
Dyspnea
Dr.Bilal
Natiq
N
u
aman
C.A.B.M.
, F.I.B.M.S. , D.I.M. ,
M.B.Ch.
B
.
Lec
t
urer
in I
r
aqia
Medic
a
l
College
201
5
-201
6
Dyspnea; Breathlessness; Shortness of
Breath(SOB)
•
‘’Dysp
n
ea’’
Dy
s
:
difficult,
painful
Pneume
a:
b
r
eath
• Breathlessness or dyspnea can be defined as the feeling
of an uncomfortable need to breathe.
DEFINITION
OF
DYSPNEA
•
Clinical
:
A subjective experience of breathing discomfort that
consists of (
q
u
a
l
it
a
ti
v
el
y
) distinct sensations that vary in
intensity.
•
Ph
y
siological:
The stimulation of pulmonary and extra
pulmonary afferent receptors and the transmission of afferent
information to the cerebral cortex, where the sensation is
perceived as uncomfortable or unpleasant
Patients
per
c
eption
s
:
ü Unsatisfied inspiration
ü Chest tightness
ü Sensation of feeling breathless
ü Cannot get enough air
ü Hunger for air
ü Incomplete exhalation
THE
PNEA’S
• DYSPNEA – SOB :
ACUTE – (PULMONARY EMBOLISM,
PNEUMOTHORAX, PULMONAR EDEMA)<30 days
CHRONIC – (COPD, CHF)>30 days
• TACHYPNEA – RR>20 BR/MIN(PNEUMONIA)
• BRADYPNEA - RR< 8 BR/MIN (DRUGS)
Pathophysiology
:
R
e
spiratory
disea
s
es
Ø
stimulating intrapulmonary sensory nerves
(e.g.
P
n
eumothora
x
,
i
n
ters
t
iti
a
l i
n
flammation
and pulmonary
embo
l
us)
Ø
increasing the mechanical load on the respiratory muscles
(e.g.
airflow
obstruction
or
p
ulmon
a
ry
fibrosis)
Ø
Causing hypoxia, hypercapnia or acidosis, stimulating
can stimulate breathing and dyspnea by:
i
n
ters
t
iti
a
l i
n
flamm
airflow
obst
r
uction
chemoreceptors.
Com
m
on
Pu
l
m
o
n
a
ry C
a
uses
• Obstructive lung disease
• Asthma/COPD (Chronic Bronchitis ,Emphysema)
• Pneumonia
• Pulmonary embolism
• Pneumothorax
c
a
rdiac
f
a
ilure
can stimulate breathing and dyspnea by:
Ø pulmonary congestion reduces lung compliance and can
also obstruct the small airways.
Ø In addition, during exercise, reduced cardiac output
limits oxygen supply to the skeletal muscles, causing
early lactic acidaemia and further stimulating breathing
via the central chemoreceptors.
Com
m
on
Card
i
ac Causes
• Acute coronary syndromes
• CHF
• Dysrhythmias
• Valvular heart disease
St
a
g
e
s
of Car
d
i
a
c dysp
n
ea
1-EXERTIONAL DYSPNEA- DYSPNEA DUE TO
EXERCISE
2-ORTHOPNEA – SOB LYING FLAT AND BETTER
SITTING UP (CHF, pregnancy, resp.muscle weakness)
3-PND -
P
AROXYSMAL
N
OCTURNAL
D
YSPNEA
characterized by acute shortness of breath almost always
accompanied by coughing and wheezing. This respiratory
distress usually occurs when a person is already sleep in
a reclining position (HEART FAILURE-early night ,
ASTHMA-late night )
4-RESTING DYSPNEA- DYSPNEA AT REST

Com
m
on
Miscell
a
n
e
o
u
s C
a
uses
• Metabolic acidosis
• Severe anemia
• Pregnancy
• Hyperthyroidsm
• Hyperventilation syndrome
CHARACTERISTICS
OF
HISTORY
•
Per
s
i
s
te
n
ce
a
n
d
v
a
ri
a
b
i
li
t
y
•
Intermittent
•
Persistent
•
Nocturnal
•
Seasonal
•
Occupational
( work,home ...etc.)
History
Taki
n
g
nature
of onset (acute, chronic) ,
duration
,
evolution
over time
associated symptoms
(cough, sputum ,wheeze, )
physiologic vs. pathologic
•
E
x
posures
• Sick contacts
• Tobacco
• Occupational
• Hobbies
• Pets
• Drugs
• Radiation
Differ
e
ntial
diag
n
osis
of
dyspnea
Patients with breathlessness present either with
Chron
i
c
e
x
erti
o
n
a
l
d
y
s
p
n
e
a
Or
Acute
dy
s
pne
a
,
when symptoms are prominent even at rest.
ACUTE
VE CHRONIC
DYSPNEA
•
Acute:
Dy
s
p
n
ea
(AP4)
<30 days
that
develops
over
hours or days :
•
A
sthma (exacerbation)
•
P
ulmonary
edema
•
P
neumothorax
•
P
ulmonary
embolism
•
P
neumonia
•
•
Chro
n
ic:
Dy
s
p
n
ea
>3
0 d
a
ys
that
develops
over
weeks, months or years.
•
C
OPD
•
L
eft ventricular
failure
•
L
ung fibrosis
•
A
sthma (uncontrolled)
•
P
leural
effusion

• How is your breathing at rest and overnight?
In
COPD, there is a fixed, structural limit to maximum ven@la@on,
and a tendency for progressive hyperinfla8on during exercise.
Breathlessness is mainly apparent when walking, and pa8ents
usually report minimal symptoms at rest and overnight.
In contrast, pa8ents with significant
asthma are oAen woken
from their sleep by breathlessness with chest 8ghtness and
wheeze,(PND).
Chro
n
ic
exert
i
o
n
al
br
e
at
h
lessness
The
cause of breathlessness
is
often
apparent
from
a
careful
K
e
y qu
e
stions
i
n
cl
u
de:
clinical history.

Orthopnoea, however, is common in
COPD, as well as in heart disease,
because airflow obstruction is made
worse by cranial displacement of the
diaphragm by the abdominal contents
when recumbent, so many patients
choose to sleep propped up.
How
much
c
a
n
y
ou
do
on
a
good
da
y
?
Noting ‘breathless on exertion’ is not enough; the
approximate distance the patient can walk on the level
should be documented, along with capacity to climb
inclines or stairs.
Variability within and between days is a hallmark of
a
s
thm
a
; in mild asthma, the patient may be free of
symptoms and signs when well.
Gradual, progressive loss of exercise capacity over months
and years, is typical of
CO
P
D
.

Relentless, progressive breathlessness that is also present
at rest, often accompanied by a dry cough, suggests
intersti
t
ial
lung
fibrosi
s
.
Hea
r
t
failure
can also cause chronic exertional
breathlessness, cough and wheeze.
A history of angina, hypertension or myocardial infarction
raises the possibility of a cardiac cause.
Did
y
ou
have
brea
t
hi
n
g
pro
b
lems
in
child
h
o
o
d
or
at
s
c
h
o
ol?
When present, a history of childhood wheeze increases the
likelihood of
a
s
thm
a
, although this history may be
absent in late-onset asthma.
A history of atopic allergy also increases the likelihood of
a
s
thma.
• Psychogenic breathlessness rarely disturbs sleep,
frequently occurs at rest, may be provoked by stressful
situations and may even be relieved by exercise.
•
The Nijmegen
questionnaire
can be used to score some
of the typical symptoms of hyperventilation.
Acute
s
e
v
e
re
bre
a
thle
s
sn
e
ss
• This is one of the most common and dramatic medical
emergencies. The history and a rapid but careful
examination will usually suggest a diagnosis which can
be confirmed by routine investigations, including chest X-
ray, ECG and arterial blood gases.
Hist
o
ry
It is important to establish the rate of onset and severity of
the breathlessness and whether associated
cardiovascular symptoms (chest pain, palpitations,
sweating and nausea)
or respiratory symptoms (cough, wheeze, haemoptysis,
stridor) are present.
A previous history of repeated episodes of left ventricular
failure, asthma or exacerbations of COPD is valuable.
In children, the possibility of inhalation of
a
f
o
r
e
i
gn
b
o
dy
or
ac
u
te
epi
g
lo
t
tit
i
s
should always be considered.
The following should be assessed and documented:
Clin
i
cal
assess
m
ent
1- level of consciousness
2-degree of central cyanosis
3-evidence of anaphylaxis (urticaria or angioedema)
4-patency of the upper airway
5-ability to speak (in single words or sentences)
6-cardiovascular status (heart rate and rhythm, blood pressure
and degree of peripheral perfusion).
P
u
lmonary
oedema
is suggested by pink, frothy sputum and
a
s
thma
or
CO
P
D
by wheeze and prolonged expiration;
p
n
eumoth
o
rax
by a silent resonant hemithorax; and
p
u
lmona
r
y
embolus
by severe breathlessness with normal
Leg swelling may suggest
c
a
rdiac
f
a
ilure
or, if asymmetrical,
veno
u
s throm
b
osis
causing
p
u
lmo
n
a
r
y
emb
o
lis
m
.
Urgent endotracheal intubation may become necessary if the
bi-basal crackles;
breath sounds.
Arterial blood gases, a chest X-ray and an ECG should be
obtained to confirm the clinical diagnosis, and high
concentrations of oxygen given pending results.
conscious level declines or if severe respiratory acidosis is
present.

Physical
signs
in dyspnic
p
a
ti
e
nt
Investigations
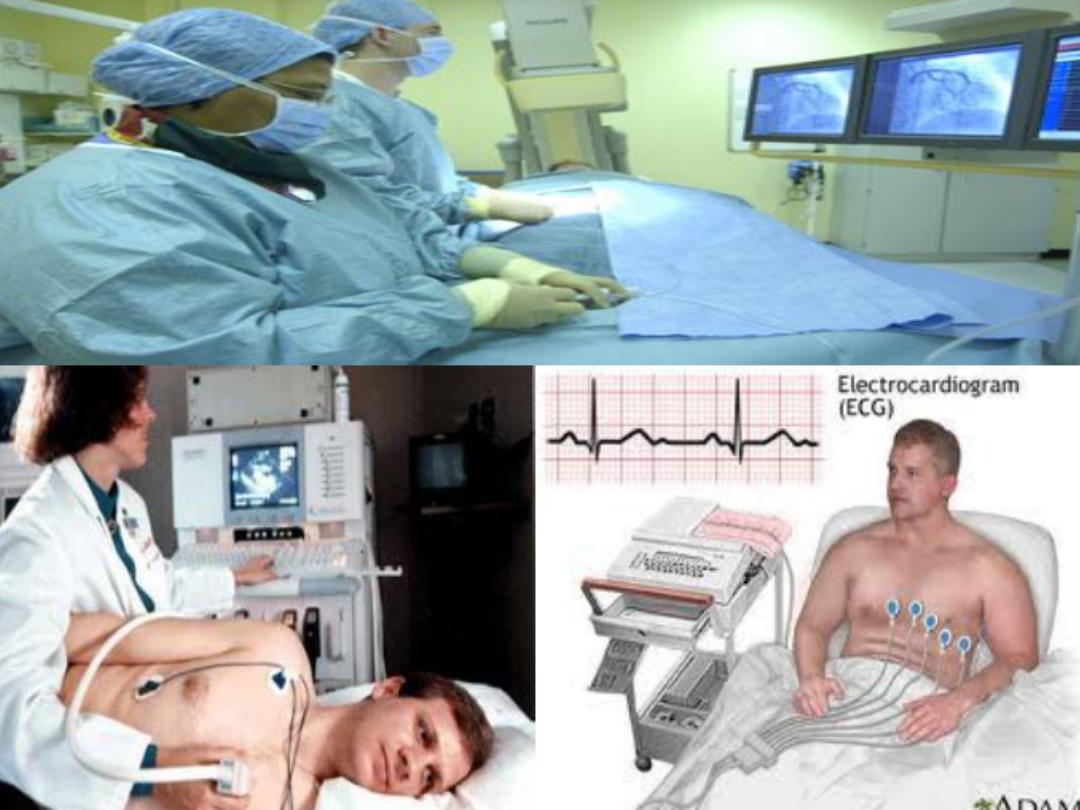
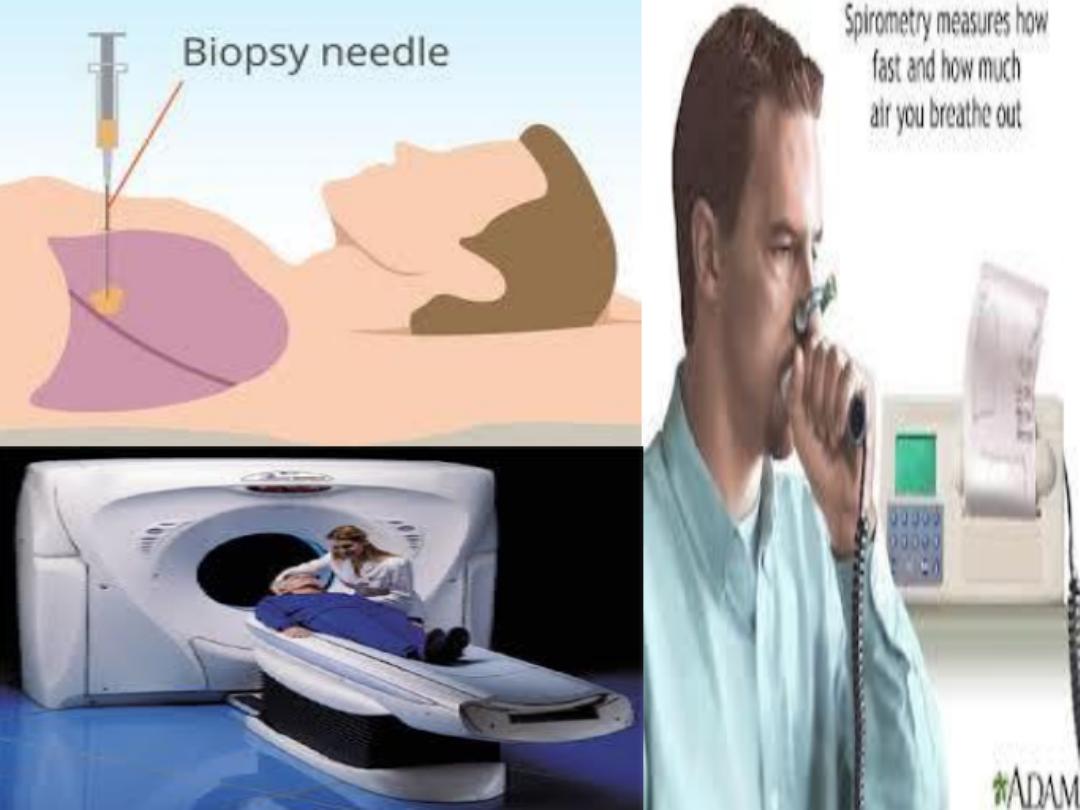
Chest radiograph (CXR): weather cardiac or pulmonary
Cardiac Causes! Pulmonary causes!
ECG Pulmonary function test(PFT)
(abnormally significant) (abnormally significant)
Echo CT scan of chest
(abnormally significant) (abnormally significant)
Coronary angiography Lung Biopsy
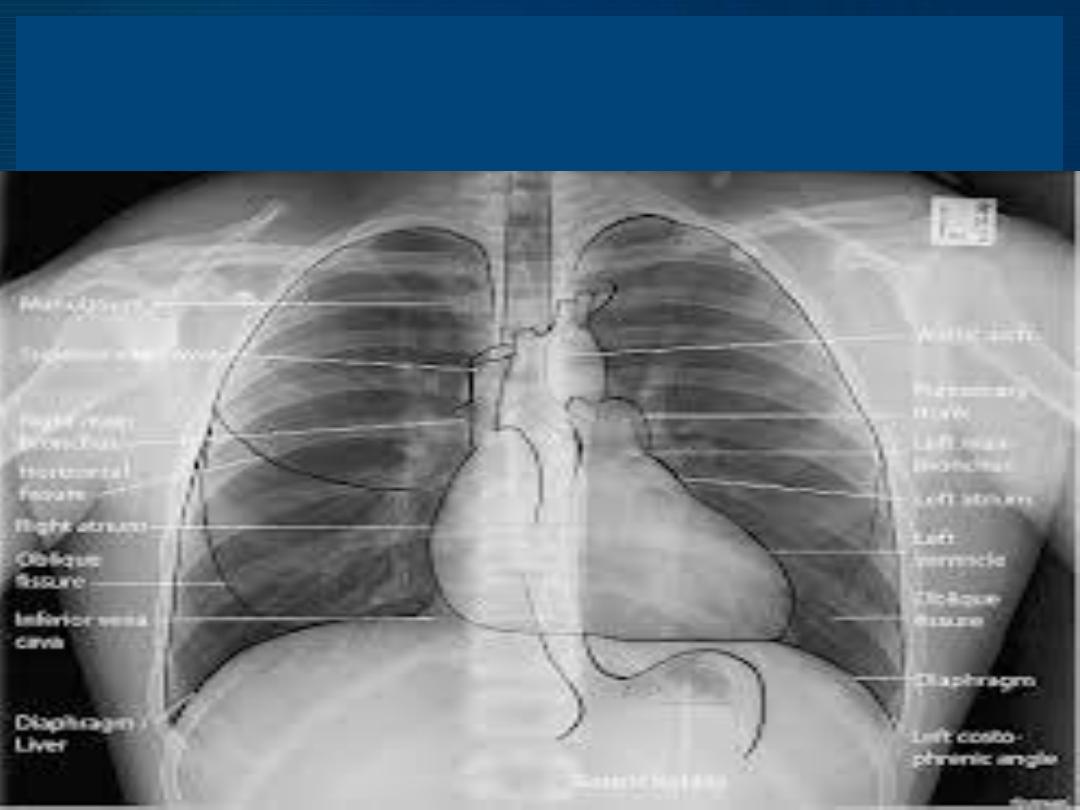
CXR

Tre
a
tm
e
nt
In an acutely dyspneic pa@ent it is important
to ensure that the Airway, Breathing,
Circula@on (ABC) are aIended to before
con@nuing with the diagnos@c process.
Ø
Non-Drug Treatments
• Positioning - sitting up
•Relaxation
• Humidified air
Ø
Oxygen

