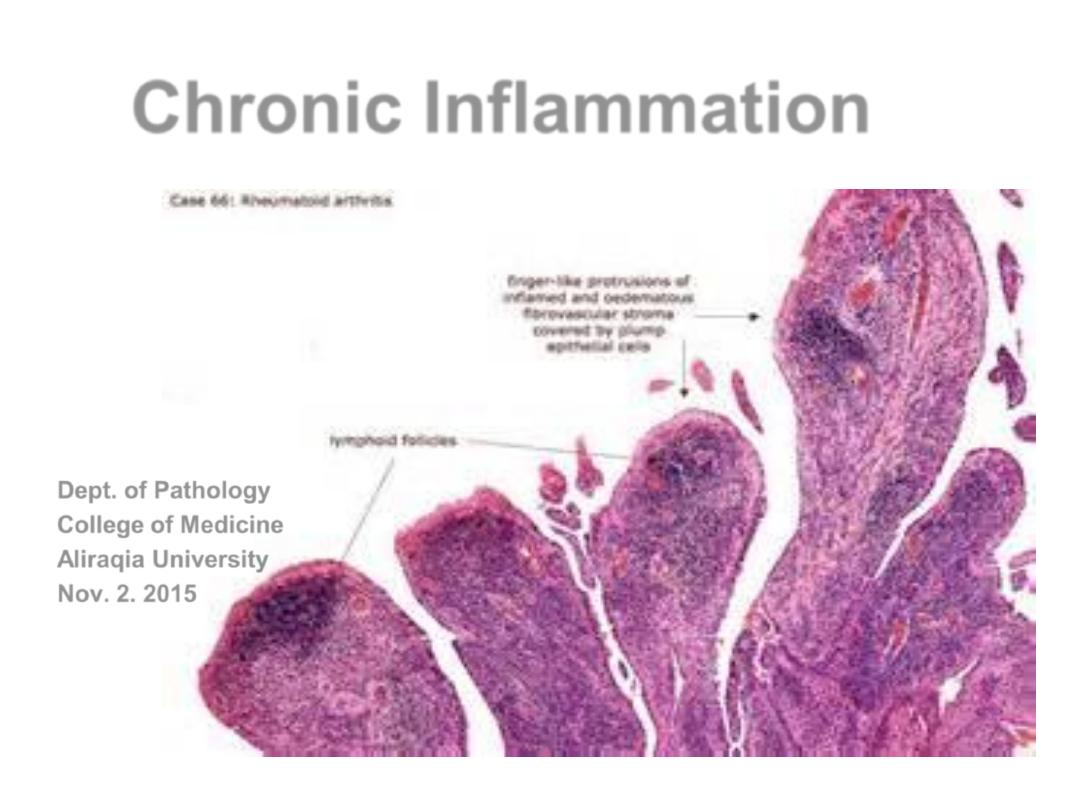
Chronic
Inflammation
Dept. of Pathology
College of Medicine
Aliraqia University
Nov. 2. 2015
Objectives
Chronic Inflammation;
• Definition
• Characteristic changes (Morphology).
• Causes.
• Ch. Inflamm. Cells & Mediators.
• Granulomatous Inflammation.
• Systemic effects of inflammation.
Chronic inflammation
;
• long lasting inflammation (weeks to years) due to
persistent stimuli.
• Continuing
inflammation
, tissue
injury
& healing by
fibrosis
.
MORPHOLOGIC FEATURES
• Mononuclear cells infiltration.
• Tissue destruction and
• repair (
fibroblast proliferation
)
.
• It can follow acute inflammation or can be chronic right
from the beginning
.
Causes of Chronic inflammation
• Arises in followings ways.
– Persistent infection
; (TB, T. pallidum, viruses & Fungi)
i.e. chronic right from the beginning
-- Immune mediated inflammatory diseases
.
-- Prolonged exposure to
toxic agents
; (Silica, lipid)
-- After
acute inflammation
,
persistent
of injurious agents
or interference with healing (peptic ulcer).
progression
of
acute inflammation.
Recurrent
attacks of acute
inflammation.
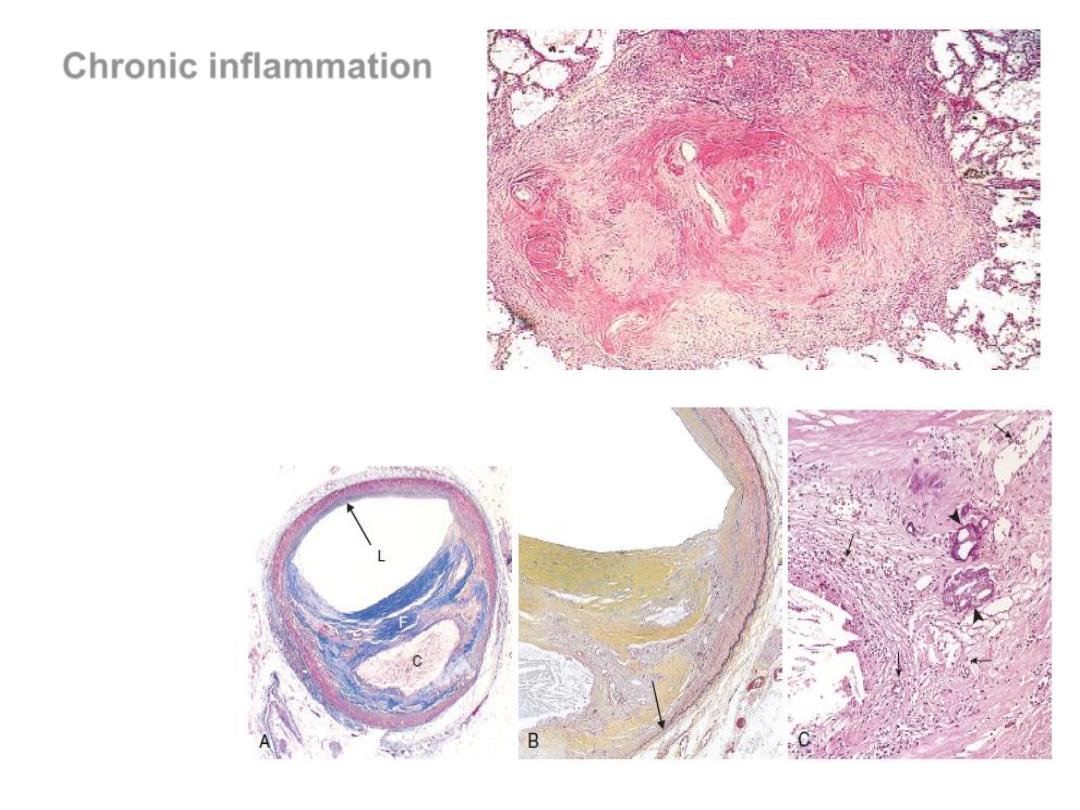
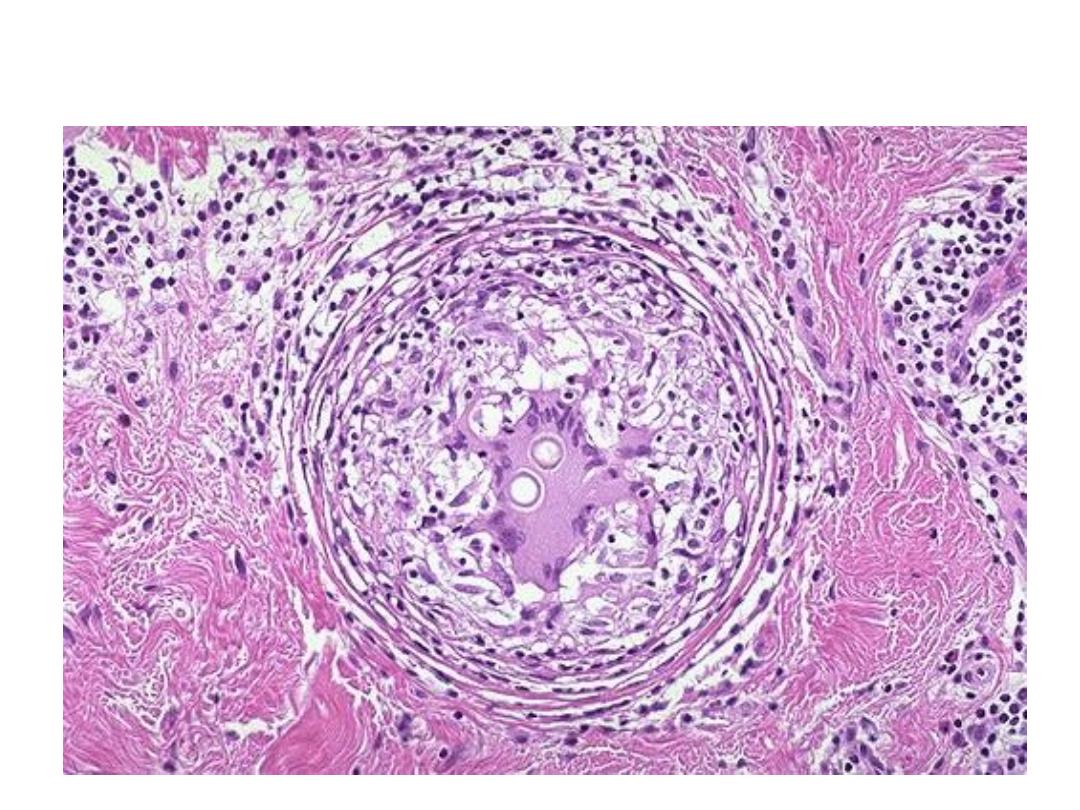
Several coalescent silicotic nodules
Atherosclerotic plaque in the coronary artery
Prolonged exposure
to toxic agents
Neurodegenerative
disorders (Alzheimer
disease), AS, DM, ca
.
Chronic inflammation
Cellular Players
• MACROPHAGES (aka, HISTIOCYTES)
• LYMPHOCYTES
• PLASMA CELLS
• EOSINOPHILS
• MAST CELLS
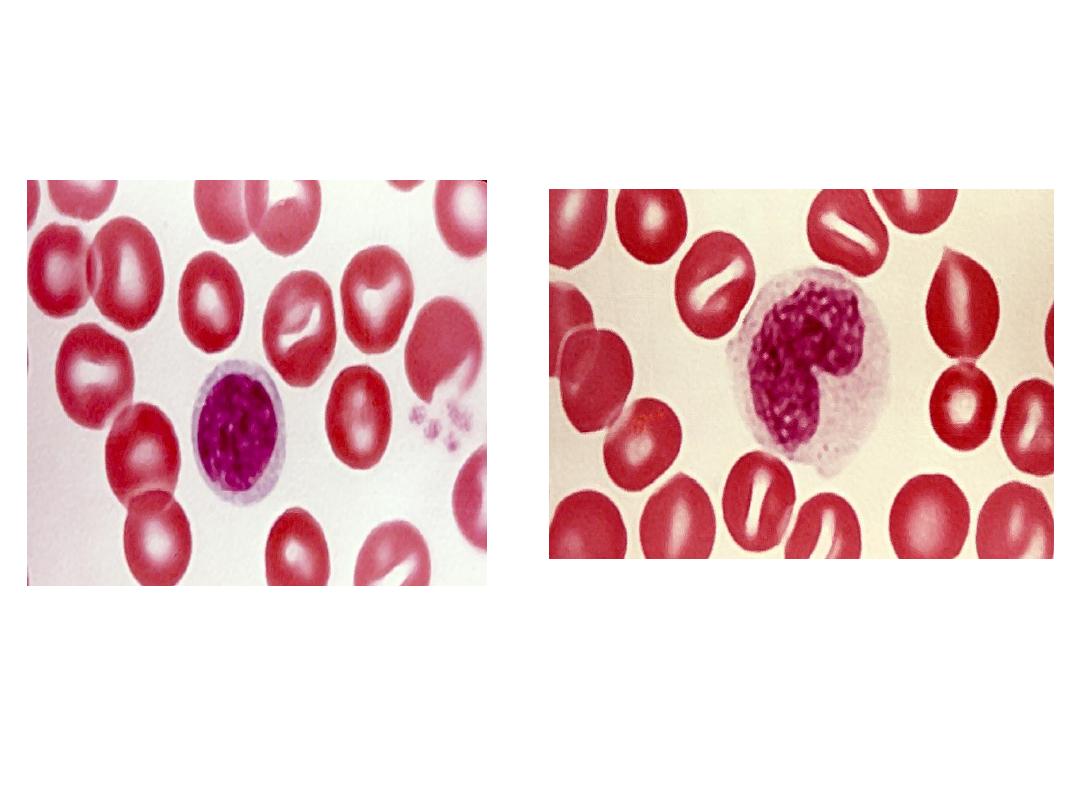
CHRONIC INFLAMMATION
Cells
(Mononuclear)
LYMPHOCYTE
MONOCYTE
MACROPHAGE
HISTIOCYTE
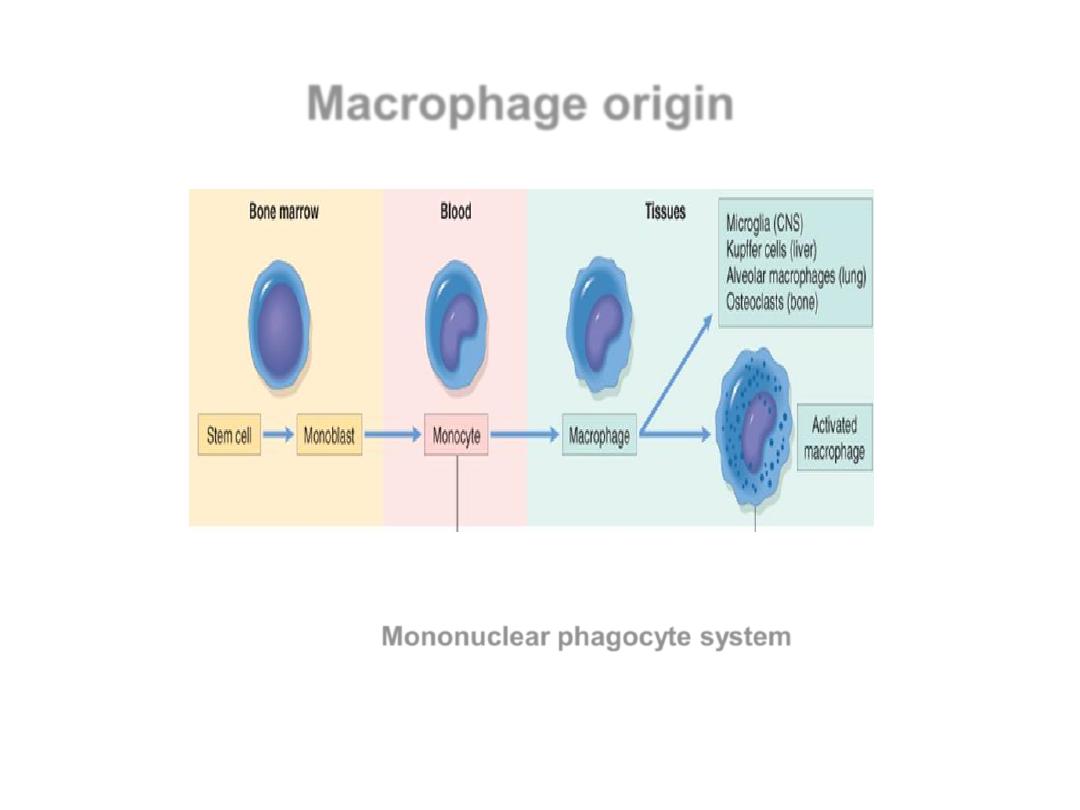
Macrophage origin
Mononuclear phagocyte system
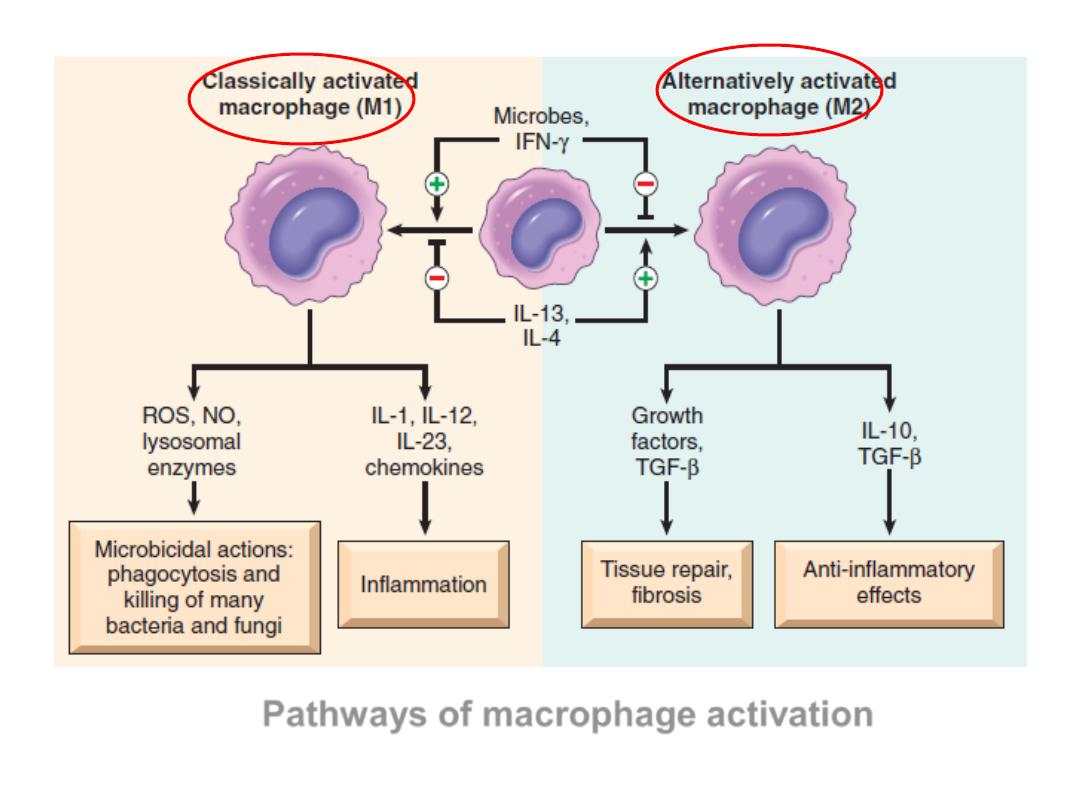
Pathways of macrophage activation
increased cell size,
lysosomal enz,
phagocytose

• Pathways of macrophage activation. Different stimuli activate
monocytes/macrophages to develop into functionally distinct
populations.
• Classically activated macrophages are induced by microbial
products and cytokines, particularly IFN-
γ, and are microbicidal and
involved in potentially
• harmful inflammation. Alternatively activated macrophages are
induced by IL-4 and IL-13, produced by TH2 cells (a helper T cell
subset) and other
• leukocytes, and are important in tissue repair and fibrosis. IFN-γ,
interferon-
γ; IL-4, IL-13, interkeukin-4, -13.
• IFN-γ can also induce macrophages to fuse into
large,multinucleate giant cells
Macrophages have several critical roles in defense &
the inflammatory response.
• Phagocytosis.
• Macrophages initiate the process of tissue repair.
• Secrete mediators of inflammation (TNF, IL-1,
chemokines, and others) and eicosanoids.
• Display Ags to T lymphocytes and respond to signals
from T cells, thus setting up cell mediated IR.
Lymphocytes
• TH1
cells produce IFN-γ, which activates macrophages.
• TH2
cells secrete IL-4, IL-5, and IL-13, which activate
eosinophils and macrophages.
• TH17
cells secrete IL-17 and other cytokines that
activate PMN & monocytes into the reaction
.
• Activated T lymphocytes
, in turn, produce cytokines,
which recruit and activate macrophages and thus
promote more antigen presentation and cytokine
secretion.
• The result is
a cycle of cellular reactions that fuel and
sustain chronic inflammation
.
• In some strong and prolonged inflammatory reactions,
the accumulation of lymphocytes, APC, and plasma
cells, is seen in the synovium in long-standing
rheumatoid arthritis and in autoimmune thyroiditis.
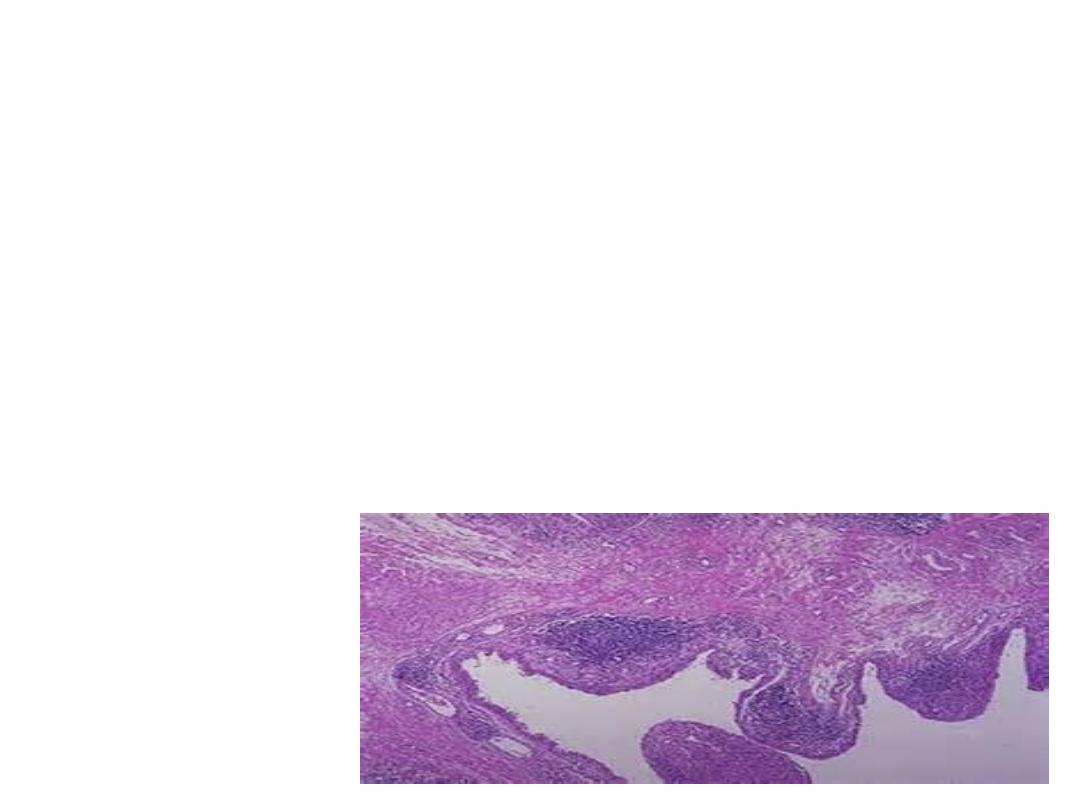
Chronic inflammation in the lung
Acute inflammation in the lung
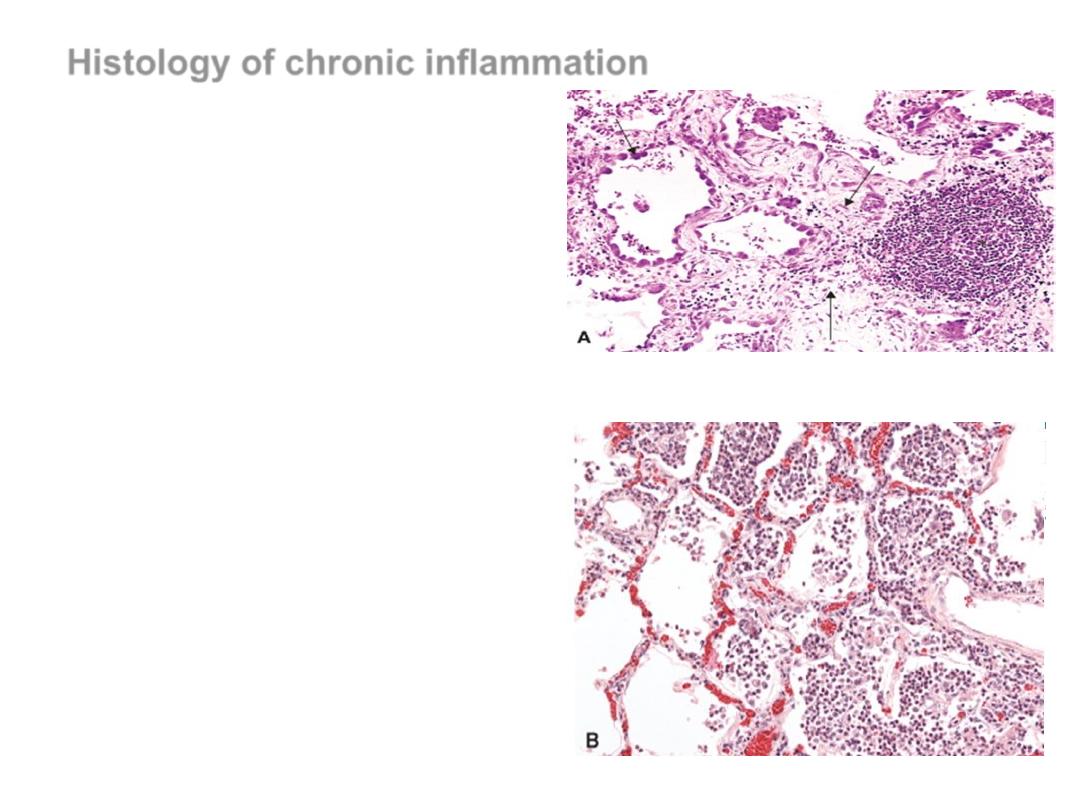
Histology of chronic inflammation
Lymphocytes, plasma cells, and
macrophages
Proliferation of fibroblasts & small
blood vessels, Increased CT
Tissue destruction
Types of chronic inflammation
•
Nonspecific,
e.g.chronic peptic ulcer
&
•
Specific
(granulomatous) Inflamm
.
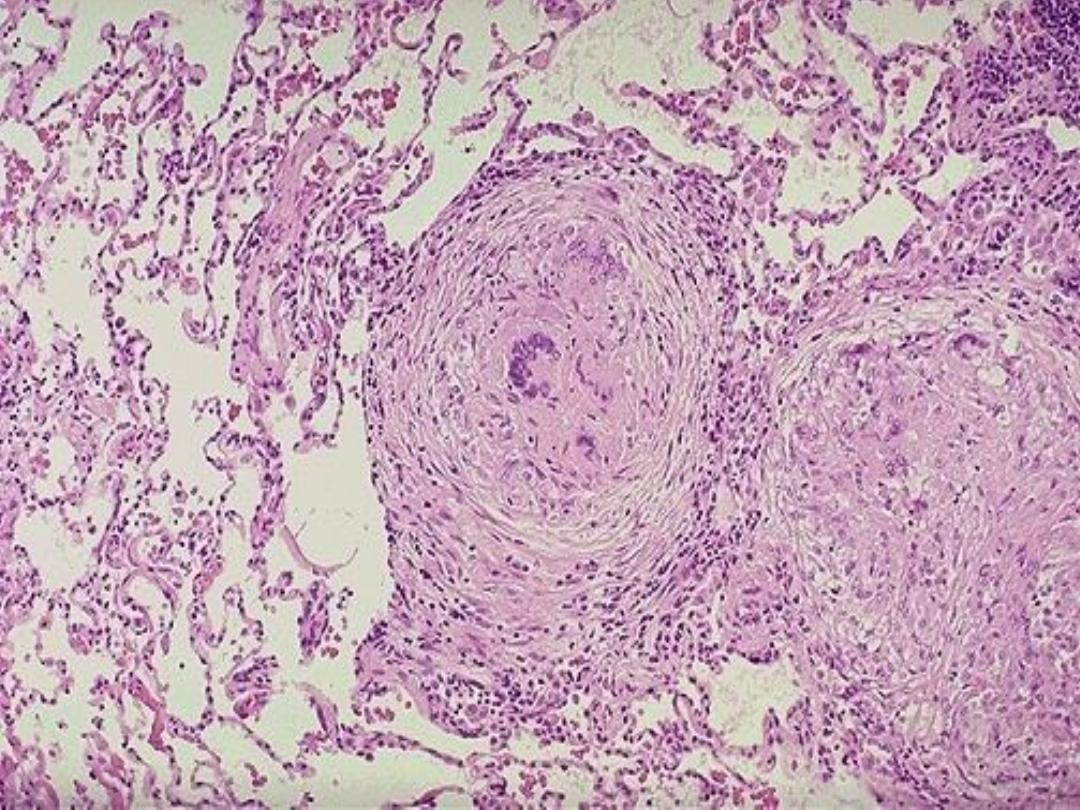
GRANULOMA

•
Granulomatous reactions are commonly
seen with mycobacteria, fungi, sarcoid,
foreign bodies, and rarely with almost
anything. Acid fast or fungal cultures may
possibly be positive in “fresh” granulomas,
gram positive or gram negative bacteria
are NOT common causes of granulomas.
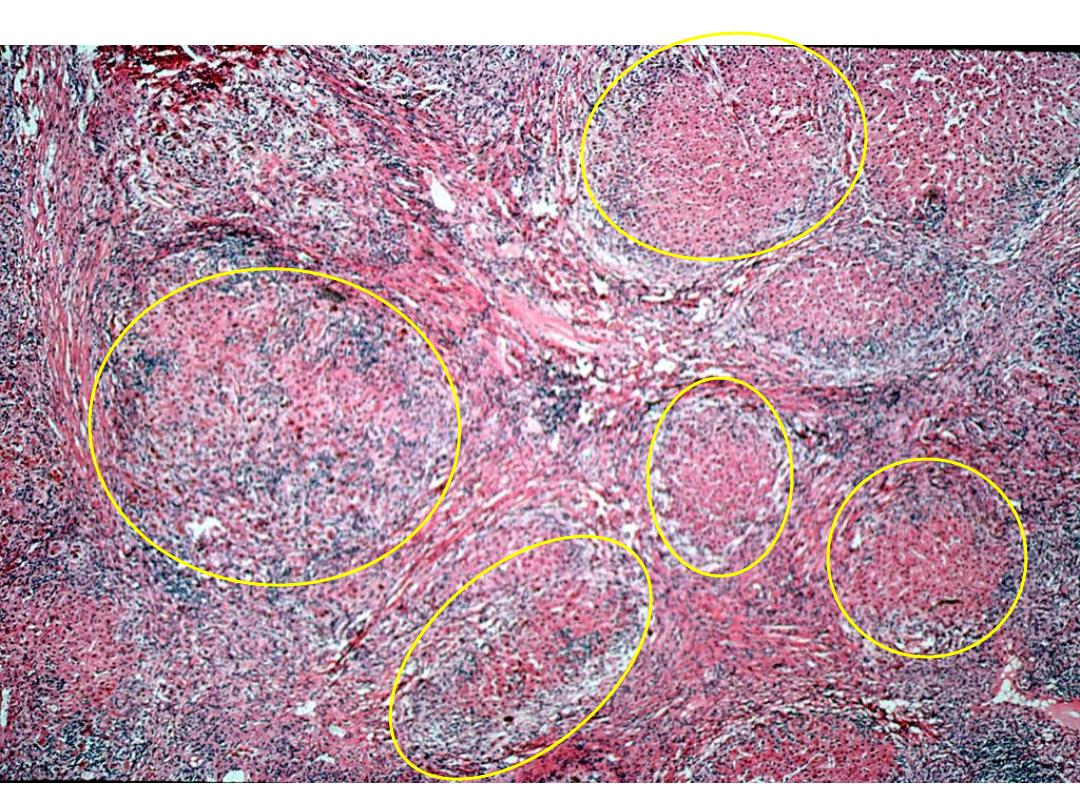

• Granulomatous inflammation
is a distinctive
pattern of chronic inflammation characterized by
aggregates of activated macrophages with
lymphocytes.
• Granulomas are characteristic of certain specific
pathologic states;
• Recognition of the granulomatous pattern is
important because of the limited number of
conditions that cause it
Chronic Granulomatous Inflammation
• Granulomas,
by aggregates of activated macrophages with
lymphocytes.
• Granulomas are characteristic of certain specific pathologic states;

• Granulomatous inflammation
is a
distinctive pattern of chronic inflammation
characterized by
aggregates of activated
macrophages with lymphocytes.
• Granulomas are characteristic of certain
specific pathologic states;
• Recognition of the granulomatous pattern
is important because of the limited number
of conditions that cause it

Classification of granulomatous
inflammation, according to the etiology
• Infectious granuloma
:
– Bacterial
:
• Mycobacterium tuberculosis (Koch bacillus) - Tuberculosis
• Mycobacterium leprae - Leprosy
• Treponema pallidum - Syphilis
• Gram-positive bacillus (Actinomyces israeli) - Actinomycosis
• Gram-negative bacillus (Bartonella henselae) - Cat-scratch disease
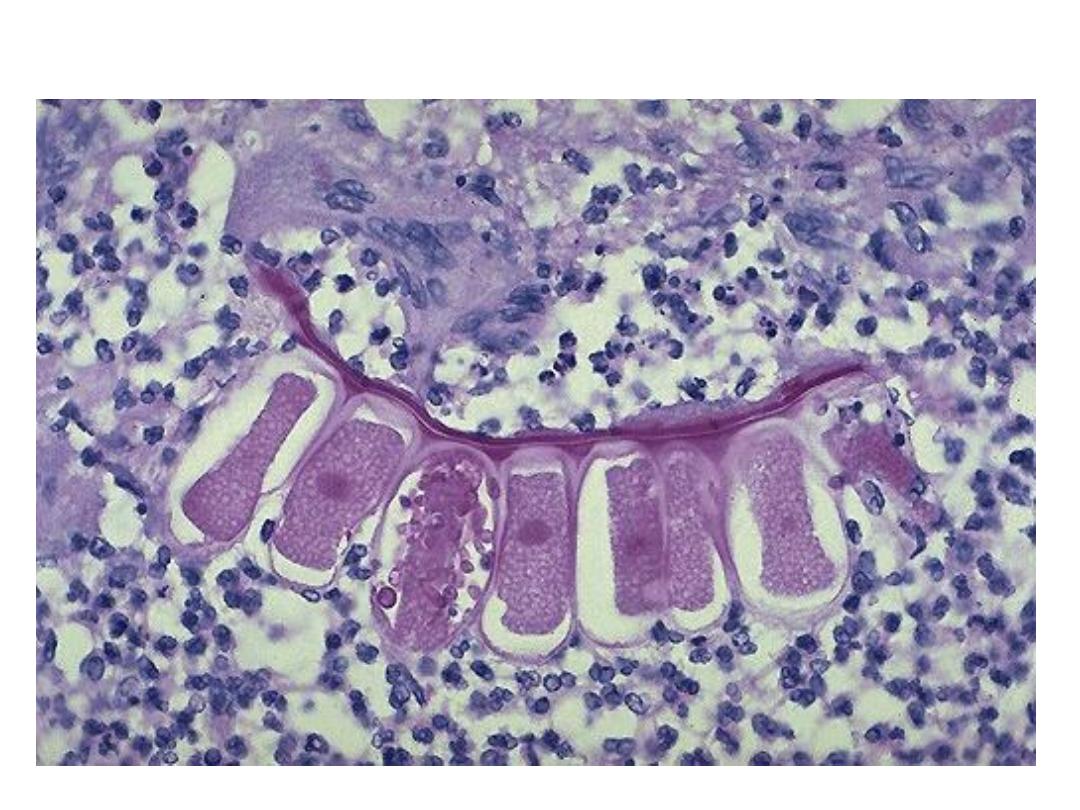
– Parasitic
:
• Schistosomiasis
• Toxoplasma gondii - Toxoplasmosis
– Fungi (Candida albicans) - Candidiasis
• Foreign body granuloma
• Unknown etiology granuloma
:
– Sarcoidosis
– Crohn's disease

Two factors necessary for granuloma formation
• Presence of indigestible organisms or particles
(Tb, mineral oil, etc)
• Cell mediated immunity (T cells)
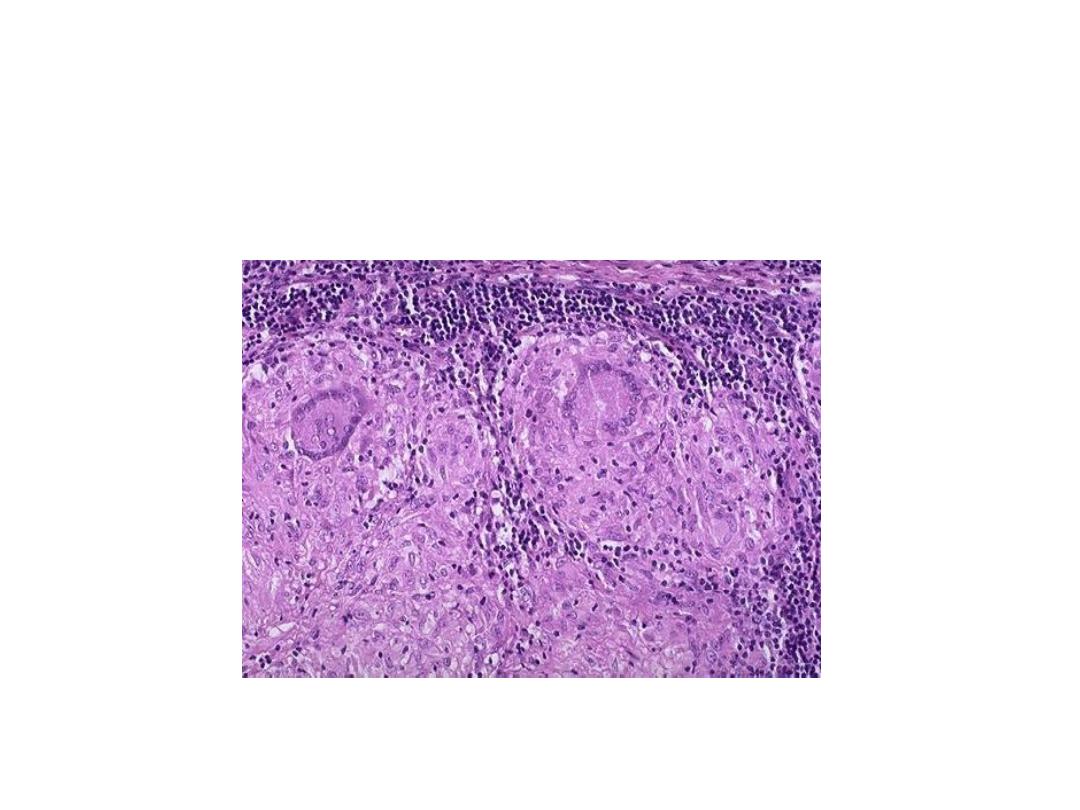
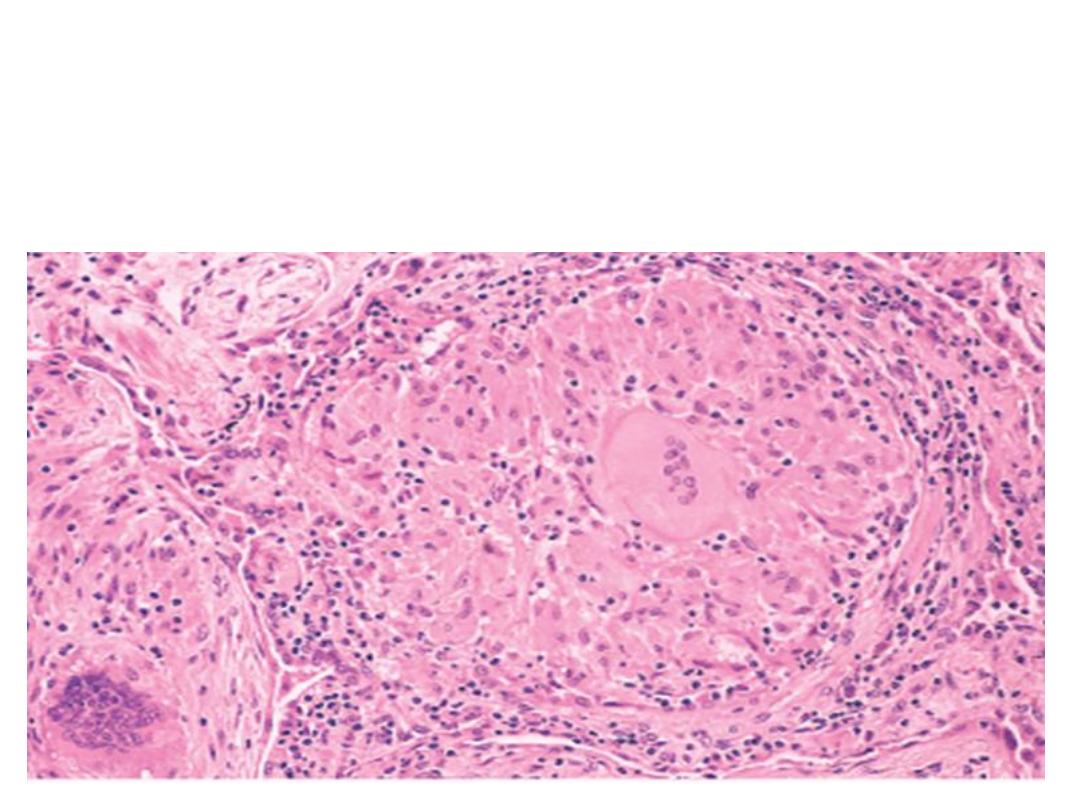
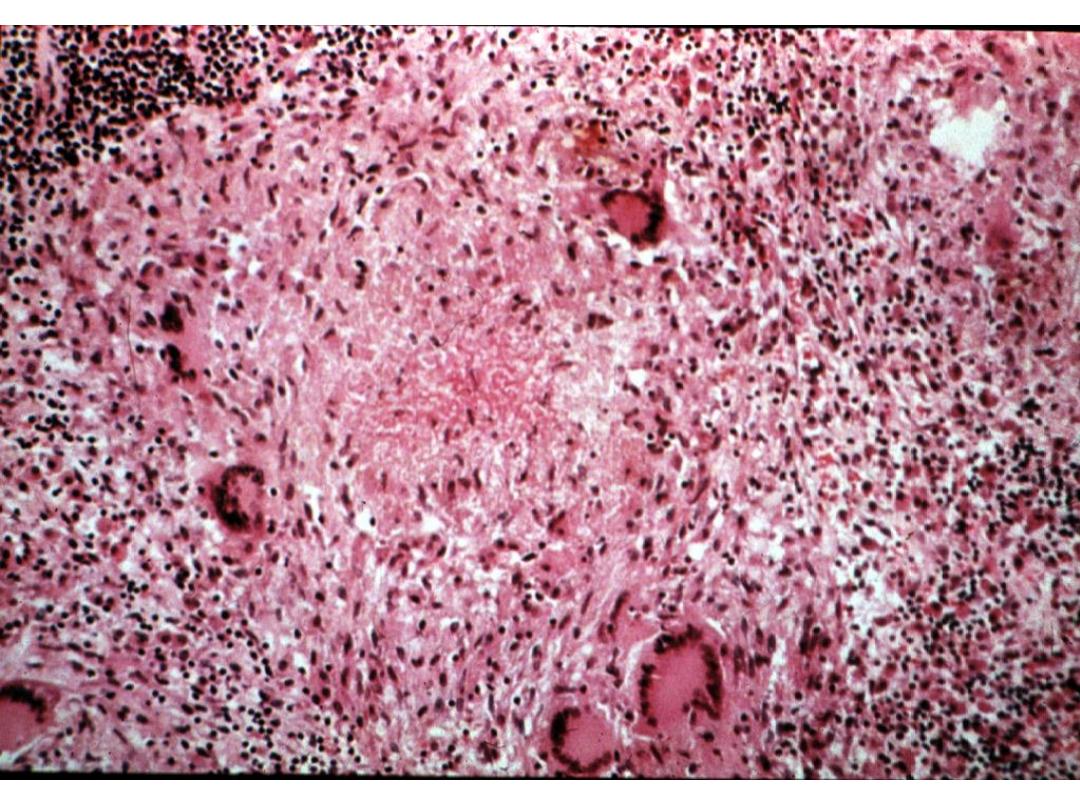
TB Granuloma
Fungal granuloma
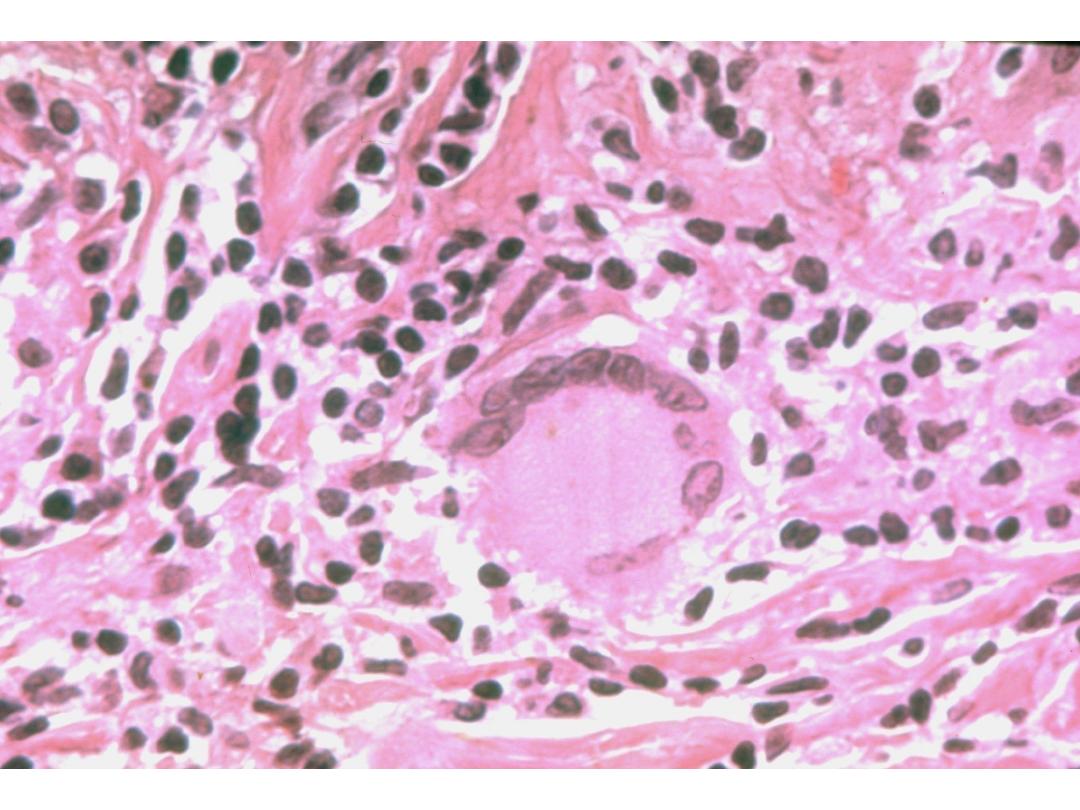
Foreign body giant cell
GRANULOMAS
GRANULOMATOUS INFLAMMATION
CASEATING (TB)
NON-CASEATING

LYMPHATIC DRAINAGE
• SITE REGIONAL LYMPH NODES

SYSTEMIC MANIFESTATIONS
(NON-SPECIFIC)
• FEVER, CHILLS
• C-Reactive Protein (CRP)
• “Acute Phase” Reactants
• Erythrocyte Sedimentation Rate (ESR) increases
• Leukocytosis
• Pulse, Blood Pressure
• Cytokine Effects, e.g., TNF(α), IL-1
Systemic effects
• Fever
– cytokine-mediated (IL-1, IL-6, TNF)
– acute-phase reactions including
• Anorexia
• Skeletal muscle protein degradation
• Hypotension
• Leukocytosis
– Elevated white blood cell count
– Bacterial infection (neutrophilia)
– Parasitic infection (eosinophilia)
– Viral infection (lymphocytosis
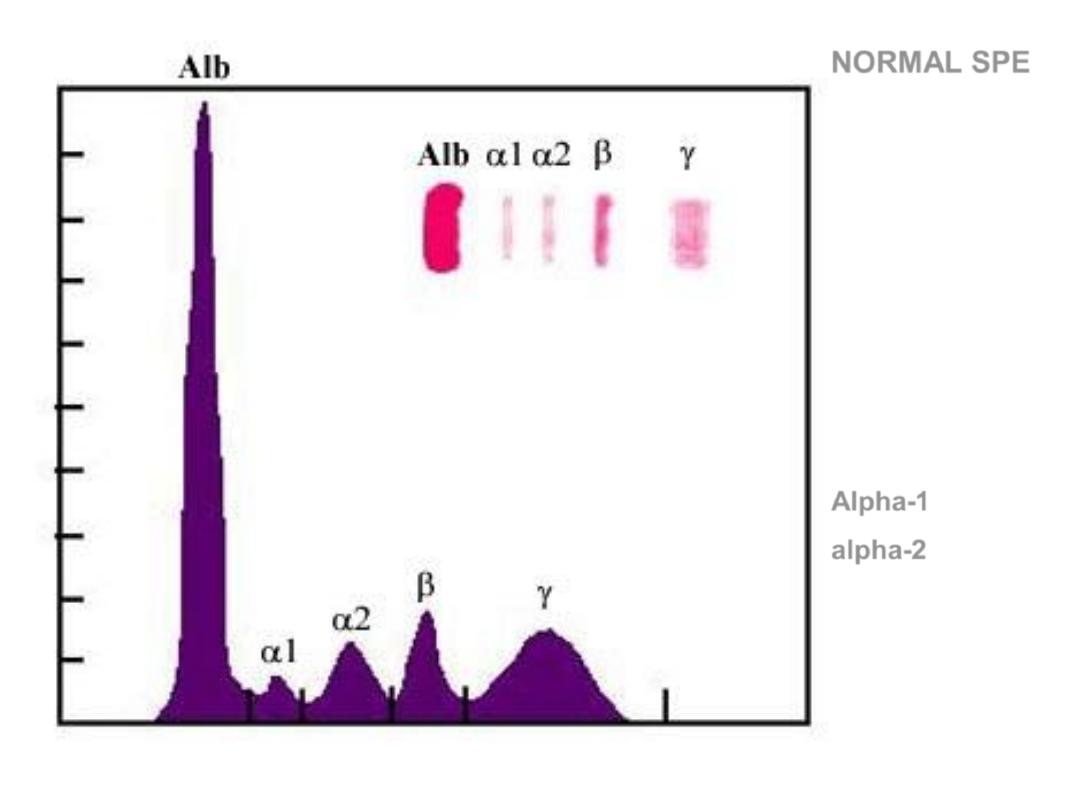
NORMAL SPE
Serum
Protein
Electrophoresis
In ACUTE
Inflammation
Alpha-1
alpha-2
are increased,
i.e.,
“acute phase”
reactants.
Outcome of chronic inflammation
• Resolution
/regeneration/restitution of normal
structure
• Repair
/organization/healing by connective
tissue/fibrosis/scarring
• It can
continue
indefinitely, e.g. rheumatoid arthritis
..
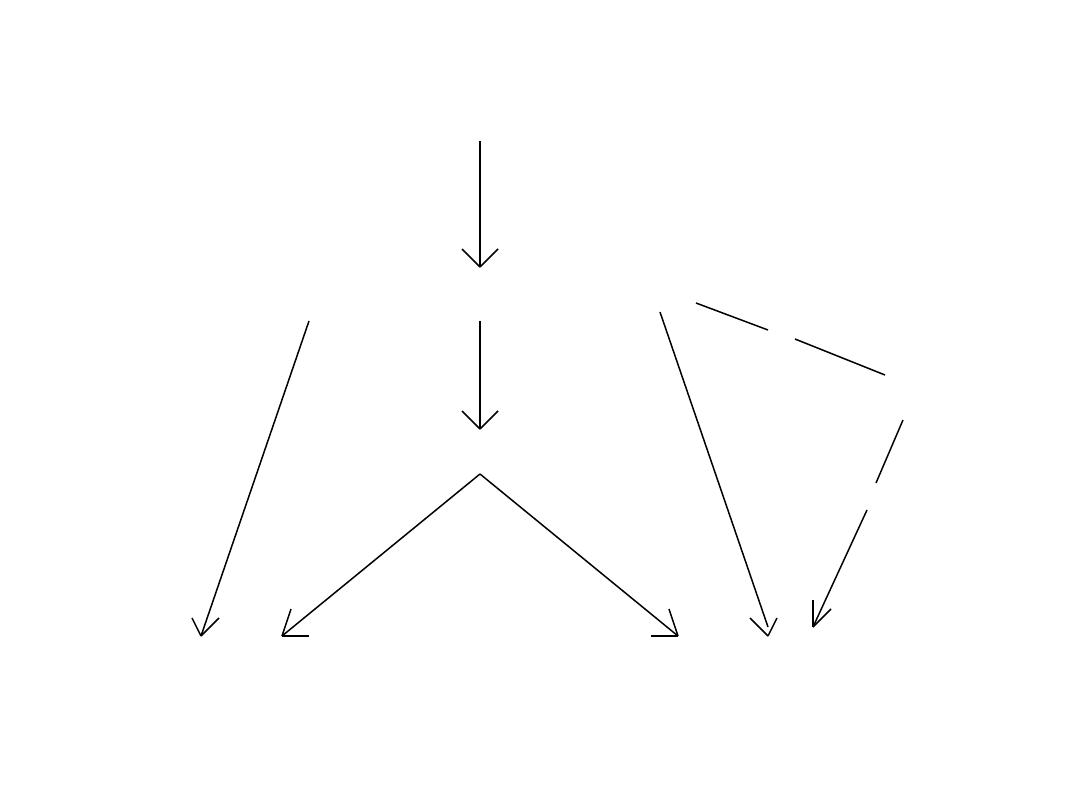
Acute inflammation
Chronic inflammation
Repair
Resolution
Abscess
Injury

Factors necessary for resolution
• Removal of the offending agent
• Regenerative ability if cells have been
destroyed
• Intact
stromal framework (ECM)
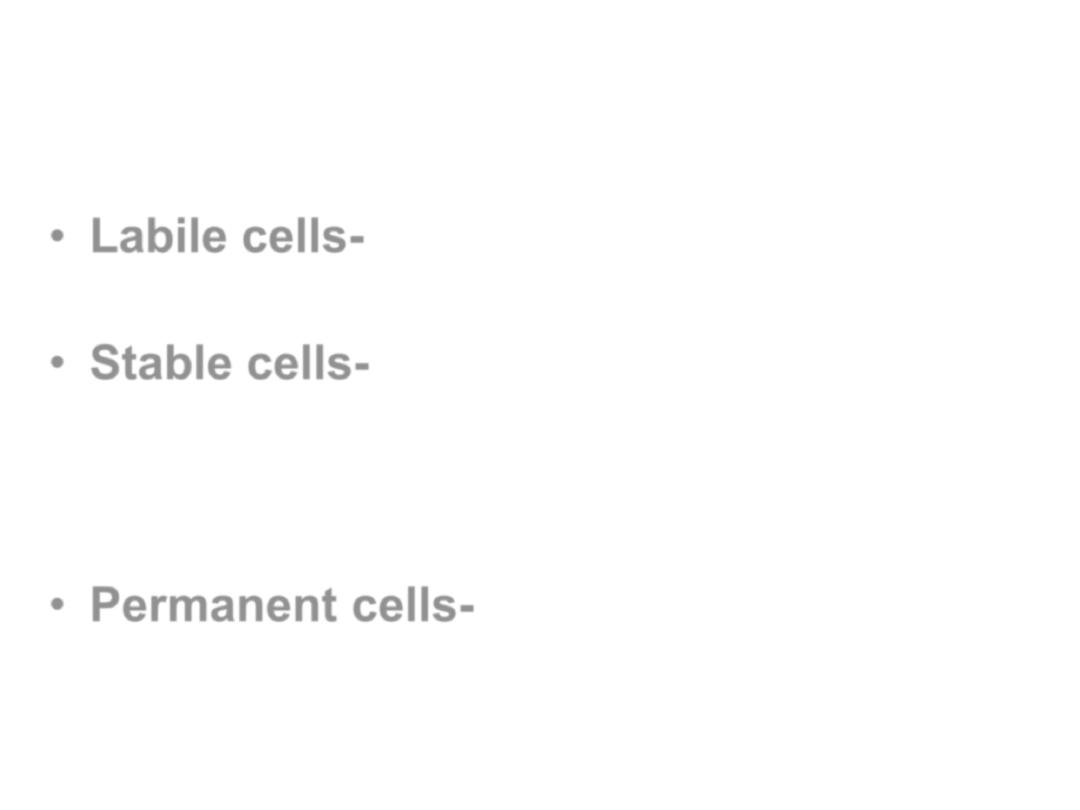
Categorization of cells based on
regenerative ability
:
• Labile cells-
-cells which continue to
proliferate throughout life (gut, skin, BM)
• Stable cells-
-cells which retain the capacity
to proliferate throughout life but usually do
not unless stimulated (liver, kidney,
pancreas, bone)
• Permanent cells-
-cells which cannot
reproduce themselves after birth (neurons,
cardiac and skeletal muscle)

Granulomatous Inflammation
•
Clusters of T cell-activated macrophages,
which engulf and surround indigestible
foreign bodies (mycobacteria,
H.
capsulatum
, silica, suture material)
•
Resemble squamous cells, therefore
called “epithelioid” granulomas
Lymph Nodes and Lymphatics
•
Lymphatics drain tissues
–
Flow increased in inflammation
–
Antigen to the lymph node
–
Toxins, infectious agents also to the node
•
Lymphadenitis, lymphangitis
•
bacteremia
Usually contained there, otherwise
ensues
•
Tissue-resident macrophages must then prevent
overwhelming infection
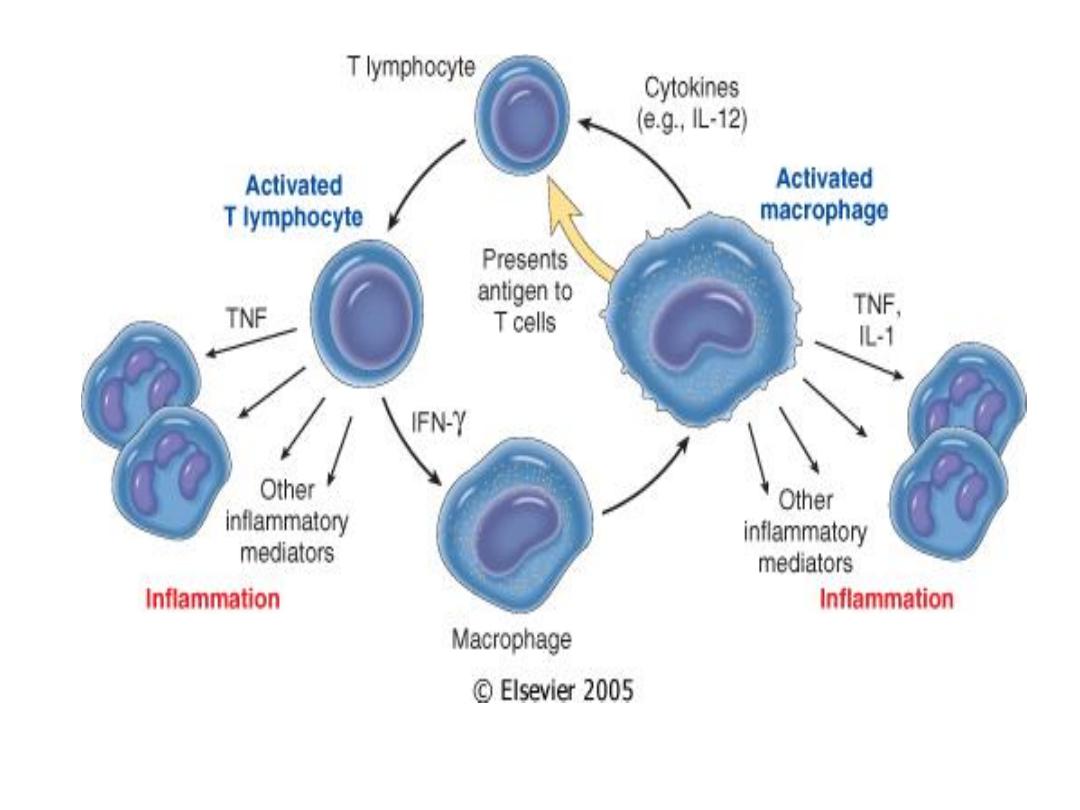
Macrophage-lymphocyte interactions in chronic inflammation
.

Patterns of acute and chronic
inflammation
• Serous
– Watery, protein-poor effusion (e.g., blister)
• Fibrinous
– Fibrin accumulation
– Either entirely removed or becomes fibrotic
• Suppurative
– Presence of pus (pyogenic staph spp.)
– Often walled-off if persistent
Patterns (cont’d)
•
Ulceration
–
Necrotic and eroded epithelial surface
–
Underlying acute and chronic inflammation
–
Trauma, toxins, vascular insufficiency

• Features of Chronic Inflammation
• • Prolonged host response to persistent stimulus
• Caused by microbes that resist elimination, immune
responses against self and environmental antigens, and
some toxic substances (e.g., silica); underlies many
important diseases
• • Characterized by persistent inflammation, tissue injury,
attempted repair by scarring, and immune response
• • Cellular infiltrate consisting of activated macrophages,
lymphocytes, and plasma cells, often with prominent
fibrosis.
• • Mediated by cytokines produced by macrophages and
lymphocytes (notably T lymphocytes), with a tendency to
an amplified and prolonged inflammatory response
owing to bidirectional interactions between these cells
