
Chapter 16
Urogenital
System

Ch.16 – Part 1
Outline:
Origin of urinary system
The role of pronephros, mesonephros, and metanephros in development of
the urinary system.
The derivatives of the ureteric bud and the metanephric mesoderm.
Epithelial mesenchymal interactions in kidney developments.
The embryologic origin of congenital cystic kidney, double ureter, horseshoe
and pelvic kidneys.
The formation of the urinary bladder and the urogenital sinus.
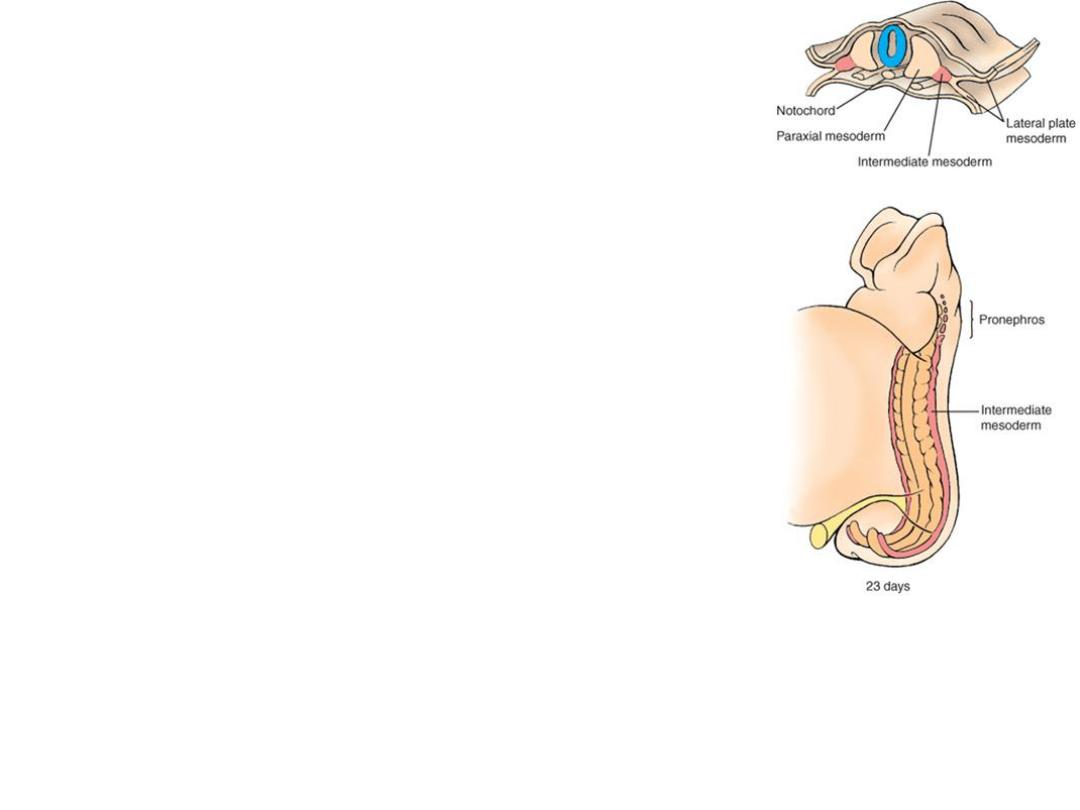
Origin
•Urogenital system =
Urinary system & Genital system
•Both systems arise from:
Intermediate Mesoderm
Urinary system
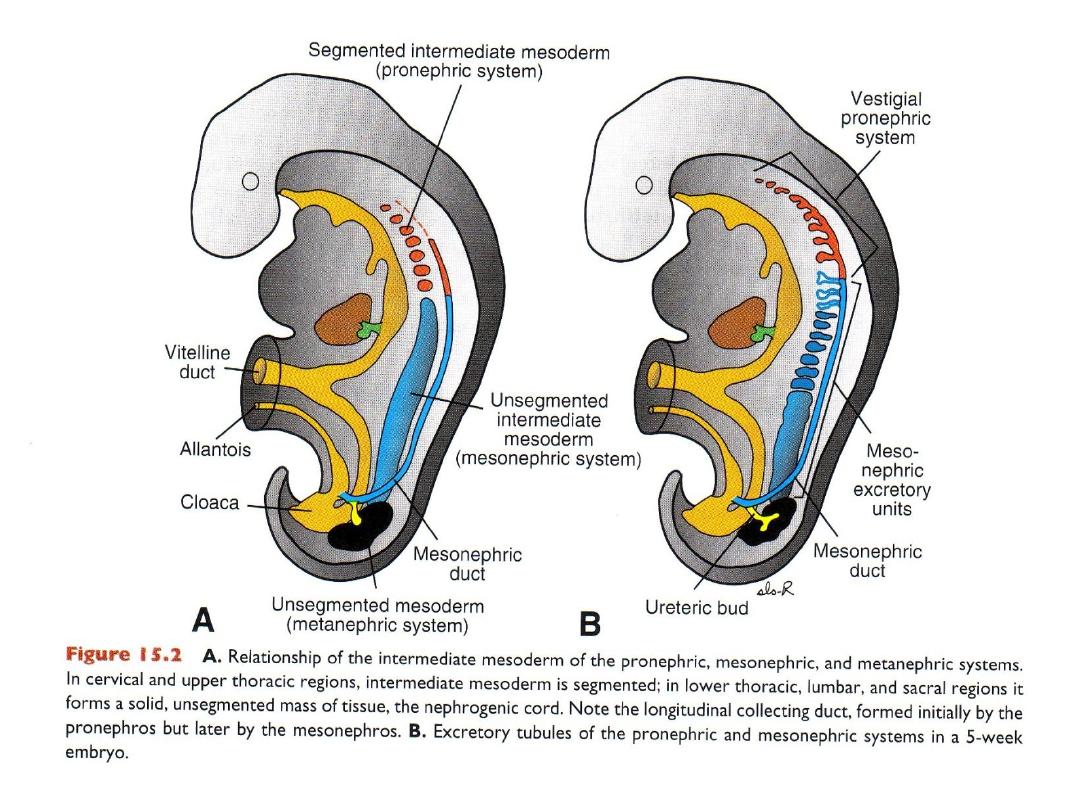
• Three kidneys in succession:
• Pronephros = cervical = nonfunctional.
• Mesonephros = thoracolumbar: duct = mesonephric duct.
• Metanephros = definitive kidney.
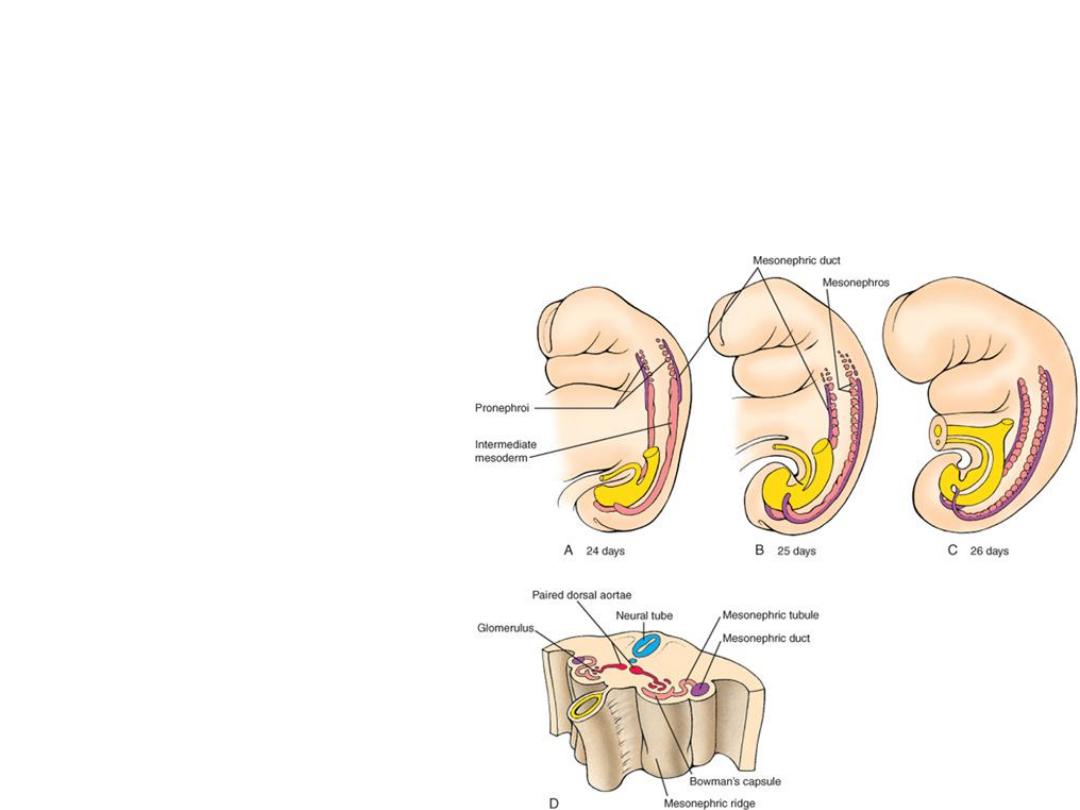
Pronephros
• In cervical region,
• Nonfunctional.
• In 4
th
week
• Nephrotomes=
excretory units,
• Disappear
Mesonephros
•Forms in thoracolumbar region
•During 5
th
week
•Form nephrons (disappear)
and open into
mesonephric
duct (wolffian duct).
•Mesonephric duct: remain in
male, disappear in female
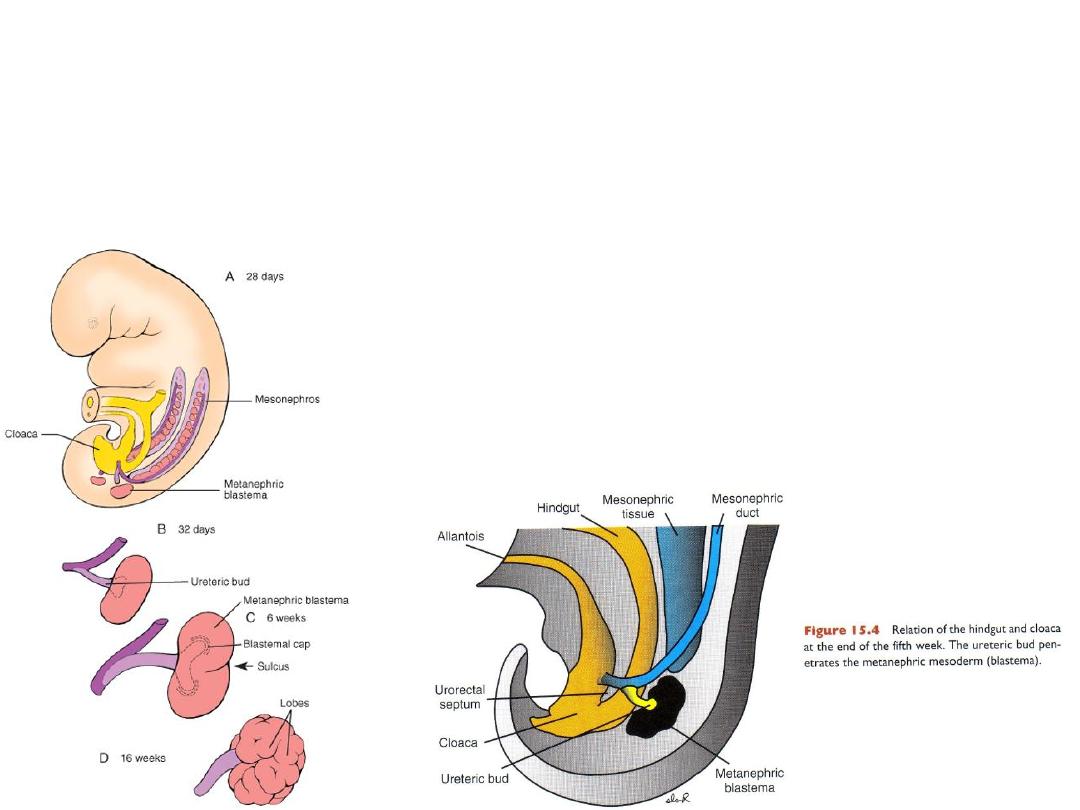
Metanephros: The Definitive Kidney
•Permanent kidney.
•During 5
th
week
•Forms from: 1- ureteric bud collecting system
2- metanephric mesoderm excretory units
Collecting system
• Ureteric bud originates from
mesonephric duct
• Ureteric bud Collecting system
• Ureteric bud: grows into and
induces metanephric mesoderm
(blastema).
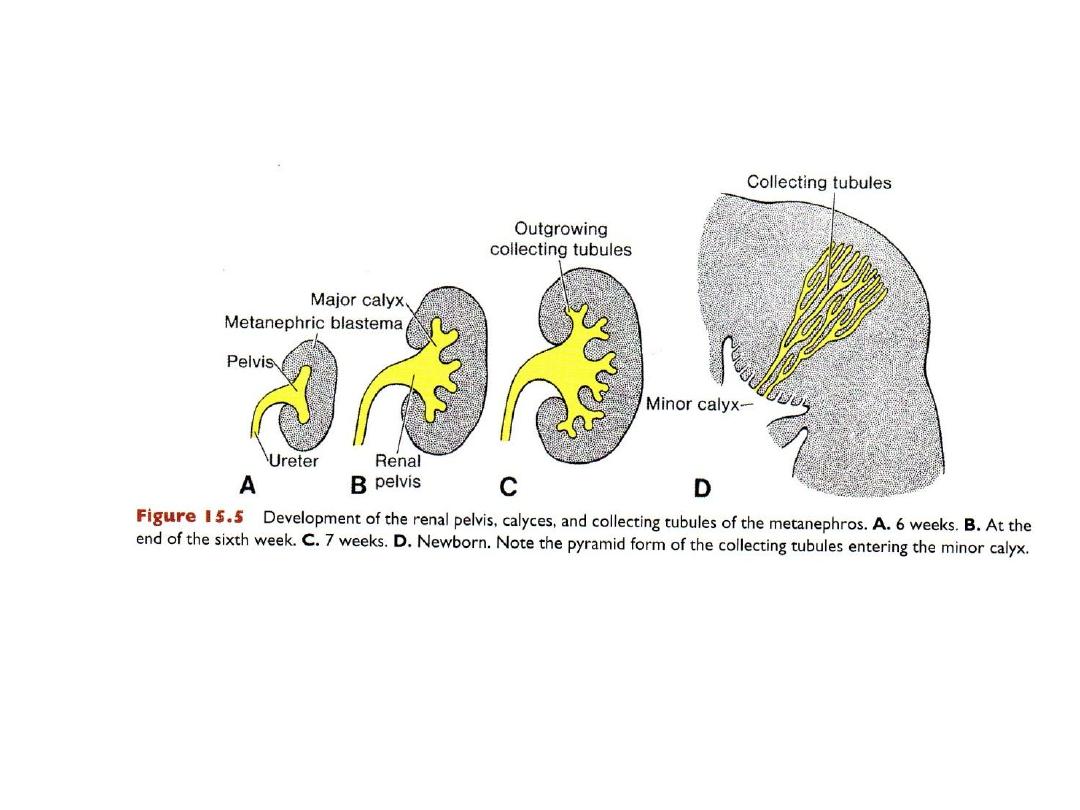
Ureteric bud continues to divide to form: ureter, renal pelvis,
major and minor calyces, collecting tubules.
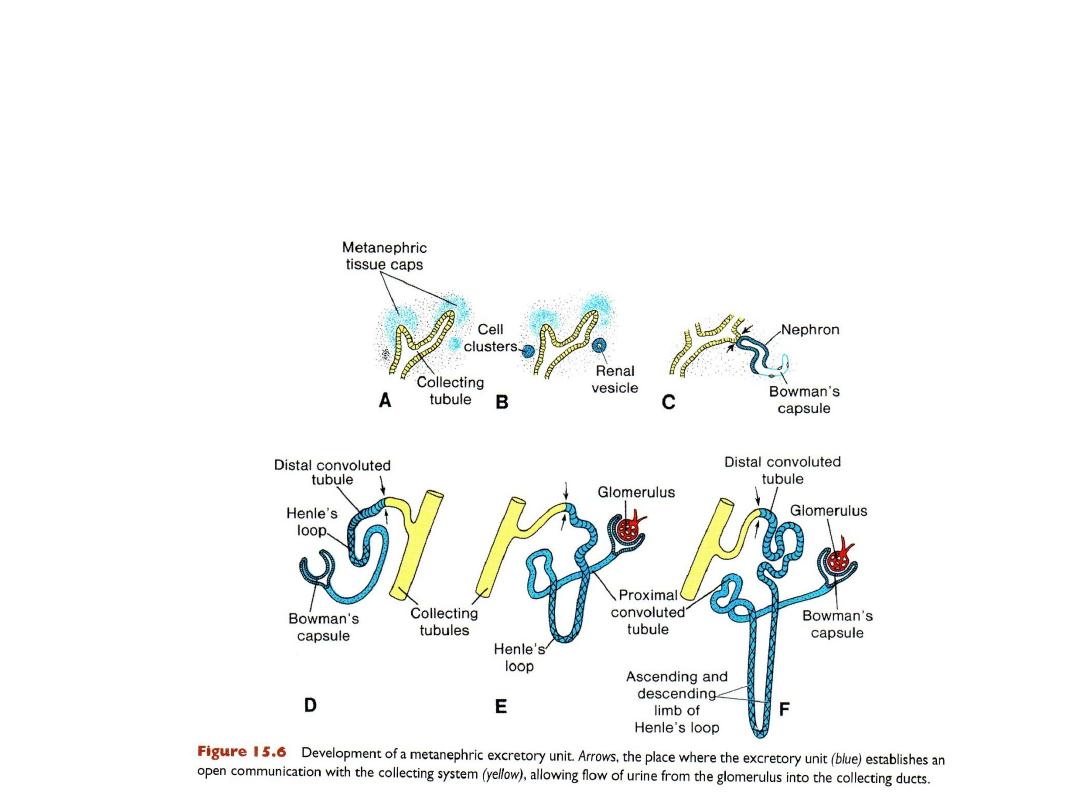
Excretory system
• Metanephric mesoderm (blastema) induced by ureteric bud forms
filtration system = glomerulus, Bowman's capsule, proximal convoluted
tubule, loop of Henle, and distal convoluted tubule.
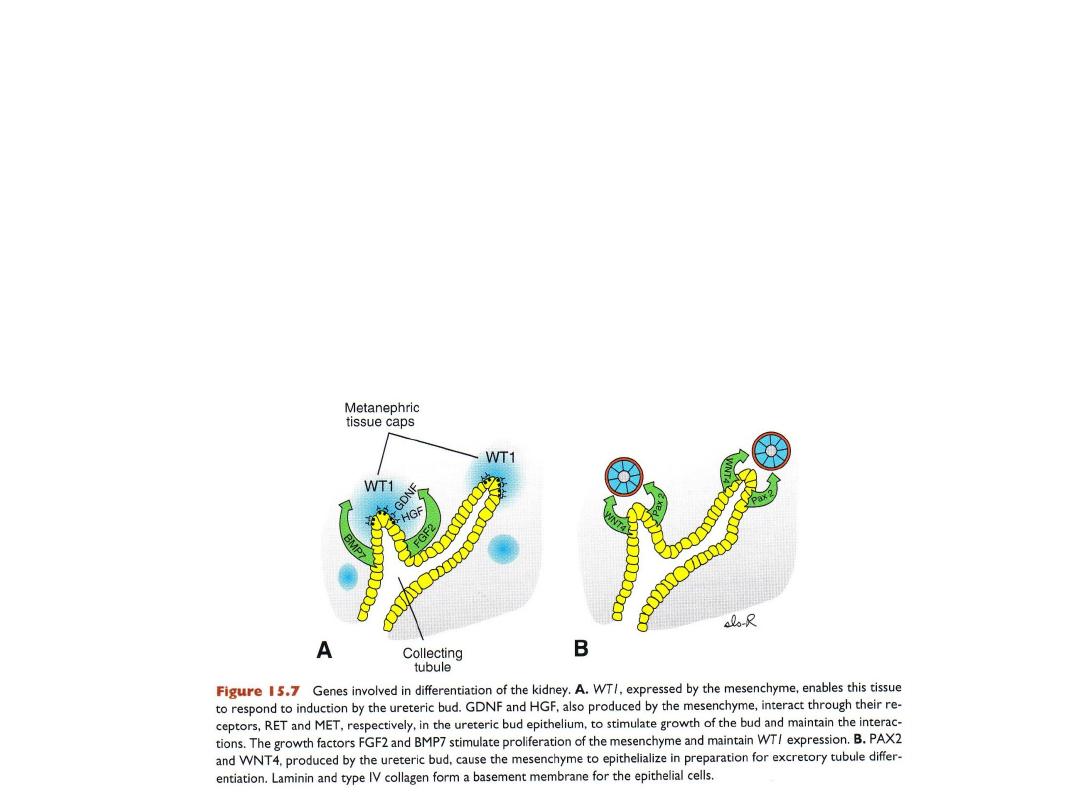
Molecular regulation of kidney development
• WT 1 gene = kidney gene = allows mesoderm to be induced by ureteric
buds.
• Kidney development is dependent upon epithelial-mesenchymal
interactions.
• Epithelium of ureteric bud
• Mesenchyme of metanephric blastema (mesoderm)
RENAL TUMORS & DEFECTS
• Wilms’ tumor:
• Cancer of the kidneys affecting children
• Due to mutations in WT1 gene
• Congenital polycystic kidney = proximal convoluted tubules do not form properly.
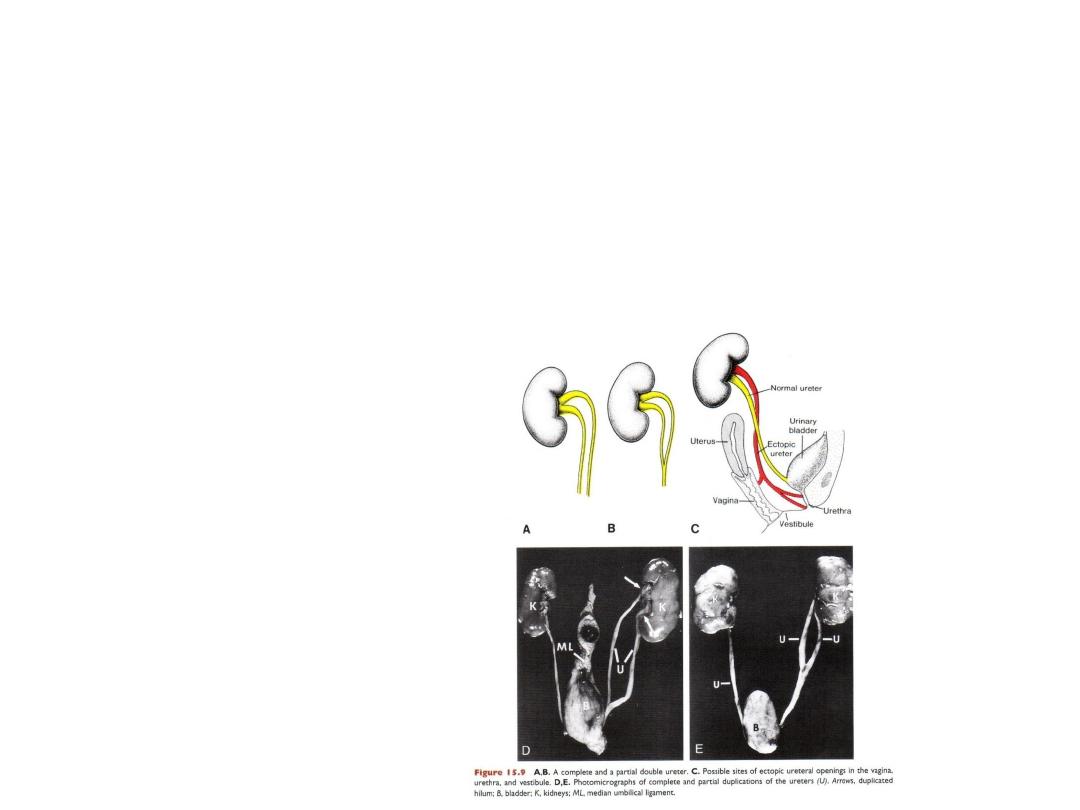
Duplication of ureter
• Early division of the
ureteric bud
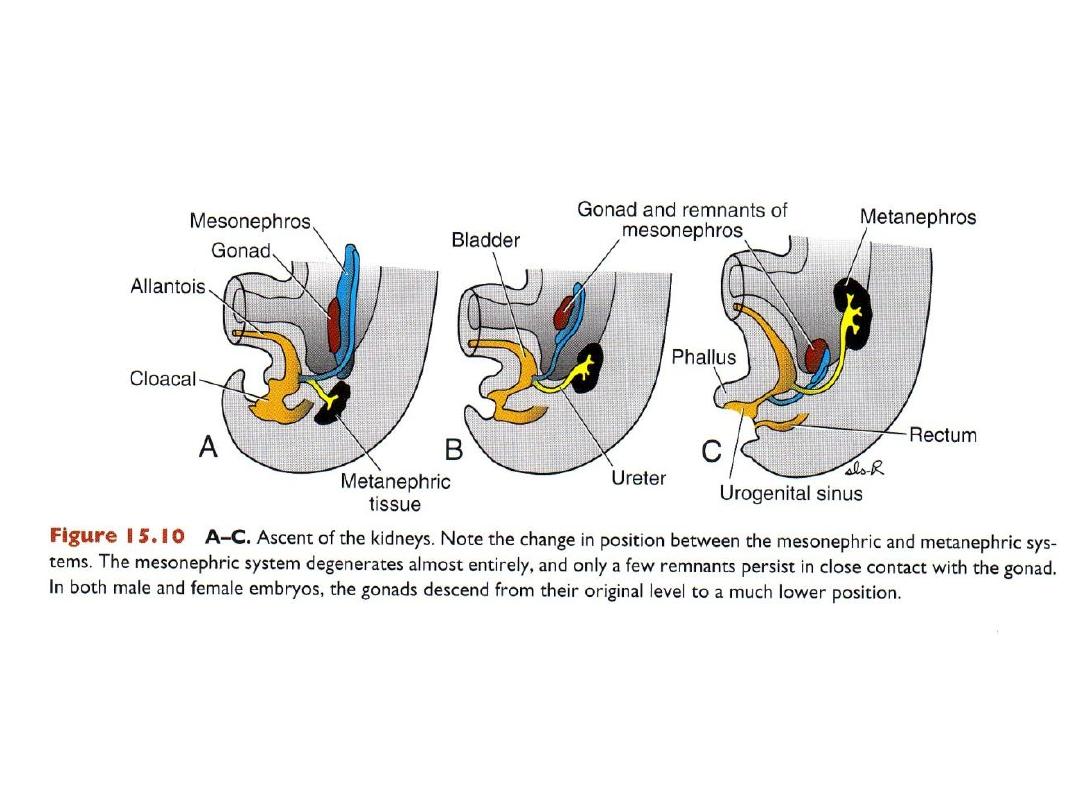
ASCENT OF THE KIDNEY
Kidneys form in pelvis. Differential growth moves them into lumbar
region.
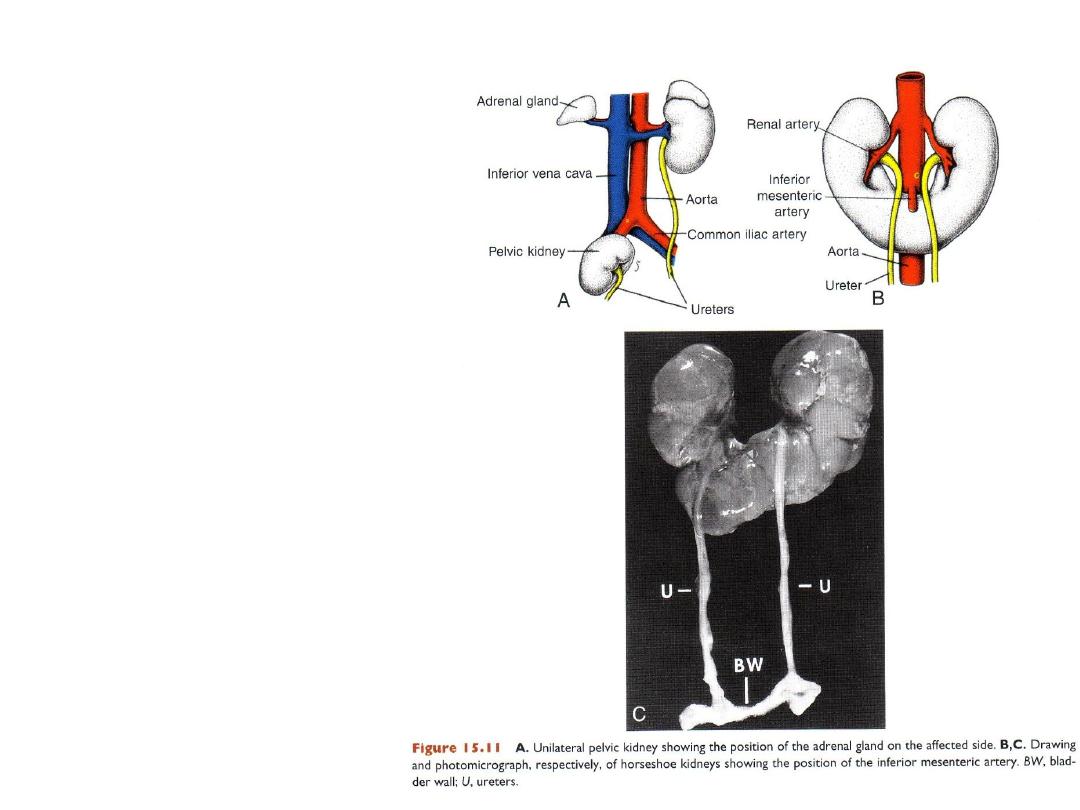
Abnormal location of
the kidneys
• Pelvic kidney.
• If kidneys fuse = horseshoe
kidney = gets stuck on inf
mesenteric a.
FUNCTION OF THE KIDNEY
• PERMANENT KIDNEY:
– FUNCTIONAL NEAR 12
th
wk
– Urine amniotic cavity
– Urine: not for waste products
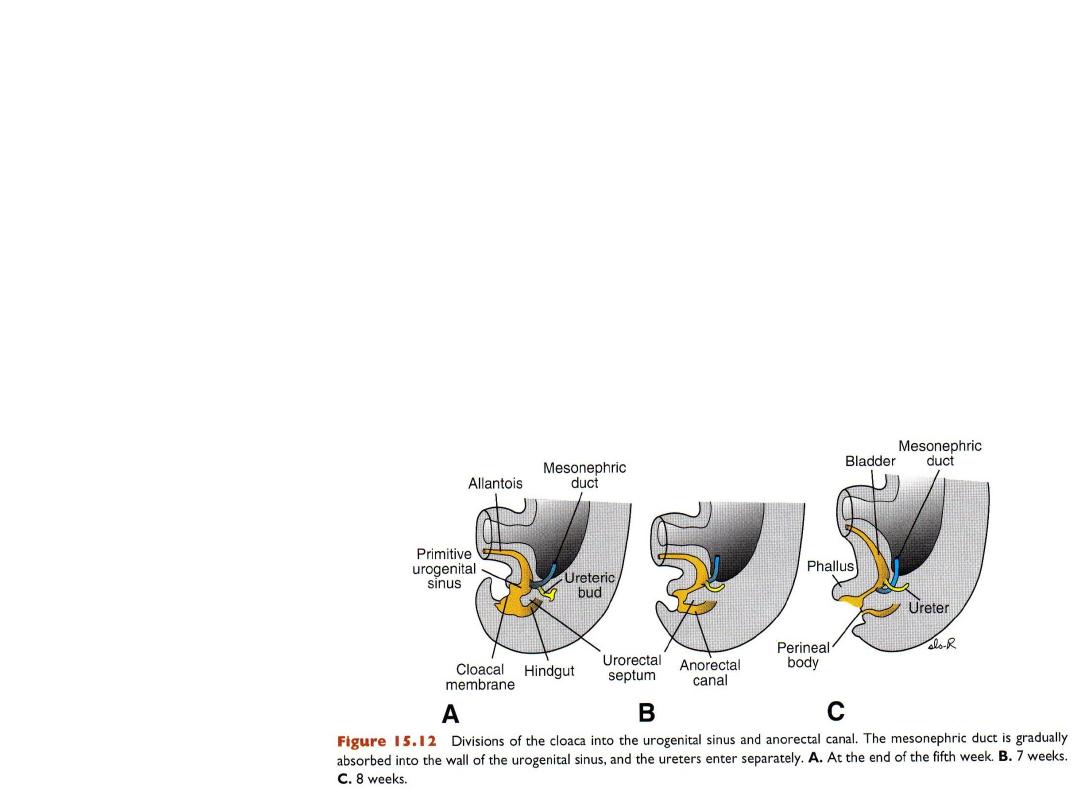
BLADDER & URETHRA
Division of cloaca
Urorectal septum:
separates hindgut
from cloaca
Cloaca: forms
primitive urogenital
sinus
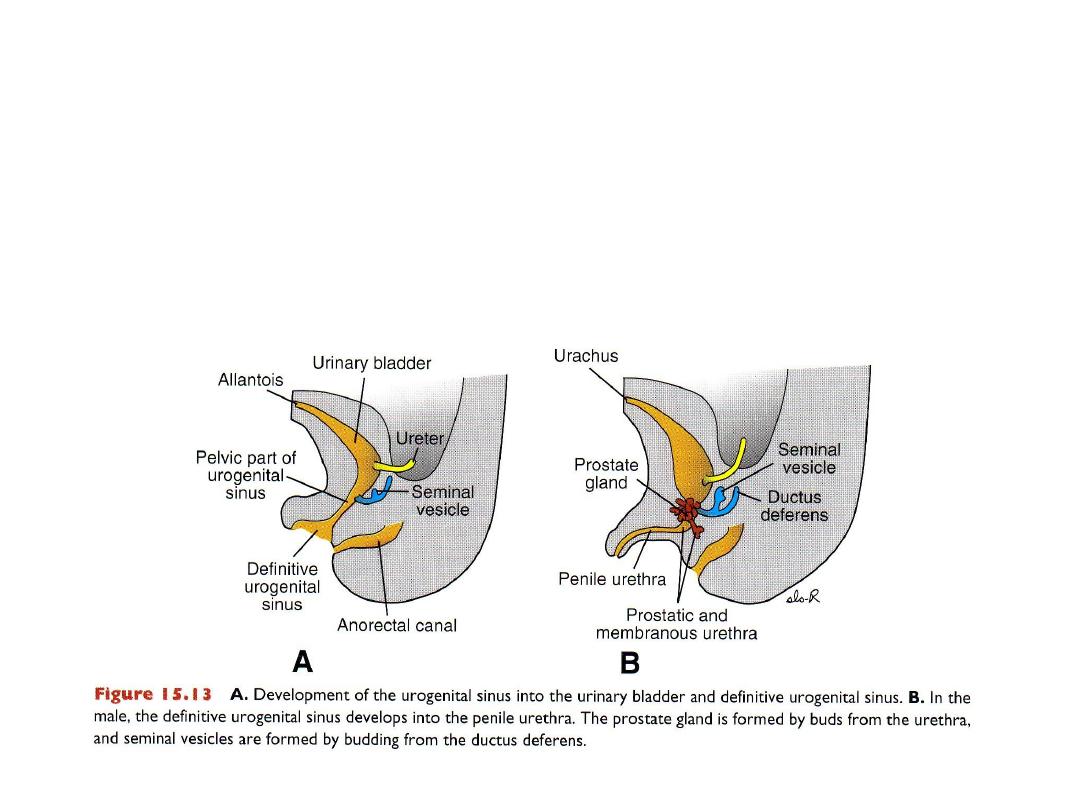
PARTS OF THE UROGENITAL SINUS
Bladder forms from upper part of urogenital sinus, expands and
incorporates ureters;
Mesopheric ducts move lower to enter urethra where prostate forms.
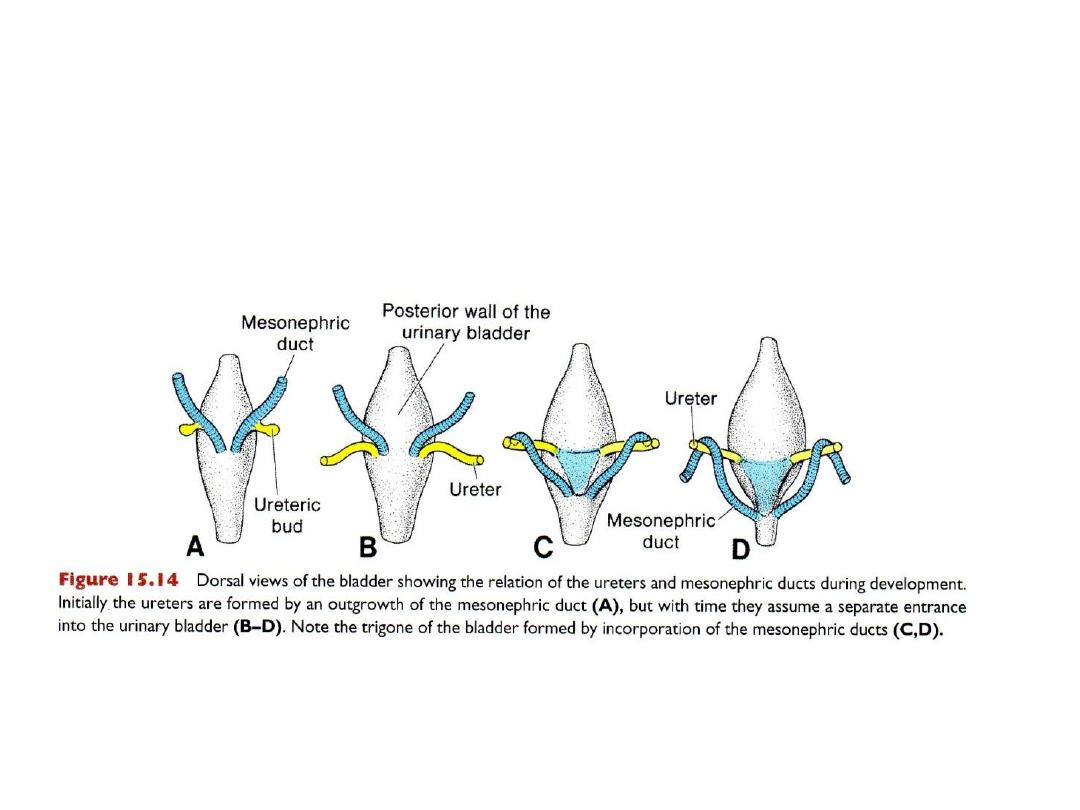
Development of ureters & mesonephric ducts
& formation of the trigone of ur bladder
Part of mesonephric ducts (MESODERM) incorporated into bladder
(ENDODERM) forms trigone area of bladder.
• Bladder connected to umbilicus by urachus (old allantois) median umbilical
ligament.
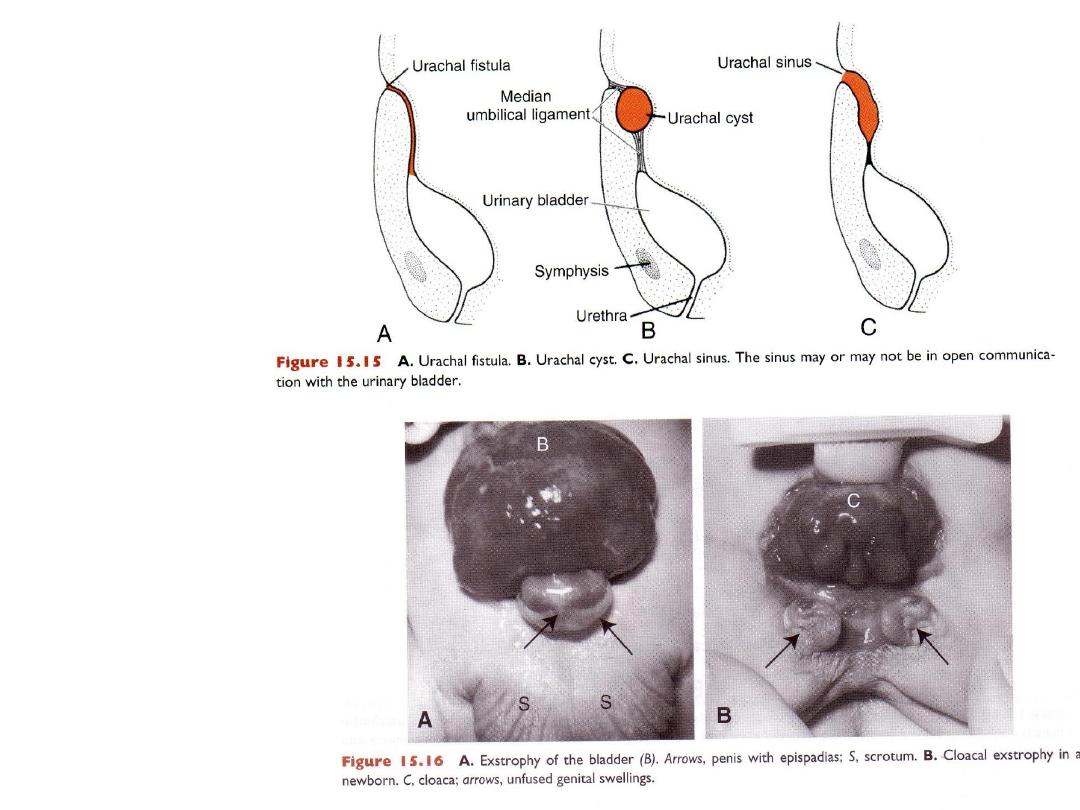
BLADDER
DEFECTS
EXTROPHY OF THE
BLADDER
EXTROPHY OF CLOACA

Ch. 16 – Part 2
Genital system

• Outline:
• The Y chromosome
• The genital ridge
• The indifferent gonads
• Migration of the primordial germ cells
• Development of ovary & testis
• Development of the mesonephric and paramesonephric duct
systems and their derivatives in the male and female.
• The formation of the vagina.
• The fate of the genital tubercle, urethral folds, and genital swellings
in the male and female.
• Defects in sex differentiation
• Descent of the testes from the abdominal cavity into the scrotum
• Congenital inguinal hernia.
• Clinical correlates.
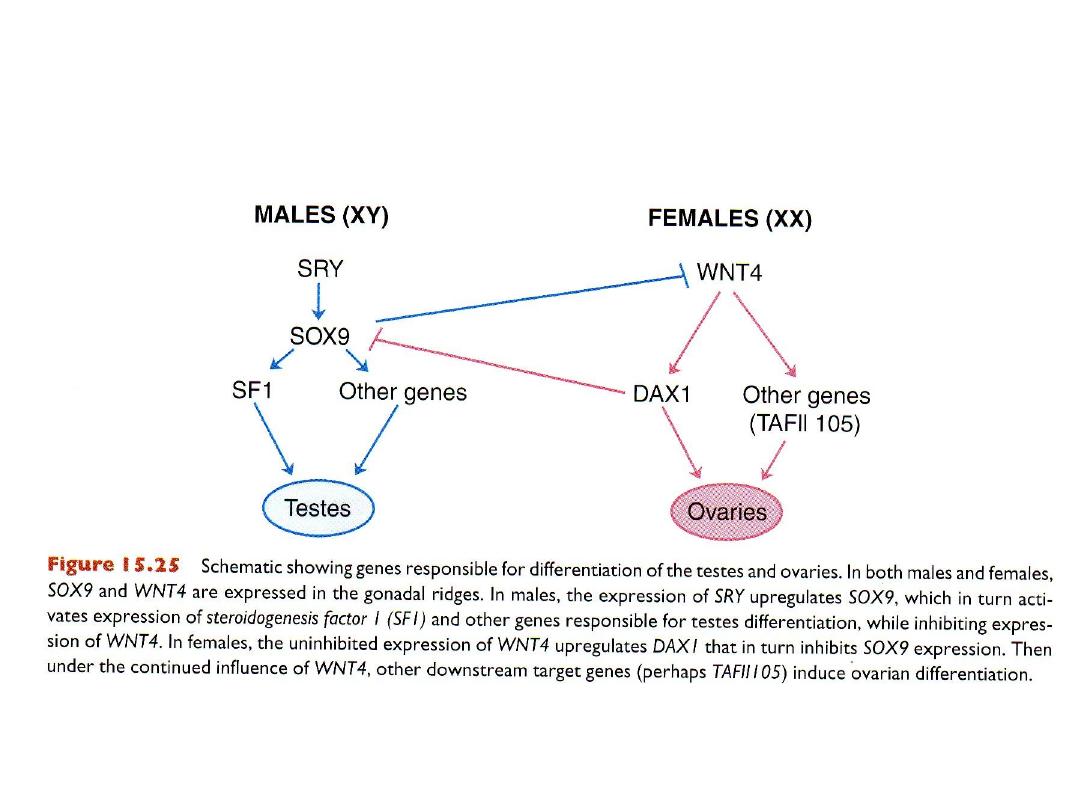
GENITAL SYSTEM
• Y chromosome:
– key to sexual dimorphism
– Y chromosome contains SRY gene (testis-determining gene) on short arm
(Yp11)
– SRY gene protein(a transcription factor): testis-determining factor
– Testis-determining factor present male development of sexual organs
– Absence of testis-determining factor female development
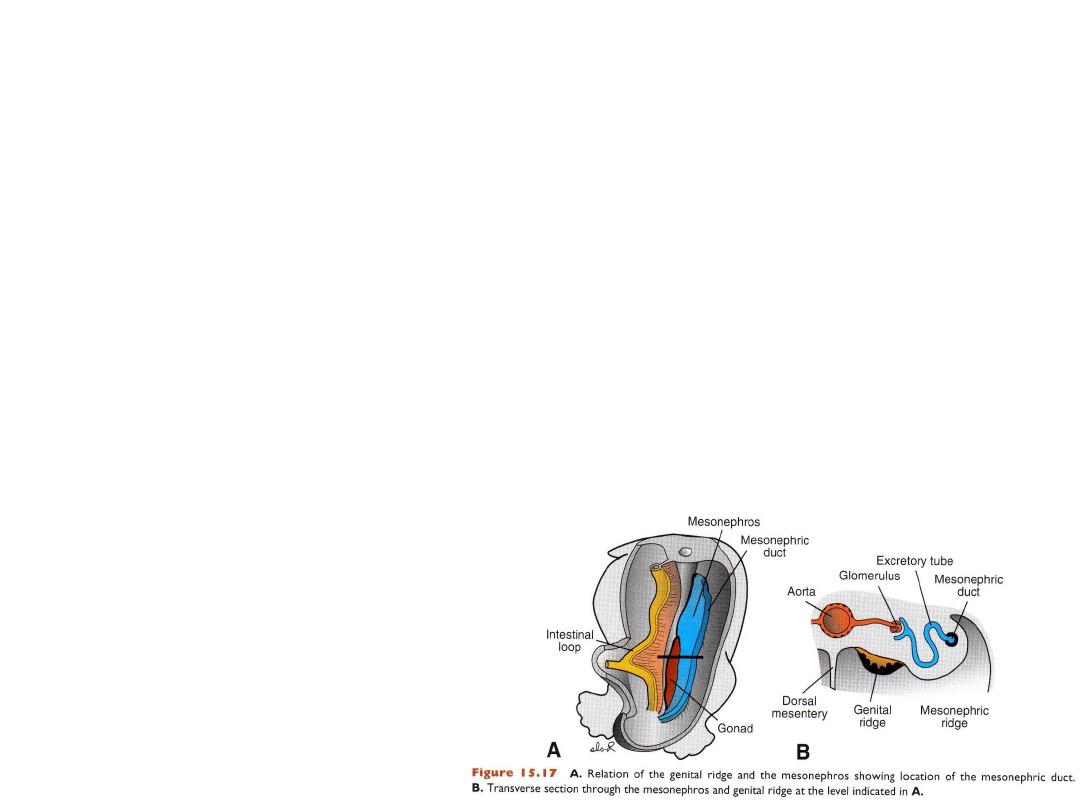
GONADS
Genital ridges
•
Sex of embryo is determined at
fertilization
•
Gonads acquire male or female
morphology at 7
th
week
•
Genital (gonadal) ridges form ovaries
or testes
•
Genital ridges originate from
intermediate mesoderm
•
Germ cells reach genital ridges in 6
th
week
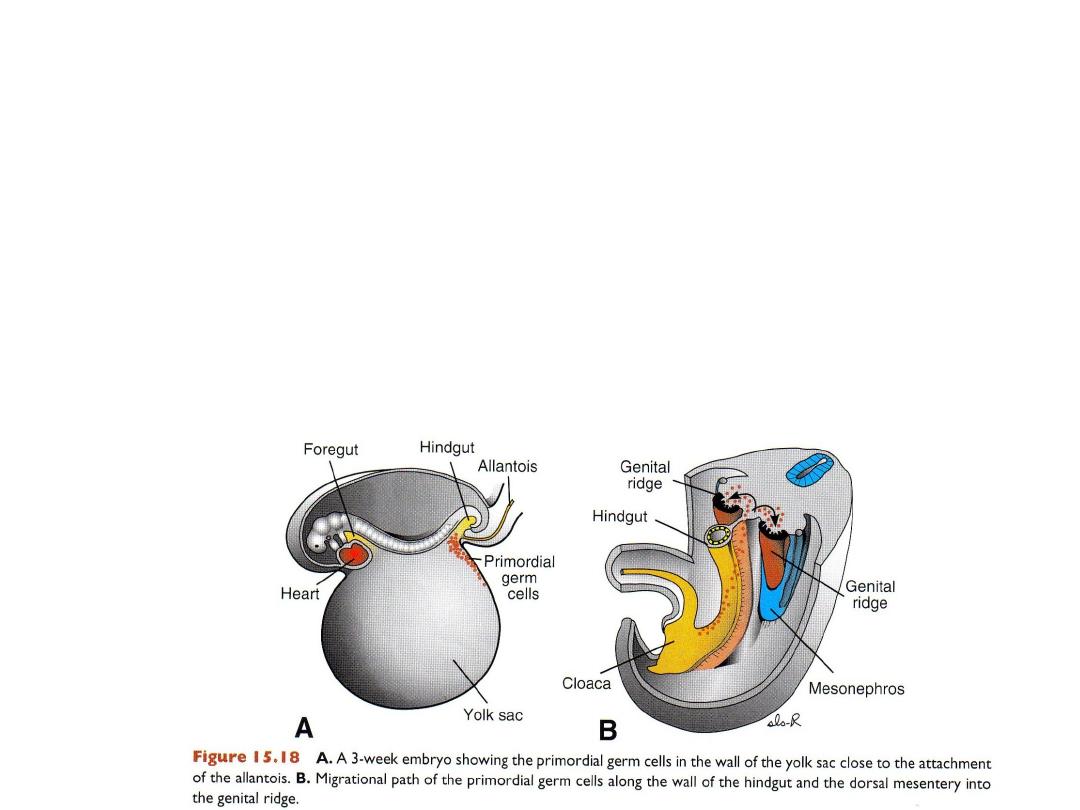
Primordial germ cells:
– Originate in epiblast
– Migrate through primitive streak
– By 3rd week reside among endoderm of yolk sac close to allantois
– In 4th week they migrate by ameboid movement along dorsal mesentry of
hindgut
– They arrive at primitive gonads at beginning of 5
th
week
– They invade the genital ridges in the sixth week
•
PGC: Inductive influence on development of the indifferent gonad to form ovary or testis
Failure of PGC to reach indifferent gonads they do not develop.
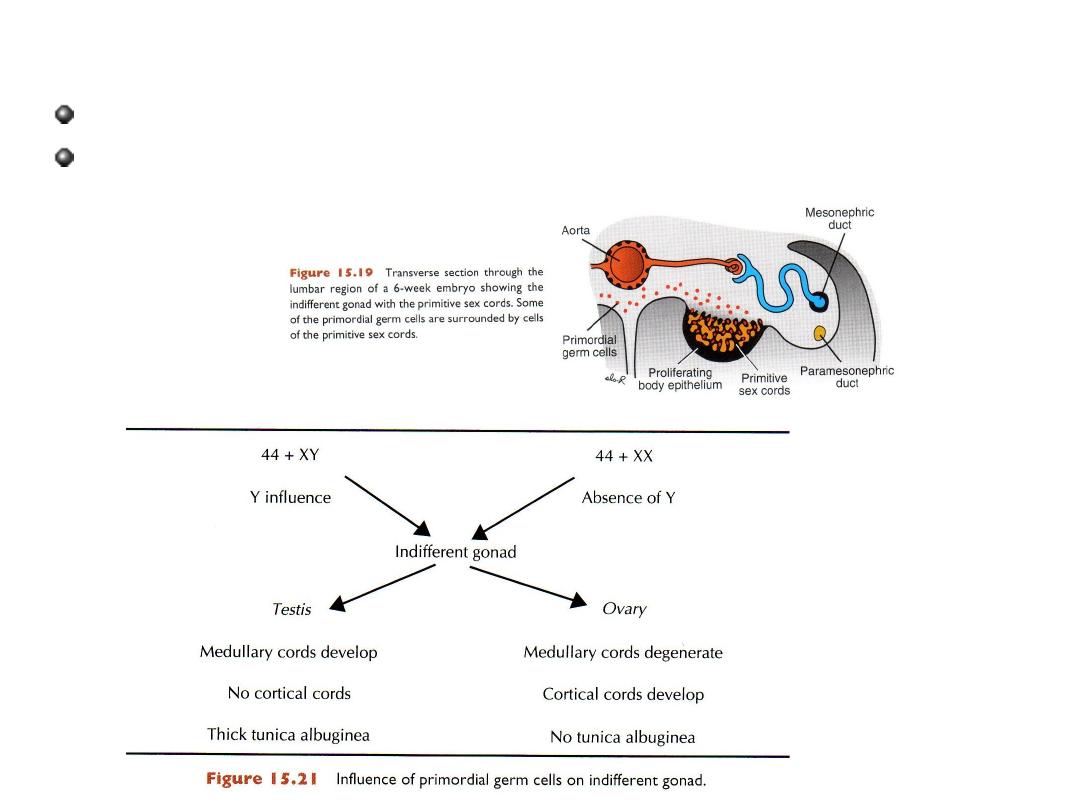
INDIFFERENT GONAD & PRIMITIVE SEX CORDS,
6
th
week
Epithelium of genital ridges form primitive sex cords
Primitive sex cords are similar in male & female and the gonad is called
indifferent.
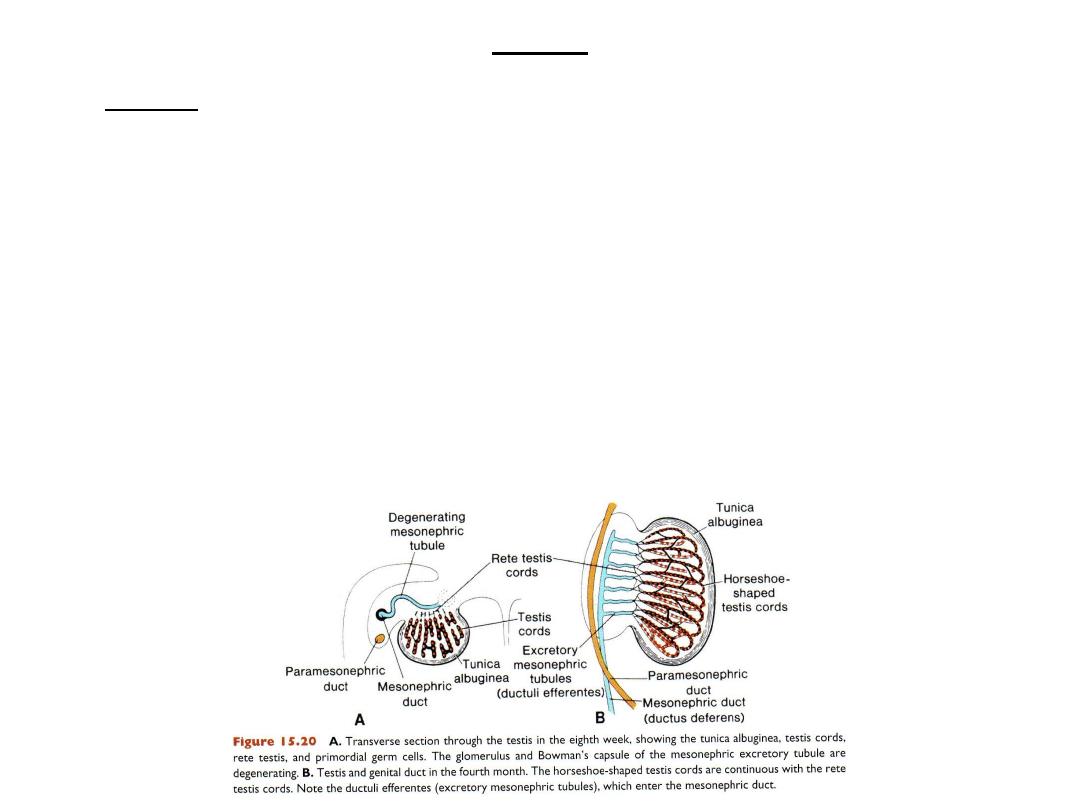
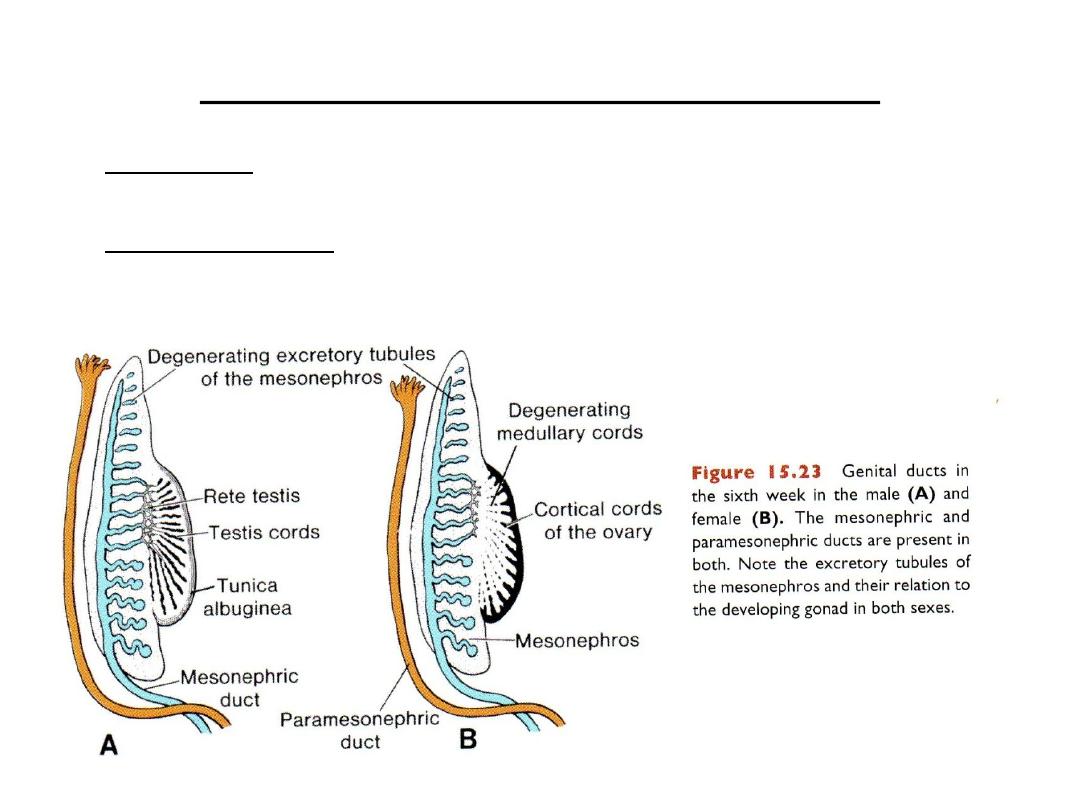
Testis
• In male: Primitive sex cords proliferate & penetrate into medulla & form
testis or medullary cords
• They lose contact with surface that gets covered by tunica albuginea.
• Testis cords are composed of PGCs & sustentacular cells of Sertoli
(derived from surface epithelium)
• Interstitial cells of Leydig: derived from mesenchyme of gonadal ridge, lie
between testis cords
• By 8th week Leydig cells produce testosterone.
• Testis cords remain solid until puberty
• At puberty they canalize forming the Seminiferous tubules
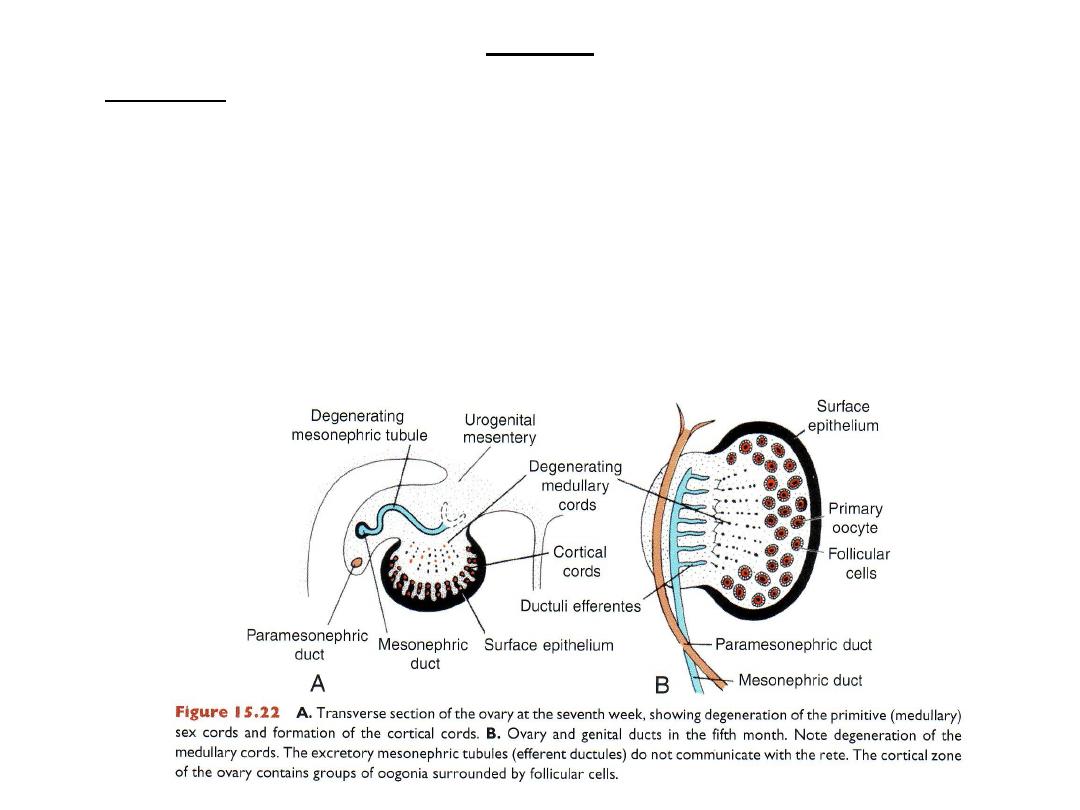
Ovary
• In female primitive cords disappear
• Cortical cords form in 7
th
week from surface epithelium
• In 3
rd
month epithelial (follicular) cells surround oogonia
• Together follicular cells & oogonia form the primordial follicle.
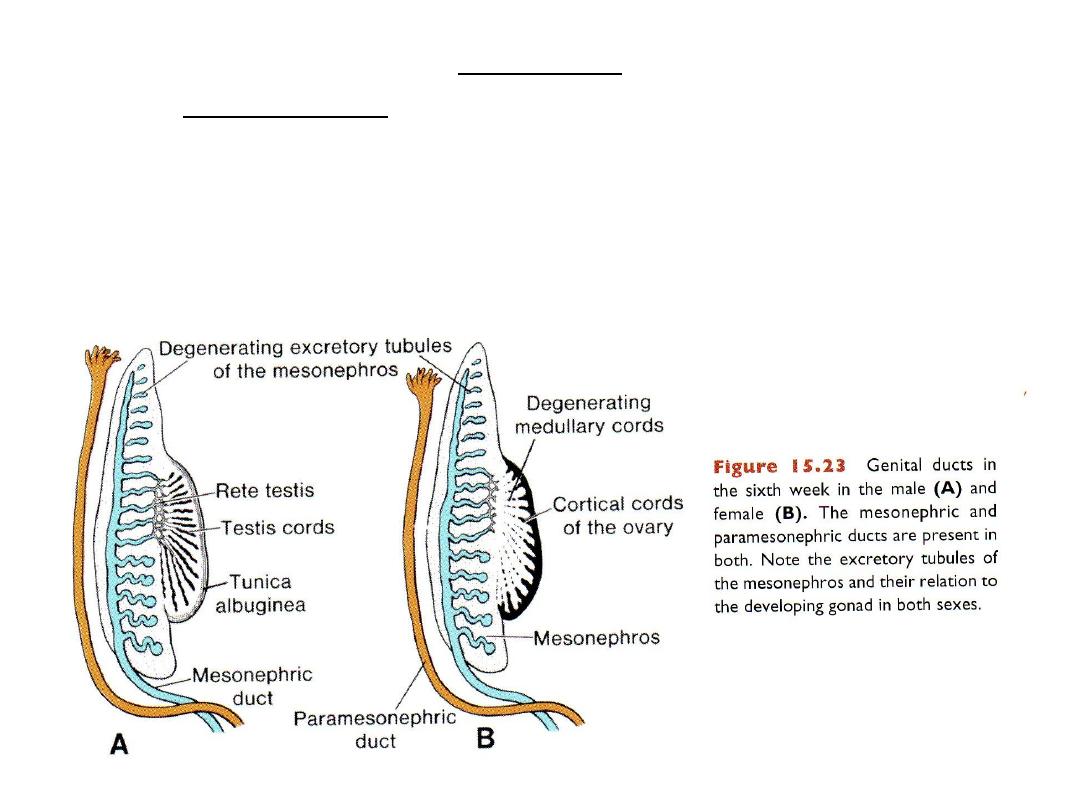
Genital ducts
• In the indifferent stage: both sexes have:
• 2 mesonephric (wolffian) ducts and 2 paramesonephric (mullerian) ducts
• Mesonephric duct = remains in male, lost in female = remnants may be
cysts.
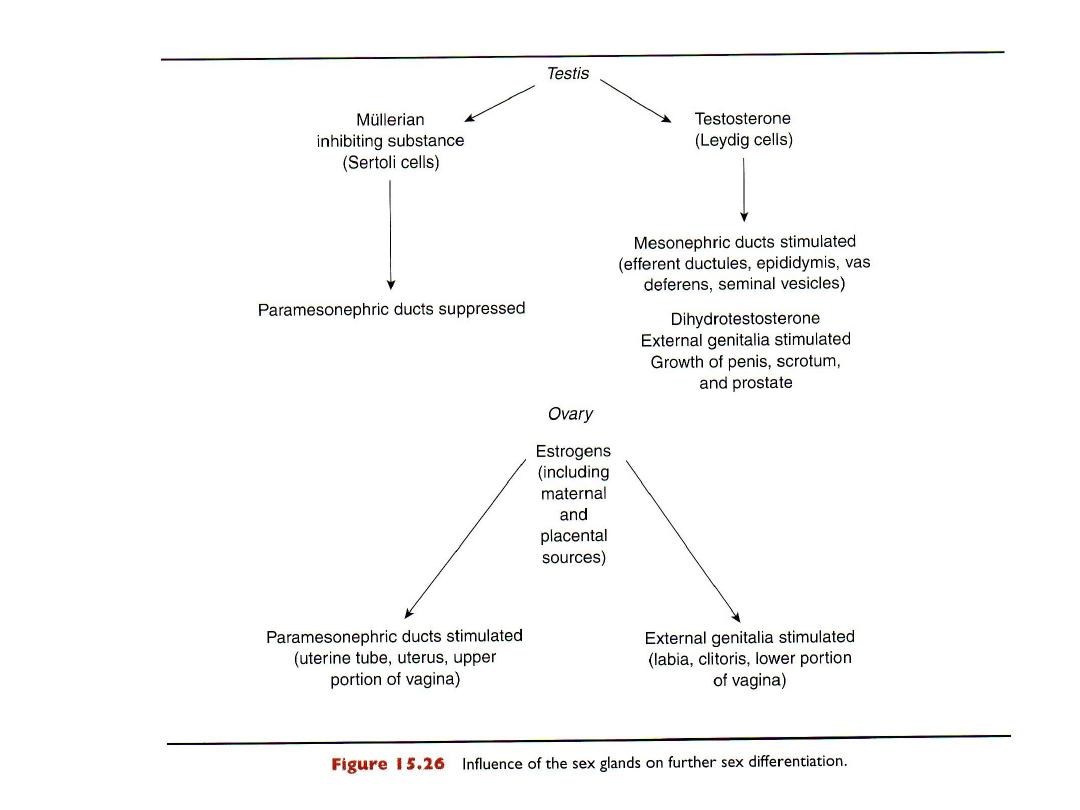
Paramesonephric duct (Mullerian)
• lost in male due to formation of mullerian inhibiting substance (MIS) or
antimullerian hormone made by Sertoli cells.
• Remain in female: because no Sertoli cells, no MIS.
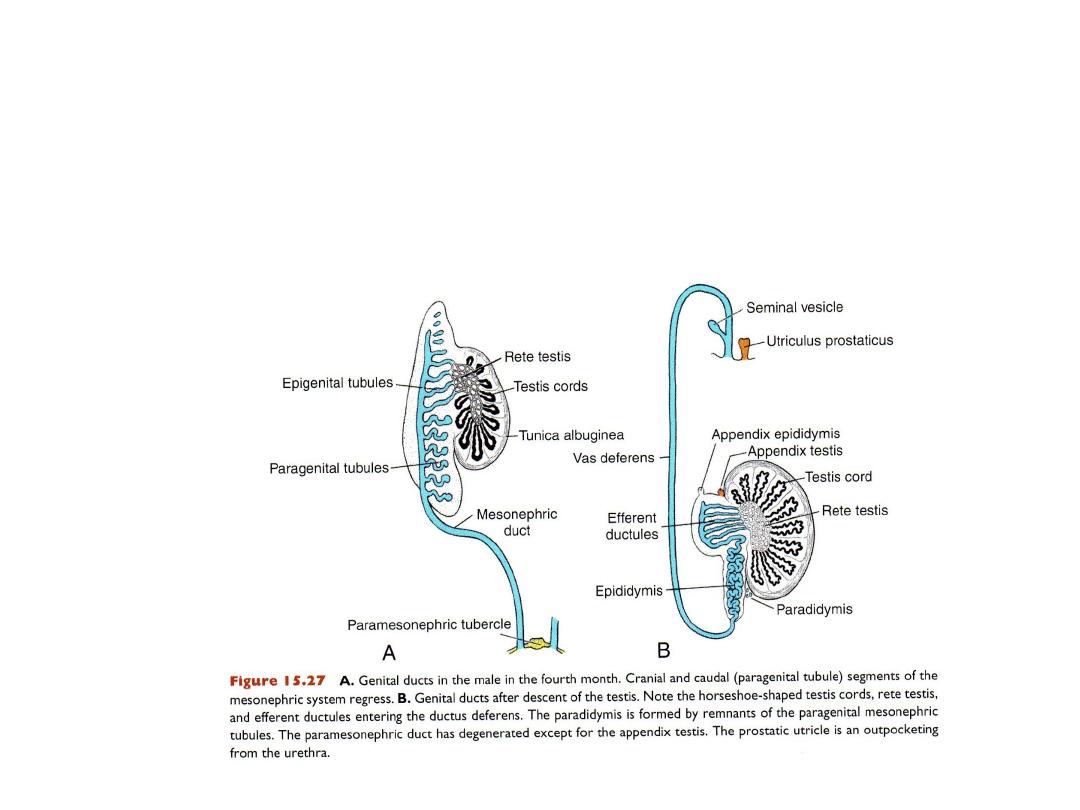
MALE GENITAL DUCTS
Mesonephros contributes tubules for male ducts = efferent ducts (from
old excretory tubules),
Mesonephric duct: gives rise to epididymis, seminal vesical, vas
deferens
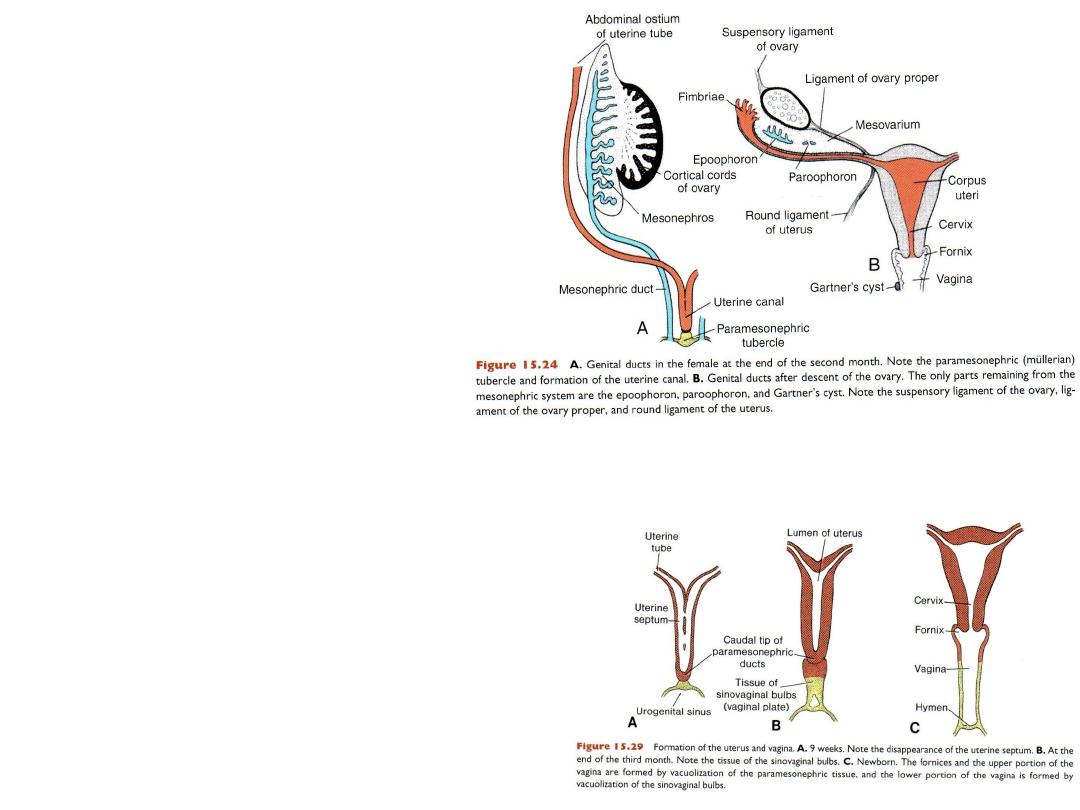
FEMALE GENITAL DUCTS
• Paramesonephric duct gives rise
to: uterine tubes (Fallopian),
uterus, upper part of vagina.
• Rest of vagina: from urogenital
sinus, vaginal bulbs.
•
Paramesonephric duct = uterine tubes
(Fallopian), uterus, upper part of
vagina.
•
Rest of vagina: from urogenital sinus,
vaginal bulbs.
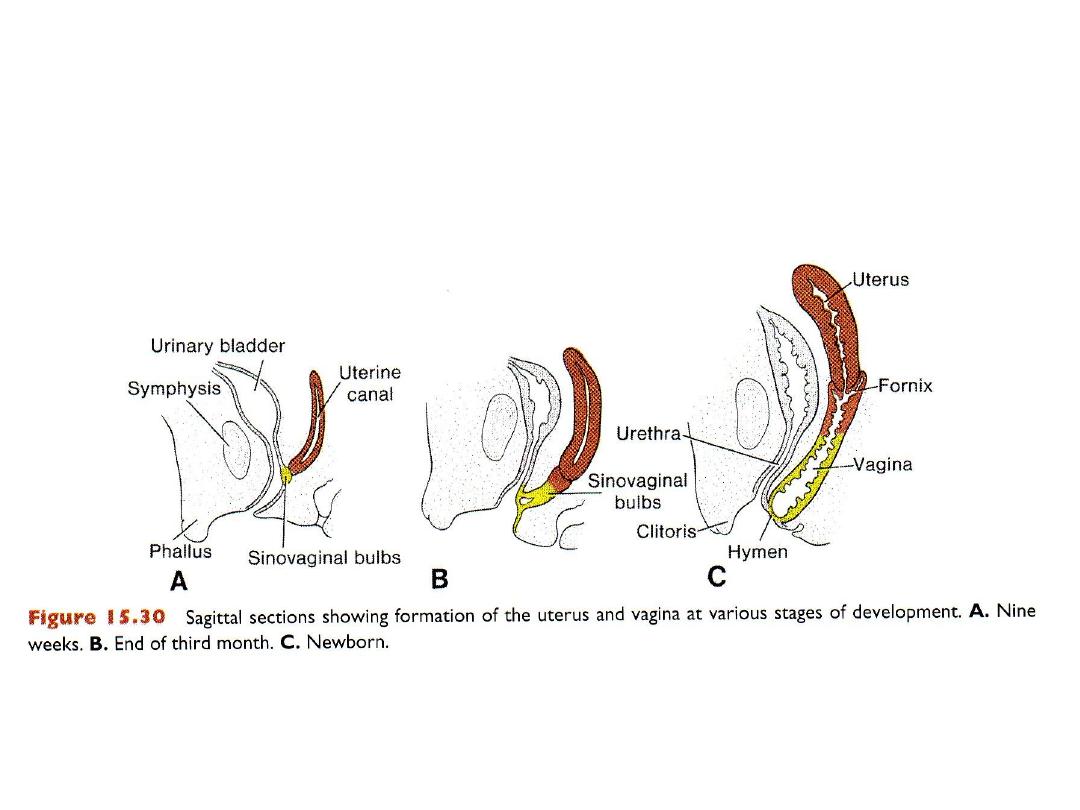
FEMALE GENITAL DUCTS
• Paramesonephric duct = uterine tubes (Fallopian), uterus, upper part of
vagina.
• Rest of vagina: from urogenital sinus, vaginal bulbs.
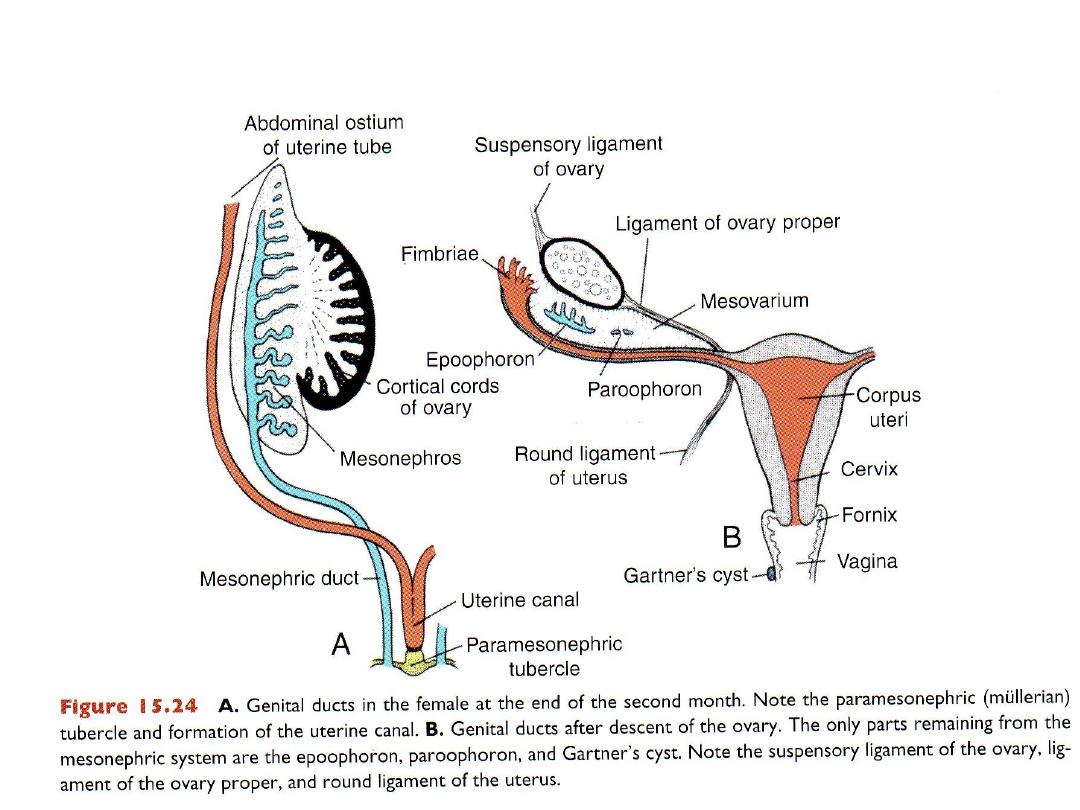
REMNANTS OF THE MESONEPHRIC DUCT
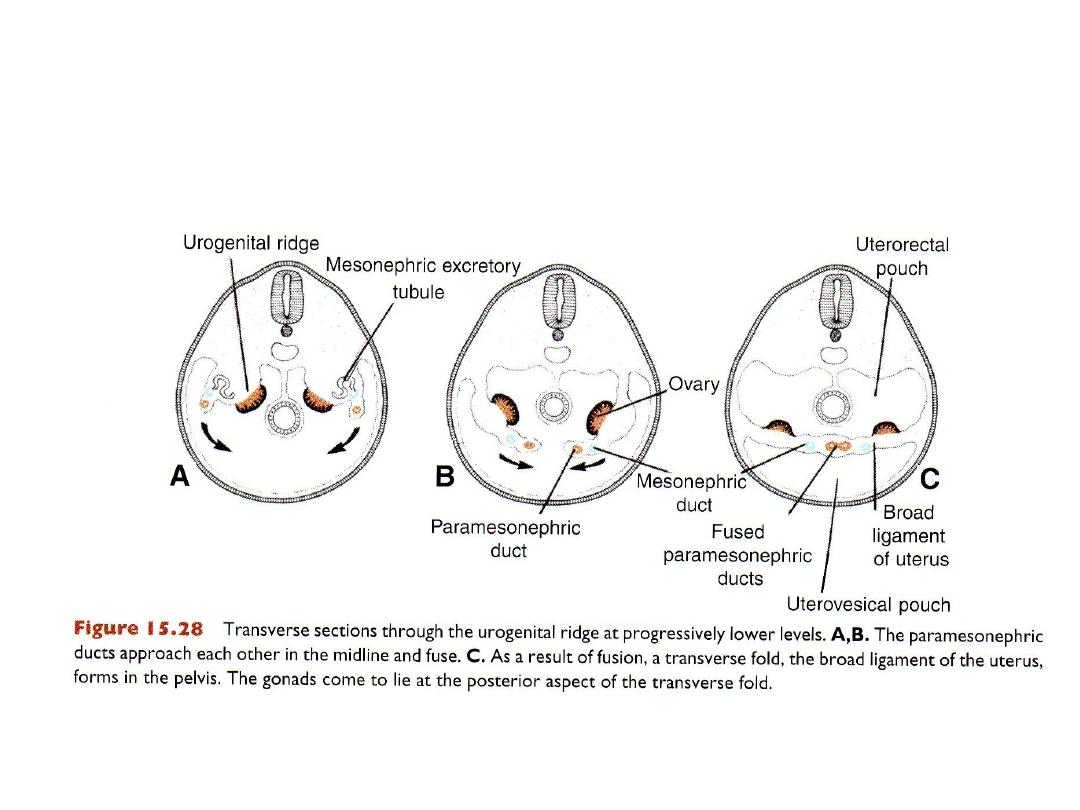
BROAD LIGAMENT OF THE UTERUS
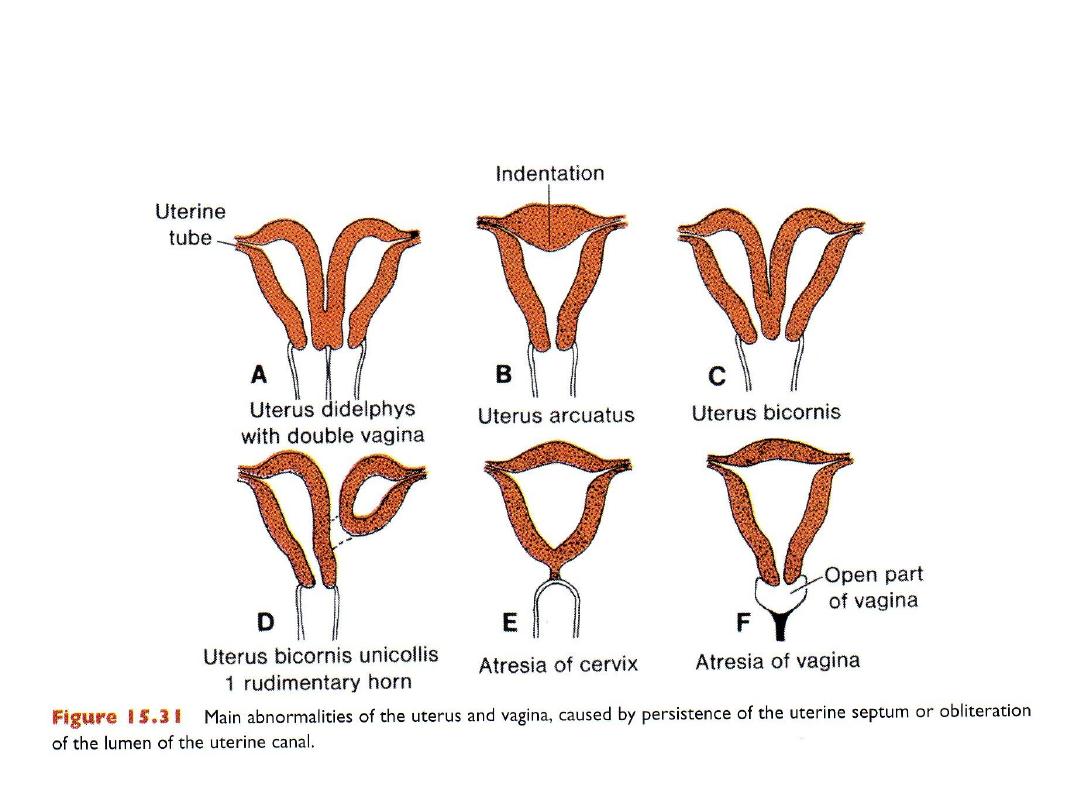
UTERINE & VAGINAL DEFECTS
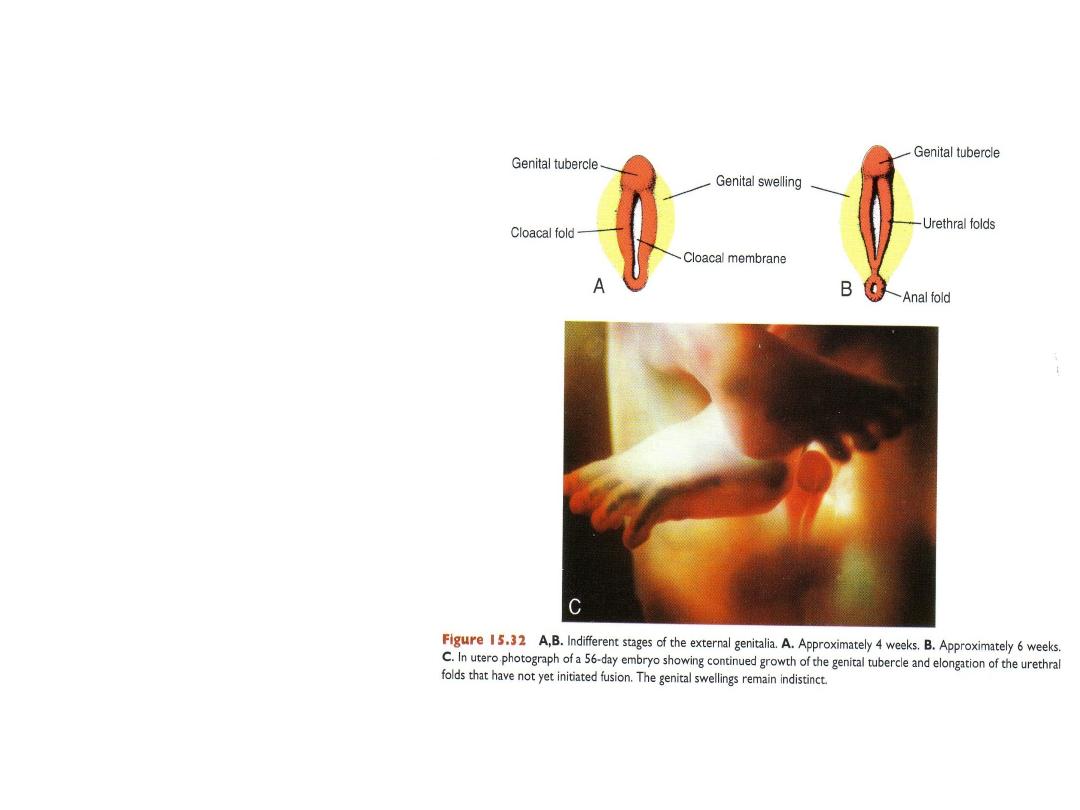
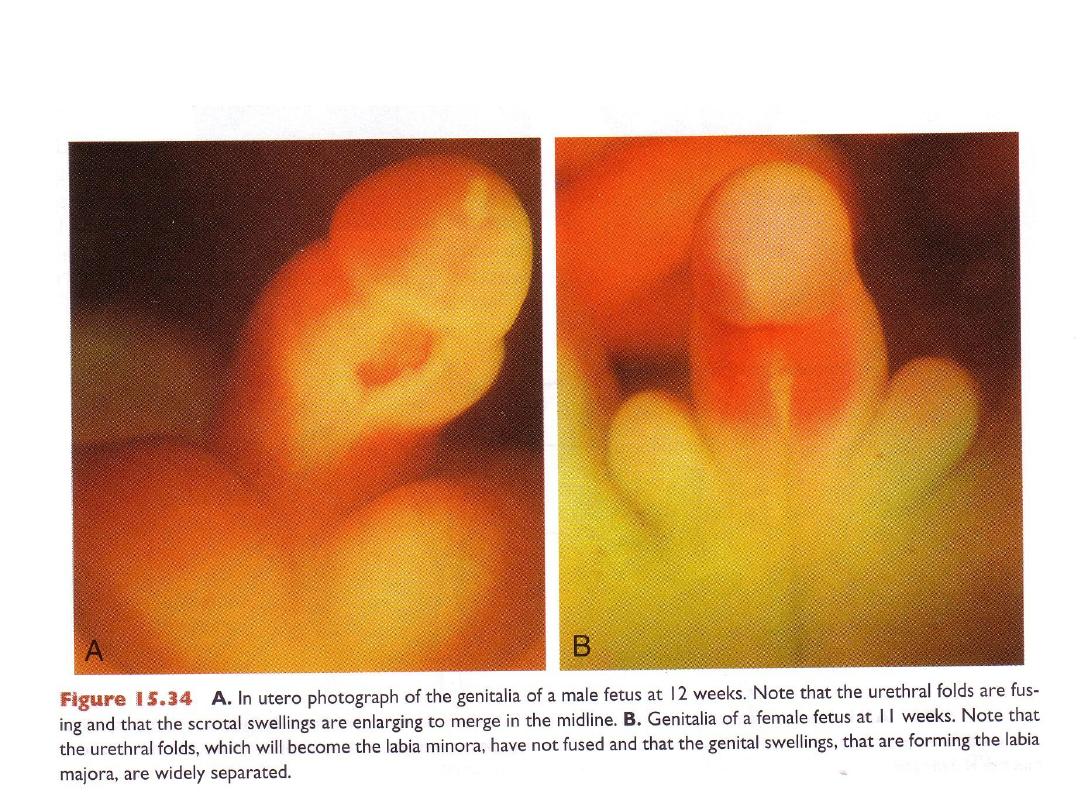
EXTERNAL GENITALIA:
Indifferent stage
External genitalia: start
with:
genital tubercle and
cloacal folds around
cloacal membrane.
Urorectal septum separates
region into urogenital
(surrounded by urethral
folds) and anal (surrounded
by anal folds) areas.
Genital swellings form on
sides of urethral folds.
In Female
In Male
clitoris
penis
Genital tubercle
no fusion = labia minora
fuse = urethra
Urethral folds
no fusion = labia majora
fuse = scrotum
Genital swellings
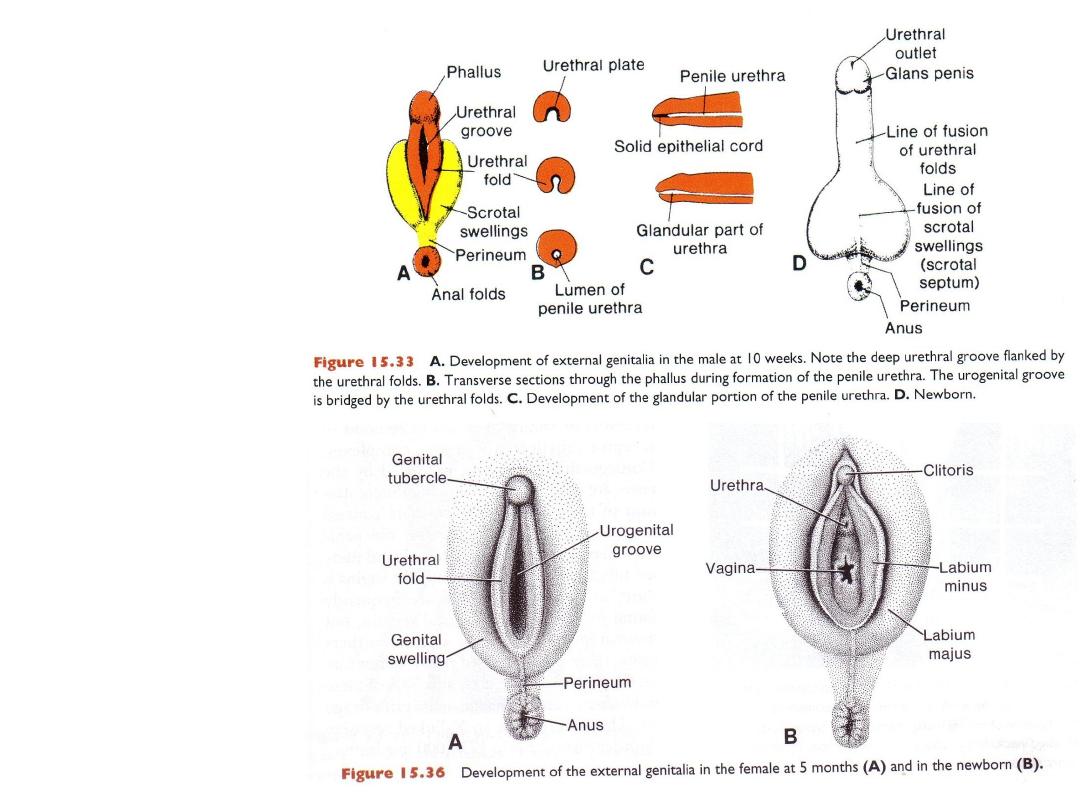
EXTERNAL
GENITALIA IN
THE MALE
EXTERNAL
GENITALIA IN
THE FEMALE
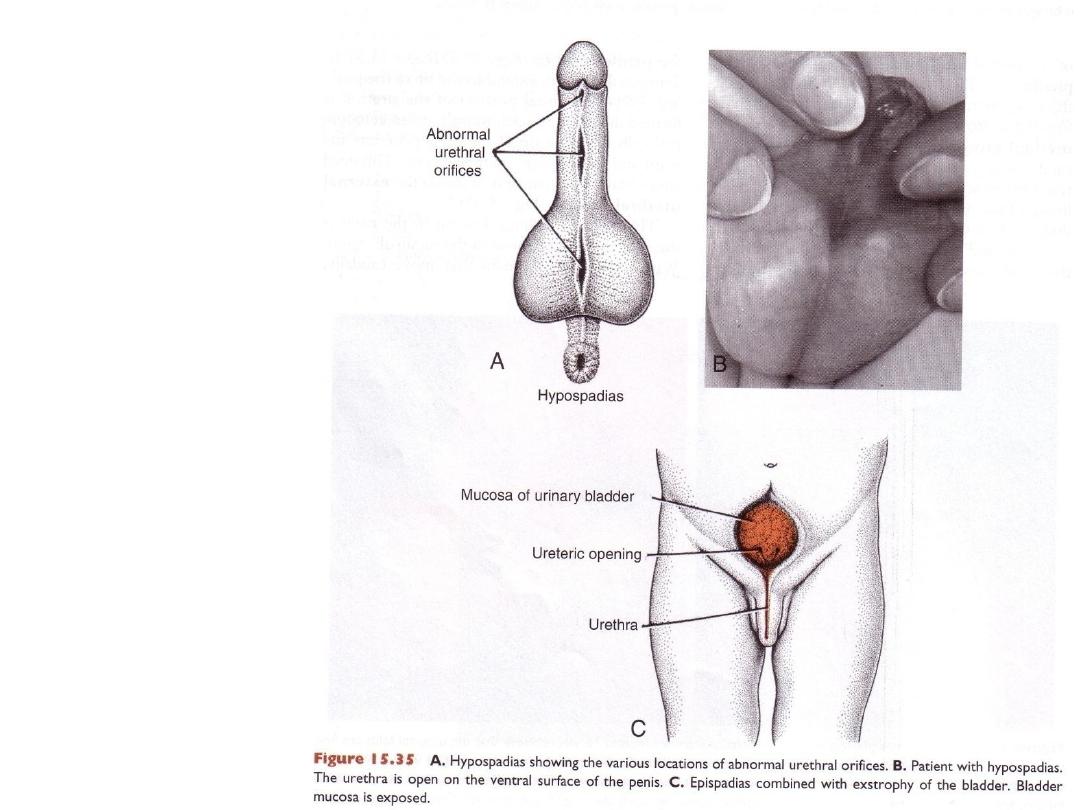
DEFECTS IN THE
MALE GENITALIA
Hypospadias &
epispadias
Micropenis
• Insufficient androgen
for growth of external
genitalia.
• Bifid penis or double
penis: if the genital
tubercle splits.

Disorders Of Sexual Development
Sexual Ambiguity
1.
Ambiguous genitalia:
1.
A female with a large clitoris or
2.
A male with a small penis
2.
Hermaphrodite: A person with characteristics of both sexes
• True hermaphrodite: a person with ovotestis, in 70% the karyotype is
46,XX, most are raised as females.
3. Congenital adrenal hyperplasia with excessive production of androgens.
• Females have a range of sexual characteristics from partial masculinization
with a large clitoris to virilization and a male appearance.
4. Androgen insensitivity syndrome: 46, XY
• Males with lack of androgen receptors or failure of tissues to respond to
receptor-testosterone complex.
DEFECTS IN SEX DIFFERENTIATION
•
Klienfelter syndrome (47,XXY)
•
Gonadal dysgenesis:
– XY female gonadal dysgenesis (Swyer syndrome): point mutations or deletions
of the SRY gene.
– Turner syndrome (45, X)
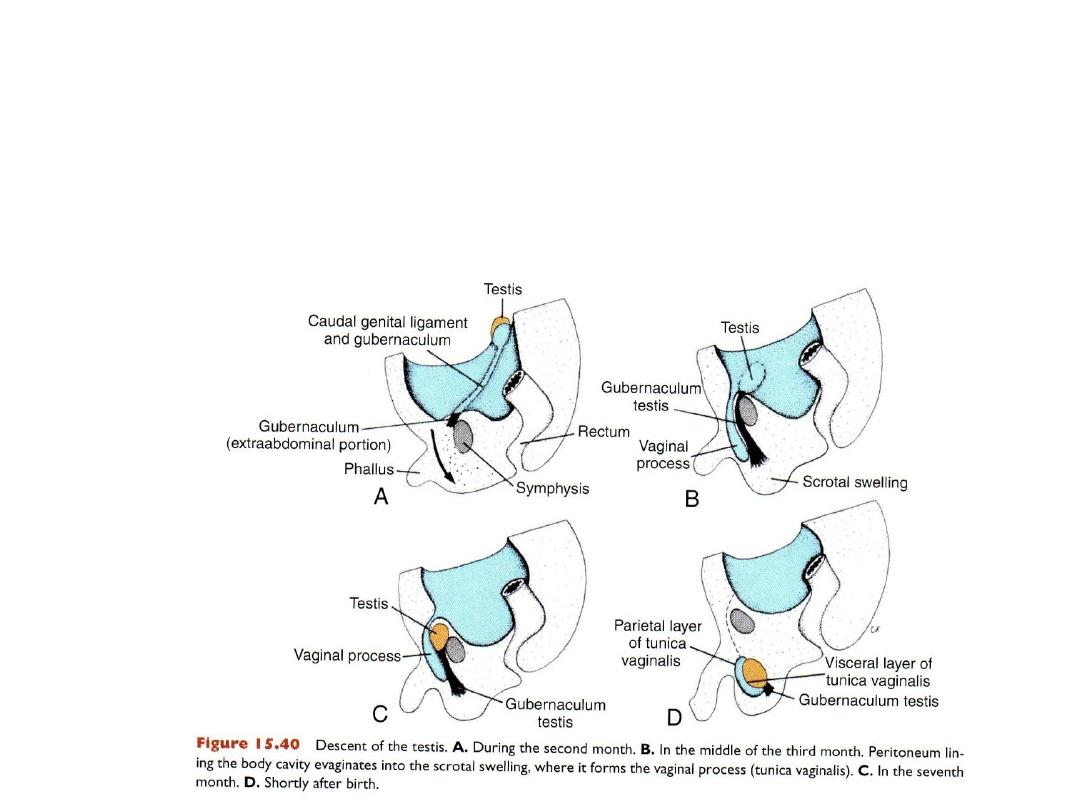
Descent of testes
Testes develop in abdomen, descend to scrotum through internal
inguinal ring, inguinal canal, external ring: preceded by processes
vaginalis that later surrounds each testis as the tunica vaginalis.
Gubernaculum attaches to caudal pole and to scrotum = assists in
descent.
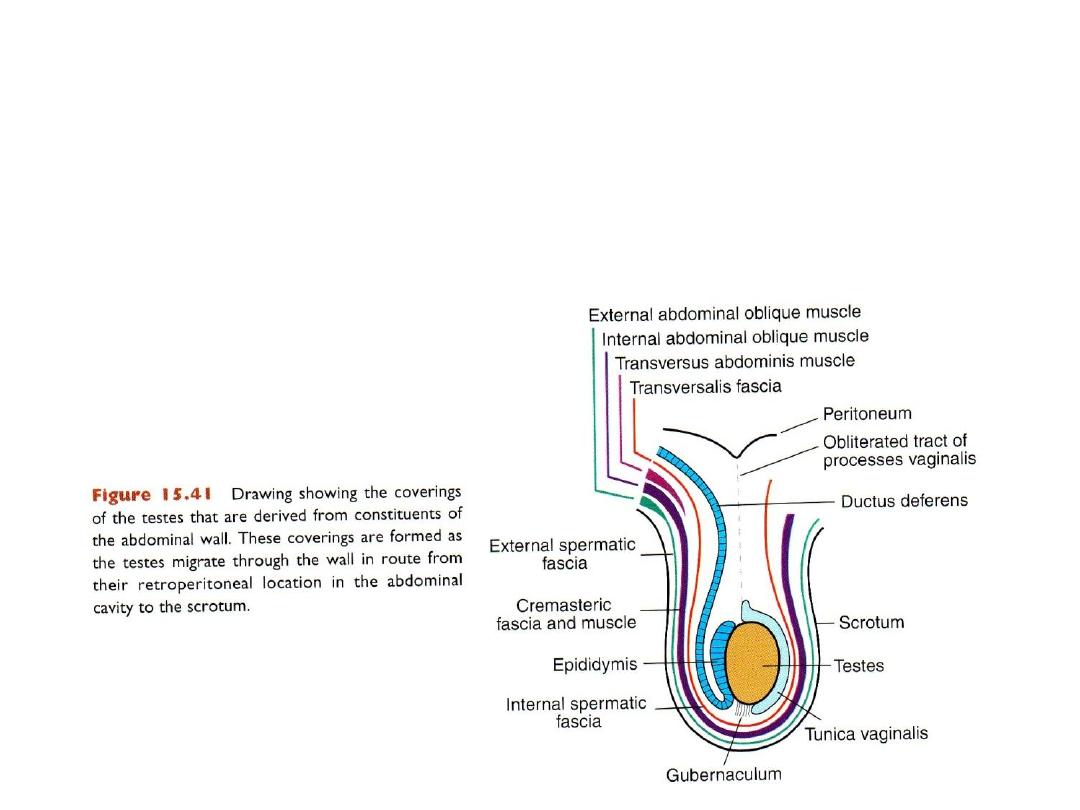
Coverings of testis
As testes passes through the abdominal wall it picks up layers:
Fascia transversalis = internal spermatic fascia.
Internal abdominal oblique = cremaster fascia and muscle.
External abdominal oblique = external spermatic fascia.
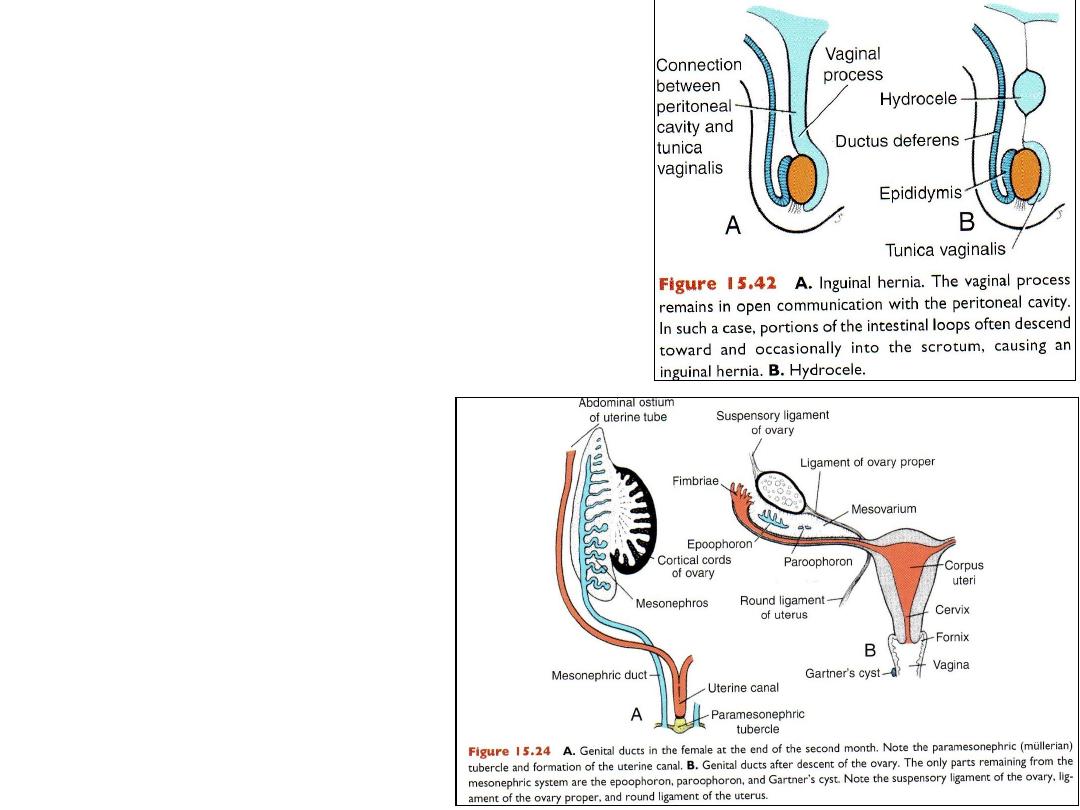
Defects in testis
descent
• Cryptorchism = one or both testes do
not descend.
• Inguinal hernia (indirect) = processes
vaginalis fails to close and intestines
pass through rings to scrotum.
• Hydrocele
DESCENT OF THE OVARIES
Ovary descends: ligament of
ovary, round ligament of
uterus.
Attachment of the ligament to
the uterus prevents ovary from
reaching labia majora.
