1
Bacteriology:
Lec. Helicobacter pylori
Helicobacterpylori pylori, is a
usually in the
. It was identified in 1982 by Australian scientists
, who found that it was present in a person with
, conditions not previously believed to have
cause. It is also linked to the development of
. However, over 80% of individuals infected with the bacterium
are
, and it may play an important role in the natural stomach ecology.
More than 50% of the world's population harbor H. pylori in their
upper
. H. pylori's helical shape (from which the
derived) is thought to have evolved to penetrate the
Scientific Classification:
The bacterium was initially named Campylobacter pyloridis, then renamed C.
pylori (pylori being the
, the circular opening leading from the
stomach into the
, from the Ancient Greek word πυλωρός, which
.. When
showed in 1989 that the bacterium did not belong to the genus
, it
"coil". According to Marshall et al. 1985 and Goodwin et al., 1989; H. Pylori
classiufied as:
Domian:
Bacteria
Phylum
Class:
Epsilonproteobacteria
order
Family:
Genus:
Species:
H. Pylori, Binomial name: Helicobacter pylori,
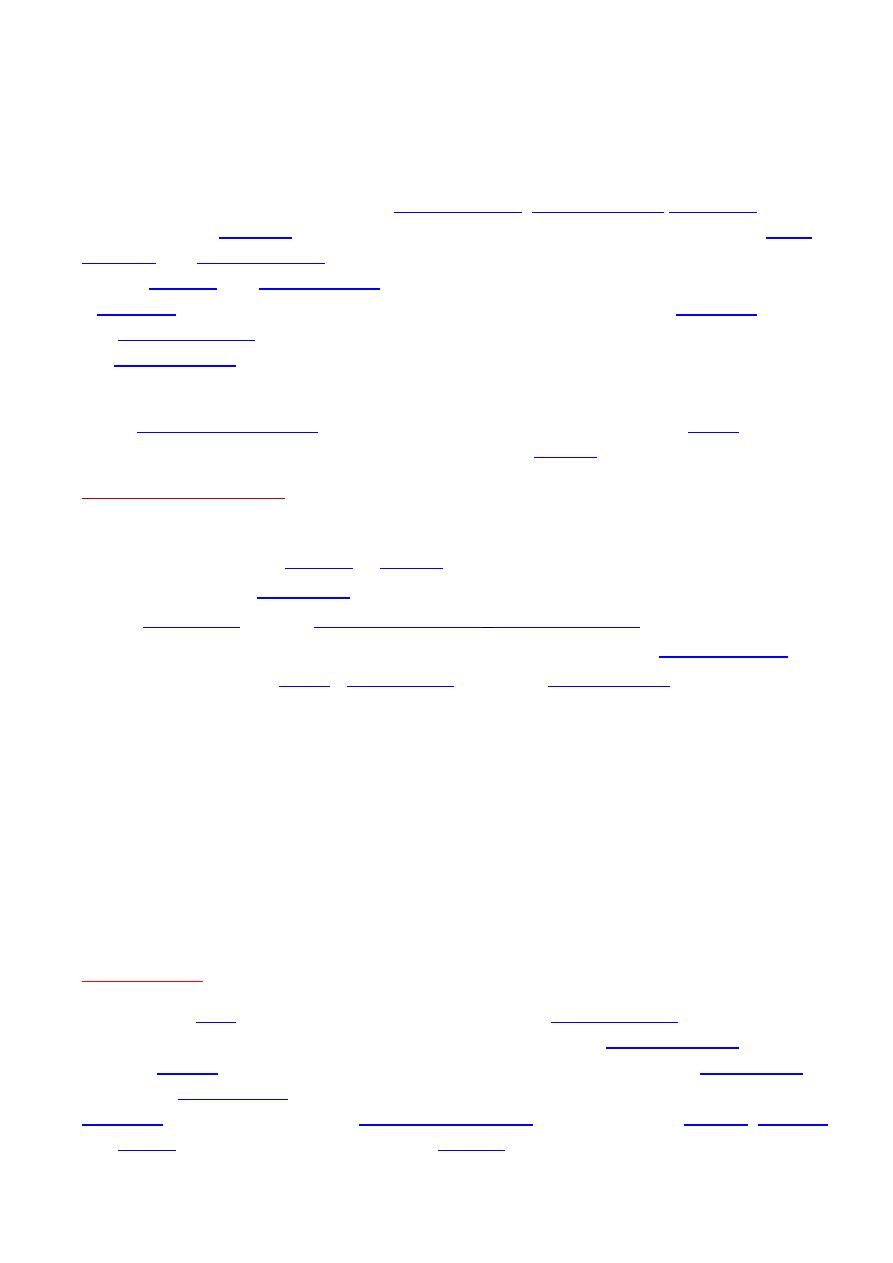
Microbiology:
-shaped (classified as a curved rod)
3 μm long with a diameter of about 0.5 μm (figure.1). It is
; that is, it
, but at lower concentration than is found in the
. It
which can be used to obtain energy by oxidizing molecular
2
) produced
It
. It is capable of forming
2
form, both likely to favor its survival and be
H. pylori possesses five major
-The largest family includes known and putative
- Iron transporters,
-associated proteins,
- Proteins of unknown function.
Like other typical Gram-negative bacteria, the outer membrane of H. pylori consists
of
epithelium. The outer membrane also contains
in few other bacteria. H. pylori has four to six
; all gastric and enterohepatic
Helicobacter species are highly motile owing to flagella.
Genes involved in virulence and pathogenesis:
Study of the H. pylori genome is centered on attempts to understand
, the
to cause disease. About 29% of the loci have a colonization
defect when mutated.
Two of sequenced strains have an around 40-
-long Cag
believed responsible for pathogenesis) that contains over 40
genes. This pathogenicity island is usually absent from H. pylori strains isolated from
humans who are carriers of H. pylori but remain
Figure.1: Helicobacter pylori (Marshall et
al. 1985) Goodwin et al., 1989
3
gene codes for one of the major H. pylori
with the cagA gene are associated with an ability to cause
. The pathogenicity
of H. pylori may be increased by genes of the cag
; about 50–70%
of H. pylori strains in Western countries carry it.
Western people infected with strains
carrying the cag PAI have a stronger inflammatory response in the stomach and are at a
greater risk of developing peptic ulcers or stomach cancer than those infected with
strains lacking the island.
H. pylori consists of a large diversity of strains, and the
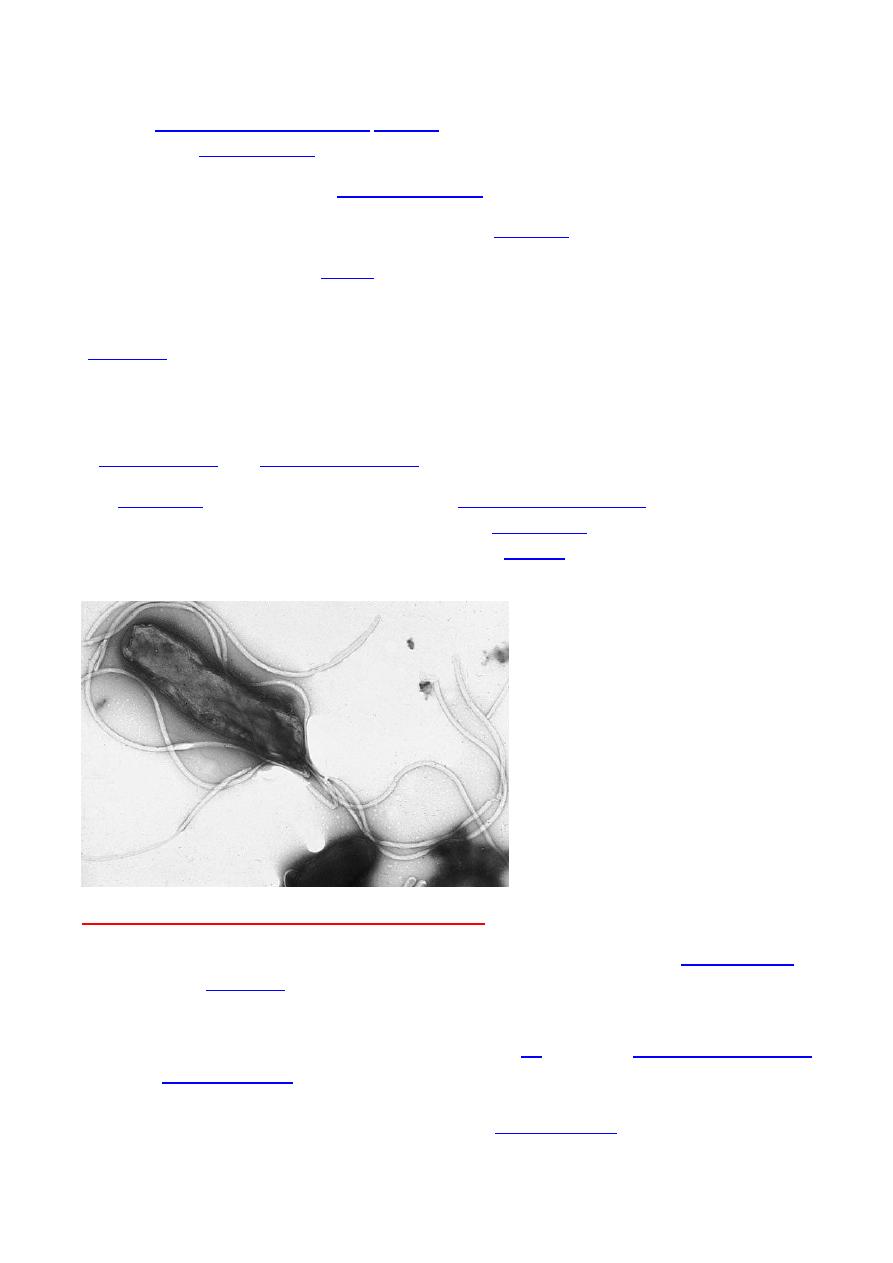
Microscopy:
H. pylori can be demonstrated in tissue by Gram stain, Giemsa stain, haematoxylin-
eosin stain, Warthin-Starry silver stain (Figure.2), acridine-orange stain, and phase-
contrast microscopy.
Signs and Symptoms:
Up to 85% of people infected with H. pylori never experience symptoms or
complications.
infection may appear as an acute
. Where this develops into chronic gastritis, the symptoms, if present, are
: stomach pains, nausea,
, and
Individuals infected with H. pylori have a 10 to 20% lifetime risk of developing
and a 1 to 2% risk of acquiring
(body of the stomach) is more likely to lead to
Figure.2: H. pylori colonized on the
surface of regenerative epithelium
(image from (
4
However,H. pylori possibly plays a role only in the first stage that leads to common
chronic inflammation, but not in further stages leading to
A meta-
analysis conducted in 2009 concluded the eradication of H. pylori reduces gastric cancer
risk in previously infected individuals, suggesting the continued presence of H.
pylori constitutes a
factor of 65% for gastric cancers.
H. pylori has been associated with colorectal polyps and
It may also
be associated with eye disease.
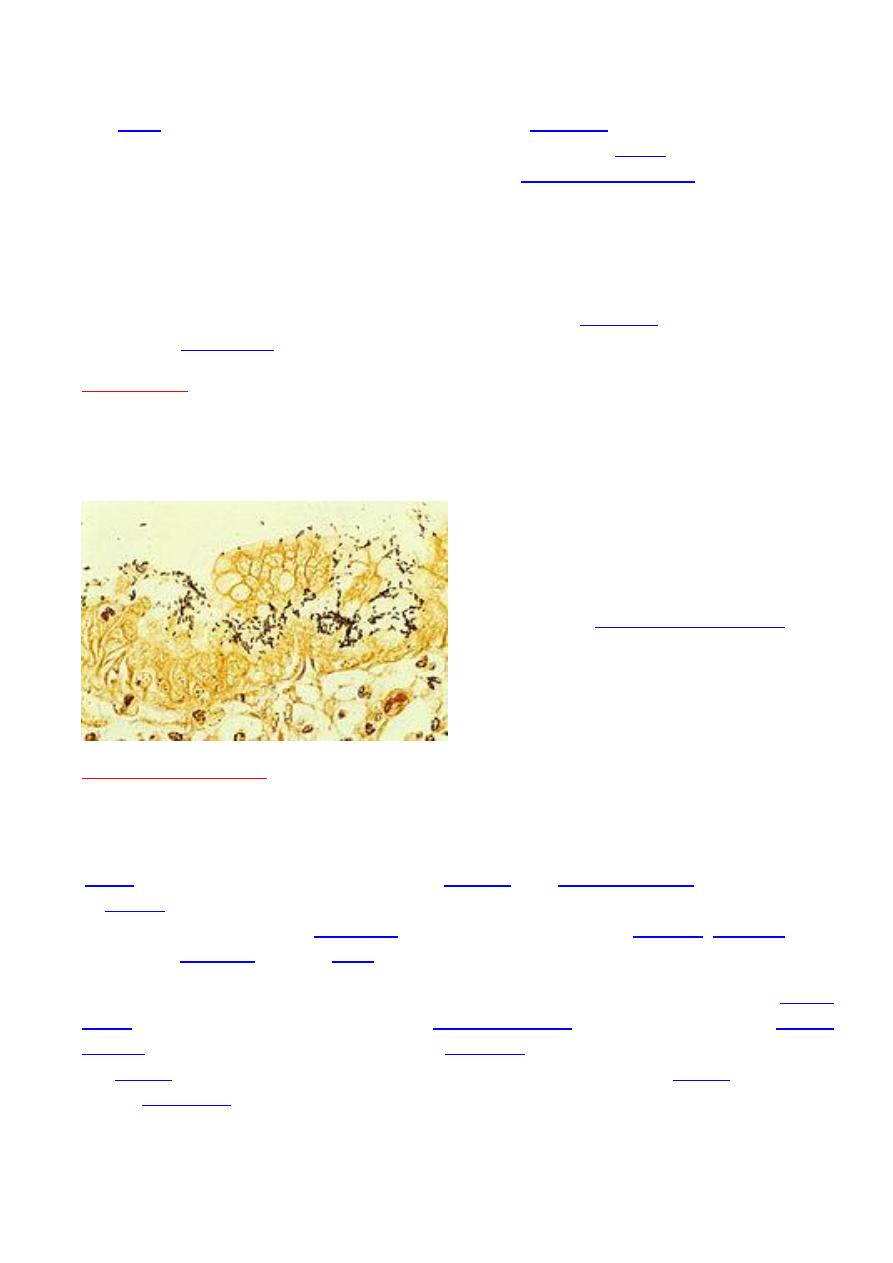
Adaptation to the stomach’s acidic environment:
To avoid the acidic environment of the interior of the stomach (
), H. pylori uses its
flagella to burrow into the mucus lining of the stomach to reach the
underneath, where the pH is more neutral (see Diagram. 1).
H. pylori is able to sense the pH gradient in the mucus and move towards the less acidic
region (
).
H. pylori is found in the mucus, on the inner surface of the epithelium, and occasionally
inside the epithelial cells themselves. It adheres to the epithelial cells by
producing
, which bind to lipids and carbohydrates in the epithelial
In addition to using
chemotaxis to avoid areas of low pH
, H. pylori also
neutralizes the
acid in its environment by producing
, which breaks down the
urea present in the stomach to
. The ammonia, which is
basic, then neutralizes stomach.
Inflammation, gastritis, and ulcer:
H. pylori harms the stomach and duodenal linings by
several mechanisms
:
Diagram.1: showing how H. Pylor
ireaches the epithelium of the stomach
5
- The ammonia
produced to regulate pH is toxic to epithelial cells.
-Biochemicals produced by H. pylori such as
, vacuolating cytotoxin A (VacA)
[this damages epithelial cells, disrupts tight junctions and causes apoptosi.
. Cytotoxin associated gene CagA can also cause inflammation
and is potentially a carcinogen.
Colonization of the stomach by H. pylori can result in
chronic gastritis
of the stomach lining, at the site of infection). Helicobacter cysteine-rich proteins (Hcp),
particularly HcpA , are known to trigger an immune response, causing inflammation.
Ulcers in the stomach and duodenum result when
the consequences of inflammation
allow stomach acid and the digestive enzyme
that protect the stomach and duodenal
The location of colonization of H. pylori, which affects the location of the ulcer, depends
on the acidity of the stomach.
-
In people producing large amounts of acid
, H. pylori colonizes near the
(exit to the duodenum) to avoid the acid-secreting
(near the entrance to the stomach).
-In people producing normal or reduced amounts of acid
, H. pylori can also colonize the
rest of the stomach.
near the pyloric
antrum
in the antrum to secrete the hormone
, which
travels through the blood stream to parietal cells in the fundus.
Gastrin stimulates the
parietal cells to secrete more acid into the stomach lumen, and over time increases the
number of parietal cells, as well. The increased acid load damages the duodenum,
which may eventually result in ulcers forming in the duodenum.
While, H. pylori colonizes
other areas
of the stomach, the inflammatory response can
of the stomach lining and eventually ulcers in the stomach. This also
may increase the risk of stomach cancer.
Cancer:
Two related mechanisms by which H. pylori could promote
investigation:
One mechanism
:involves the enhanced production of
6
The Second
proposed mechanism:
has been called a "perigenetic pathway",
that
involves enhancement of the transformed host cell phenotype by means of alterations
in cell proteins, such as
H. pylori has been proposed to induce
and/or
(IL-6). According to the proposed perigenetic mechanism,
inflammation-associated signaling molecules, such as TNF-α, can alter gastric epithelial
cell adhesion and lead to the dispersion and migration of mutated epithelial cells
without the need for additional mutations in
, such as genes
that code for cell adhesion proteins.
The strain
of H. pylori to which a person is exposed may
influence the risk
of developing
gastric cancer.
Strains of H. pylori those appear to cause greater tissue damage found to produce high
levels of two proteins:
a-vacuolating toxin A (VacA)
.
b-the cytotoxin-associated gene A
(CagA
),.
These proteins are directly toxic to cells lining the stomach and signal strongly to the
immune system that an invasion is underway. As a result of the bacterial presence,
neutrophils and macrophages set up residence in the tissue to fight the bacteria.
Diagnosis:
One can test non invasively for H. pylori infection with:
, or with the
— or
-labelled
, which the bacterium metabolizes, producing that can
be detected in the breath).
3-A urine
test with a 96% sensitivity and 79% specificity is available.
None of the test methods is completely failsafe. Even biopsy is dependent on the
location of the biopsy. Blood antibody tests, for example, range from 76% to
84%
. Some drugs can affect H. pylori urease activity and give
4-The
most
accurate
method
for
detecting H.
pylori infection
is
with
examination from two sites after endoscopic
, combined with either
Treatment:
7
Once H. pylori is detected in a person with a peptic ulcer, the normal procedure is to
eradicate it and allow the ulcer to heal.
is a one-week (triple therapy) consisting of
Variations of the triple therapy have been developed over the years, such as using a
different proton pump inhibitor, as with
, or replacing
for people who are allergic to
Such a therapy
has revolutionized the treatment of peptic ulcers and has made a cure to the disease
possible. Previously, the only option was symptom control using
or proton pump inhibitors alone.
exerts a suppressive effect on H. pylori infection in both
animals and humans, and supplementing with
- and
containing yogurt improved the rates of eradication of H. pylori in humans.
[
Symbiotic
butyrate-producing bacteria which are normally present in the intestine are
sometimes used as probiotics to help suppress H. pylori infections as an adjunct to
antibiotic therapy.
it self is an antimicrobial which destroys the
Prevention:
H. pylori is a major cause of certain diseases of the upper gastrointestinal tract.
Rising
increases the need to search for new therapeutic
strategies; this might include prevention in form of vaccination. Much work has been
done on developing viable vaccines aimed at providing an alternative strategy to
control Helicobacter pylori infection and related diseases, including stomach cancer.
The presence of bacteria in the stomach may be beneficial, reducing the prevalence
of
, and
by influencing systemic immune responses.
Recent evidence suggests that nonpathogenic strains of H. pylori may be beneficial,
e.g., by normalizing stomach acid secretion, and may play a role in regulating appetite,
since its presence in the stomach results in a persistent but reversible reduction in the
level of
Epidemiology:
Person-to-person transmission of H. pylori by either the oral-oral or
most likely. Consistent with these transmission routes, the bacteria have been isolated
from
, and
8
Findings suggestthat H. pylori is more easily transmitted by gastric mucus than
saliva. H. pylori may also be transmitted orally by means of fecal matter through the
ingestion of waste-tainted water.
At least half the world's population is infected by the bacterium, making it the most
widespread infection in the world.
Actual infection rates vary from nation to nation;
the
has much higher infection rates than the West (
), where rates are estimated to be around 25%.
.
People infected with it at
an early age
are likely to develop more intense
inflammation that may be followed by atrophic gastritis with a higher subsequent risk
of gastric ulcer, gastric cancer, or both.
Acquisition at an
older age
brings different gastric changes more likely to lead to
duodenal ulcer.
Infections are usually acquired in early childhood in all
countries. However, the infection rate of children in developing nations is higher than
in
, probably due to poor sanitary conditions, perhaps combined
with lower antibiotics usage for unrelated pathologies.
In developed nations, it is currently uncommon to find infected children, but the
percentage of infected people increases with age, with about 50% infected for those
over the age of 60 compared with around 10% between 18 and 30 years.
The lower rate of infection in the West is largely attributed to higher hygiene
standards and widespread use of antibiotics and most likely due to socioeconomic
factors.
Despite high rates of infection in certain areas of the world, the overall frequency of H.
pylori infection is declining.
-resistant strains are found in most parts of
the world.
History:
Recent research states that genetic diversity in H. pylori, like that of its host, decreases
with geographic distance from East Africa, the birthplace of modern humans. H. Pylori
belived to migrated out of Africa along with its human host about 60,000 years ago. Its
subsequent evolution created seven prototypes.
H. pylori was first discovered in the stomachs of patients with gastritis and ulcers in
1982 by Drs.
. At the time, the
conventional thinking was that no bacterium could live in the acid environment of the
human stomach.
9
Before the research of Marshall and Warren, German scientists found spiral-
shaped
in the lining of the human stomach in 1875, but they were unable
them, and the results were eventually forgotten. Several small studies
conducted in the early 20th century demonstrated the presence of curved rods in the
stomachs of many people with peptic ulcers and stomach cancers.
After unsuccessful attempts at culturing the bacteria from the stomach; Barry
Marshall finally succeeded in visualizing colonies in 1982, when they unintentionally
left their
incubating for five days over the
paper, Warren and Marshall contended that most stomach ulcers and gastritis were
caused by bacterial infection and not by
, as had been assumed
before.
To demonstrate H. pylori caused gastritis and was not merely a bystander; Marshall
drank a beaker of H. pylori culture. He became ill with nausea and vomiting several
days later. An
10 days after inoculation revealed signs of gastritis and the
presence of H. pylori. These results suggested H. pylori was the causative agent.
therapy for the treatment of duodenal ulcers.
[
stated most recurrent duodenal and gastric
ulcers were caused by H. pylori, and recommended antibiotics be included in the
treatment regimen.
