Chapter 3
First Week of
Development:
Ovulation to
Implantation
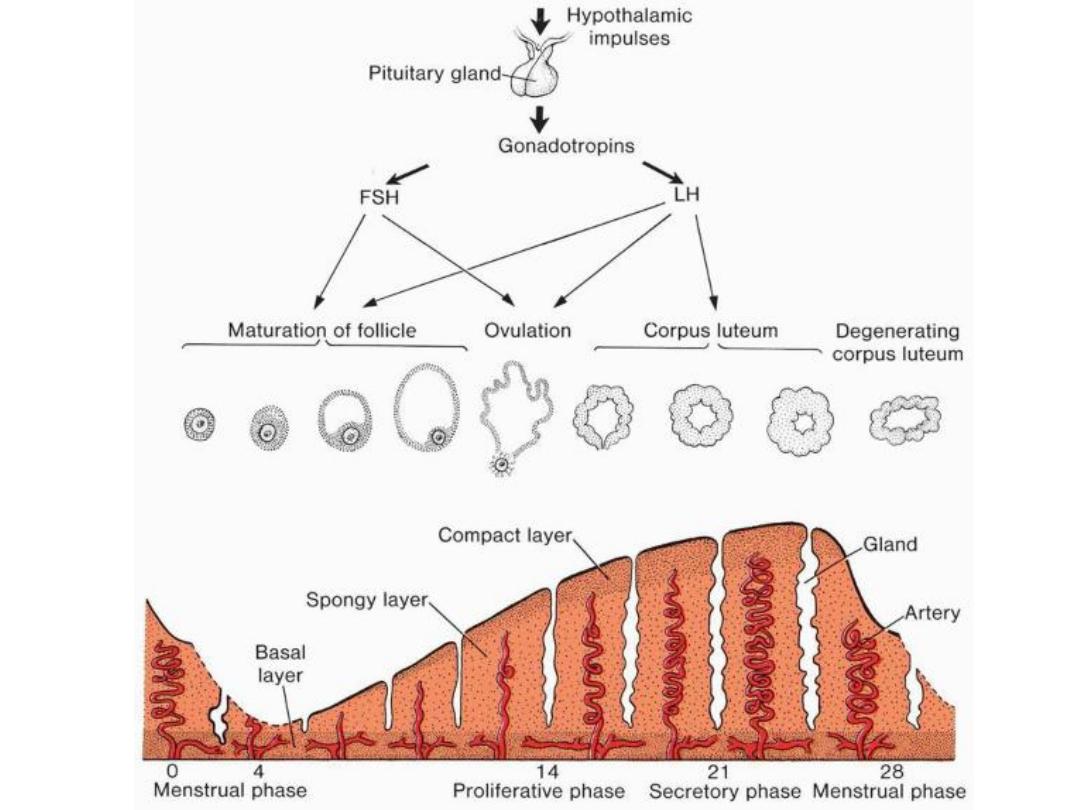
OVARIAN CYCLE
• At puberty,
• sexual cycles
• Hypothalamus: Gonadotropin releasing hormone (GnRH),
• pituitary gland
gonadotropins
,
– (follicle-stimulating hormone (
FSH
) and
– luteinizing hormone (
LH
)),
– stimulate and control cyclic changes in the ovary.
• 15 to 20 primary-stage (preantral)
follicles are stimulated to grow
under the influence of FSH. (FSH
rescues 15 to 20 of these cells
from a pool of continuously
forming primary follicles)
• only one of these follicles reaches
full maturity, and only one oocyte
is discharged;
• the others degenerate and
become
atretic
(the oocyte and
surrounding follicular cells
degenerate and are replaced by
connective tissue, forming a
corpus atreticum
)
FSH effect on granulosa cells
• FSH
also stimulates maturation of follicular (
granulosa
) cells surrounding the oocyt
• In turn, proliferation of these cells is mediated by
growth differentiation factor 9
, a
member of the
transforming growth factor-β (TGFβ) family
.
Formation & secretion of estrogens
• FSH stimulates theca interna cells & granulosa cells to secrete estrogens
during the follicular stage
• In cooperation,
theca interna and granulosa
cells produce
estrogens:
– Theca interna cells produce androstenedione & testosterone
– Granulosa cells convert these hormones to estrone & estradiol
ESTROGEN EFFECT
1.
The uterine endometrium enters the follicular or proliferative phase;
2.
Thinning of the cervical mucus occurs to allow passage of sperm; and
3.
The anterior lobe of the pituitary gland is stimulated to secrete LH.

LH surge
• At midcycle, there is an LH surge that:
• Elevates concentrations of maturation-
promoting factor, causing oocytes to
complete meiosis I and initiate meiosis
II;
• Stimulates production of progesterone
by follicular stromal cells (luteinization);
and
• Causes follicular rupture and ovulation.
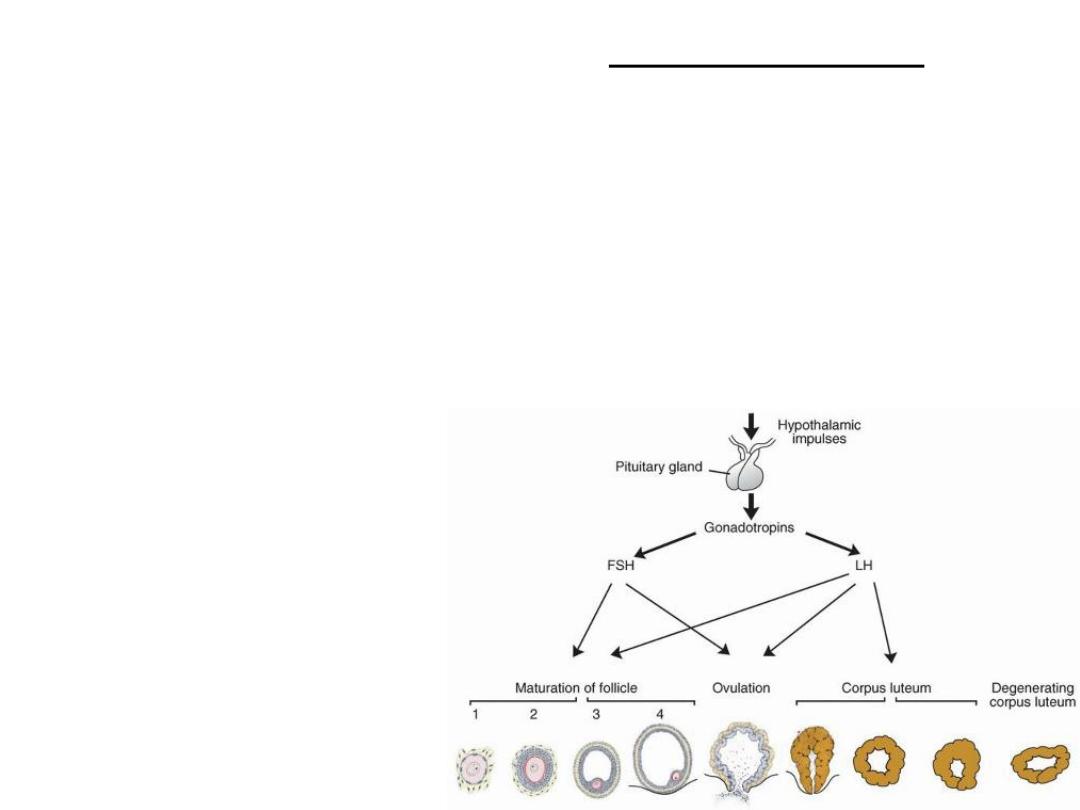
Stages of growth
of ovarian
follicles
Ovulation
• Seconday follicle: diameter of 25 mm.
• abrupt increase in LH
that causes the primary oocyte to complete meiosis I
and the follicle to enter the preovulatory stage.
• Meiosis II is also initiated, but the oocyte is arrested in metaphase
approximately 3 hours before ovulation.
• an avascular spot, the
stigma,
appears.
• LH increases
collagenase
activity
• Prostaglandincause
local muscular contractions in the ovarian wall.
• OVULATION
: release of oocyte, which together with its surrounding
granulosa cells from the region of the cumulus oophorus,
• coronaradiata
Clinical Correlates - Ovulation
• Mittelschmerz “middle pain” : mid-cycle pain
• Rise in basal temperature with ovulation.
• Failure of ovulation: low concentrations of gonadotropins: - administration
of drugs to stimulate gonadotropins
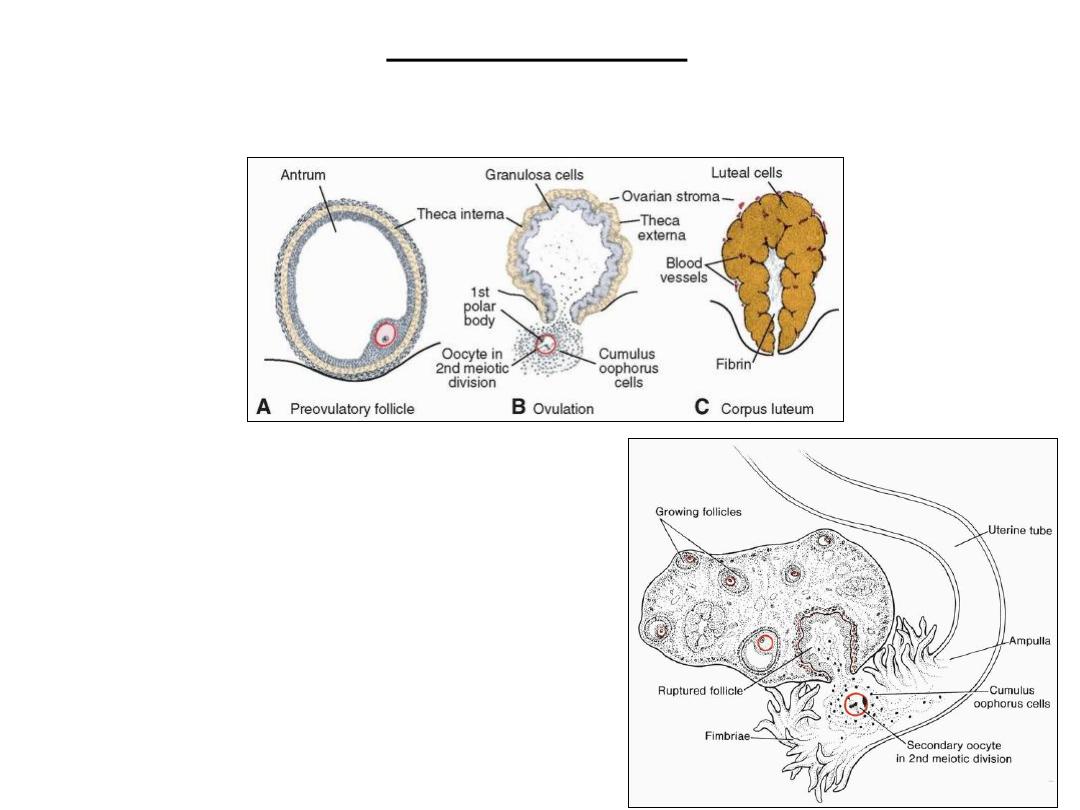
Corpus Luteum
• LH lutein cells in corpus luteum progesterone secretory phase of endometrium
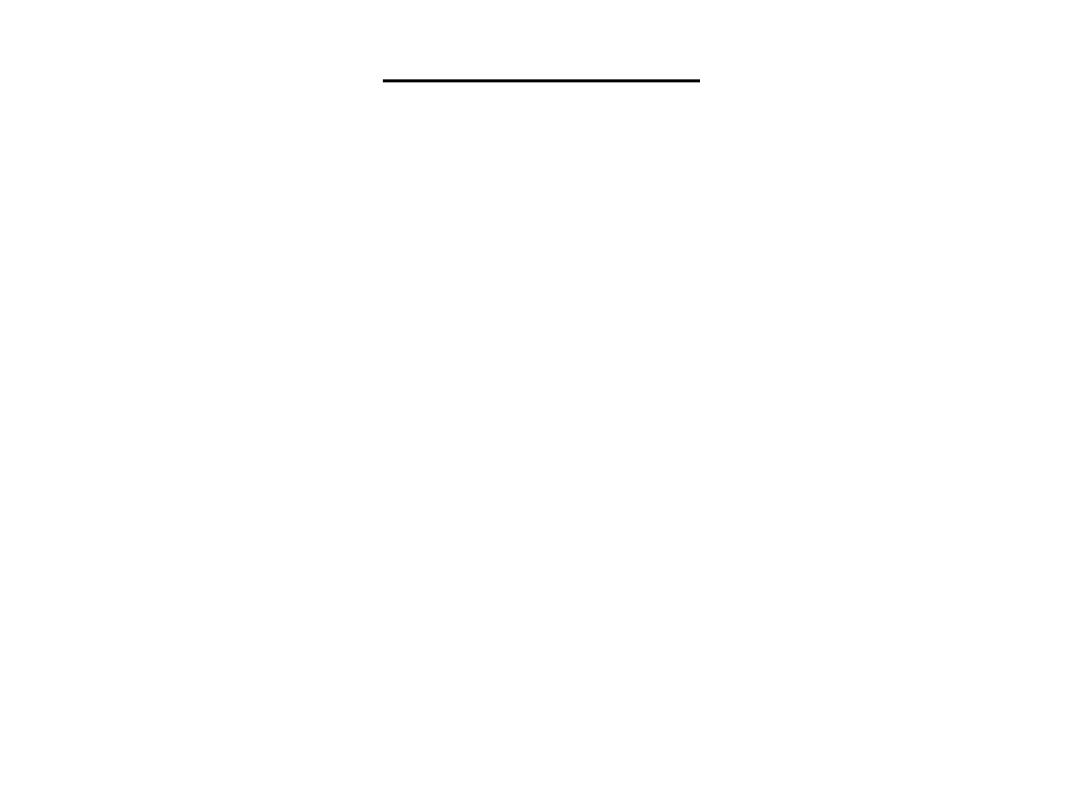
Oocyte transport
Corpus Albicans
• If fertilization does not occur, the corpus luteum reaches maximum development
approximately 9 days after ovulation, then degenerates
• forms a mass of fibrotic scar tissue, the
corpus albicans.
• Simultaneously, progesterone production decreases, precipitating menstrual
bleeding.
• If the oocyte is fertilized, degeneration of the corpus luteum is prevented by human
chorionic gonadotropin
(hCG),
a hormone secreted by the developing embryo.
• The corpus luteum continues to grow and forms the
corpus luteum of pregnancy
.
• secrete progesterone until the end of the fourth month;
• progesterone by the trophoblastic component of the placenta becomes adequate
for maintenance of pregnancy.
• Removal of the corpus luteum of pregnancy before the fourth month usually leads
to abortion.
Fertilization
• Fertilization, the
process by which male
and female gametes
fuse,
• occurs in the
ampullary region
of
the uterine tube.
• Spermatozoa may
remain viable in the
female reproductive
tract
for several days.
• Only 1% of sperm
deposited in the
vagina enter the
cervix, where they
may survive for many
hours.
• Spermatozoa
are not
able to fertilize the oocyte immediately upon arrival in the
female genital tract but must undergo
• (1) capacitation and
• (2) acrosome reaction
Capacitation
• is a period of conditioning
in the female reproductive tract
that in the
human lasts approximately
7 hours.
• During this time, a
glycoprotein coat and seminal plasma proteins
are
removed from the plasma membrane that overlies the acrosomal region
of the spermatozoa.
• Only capacitated sperm can pass through the corona cells and undergo the
acrosome reaction.
The acrosome reaction
• which occurs after binding to the zona
pellucida,
• is
induced by zona proteins.
• This reaction culminates in the release of
enzymes needed to penetrate the zona
pellucida, including
acrosin- and trypsin-
like substances
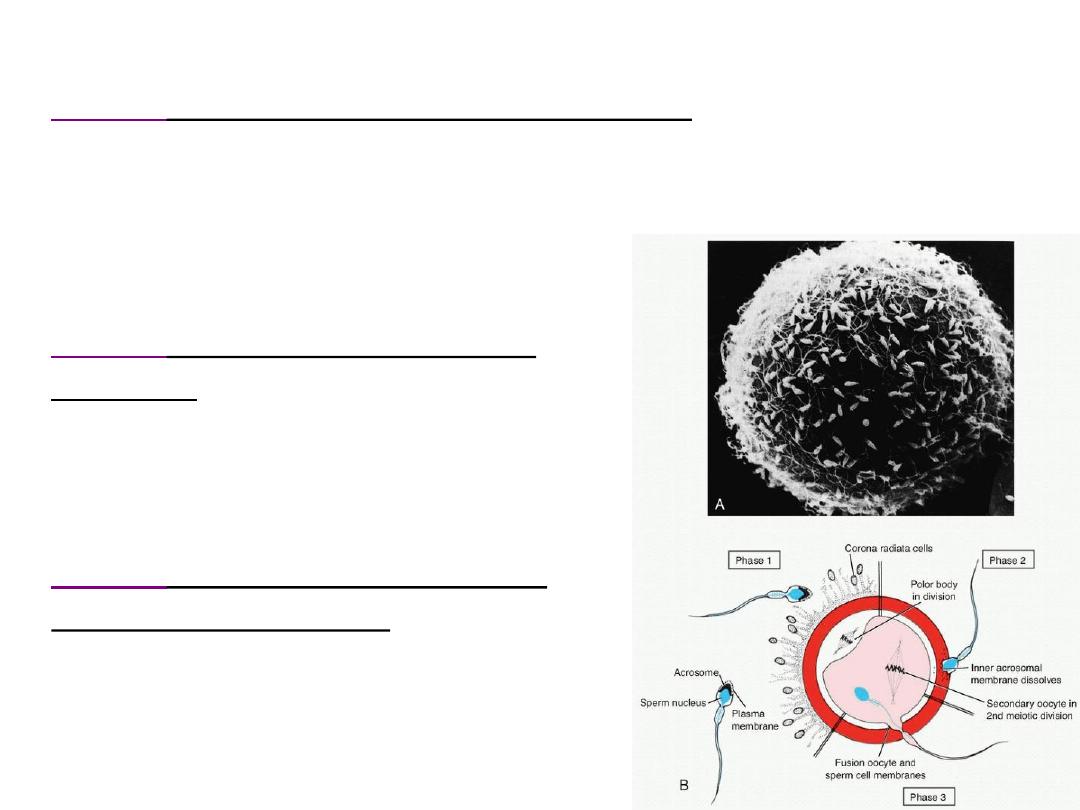
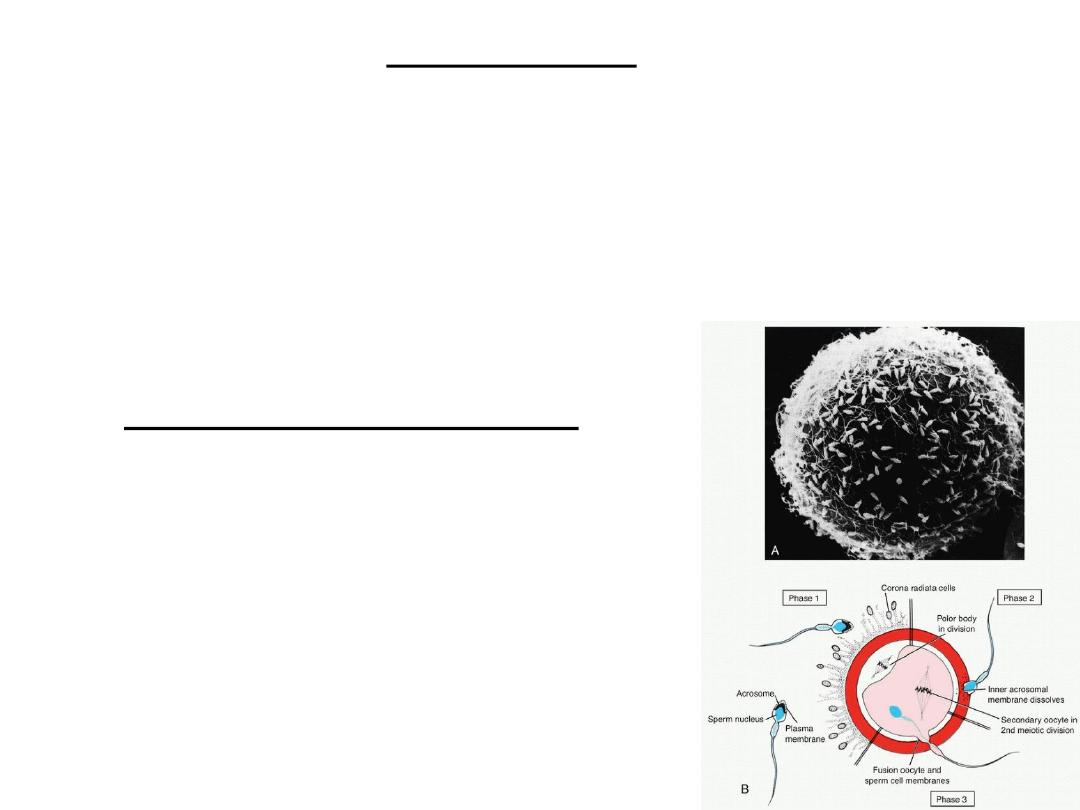
The phases of fertilization
• phase 1
, penetration of the corona radiata;
Capacitated sperm pass freely
Of the 200 to 300 million spermatozoa normally deposited in the female genital
tract, only 300 to 500 reach the site of fertilization.
Only one of these fertilizes the egg.
• phase 2
, penetration of the zona
pellucida;
Both binding and the acrosome reaction are
mediated by the ligand
ZP3
, a zona protein.
zona reaction
: to prevent sperm penetration
• phase 3
, fusion of the oocyte and
sperm cell membranes
In the human, both the head and tail of the
spermatozoon enter the cytoplasm of the oocyte,
but the plasma membrane is left behind on the
oocyte surface.
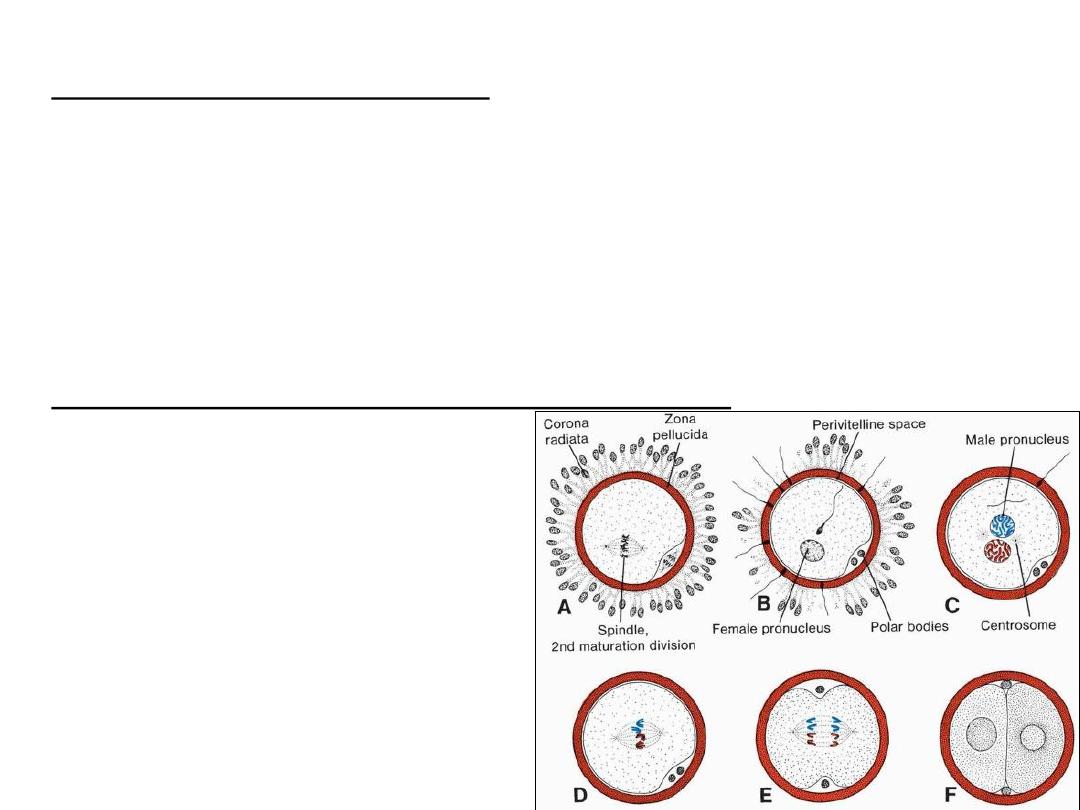
As soon as the spermatozoon has entered the oocyte, the egg responds in three ways:
• 1. Cortical and zona reactions
As a result of the release of cortical oocyte granules, which contain lysosomal
enzymes,
(1) the oocyte membrane becomes impenetrable to other spermatozoa, and
(2) the zona pellucida alters its structure and composition to prevent sperm binding
and penetration.
These reactions prevent
polyspermy
(penetration of more than one spermatozoon
into the oocyte).
• 2. Resumption of the second meiotic division.
Finishing of second meiotic division
immediately after entry of the
spermatozoon.
second polar body + definitive oocyte
Definitive oocyte chromosomes: (22 plus
X) in the
female pronucleus
The spermatozoon, meanwhile, moves
forward until it lies close to the female
pronucleus. Its nucleus becomes
swollen and forms the
male
pronucleus
• 3. Metabolic activation of the egg.
The activating factor is probably carried by the spermatozoon.
Activation encompasses the initial cellular and molecular events associated with early
embryogenesis.
Female & male pronuclei
• DNA replication in pronuclei.
• mitotic division.
• sister chromatids move to opposite poles
• Furrow dividing the cytoplasm into 2 parts
The main results of fertilization
• Restoration of the diploid number of chromosomes
, half from the father
and half from the mother. Hence, the zygote contains a new combination
of chromosomes different from both parents.
• Determination of the sex of the new individual
. An X-carrying sperm
produces a female (XX) embryo, and a Y-carrying sperm produces a male
(XY) embryo. Therefore, the
chromosomal sex of the embryo
is
determined at fertilization.
• Initiation of cleavage
. Without fertilization, the oocyte usually degenerates
24 hours after ovulation.
Clinical Correlates
Contraceptive Methods
• Barrier techniques
• The contraceptive pill
• Depo-Provera
• A male “pill”
• The intrauterine device (IUD)
• The drug RU-486 (mifepristone) causes abortion if it is administered within
8 weeks of the previous menses.
• Sterilization: Vasectomy and tubal ligation
Infertility causes
• Male infertility
: insufficient numbers of sperm and/or poor motility.
• Normally, the ejaculate has a volume of 2 to 6 mL, with as many as 100 million
sperm per milliliter.
• Men with 20 million sperm per milliliter or 50 million sperm per total ejaculate are
usually fertile.
• Infertility in a woman
may be due to a number of causes, including
– occluded uterine tubes (most commonly caused by pelvic inflammatory disease),
– hostile cervical mucus,
– immunity to spermatozoa,
– absence of ovulation, and others.
Assisted Reproductive Technology (ART).
• In vitro fertilization (IVF)
– Follicle growth in the ovary is stimulated by administration of gonadotropins.
– Oocytes are recovered by laparoscopy from ovarian follicles with an aspirator just
before ovulation when the oocyte is in the late stages of the first meiotic division.
– The egg is placed in a simple culture medium, and sperm are added immediately.
– Fertilized eggs are monitored to the eight-cell stage and then placed in the uterus
to develop to term.
• To increase chances of a successful pregnancy, 4 or 5 ova are collected, fertilized,
and placed in the uterus. This approach sometimes leads to multiple births.
intracytoplasmic sperm injection (ICSI).
• Severe male infertility, in which the ejaculate contains very few live sperm
(oligozoospermia) or even no live sperm (azoospermia), can be overcome
using
intracytoplasmic sperm injection (ICSI).
• With this technique, a single sperm, which may be obtained from any
point in the male reproductive tract, is injected into the cytoplasm of the
egg to cause fertilization.
• The technique carries an increased risk for fetuses to have Y chromosome
deletions but no other chromosomal abnormalities.
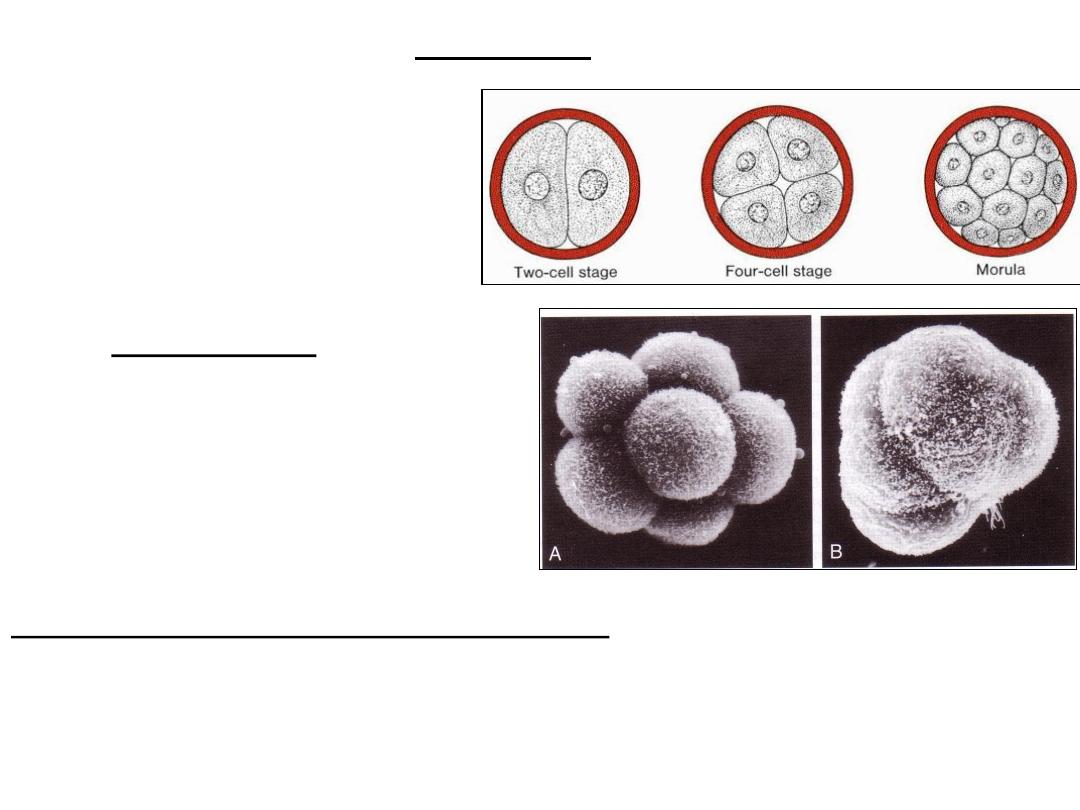
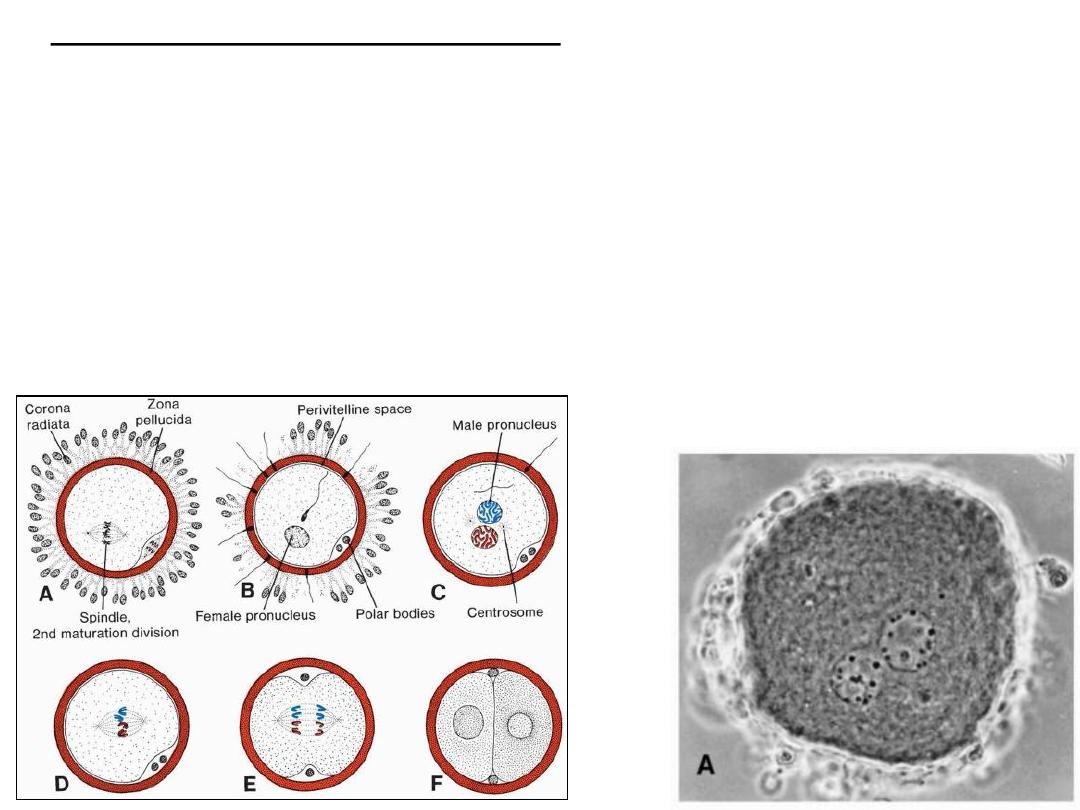
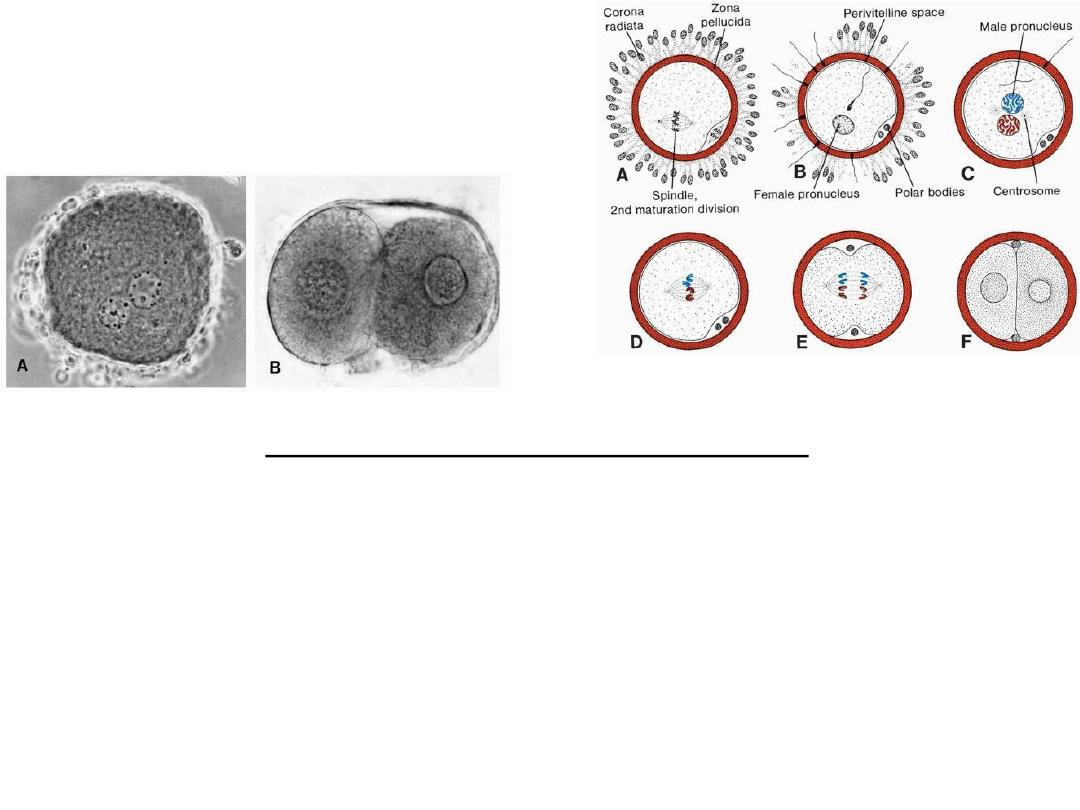
Cleavage
• series of mitotic divisions,
increasing the numbers of cells,
blastomeres
compaction
• After the third cleavage,
•
blastomeres
maximize their contact
with each other, forming a compact
ball of cells held together by
tight
junctions
Organization of cells in the morula
• compacted embryo divide again to form a 16-cell morula (mulberry).
• Inner cell mass, embryo proper
• Outer cell mass, trophoblast (placenta).
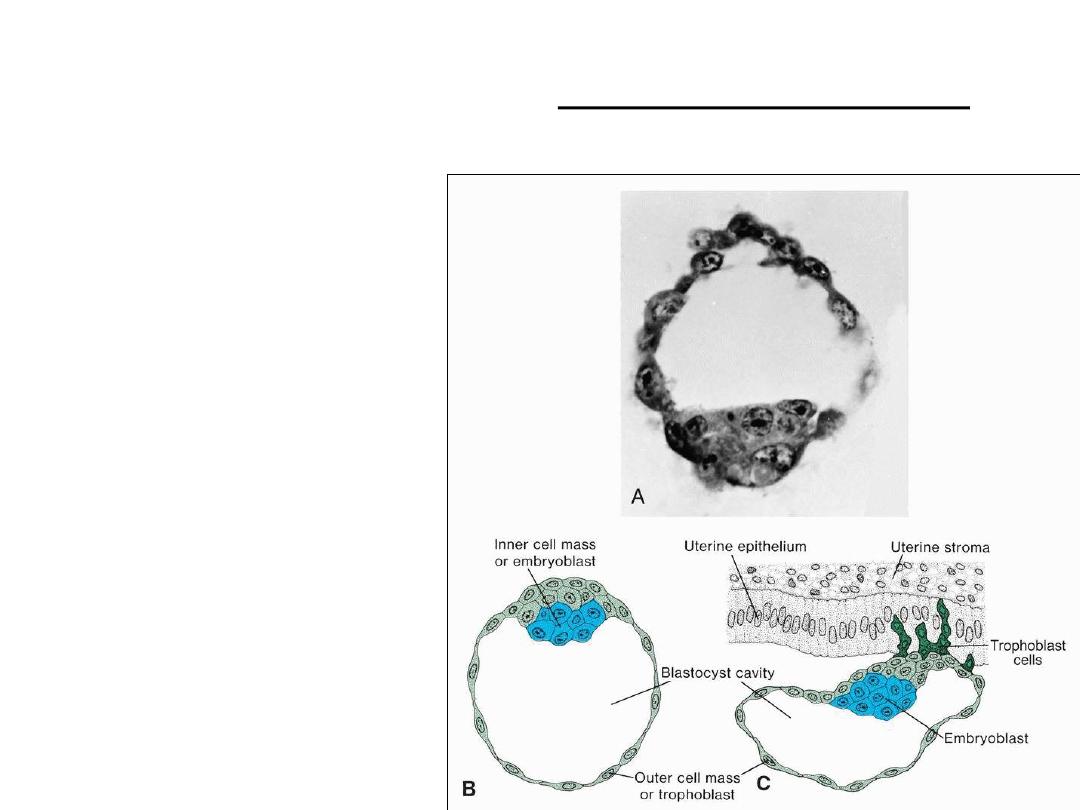
Blastocyst formation
• Blastocyst = blastocele,
• Inner cell mass=embryoblast
• Outer cell mass=trophoblast
• The zona pellucida has
disappeared,
• Day 6: attachment &
Penetration of uterine mucosa
by trophoblastic cells
• L-selectin on trophoblast cells
and its carbohydrate receptors
on the uterine epithelium
mediate initial attachment of
the blastocyst to the uterus.
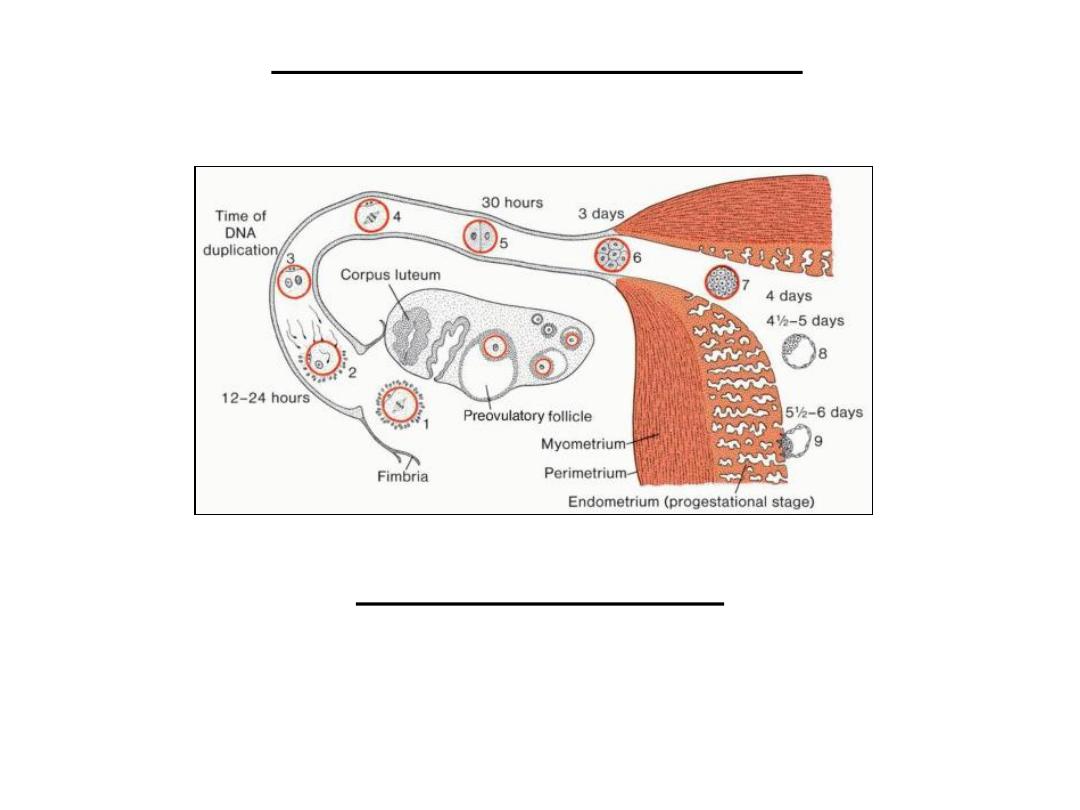
First week of development
• Human zygote morula blastocyst beginning of implantation in uterine
mucosa
Clinical Correlates
• Embryonic Stem Cells
• Adult Stem Cells
• Abnormal Zygotes
• 50% of pregnancies end in spontaneous abortion
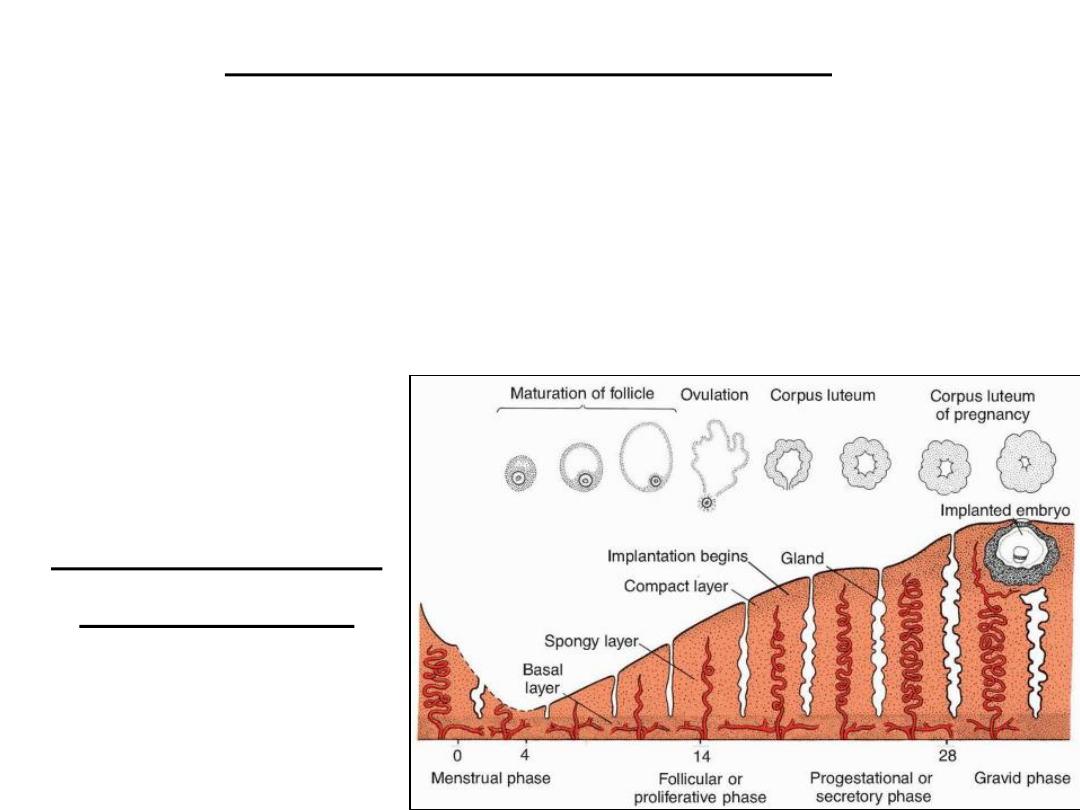
Uterus at time of implantation
• Wall of uterus:
– Endometrium
– Myometrium
– Perimetrium
• The menstrual cycle: phases of the endometriu:
– Proliferative phase
– Secretory phase
– Menstrual phase
Cyclic changes in
endometrium