pancreas
DEFINITION
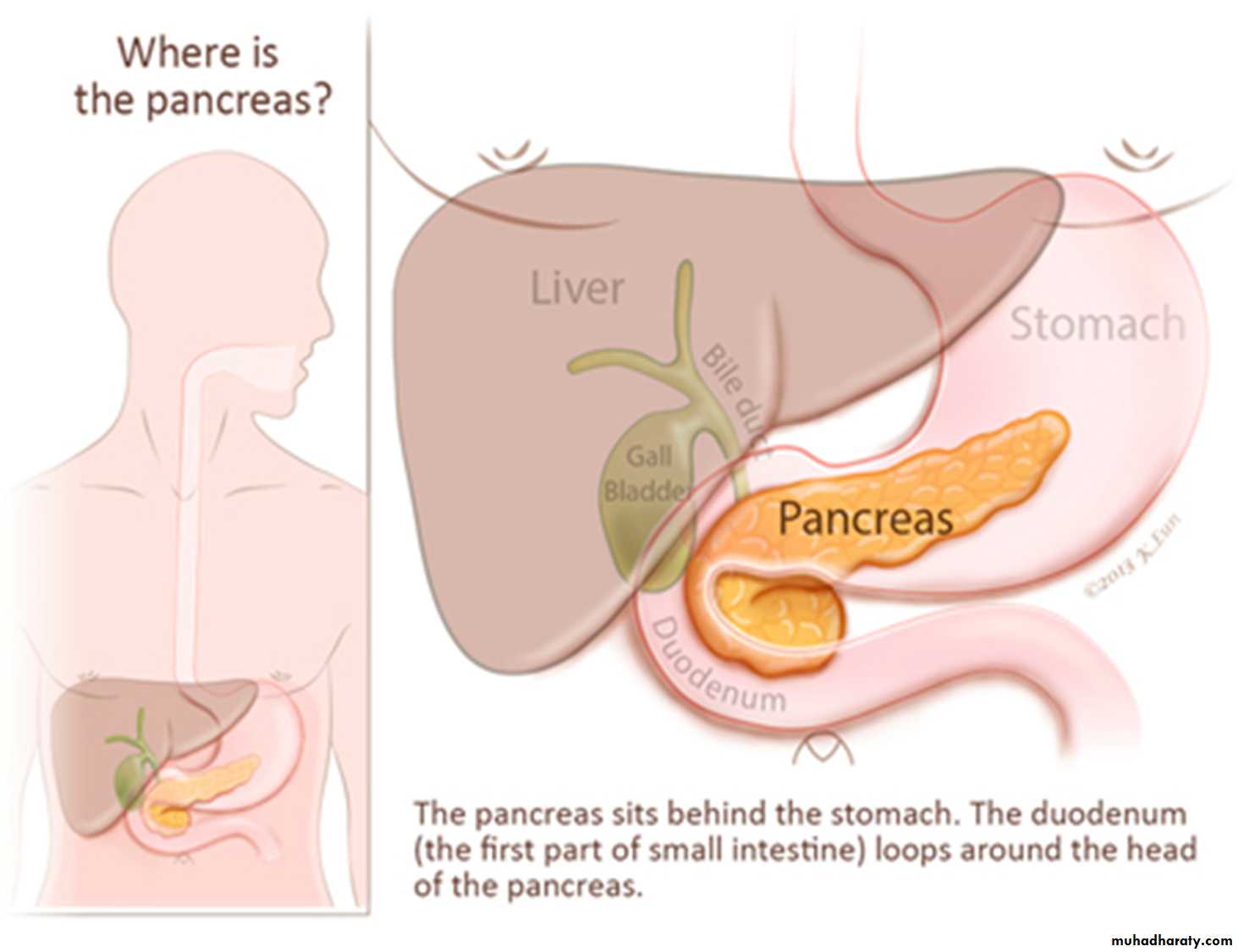
The pancreas (pan= all , kreas = flesh) is a gland that is partly exocrine and partly endocrine. The exocrine part secretes the digestive pancreatic juice, and the endocrine part secretes hormones, eg. Insulin.It is soft, lobulated and elongated organ.
It is J – shaped or retort shaped, set obliquely. The bowl of the retort represents its head , and the stem of the retort , its neck , body and tail.
It is about 15-20 cm long
2.5-3.8 cm broad and 1.2-1.8 cm thick and weighs about 90 g
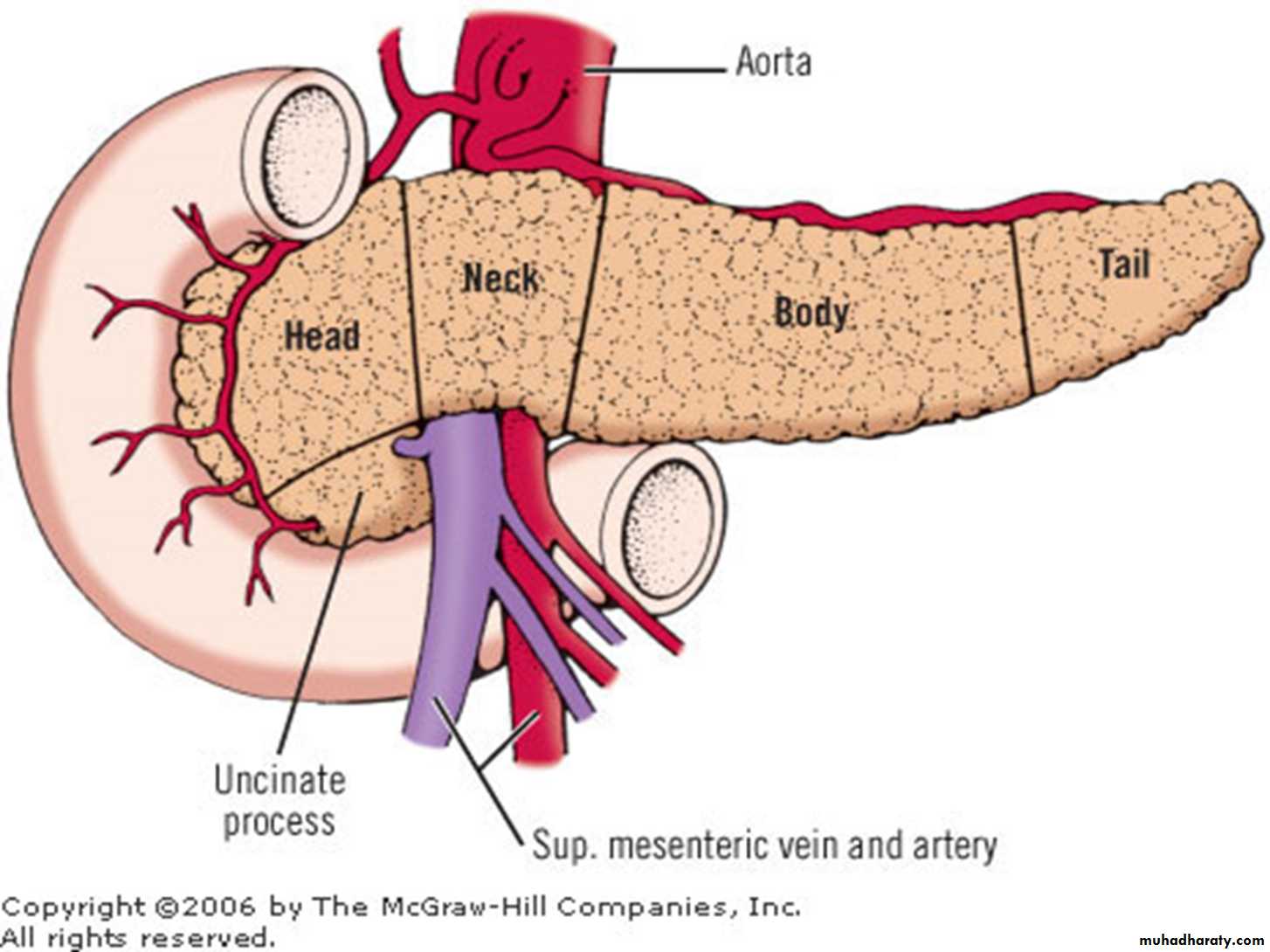
The pancreas is divided( from right to left ) into the head , the neck, the body and tail.
The head is enlarged and lies within the concavity of the duodenum.The tail reaches the hilum of the spleen.
The entire organ lies posterior to the stomach separated from it by the lesser sac.
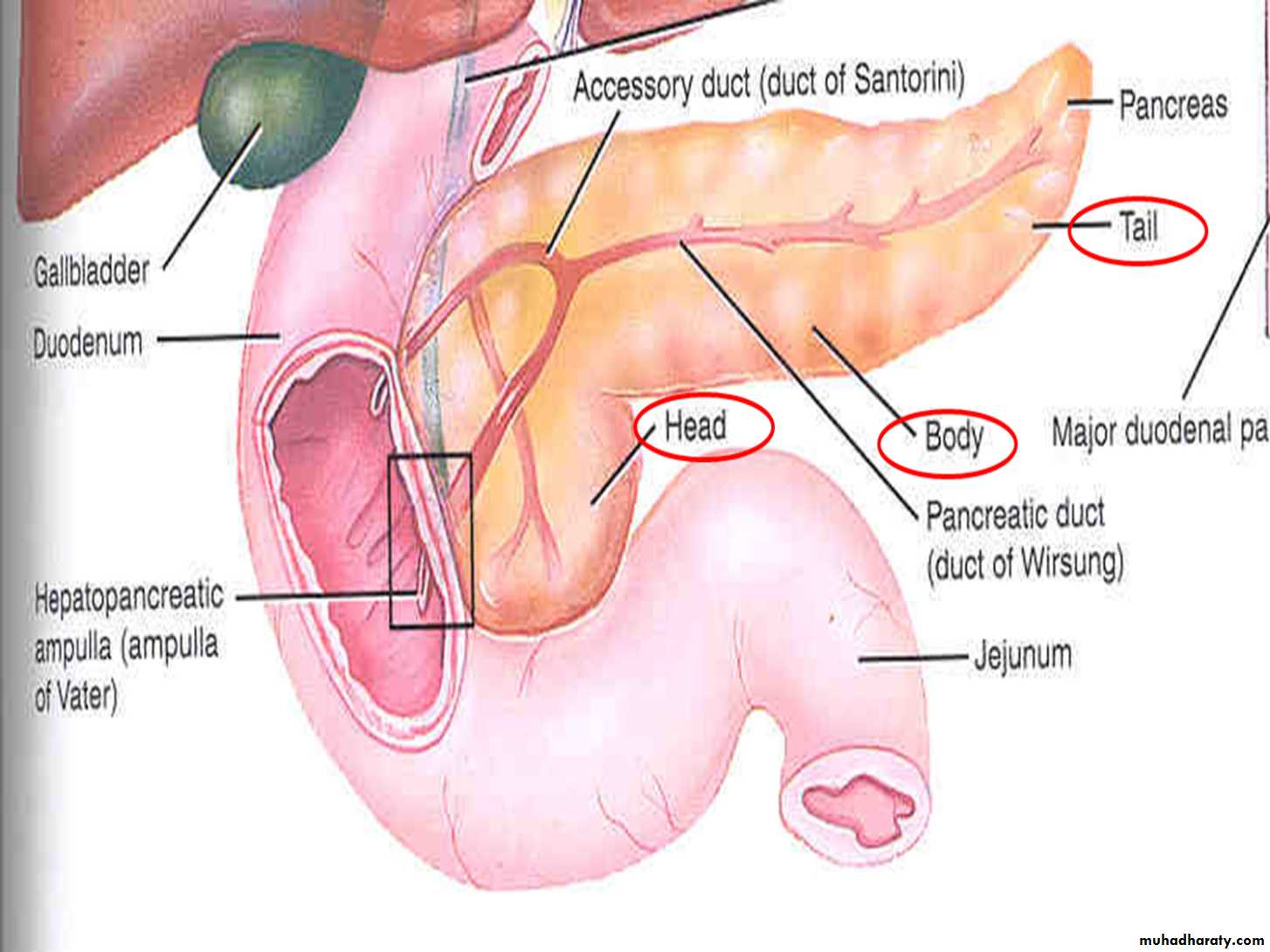
Ducts of the pancreas
The exocrine pancreas is drained by two ducts,1.The main pancreatic duct (duct of wirsung)
2. the accessory pancreatic duct( duct of santorini)
Blood Supply of Pancreas
Arterial:Pancreatic Branches of splenic artery
Superior pancreaticoduodenal artery
Inferior pancreaticoduodenal artery
Venous:
Drain into splenic, superior mesenteric and portal veins
Lymphatic drainage
Head & Neck – Pancreaticoduodenal
Body & Tail - Pancreaticosplenic
Functions of pancreas
THE EXOCRINE PANCREASThis consists of a large number of lobules made up of small acini, the walls of which consist of secretory cells.
Each lobule is drained by a tiny duct and these unite eventually to form the pancreatic duct, which extends the whole length of the gland and opens into the duodenum.
The function of the exocrine pancreas is to produce pancreatic juice containing enzymes that digest carbohydrates , proteins and fats.
The endocrine pancreas
Clusters of endocrine cells distributed throughout called Islets of LangerhansIslet:
75% - B Cells – Insulin
20% - A Cells – Glucagon
5% - D Cells – Somatostatin
Small number of pancreatic polypeptide cells
B cells form inner core surrounded by other cells.
Capillaries draining islet cells drain into portal vein.
INVESTIGATIONS
Serum enzyme levels Pancreatic function tests MorphologyUltrasound scan
Computerised tomography
Magnetic resonance imaging
Endoscopic retrograde cholangiopancreatography
Endoscopic ultrasound
Plain radiography Chest Upper abdomen
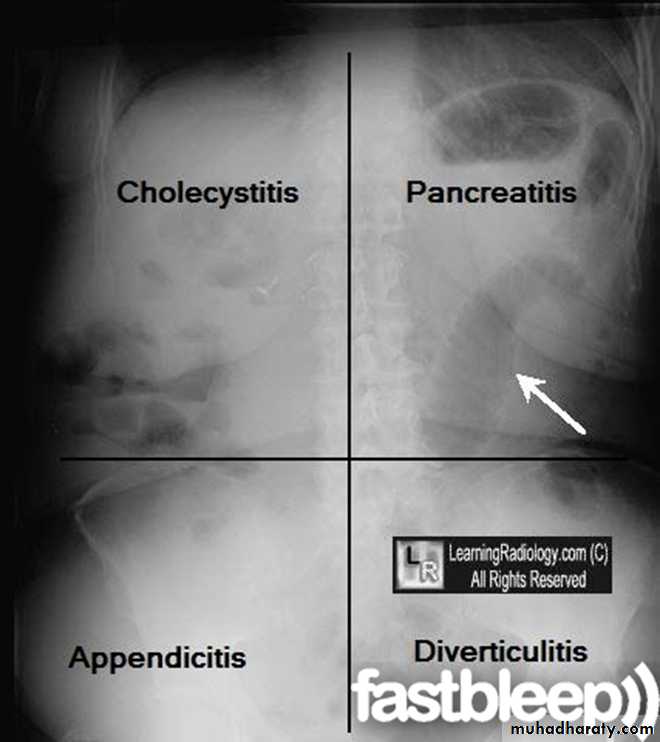
Causes of raised serum amylase level other than acute pancreatitis
■ Upper gastrointestinal tract perforation■ Mesenteric infarction
■ Torsion of an intra-abdominal viscus
■ Retroperitoneal haematoma
■ Ectopic pregnancy
■ Macroamylasaemia
■ Renal failure
■ Salivary gland inflammation
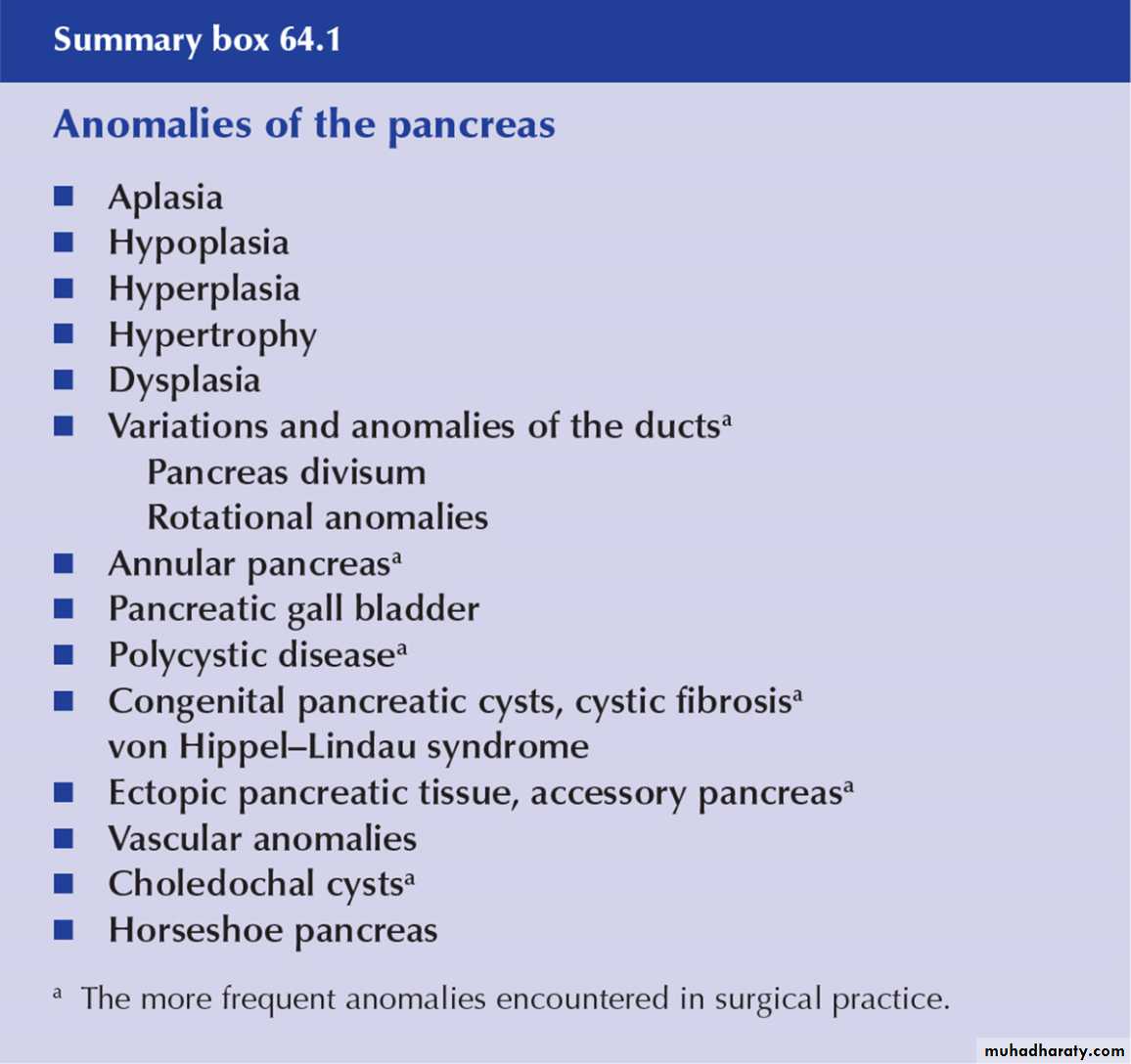
Annular pancreas
This is the result of failure of complete rotation of the ventral pancreatic bud during development, so that a ring of pancreatic tissue surrounds the second or third part of the duodenum.
It is most often seen in association with congenital duodenal stenosis or atresia and is therefore more prevalent in children with Down’s syndrome.
Duodenal obstruction typically causes vomiting in the neonate The usual treatment is bypass (duodenoduodenostomy).
The disease may occur in later life as one of the causes of pancreatitis, in which case resection of the head of the pancreas is preferable to lesser procedures.
Ectopic pancreas
Islands of ectopic pancreatic tissue can be found in the submucosa in parts of the stomach, duodenum or small intestine (including Meckel’s diverticulum), the gall bladder, adjoining the pancreas, in the hilum of the spleen and within the liver.Ectopic pancreas may also be found in the wall of an alimentary tract duplication cyst
INJURIES TO THE PANCREAS
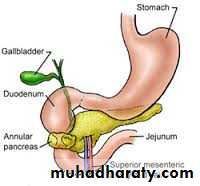
The pancreas, thanks to its somewhat protected location in the retroperitoneum, is not frequently damaged in blunt abdominal trauma.Penetrating trauma to the upper abdomen or the back carries a higher chance of pancreatic injury.
Pancreatic injuries may range from a contusion or laceration of the parenchyma without duct disruption to major parenchymal destruction with duct disruption (sometimes complete transection) and, rarely, massive destruction of the pancreatic head.
Diagnosis
1: history and examinations2: A rise in serum amylase occurs in most cases. 3: A CT scan of the pancreas will delineate the damage that has occurred to the pancreas.
4: If there is doubt about duct disruption, an urgent ERCP should be sought.
5: MRCP may also provide the answer,
Treatment
1: nothing by mouth2: intravenous fluid and antibiotic
3: if the patient vitally stable with no signs of peritonitis and no major duct disruption can be managed conservatively.
4: in penetrating injury laparotomy indicated
Pancreatic fistula
Pancreatic fistula usually follows:1: operative trauma to the gland or
2: may occur as a complication of acute or chronic pancreatitis.
It is important to define the site of the fistula and the epithelial structure with which it communicates (e.g. externally to skin, or internally to bowel).
If there is uncertainty about whether the fluid issuing from a drain site or a wound is pancreatic, measurement of the amylase content will be diagnostic
Management
Tests
■ Measure amylase level in fluid
■ Determine the anatomy of the fistula
■ Check whether the main pancreatic duct is blocked or disrupted
management
■ Correct fluid and electrolyte imbalances■ Protect the skin
■ Drain adequately
■ Parenteral or nasojejunal feeding
■ Octreotide to suppress secretion
■ Relieve pancreatic duct obstruction if possible (ERCP and stent)
■ Treat underlying cause
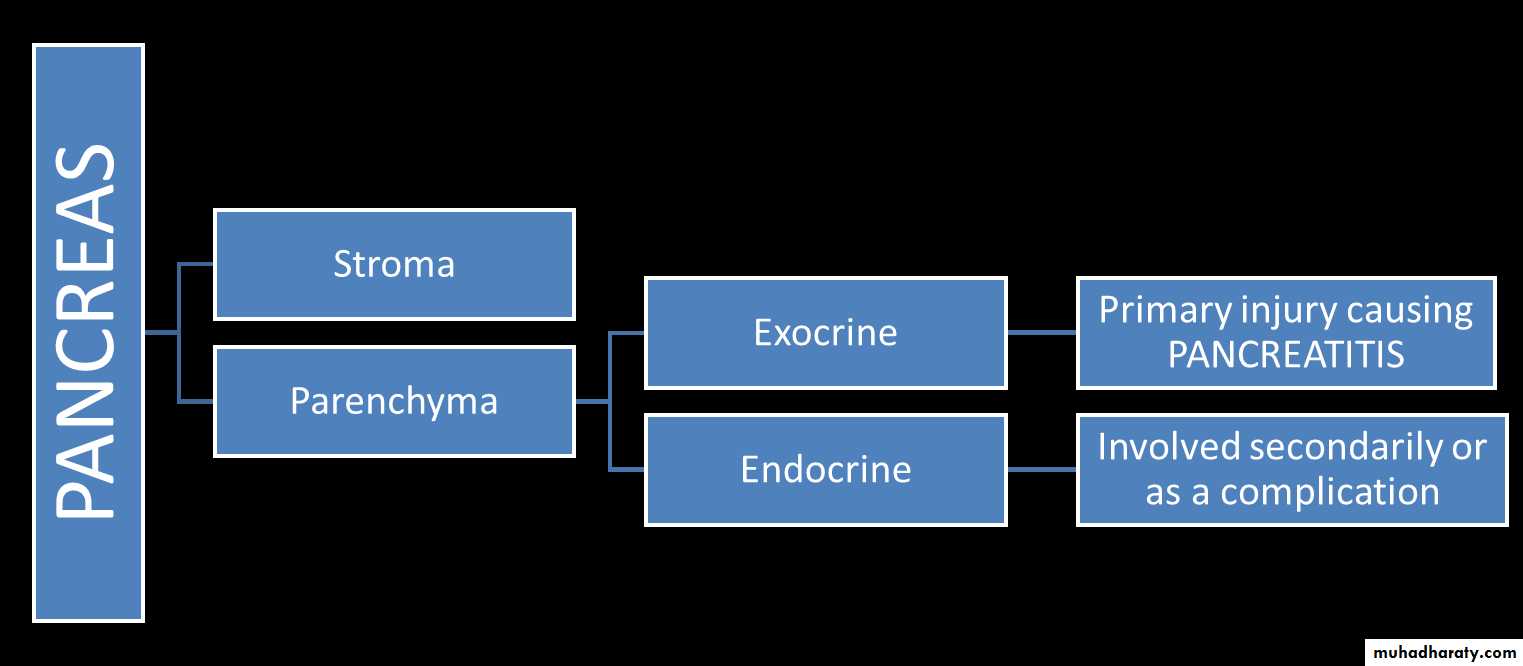
Pancreatitis
Classification
ACUTE PANCREATITIS
CLINICAL DEFINITIONAn acute condition presenting with abdominal pain-usually associated with raised blood/urine pancreatic enzymes as a result of pancreatic inflammation
PATHOLOGICAL DEFINITION
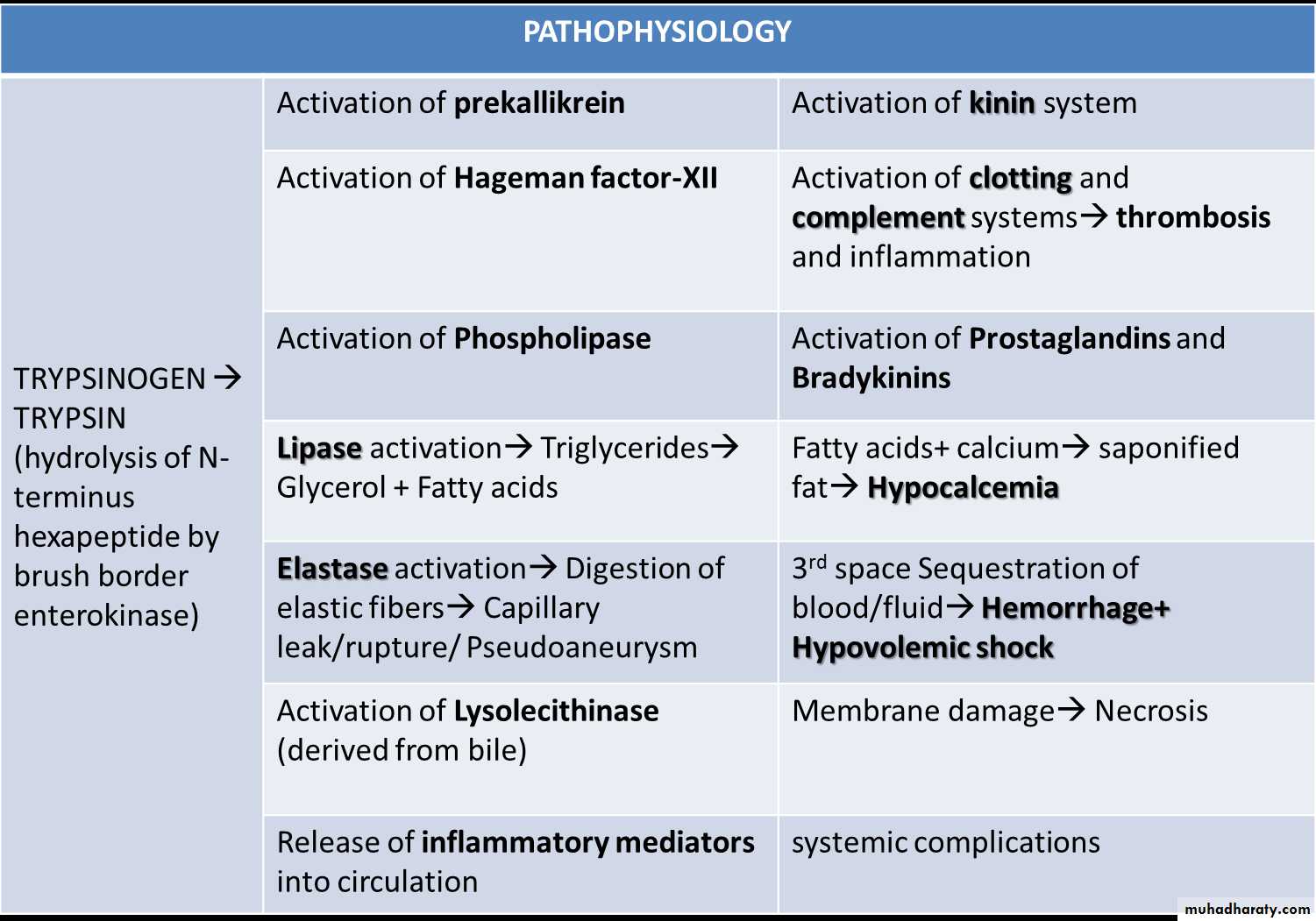
Reversible pancreatic parenchymal injury associated with inflammationPATHOPHYSIOLOGY
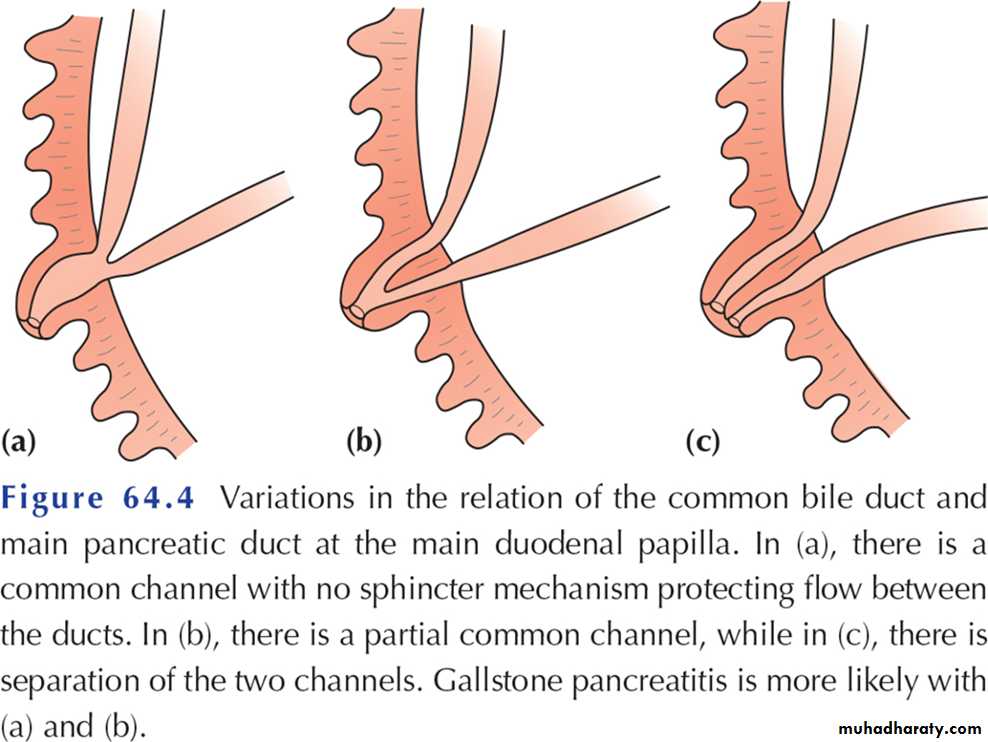
Autodigestion of pancreatic substance by inappropriately activated pancreatic enzymes (especially trypsinogen)Possible causes of acute pancreatitis
Gallstones■ Alcoholism
■ Post ERCP
■ Abdominal trauma
■ Following biliary, upper gastrointestinal or cardiothoracic surgery
■ Ampullary tumour
■ Drugs (corticosteroids, azathioprine, asparaginase, valproic acid, thiazides, oestrogens)
■ Hyperparathyroidism
■ Hypercalcaemia
■ Pancreas divisum
■ Autoimmune pancreatitis
■ Hereditary pancreatitis
■ Viral infections (mumps, coxsackie B)
■ Malnutrition
■ Scorpion bite
■ Idiopathic
presentations
ABDOMEN PAIN-Cardinal SymptomSITE: usually experienced first in the epigastrium
but may be localized to either upper quadrant or felt diffusely throughout the abdomen or lower chestONSET: characteristically develops quickly, generally following substantial meal and precedes NV
SEVERITY: frequently severe, reaching max. intensity within minutes rather than hours
NATURE: “boring through”, “knifing” (illimitable agony)
DURATION: hours-days
COURSE: constant (refractory to usual doses of analgesics, not relieved by vomiting)
RADIATION: directly to back(50%), chest or flanks
RELEIVING FACTOR: sitting or leaning/stooping forward ()
due to shifting forward of abdominal contents and taking pressure off from inflamed pancreas
AGGRAVATING FACTOR: food/alcohol intake, walking, lying supine
_______________________________________________________________________________
General Physical Examination
Appearance: well gravely ill with profound shock, toxicity and confusionVitals: Tachypnea(and dyspnea-10%), Tachycardia(65%), Hypotension, temp high(76%)/normal/low (acute swinging pyrexia in cholangitis)
Icterus(28%)
gallstone pancreatitis or due to edema of pancreatic headCyanosis
Improper lung perfusionPallor, cold clammy skin,diaphoretic
ABDOMEN EXAMINATIONTenderness + Rebound tenderness:
epigastrium/upper abdomen
Distension:
Ileus(BS decreased or absent)ascites with shifting dullness
Mass in epigastrium(usually absent)
due to inflammation
Guarding(also called “defense musculaire” )-upper abdomen
tensing of the abdominal wall muscles to guard inflamed organs within the abdomen from the pain of pressure upon them(i.e. during palpation)Rigidity(involuntary stiffness)-unusual
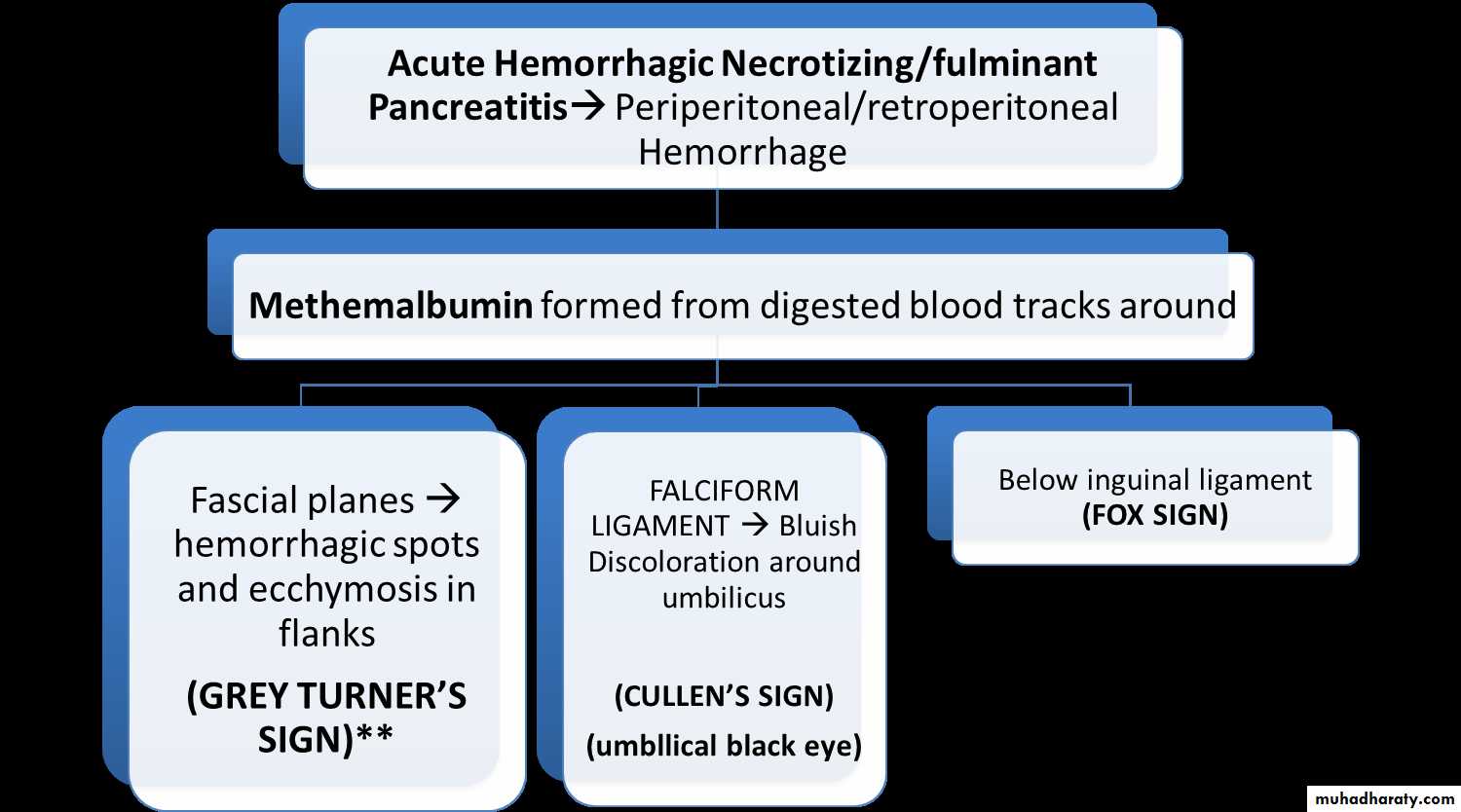
Tensing of the abdominal wall muscles to guard inflamed organs even if patient not touchedGREY TURNER/CULLEN/FOX SIGNs
Acute PancreatitisPancreatic Hemorrhage
Ruptured AAA
Blunt abdominal trauma
Ruptured ectopic pregnancy
Retroperitoneal hemorrhage
Coagulopathy
GREY TURNER SIGN
CULLEN SIGN
FOX SIGN
Diagnostic criteria
Most often established by the presence of two of the three following criteria:(i) abdominal pain consistent with the disease,
(ii) serum amylase and/or lipase greater than three times the upper limit of normal, and/or
(iii) characteristic findings from abdominal imaging.
A normal serum amylase level does not exclude acute pancreatitis, particularly if the patient has presented a few days later
Pancreatic enzymes assays
Serum Amylase:
ONSET: almost immediately
PEAK: within several hours
3-4 times upper limit of normal within 24 hrs (90%)
RETURN to normal depends on severity(3-5 days)
normal at time of admission in 20% cases
Compared with lipase, returns more quickly to values below the upper limit of normal.
Serum Lipase:
more sensitive/specific than amylaseRemains elevated longer than amylase(12 days)
Useful if late presentation
Pancreatic Enzymes’ Assays
Urine AmylaseMore sensitive than serum levels
Remain elevated for several days after serum levels returned to normal
Pancreatic-specific amylase(p-amylase)
Measuring p-amylase instead to total amylase(also includes salivary amylase) makes diagnosis more specific(88-93%)Imaging of pancreatitis
1: xray
2: abdominal ultrasound
3: endoscopic ultrasound.
4: ERCP.
5: CT scan of abdomen.
6: MRI.
d
SENTINEL LOOP SIGN
COLON CUT-OFF SIGN
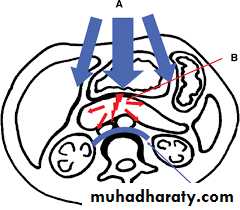
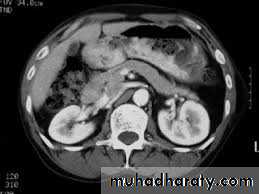
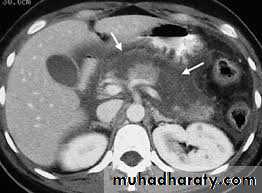
IV Contrast enhanced Computed Tomography Scan
contrast enhanced CT is indicated in the following situations:• if there is diagnostic uncertainty;
• in patients with severe acute pancreatitis, to distinguish interstitial from necrotising pancreatitis;
• in patients with organ failure, signs of sepsis or progressive clinical deterioration;
• when a localised complication is suspected, such as fluid collection, pseudocyst or a pseudoaneurysm.
SEVERITY SCORING SYSTEMS
ACUTE PANCREATITIS SPECIFIC SCORING SYSTEMSRanson score
Glagsow score
Ranson scoreOn admision
Age > 55 yrs
TLC > 16,000/mm3
BSR> 200 mg/dLAST > 250 IU/L
LDH > 350 IU/L
WITHIN 48 HOURS
BUN rise >5 mg/dLPa02 < 60 mmHg ( 8 KPa)
Serum Calcium < 8 mg/dLBase deficit > 4 meq/L
Fluid Sequestration > 6000 mLHct fall > 10 %
Glasgow-Imrie scoreON ADMISSION
Age > 55 yrs
TLC > 15 x 109 l-1
BSR>180 mg/dL (10 mmol l-1) (no H/O diabetes)
BUN > 16 mmol l-1 (no response to IV fluids)Pa02 < 60 mmHg ( 8 KPa)
WITHIN 48 HOURSSerum Calcium < 2.0 mmol l-1
Serum albumin <32 g l-1LDH > 600 units l-1
AST/ALT > 200 units l-1MANAGEMENT
Mild acute pancreatitisConservative Approach
Admit in general ward
Non invasive monitoring
(Moderate)Severe acute pancreatitis
Aggressive Approach
Admit in HDU/ICU
Invasive monitoring
__________________________________________
Recognizing patients with severe acute pancreatitis ASAP is critical for achieving optimal outcomes
Admission to HDU/ICU
AnalgesiaAggressive fluid rehydration
Oxygenation
Invasive monitoring of vital signs, central venous pressure, urine output, blood gases
Frequent monitoring of haematological and biochemical parameters (including liver and renal function, clotting, serum calcium, blood glucose)
Nasogastric drainage
Antibiotic prophylaxis can be considered (imipenem, cefuroxime)
CT scan essential if organ failure, clinical deterioration or signs of sepsis develop
ERCP within 72 hours for severe gallstone pancreatitis or signs of cholangitis Supportive therapy for organ failure if it develops (inotropes, ventilatory support, haemofiltration, etc.)
If nutritional support is required, consider enteral (nasogastric) feeding
SYSTEMIC COMPLICATIONS
CARDIOVASCULARShock- hypovolemic and septic
Arrhythmias/pericardial effusion/sudden death
ST-T nonspecific changes
Pulmonary
Respiratory failure/pneumonia/atelectasis/pleural effusion
Acute Respiratory Distress Syndrome (ARDS)
• Renal Failure
• Oliguria• Azotemia
• Renal artery/vein thrombosis
• Hematological
• Hemoconcentation
• Disseminated Intravascular Coagulopathy (DIC)
SYSTEMIC COMPLICATIONS
MetabolicHypocalcemia
Hyperglycemia
Hyperlipidemia
Gastrointestinal
Peptic Ulcer/Erosive gastritisIleus
Portal vein or splenic vein thrombosis with varices
• Neurological
• Visual disturbances-Sudden blindness(Purtscher’s retinopathy)
• Confusion,irritability,psychosis
• Fat emboli
• Alcohol withdrawal syndrome
• Encephalopathy
• Miscellaneous
• Subcutaneous fat necrosis
• Intra-abdominal saponification
• Arthralgia
LOCAL COMPLICATIONS
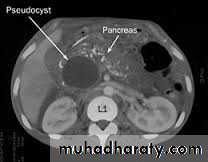
• PANCREATIC PSEUDOCYSTS
• Collection of amylase rich pancreatic fluid enclosed in a wall of fibrous or granulation tissue• Develops in
• Acute pancreatitis
• Chronic pancreatitis
• Pancreatic trauma
• Single or multiple
• Sites
• In the lesser sac in association with stomach,duodenum,jejenum,splenic hium,colon
• Types
• Communicating
• Non communicating
• Acute or chronic
• Unformed-thin cyst wall
• Formed- thickened and fibrosed cyst wall• Lined by fibrin and not by epithellium
• Contains
• - brownish fluid with necrotic material
• - infected pseudocyst and pancreatic abscess
• - high amylase content
Clinical features :
Develop after 4 weeks of acute attack of pancreatitis.Early fullness and repeated vomiting
Swelling in epigastria region
soft,smooth,not mobile,does not move on respiration,hemispherical,
infection: tender,fever and chills
Investigations
• US abdomen:size and thickness of cyst
• CT scan:size,shape,number,wall thickness,extent of necrosis,calcification,regional vessels
• MRCP and ERCP:communication with duct and ductal anomalies,chronic pancreatitis
• EUS guided apiration
• to differentiate from cystic neoplasm
• *CEA-low
• *amylase level-high
• *cytology-infected cells
Treatment
• Resolves by itself• Indications for surgery
• >6cm
• formed cyst
• infected cyst
• cyst persisting after 6 weeks
• multiple cyst
• communicating cyst/pain
• thick walled
Surgery
• Percutaneous transgastric cystgastrostomy
• Endoscopic drainage under EUS guidance
• ERCP and placement of a pancreatic stent across ampulla
• Surgical drainage into the gastric or jejunal lumen
Complications
• Infections- abscess,sepsis• Rupture –gut:GI bleeding
• -peritoneum: peritonitis
• Enlargement-pressure effects:bowel obstruction and obstructive jaundice
• -pain
• Erosion into a vessel-haemorrhage
• -hemoperitoneum
Chronic pancreatitis
Chronic pancreatitis is a chronic inflammatory disease in which there is irreversible progressive destruction of pancreatic tissue.Its clinical course is characterized by severe pain and, in the later stages, exocrine and endocrine pancreatic insufficiency
Epidmiology
incidence ranges from 2 to 10 new cases per 100 000 population per year, with a prevalence of around 13 cases per 100 000, although there are suspicions that the prevalence is actually higher.The disease occurs more frequently in men (male to female ratio of 4:1), and the mean age of onset is about 40 years.
Aetiology
1: high alcohol intake (60-70% of cases)
2: pancreatic duct obstruction( acute
pancreatitis, trauma or tumour )
3: congenital anomalies like annular pancreas and pancreatic divisum
4: idiopathic group ( cystic fibrosis, hereditary pancreatitis and infantile malnutrition )
5:auto-immune pancreatitis.
presentation
pain and The site of pain depends to some extent on the main focus of the disease.Nausea is common during attacks, and vomiting may occur.
The patient’s lifestyle is gradually destroyed by pain, analgesic dependence, weight loss and inability to work.
Loss of exocrine function leads to steatorrhoea in more than 30% of patients with chronic pancreatitis.
Loss of endocrine function and the development of diabetes are not uncommon, and the incidence increases as the disease progresses.
Tests of function – hormone stimulation
Direct Testslipase elevated only in exacerbations
Indirect Tests
Fecal elastase
Fecal chymotrypsin
Serum trypsinogen (trypsin)
Fecal fat
Blood glucose
Tests of structure
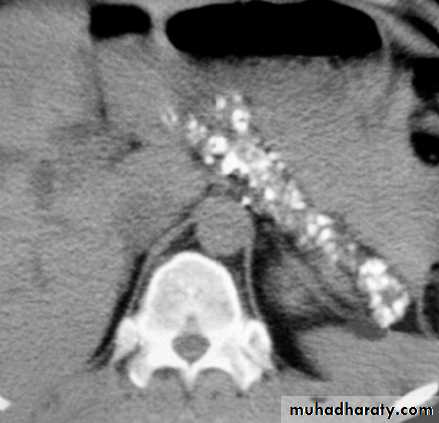
Plain film of the abdomen
CT
Ultrasonography
MRI, particularly MRCP
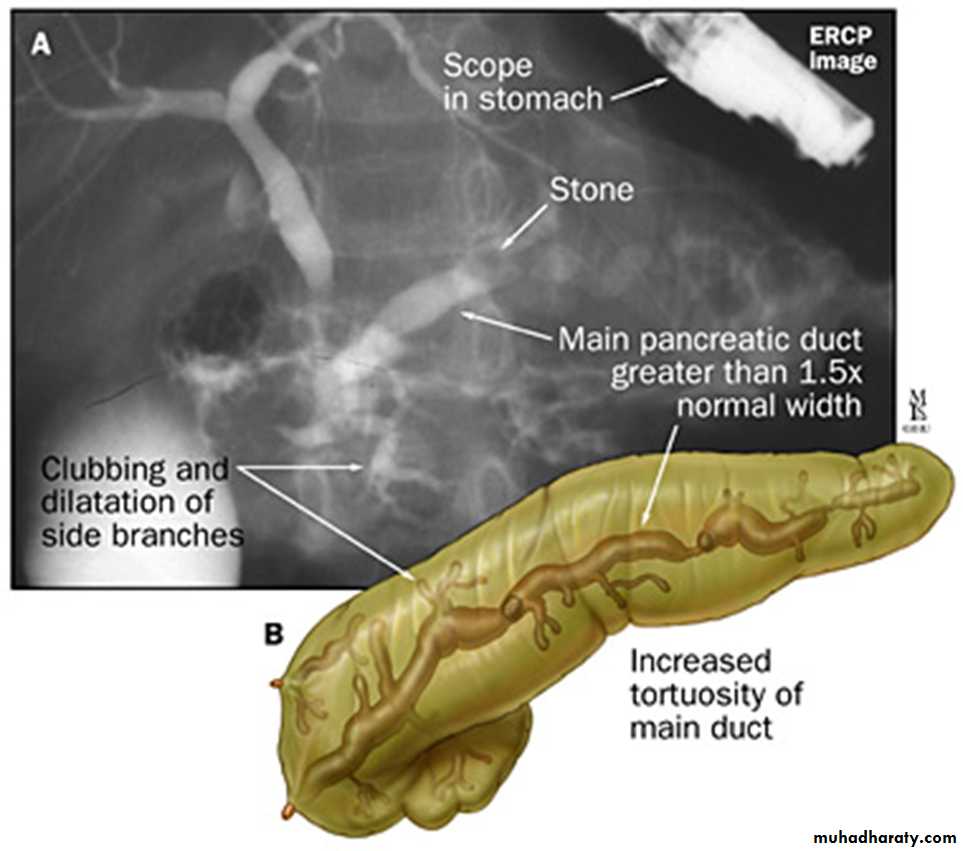
ERCP
Pancreatic calcifications
CT scan in chronic pancreatitis
ERCP finding in chronic pancreatitis
Surgical treatment
• Surgical pain control and drainage procedures.• Resection (local - - - - 95%) –causes pancreatic insufficiency
• Splanchinectomy, celiac ganglionectomy, nerve block
• Endoscopic treatment
• Sphinctorotomy, dilatation of strictures, caliculi removal, duct stenting
• Complications– acute pancreatitis, abscess, ductal damage, death
Medical treatment of chronic pancreatitis
Treat the addiction
■ Help the patient to stop alcohol consumption and tobacco smoking
■ Involve a dependency counsell
or or a psychologist
Alleviate abdominal pain
■ Eliminate obstructive factors (duodenum, bile duct, pancreatic duct)
■ Escalate analgesia in a stepwise fashion
■ Refer to a pain management specialist
■ For intractable pain, consider CT/EUS-guided coeliac axis block
• Nutritional and digestive measures
• ■ Diet: low in fat and high in protein and carbohydrates• ■ Pancreatic enzyme supplementation with meals
• ■ Correct malabsorption of the fat-soluble vitamins (A, D, E, K) and vitamin B12
• ■ Medium-chain triglycerides in patients with severe fat malabsorption (they are directly absorbed by the small intestine without the need for digestion)
• ■ Reducing gastric secretions may help
• Treat diabetes mellitus
CARCINOMA OF THE PANCREAS
Pancreatic cancer is the sixth leading cause of cancer death in the UK, and the incidence is 10
cases per 100 000 population per year. Worldwide, it constitutes 2–3% of all cancers and, in the USA, is the fourth highest cause of cancer death.
The incidence has declined slightly over the last 25 years.
Pathology
More than 85% of pancreatic cancers are ductal adenocarcinomas.Ductal adenocarcinomas arise most commonly in the head of the gland. They are solid,
scirrhous tumours.
Ductal adenocarcinomas infiltrate locally, typically along nerve sheaths, along lymphatics and into blood vessels. Liver and peritoneal metastases are common.
Cystic tumours of the pancreas may be serous or mucinous ,
Pathology
Ampullary adenocarcinomas often present early with biliaryObstruction.
Their natural history is distinctly more favourable compared with pancreatic ductal adenocarcinoma. Ampullary carcinomas are relatively small when diagnosed, which may account for their better prognosis.
Occasionally, other malignant neoplasms can arise at the ampulla, such as carcinoid tumours and high-grade neuroendocrine carcinomas.
Risk factors for the development of pancreatic cancer
Demographic factorsAge (peak incidence 65–75 years)
Male gender
Black ethnicity
Environment/lifestyle Cigarette smoking
Risk factors for the development of pancreatic cancer
Genetic factors and medical conditions
Family history Two first-degree relatives with pancreas cancer:
relative risk increases 18- to 57-fold Germline
BRCA2 mutations in some rare high-risk families
Hereditary pancreatitis (50- to 70-fold increased risk)
Chronic pancreatitis (5- to 15-fold increased risk)
HNPCC
Ataxia telangiectasia
Peutz–Jeghers syndrome
Familial breast–ovarian cancer syndrome
Familial atypical multiple mole melanoma
Familial adenomatous polyposis – risk of ampullary/duodenal carcinoma
Diabetes mellitus
Clinical features
1: JAUNDICE due to obstruction of the biliary duct(obstructive jaundice).2: epigastric pain with nausea and vomiting
3: weight loss.
4: back pain.
5: recently diagnosed DM with upper GIT symptoms.
6: distally located tumour present with inresectable tumour.
.
On examination,
there may be evidence of jaundice, weight loss, a palpable liver and a palpable gall bladder. Courvoisier low.
Other signs of intra-abdominal malignancy should be looked for with care, such as a palpable mass, ascites, supraclavicular nodes and tumour deposits in the pelvis; when present, they indicate a grim prognosis
Investigation
1: usual blood test and liver function test.2: abdominal ultrasound.
3: CT scan of abdomen.
4: MRI and MRCP.
5: ERCP.
6: endoscopic ultrasound.
7: PET scan.
8: laparoscopy.
treatment
At the time of presentation, more than 85% of patients with ductal adenocarcinoma are unsuitable for resection because thedisease is too advanced.
The standard resection for a tumour of the pancreatic head or the ampulla is a pylorus-preserving pancreatoduodenectomy (PPPD). This involves removal of the duodenum and the pancreatic head, including the distal part of the bile duct.
The original pancreatoduodenectomy as proposed by Whipple included resection of the gastric antrum
Palliation of pancreatic cancer
Relieve jaundice and treat biliary sepsis■ Surgical biliary bypass
■ Stent placed at ERCP or percutaneous transhepatic cholangiography
Improve gastric emptying
■ Surgical gastroenterostomy
■ Duodenal stent
Pain relief
■ Stepwise escalation of analgesia
■ Coeliac plexus block
■ Transthoracic splanchnicectomy
Symptom relief and quality of life
■ Encourage normal activities
■ Enzyme replacement for steatorrhoea
■ Treat diabetes
Consider chemotherapy