
Chapter 10
The Axial
Skeleton
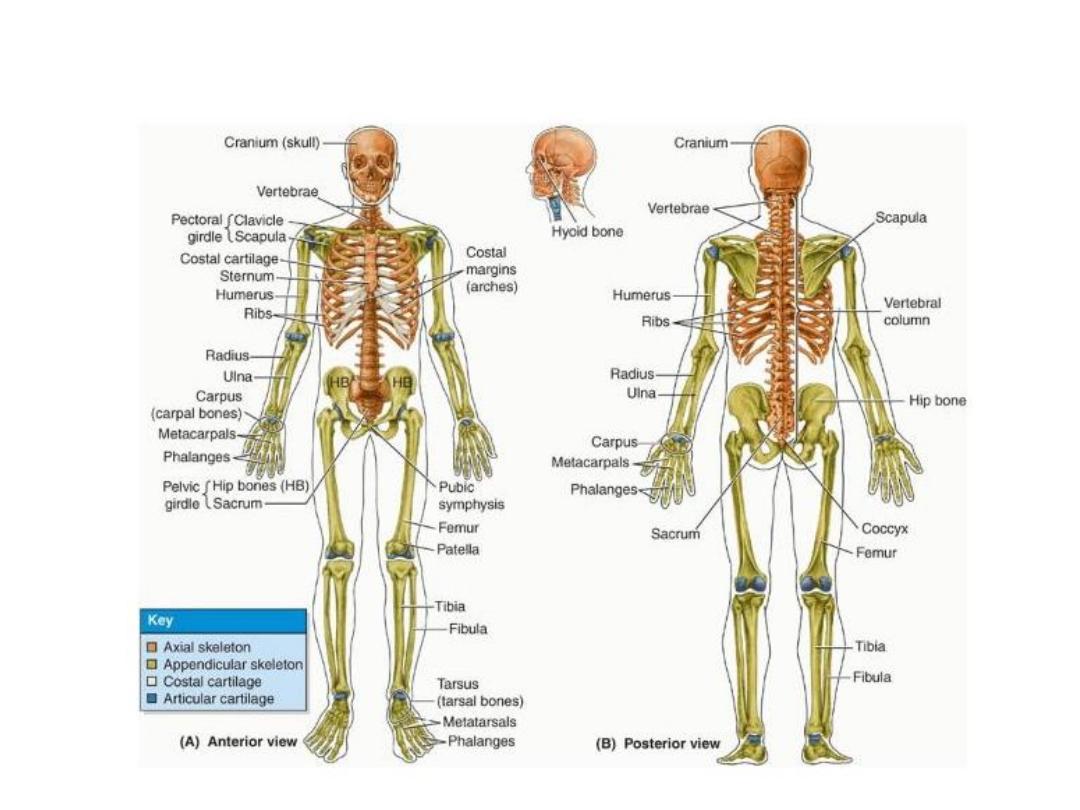
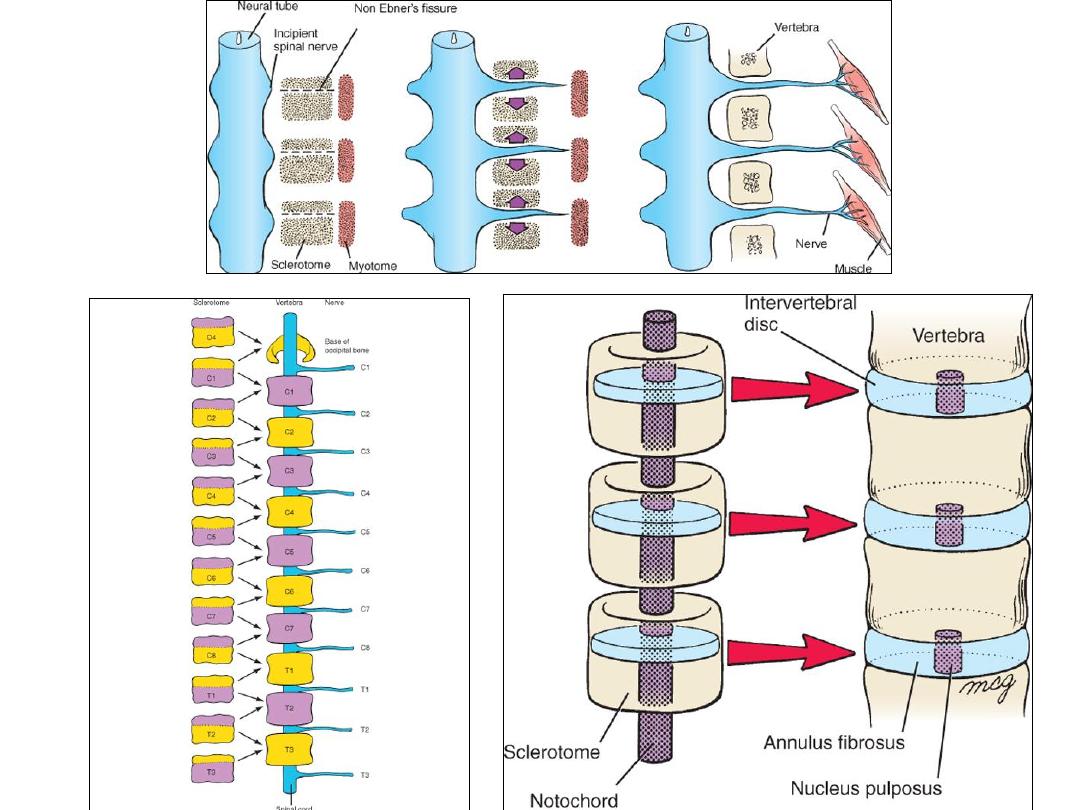
Skeletal system

ORIGIN OF SKELETAL SYSTEM
– MESODERM:
• PARAXIAL MESODERM
• LATERAL PLATE (PARIETAL LAYER) MESODERM
– NEURAL CREST
• The axial skeleton includes: The skull, Vertebral column, Ribs & sternum
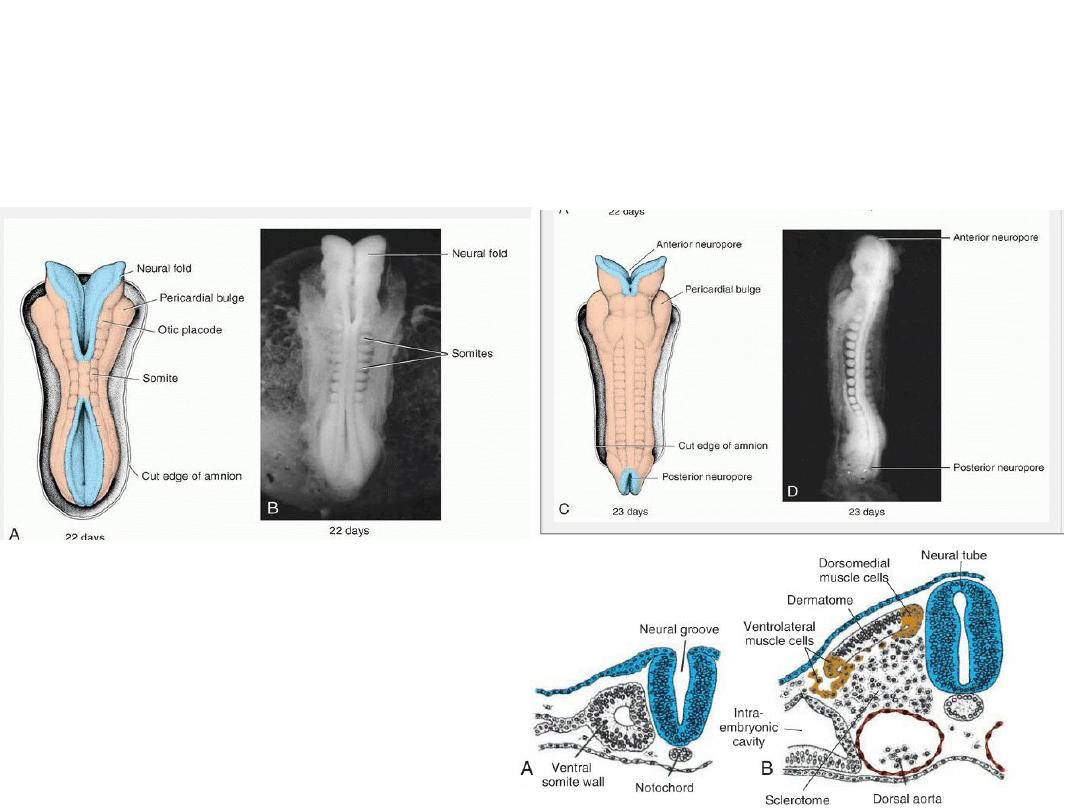
Paraxial mesoderm
• forms a segmented series of tissue blocks on each side of the neural tube, known
as:
o somitomeres in the head region and
o somites from the occipital region caudally
Somites
Differentiate into:
1) Sclerotome
2) Dermomyotome
Sclerotome becomes mesenchyme (embryonic connective tissue)
• Mesenchymal cells migrate and differentiate in many ways.
• They may become fibroblasts, chondroblasts, or osteoblasts (bone-forming cells) .
Neural crest cells in the head region also
become mesenchyme which forms
certain bones of the face and skull.
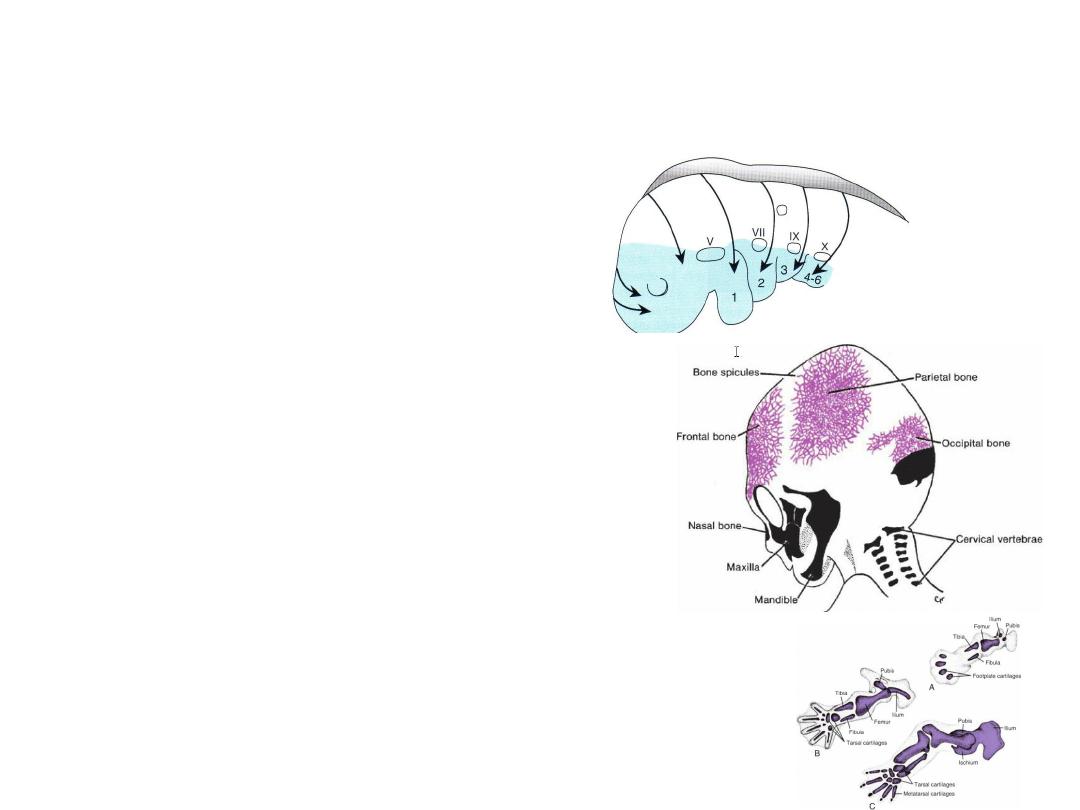
Ossification
• MEMBRANOUS OSSIFICATION
– Mesenchyme in the dermis differentiates
directly into bone: FLAT BONES OF SKULL
• ENDOCHONDRAL OSSIFICATION
– Mesenchyme differentiates first into hyaline
cartilage models which become ossified by
endochondral ossification: BASE OF THE SKULL
and the LIMS
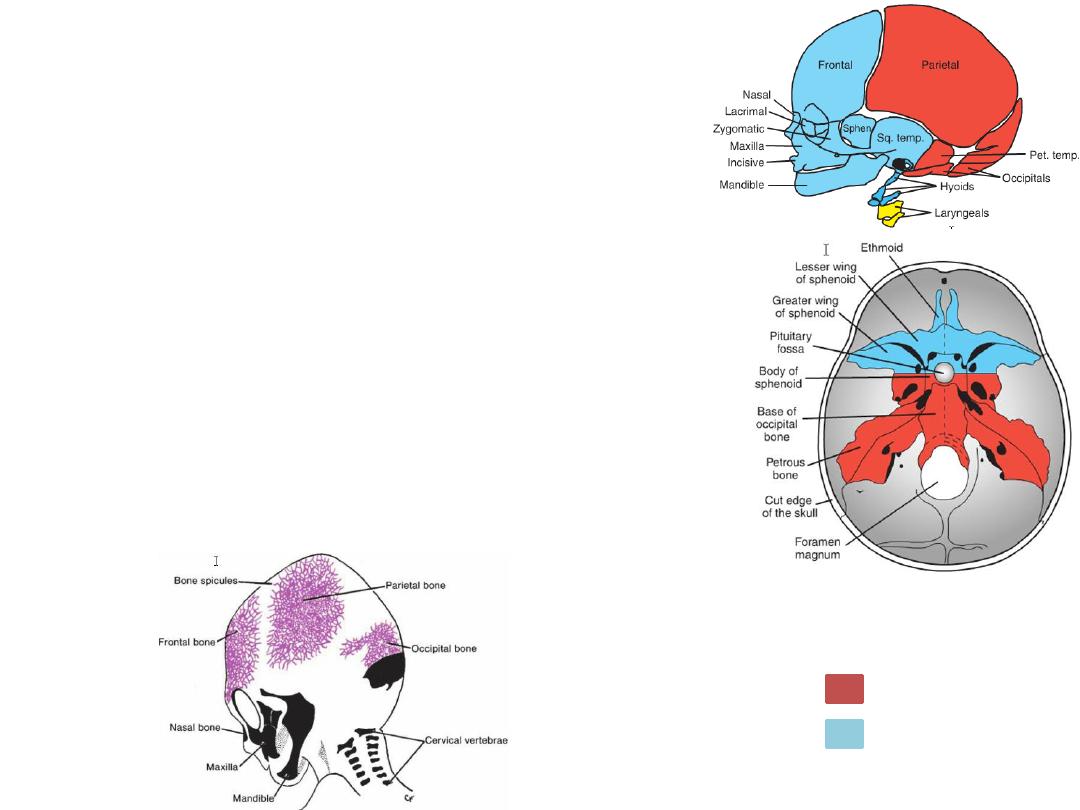
SKULL
• NEUROCRANIUM: a protective case around the brain
• VISCEROCRANIUM: the skeleton of the face.
NEUROCRANIUM
1.
Membranous part: vault of skull, flat bones.
2.
Cartilaginous part (Chondrocranium), bones of
the base of the skull.
Origin: mesenchyme of paraxial mesoderm & neural
crest
Membranous Neurocranium
• Derived from neural crest cells and paraxial mesoderm.
• Membranous ossification, flat bones.
Paraxial mesoderm:
Neural crest:
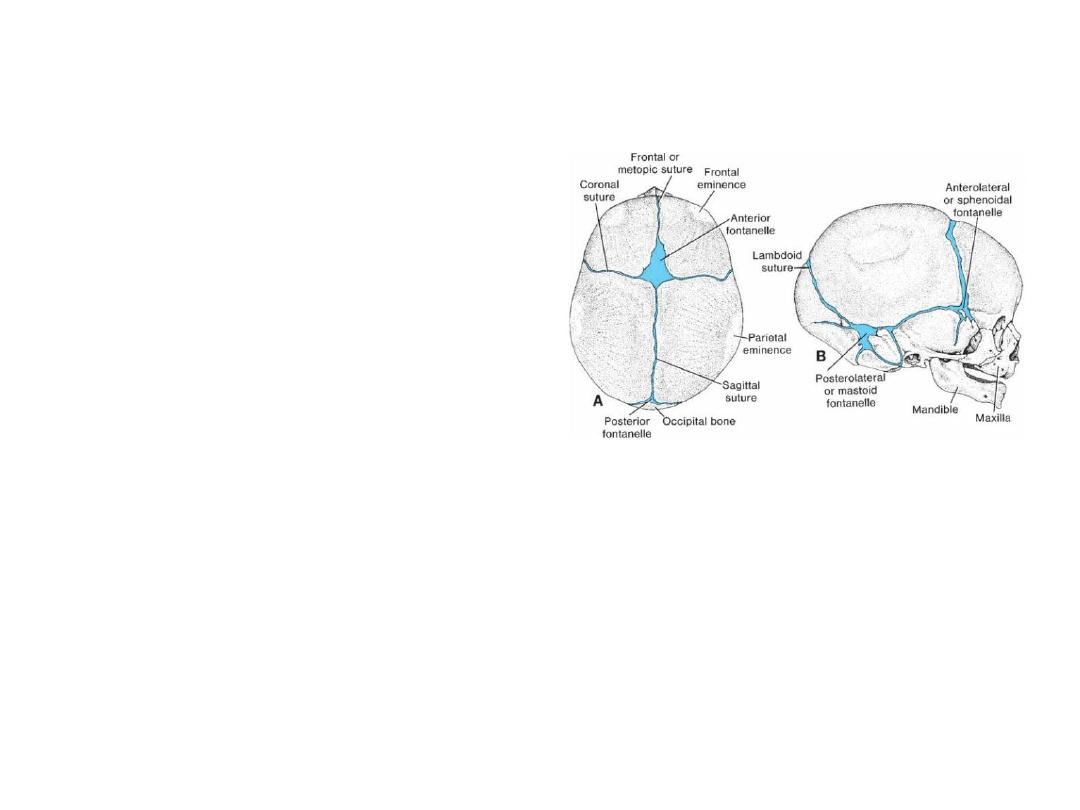
Newborn Skull
• Sutures: narrow seams of connective
tissue separate flat bones of the skull
• Origin:
1.
neural crest cells (sagittal suture)
2.
paraxial mesoderm (coronal suture).
• Fontanelles: At points where more than
two bones meet,
the anterior fontanelle , which is found
where the 2 parietal & 2 frontal bones
meet
Significance of sutures & fontanelles
• Sutures and fontanelles allow the bones of the skull to overlap (molding).
• Sutures and fontanelles remain membranous, allow bone growth after birth, to
allow brain growth
• In most cases, anterior fontanelle closes by 18 months of age, and the posterior
fontanelle closes by 1 to 2 months of age.
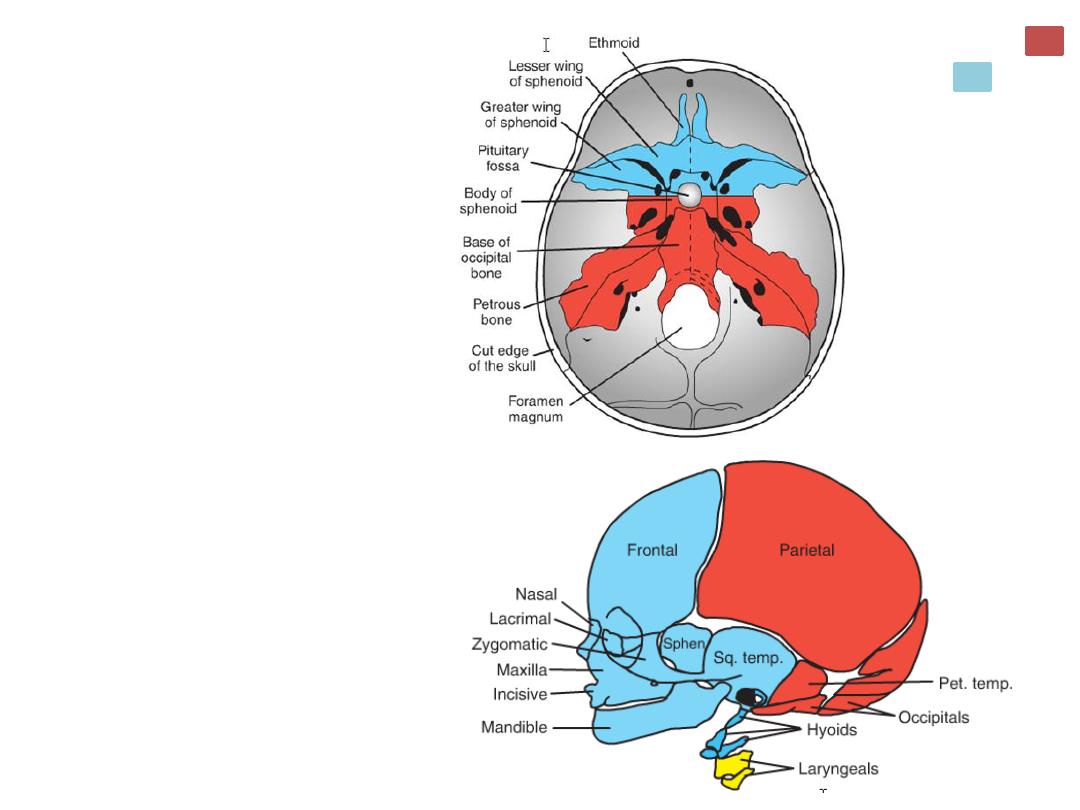
Cartilaginous
Neurocranium or
Chondrocranium
Initially consists of a number of
separate cartilages.
• Prechordal chondrocranium:
From neural crest cells.
• Lie in front of the rostral limit
of the notochord, which ends
at the level of the pituitary
gland in the center of the sella
turcica
• Chordal chondrocranium:
From paraxial mesoderm
(occipital sclerotomes).
• Lie posterior to pituitary.
The base of the skull is formed
when these cartilages fuse and
ossify by endochondral ossifi-
cation
Paraxial mesoderm:
Neural crest:
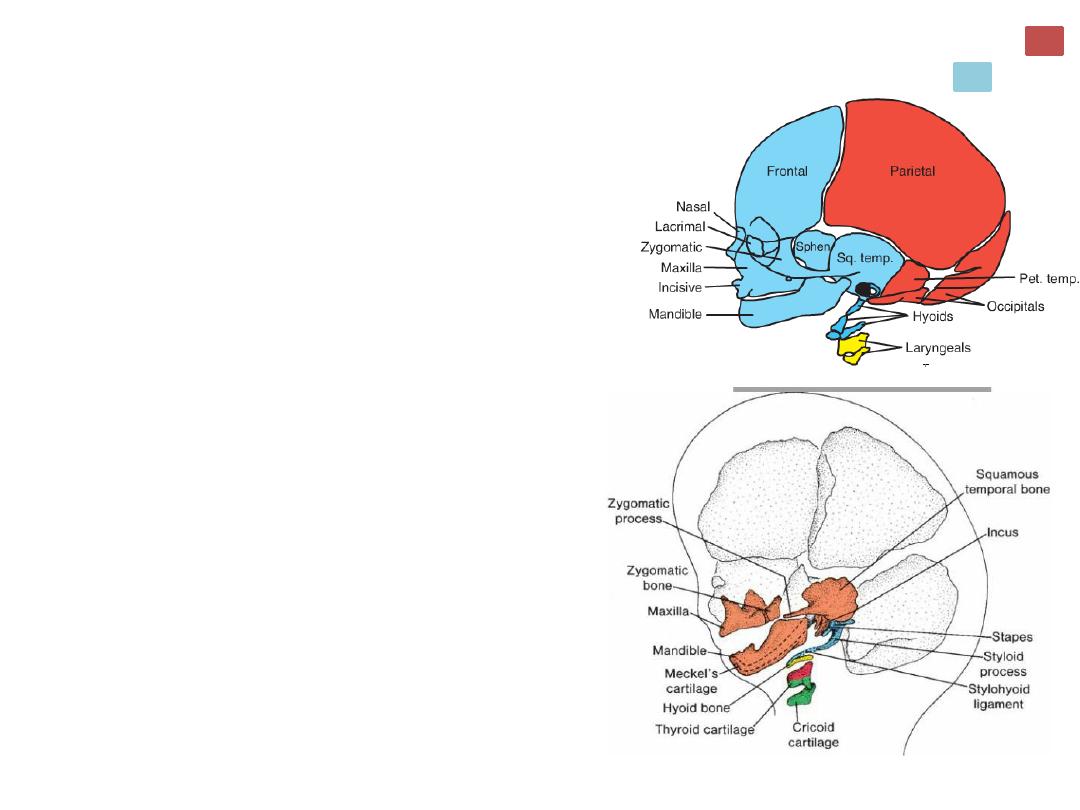
Viscerocranium
•Bones of the face.
•Mesenchyme for formation of the bones of the
face is derived from neural crest cells
•The nasal and lacrimal bones.
•Bones from the first two pharyngeal arches.
• The first arch:
• A dorsal portion, the maxillary process
maxilla, zygomatic bone, and part of the
temporal bone.
• A ventral portion, the mandibular process
contains the Meckel cartilage. Mesenchyme
around the Meckel cartilage condenses and
ossifies by membranous ossification to give rise
to the mandible.
• The second pharyngeal arch dorsal tip (and
dorsal tip of the mandibular process) gives
rise to the incus, the malleus , and the stapes.
Paraxial mesoderm:
Neural crest:

Craniofacial Defects and
SkeletalDysplasias
Neural Crest Cells
• Neural Crest Cells originating in the neuroectoderm form the facial skeleton and
most of the skull.
• These cells also constitute a vulnerable pop-ulation as they leave the
neuroectoderm; they are often a target for teratogens.
• Therefore, it is notsurprising that craniofacial abnormalities are common birth
defects.
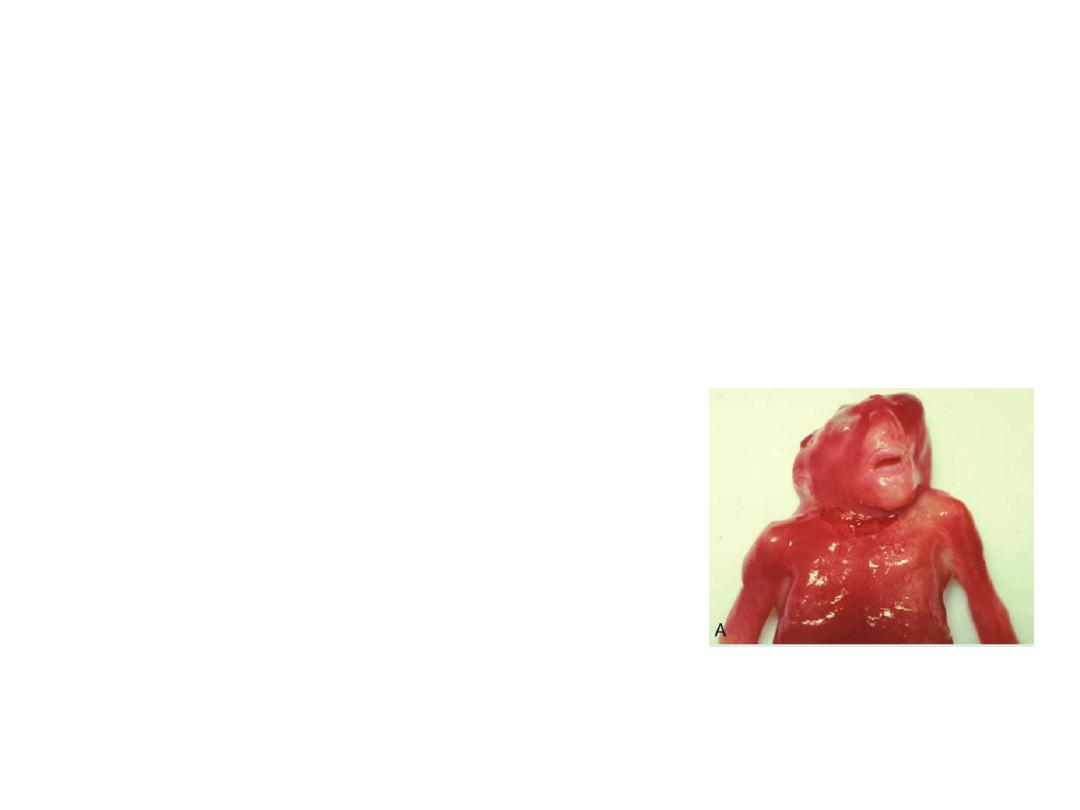
Cranioschisis
• Cranioschisis: when the cranial vault fails to form
and brain tissue exposed to amniotic fluid
degenerates, resulting in anencephaly.
• Cranioschisis is caused by failure of the cranial
neuropore to close.
• Children with such severe skull and brain defects
cannot survive.
Anencephaly

Children with relatively small defects in the skull through
which meninges and/or brain tissue herniate (cranial
meningocele and meningo-encephalocele, respectively)
may be treated successfully.
In such cases, the extent of neurological deficits depends
on the amount of damage to brain tissue.
Meningocele

Craniosynostosis:
Cranial abnormalities caused by
premature closure of one or more
sutures.
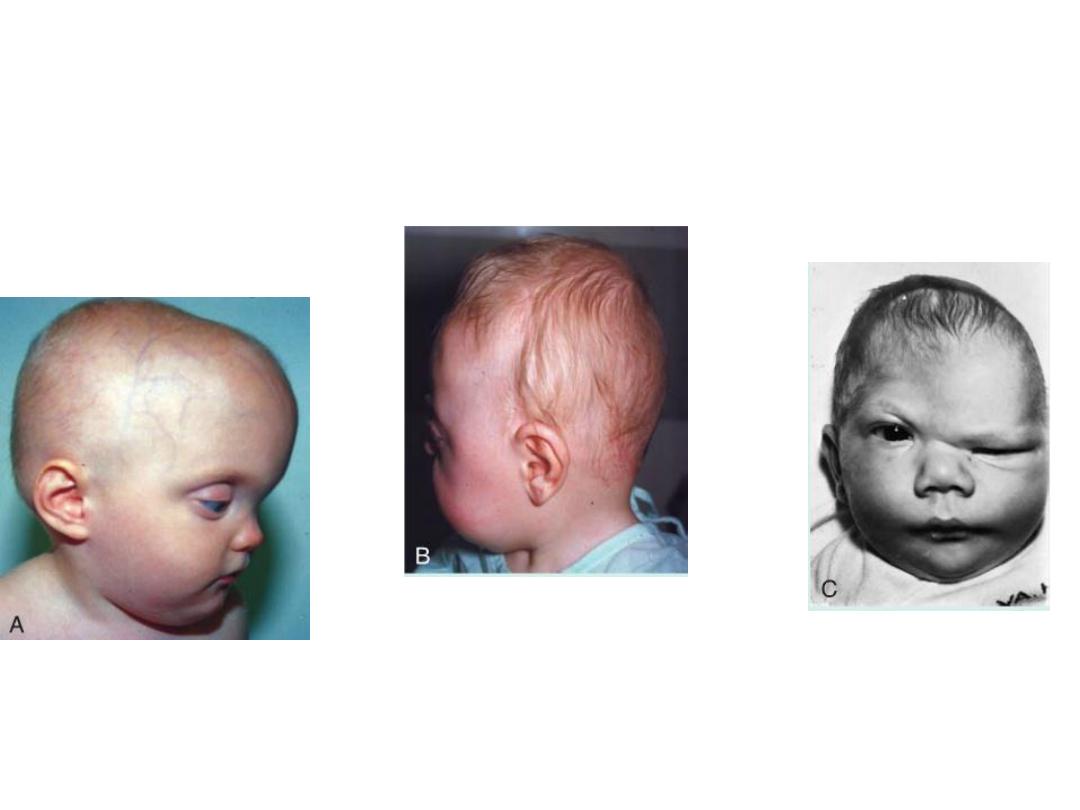
Scaphocephaly
Early closure of the
sagittal suture, results in
frontal and occipital
expansion, and the skull
becomes long and
narrow.
Brachycephaly
Premature closure of the coronal
suture results in a short skull
Plagiocephaly
If the coronal sutures
close prematurely on
one side only, then the
result is an asymmetric
flattening of the skull
• Regulation of suture closure involves secretion of various isoforms of
transforming growth factor beta.

Fibroblast growth factors (FGFs)
Fibroblast growth factor receptors
Important for skeletal development

Genetic causes of craniosynostosis
MUTATIONS IN FGFR1, FGFR2 & FGFR3
• FIBROBLAST GROWTH FACTOR RECEPTORS (fgfrs):
– FGFR1 & FGFR2: expressed in prebone & precartilage regions including
cranio-facial structures
– FGFR3: expressed in cartilage growth plates of long bones & occipital region
SKELETAL DYSPLASIAS
• Achondroplasia (ACH): the most common form of skeletal dysplasia
• Primarily affects the long bones.
• ACH is inherited as anautosomal dominant, and 90% of cases appear
sporadically due to new mutations.
• Other skeletal defects include a large skull (megalocephaly) with a small
mid face, short fingers, and accentuated spinal curvature
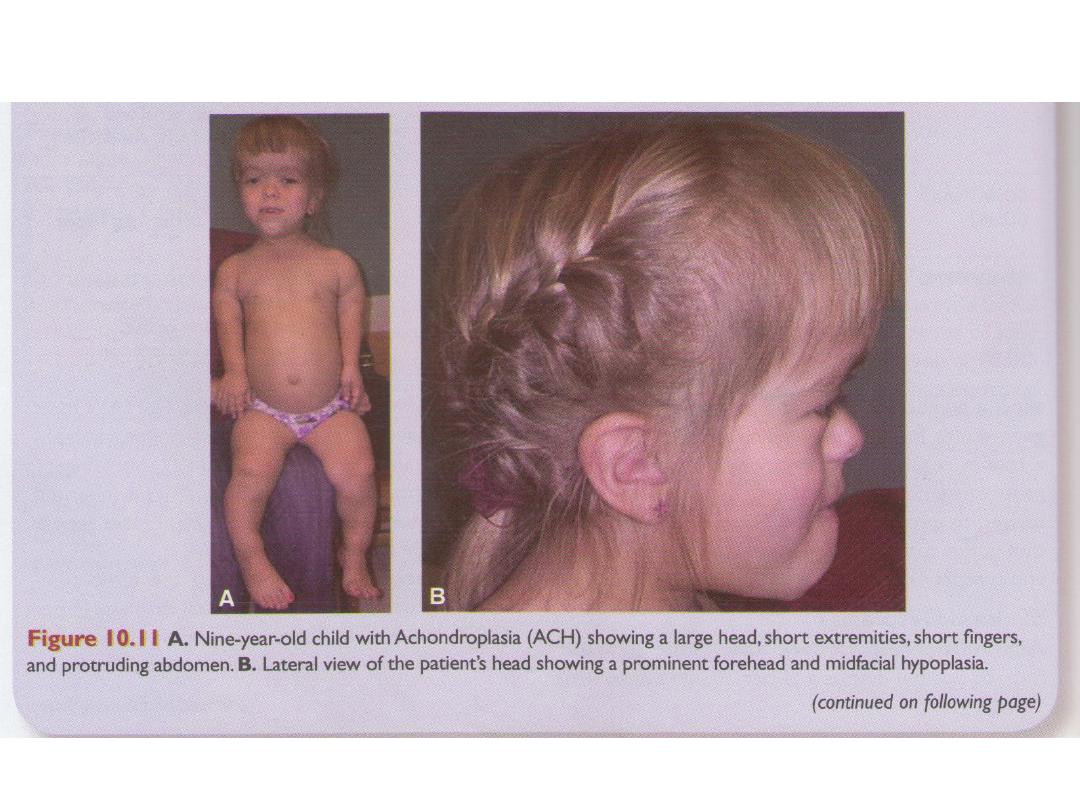

GENETIC CAUSES OF SKELETAL DYSPLASIAS
MUTATION IN FGFR3
Generalized Skeletal Dysplasia
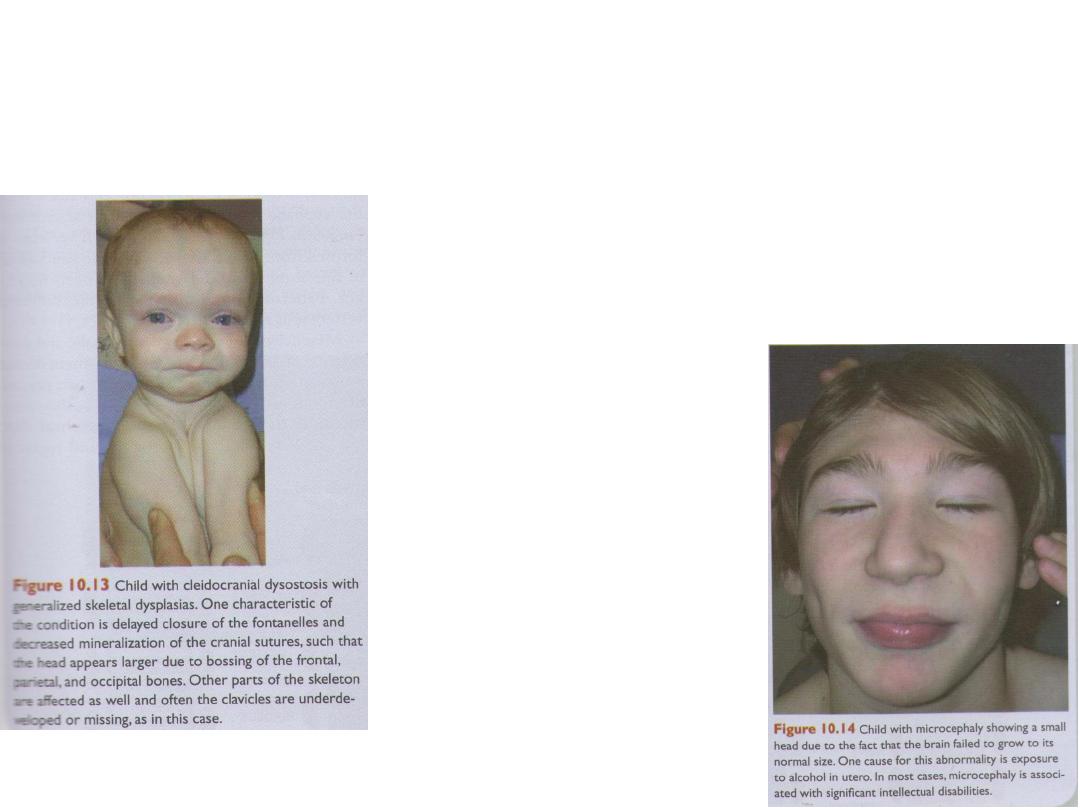
Cleidocranial dysostosis
generalized dysplasia of
osseus & dental tissue
• Acromegaly: is
caused by congenital
hyperpi-tuitarism
and excessive
production of growth
hormone.
• It is characterized by
disproportional
enlargement of the
face, hands, and feet.
• Sometimes, it causes
more symmetrical
excessive growth and
gigantism.
Microcephaly
• is usually an abnormality
in which the brain fails
to grow and the skull
fails to expand.
• Many children with
microcephaly are
severely retarded.
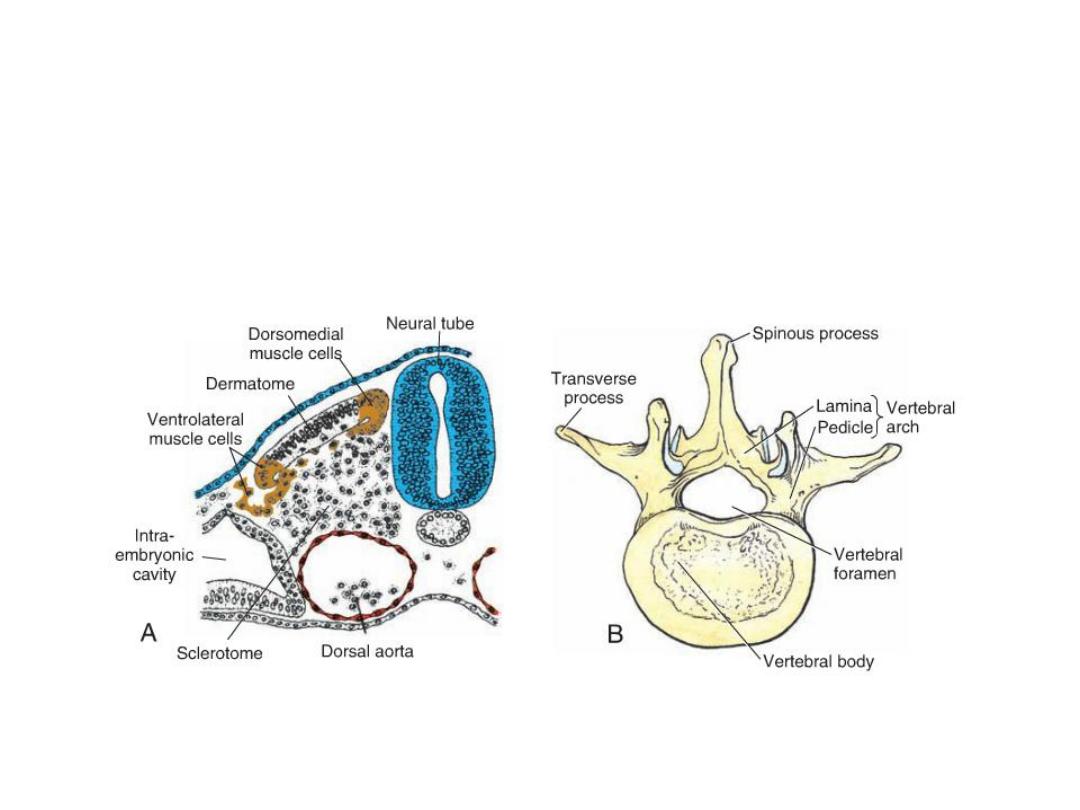
VERTEBRAE AND THE VERTEBRAL COLUMN
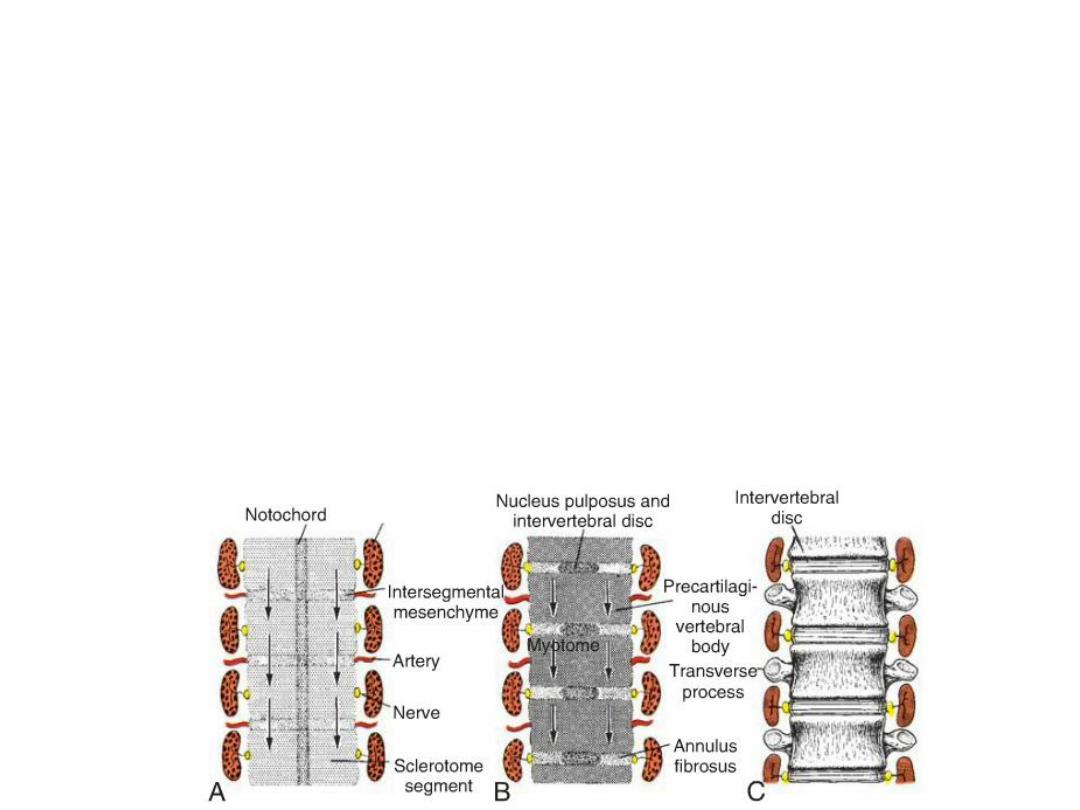
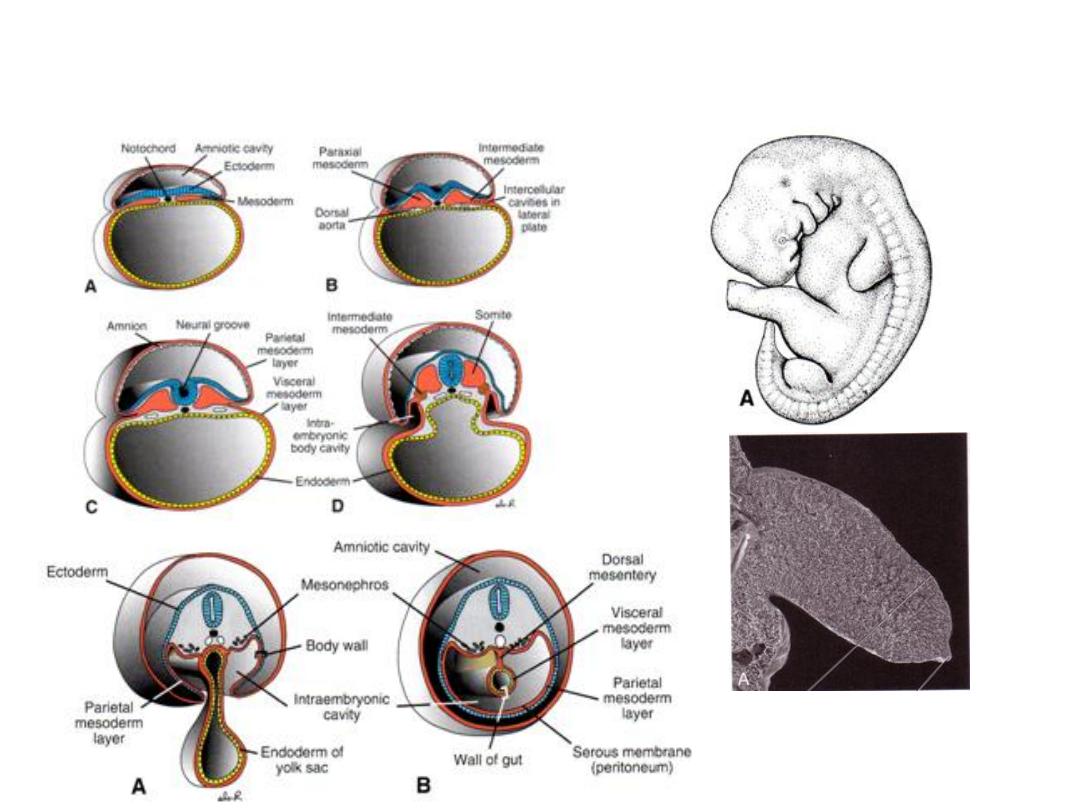
• Vertebrae form from the sclerotome portions of the somites, which are
derived from paraxial mesoderm.
• During the fourth week, sclerotome cells migrate around the spinal cord
and notochord to merge with cells from the opposing somite on the other
side of the neural tube.
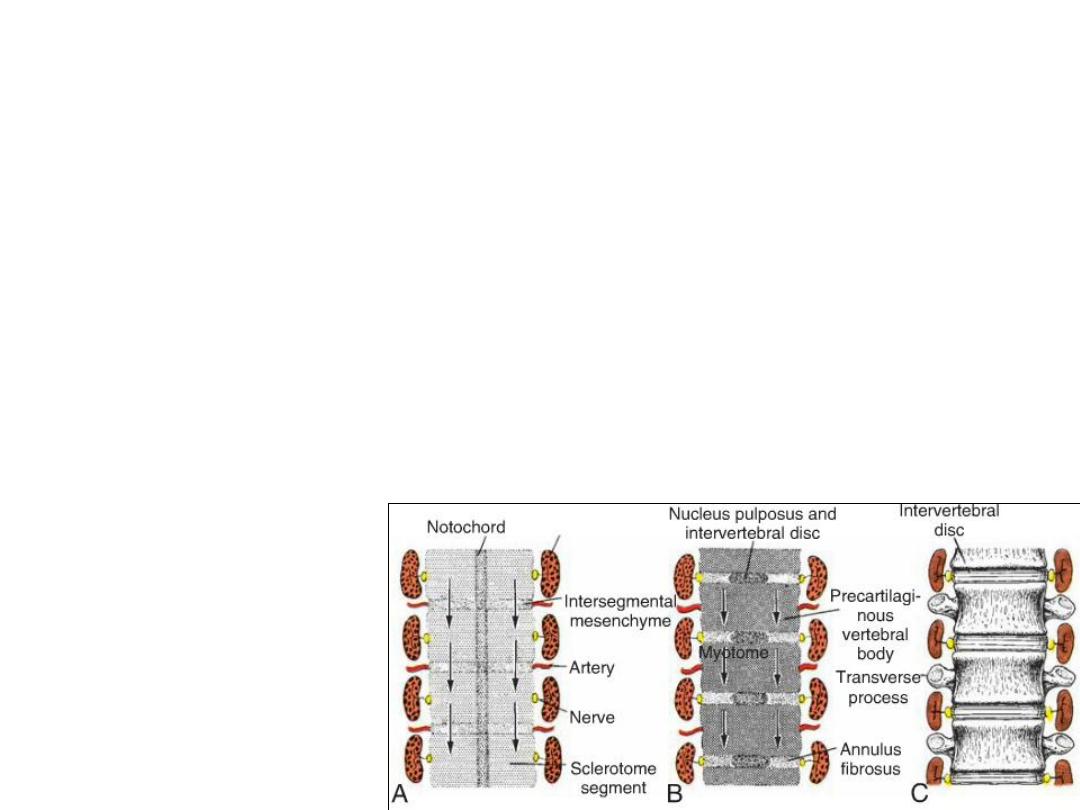
RESEGMENTATION
•Resegmentation occurs when the caudal half of each sclerotome
grows into and fuses with the cephalic half of each subjacent sclerotome.
• Thus, each vertebra is formed from the combination of the caudal
half of one somite and the cranial half of its neighbor.
• Patterning of the shapes of the different vertebrae is regulated by HOX
genes.
THE INTERVERTEBRAL DISC
• Mesenchymal cells between cephalic and caudal parts of the original
sclerotome segment do not proliferate but fill the space between two
precartilaginous vertebral bodies. In this way, they contribute to formation
of the inter-vertebral disc.
• The Inter-vertebral disc:
combination of
– Nucleus pulposus
– Anulus fibrosus
• Although the notochord regresses entirely in the region of the vertebral bodies, it
persists and enlarges in the region of the intervertebral disc. Here it contributes to
the nucleus pulposus, which is later surrounded by circular fibers of the annulus
fibrosus.
• Resegmentation of sclerotomes into definitive vertebrae causes the myotomes to
bridge the intervertebral discs, and this alteration gives them the capacity to move
the spine.
• For the same reason, intersegmental arteries, at first lying between the
sclerotomes, now pass mid-way over the vertebral bodies.
• Spinal nerves, however, come to lie near the intervertebral discs and leave the
vertebral column through the intervertebral foramina

Clinical Correlates
•
Vertebral Defects
•
The process of formation and rearrangement of segmental sclerotomes into definitive
vertebrae is complicated, and it is fairly common to have two successive vertebrae fuse
asymmetrically or have half a vertebra missing, a cause of scoliosis (lateral curving of the
spine)
•
Also, the number of vertebrae is frequently more or less than the norm. A typical example of
these abnormalities is found in patients with Klippel-Feil sequence.
•
These patients have fewer than normal cervical vertebrae, and often other vertebrae are
fused or abnormal in shape. These anomalies are usually associated with other defects.
•
One of the most serious vertebral defects is the result of imperfect fusion or nonunion of the
vertebral arches. Such an abnormality, known as Cleft vertebra (spina bifida), may involve
only the bony vertebral arches, leaving the spinal cord intact. In these cases, the bony defect
is covered by skin, and no neurological deficits occur (spina bifida occulta).
•
A more severe abnormality is spina bifida cystica, in which the neural tube fails to close,
vertebral arches fail to form, and neural tissue is exposed.
•
Any neurological deficits depend on the level and extent of the lesion.
•
This defect, which occurs in one per 1,000 births, may be prevented, in many cases, by
providing mothers with folic acid prior to conception.
•
Spina bifida can be detected prenatally by ultrasound, and if neural tissue is exposed,
amniocentesis can detect elevated levels of alpha fetoprotein in the amniotic fluid.
Mesenchyme forms in the parietal layer of the lateral plate mesoderm of the
body wall pelvic and shoulder girdles, limbs, and sternum.
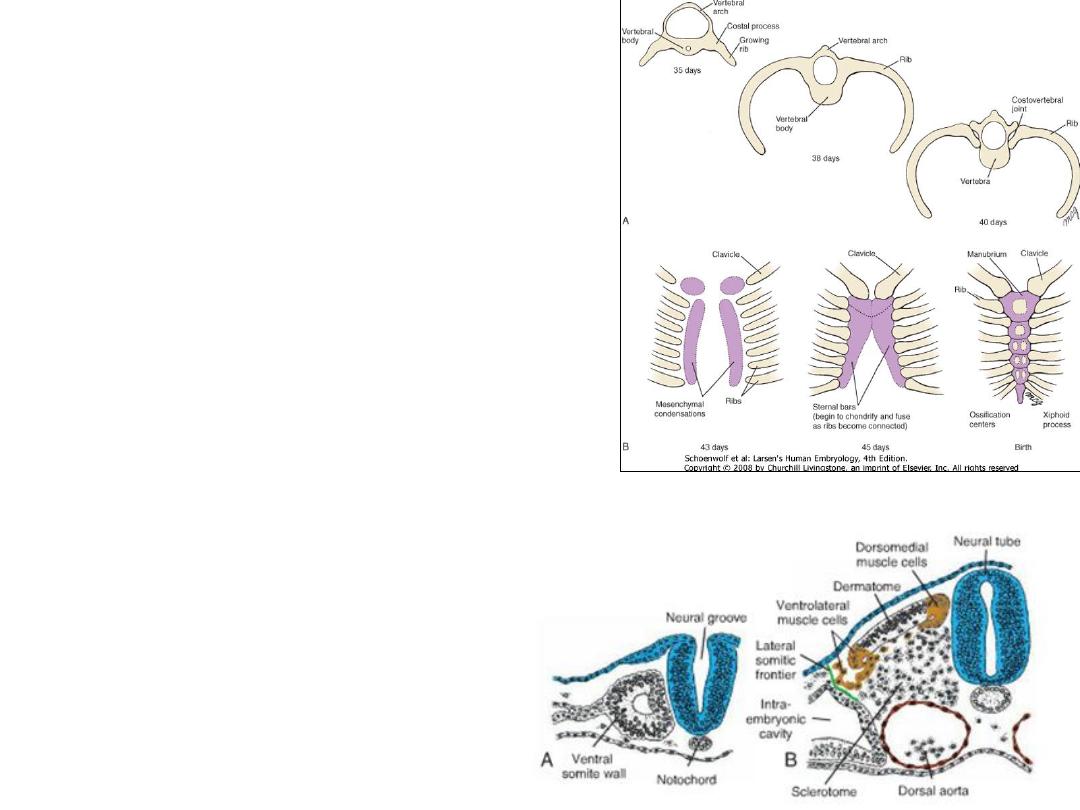
Ribs
The ribs:
The bony portion of each rib is derived
from sclerotome cells that remain in
the paraxial mesoderm and that grow
out from the costal processes of thoracic
vertebrae.
Costal cartilages are formed by
sclerotome cells that migrate across
the lateral somitic frontier into the
adjacent lateral plate mesoderm.
Sternum
The sternum develops independently
in the parietal layer of lateral plate
mesoderm in the ventral body wall.
Two sternal bands are formed in the
parietal (somatic) layer of lateral plate
mesodermon either side of the
midline, and these later fuse to form
cartilaginous models of the
manubrium, sternebrae, and xiphoid
process.

Clinical Correlates
• Rib Defects
• Occasionally extra ribs are formed, usually in the lumbar or cervical
regions.
• Cervical ribs are usually attached to the seventh cervical vertebra.
Because of its location, this type of rib may impinge on the brachial plexus
or the subclavian artery, resulting in varying degrees of anesthesia in the
limb.
