IMMUNOLOGY
Lecture-Major Histocompatibility Complex(MHC) and organ Transplantation
By
Dr.Sana'a Khudhur
Major Histocompatibility Complex(MHC)
The major histocompatibility complex (MHC) :is a locus on a chromosome 6 comprised of multiple genes encoding histocompatibility antigens. MHC is also called human leukocyte antigen (HLA).
Important properties of MHC
1-Cluster of genes found in all mammals.
2-Its products play role in discriminating self/non-self.
3-Participant in both humoral and cell-mediated immunity.
4-MHC Act As Antigen Presenting Structures.
5-In Human MHC is Found on Chromosome 6 referred to as HLA complex.
6- MHC genes are highly polymorphic.
7-Bind peptide: recognized by T cells: Th__MHCII , Tc__MHCI.
8- MHC structure determined by X-ray crystallography.
Human HLA Gene Complex
In man, the MHC locus is designated as HLA (Human Leukocyte Antigen).
HLA=Human Leukocyte Antigen.
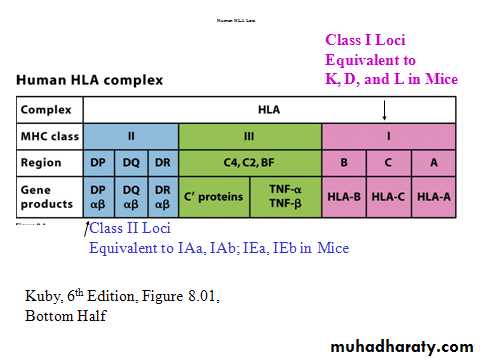
Genes Of MHC Organized In 3 Classes (figure 1)
Class I MHC genes
1-Glycoproteins expressed on all nucleated cells.
2-Major function to present processed Ags to TC .
3-The Class I region consists of HLA-A, HLA- B, and HLA-C loci.
Class II MHC genes
1-Glycoproteins expressed(found on the surface )on professional antigen presenting macrophages( M), B-cells, Dentritic cells (DCs), langerhans cells.
2- The Class II region consists of the D region which is subdivided into HLA-DP, HLA-DQ, and HLA-DR sub regions (several HLA-D loci determine the class II MHC proteins i.e. DP, DQ and DR).
3-Major function to present processed Ags to TH.
4-Helper T-cells recognize antigens on antigen-presenting cells only when the antigens are presented on the surface of cells in association with class II MHC.
5-Class II antigens react with the CD4 molecule on the helper T-cells which secrete cytokine.
Class III MHC genes
Products that include secreted proteins that have immune
functions. Ex. Complement system, inflammatory molecules. Class III molecules are encoded by genes located between those that encode class I and class II molecules.
Table 1:Human HLA complex
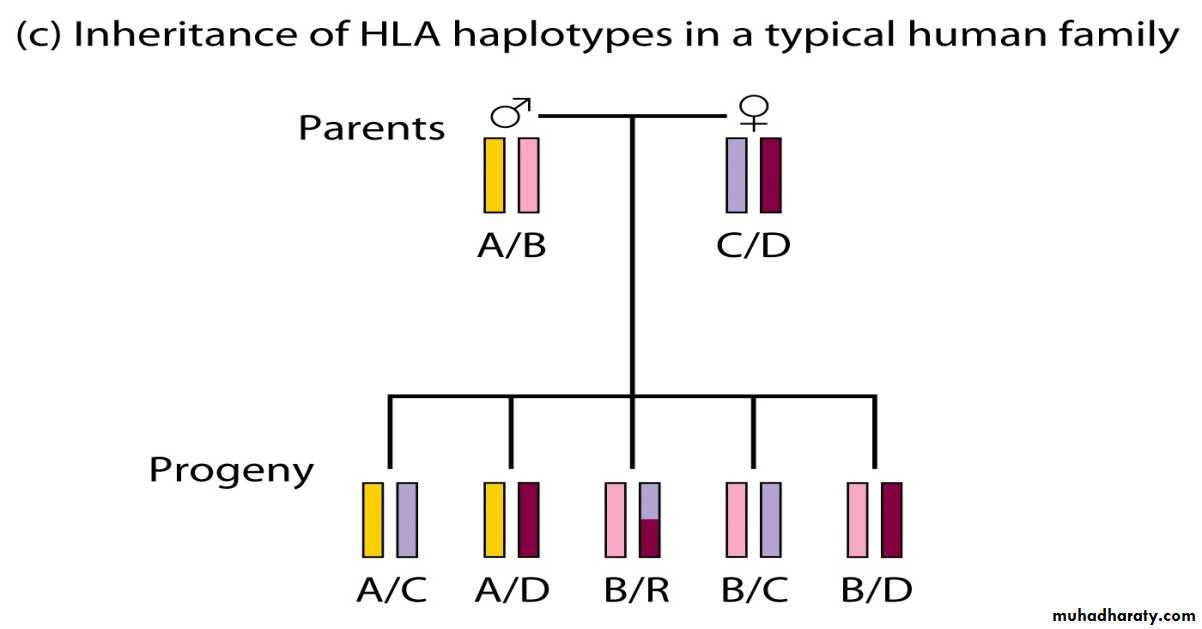
MHC Genes Are PolymorphicInherited as 2 sets (one from father, one from mother):
1-Haplotype refers to set from mother or father.
MHC Products Are Highly Polymorphic. 2-
3-Vary considerably from person to person .
Inheritance Of HLA Haplotypes
MHC protein
MHC class I protein molecule
MHC I occurs as an α chain composed of three domains—α1, α2, α3. The α1 rests upon a unit of the non-MHC molecule β2 microglobulin . The α3 subunit is transmembrane, anchoring the MHC class I molecule to the cell membrane(figure 1).
Figure1:
MHC class I protein molecule
MHC class II protein molecule
MHC II is formed of two chains, α and β, each having two domains—α1 and α2 and β1 and β2—each chain having a transmembrane domain, α2 and β2, respectively, anchoring the MHC class II molecule to the cell membrane.The peptide-binding groove is formed of the heterodimer of α1 and β1(figure 2).
Figure 2: MHC class II
protein moleculeMHC Class III
Class III molecules have physiologic roles unlike classes I and class II, but are encoded between them in the short arm of human chromosome 6. Class III molecules include several secreted proteins with immune functions: components of the complement system (such as C2, C4), cytokines (such as TNF-α and heat shock proteins (hsp).Antigen processing and presentation
Antigen processing:
Proteolytic cleavage of proteins into small fragments(antigen peptides) that can bind to MHC molecules on antigen presenting cells.
Antigen presentation: Presentation of antigen peptides to T cell receptor on T cells. Different antigen degradation and processing pathways produce MHC-peptide complexes.
Peptides are processed and presented by two classical pathways:
Endogenous” peptides associate with Class I molecules.All nucleated cells are able to present with Class I.
In MHC class I any nucleated cell normally presents cytosolic peptides, mostly self peptides derived from protein turnover and defective ribosomal products.
During viral infection, intracellular microorganism infection, or cancerous transformation, such proteins degraded in the proteosome are as well loaded onto MHC class I molecules and displayed on the cell surface.
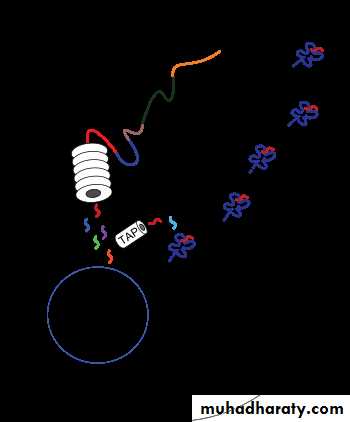
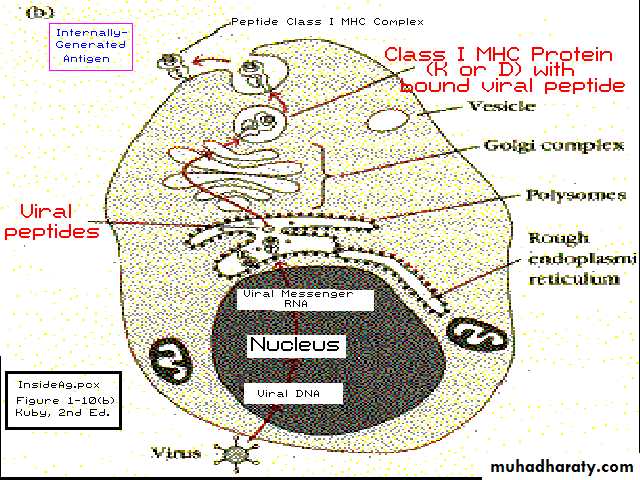
MHC class I pathway:
Proteins in the cytosol are degraded by the proteasome, liberating peptides internalized by TAP channel in the endoplasmic reticulum, there associating with MHC-I molecules .
MHC-I/peptide complexes enter Golgi apparatus, enter secratory vesicles, fuse with the cell membrane, and externalize on the cell membrane interacting with T lymphocytes( figure 3,4).
Figure 3: MHC class I pathway
Figure 4: MHC class I pathway
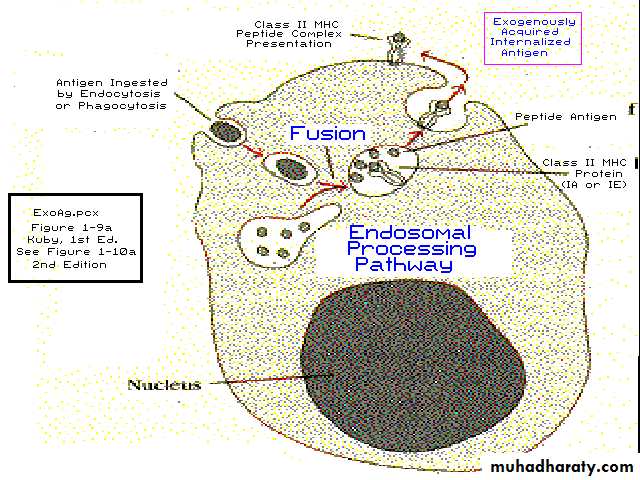
MHC class II Pathway“Exogenous” peptides associate with Class II molecules
Only specialized APCs may present with Class II, such as macrophages, B cells and dendritic cells, and thymic epithelial cells.
In MHC class II phagocytes such as macrophages and immature dendritic cells uptake entities by phagocytosis into phagosomes which fuse with lysosomes whose acidic enzymes cleave the uptaken protein into many different peptides interaction with the particula. These are trafficked to and externalized on the cell surface(Figure 5).
Figure 5: MHC class I I pathway
Biologic importance of MHC1-Role in immune response through MHC Restriction
MHC Restriction
MHC restriction means that different T cells are restricted to either Class I or Class II MHC antigens The T cell receptor will recognise a peptide only when it is bound to a particular MHC molecule(Figure 6).
Cytotoxic T cells are restricted to Class I antigens present on nucleated body cells, thus play a role in protecting against virus-infected cells or cancerous cells.
Helper CD4 cells are restricted to Class II MHC antigens present on immune cells, thus play a role in increasing the humoral immune response and protecting against bacterial,parasitic infection and toxin.
Figure 6: MHC restriction
3-Role in organ transplantation,the success of organ transplantation determind by the compatibility of the MHC genes of the donor and recipient.4-MHC gene and proteins important in autoimmune disease which occur in people who carry certain MHCgene.
Transplantation and Graft Rejection
Types of grafts1) Autografts :
The transfer of an individual’s own tissues from place to place e.g. Skin grafts (regularly accepted).
2) Isografts :
Transfer of tissues between genetically identical personse.g. Identical twins ( accepted permanently).
3) Allografts (homograft):
- Transfer of a graft between genetically different members of same speciese.g from one human to another.
- Rejection occur if donor and recipient are not matched.
4) Xenograft (heterograft):
- Transfer of tissues between different species
- Always rejected
Transplant rejection
The rapid and very potent cell-mediated immune response to the transplanted tissue results from a large number of T cells that are specifically reactive to non-self.
Mechanism Of Graft Rejection
1) Both TH and TC are activated
- TC cells destroy graft cells by direct contact
-TH cells secrete cytokines that attract and activate macrophages, NK cells and polymorphs leading to cellular infiltration and destruction of graft (Type IV)
- B cells recognize foreign antigens on the graft and produce antibodies which bind to graft cells and:
. Activate complement causing cell lysis.
. Enhance phagocytosis, i.e. opsonization (Type II).
. Lead to ADCC by macrophages, NK,PML(Type II).
-Immune complex deposition on the vessel walls induce platelets aggregation and microthrombi leading to ischemia and necrosis of graft (Type II).
Types Of Graft Rejection
1) Hyperacute rejection:
- It occurs hours after transplantation
- In individual with preformed antibodies either due to - blood groups incompatibility or previous sensitization by blood transfusion, previous transplantation
2) Acute Rejection:
- It occurs 10 to 30 days after transplantation
- It is mainly T-cell mediated
3) Chronic or late rejection:
- It occurs over a period of months or years.
- It may be cell mediated, antibody mediated or both.
Graft Versus Host (GVH) Reaction
Immunologically competent graft is transplanted into an immunologically suppressed recipient (host).
The grafted cells survive and react against the host cells
i.e instead of reaction of host against the graft, the reverse occurs.
* GVH reaction is characterized by fever, pancytopenia, weight loss, rash , diarrhea, hepatsplenomegaly and death