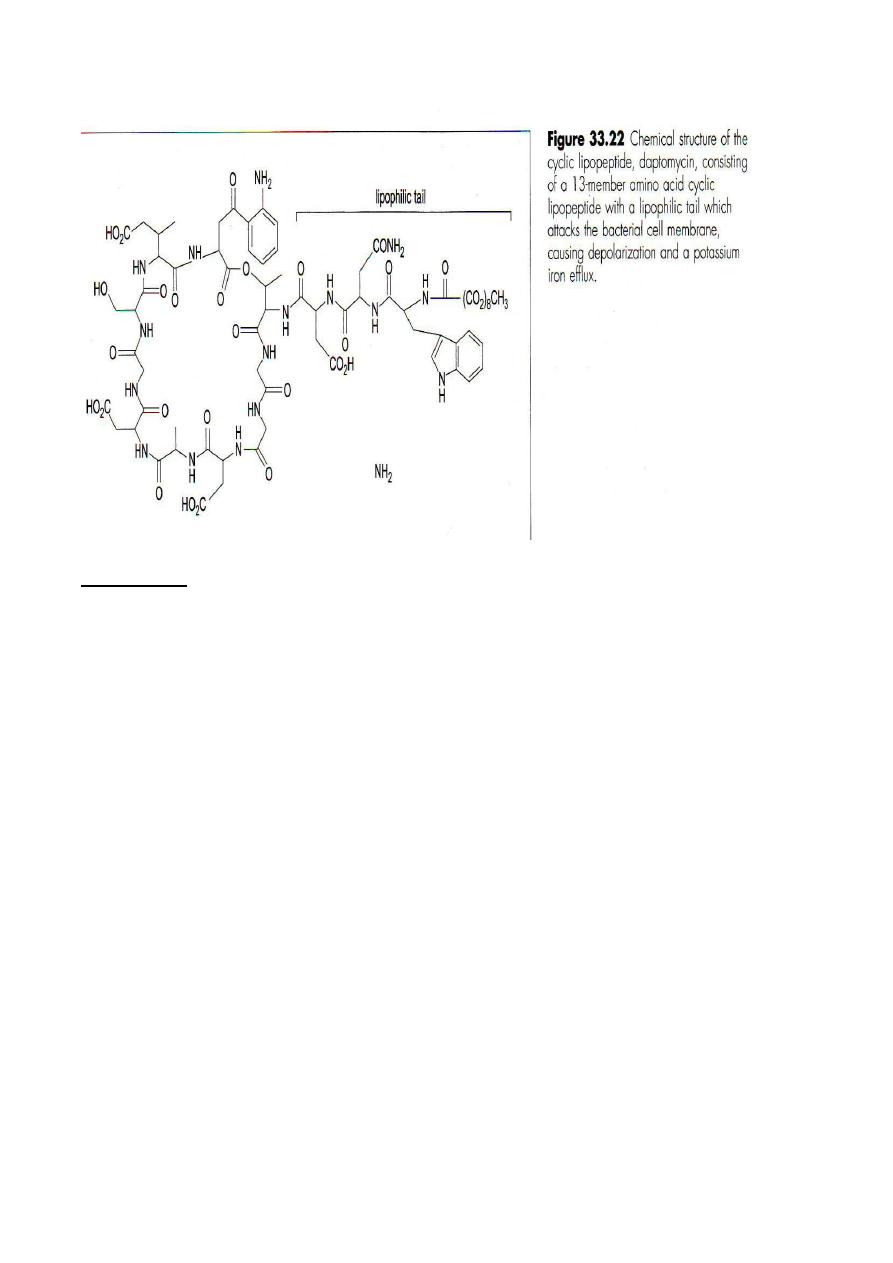
Polymyxins:
Are antifungal as gents act on the membranes of G-ve bacteria (Except Proteus) as
bactericidal cyclic polypeptides that disrupt the structure of cell membrane .
The free amino acid groups of polymyxins act as cationic detergents, disrupting
phospholipids structure of the cell membrane, Polymyxin B is the most common
member of the family still in clinical use.
Polymyxins are primarily used topically but have also been used in the past for gut
decontamination ( polymyxin E specially in neutropenic patients, with caution due to
concerns regarding renal toxicity) . Wound irrigation & as a bladder washout.
Resistance is due to chromosomal mediated alterations in membrane structure or
inhibit uptake.
Other antibacterial drugs:
Nitrofuration & methenamine are both synthetic compounds, that when taken orally
are absorbed & excreted in the urine in concentrations high enough to inhibit urinary
pathogen. At Acidic pH methenamine is hydrolyzed to produce ammonia &
formaldehyde, the later has antibacterial activity. Nitrofurationm is used to treat
uncomplicated UTI, Both agents prevents recurrent UTI. Resistance to nitrofuration
prior to treatment is a concern.
Ant-tuberculosis agents:-
Mycobacterial tuberculosis need prolonged treatment because of it posses' waxy outer
layer, as intracellular location & grow & multiply extremely slowly & effective
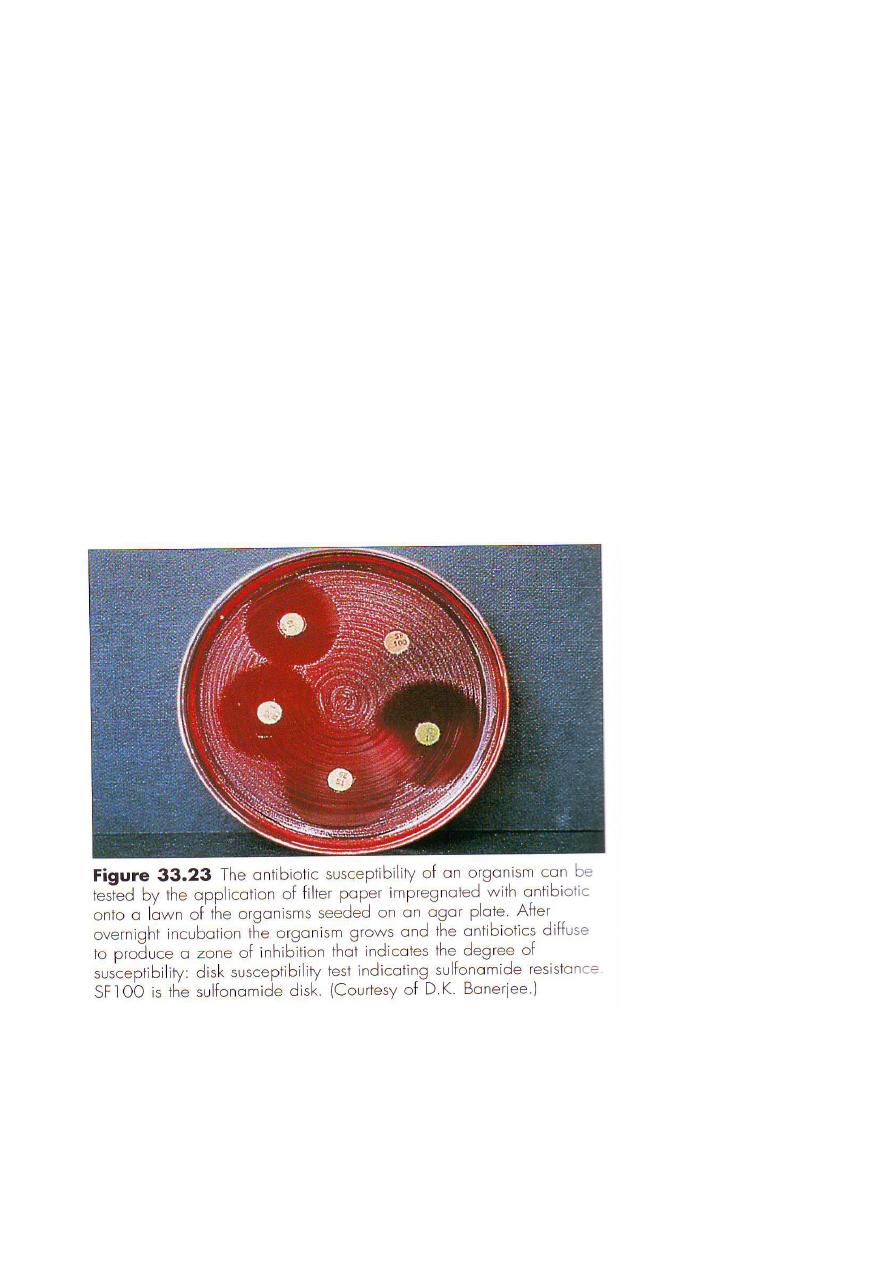
inhibition takes weeks to months. The drugs of the first line therapy of tuberculosis
are:
Isonazid : that inhibit mycolic acid synthesis of mycobacteria cell wall.( bactericidal)
& is given with pyridoxine to prevent neurologic side-effects.
Ethambutol:- Is a synthetic molecule that inhibit but not kill mycobacteria ,so be used
in combination with other drugs in anti-tuberculous therapy.
The most important toxic side-effect is nuritis.
Parazinamide:
Is a synthetic analogue of nicotinamide which appears to target mycolic acid synthesis.
Hepa-totoxicity is more common side effect of pyrazinamide use.
Other drugs of first line included: rifampicin & streptomycin.
Treatment of leprosy:
Infection caused by mycobacterium leprae is characterized by persistence of the
organism in the tissues for years & necessitates very prolonged treatment to prevent
relapse. Dapsone (related to salfonamides ) has been used, but resistance during
dapsone monotherapy for leprosy has led to its use in combination with rifampicin.
Clofazimine, a phenazine compound is now commonly used as multi-drug therapy.
Antibacterial agents in practice:
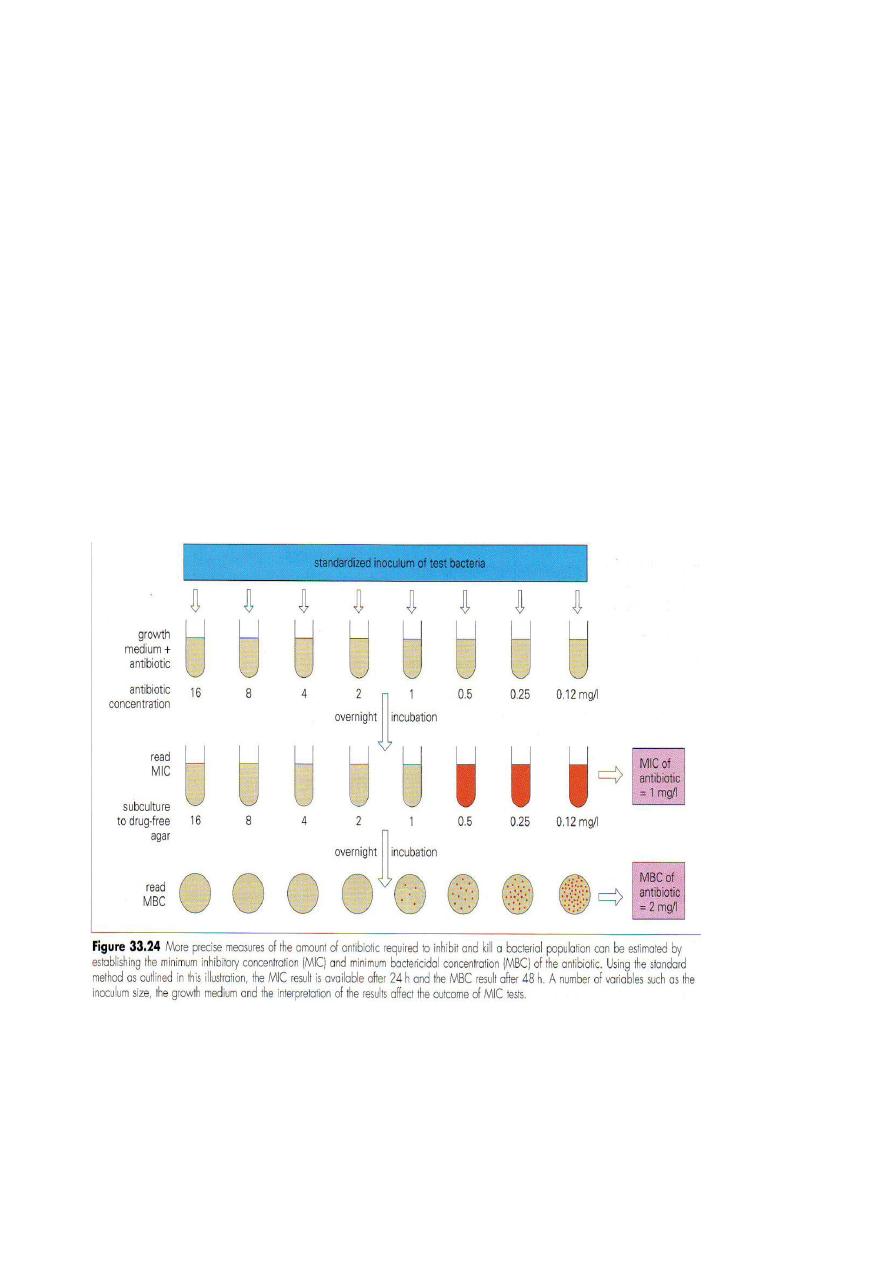
Susceptibility tests performed in the laboratory examine the interaction between
antibiotics & bacteria in an isolated & rather than fashion. Susceptibility tests fall into
two main categories:
1- Diffusion tests: involve seeding the organism on an agar plate & applying filter
paper disks containing antibiotics. The result recorded zones as S (sensitive) , I(
intermediate) & R( resistant) . Intermediate indicates that the isolate is less susceptible
less than norm, but may respond to higher doses of antibiotic, or in site when the
antibiotic is concentrated.
2- Dilution test:
Provides a quantitative estimate of susceptible to an antibiotic. Serial dilutions of the
test antibiotic are prepared in broth or agar medium & inoculated with a suspention of
the test organism. Overnight incubation, The Minimum inhibition concentration (MIC)
is recorded as the highest dilution in which there is no macroscopic growth.
The advantage of an MIC that it can extended to determine the MBC( minimum
bacterial concentration) which is the lowest concentration of antibiotic required to kill
the organism.
The test dilution sub-culturing onto afresh drug free medium & incubated for 18 hours
is an evaluation the efficacy of dilution test.
The antibacterial agent is considered to be bactericidal if the MBC is equal to or not
greater than four fold of MIC.
Killing curve provide a dynamic estimate of bacterial susceptibility.
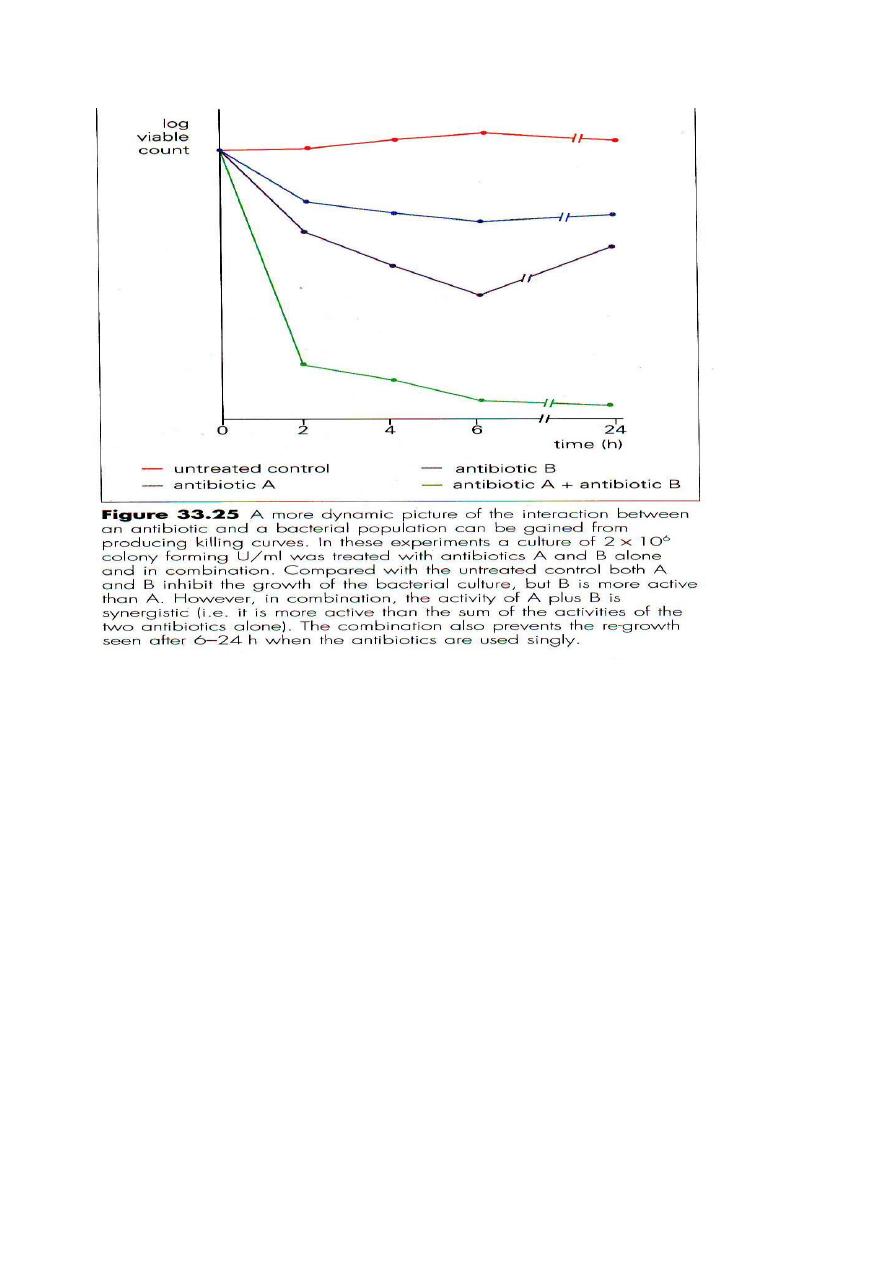

Factors affecting antimicrobial activity:
A- The pH of environment: some drug are more active at acid pH ( e.g.nitrofuration),
at alkaline pH( e.g. aminoglycosides, salfonamides).
B- Components of medium: Anionic detergents inhibit aminoglycosides,addition of
NaCl to the medium enhances the detection of methicillin resistance in Staph. Aureus.
C- Stability of drug: At incubator temperature, several antimicrobial agents lose their
activity such as chlortetracycline inactivated rapidly while penicillin's more slowly.
D- Size of inoculum: large bacterial inoculum reveal lower apparent sensitivity of the
organism. In addition, a resistant mutant is much more likely to emerge in large
population.
E- Length of incubation: Short incubation is doubtful because most of microorganisms
are not killed but only inhibited.
F- Metabolic activity of microorganisms: In general, actively & rapidly growing
organisms are more susceptible to drug action than those in the resting phase.

Metabolically inactive organisms that survive long exposure to a drug may have
offspring that are fully susceptible to the same drug.
Antimicrobial activity in-vivo:
The problem of antimicrobial agents is much more complex in
–vivo than in-vitro it
involves:
1- Drug-pathogen relationships include:
A- Environment:
*State of metabolic activity.
* Distribution of drug.
*Location of organisms.
*Interfering substance.
B- Concentration:
* Absorption.
* Distribution of drugs.
* Variability of concentration.
* Post antibiotic effect.
2- Host pathogen relationships:
It may be altered by antimicrobial drugs in several ways:
* Alteration of tissue response.
*Alteration of immune response.
* Alteration of microbial flora.
Antiviral therapy:-
Based on selective inhibitory of:-
1- Inhibition of viral replication.
One of the challenges in the development of antiviral agents is identification of the
steps in viral replication, which are unique to the virus & not used by the normal
cell. Among the unique viral events are: attachment, penetration, uncoating, RNA-
direct DNA synthesis ( reverse transcription) & assembly & release of the intact
virion.
2- DNA-polymerase inhibition:
Inhibition advantage based on fact that virus is synthesizing nucleic acids more
rapidly than the cell, so there is relatively greater inhibition of viral than cellular
DNA.
3- Other viruses are ongoing viral replication & do not benefit from
viral inhibition, such as HIV& infection with chronic hepatitis
B & C.
HSV,VZV
HSV,VZV
HSV,VZV
HSV,VZV
HSV
HSV
HSV,VZV
HSV,VZV
HSV,VZV
HSV,VZV
&
&
CMV
CMV
CMV & resistant
CMV & resistant
HSV
HSV
CMV
CMV
HSV,VZV
HSV,VZV
Acyclovie
Acyclovie
,
,
Famciclovir
Famciclovir
,
,
Penciclovir
Penciclovir
,
,
Valacycliovir
Valacycliovir
,
,
Gancicyclovir
Gancicyclovir
,
,
Foscatrnet
Foscatrnet
,
,
Cidofovir
Cidofovir
,
,
Trifluridine
Trifluridine
Inhibition of viral
Inhibition of viral
DNA polymerase
DNA polymerase
Influenza A & B
Influenza A & B
Oseltamivir
Oseltamivir
,
,
Zanamivir
Zanamivir
Neuraminidase
Neuraminidase
Influenza A & B
Influenza A & B
Amantidine
Amantidine
&
&
Rimantidine
Rimantidine
Inhibiting of viral &
Inhibiting of viral &
uncoatingh
uncoatingh
,
,
penetration
penetration
Viral spectrum
Viral spectrum
ِ
ِ
antiviral agents
antiviral agents
Mechanism of
Mechanism of
action
action
HIV
HIV
Efavirenz
Efavirenz
HIV
HIV
Delavirdine
Delavirdine
HIV
HIV
Nevrapine
Nevrapine
HIV & HBS
HIV & HBS
Lamivudine
Lamivudine
HIV
HIV
Stavudine
Stavudine
HIV
HIV
Dideoxycytidine
Dideoxycytidine
HIV
HIV
Dideoxyinosine
Dideoxyinosine
HIV
HIV
Zidofudin
Zidofudin
Inhibition of viral
Inhibition of viral
reverse transcription
reverse transcription
HIV
HIV
Lopinavir
Lopinavir
HIV
HIV
Nelfinavir
Nelfinavir
HIV
HIV
Retonavir
Retonavir
HIV
HIV
Indinavir
Indinavir
HIV
HIV
Sequinavie
Sequinavie
Inhibition of viral
Inhibition of viral
Protease
Protease
CMV
CMV
Fomivirsen
Fomivirsen
Antisense
Antisense
inhibition of viral
inhibition of viral
mRNA synthesis
mRNA synthesis
RSV ,HCV &
RSV ,HCV &
Lassa fever
Lassa fever
Ribavirin
Ribavirin
Inhibition of viral
Inhibition of viral
RNA polymerase
RNA polymerase
HBV,HCV &
HBV,HCV &
HPV
HPV
Interferone
Interferone
alpha
alpha
Inhibition of viral
Inhibition of viral
protein Synthesis
protein Synthesis
HSV
=Herpes simplex virus
VZV+ Varicell-Zoster virus
CMV=Cytomegalovirus
HIV=Hum immnuno-deficiency virus
HBV= Hepatitis B virus
HCV =Hepatitis C virus,
HPV= Human papilloma- virus
RSV=Respiratory syncytial virus.
Antiviral resistance:-
Genetic alterations (Mutations or deletion) are the bases of antiviral resistance
:
The likelihood of resistant mutations results from at least 4 functions
1-
Rate of viral replication:
Higher rate of replication are associated with higher rates of spontaneous
mutations.
2
- Selective pressure of the drug:
It can increase the probability of mutations to the point that virus replication is
substantially reduced.
3-
Rate of viral mutation:
Single strand RNA viruses (HIV, FLU viruses) have more rapid rates of mutation
than Ds-DNA viruses ( HSV)
4
- Rate of mutation in differing viral genes:
For example in HSV the genes for phosphorylation nucleosides( e.g. UL97) are
more susceptible to mutation than the viral DNA-polymetrase.
everal ways:
Resistance to viral detection may be detected in s
1- Phenotypic:-
Phenotypic resistance is detected by in vitro methods.
2- Genotypic:-
By molecular detection of expected mutation .
3- Viral quantitation in response to treatment:-
No reduction or increase in patient's viral burden suggests development of resistant
mutations.
This step can be assessed by various methods such as culture, PCR, antigen assay.
Lecture Number : Dr. Yahya G.Salman
Subject Medical Virology.
Influenza, Respiratory syncytical virus, Adenovirus
& other respiratory viruses .
The major causes of acute respiratory disease (ARD) include:
Influenza viruses, Parainfluenza viruses, Rhinoviruses, Adenoviruses, Respiratory
syncytial virus (RSV) & respiratory Coronaviruse. Reoviruses are of questionable
importance, but also considered, other such as enterovirus& measles virus, can also
cause respiratory symptoms.
Influenza viruses:-
They are members of Orthomyxovirus, which are enveloped, single strand RNA
viruses, they are classified into 3 major serotypes, (A,B,&C), based on different
ribonucleoprotein antigens.
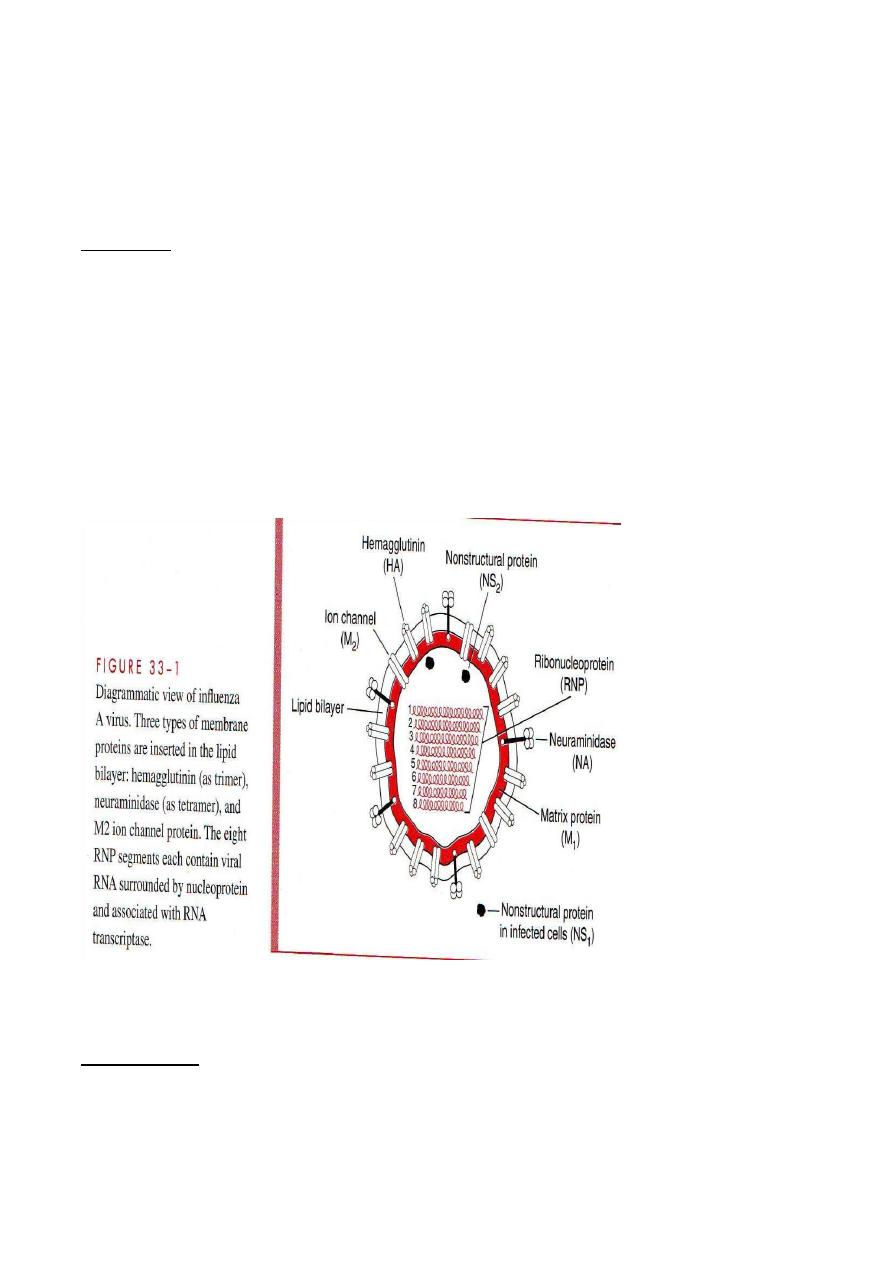
Type A has greatest virulence & epidemic spread (mammals & birds). Type B is
antigenically stable; are only known to naturally infect humans & usually occur in
more localized outbreaks.
Type C viruses appear to be relatively minor causes of disease, affecting humans &
pigs.
-
Structure:
Each virus consist of nucleocapsid containing 8 segments of negative sense, single
strand RNA( ssRNA), which is enveloped in a glycolipid membrane derived from
the host cell plasma membrane. The inner side of envelope contains a layer of virus
specified protein ( M1).Two virus specified glycoproteins, haemagglutinin(HA)
that acts in viral attachment& neuraminidase( NA), which has role in envelope
fusion & viral release. Both are embedded in the outer surface of the envelope &
appear as spikes over the surface of virion.
Influenza B is similar to A but has a unique NB protein instead of M2.
Influenza C differ from the others in that it possesses only RNA segments & has no
NA, also the haemagglutinin of C binds to a cell receptor different from that for
types A &B.
Influenza A :
A unique aspect of influenza A viruses is their ability to develop a variety of
subtypes through the processes of mutation Whole gene swapping between strains,
called re-assortment, which results in antigenic changes called drifts & shifts.
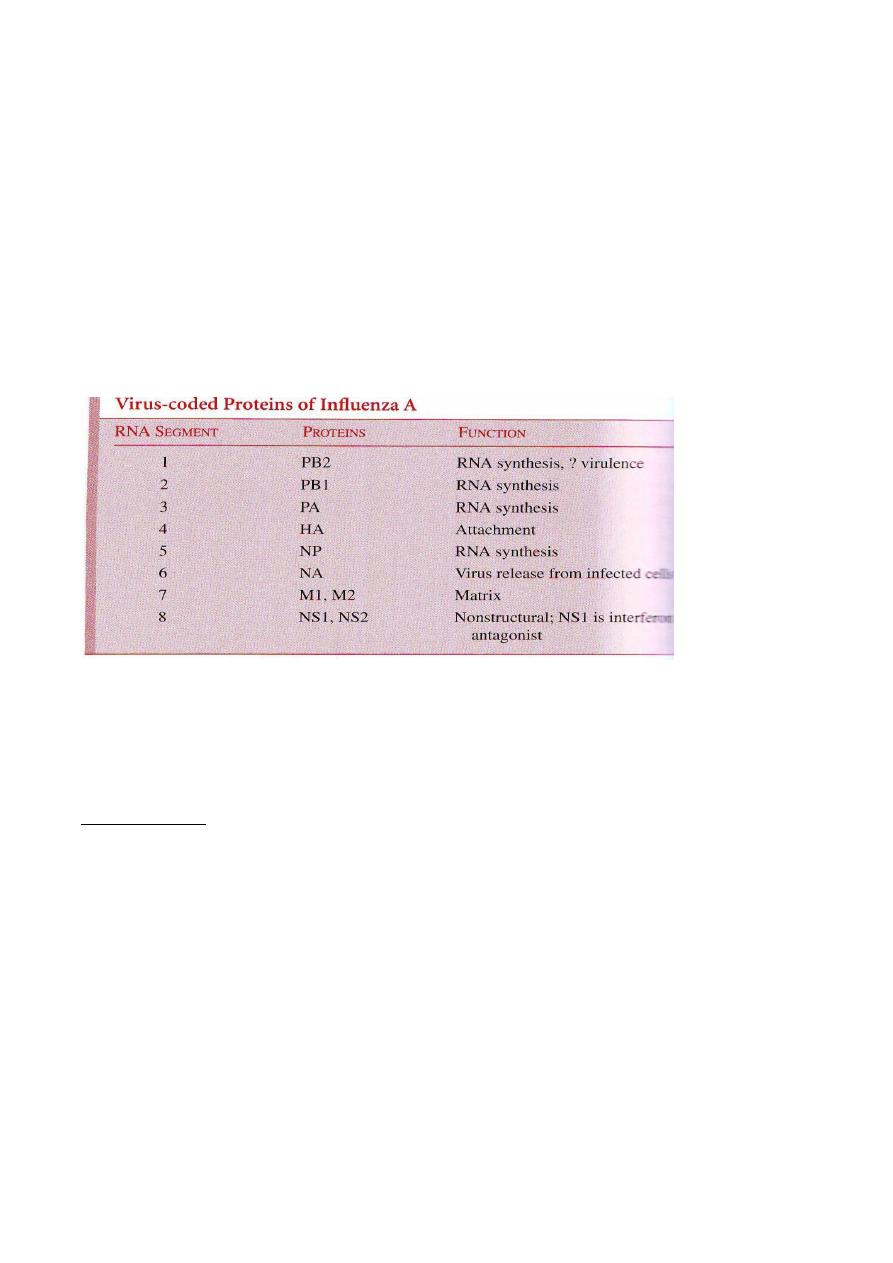
From 15 subtypes of HA & 9 NA that are circulated in birds & mammals represent
a reservoir of viral genes that undergo re-assortment or mixing with human strains.
Three Ha as ( H1,H2& H3) & (NI & N2) appear to be of greatest importance in
human infections.
These subytypes are designated according to the H & N antigens on their surface (
H1N1, H3N2),Subtle changes known as antigenic drift, e.g. two H3N2 strains that
differ antigenically only slightly are A/Texas/1/77(H3N2) &
A/Bangkok/1/79H3N2.Also antigenic drift may involve the gene encoding non-
structural protein ( NP). Incidence of drift in influenza B is lower than that in A.
Major antigenic shifts correlate with epidemics; e.g Russian flue which appeared in
1977 was caused by an H1N1 subtype very similar to that which dominated in
1947 & 1957.
Epidemiology:
1- Influenza A viruses closely related to those prevalent in humans circulate
among many mammalian & avian species.
2- Pandemic influenza may have high mortality usually the elderly & persons
of any age with cardiac & pulmonary disease.
3- Seasonality favours winter months, & the most common mode of
transmission is by direct droplet spread.
4- Epidemic intervals usually a few years.
5- Excess mortality or increased absenteeism is indicator of epidemic.
6- Influenza B rarely causes such sever epidemics.
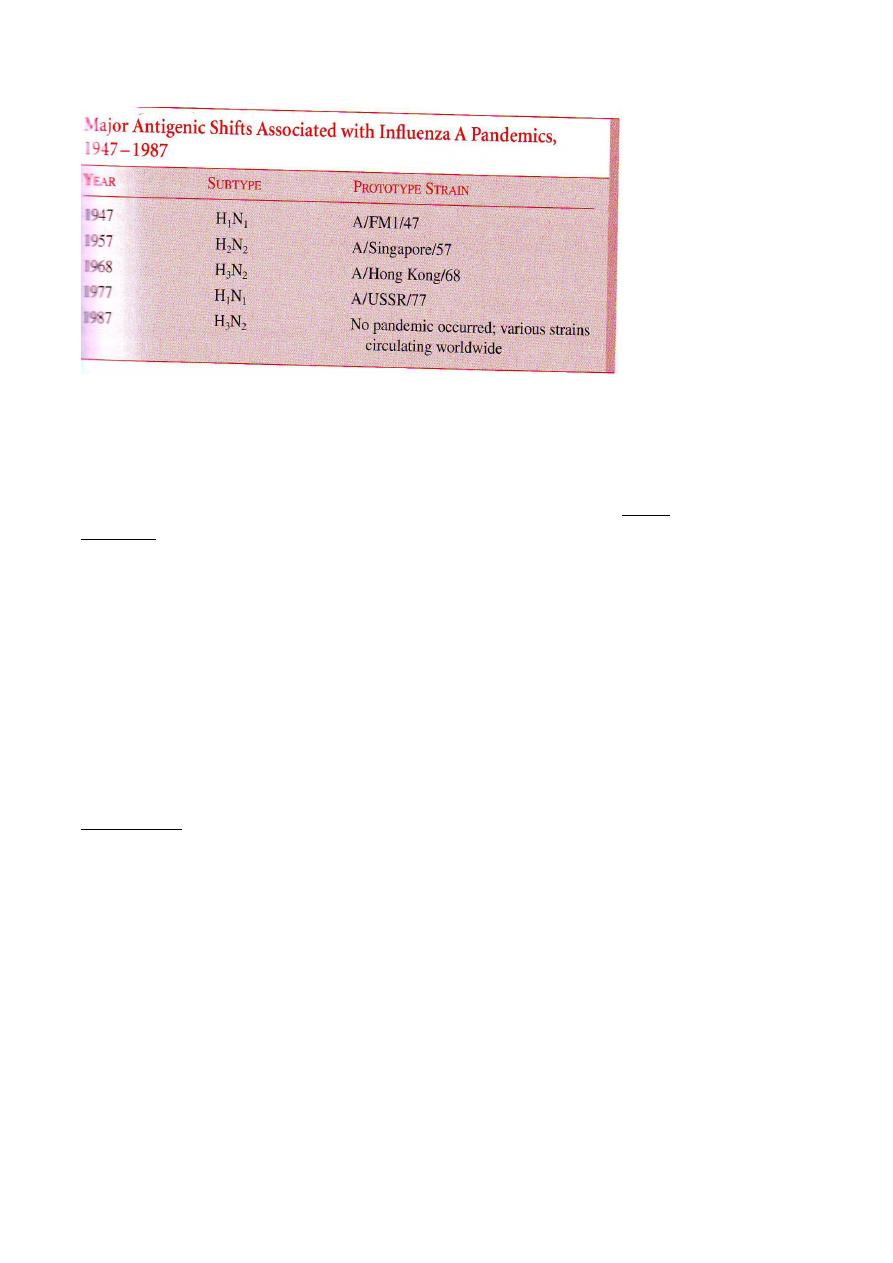
Patho
-
genesis:
Functional &structural respiratory epithelia ciliary abnormalities with
out detecting viremia can occur, the process of programmed cell death
(apoptosis) result in the cleavage of complement components, leading to
localized inflammation. Other host cell functions are also severely
impaired, particularly during the acute phase of infection. These functions
include: chemotactic, phagocytic & intercellular killing functions of
polymorphnuclear leukocytes & perhaps of alveolar macrophage activity
.The damage renders the host highly susceptible to invasive bacterial
super- infection.
Interferon & Cytotoxic T-cell responses associated with recovery.
Typically patient's responds to infection within a few
-
Immunity:
days by producing antibodies directed toward the ribonucleoprotein
antigen. The haemagglutinin which neutralize virus on re-exposure &
neuraminidase may limit viral spread. However, such immunity is
relative & quantitative differences in responsiveness exist between
individuals. Antigenic shifts & drifts often allow the virus to subvert the
antibody response on subsequent exposures.
Manifestations:
Short incubation period( average 2 days).onset is abrupt, followed by
active illness with the following symptoms : fever, myalgia, headache &
occasionally shaking chills, within 6 to 12 hours, the illness reaches its

severity, & a dry ,non-productive cough develops, the acute findings
sometimes with worsening cough for 3 to 5 days. . By about one week
after onset, patients feel significantly better.
Unusual acute manifestations are pneumonia, CNS dysfunction,
myositis & myocarditis. In infant Reyes syndrome may follow after 12
days from the onset.
The most common complication is bacterial super-infections by ,
Streptococcus pneumoniae, Haemophilus influenzae & Staphylococcus
aureus.
Death due influenza infection can occur:-
1- Underlying disease with de-compensation.
2- Super-infections (disseminated bacterial infections).
3- Direct rapid progression: Less commonly, progression of the viral
infection can lead to overwhelming viral pneumonia with asphyxia.
Diagnosis:-
During acute phase of illness, influenza viruses can be readily isolated
from respiratory tract specimen, such as naso-pharyngeal & throat swab.
Most strains grow in primary monkey kidney cell cultures, & then can
be detected by hemadsorption or hemagglutination. Rapid diagnosis can
be done by direct IF & ELISA detection of viral antigen in epithelia cells
or secretions from the respiratory tract. Serodiagnosis is useful
epidemiologically (by demonstrating fourfold or greater increases in
hemagglutination inhibition antibody titers in acute & convalescent
specimen collected 10 to 14 days a part.
Treatment:-
Symptomatic care & anticipation of potential
complications,particularly bacterial super infection are bases to
management of influenza disease .
After diagnose, rest, adequate fluid intake, conservative use of
analgesic for myalagia & headache& anti-tussives for sever cough are
commonly prescribed.
Antibiotic prophylaxis has not been shown to enhance or diminish the
like hood of superinfection, but can increase the risk of acquisition of
more resistant bacterial flora in the respiratory tract & make
superinfection more difficult to treat.
When influenza A is proved or strongly suspected, early antiviral
therapy must be given ( 4 to 5 days of therapy) as in the following table(
comparison of different .
Oral
Inhalation
Oral
Oral
Administration
Not Known
Not Known
Yes
Yes
Emergent
resistant
strains
Influenza A
& B
Influenza A
& B
Influenza B
only
Influenza
A only
Susceptible
viruses
Oseltamivir
Zanamivie
Rimantidine
Amantidine
Feature
Prevention:
Killed viral vaccine (whole virus) & spilt vaccines are protective but variable &
short duration.
Annual reactivation against most current strains is necessary.
Vaccination should be directed primarily the elderly individuals of all ages who are
at high risk( those of chronic lung & heart disease), and their close contacts
including medical personnel & household members.
Amantidine & rimantidine are effective prophylaxis effectively short term for
influenza A only(by blocking the ion channel of viral M2 protein, that interfere in
early viral uncoating & assembly.
Neuraminidase inhibitors such as zamanivir & oseltamivir are useful in treatment
for influenza A & B( by blocking enzymatically active neuraminidase glycoprotein
present on the surface of Influenza A & B , that limit virus releasing from infected
cells & subsequent spread in the host).
Respiratory syncytial virus infection(RSV):
It can cause Bronchitis & pneumonia in infants.
Classification:
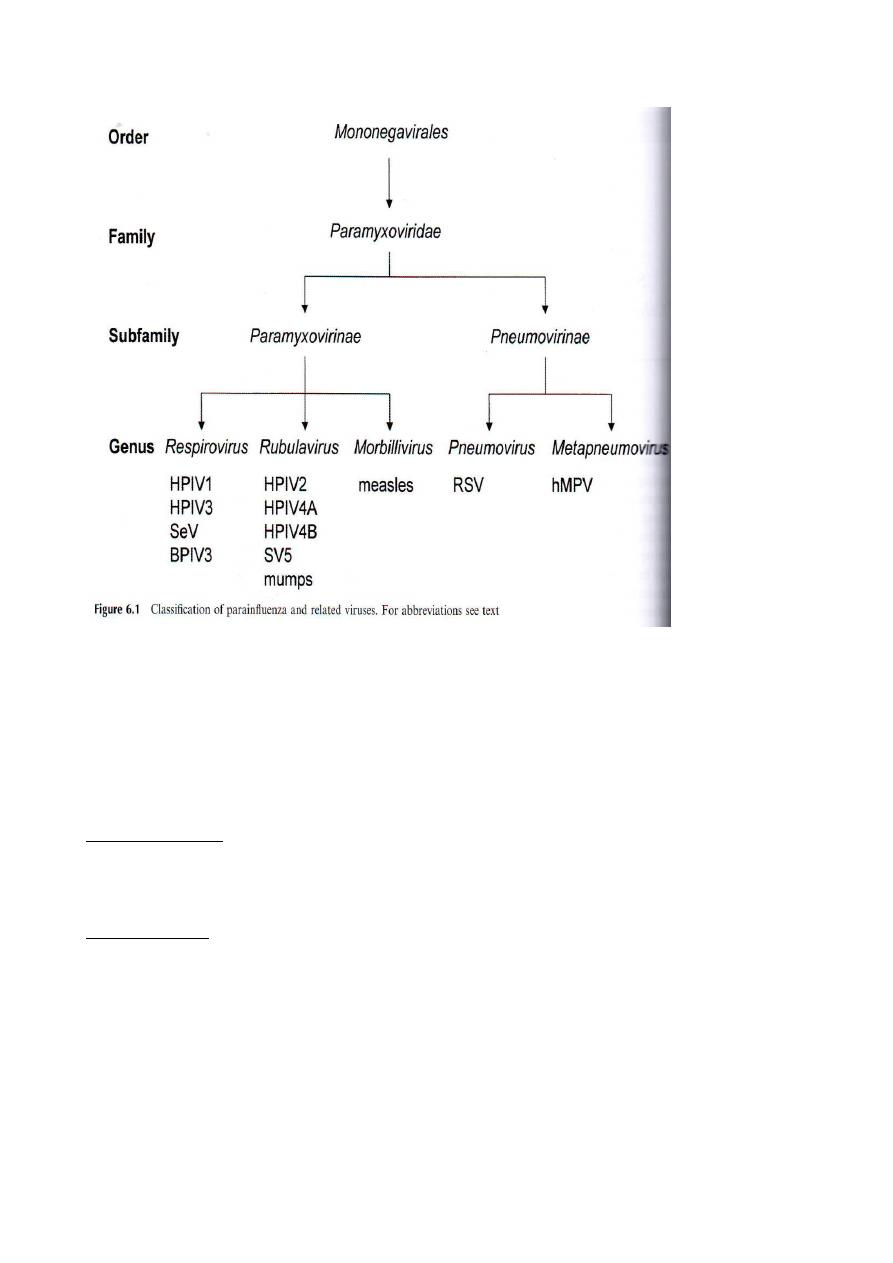
RSV is atypical paramyxovirus & Two major strains have been
identified: group A & B , Its surface spikes bear G protein( not
haemagglutinin or neuraminidase) For attachment to the cell&
fusion(f) protein, the latter initiate viral entery to the cell membrane,
& also fuse host cells to form Syncytia.
by droplets & to some extend by hands.
-
Transmission :
Outbreaks can occur each winter & it can spread in Hospitals as well
as in the community mostly among individual up to 2 years.
-
Pathogenesis:
The direct effect of virus on respiratory tract epithelial cells is similar
to that occurred by Influenza viruses. Cytotoxic T- cells appear to play
similar role in early control of the acute infection.
Factors that have been proposed to plays a role includes:
1- Qualitative& quantitative deficits in humoral or secretory antibody
response to critical virus specified protein.
2- Formation of antigen antibody complexes in RT resulting in
complement activation.
3- Excess size damage from inflammatory cytokines( specially those
produced bt T-helper Type 2 including
IL-2,IL-5,IL-6,LI -10 & IL-13) .
Necrosis of epithelial Severity of infection in infants may have
immunological basis .cells & interstitial mononuclear cell.
Inflammatory plugs bronchioles & alveoli occasionally seen in the
affected tracheobroncheal epithelium.
-
Immunity:
In spite of the humoral & secretory antibody responses ( IgG & IGA)
but immunity to reinfection is quite tenuous( partial). Illness severity
to diminish increasing age & successive reinfection .
Manifestations:
Incubation period is 2 to 4 days, followed by the onset of rhinitis,
infant bronchitis & pneumonitis( cough, wheezing& respiratory
distress lasts up to 2 weeks). Clinical finding includes: hyper
expansion of lungs & hypoxia with duration of acute illness is often
10 to 14 days.
Mortality is highest with underlying disease & cause of death include
respiratory failure, right side heart failure (cor pulmonali) & bacterial
super infection.
Children &adults have milder illness. RSV infection triggers wheezing
in asthmatics.
-
Diagnosis:
Is by Virus isolation by cell cultures syncytial cytopatic effects
develop over 2 to 7 days. Also by IFAT & ELISA tests .
-
Treatment:
Supportive treatment (oxygenation, ventilator support when
necessary) & close observation for complications are indicated.
Ribavirin aerosol may be effective in selected circumstances.
-
Prevention:
No vaccine is currently is available, but monoclonal antibody(
palivizumab) & immunoglobulin used for prophylaxis to prevent RSV
infection in under 2 years old infants , this method requires monthly
injections during the RSV season( usually 5 months ) & is extremely
expensive.
Para-influenza viruses (HPIV):-
Virology:
Four serotypes of HPIV as 1.2.3.&4 are present. They belong to
enveloped viruses of Paramyxovirus group; contain non segmented,
negative sense ss-RNA & like Influenza viruses possesses
haemagglutinin & neuraminidase. The mode of spread & pathogenesis
is similar to that of influenza viruses.
They differ from influenza viruses in that RNA synthesis occurs in the
cytoplasm rather than in nucleus. In addition the antigenic makeup of
the 4 serotype is relatively stable, & significant antigenic shift or drift
does not occur. Each serotype is considered separately.
Disease:
HPIV are important because of the serious diseases they can cause in
infants &young children, HPIV 1 & 3 are particularly common in this
regard. They are responsible for 15 to 20 % of all nonbacterial
respiratory disease requiring hospitalization in infancy & childhood.
Immunity to reinfection is transient, although repeated infection can
occur in older children & adults; they are usually milder than the
illness of infancy & early childhood.
-
Manifestations:
The onset of the illness may be abrupt, as in acute spasmodic croup
with variable progression over 12 to 3 days to involvement of the
middle or lower RT.
Duration of acute illness can vary from 4 to 21 days but is usually 7 to
21 days.
Parainfluenza 1:
Is a major cause of acute croup( laryngotracheitis) in infant & young
children, But it may also causes less sever diseases such as mild upper
respiratory illness(URI), pharyngitis & tracheobronchitis in
individuals of all ages. Outbreaks of infection tent to occur most
frequently during fall months.
-
Parainfluenza 2 :
This infection is slightly less significant than parainfluenza 1 & 3. It
has been associated with croup, primarily in children, with mild URI
& occasionally with acute lower respiratory disease.
As parainfluenza 1 , outbreaks usually occur during the fall months
-
Parainfluenza 3 :
Produces sever lower respiratory disease in infants. It often causes
bronchitis, pneumonia & croup in children less than one year of age.
In older children & adults, it may cause URI or tracheobronchitis.
Infections are common & can occur in any season.
Parainfluenza 4 :-
Is the least common group . It is generally associated with mild URI
only.
-
Diagnosis:
Laboratory diagnosis involves isolation usually in monkey cell
cultures or serology using haemagglutination inhibition, complement
or neutralization (pared sera for watching of rising antibody titer, also
IFAT & ELISA can be used for rapid detection of antigen in
respiratory epithelial cells.
Treatment & prevention:
Currently, there is no method of control or specific therapy for these
infections.
Adenoviruses( ADVs):-
These viruses are responsible for gastrointestinal & ocular infections
worldwide, more recently, these viruses have been associated with
additional important syndrome including pharyangitis , pharyango-
conjunctival fever , conjunctivitis, pertussis like syndrome, kerato-
conjunctivis,bronchiolitis, pneumonia & acute haemorrhagic cystitis.
-
Virology:
From a total of 100 different serotypes of ADVs, 49 are known to
affect humans. They are naked, 70-90 nm in diameter & have 10
structural proteins, icosahedral with 252 capsomers divided into 240
hexones( 20 triangular faces) & 12 pentons, each penton consist of
base & a fiber( rod like outword projection of variable length) with
terminal knob that is responsible for interaction with cellular receptor.
The pentons are specially active in haemagglutination, all
polypeptides are numbered with Roman numerals ( I-X).
ADVs have a liner, non segmented Ds-DNA of about 36 Kb.
Replication & assembly occur in the nucleus, the virion is released by
cell destruction.
All adenoviruses share a common group specific, complement-fixing
antigen associated with the hexon component of the viral capsid.
Potential for prolonged periods of infection ranging from a few days
to several years .
The group name is derived from its discovery in 1953 as a latent agent
in many adenoid tissue specimens & by prolonged intermittent
shedding of virus from the pharynx & intestinal tract after initial
infection.
-
Epidemiology:
High endemicity is by type 1 & 2, followed by type 5.
Overall, only 45 % of adenovirus infection result in disease of
children (acute illness) & by type 4 & 7 among military recruits.
Infection can spread by the respiratory or fecal-oral route. All
serotypes can occur during any season of the year but mostly
frequently in winter or early spring. Swimming pool & medication
associated conjunctivitis occur in outbreaks.
Transmission:
Usually by inhalation of droplet nuclei or by the oral route, direct
inoculation onto nasal or conjunctival mucosa by hands, contaminated
towels, or ophthalmic medication may also occur.
-
Pathogenesis:
Due to virus replication in epithelial cells, necrosis & inflammation
are produced, may be followed by viremic spread (kidney, bladder,
liver lymphoid tissue & occasionally the CNS& remote disease).
After the acute phase of illness, the viruses may remain in tissues such
as tonsils, adenoids & intestinal pyers patches & become reactivated
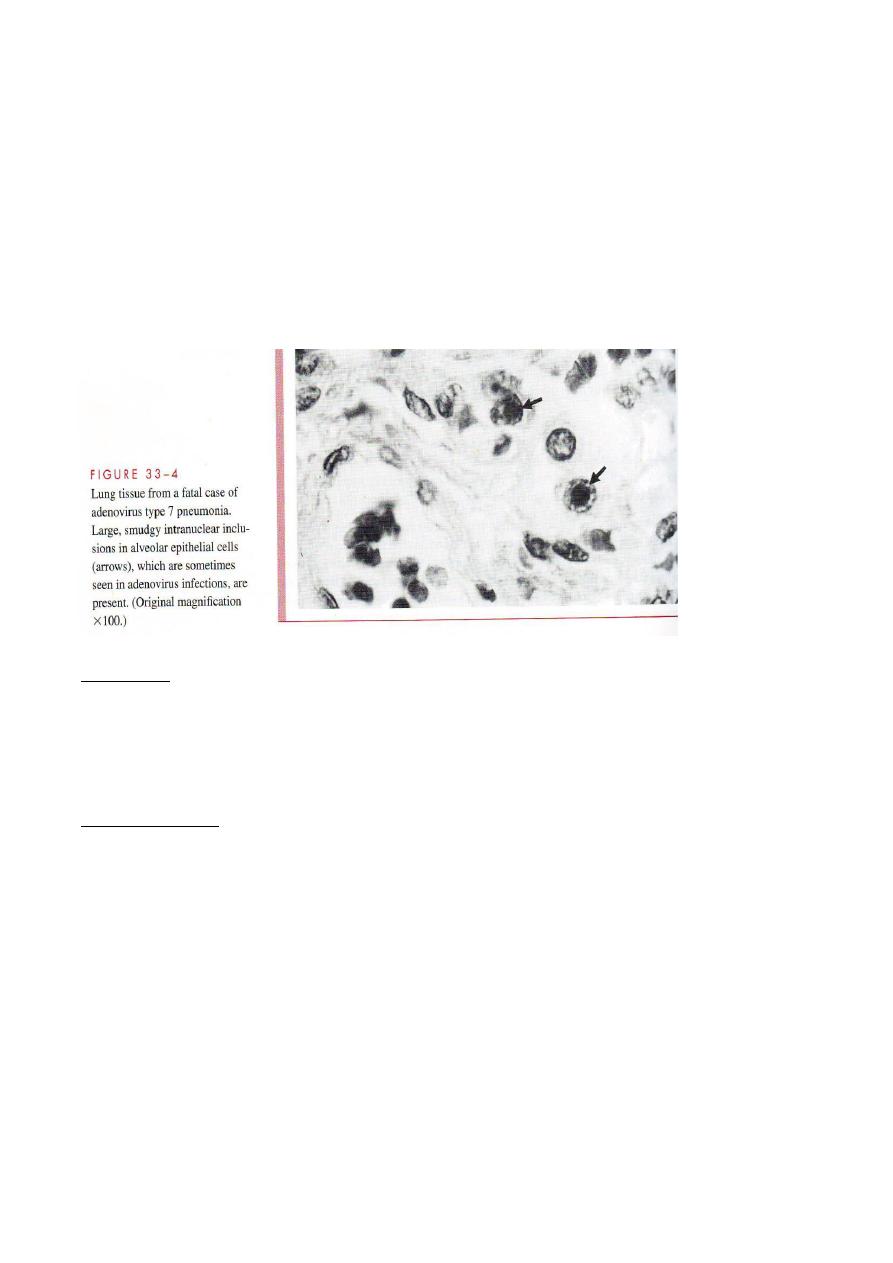
& shed without producing illness for 6 to 18 months thereafter.
Integration of ADVs produces latency, which can persist for years in
tonsillar tissue & peripheral blood lymphocytes.
Penton projections appear to be responsible for toxic effect on cells,
which manifests as clumping or detachment in vitro.
Proteins restrict cyto-toxic T cells & enhance cytokine susceptibility.
Of epithelia cells to destruction by tumor necrosis factor (TNF) &
other cytokines. Adenovirus death protein is considered important for
efficient lysis of infected cells & release of newly formed virions..
Immunity:
Long standing immunity specific to ADVs serotype after infection can
produce in addition to group-specific complement-fixing antibodies
appear in response to infection. These antibodies useful indicator to
infection, but do not specify the infecting serotype.
-
tions:
Manifesta
The acute respiratory syndromes vary in both clinical manifestation &
severity. Symptoms include fever, rhinitis, pharyngitis, cough &
conjunctivitis.
In children below 3 years, ADVs are also common causes of non-
streptococcal exudative pharyngitis . Acute, occasionally chronic,
conjunctivitis& kerato-conjunctitis have been associated several
serotypes. More sever disease, such as laryangitis, croup, bronchiolitis
& pneumonia may also occur.
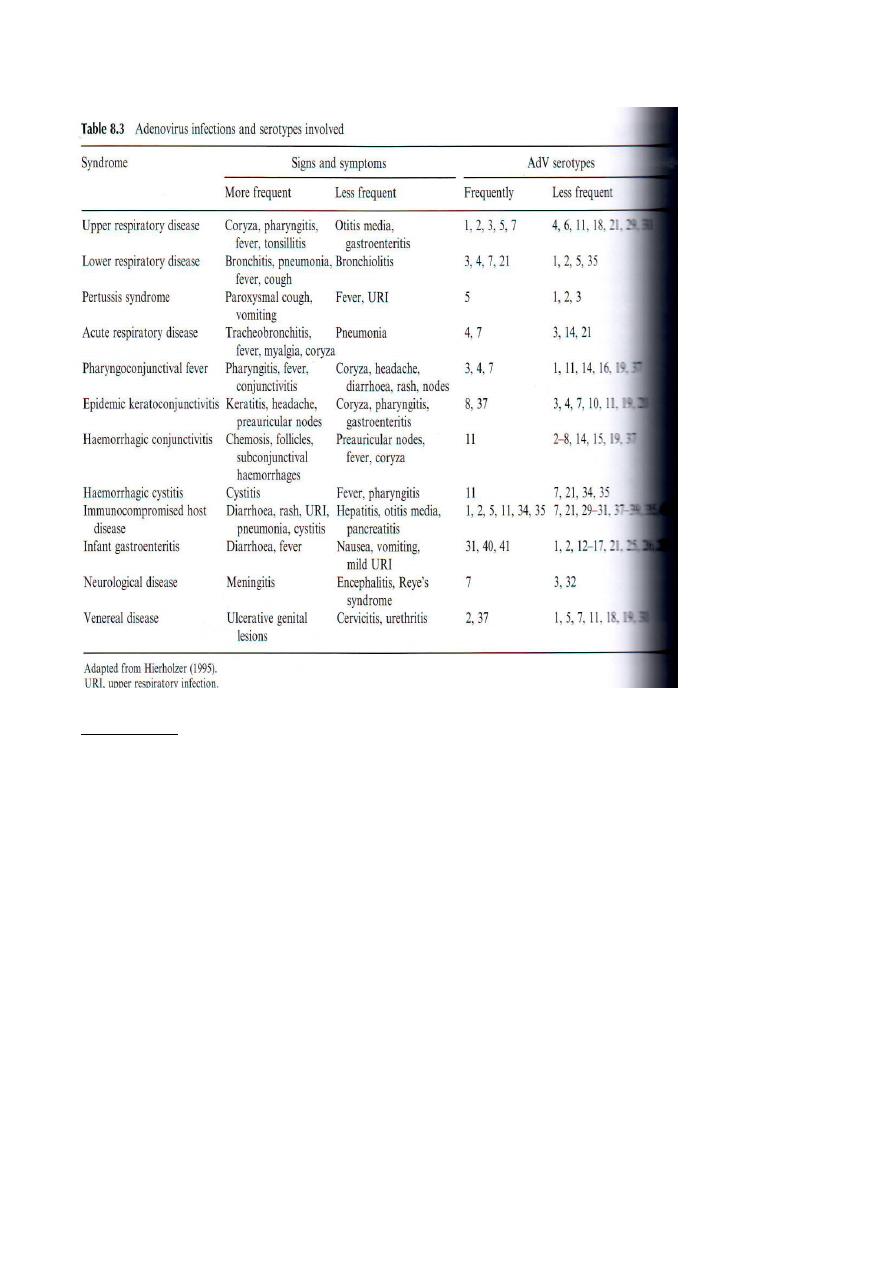
-
Diagnosis:
Is by:
1- Viral isolation using heteropoliod culture. Viral isolation from oro-
pharynx or feces may not mean disease ( because of the known
tendency for intermittent asymptomatic shedding into oro-pharynx &
feces.
2- Histopathology: via which, infected cells have enlarged nucleiwith
basophilic inclusions, surrounded by a thin rim of cytoplasm & are
called Smudge cells which are typical of ADVs infection.
3- Direct antigen detection by
A-Using IF ( rapid test but less sensitive than culture).
B- Using EIA( particular for diagnose of enteric ADVs in fecal
smears.
C- Immuno-histochemistry( Specific but less sensitive).
Serologic testing of acute & convalescent sera may be necessary to
confirm the relationship between the virus & the illness in question.
3- Direct particle detection using electron microscopy.
4- Direct viral genome detection:
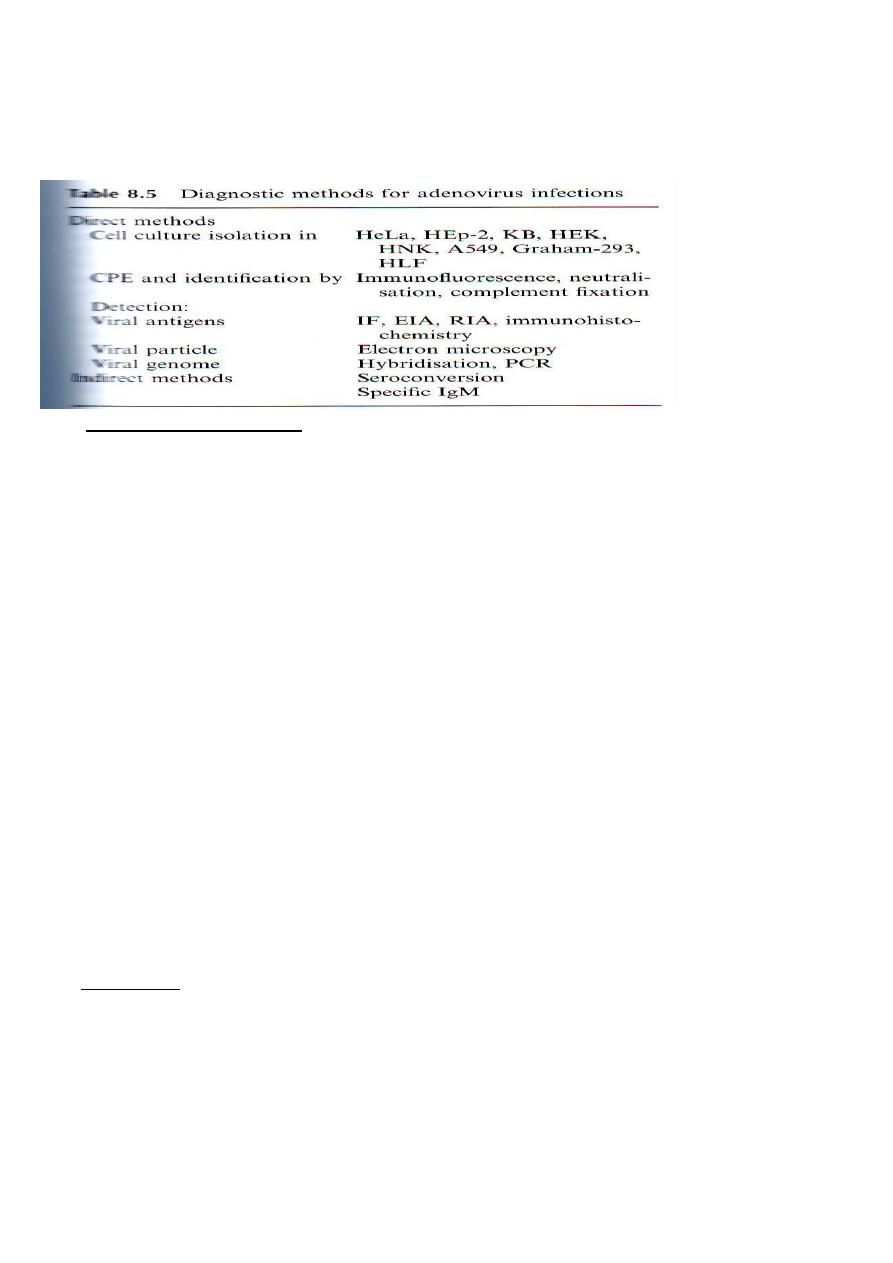
A- Hybridisation: useful method of detecting ADVs in tissue sections.
B- PCR.
-
Treatment & prevention:
There is no specific therapy fro infection, although more experience
has been obtained with ribavirin, cidovirin . A live vaccine containing
serotype 4 & 7 enclosed in enteric coated capsules & administered
orally has been used in military recruits. The viruses are released into
the small intestine, where they produce an asymptomatic, non-
transmissible infection, but this vaccine neither a available nor
recommended for civilian group.
Rhinoviruses:-
Rhinoviruses are small RNA viruses belonging to the family
Picronaviridae( pico=small +RNA), which also include the
enteroviruses,e.g. polio,coxsackie)( they are distinguished from
enteroviruses by their acid liability& an optimum temperature of 33C
for invitro replication.) ,echo viruses & cardio-viruses( rodent
encephalo-myocarditis). Rhinoviruses comprise at least 115 serotypes
& more than that are not classified.
Rhinoviruses are the major causes of common cold, which was
recorded over 2000 years old by Hippocrates around 400 BC.
The first isolation was in 1953 in tissue culture using human embryo
kidney cells & from patients in 1957.
Structure: _
The virion is small 28 to 34µm & consists of a non-enveloped capsid
surrounding a ss-RNA, positive sense genome. Capsid is composed of
60 identical subunits, arranged as 12 pentamers in an icosahedron
.Each subunit consists of all 4 structural proteins named as
VP1,VP2,VP3 & VP4, with molecular mass of 32,29, 26 & 7 KDa
respectively. VP1,2 & 3 are surface proteins interacting with antibody
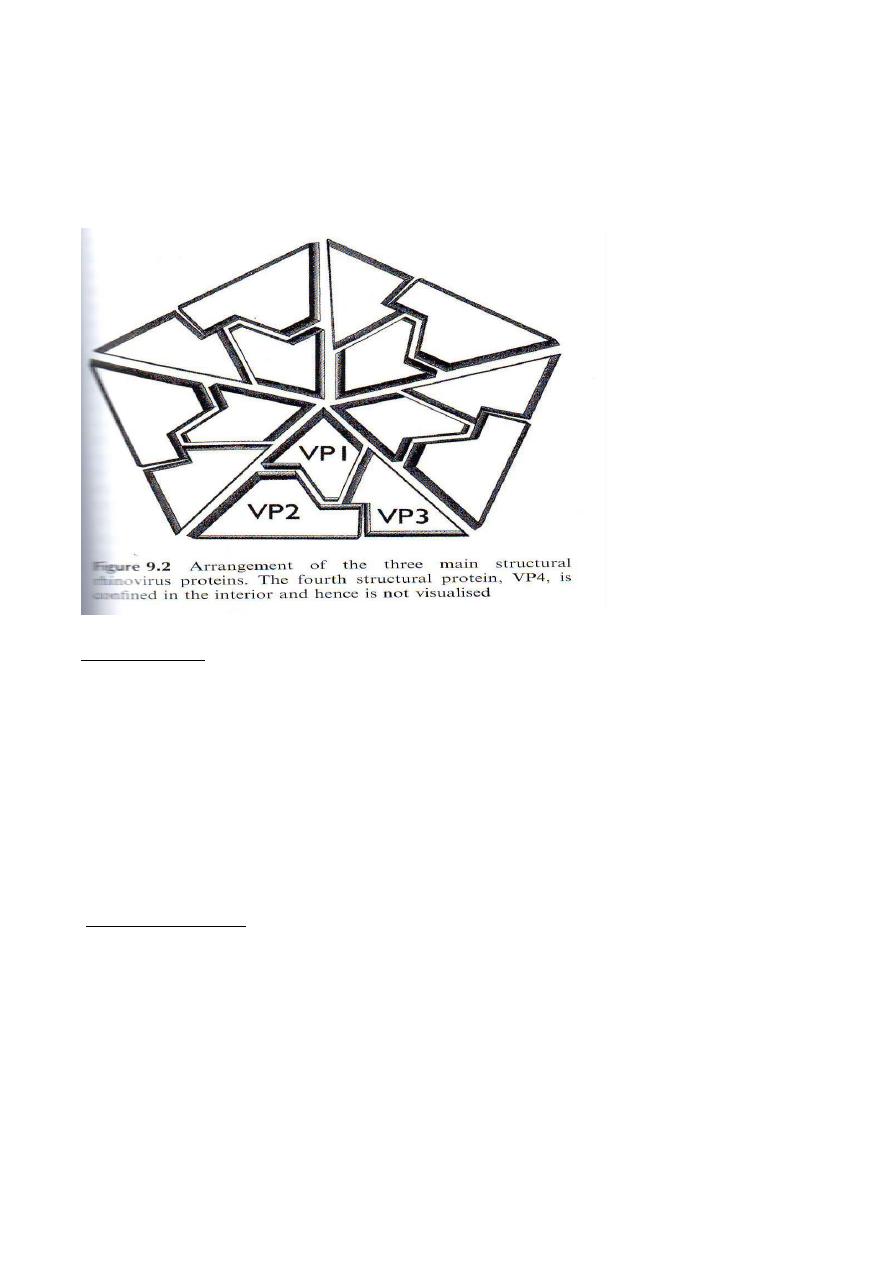
& corresponding to the part of the genome with highest variability.
VP4 is confined to the interior of the capsid & is closely associated
with the Viral RNA. VP1 has five depression shape by 5 VP1 forming
canyon ,also VP1 posses' hydrophobic pockets thought to be involved
in virus uncoating & are the major target of antiviral.
Transmission:
The nose is the main portal for rhinovirus entry. The mode of person-
to-person transmission has been debated, but it is likely that both
direct & indirect hand surface-hand contact & aerosol inhalation.
Rhinoviruses are capable of surviving on surfaces for several hours
under ambient conditions & transfer or rhinoviruses through hand
touch can occur in only a few seconds, so that direct inoculation by
rubbing the nares or eyes with infected hands can readily occurred.
Also transmitted via oral & pharyngeal secretions, but with lower rate
compare to nasal mucus.
period:
Incubation
Is short 1 to 4 days commonly 2 to 3 days, generally viral shedding
peaks 2 to 4 days post infection, lasting usually for 7 to 10 days( some
time persist for as long as 3 weeks).
Natural transmission increases in relation to :- high virus titers in nasal
secretion, increases symptoms, time spend in contact & social factors
such as crowding & poor hygiene .In families, the interval between the
initial & secondary infections relates to the quantity & duration of
virus shedding ranging to 10 days with an average of 3 days.
-
Pathogenesis:
The nasal epithelium is the primary site of infection & the infection
can initiate in naso-pharynx , in the area of the adenoids & virimia is
not detected in normal adults.
Rhinovirus infection does not produce extensive cytopathology of the
nasal mucus membrane but exposure of human primary bronchial
epithelial cells to rhinovirus may result in extensive CPE, depending
on serotype & culture condition. Mucosal oedemas with sparse
infiltration of inflammatory cells, mainly neutrophils are the dominant
histological changes. Nasal mucociliary clearance is reduced, as a
result of a reduced ciliary beat frequency & loss of ciliated epithelium.
Increased of plasma proteins ( lactoferrin, lysozyme & secretory IgG ,
7F 10 immuno-reactive mucin ) can seen in nasal secretion of infected
individuals. These finding reflects vascular permeability (mediated by
vasocate amines) & glandular secretion commonly induced by
cholinergic reflexes & neuropeptides. Kinins are generated in nasal
secretions during natural & experimental colds, while their intranasal
instillation causes sore throat.
Vascular leakage & mucus secretion result in nasal blockage &
stimulation of the sneeze & cough reflexes, resulting common cold
symptomatology.
Otitis & sinusitis resulted from vascular leakage of rhinovirus
infection & paranasal occlusion is a common event in rhinovirus
colds. Upper respiratory tract infection by rhinoviruses can exacerbate
up to 80 % of asthma episodes in schoolchildren.
Clinical features:
Rhinovirus produce the symptoms of common cold including:
rhinorrhea , sneezing, nasal obstruction, sore throat & cough.
Symptoms severity is highly variable, on many occasions the disease
may be hardly noticed, while around 20% of non-influenza flu-like
illness can be attributed to rhinoviruses.
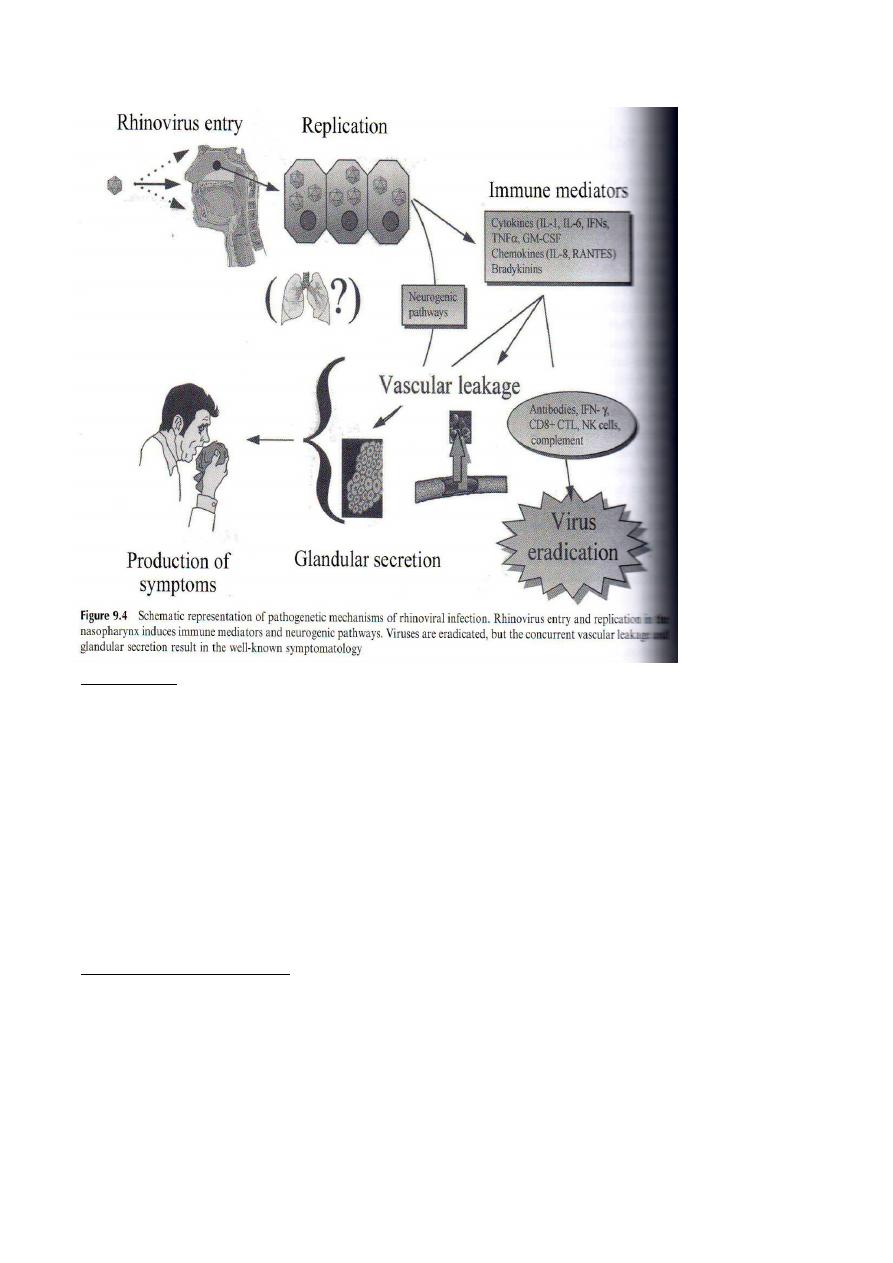
-
Immunity:
Both cellular & humoral immunity are activated in response to
rhinovirus infection.
Pro-inflammatory & anti-inflammatory cytokines are induced by
rhinovirus infections, altered cell mediated immunity, virus IgE &
other mechanisms have been proposed.
Peripheral blood lymphocyte counts are decreased during infection.
Diagnose:-
Viral culture, serological tests & more recently nucleic acid detection
by PCR have been used in the diagnosis of rhinovirus infection.
& prevention:
Treatment
Although there is no specific therapy but a soluble form of the major
rhinovirus receptor ICAM-1(immunologic cell adhesion molecule)
can inhibit viral entry & inactivate
the virus in-vitro.
Also pleconaril( a drug of choice of picronaviruses, including
enteroviruses) , a capsid inhibitor that integrates into the viral capsid
in the VP1 hydrophobic pockets of the virus can lead to block capsid
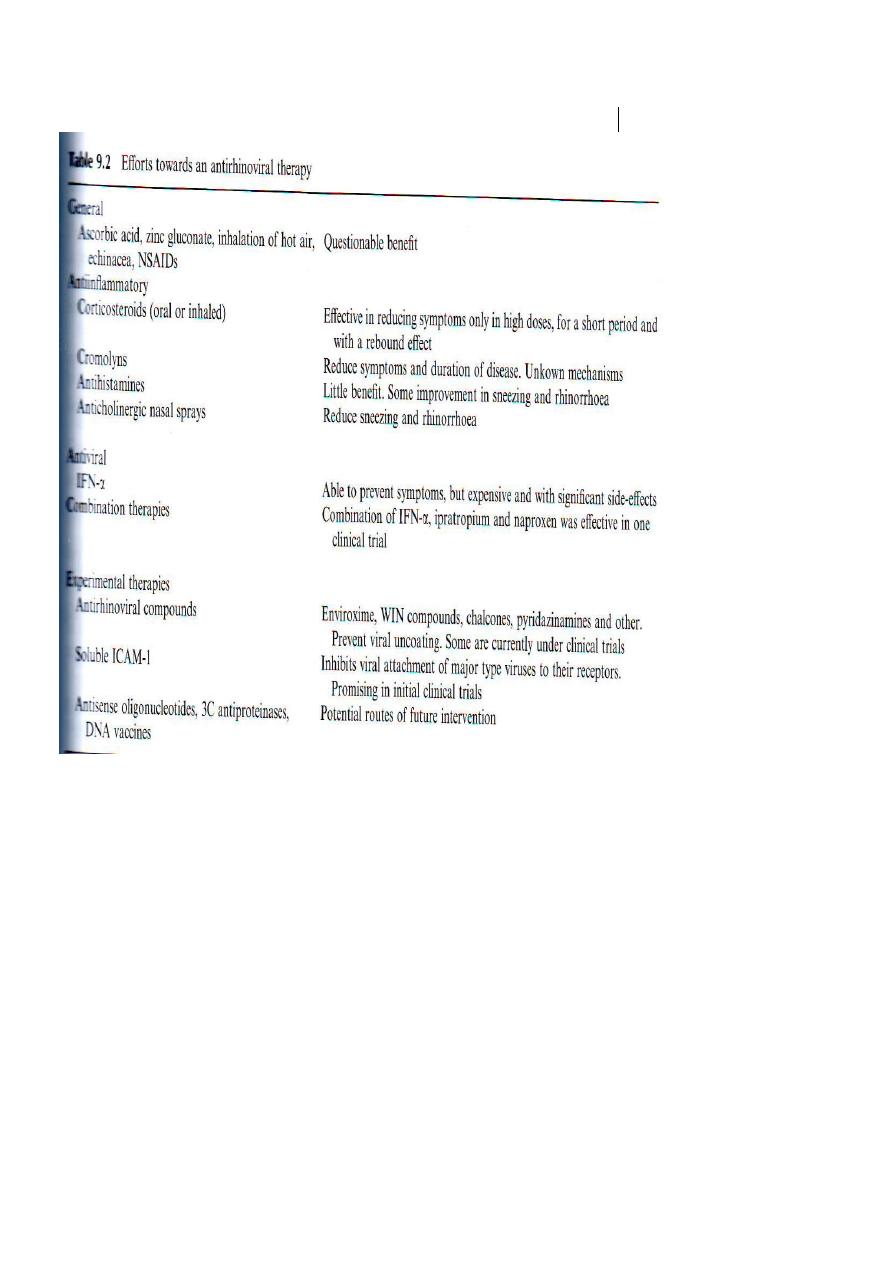
affect viral uncoating after entry.
attachment to cells & perhaps
The multiplicity of serotypes & their tendency to be type of specific in
production of antibodies seem to demand the development of a
multivalent vaccine, which would be extremely difficult to
accomplish.
Coronaviruses( CoV) :
Are enveloped ss- RNA, positive sense viruses. This is surrounded
by an envelope that includes a lipid bilayer derived from intracellular
rough endoplasmic membrane & Golgi membranes of infected cells.
Petal or club-shaped spikes ( peplomers) measuring approximately 13
nm project from the surface of the envelope, giving the appearance of
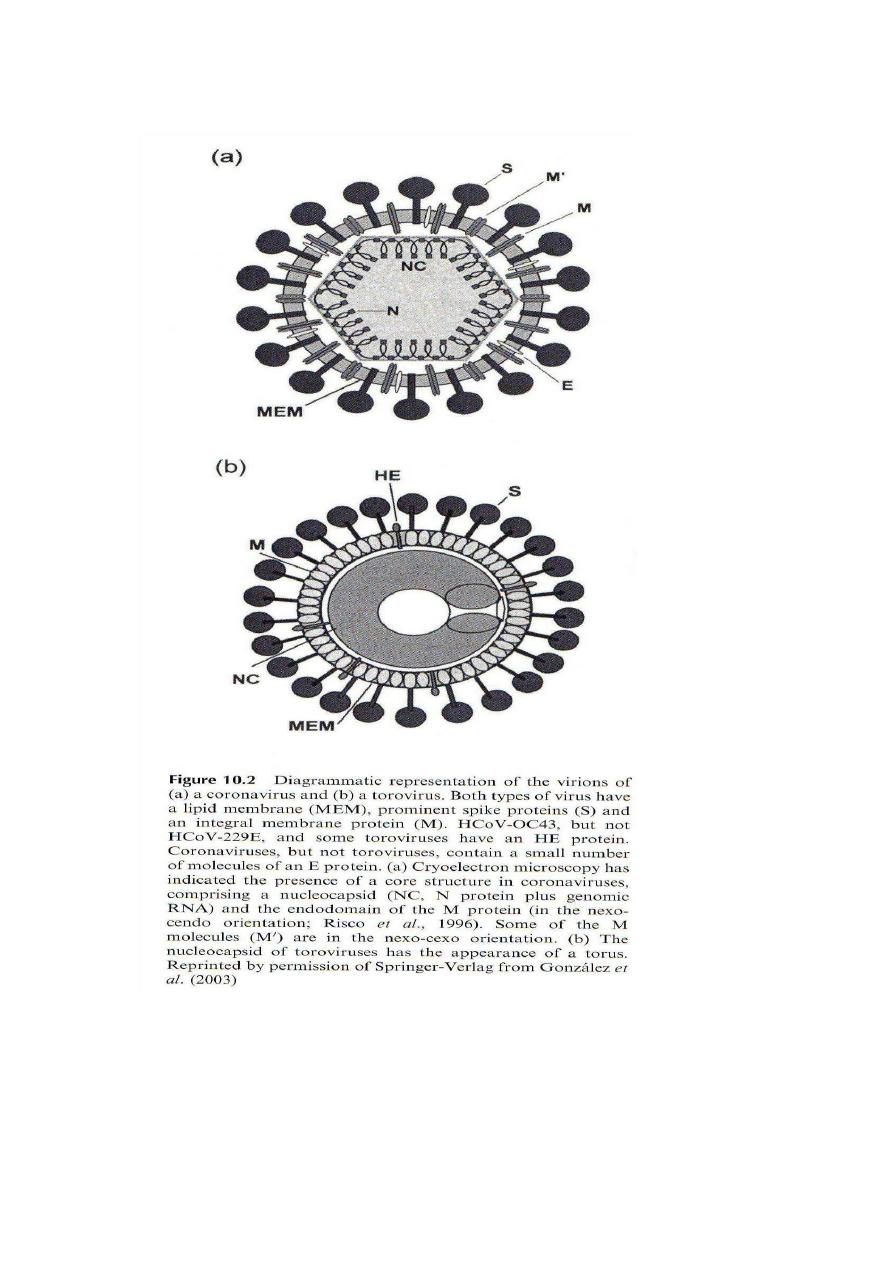
a crown or thorns or solar
corona
The peplomers platy an important role in inducing neutralization &
cellular immune responses .
Like the rhinoviruses, coroviruses are considered primary causes of
the common cold about 5-10 % of common cold in adults & similar
proportion of lower respiratory illness in children.
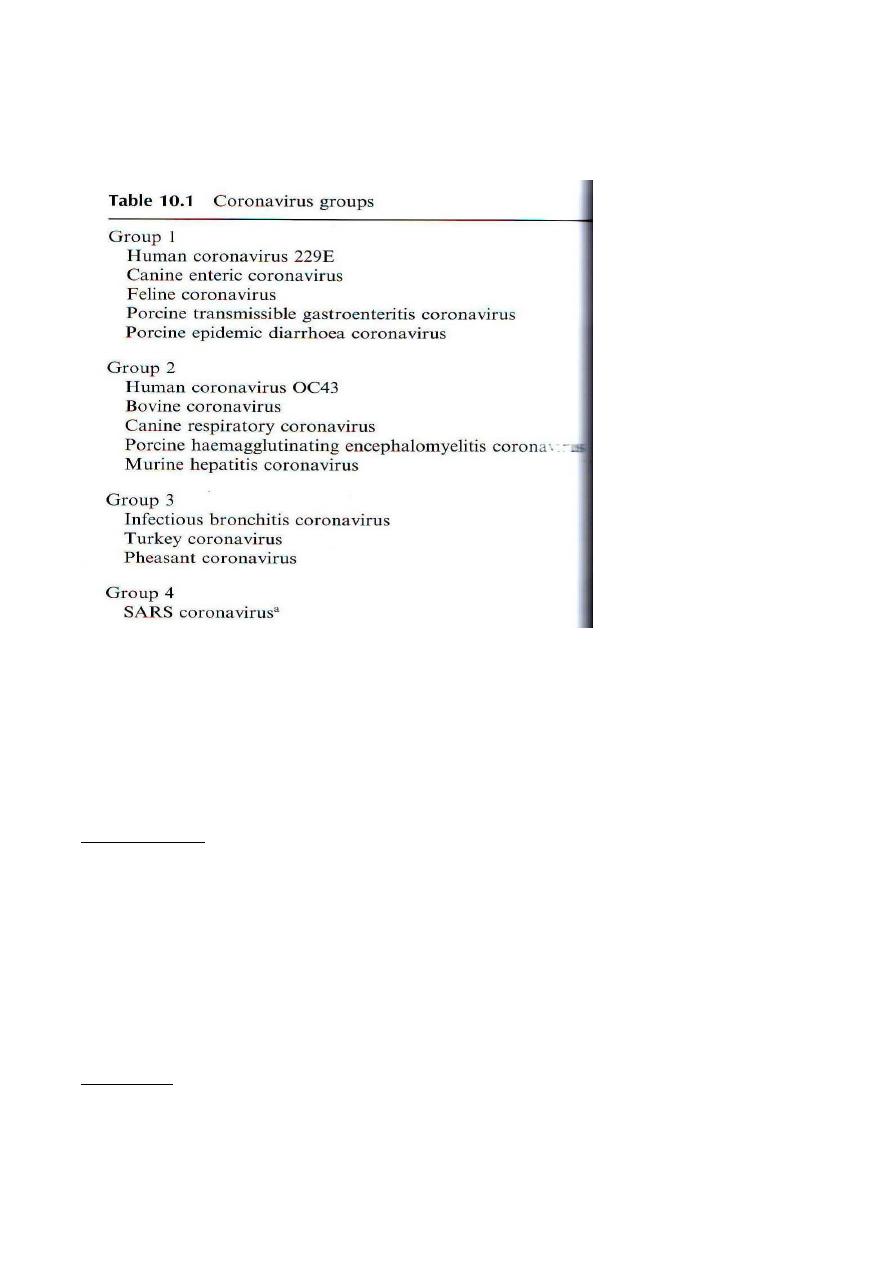
The number of serotypes is unknown, but 2 strains have been studied (
229E & OC43) , it is clear that they cause outbreaks similar to those of
rhinoviruses & that reinfection with the same serotype can occur.
The cellular receptors for these strains are a cell surface
metalloprotease & a sialic receptor similar to that bound by Influenza
C virus.
The SARS- associated coronavirus( SARS CoV) a new member of the
coronavirus family was identified in October 2002 in china by virus
isolation in cell culture & electron microscopy in conjunction with
molecular methods.
prepared
nature (food
ng & it is
is related to habit eati
Transmission:
freshly from live animals, eating a range of exotic wild animals
including bats & cats, resulted in ability to transmit to & between
humans. However transmission also occur by direct & indirect contact
with respiratory secretions (survives for up to 2 days) ,or by feces(
survives for up to 4 days).
Laboratory diagnosis was carried out using PCR for detecting SARS-
CoV RNA in clinical specimens including Respiratory samples &
faeces.
Treatment:
No specific antiviral treatment was available, although ribavirin was
used for treatment some individuals.
Corticosteroids damped down the effect of virally induced cytokine
responses that could damage tissue response to inhibit the virus. Also
protease inhibitors are useful in treatment.
-
Prevention:
With regards to potential vaccine & the correlates of protection,
neutralizing are found in convalescent human serum ( as these
antibodies to the viral spikes protein prevent virus entry & neutralize
infectivity in vitro. Whole inactivated virus & recombinant protein
vaccines have been developed to elicit neutralizing antibody response.
These have been seen in preventing SARS, although cell-mediated
immunity may also assist viral clearance & disease resolution.
Mumps virus, Measles, Rubella &other childhood exanthems.
These viruses are genetically unrelated; however, they shared several
common epidemiologic characteristics:
1- Distribution is world wide, with high occurrence in non immune
individuals.
2- Human appear to be a sole reservoir of infection.
3- person to person spread is primarily by the respiratory aaaa9
aerosol ) route.
Mumps virus:
Before the discovery of effective vaccine, the disease was a common
childhood illness, commonly called as parotitis . It is also capable of
causing meningitis, encephalitis& in adults acute orchitis.
The virus:
Mumps virus is belongs to Paramyxoviridae, which is enveloped
spherical particles with the surface spikes projecting from the envelop.
The genome has about 16000 nucleotides,
rion contains
The vi
1- RNA polymerase, haemgglutinin, neuraminidase.
2-Tthe following peptides: L( Large polymerase), HN
( haeagglutinin- neuraminidase).
3- Three fusion proteins F
0
F
1
& F
2
(plays an essential role in the
fusion of membranes. Antibodies reacting with F proteins
inhibit hemolysis caused by mumps virus & neutralise it.
4-Nucleocapsid protein( NP)( plays a central role in the
encapsidation, transcription & replication of viral RNA).
5- Matrix protein (Forms the structure which underlies the viral
envelop, also it is important in assembly of virus during the
replicative cycle).
6- Phosphoroprotein( P)& SH.
7- Four non-structural proteins designated C, V, W & I.
HN,F (V antigen )& lipid bilayer ---------------- envelop.
NP+RNA+NP=S antigen+M +P + L proteins----- neuclocapsid.
Antigenic structure of the virus:
Only one serotype of mumps virus is known. Cross reaction with Para
influenza type1 may occur mostly due to HN & F glycol-proteins,
while NP & M elicit a more type specific response. Two different
antigenic preoparations are used in the diagnostic laboratory. Mumps
V antigen (consist of HN glycoprotein) while S antigen is largely NP.
In mumps infections antibodies develop first against S antigen & only
later against V antigen.
Antibodies against HN & F proteins neutralise infectious virus, but
immuno-blot analysis reveals that all components of the virion are
immunogenic.
Epidemiology:-
1- Highest frequency observed in the 5 to 10 years age group.
Infection is rare in first year of life.
2- High infectivity is present before & after onset of illness, however,
virus has been recovered in urine for up to 14 days following onset.
3- It can occur during any season, but highest incidence during late
winter& spring months.
Pathogenesis:-
Locally replication at the site of infection (respiratory tract) mostly
followed by viremic dissemination to target tissue such as the salivary
glands & CNS, are the beginning events.
Secondary viremia can result from virus replication in target tissue
(initial parotid involvement, later spread to other organ)before
development of immune responses also occur.
Viremia is common probably as a result of direct spread from blood
into urine, as well as active viral replication in the kidney.
The tissue response is that of cell necrosis & inflammation, with
predominantly mono-nuclear cell infiltration.
In the salivary glands, swelling & desquamation of necrotic epithelial
lining cells a accompanied by interstitial inflammation & edema , may
be seen within dilated ducts.
Manifestations:-
Incubation period is 12 to 29 days with average 16 to 18 days.

Typical case is characterized by fever & swelling( Uni or lateral)
salivary glands( specially parotid glands).
Complications,which can occur without parotitis, include infection of
the following:
1- Mild meningitis due to bacterial meningitis are developed in 10 %
of all infected patients.
2- Encephalitis is occasionally sever.
3- Spinal cord & peripheral nerves : transver myelitis & polyneuritis
are rare.
4- Pancreatitis is suggested by abdominal pain & vomiting.
5- Orchitis is estimated to occur in 190 to 20 % of infected men
although subsequently sterility is a concern.
6- Oophoritis is an unusual, usually benign inflammation of the
ovarian glands.
Rare complications include: myocarditis, nephritis, arthritis,
thyroditis, thrombocytopenia purpura mastitis & pneumonia.
Occasional permanent effects such as sensorineural hearing loss &
other impairment can occur, particularly in cases of sever CNS
infection.
Immunity:
IgM antibody production is gradually replaced over several weeks by
IgG antibodies can be seen. The later persists for a lifetime but can be
often detected only by specific neutralization assays. Cellular
immunity is not clear, it may contribute both to the pathogenesis of
acute disease & to recovery from infection.
After primary infection, immunity to reinfection is virtually always
permanent.
Diagnosis:
Samples: Saliva, throat swab, CSF &Urine.
Culture:- Syncytial gaint cells & viral haemaglutinin can derive from
monkey kinder monolayer cell culture.
Viral antigen detection from pharyngeal cells & urine sediment.
Neutralization test is the most sensitive fro detection of immunity to
infection, although other serological tests such as IFAT, ELISA &
HAIT are useful in diagnosis of mumps infection.
Prevention:
Live vaccine given at 12 to 15 months of age can combined with
measles & rubella vaccines (MMR) given as a single injection. A
second dose of MMR is recommended at 4 to 6 years of age, those
who missed the second dose should receive it on later than 10 to 12

years of age. Duration of immunity, especially, if two dose regimens
is followed, appears to be more than 25 years & may be lifelong.
Measles(Rubeola) virus:-
Common names: rubeola, 5-days measles & hard measles .
Classification: It belongs to genus Morbilivirus within
Paramyxodiridae family.
Structure:-
It contains linear, negative-sense, ss-RNA, which encoded 6 viral
proteins. Of these 3 are envelope comprising a matrix (M) protein that
plays a key role in viral assembly & 2 types of glycoprotein
projections ( Peplomers).
One of these projection is Haemagglutinin(H) Which mediates
adsorption to cell surfaces;& other (F) mediates cell fusion, hemolysis
& viral entry into the cell.
No neuraminidase activity is present.
The receptor for measles virus is CD46( membrane cofactor protein),
a regulator of complement activity.
Only single serotype restricted to human infection is recognized,
however subtle antigenic variations among wild type measles strains
do occur. These variations can be determined by sequencing analyses',
enabling more precise epidemiologic tracking of outbreaks & their
origins, such ongoing molecular surveillance is also extremely
important in determining whether significant antigenic drifts evolve
overtime.
Epidemiology:-
1- Measles infection is usually sparing infants less than 6 months of
age because of passively acquired antibody, however, a shift in age-
specific attack rates to greater involvement of adolescents &young
adults was observed in some where.
2- Epidemics occur in winter & spring.
3- Highly occur in unimmunized groups.
4- Highly transmitted among subjects in classroom & household
setting with an estimated rate of 85% & more than 95 % of those
infected become ill.
5- The period of communicability is estimated to be 3 to 5 days before
appearance of the rash to 4 days afterward.
Pathogeneses:-
Viral replication proceeds in the respiratory mucosal epithelium
damage, and also promote of cell fusion with formation of syncytia,
this result in disruption of cellular cytoskeleton, chromosomal
disorganization& appearance of inclusion within the nucleus &
cytoplasm.
Replication is followed by viremic& lymphatic dissemination
throughout the host to distant sites, including, lymphoid tissue, bone
marrow, abdominal viscera & skin.
Virus can be demonstrating in the blood during the first week after
illness onset & viruria persists for up to 4 days after appearance of
rash.
During virimia both T & B lymphocytes are infected:
1-Profound depression of cell mediated immunity occurs during acute
phase of illness & persists for several weeks thereafter ( results of
virus induced down regulating of IL-12 production by monocytes &
macrophages.
2-The effects on B-lymphocytes has been shown to suppress
immunoglobulin synthesis, in addition to generation of natural killer
cell (NKC) activity appears to be impaired.
3- Susceptibility to bacterial super-infections (
β-hemolytic
streptococci), due to diminishing of polymorphnuclear leucocytes to
generate radical oxygen.
Viral antigen, nucleocapsids & giant cells can be detected in biopsy
specimens of Kopliks spots ( small white-bluish ulceration on the
buccal mucosa , opposite to lower molars .
Skin vasculitis, edema & perivascular mononuclear cell infiltrates,
hyperplastic changes of lymphoid tissues are often observed.
Sub-acute sclerosing panencephalitis , the rare late complication of
measles infection.
Immunity:-
Antibodies to the virus appear in the first few days of illness, peak in
2 to 3 weeks, & then persist at low levels.
Immunity to reinfection is lifelong & associated with the presence of
neutralizing antibody.
Defects in cell mediated immunity, particularly among patients with
low calorie of protein ( malnutrition) ,give rises in prolonged infection
with progressive viral pneumonia.
Manifestations:-
Incubation period is 7 t0 18 days, a typical illness usually begins 9 to
11 days after exposure, with cough, coryza ,conjunctivitis & fever. On
3 days after onset, pinpoint grey-whitish spots surrounded by
erythemia( sign of salt appearance) appear on mucus membranes(
Kopliks spots) are usually notable on buccal mucosa& lower molars
persists for 2 days.
Lymph-adenopathy is also common (particularly cervical nodes).

Measles can be sever in immuno-compromised or malnourished
patients& death can result from overwhelming viral infection of the
host.
Complications:
1- Bacterial super infection (mostly
by β-Streptococci) occurs in 5 to
15 % of all cases, includes: acute otitis media, mastoiditis, sinusitis,
pneumonia, sepsis, & pneumonia.
2- Encephalitis develops in 1 of 500 to 1000 cases usually 3 to 14 days
after onset of illness.
3- Acute thrombocytopenic purpura may also develop during the acute
phase of measles leading to bleeding episodes.
4- Abdominal pain & acute appendicitis can occur secondary to
inflammation & swelling of lymphoid tissue.
Diagnosis:
Measles can often be diagnosed on the basis of clinical findings.
Laboratory diagnosis is by
1- Viral isolation using oropharynx or urine samples in first 5 days,
human or monkey kidney cells or human amnion cells are optimal for
isolation attempts.
Hemadsorption or IF assays can be used to confirm measles antigens
in the inoculated cultures .
2- Serology:
Serological confirmation of measles infection depends on a fourfold
rise in antibody titer between acute & convalescent phase sera or on
demonstration of measles specific IgM antibody in single serum
specimen. HI, NT & CF tests may be used to measure measles
antibodies.
Treatment:-
No specific therapy is available other than supportive measures &
close observation for the development of complications such as
bacterial super infection. Ribavirin ( I.M) has been suggested for
patients with sever measles pneumonia, but not controlled studies
have been performed .
Prevention:_
Live, attenuated vaccine is highly immunogenic & induced lifelong
immunity; the vaccine should be administrated to infants at 12 to 15
months of age with a second dose at 4 to6 or 11 to 12 years of age.
Vaccination is contraindicated in pregnancy & immunocompromised
individuals.

Passive protection is appropriate for immuno-compromised, if
immune serum immunoglobulin (0.25 to 0.5 ml/kg I.M) is given
within 6 days of exposure, but protection is transient.
Rubella[RV] ( German measles) viral infection:-
Infection by rubella virus is often mild, or even asymptomatic.
The major concern is the profound effects on developing fetuses,
resulting in multiple congenital malformations.
Historical view:
In 1881, Rubella is accepted as a distinct disease by international
congress of medicine.
In 1938 first evidence to show that rubella caused by virus .
In 1941Teratogenic effects of rubella first recognised by Gregg in
Australia .
1962 Rubella virus isolated in cell cultures. Neutralisation test
developed.
1965 to 1967 Development of attenuated vaccine strains & first
vaccine trails.
In 1986 Rubella virus genome sequenced.
In 2000 WHO recommends immunisation policies for elimination of
Congenital rubella syndrome(CRS).
In 2002 57% of countries/territories include rubella vaccination in
national immunization programmes.
Virus classification:-
RV is classified as a non-earthropod-borne togovirus ,& is member of
genus Rubivirus.
Structure:-
The diameter of virus particle is 58± 7 nm, while the nucleocapasid is
33± 1 nmin diameter & surrounded by ss-RNA, positive sense RNA.
The virion consists of 2 membrane-bound glycoproteins,E1( 58KDa)
& E2( 42-47KDa)& C ,a non glycosylated capsid protein.
The symmetry of the nucleocapsid is icosahedron, with 32 capsomers.
The lipoprotein envelope bears surface of spikes of 5 to 8 nm
composed of 2 glycoproteins.
Virus particle being pleomorphic(elliptical & oblong) ,so the envelope
has non rigid delicate character.
The base composition of the genome is G 30.8 %,C 38 .7 % ,A 14.9 %
& U 15.4 %.
Epidemiology:-
1- Virus has high infectivity, but low virulence & are usually observed
during winter & spring months.

2- Childbearing women are the major concern.
3- Patients with primary acquired infections are contagious from 7
days before to 7 days after the onset of rash.
4- Congenitally infected infants may spread the virus to others for 6
months or longer after birth.
Clinically rubella infection can be classified as:
1- Postnatal rubella:-
A- Incubation period ranges from 2 to 3 weeks, initial viral replication
occurs in RT, followed by multiplication in cervical lymph nodes.
B- Viremia develops after 5-7 days & lasts until the appearance of
antibody on about 13-15 days.
C- The development of antibody coincides with the appearance of
rash, suggesting an immunologic basis for the rash.
D- After rash appearance, the virus detectable only in nasopharynx.
E- In about 25 % of cases, primary infection is subclinical.
Clinical findings:
Infection usually begins with malaise, low grade of fever.
Rash ( on face , extends over trunk& extremities& lymphadenopathy(
posterior auricular & sub occipital) may occur without systemic
symptoms.
Transit arthralgia & arthritis are commonly seen in women.
Rare complications include thrombocytopenic purpura & encephalitis.
Rash caused by rubella is similar to that caused by other viruses such
as enteroviruses, so the diagnosis is difficult.
Immunity:-
AS the rash fades, antibody titer rises rapidly over the next 3 weeks,
mostly consists of IgM that generally persist beyond 6 weeks after the
illness.
IgM antibodies found in a single serum sample obtained 2 weeks after
the rash give evidence of recent rubella infection.
IgG rubella antibodies usually persist for life.
Immune mothers transfer antibodies to their offspring, who are then
protected for 4-6 months.
Laboratory diagnosis:
1- Isolation & identification of virus:-
Naso-pharyngeal or throat swabs taken within 3-4 2days after symptoms appear are
the best source of rubella virus.
Tissue culture of cell lines of monkey (BSC1,Vero) or rabbit( RK-13,SIRC) origin
may be used.

Absolute identification of an isolate requires specific neutralization with reference
rubella antibody.
2- serology:-
The standard serological test for rubella is HI test, serum must be treated to remove
nonspcific inhibitors before treatment. C.F. tests are limited usefulness.
ELISA test is useful test to detect specific IgM.
Detecting of IgG is evidence of immunity.
To accurately confirm a recent rubella infection,( Critically important in the case of
pregnant woman), either a rise in an antibody titer must be demonstrated between 2
serum samples taken at least 10 days apart, or rubella specific IgM must be detected in
a single specimen.
Treatment:
Rubella is mild & self limit illness & no specific treatment is given.
Therapeutic abortion is the only means of avoiding the risk of malformed infants in
such cases.
Immunoglobulin should be administrated in cases in which infections occur early in
pregnancy & termination of pregnancy will not be considered.
Prevention & control:
A live attenuated rubella vaccines have been available since 1969, as HPV77, which
replaced by RA27/3, that may produce much higher antibody titer, when it was given
either as a single antigen or combined with measles& mumps vaccine.
The vaccine induces immunity at least 95 % of recipients,& that immunity endures for
at least 10 years.
Mild fever & lymph-adenopathy & a feeling rash may appear in spite of the vaccine is
safe.
Rubella vaccine can cross the placenta & infect the fetus, but it's not teratogenic.
It may be wise for all pregnant women to undergo a serum antibody test for rubella &,
if found to be susceptible, receive a vaccination immediately after delivery.
2- Congenital Rubella:_
Maternal viremia associated with rubella infection during pregnancy may result in
infection of the placenta & fetus. Timing of the fetal infection determines the extent of
teratogenic effect, in first trimester; rubella infection can produce more damage to
fetus, that lead to abnormalities in the infant in about of 50 %, while the rates were 20
% & 4 %. in second & third trimesters respectively .
Rubella infection can also result in fetal death& spontaneous abortion.
Intra-uterine infection with rubella is associated with chronic persistence of virus in
the newborn. At birth, virus is easily detectable in pharyngeal secretions, multiple
organs, CSF, urine& rectal swabs.
Viral excretion may last for 12-18 months after birth, but the level of shedding
gradually decreases with age.

Clinical manifestations:
It can be grouped into 3 categories:
1- Transient effects in infants.
2- Permanent manifestations that may be apparent at birth or become recognized
during the first year. The most common are Congenital heart disease (patent ducts
arteriosus , pulmonary & aortic stenosis, pulmonary valvular sdtyenosis& ventricular
or atrial septal defects), Total or partial blindness( cataracts, glaucoma, chorioretinitis)
& necessary deafness.
3- Development of abnormalities that appear & progress during childhood &
adolescence. Such as mental retardation, problems with balance & motor skills
develop in preschool children.
There is a 20 % mortality rate among congenitally virus infected infant symptomatic
at birth. Progressive rubella pan-encephalitis, a rare complication can develop in the
second decade of life in children with congenital rubella.
Immunity:
In infants infected in utero, persistence of rubella virus causes a rising titer of rubella
specific IgM & a rise in specific IgG level that persists long after the fall of in
maternal IgG.
Maternal rubella IgG is transferred to infants & is gradually lost over a period of 6
months.
Epidemiology:
Congenitally infected infants who shed virus can transmit rubella to susceptible
contacts, such as the nurses & physicians caring for them.
Persons at risk should therefore avoid contact with these babies..
Mortality rates vary, depending on the timing of maternal infection & the particular
congenital defects.
Diagnosis:-
Congenitally acquired rubella infected infants' sheds large amount of virus in
pharyngeal secretions& other body fluids for up to 18 months of age .
Virus has been recovered from many tissues tested post-mortem.
Demonstration of IgM antibody in infants is diagnostic of congenital rubella.
IgM antibodies do not cross the placenta, so their presence indicates that may have
synthesized by the infant in utero.
Children with congenital rubella exhibit impaired cell-mediated immunity specific for
rubella virus.
Treatment:-
There is no specific treatment for congenital rubella. Many abnormalities can be
corrected by surgery or may responds to medical therapy. Specific lesions atre

managed clinically without regard to the fact that they resulted from rubella virus
infection.
Prevention:
Live attenuated rubella vaccine is indicated for children & hospital workers.
Vaccine does not produce defects in fetus.
Vaccine induced immunity may be lifelong.
The vaccine is contraindicated in immuno-compromised patients & in pregnancy. It is
strongly recommended that immunization be avoided in this setting & that non
pregnant women avoid conception for at least 3 months after receiving the vaccine.
Parvovirus B19 infections:-
They are very small (18 to 26 nm), naked virions that contain a linear ss-DNA
molecule. Parvovirus B19 encodes 3 capsid proteins( VP1,VP2& VP3).
Parvoviruses have been recognized among nonhuman hosts for a number of years.
Notably among these are canine parvovirus & feline panleukopenia, which produce
sever infections among puppies& kittens. These do not appear to cross species
barriers. The human parvovirus B19 has been well described, but its origin is unclear.
The virus can be cultured on human bone marrow cells, fetal liver cells, hematopoietic
progenitor cells generated from peripheral blood& a megakaryocytic leukaemia cell
line.
Globoside(also known as blood group P antigen, which is commonly found on
erythroid progenitors, erythroblasts, megakaryocytes & endothelial cells) is the major
cellular receptor for the virus.
Nucleus of immature cell in the erythrocyte lineage is primary replication site of the
virus. Such infected cells then cease to proliferate, resulting in an impairment of
normal RBC development.
Primary infections in sickle cell& thalassemia patients can produce an acute, sever &
sometimes fatal anemia manifested as rapid fall in RBC count & haemoglobin . A
plastic crisis develops in patients with chronic haemolytic anemia.
Parvovirus B19 has also been occasionally implicated as a cause of persistent bone
marrow failure & an acute hemophagocytic syndrome.
Erythema infectiosum:-
Is common disease that is clearly attributed to parvovirus B19.After 4 to 12 days as
incubation period, a mild illness appears, characterized by fever, malaise, headache,
myalgia, &itching in very degrees. A confluent, indurate rash appears on the face,
giving a slapped-cheek appearance. Within the next 2 days ,rash will spread to other
area such as arms & legs.
During the acute phase generalized lymphadenopathy or splenomegaly may be seen,
along with mild leukopenia & anemia.
The illness lasts 1 to2 weeks, but rash may recur for 2 to 4 weeks, thereafter
exacerbated by heat, sunlight, exercise, or emotional stress.
Serious complications such as hepatitis, thrombocytopenia, nephritis, or encephalitis
are rare.
transplacental transmission
is occasionally sever ( due to the parvovirus
Fatal infection
like rubella virus),resulting in stillbirth of fetuses. The progress can be sever that
hypoxic damage to the heart, liver, & other tissue leads to extensive edema( hydrops
fetalis).
is primarily by the respiratory route, with high occurrence in households
Transmission
specially during the spring months. Incident rate is high among children & young
adults.
Diagnosis:-
Detection requires DNA probe or PCR methods.
The presence of IgM specific antibody late in the acute phase or during convalescence
strongly supports the diagnosis.
Roseola Infantum( Exanthem Subitum):-
Is the common illness observed in infants & children 6 months to 4 years of age. Its
alternative name exanthema subitum means sudden rash.
Roseola has more than one cause such as herpesvirus type 6& less frequent
herpesvirus type 7. Several other agents including adenoviruses , coxsakieviruses &
echoviruses.
The illness is characterized by abrupt of high fever, sometimes accompanied by
generalized convulsion & leukopenia. After 2 to 3 days the fever diminishes rapidly,
followed in a few hours by a faint, transient, macular rash.
Other causes of rubella like rashes:
Other agents can mimic rubella involves:
1- Arboviruses such as dengue, Epstien-Barr virus, scarlet fever & drug toxic
eruptions.
2- Serotypes of echoviruse at least 17 serotypes & 9 coxsackieviruses.
Because of the wide variety of diagnostic possibilities, it is not possible to diagnose, or
rule out rubella confidently on clinical grounds alone. Therefore, a specific diagnosis
requires specific laboratory studies.
Arthropoda-Borne ( Arboviruses) & other Zoonotic viruses
Arboviruses are a group of infectious agents that are transmitted by
blood sucking arthropods from one vertebrate host to another.
Replication in the vertebrate host produces viremia high enough titer
that other blood feeding arthropods will be infected.
The major arbovirus diseases worlds wide are yellow fever, dengue,
Japanese B encephalitis, ST.Louis encephalitis, western& eastern

equine encephalitis, Russian spring summer encephalitis, West Nile
fever & sand fly fever.
The zoonotic viruses are divided into two groups. The arboviruses are
transmitted to humans by infected bloodsucking insects such as
mosquitoes, ticks & phlebotomus flies (sand fly).
The other zoonotic RNA viruses are transmitted by inhalation of
inflected animal excretions, by the conjunctival route, or occasionally
by direct contact with infected animals.
Rabies virus is commonly transmitted by animal bites.
-
Classificati on:
Classification:-
They are more than 450 arboviruses & rodent viruses: of these about 100 are known
pathogens for humans. They are classified according to their chemical & physical
properties& their antigenic relationships. Also they classified after the geographic area
where the virus was first isolated, or named after disease( dengue, yellow fever).
1- Togoviruses:-
A-They are enveloped virion containing ss-RNA
–positive sense RNA measuring 40
to 70nm.
B- The envelope contains a haemagglutinin &lipoprotein.
C-Virions mature by budding from cellular membranes.
D-Replication can occur in cells of infected arthropods & vertebrate hosts.
E-The viruses are inactivated by acid pH, heat, organic solvents& detergents.
F-They are transmitted between vertebrates by mosquitoes or other blood feeding
arthropods.
H
—Rubella virus is classified in separate genus, has no arthropod vector & is not an
arbovirus.
2-Flaviviruses:
A- This family consists about 70 viruses, measures 45 to 60 nm that have ssRNA,
positive-sense RNA
B-The envelope conatians glycoprotiens & lipid.
C- Virions mature by budding in cytoplasm& through cytoplasmic membrane (
endoplasmic reticulum).
D-Flaviviruses are transmitted d between vertebrates by mosquitoes & ticks.
E- The viruses are inactivated by acid pH, heat, organic solvents& detergents.
H- Hepatitis C virus, classified in separate genus , has no arthropod vector.
3- Bunyaviruses:-
A- Sperical particle contain a ss-RNA, negative sense or ambiesense, triple
segmented RNA genome 11-21 kb in total size.
B- The envelope contains two glycoproteins & lipid, measure 80 to 120 nm.
C-They mature by budding into smooth surfaced vesicles in or near the Golgi region
of infected cell.
D- Transmission either by sand flies or by trans-ovarian occurs by some ticks &
mosquitoes. While Hantavirus pulmonary syndrome is caused by a virus transmitted
by deer mice .
E- They are sensitive to inactivation by heat, detergents, formaldehyde & low pH &
some are haemagglutinating.
4- Reoviruse:-
A- They are spherical, enveloped Ds-RNA viruses, measures about 80 nm,with
segmented genome.
B- The most important North American arbovirus of this family, which is a member of
the genus Coltivirus, causes Colorado tick fever.
They transmitted by ticks.
5- Arenaviruses:-
A- They are envelioped, spherical or pleomorphic viruses, contasining ss-RNA,
negative sense RNA in several segments & measuring 50 to 300 nm in diameter.
B- They mature by budding from host cell cytoplasm membrane& contain host cell
ribosomesr in their interior. The ribosomes confer a granular appearance to the
viruses, hence the name ( frtom Latin arenosus for sandy).
C- The most common & serious disease to humans caused by the members of this
family is haemorrhagic fevers, including: Lassa fever.
D- The virus of lymphatic chorio-meningitis is occasionally transmitted to humans
from infected mice & other rodents.
6- Filoviruses:
A- Long filamentous particles of varying length 80 nm in diameter& 300 to 1400 nm
in length.
B- They are enveloped, ss-RNA ,negative sense RNA viruses, non segmented
genonme.
C- They mature by budding from cellular membranes.
D- They are sensitive to inactivation by heat, lipid solvents & bleach.
E- They are the cause of Marburg & Ebola fevers, two highly fatal haemorrhagic
fevers.
H- The natural host & vectors, if any, are unknown.
7- Rhabdoviruses:
A- Several bulleted shaped arboviruses fall into this group, the genome is ss-RNA,
negative sense RNA, non segmented& linear .
B-The envelope is a ribonucleocapsid with spikes ( peplomers) composed of trimers of
glycoprotein G.

C- They are inactivated by CO2, on dry ice; therefore it must be stored in glass-sealed
vials. Rabies virus rapidly killed by UV exposure or sunlight, by heat ( I hr at 50 C),
by lipid solvents, by trypsin, by detergents & by extremes of pH.
C- Replication: cytoplasm, virus matures by budding from plasma membrane.
D- Wide array of viruses with broad host range. Group includes the deadly rabies
virus, belong to genus Lyssavirus, and has no arthropod or rodent virus.
Epidemiology:-
Arboviruses involves non human vertebrates such as birds, small mammals & monkey
,others transmitted between humans & mosquitoes.
In general the infection is transmitted within the host species by arthropods
( e.g. Mosquitoes & ticks),in some cases maintained from generation to generation by
transovarial transmission. Infection does not appear to harm the insect.
Sustained viremia required for vertebrate host to be significant reservoir.
Season to season survival has multiple mechanisms.
There are 3 basic cycles of arbovirus transmission:
1- Urban cycle: this cycle is favour by the presence of relatively large number of
human living in close to arthropod( usually mosquito) species capable of virus
transmission. Examples to this cycle include dengue, urban yellow fever.
2- Sylvatic cycle:-
A single nonhuman vertebrate reservoir may be involved & human becomes a
tangential host through accidental intrusion into a zoonotic transmission cycle.
Examples: western, eastern equine encephalitis& California virus.
3- Arthropod- sustained: by tick transovarial transmission .The climate & ecological
conditions such as swamps & ponds are optimal for arthropod breeding & egg
hatching ,arbovirus amplification may begin.
Pathogenesis:-
1- Central nervous system is primarily affected leading to aseptic meningitis or
meningoencephalitis. The CNS pathology consists of meningeal & perivascular
mononuclear cell infiltrates, degenerating of neurons with neuronophagia.
2- Liver damage includes hyaline necrosis of hepatocytes producing cytoplasmic
eosinophic masses called Councilman bodies as in yellow fever.
3- Haemorrhagic fever in which damage is particularly sever to small blood vessels
with skin petechiae ; intestinal & other haemorrhages. Haemorrhage mostly due to the
lack of liver produced clotting factors as a result of liver necrosis.
4- Dengue haemorrhagic fevers involve perivascular & endothelial injury, often
complicated by shock. The major vascular abnormalities, may provoked by circulating
virus-antibody complexes (immune complex) that mediate activation of complement
& subsequent release of vasoactive amines.
Immunity:
1- Typical patterns of antibody response after arbovirus infection can be
assessed using HI, CF, neutralization & precipitation tests.
2-The rise in antibody titer generally correlates with recovery from infection.
3- Neutralizing antibodies, which are the most serotype specific, generally
persist many years after infection.
4- The IgM specific antibodies indicate that primary infection likely occurred
within previous 2 months.
5- Activation of previously sensitized T- cells by viral antigen present on the
surface of macrophages may result in release of cytokines, which mediate the
development of shock & haemorrhage.
5- Cellular & humoral immunity to reinfection are serotype specific & appear
to be permanent.
Diagnosis:
1-Blood is best source but must be early in disease.
2-Virus can be detected in CSF or affected tissue by reverse transcriptase PCR.
3-Sometimes by culturing during the acute phase of illness .
4- Various tests have been used including : HI,CFT,ELISA & NT.
Treatment :
Treatment is only supportive care; ribavirin has been used on occasion.
Prevention:
1- Protection from bites & vector control are primary prevention.
2-Yellow fever vaccine ( 17d strain) is used to protect rural populations exposed to
sylvatic cycle & international travellers to endemic area.
Other RNA viruses of zoonotic origin:
-
Arenaviruses:
1- Sustained in small rodent reservoirs.
2- Vertical transmission usually leads to chronic lifelong viremia .
3- Spread to humans by aerosols & close contact.
4-Person to person spread occurs by contact with body fluid.
5- All species cause fever, shock & haemorrhage.
6- Hepatitis & myocarditis also occur with Lassa fever.
7- High mortality & risk of further transmission.
8- The diagnosis is suggested by clinical finding & travel history. Virus isolation &
serology may be performed only in reference centres.
9- Treatment is supportive & IV ribavirin is helpful in Lassa fever.
Lymphocytic Choriomeningitis virus:
1-Virus is common in hamsters& mice, most human illness have been traced to
contact to rodent breeding colonies in research or pit supply centres.

2- The illness usually consist of headache, fever & myalagia, CNS infection may
persist as long as 3 months.
3- Transplacental infection can occur in human resulting in fetal death,
hydrocephaly& chorioretinitis.
4- No person to person transmission of infection has been documented.
5- Diagnosis by culturing of blood & CSF into mice or guinea pigs& serological test is
by IFAT.
Filvoviruses: Marburg & Ebola viruses:
1- Initial cases are transmitted from monkeys in 1967 as Marburg virus
2- Antigenitically Marburg virus are differ from Ebola virus recorded in 1976 in
Northern Zaire.
3- Small mammals( rodents) are reservoirs.
4- Mortaltiy is high in symptomatic infection.
5- Diagnosis & precautions similar to arenavirus haemorrhagic fevers.
Hantaviruse( Hantavirus haemorrhagic fever):
1- Also called Korean haemorrhagic fever( KHF) was first recorded in 1978, when the
antigen was detected in the lung tissues of wild rodent by IFAT using convalescent
sera from affected patients.
2- KHF virus is responsible for haemorrhagic-renal failure syndrome, also it called
neppheropathia epidemica..

