Mycoplasma pneumoniae
ByDr. Athal Humo
2016-2017
Lec 5
EPIDEMIOLOGYMycoplasma pneumoniae causing respiratory infections in school-age children and young adults.
The incubation period is 2-3 wk
Immunity after infection is not long lasting.
Asymptomatic carriage after infection can last up to 4 mo despite antibiotic therapy and may contribute to prolonged outbreaks.
CLINICAL MANIFESTATIONS
Tracheobronchitis and pneumonia are the most commonly recognized clinical syndromes associated with M. pneumoniae infection.Although the onset of illness may be abrupt, it is usually characterized by gradual onset of headache, malaise, fever, and sore throat, followed by progression of lower respiratory symptoms, including hoarseness and nonproductive cough.
Coryza or gastrointestinal complaints are unusual with M. pneumoniae pneumonia and usually suggest a viral etiology.
Although the clinical course in untreated patients is variable, cough, the clinical hallmark of M. pneumoniae infection, usually worsens during the 1st wk of illness, and symptoms generally resolve within 2 wk. Cough can last up to 4 wk and may be accompanied by wheezing. Patients generally recover without complications.
Chest exam is often unrevealing, even in patients with severe cough. There may be no auscultative or percussive findings or only minimum dry rales.
Clinical findings are often less severe than suggested by the patient chest radiograph, that is why term “walking pneumonia”
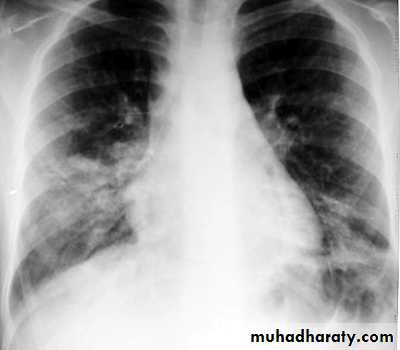
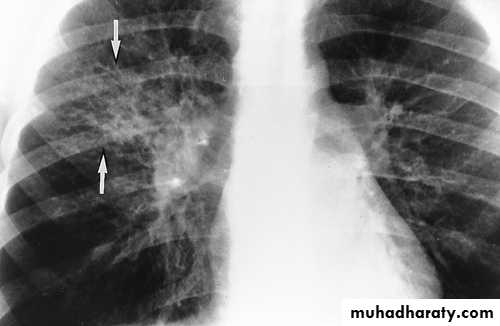
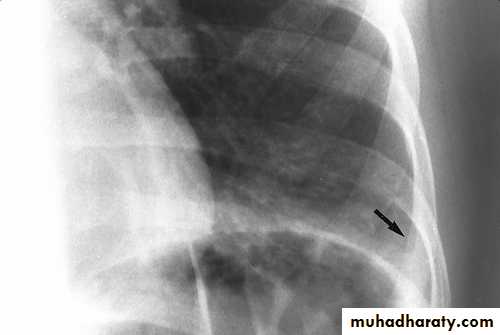
CXR: interstitial or bronchopneumonic, involve mainly the lower lobes. Bilateral diffuse infiltrates, lobar pneumonia or hilar lymphadenopathy can occur in up to 30% . Pleural effusions may occur.
The WBC and differential counts are usually normal.
ESR is often elevated.Lower lobe pn
Hilar involvement
Pleural effusionOther respiratory illnesses caused occasionally by M. pneumoniae include:
PharyngitisSinusitis
Otitis media
Croup
Bronchiolitis
M. pneumoniae is a common trigger of wheezing in asthmatic children
Extrapulmonary Disease:
CNS disease, as encephalitis, transverse myelitis, aseptic meningitis, Guillain-Barré syndrome.Dermatologic disease, which includes a variety of exanthemas, most notably maculopapular rash urticaria, erythema multiforme or Stevens-Johnson syndrome (SJS), & erythema nodosum.
Hematologic abnormalities, hemolytic anaemia, thrombocytopenia, aplastic anemia, and coagulation defects occur occasionally.
Arthritis
Other conditions: such as hepatitis, pancreatitis, AGN, and cardiac complicationStevens-Johnson-like syndrome
associated with Mycoplasma pneumoniae infectionDIAGNOSIS
PCR of a nasopharyngeal or throat swab for M. pneumoniae DNA carries a sensitivity and a specificity of 80% to >97%.Serologic tests (immunofluorescence tests or enzyme-linked immune assays) to detect serum Ig M and IgG antibodies.
Cold hemagglutinins, but not specific.
Cultures on special media (SP4 agar media)
TREATMENT
M. pneumoniae illness is usually mild, and most cases of pneumonia can be managed without the need for hospitalization.Because mycoplasmas lack a cell wall, they inherently are resistant to β-lactam agents that act by inhibiting the cell wall synthesis.
M. pneumoniae is typically sensitive to macrolides (erythromycin, clarithromycin, azithromycin).
Macrolide-resistant strains
> 8 yr, can use doxycycline.
< 8 yr, quinolone tosufloxacin are approved in Japan for pediatric use to treat macrolide-resistant M. pneumoniae infections.