When Simple and Natural
Gets Complicated
Failure to Thrive

Definition
• Failure to Thrive (FTT):
• Sign that describe a particular problem rather
than diagnosis which is failure to gain weight
in childhood.
– Weight below the 5
th
percentile for age and sex
– Weight for age curve falls across two major
percentile lines
– weight gain is less than expected
• Other definitions exist, but are not superior in
predicting problems or long term outcomes

Foster
placement
7/1/11

Introduction
•
Specific infant populations:
–
Premature/IUGR – wt may be less than 5
th
percentile, but if following the growth curve
and normal interval growth then FTT should
not be diagnosed
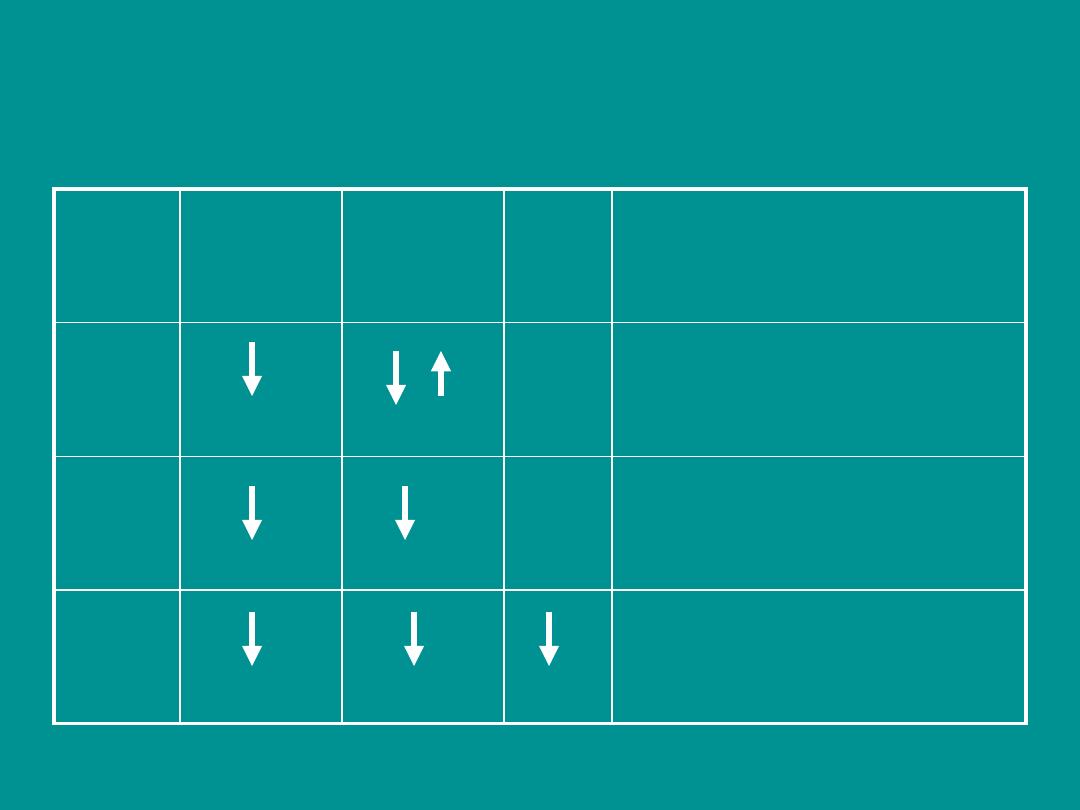
Major Anthropologic Categories of FTT.
WEIGHT
HEIGHT
HC
TYPE I
NOR
Malnutrition of organic or non-
organic etiology
TYPE II
NOR
Endocrine, bony dystrophy,
Constitutional short stature
TYPE III
Chromosomal, metabolic,
severe malnutrition
HC: Head Circumference
NORM: Normal
ETIOLOGY
• 2 BIG categorize but large differential pool.
ORGANIC
INORGANIC
MIXED
Causes of Failure to Thrive
Inadequate
Input
Excessive
Output
Increased
Utilization
CLASSIFICATION
More useful classification system is
Malnutrition
&
FTT
Inadequate
Caloric Intake
Malabsorption
Excessive
Caloric
Expenditure

FAILURE TO THRIVE
Psychosocial
Nutritional
Kwashiorkor
Marasmus
Zinc/iron deficiency
Feeding disorders
Oral-motor apraxia
Cleft palate
Dentitions
GI
Vomiting
Gastroesophageal reflux
Structural anomalies
Central nervous system lesion
Diarrhea
Chronic toddler diarrhea
Infectious
Malabsorption
Celiac disease
Inflammatory bowel disease
Hepatic
Chronic hepatitis
Glycogen storage diease
Infectious
Tuberculosis
Human immunodeficiency virus
Cardiac
Pulmonary
Tonsillar hypertrophy
Cystic Fibrosis
Renal
Chronic pyelonephritis
Fanconi syndrome (and variants)
Chronic renal insufficiency
Endocrine
Hypothyroidism
Rickets
Viitamin D deficiency
Vitamin D resistance
Central nervous system lesion
Hypophosphatemic
Growth hormone deficiency/resistance
Growth hormone deficiency/resistance
Hypercortisolism
Pseudohypoparathyroidism
Type I diabetes mellitus (poorly controlled,
Mauriac syndrome)
Central nervous system
Pituitary insufficiency
Diencephalic syndrome
Other chronic diseases
Oncologic

Calories, Calories,……
• Root of growth failure stems from
• inadequate calories
• – Inadequate intake
• – Increased demands
• – Poor absorption
• Infants require approximately
110-120 kcal/kg/day
At age 1 year, 100 kcal/kg/day

CALORIC INTAKE
• Inadequate Caloric Intake
– Incorrect preparation of formula
– Poor feeding habits (ex: too much
juice)
– Poverty
– Mechanical feeding difficulties
(reflux, cleft palate, oro-motor
dysfunction)
– Neglect
Consider child abuse and
neglect in cases of
FTT that don t respond to appropriate
interventions

Inadequate absorption
– Celiac disease
– Cystic fibrosis
– Milk allergy
– Vitamin deficiency
– Biliary Atresia
– Necrotizing enterocolitis

Increased metabolism
– Hyperthyroidism
– Chronic infection
– Congenital heart disease
– Chronic lung disease
• Other considerations
– Genetic abnormalities, congenital infections,
metabolic disorders (storage diseases, amino
acid disorders)

COMPREHENSIVE NUTRITIONAL
ASSESMENT
• Dietary history
• Medical and medication history
• Physical examination
• Growth and anthropremetric measurements
• Laboratory tests.
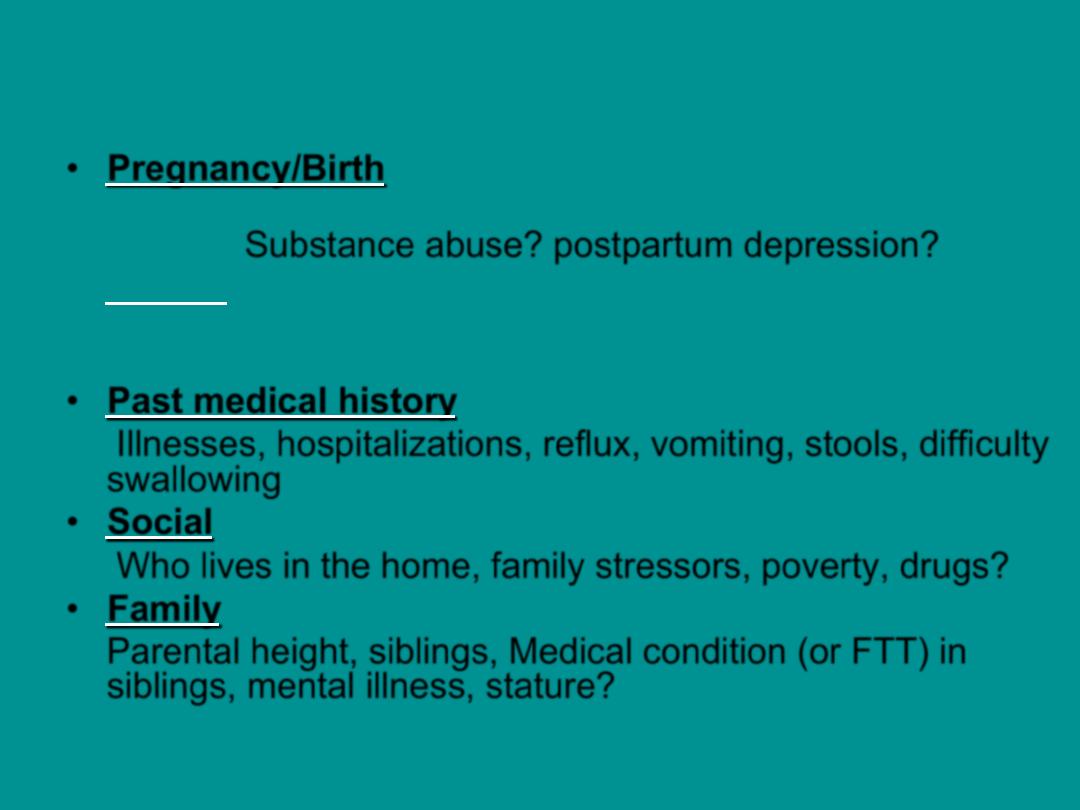
HISTORY
• Pregnancy/Birth
LBW, IUGR, prematurity, postnatal complications, tube
feeding. Substance abuse? postpartum depression?
• Dietary type of food, time spent over meal, number of
meals, self feed, formula/supplements, unusual feeding
behavior, who feeds?
• Past medical history
Illnesses, hospitalizations, reflux, vomiting, stools, difficulty
swallowing
• Social
Who lives in the home, family stressors, poverty, drugs?
• Family
Parental height, siblings, Medical condition (or FTT) in
siblings, mental illness, stature?

DIETARY HISTORY
• Assess methods of feeding
• breastfeeding patterns (including maternal diet use
of medications that can affect milk production and
let-down such as alcohol or diuretics)
• formula preparation
• volume consumed
• feeding techniques.
• Caloric counts- food diary
• A detailed history of formula preparation :may
reveal a dilute formula that contains insufficient
calories and excess water.

Dietary Associations With Poor
Growth in Young Children
– Breastfeeding difficulties
– Improper formula mixing
– Poor transition to food (6 to 12 months of
age)
– Excessive juice consumption
– Avoidance of high-calorie foods

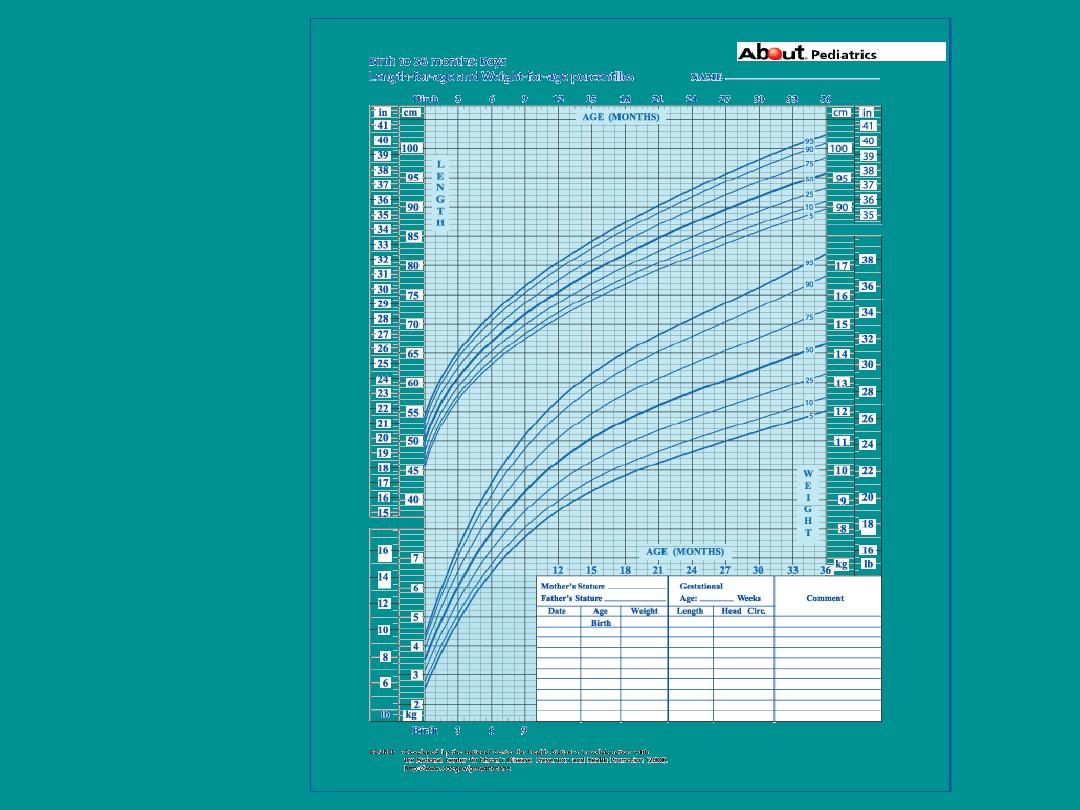
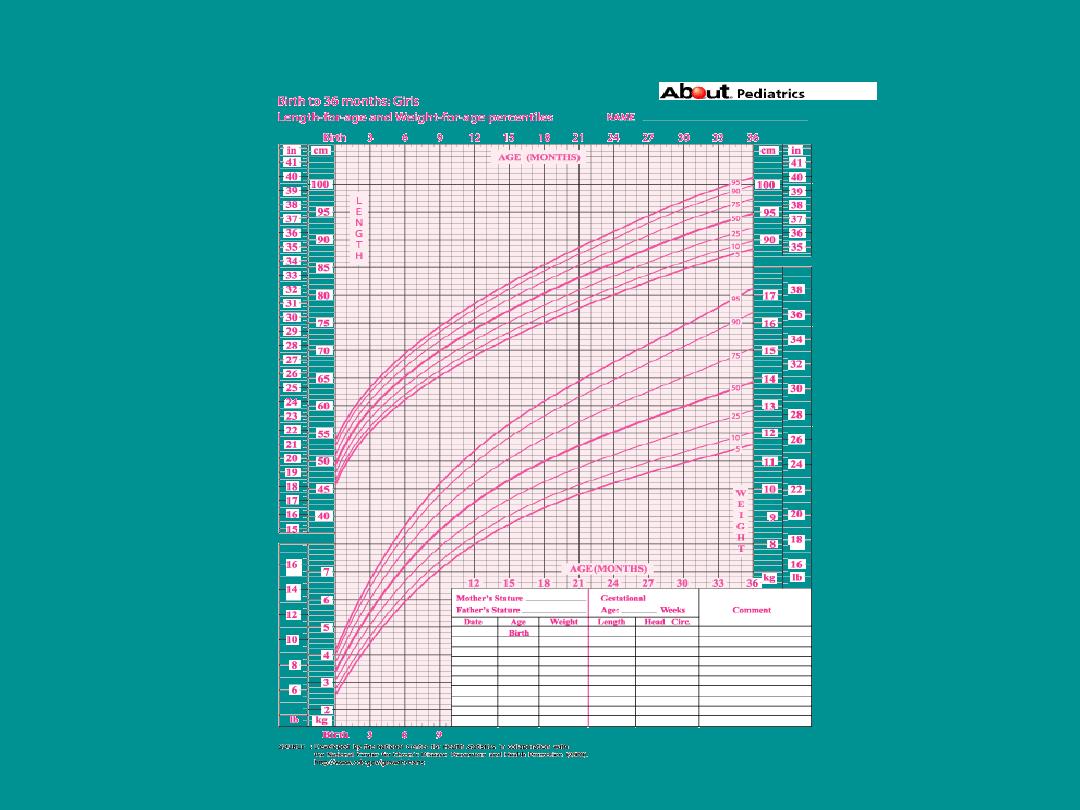
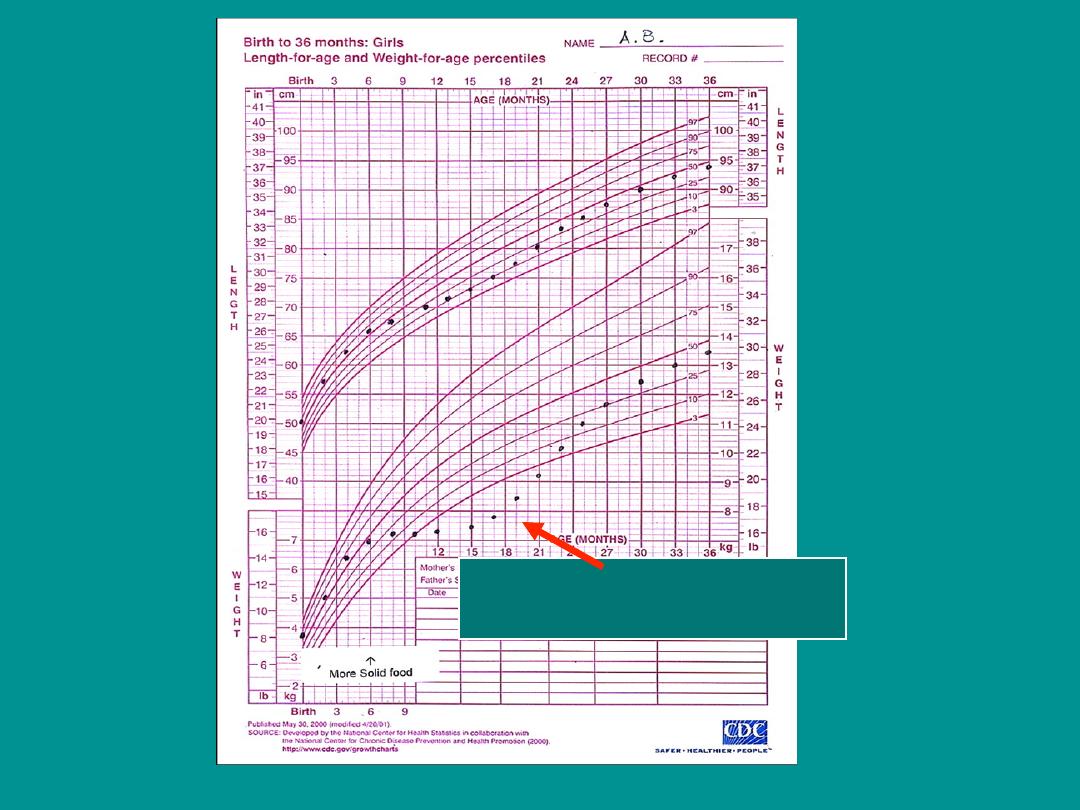
EVALUATION
• Accurately plotting growth charts at every
visit.
• Use correct growth charts!
• Evaluate the trends
• History and Physical more important than
labs

Examination: Key Points
• Infant eye contact (if avoids may be abuse)
• Poor suck or motor skills
• Watch caretaker feed the infant!!!
• Plot height, weight and head circumference
• Dysmorphic features
• Lung or heart exam
• Skin: scars, jaundice, eczema, bruises or rash
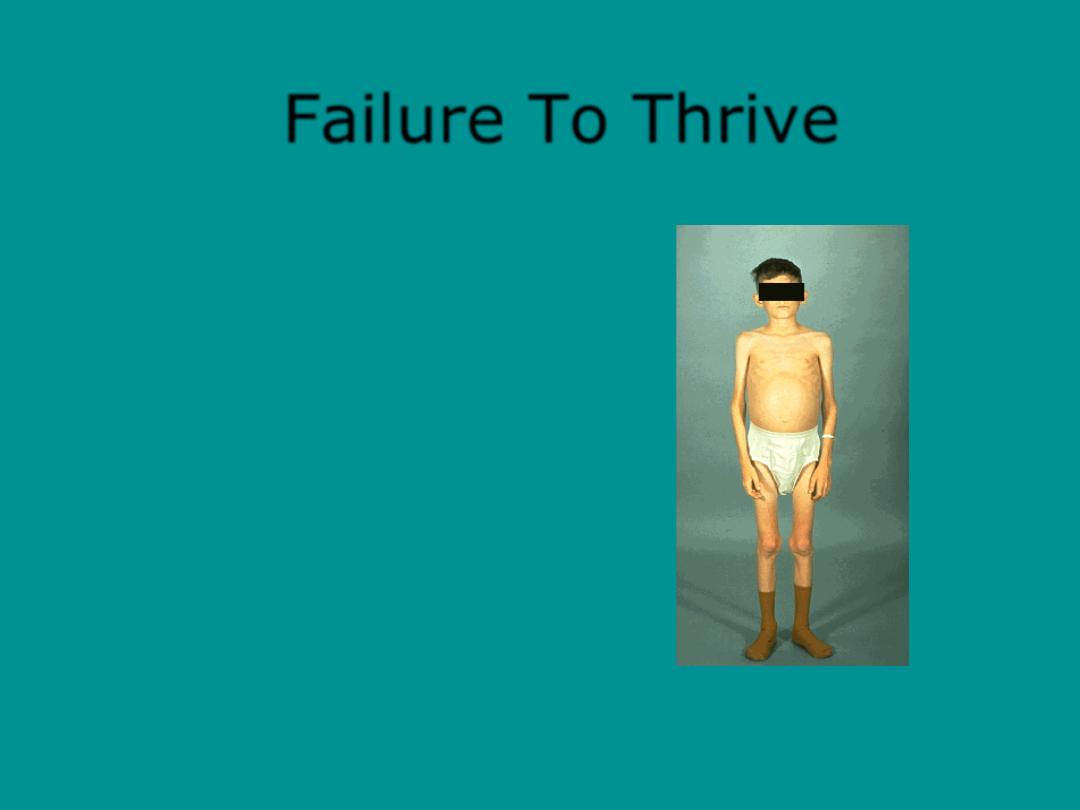
Failure To Thrive
This child has
Celiac Syndrome.
It is an intestinal
mal-absorption
syndrome.
7/1/11
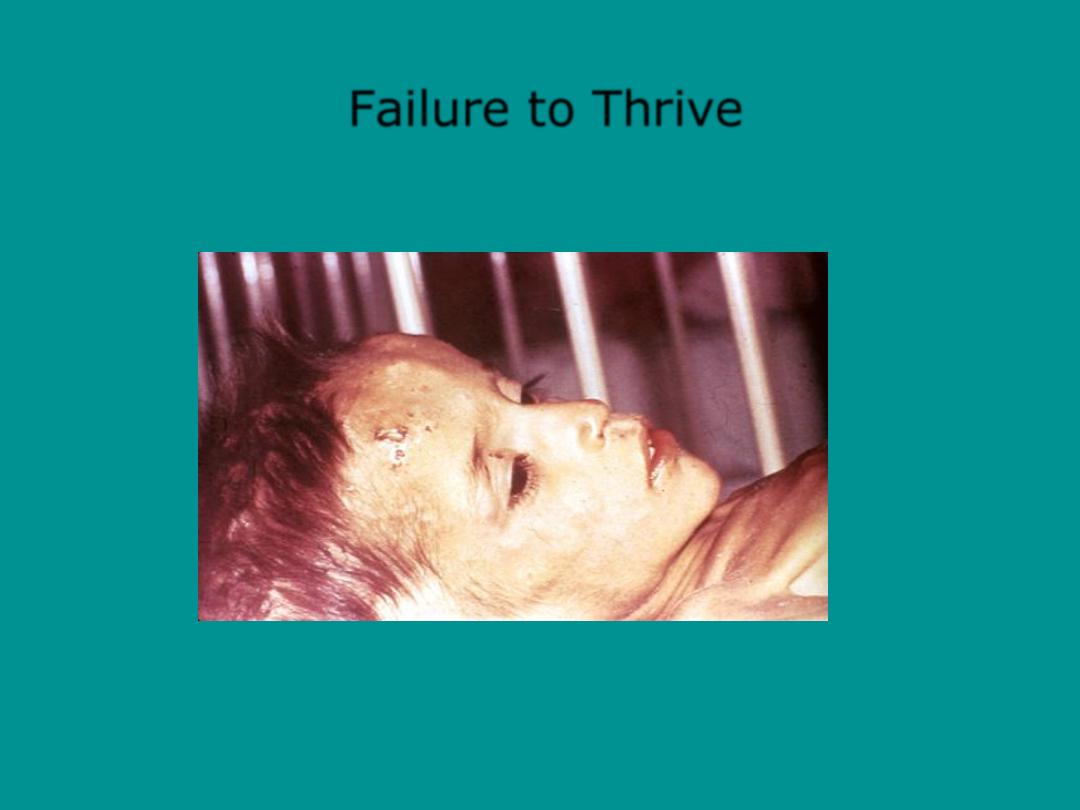
Failure to Thrive
7/1/11
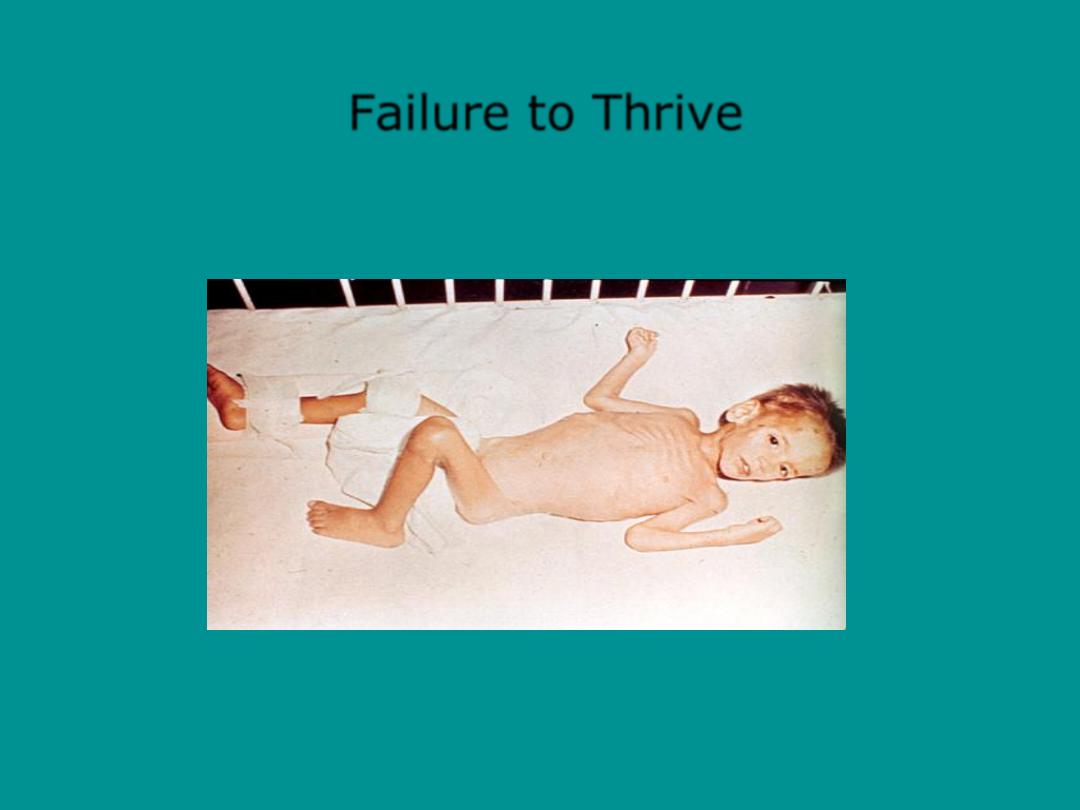
Failure to Thrive
7/1/11
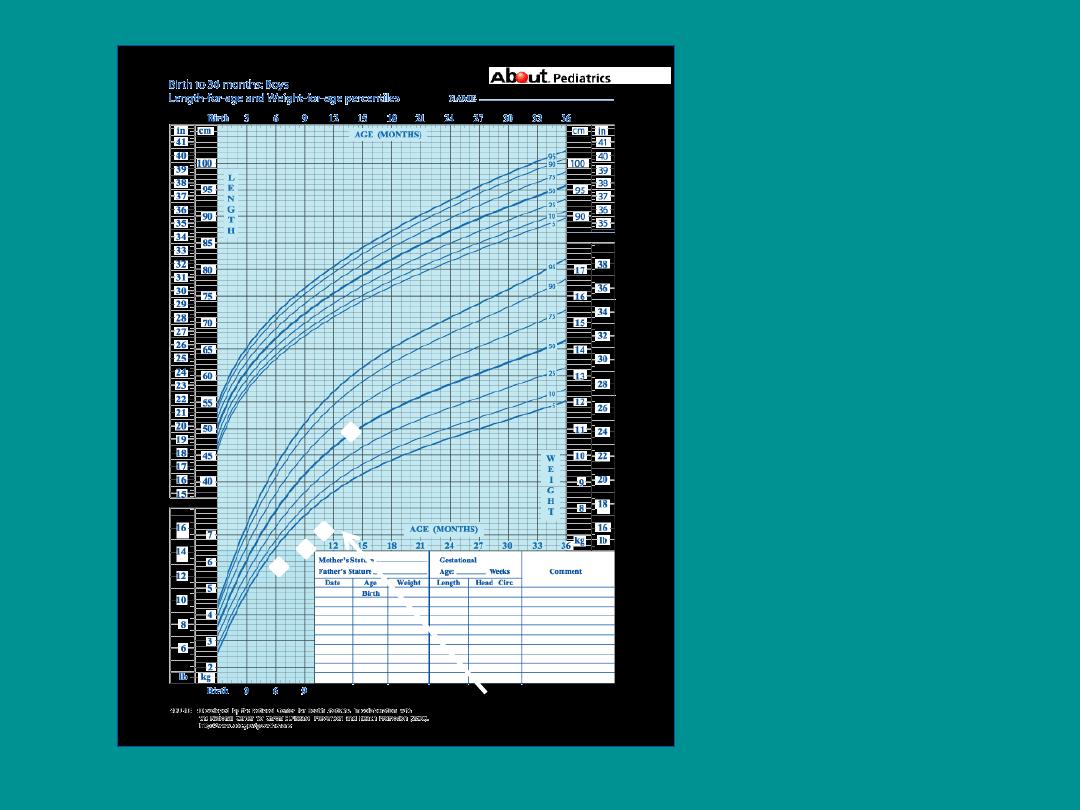
Foster
placement
7/1/11
Failure To Thrive
7/1/11

INVESTIGATIONS
• Lab tests should be guided by H&P.
• Less than 2% of the lab studies performed
in evaluating children with FTT were
useful.
Sills RH AM J Dis Child 1978

INVESTIGATIONS
HISTORY AND
PHYSICAL
FIRST LINE
CBC
ESR, CRP
UA/Cx,
Cr, glucose,
Ca
Thyroid
functions
Sweat Chloride
Celiac serology
(age)
SECOND LINE
Serum AA
Lead level
Ur organic acids
LFTs
PPD
Abd US
CXR
Head US
EKG/Eho
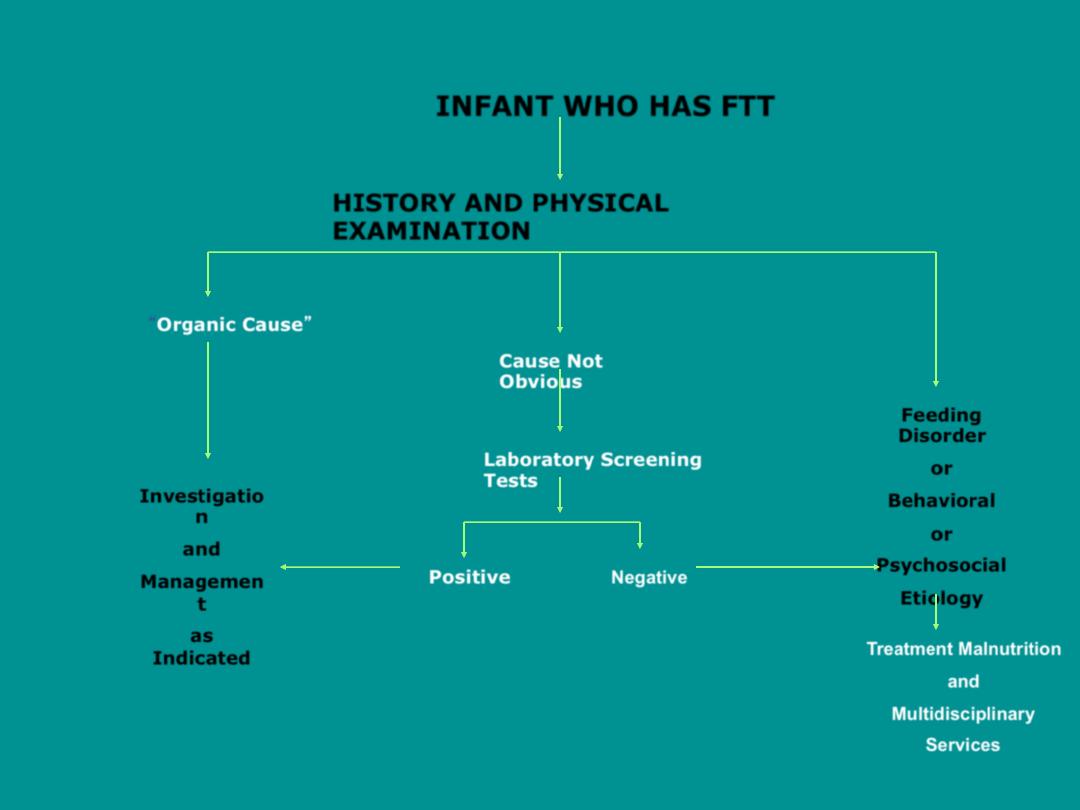
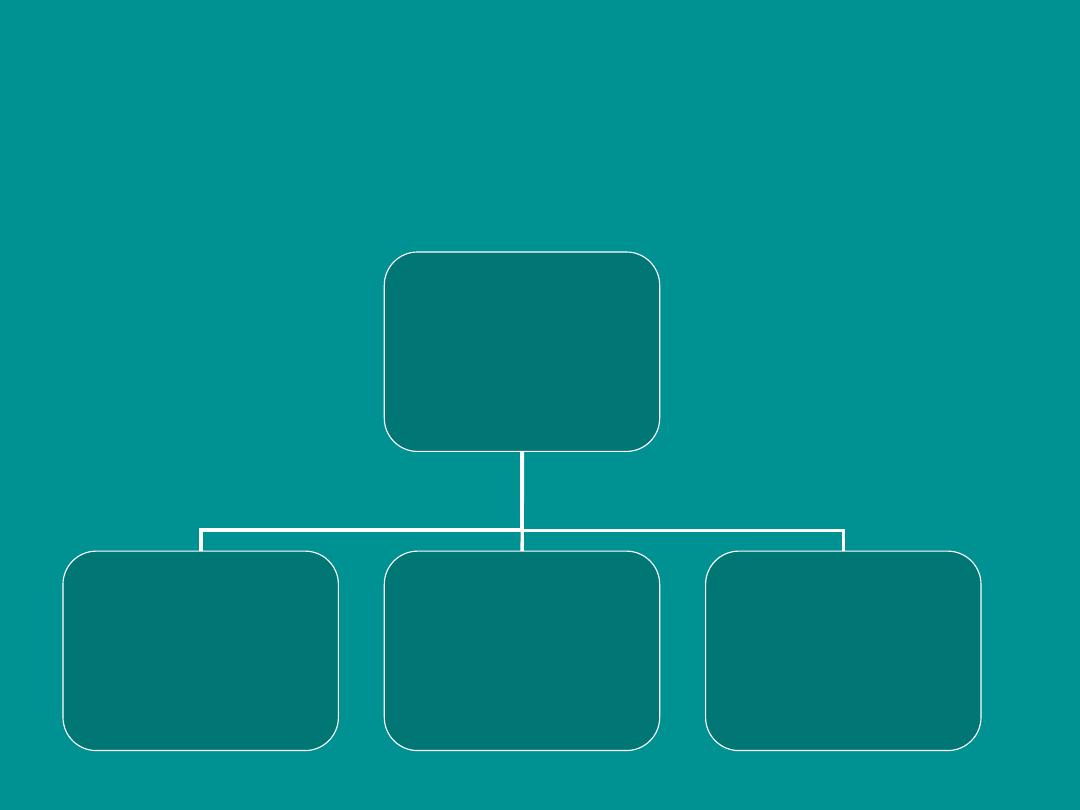
HISTORY AND PHYSICAL
EXAMINATION
Organic Cause
Cause Not
Obvious
Feeding
Disorder
or
Behavioral
or
Psychosocial
Etiology
Investigatio
n
and
Managemen
t
as
Indicated
Laboratory Screening
Tests
Positive
Negative
Treatment Malnutrition
and
Multidisciplinary
Services
INFANT WHO HAS FTT

MANAGEMENT
• Goal is catch-up weight gain
• Most cases can be managed with nutrition
intervention and/or feeding behavior modification
• General principles:
– High Calorie Diet
– Close Follow-up
• Keep a prospective feeding diary-72 hour

CALORIC REQUIREMENT
• Stabilization phase (1-7 days):
1-Rehydaration
2-treatment of infection
3- F75
• Rehabilitation phase(2-6 weeks)
1- Treatment of infection
2-F100
• Ready to use therapeutic foods.

INTAKE
• Energy intake should be 50% greater than
the basal caloric requirement
• Concentrate formula, add rice cereal to pureed
foods
• Add taste pleasing fats to diet (cheese, peanut
butter, ice cream)
• High calorie milk drinks (e.g Pediasure has 30 cal/
oz vs 19 cal per oz in whole milk)
• Multivitamin with iron and zinc
• Limit fruit juice to 8-12 oz per day
Vitamin and Mineral Supplementation
• ZINC
– No reliable lab assessment
– Baseline addition
• IRON
– If Hemoglobin, Hematocrit or MCV labs indicate
further work up add to diet ( After phases Interfere with
host defense mechanism)
Medical Appetite Stimulation
Cyprohepatidine has no proven
long-term benefit
Lemons PK, Dodge NN. Persistent failure-to-thrive: a case study. J Pediatr
Health Care 1998; 12: 27.
Refeeding Syndrome
• Sweatiness
• Hyperthermia
• Hepatomegaly – increased glycogen
deposition
• Widening of the cranial sutures- brain
growth faster than the skull
• Increased periods of sleep
• Fidgetiness or hyperactivity
Refeeding Syndrome
• Follow Potassium and Phosphorus
in the acute period of
reinstating nutrition
• Initial intracellular ion shifts my
cause
–
Hypokalemia
–
Hypophosphotemia
• Can produce serious arrhythmias
and muscle weakness

WHEN TO HOSPITILIZE
• Do you hospitalize?
– Rarely necessary
– Consider if:
• the child has failed output management
• FTT is severe
– Medical emergency if wt <60-70% of ideal wt
– Hypothermia, bradycardia, hypotension
• safety is a concern

HOSPITILIZATION
• For difficult cases:
– Multidisciplinary team approach produces
better outcomes
• Dietitians
• Social workers
• Occupational therapists
• Psychologists
– NG tube supplementation may be necessary
DIAGNOSED WITH CELIAC DISEASE
AND GLUTEN FREE DIET STARTED

THANK YOU
