
Malaria
Malaria is caused by Plasmodium falciparum, P. vivax, P. ovale, P. malariae.
It is transmitted by the bite of female anopheline mosquitoes and occurs
throughout the tropics and subtropics at altitudes below 1500 metres.
P. falciparum has now become resistant to chloroquine especially in Asia
and Africa.
Pathogenesis
Life cycle
The female anopheline mosquito becomes infected when it feeds on human
blood containing gametocytes, the sexual forms of malaria develop in the
mosquito, takes from 7 to 20 days, in which sporozoites invade (accumulate
in) the salivary glands of mosquito.
When mosquito bite human, the sporozoites inoculated into the human
blood stream. Sporozoites disappear from human blood within half an hour
(
1
/
2
hr) and enter the liver.
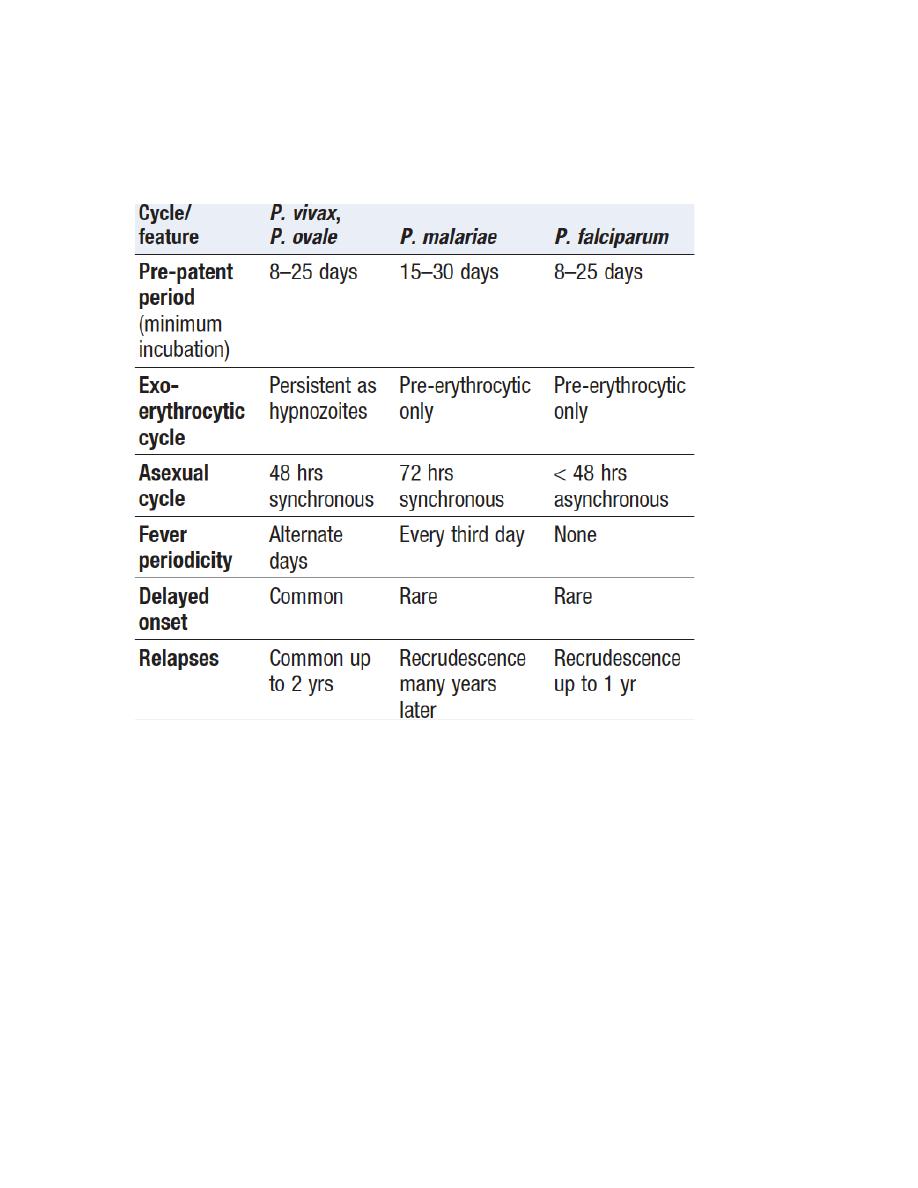
After some days, merozoites leave the liver and invade red blood cells,
where further asexual cycles of multiplication take place, producing
schizonts. Rupture of the schizont releases more merozoites into the blood
and causes fever, the periodicity of which depends on the species
of parasite.
P. vivax and P. ovale may persist in the liver, capable of developing into
merozoites months or years later. The disease may relapse after treatment
with drugs that kill only the erythrocytic stage.
P. falciparum and P. malariae have no persistent exoerythrocytic phase but
recrudescence of fever may result from multiplication of parasites in red
cells which have not been eliminated by treatment and immune processes.
Pathology
The pathology in malaria is due to hemolysis of infected red cells and
adherence of red blood cells to the capillaries.
Malaria is always accompanied by hemolysis.
Hemolysis is most severe with P. falciparum, which invades red
cells of all ages while P. vivax and P. ovale invade reticulocytes, and P.
malariae invades normoblasts, so anaemia remain mild
Effects on red blood cells and capillaries:
In P. falciparum, red cells containing schizont adhere to vascular
endothelium in postcapillary venules in brain, kidney, liver, lungs and
Gut, The vessels become congested and the organ anoxic, rupture of
schizonts, liberate toxic and antigenic substances which cause further
damage, so the main effect of malaria is hemolytic anaemia, while in p.
falciparum widespread organ damage and anaemia
P. falciparum does not grow in red cells that contain haemoglobin F, C or S.
P. vivax cannot enter red cells that lack the Duffy blood group.
Clinical features
P. falciparum
This is the most dangerous of the malarias. The onset is insidious, with
malaise, headache and vomiting and often mistaken for influenza.
The fever has no particular pattern. Jaundice is common due to haemolysis
and hepatic dysfunction. The liver and spleen enlarge and may become
tender. Anaemia develops rapidly.
Patients may develop serious complications:
- cerebral malaria
- hyperpyrexia
- convulsions
- acute renal failure
- acute pulmonary oedema
- severe anaemia

- aspirate pneumonia
- hypoglycemia
abortion in pregnancy or intrauterine growth retardation
children may die rapidly
P. vivax and P. ovale
The illness starts with several days of continued fever before the
development of classical bouts of fever on alternate days. Fever starts with a
rigor, The patient feels cold and the temperature rises to about 40°C. After
half an hour to an hour, the hot or flush phase begins. It lasts several hours
and associated with profuse sweating and a gradual fall in temperature. The
cycle is repeated 48 hours later, Gradually, the spleen and liver enlarge and
may become tender. Anaemia develops slowly and herpes simplex is
common, Relapses are common in the first 2 years after leaving (up to two
years of leaving) the endemic area.
P. malariae
This is usually associated with mild symptoms and bouts of fever every third
day. Parasitaemia may persist for many years, with the occasional
recrudescence of fever or without producing any symptoms. Chronic P.
malariae infection causes glomerulonephritis and longterm nephrotic
syndrome in children.
Diagnosis
Thick and thin blood films should be examined, Thick blood film contains
more blood to facilitate the diagnosis (and
erythrocytes are lysed, releasing
all blood stages of
the parasite) while thin blood film is used to confirm the
diagnosis and identify the species.
P. falciparum, only ring forms are found in the early stages, while other
species, all stages of the erythrocytic cycle may be found.
Immunochromatographic tests for p. falciparum antigen are now present,
ParasightF® and OptiMal® test (which detects the Plasmodium lactate
dehydrogenase of several species).
which are sensitive and specific for p. falciparum but not for others, They
should be used in parallel with blood film.
PCR for DNA detection is used mainly in research and is useful for
determining whether a patient has a recurrent infection (with the same
malaria) or a re-infection with a new parasite.
Management
P. falciparum is now resistant to chloroquine and sulfadoxine-
pyrimethamine (Fansidar) almost worldwide, an artemisinin-based treatment
is recommended. Co-artemether (CoArtem® or Riamet®) contains

artemether and lumefantrine and is given as 4 tablets at 0, 8, 24, 36, 48 and
60 hours. Alternatives are quinine by mouth (600 mg of quinine salt 3 times
daily for 5–7 days), together with or followed by either doxycycline (200 mg
once daily for 7 days) or clindamycin (450 mg 3 times daily for 7 days) or
atovaquoneproguanil (Malarone®, 4 tablets once daily for 3 days).
Doxycycline should not be used in pregnancy and artemether should be
avoided in early pregnancy. WHO policy in Africa is moving towards
always using artemisinin-based combination therapy (ACT), e.g. co-
artemether or artesunate-amodiaquine. In India and other areas, artesunate
(200 mg orally daily for 3 days) and mefloquine (1 g orally on day 2 and 500
mg orally on day 3) may be used. Unfortunately, artemisinin resistance has
now been reported in Cambodia.
Management of Complicated P. falciparum
Cerebral malaria is the most common cause of death
In adults the complications include: severe anaemia, hypoglycemia, renal
failure and metabolic acidosis
So treatment include early chemotherapy, correction of fluid and electrolyte
balance.
Artesunate given as 2.4 mg/kg IV at 0, 12 and 24 hours and then once daily
for 7 days. However, as soon as the patient has recovered sufficiently to
swallow tablets, oral artesunate 2 mg/kg once daily is given instead of
intravenous therapy, to complete a total cumulative dose of 17– 18 mg/kg.
Rectal administration of artesunate is also available.
Quinine is given I.V loading dose infusion of 20 mg/kg over 4 hours, up to
a maximum of 1.4 g. Followed by maintenance doses of 10 mg/kg as 4-hour
infusions 2–3 times daily, up to a maximum of 700 mg per dose until the
patient can take drugs orally.
(ECG monitoring of the heart for side effects of Quinine)
Management of P. vivax, P. ovale and P. malariae
infections:
Treatment with chloroquine: 600 mg, followed by 300 mg in 6 hours, then
150 mg twice daily (every 12 hours) for 2 more days.
relapses can be prevented (p. vivax, P. ovale) by eradicating the hepatic
phase using primaquine (15 mg daily for 14 days).
Haemolysis may develop in those with G6PD-deficient. Cyanosis due to the
formation of methaemoglobin in the red cells is more common but not
dangerous.
Prevention
Any person who is going to an endemic area should avoid bites and take
chemoprophylaxis.
Avoiding bites by using long sleeve and trousers, repellent cream, screened
windows and mosquito nets.
Chemoprophylaxis:
Is begun before travelling to an endemic area and continued for 4 weeks
after leaving the area, pregnant and lactating woman can take proguanil or
chloroquine safely.
Mefloquine is useful in areas with multiple drug resistance.
Chloroquine resistance high
- Mefloquine
250 mg weekly Started 2–3 wks before travel and continued
until 4 wks after
- Doxycycline
100 mg daily Started 1 wk before and continued until 4 wks
after travel
- Malarone
1 tablet daily From 1–2 days before travel until 1 wk after return
Chloroquine resistance absent
Chloroquine
and
300 mg base weekly
Proguanil 100–200 mg daily Started 1 wk
before and continued until 4 wks after travel
Giardiasis
Infection with Giardia Intestinalis also known as Giardia Lamblia is found
worldwide and is common in the tropics. It particularly affects children,
travellers and immunosuppressed individuals.
The cyst remains viable in water for up to 3 months and infection usually
occurs by ingesting contaminated water, the parasite attach to the duodenal
and jejunal mucosa, causing inflammation.
Clinical features
After an incubation period of 1–3 weeks, there is diarrhoea, abdominal pain,
weakness, anorexia, nausea and vomiting. On examination, there may be
abdominal distension and tenderness. Stools obtained at 2–3-day intervals
should be examined for cysts. Duodenal or jejunal (fluid) aspiration by
endoscopy gives a higher diagnostic yield.
Management
Treatment is with a single dose of tinidazole 2 g
Metronidazole 400 mg 3 times daily for 10 days, or 2 g once daily for 3 days
Nitazoxanide 500 mg orally twice daily for 3 days.
