
loose connective tissue, but the muscle bundles fuse with one another at many
each bundle but more rapidly along the length of the bundle than sideways.
ment of ions from one muscle cell to the next. Therefore, electrical signals that
Within each bundle, the muscle fibers are electrically connected with one
, they extend
circular muscle layer
longitudinally down the intestinal tract; in the
, the bundles extend
longitudinal muscle layer
many as 1000 parallel fibers. In the
and 2 to 10 micrometers in diameter, and they are arranged in bundles of as
The individual smooth
the following.
tions of this chapter. The specific characteristics of smooth muscle in the gut are
in Chapter 8, which should be reviewed as a background for the following sec-
The general characteristics of smooth muscle and its function are discussed
the different layers of smooth muscle.
deeper layers of the mucosa. The motor functions of the gut are performed by
, lie in the
tion, sparse bundles of smooth muscle fibers, the
. In addi-
, (4) the
circular muscle layer
, (3) a
layer
, (2) a
lowing layers from outer surface inward: (1) the
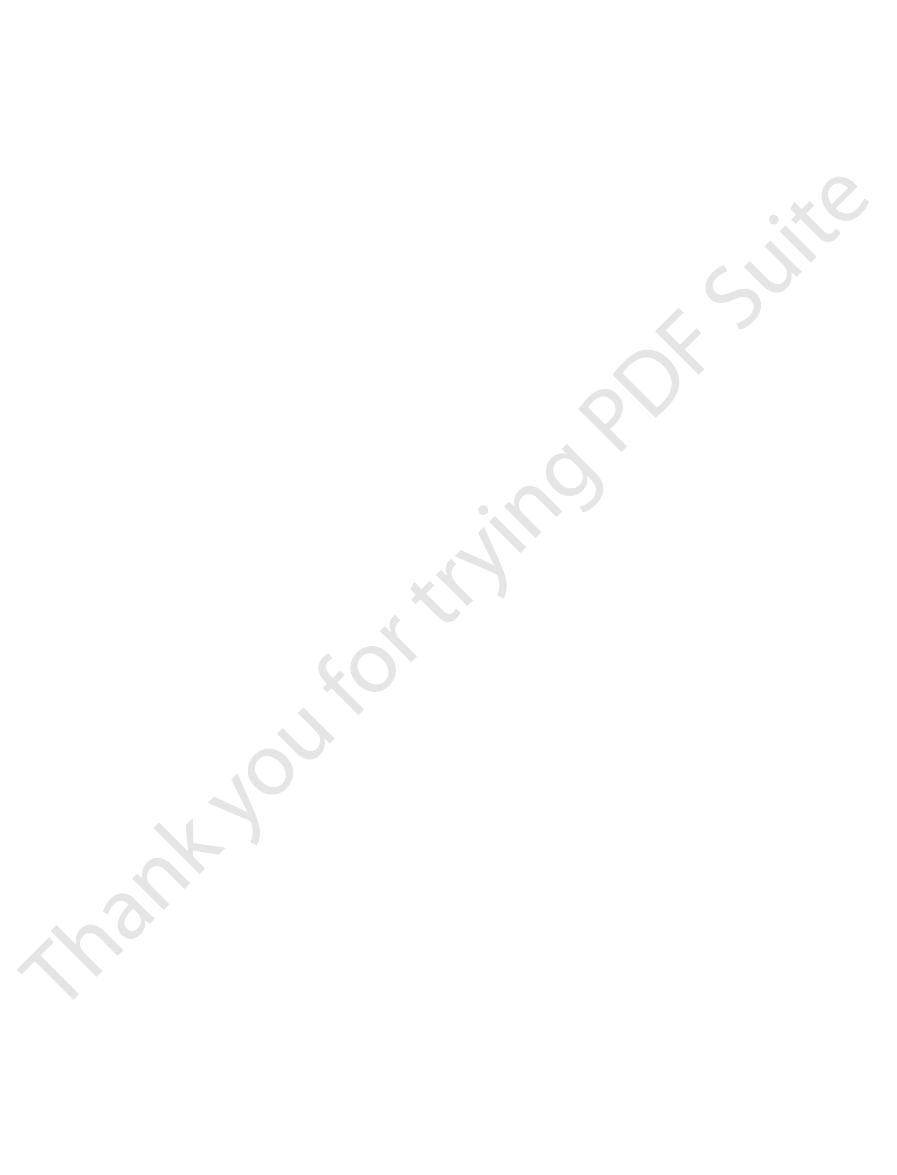
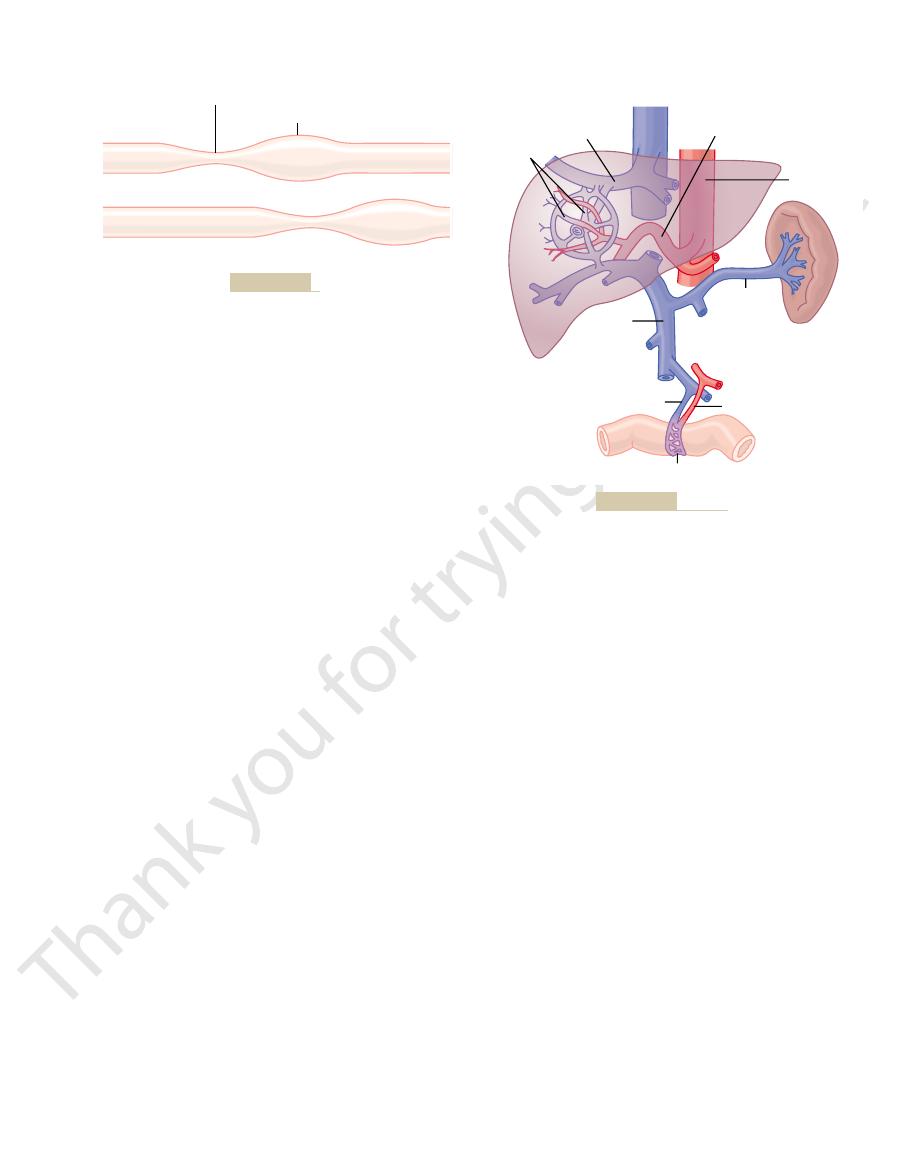
Figure 62–2 shows a typical cross section of the intestinal wall, including the fol-
Physiologic Anatomy of the Gastrointestinal Wall
General Principles of Gastrointestinal Motility
ciples of function in the entire alimentary tract; in the following chapters, we
absorption, such as the small intestine. In this chapter, we discuss the basic prin-
temporary storage of food, such as the stomach; and others to digestion and
cific functions: some to simple passage of food, such as the esophagus; others to
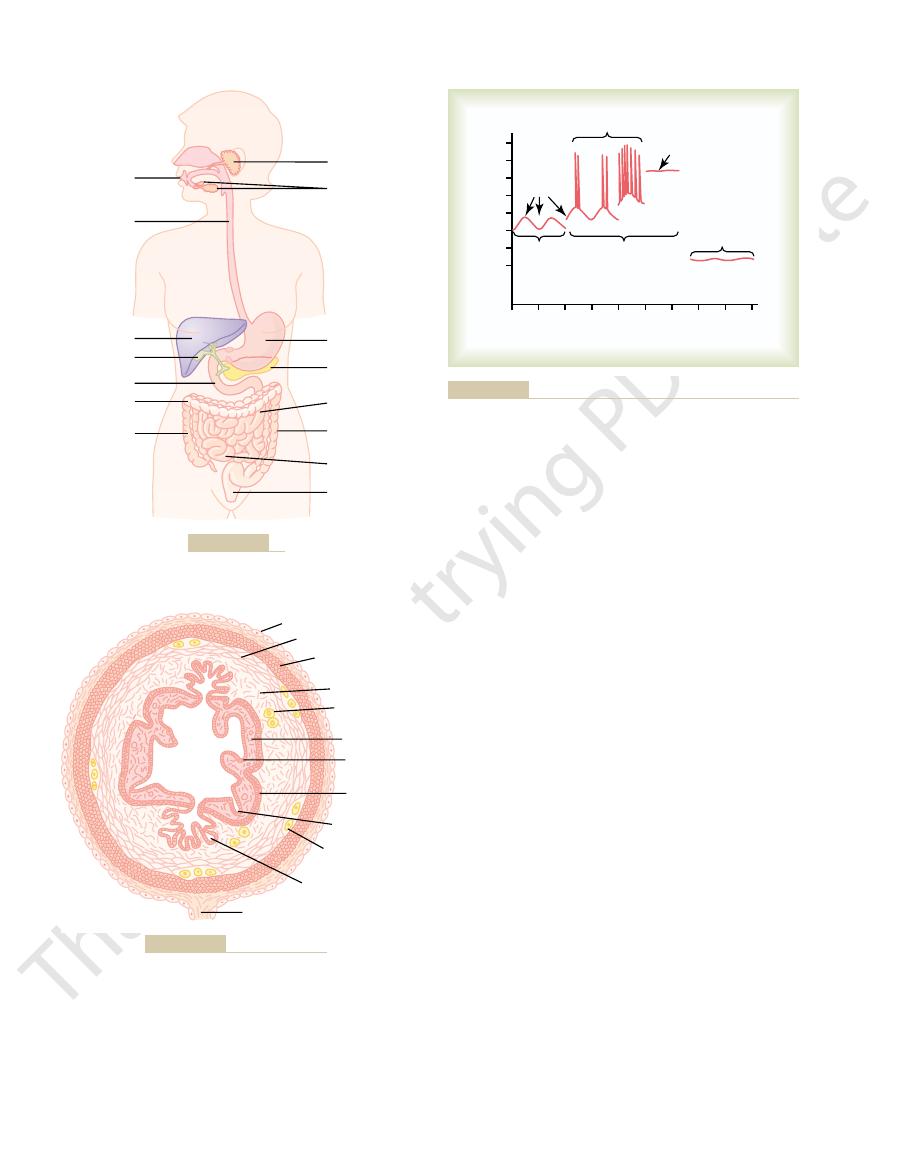
Figure 62–1 shows the entire alimentary tract. Each part is adapted to its spe-
(5) control of all these functions by local, nervous, and hormonal systems.
organs to carry away the absorbed substances; and
various electrolytes, and digestive products; (4)
and digestion of the food; (3) absorption of water,
the alimentary tract; (2) secretion of digestive juices
tinual supply of water, electrolytes, and nutrients. To
The alimentary tract provides the body with a con-
Motility, Nervous Control, and
C
H
A
P
T
E
R
6
2
771
General Principles of
Gastrointestinal Function—
Blood Circulation
achieve this requires (1) movement of food through
circulation of blood through the gastrointestinal
will discuss the specific functions of different segments of the tract.
serosa
longitudinal muscle
submucosa, and (5) the mucosa
mucosal muscle
Gastrointestinal Smooth Muscle Functions as a Syncytium.
muscle fibers in the gastrointestinal tract are 200 to 500 micrometers in length
around the gut.
another through large numbers of gap junctions that allow low-resistance move-
initiate muscle contractions can travel readily from one fiber to the next within
Each bundle of smooth muscle fibers is partly separated from the next by
pletely understood, although they appear to be caused
The precise cause of the slow waves is not com-
the ileum 8 to 9 per minute.
minute, of the duodenum about 12 per minute, and of
terminal ileum. Therefore, the rhythm of contraction
much as 12 in the duodenum, and about 8 or 9 in the
per minute: about 3 in the body of the stomach, as
15 millivolts, and their frequency ranges in different
potential. Their intensity usually varies between 5 and
slow, undulating changes in the resting membrane
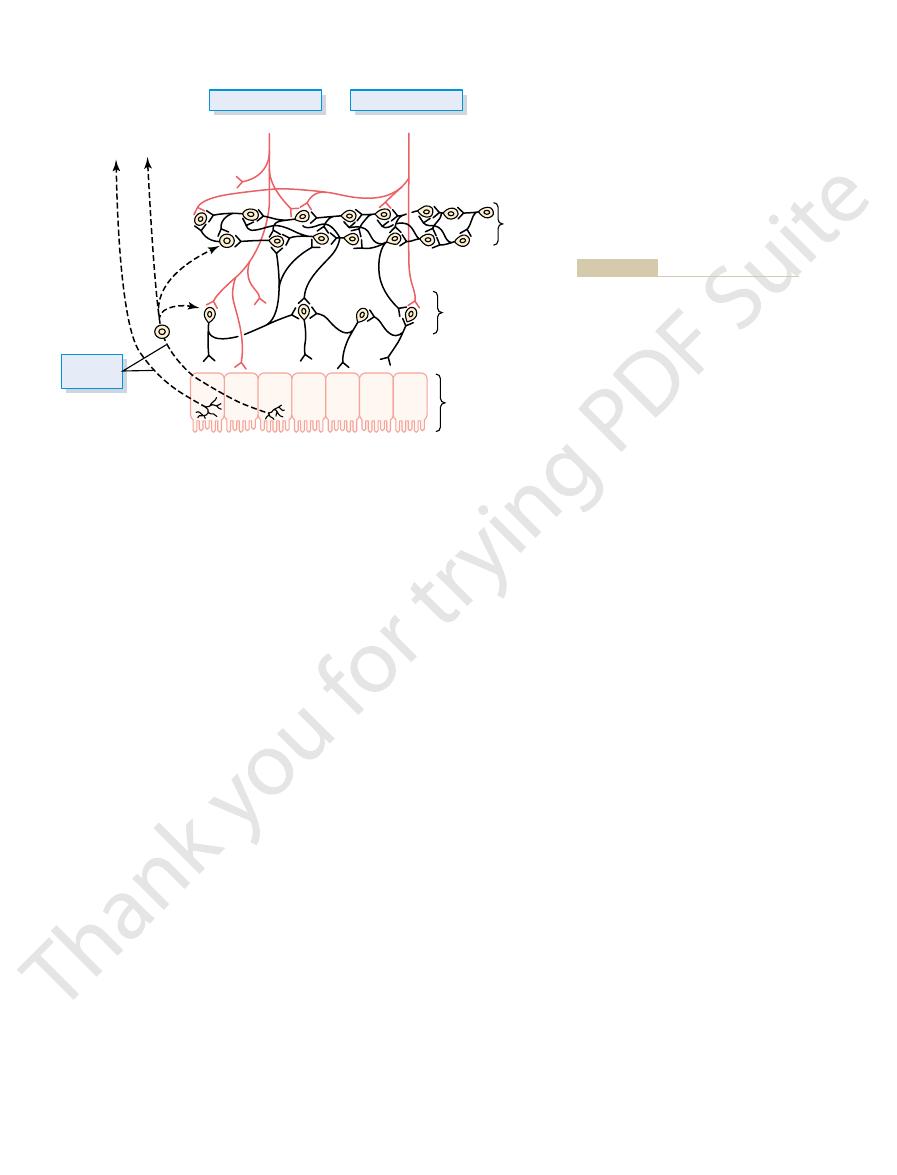
Figure 62–3, are not action potentials. Instead, they are
muscle membrane potential. These waves, shown in
the frequency of so-called “slow waves” of smooth
rhythmically, and this rhythm is determined mainly by
Slow Waves.
muscle can be made to change to different levels, and
in Figure 62–3. In addition, the voltage of the resting
, both of which are shown
slow waves
This activity has two basic types of electrical waves: (1)
activity along the membranes of the muscle fibers.
excited by almost continual slow, intrinsic electrical
The smooth muscle of the gastrointestinal tract is
Electrical Activity of Gastrointestinal
dinal and circular muscle layers, so that excitation of
Also, a few connections exist between the longitu-
on the excitability of the muscle; sometimes it stops
tions in the muscle. The distance that it travels depends
within the muscle mass, it generally travels in all direc-
that is, when an action potential is elicited anywhere
Therefore, each muscle layer functions as a
a branching latticework of smooth muscle bundles.
points, so that in reality each muscle layer represents
772
Unit XII
Gastrointestinal Physiology
syncytium;
after only a few millimeters and at other times it
travels many centimeters or even the entire length and
breadth of the intestinal tract.
one of these layers often excites the other as well.
Smooth Muscle
and (2) spikes
membrane potential of the gastrointestinal smooth
this too can have important effects in controlling
motor activity of the gastrointestinal tract.
Most gastrointestinal contractions occur
parts of the human gastrointestinal tract from 3 to 12
of the body of the stomach usually is about 3 per
Parotid gland
Mouth
Salivary glands
Esophagus
Liver
Gallbladder
Duodenum
Ascending
colon
Transverse
colon
Stomach
Pancreas
Jejunum
Descending
colon
Ileum
Anus
Alimentary tract.
Figure 62–1
Serosa
Circular muscle
Longitudinal
muscle
Submucosa
Mucosa
Meissner's
nerve plexus
Epithelial
lining
Mucosal
muscle
Mucosal gland
Submucosal gland
Mesentery
Myenteric nerve
plexus
Typical cross section of the gut.
Figure 62–2
24
30
36
42
48
54
0
6
12
18
Membrane potential (millivolts)
-
70
-
60
-
50
-
40
-
30
-
20
-
10
0
Spikes
Depolarization
Stimulation by
1. Norepinephrine
2. Sympathetics
Stimulation by
1. Stretch
2. Acetylcholine
3. Parasympathetics
Resting
Hyperpolarization
Slow
waves
Seconds
Seconds
ization, all of which occur under different physiologic conditions
Figure 62–3
Membrane potentials in intestinal smooth muscle. Note the slow
waves, the spike potentials, total depolarization, and hyperpolar-
of the intestine.
. It lies entirely
The gastrointestinal tract has a nervous system all its
Enteric Nervous System
Gastrointestinal Function—
Neural Control of
details of these mechanisms are still unclear.
associated with changes in membrane potential. The
without causing action potentials. A third cause of
other times, tonic contraction is caused by hormones
frequency, the greater the degree of contraction. At
Tonic contraction is sometimes caused by con-
intensity but continues.
The tonic contraction often increases or decreases in
waves but often lasting several minutes or even hours.
mical contractions. Tonic contraction is continuous, not
Tonic Contraction of Some Gastrointestinal Smooth Muscle.
generated at the peaks of the slow waves, that signifi-
contraction. Instead, it is during the spike potentials,
the smooth muscle fiber (only sodium ions). Therefore,
The slow waves do not cause calcium ions to enter
myosin filaments and the actin filaments, thereby
mechanism, activate the myosin filaments in the fiber,
calcium ions, acting through a calmodulin control
into the muscle fiber. As explained in Chapter 8,
endings.
tial more negative—that is, hyperpolarize the mem-
choline at their endings, and (4) stimulation by several
, (3) stimula-
acetylcholine
muscle, (2) stimulation by
stretching
Factors that depolarize the membrane—that is,
, the fibers become less excitable.
tial becomes more negative, which is called
muscle fibers become more excitable. When the poten-
of the membrane, the
this level. When the potential becomes less negative,
56 millivolts, but multiple factors can change
conditions, the resting membrane potential averages
membrane potential also can change. Under normal
addition to the slow waves and spike potentials, the
Changes in Voltage of the Resting Membrane Potential.
as we discuss shortly.
tion of the action potentials. Also, the movement of
fibers. The slowness of opening and closing of the
These channels are much slower to open and close
calcium-sodium channels
ferent; they allow especially large numbers of calcium
In gastrointestinal smooth muscle fibers, the channels
through sodium channels to the interior of the fibers.
generated. In nerve fibers, the action potentials are
as 10 to 20 milliseconds.
nerve fibers, each gastrointestinal spike lasting as long
The spike potentials last 10 to 40 times as long in gas-
usually ranging between 1 and 10 spikes per second.
the greater the frequency of the spike potentials,
these peaks. The higher the slow wave potential rises,
40 millivolts, spike potentials appear on
60 millivolts).Thus, note in Figure 62–3 that each time
potentials. They occur automatically when the resting
The spike potentials are true action
potentials, and the spike potentials in turn actually
. Instead, they
except perhaps in the stomach
The slow waves usually do not by themselves cause
erate slow wave activity.
undergo cyclic changes in membrane potential due
to smooth muscle cells. The interstitial cells of Cajal
the smooth muscle layers, with synaptic-like contacts
for smooth muscle cells. These interstitial cells form a
, that are believed to act as
cells and specialized cells, called the
General Principles of Gastrointestinal Function—Motility, Nervous Control, and Blood Circulation
Chapter 62
773
by complex interactions among the smooth muscle
interstitial cells of
Cajal
electrical pacemakers
network with each other and are interposed between
to unique ion channels that periodically open and
produce inward (pacemaker) currents that may gen-
muscle contraction in most parts of the gastrointesti-
nal tract,
mainly excite the appearance of intermittent spike
excite the muscle contraction.
Spike Potentials.
membrane potential of the gastrointestinal smooth
muscle becomes more positive than about
-40 milli-
volts (the normal resting membrane potential in the
smooth muscle fibers of the gut is between
-50 and
-
the peaks of the slow waves temporarily become more
positive than
-
trointestinal muscle as the action potentials in large
Another important difference between the action
potentials of the gastrointestinal smooth muscle and
those of nerve fibers is the manner in which they are
caused almost entirely by rapid entry of sodium ions
responsible for the action potentials are somewhat dif-
ions to enter along with smaller numbers of sodium
ions and therefore are called
.
than are the rapid sodium channels of large nerve
calcium-sodium channels accounts for the long dura-
large amounts of calcium ions to the interior of the
muscle fiber during the action potential plays a special
role in causing the intestinal muscle fibers to contract,
In
baseline voltage level of the smooth muscle resting
about
-
which is called depolarization
hyperpo-
larization
make it more excitable—are (1)
of the
tion by parasympathetic nerves that secrete acetyl-
specific gastrointestinal hormones.
Important factors that make the membrane poten-
brane and make the muscle fibers less excitable—are
(1) the effect of norepinephrine or epinephrine on the
fiber membrane and (2) stimulation of the sympathetic
nerves that secrete mainly norepinephrine at their
Calcium Ions and Muscle Contraction.
Smooth muscle con-
traction occurs in response to entry of calcium ions
causing attractive forces to develop between the
causing the muscle to contract.
the slow waves by themselves usually cause no muscle
cant quantities of calcium ions do enter the fibers and
cause most of the contraction.
Some smooth muscle of the gastrointestinal tract
exhibits tonic contraction as well as or instead of rhyth-
associated with the basic electrical rhythm of the slow
tinuous repetitive spike potentials—the greater the
or other factors that bring about continuous partial
depolarization of the smooth muscle membrane
tonic contraction is continuous entry of calcium ions
into the interior of the cell brought about in ways not
own called the enteric nervous system
intestine. For instance, many sensory signals originate
plexus, is mainly concerned with controlling function
, in contrast to the myenteric
The
, which
denum, and the
pyloric sphincter
gastrointestinal tract, such as the
or some other inhibitory peptide. The resulting
transmitter, possibly
; their fiber endings secrete an inhibitory
The
ment of the gut peristaltic waves.
waves along the gut wall, causing more rapid move-
(2) increased intensity of the rhythmical contractions,
increased tonic contraction, or “tone,” of the gut wall,
plexus is stimulated, its principal effects are (1)
muscle activity along the length of the gut. When this
smooth muscle, it is concerned mainly with controlling
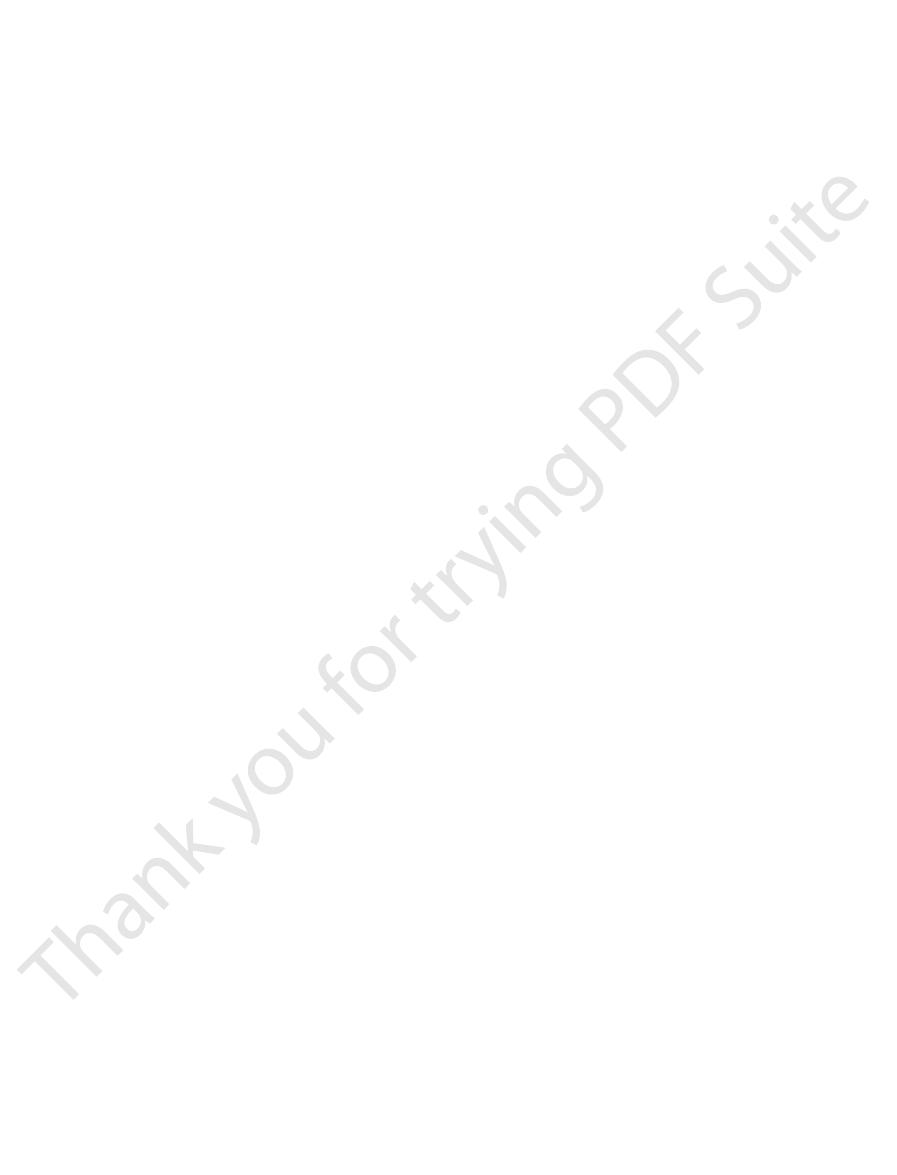
this chain is shown in Figure 62–4.
entire length of the gastrointestinal tract. A section of
The
Differences Between the Myenteric
the way to the brain stem. These sensory nerves can
(2) to the spinal cord, and (3) in the vagus nerves all
plexuses of the enteric system, as well as (1) to the pre-
Also shown in Figure 62–4 are sensory nerve
discuss later.
enhance or inhibit gastrointestinal functions, as we
pendently of these extrinsic nerves, stimulation by the
enteric nervous system can function on its own, inde-
the myenteric and submucosal plexuses. Although the
Note especially in Figure 62–4 the extrinsic sympa-
flow.
testinal movements, and the submucosal plexus con-
The myenteric plexus controls mainly the gastroin-
two plexuses are also shown in Figure 62–4.
The nervous connections within and between these
, that lies in the submucosa.
, and (2) an inner plexus, called the
Auerbach
layers, called the
two plexuses, shown in Figure 62–4: (1) an outer plexus
The enteric nervous system is composed mainly of
cord. This highly developed enteric nervous system is
extending all the way to the anus. The number of
in the wall of the gut, beginning in the esophagus and
774
Unit XII
Gastrointestinal Physiology
neurons in this enteric system is about 100 million,
almost exactly equal to the number in the entire spinal
especially important in controlling gastrointestinal
movements and secretion.
lying between the longitudinal and circular muscle
myenteric plexus or
’s
plexus
submucosal
plexus or Meissner’s plexus
trols mainly gastrointestinal secretion and local blood
thetic and parasympathetic fibers that connect to both
parasympathetic and sympathetic systems can greatly
endings that originate in the gastrointestinal epithe-
lium or gut wall and send afferent fibers to both
vertebral ganglia of the sympathetic nervous system,
elicit local reflexes within the gut wall itself and still
other reflexes that are relayed to the gut from either
the prevertebral ganglia or the basal regions of the
brain.
and Submucosal Plexuses
myenteric plexus consists mostly of a linear chain
of many interconnecting neurons that extends the
Because the myenteric plexus extends all the way
along the intestinal wall and because it lies between
the longitudinal and circular layers of intestinal
(3) slightly increased rate of the rhythm of contraction,
and (4) increased velocity of conduction of excitatory
myenteric plexus should not be considered
entirely excitatory because some of its neurons are
inhibitory
vasoactive intestinal polypeptide
inhibitory signals are especially useful for inhibiting
some of the intestinal sphincter muscles that impede
movement of food along successive segments of the
,
which controls emptying of the stomach into the duo-
sphincter of the ileocecal valve
controls emptying from the small intestine into the
cecum.
submucosal plexus
within the inner wall of each minute segment of the
from the gastrointestinal epithelium and are then
To prevertebral
ganglia, spinal
cord, and brain
stem
Sensory
neurons
Submucosal
plexus
Myenteric
plexus
Epithelium
Sympathetic
(mainly postganglionic)
Parasympathetic
(preganglionic)
directly to the spinal cord and brain stem
vertebral ganglia of the spinal cord and
to the enteric plexuses, then to the pre-
from the luminal epithelium and gut wall
); and (3) sensory fibers passing
red
); (2) extrinsic control of these
Neural control of the gut wall, showing (1)
Figure 62–4
the myenteric and submucosal plexuses
(black fibers
plexuses by the sympathetic and
parasympathetic nervous systems (
fibers
(dashed fibers).
These include reflexes
Reflexes that are integrated entirely within the gut
testinal control. They are the following:
The anatomical arrangement of the enteric nervous
Gastrointestinal Reflexes
its functions.
medulla, which in turn initiates vagal reflex signals that
than efferent. These afferent fibers transmit sensory
nerve fibers in the vagus nerves are afferent rather
even the brain stem. For example, 80 per cent of the
In addition, other sensory signals from the gut go all
under other conditions,
or,
cific chemical substances in the gut. Signals trans-
excessive distention of the gut, or (3) presence of spe-
stimulated by (1) irritation of the gut mucosa, (2)
ganglia of the spinal cord. These sensory nerves can be
Nerve Fibers from the Gut
Sensory
Afferent
muscle (except the mucosal muscle, which it excites)
ways: (1) to a slight extent by direct effect of secreted
parasympathetic system. It exerts its effects in two
In general, stimulation of the sympathetic nervous
the parasympathetics. The sympathetic nerve endings
of the gastrointestinal tract, rather than being more
of the gut.. The sympathetics innervate essentially all
these ganglia, and postganglionic fibers then spread
. Most of
spinal column, and many of these fibers then pass on
sympathetic chains
cord, enter the
glionic fibers that innervate the gut, after leaving the
between segments T-5 and L-2. Most of the pregan-
The sympathetic fibers to the
Sympathetic Innervation.
functions.
in activity of the entire enteric nervous system. This
myenteric and submucosal plexuses. Stimulation of
The
to execute the defecation reflexes, discussed in
other intestinal areas. These fibers function especially
moidal, rectal, and anal regions are considerably better
large intestine and all the way to the anus. The sig-
third, and fourth sacral segments of the spinal cord and
The
through the first half of the large intestine.
extensive innervation to the esophagus, stomach, and
. These fibers provide
, which were discussed in Chapter 60.
The parasympathetic sup-
Parasympathetic Innervation.
Gastrointestinal Tract
Autonomic Control of the
following chapter.
inhibitory agents, some of which we will discuss in the
lae into the circulation. The other aforementioned
trointestinal activity. This is also true of
activity.
Acetylcholine
discussion here, other than to point out the following.
. The specific functions
vasoactive intestinal polypeptide,
substance P,
cholecystokinin,
dopamine,
adenosine triphosphate,
. Others are (3)
acetylcholine
types of enteric neurons. Two of them with which we
Types of Neurotransmitters Secreted
contraction of the submucosal muscle
, and local
General Principles of Gastrointestinal Function—Motility, Nervous Control, and Blood Circulation
Chapter 62
775
integrated in the submucosal plexus to help control
local intestinal secretion, local absorption
that causes
various degrees of infolding of the gastrointestinal
mucosa.
by Enteric Neurons
In an attempt to understand better the multiple func-
tions of the gastrointestinal enteric nervous system,
research workers the world over have identified a
dozen or more different neurotransmitter substances
that are released by the nerve endings of different
are already familiar are (1)
and (2) nor-
epinephrine
(4) serotonin, (5)
(6)
(7)
(8)
(9) somatostatin, (10) leu-enkephalin, (11) met-
enkephalin, and (12) bombesin
of many of these are not known well enough to justify
most often excites gastrointestinal
Norepinephrine almost always inhibits gas-
epinephrine,
which reaches the gastrointestinal tract mainly by way
of the blood after it is secreted by the adrenal medul-
transmitter substances are a mixture of excitatory and
ply to the gut is divided into cranial and sacral divi-
sions
Except for a few parasympathetic fibers to the
mouth and pharyngeal regions of the alimentary tract,
the cranial parasympathetic nerve fibers are almost
entirely in the vagus nerves
pancreas and somewhat less to the intestines down
sacral parasympathetics originate in the second,
pass through the pelvic nerves to the distal half of the
supplied with parasympathetic fibers than are the
Chapter 63.
postganglionic neurons of the gastrointestinal
parasympathetic system are located mainly in the
these parasympathetic nerves causes general increase
in turn enhances activity of most gastrointestinal
gastrointestinal tract originate in the spinal cord
that lie lateral to the
through the chains to outlying ganglia such as to the
celiac ganglion and various mesenteric ganglia
the postganglionic sympathetic neuron bodies are in
through postganglionic sympathetic nerves to all parts
extensive nearest the oral cavity and anus as is true of
secrete mainly norepinephrine but also small amounts
of epinephrine.
system inhibits activity of the gastrointestinal tract,
causing many effects opposite to those of the
norepinephrine to inhibit intestinal tract smooth
and (2) to a major extent by an inhibitory effect of
norepinephrine on the neurons of the entire enteric
nervous system.
Strong stimulation of the sympathetic system can
inhibit motor movements of the gut so greatly that this
literally can block movement of food through the gas-
trointestinal tract.
Many afferent sensory nerve fibers innervate the gut.
Some of them have their cell bodies in the enteric
nervous system itself and some in the dorsal root
mitted through the fibers can then cause excitation
inhibition of intestinal move-
ments or intestinal secretion.
the way to multiple areas of the spinal cord and
signals from the gastrointestinal tract into the brain
return to the gastrointestinal tract to control many of
system and its connections with the sympathetic and
parasympathetic systems support three types of gas-
trointestinal reflexes that are essential to gastroin-
1.
wall enteric nervous system.
that control much gastrointestinal secretion,
movement. Other stimuli that can initiate peristalsis
the gut wall 2 to 3 centimeters behind this point, and
lects at any point in the gut, the stretching of the gut
. That is, if a large amount of food col-
The usual stimulus for intestinal peristalsis is
of the body.)
lar ducts, ureters, and many other smooth muscle tubes
tube. (Peristalsis also occurs in the bile ducts, glandu-
lar muscle, and this ring then spreads along the gut
smooth muscle tubes; stimulation at any point in the
Peristalsis is an inherent property of many syncytial
the fingers and sliding them forward along the tube.
fingers around a thin distended tube, then constricting
moves forward; this is analogous to putting one’s
which is illustrated in Figure 62–5.
peristalsis,
The basic propulsive movement of the gastrointestinal
thoroughly mixed at all times.
, which keep the intestinal contents
mixing movements
to accommodate digestion and absorption, and (2)
, which cause food to
propulsive movements
tract: (1)
Two types of movements occur in the gastrointestinal
Gastrointestinal Tract
Functional Types of
intestine every 90 minutes in a fasted person. Motilin
plexes
interdigestive myoelectric com-
released cyclically and stimulates waves of gastroin-
. Motilin is
fasting, and the only known function of this hormone
food products.
to carbohydrate. It has a mild effect in decreasing
, mainly in response to fatty
tralize the acid in the small intestine.
stomach. Secretin has a mild effect on motility of the
covered and is secreted by the “S” cells in the
tying of the gallbladder, it also slows the emptying of
fore, at the same time that this hormone causes emp-
also inhibits stomach contraction moderately. There-
ing them to be digested and absorbed. Cholecystokinin
important roles in emulsifying fatty substances, allow-
hormone strongly contracts the gallbladder, expelling
and monoglycerides in the intestinal contents. This
response to digestive products of fat, fatty acids,
is secreted by “I” cells in the
stimulation of growth of the gastric mucosa
during vagal stimulation. The primary actions of
the products of proteins, and
ingestion of a meal, such as distention of the stomach,
the stomach
is secreted by the “G” cells of the
following.
important than the secretory effects of the hormones,
tract. Although the motility effects are usually less
secretion. Most of these same hormones also affect
In Chapter 64, we discuss the extreme importance of
Hormonal Control of
to produce the powerful colonic, rectal, and
inhibition of the entire gastrointestinal tract; and
activity; (2) pain reflexes that cause general
These include especially (1) reflexes from the
stem and then back to the gastrointestinal tract.
Reflexes from the gut to the spinal cord or brain
), and
enterogastric reflexes
), signals from the colon and
gastrointestinal tract, such as signals from the
These reflexes transmit
sympathetic ganglia and then back to the
Reflexes from the gut to the prevertebral
effects, and so forth.
peristalsis, mixing contractions, local inhibitory
776
Unit XII
Gastrointestinal Physiology
2.
gastrointestinal tract.
signals long distances to other areas of the
stomach to cause evacuation of the colon (the
gastrocolic reflex
small intestine to inhibit stomach motility and
stomach secretion (the
reflexes from the colon to inhibit emptying of ileal
contents into the colon (the colonoileal reflex).
3.
stomach and duodenum to the brain stem and
back to the stomach—by way of the vagus
nerves—to control gastric motor and secretory
(3) defecation reflexes that travel from the colon
and rectum to the spinal cord and back again
abdominal contractions required for defecation
(the defecation reflexes).
Gastrointestinal Motility
several hormones for controlling gastrointestinal
motility in some parts of the gastrointestinal
some of the more important of them are the
Gastrin
antrum of
in response to stimuli associated with
gastrin releasing peptide,
which is released by the nerves of the gastric mucosa
gastrin are (1) stimulation of gastric acid secretion and
(2)
.
Cholecystokinin
mucosa of the duodenum and jejunum mainly in
bile into the small intestine where the bile in turn plays
food from the stomach to give adequate time for diges-
tion of the fats in the upper intestinal tract.
Secretin was the first gastrointestinal hormone dis-
mucosa
of the duodenum in response to acidic gastric juice
emptying into the duodenum from the pylorus of the
gastrointestinal tract and acts to promote pancreatic
secretion of bicarbonate which in turn helps to neu-
Gastric inhibitory peptide is secreted by the mucosa
of the upper small intestine
acids and amino acids but to a lesser extent in response
motor activity of the stomach and therefore slows
emptying of gastric contents into the duodenum when
the upper small intestine is already overloaded with
Motilin is secreted by the upper duodenum during
is to increase gastrointestinal motility
testinal motility called
that move through the stomach and small
secretion is inhibited after ingestion by mechanisms
that are not fully understood.
Movements in the
move forward along the tract at an appropriate rate
Propulsive Movements—Peristalsis
tract is
A contractile ring appears around the gut and then
Any material in front of the contractile ring is moved
forward.
gut can cause a contractile ring to appear in the circu-
disten-
tion of the gut
wall stimulates the enteric nervous system to contract
a contractile ring appears that initiates a peristaltic
include chemical or physical irritation of the epithelial
into the vena cava, allows the
This flow of blood through the liver, before it empties
. In the liver, the blood
spleen, and pancreas then flows immediately into the
spleen, pancreas, and liver. The design of this system is
, shown in Figure 62–6. It includes the blood
splanchnic
The blood vessels of the gastrointestinal system are
“Splanchnic Circulation”
Gastrointestinal Blood Flow—
testinal tract for proper propulsion and mixing, as
then there. These peristaltic and constrictive move-
“chopping” and “shearing” the contents first here and
strictions occur at other points in the gut, thus
tions usually last only 5 to 30 seconds; then new con-
every few centimeters in the gut wall. These constric-
times,
tents, rather than propelling them forward. At other
tinal contents is blocked by a sphincter, so that a
tions themselves cause most of the mixing. This is
mentary tract. In some areas, the peristaltic contrac-
of the peristalsis is called the “law of the gut.”
. The
of the myenteric plexus. Therefore, the complex is
This complex pattern does not occur in the absence
called “receptive relaxation,” thus allowing the food to
centimeters downstream toward the anus, which is
At the same time, the gut sometimes relaxes several
tended segment, pushing the intestinal contents in the
and thereby initiates peristalsis, the contractile ring
When a
Peristaltic Reflex and the “Law of the Gut.”
follows.
ized” in the anal direction, which can be explained as
from the fact that the myenteric plexus itself is “polar-
been ascertained, although it probably results mainly
considerable distance toward the anus. The exact cause
from a stimulated point, but it normally dies out
Peristalsis, theoretically, can occur in either direction
Directional Movement of Peristaltic Waves Toward the Anus.
peristalsis requires an active myenteric plexus.
endings of the myenteric plexus. Therefore,
the myenteric plexus. Also, it is greatly depressed or
signals to the gut will elicit strong peristalsis.
lining in the gut. Also, strong parasympathetic nervous
General Principles of Gastrointestinal Function—Motility, Nervous Control, and Blood Circulation
Chapter 62
777
Function of the Myenteric Plexus in Peristalsis.
Peristalsis
occurs only weakly or not at all in any portion of the
gastrointestinal tract that has congenital absence of
completely blocked in the entire gut when a person is
treated with atropine to paralyze the cholinergic nerve
effectual
rapidly in the orad direction while continuing for a
of this directional transmission of peristalsis has never
segment of the intestinal tract is excited by distention
causing the peristalsis normally begins on the orad side
of the distended segment and moves toward the dis-
anal direction for 5 to 10 centimeters before dying out.
be propelled more easily anally than orad.
called the myenteric reflex or the peristaltic reflex
peristaltic reflex plus the anal direction of movement
Mixing Movements
Mixing movements differ in different parts of the ali-
especially true when forward progression of the intes-
peristaltic wave can then only churn the intestinal con-
local intermittent constrictive contractions occur
ments are modified in different parts of the gastroin-
discussed for each portion of the tract in Chapter 63.
part of a more extensive system called the
circulation
flow through the gut itself plus blood flows through the
such that all the blood that courses through the gut,
liver by way of the portal vein
passes through millions of minute liver sinusoids and
finally leaves the liver by way of hepatic veins that
empty into the vena cava of the general circulation.
reticuloendothelial cells
that line the liver sinusoids to remove bacteria and
Leading wave of distention
Zero time
5 seconds later
Peristaltic contraction
Figure 62–5
Peristalsis.
Vena cava
Hepatic artery
Aorta
Splenic
vein
Intestinal artery
Intestinal vein
Capillary
Portal
vein
Hepatic vein
Hepatic
sinuses
Splanchnic circulation.
Figure 62–6
instance, after a meal, the motor activity, secretory
increases with increased motor activity in the gut. For
submucosa is increased as much as eightfold. Likewise,
ents, blood flow in the villi and adjacent regions of the
activity. For instance, during active absorption of nutri-
the gut wall, is directly related to the level of local
of the gastrointestinal tract, as well as in each layer of
Under normal conditions, the blood flow in each area
Effect of Gut Activity and Metabolic
controlling villus blood flow.
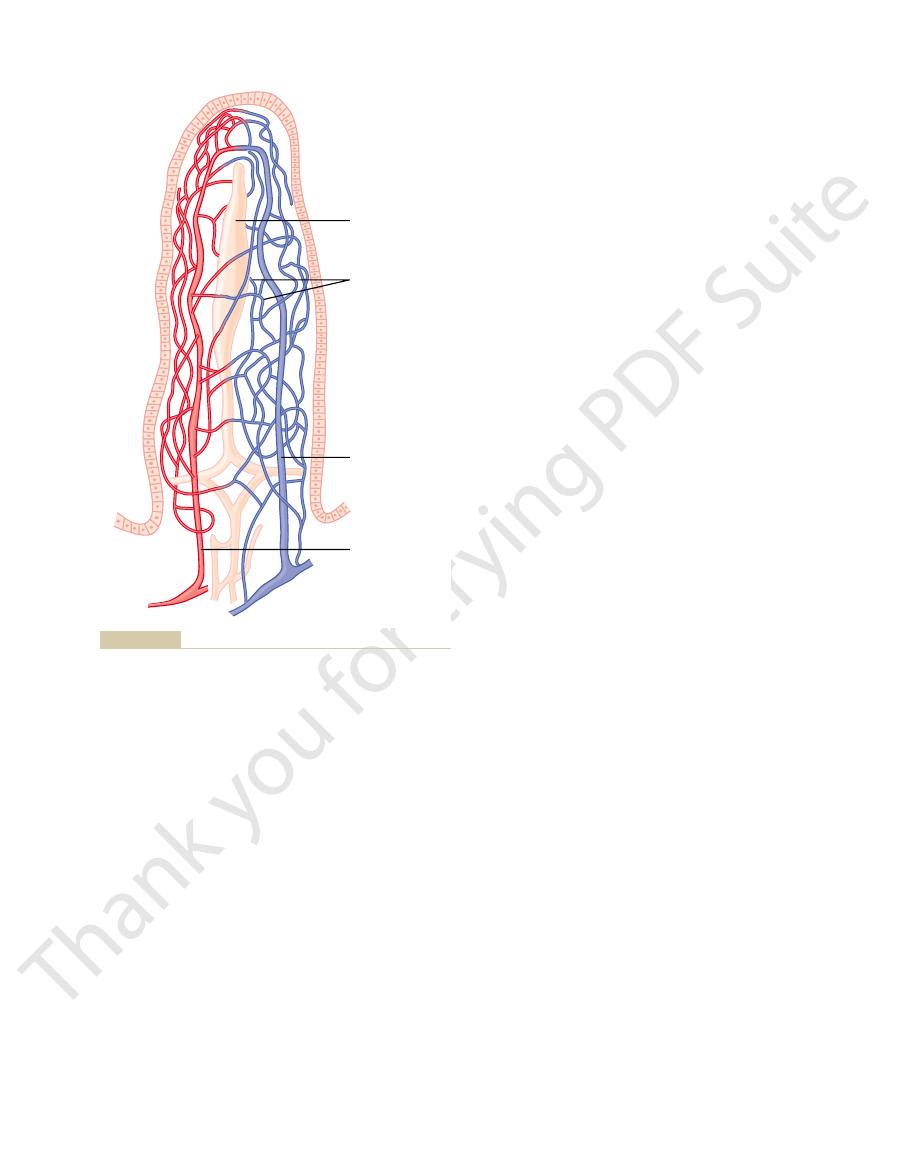
system of multiple looping capillaries. The walls of the
blood flow through an intestinal villus, including a
Figure 62–8 shows the special organization of the
tinal villi, and (3) into submucosal vessels beneath the
spread (1) along the muscle bundles, (2) into the intes-
attachment. From the circling arteries, still much
around the gut, with the tips of these arteries meeting
On entering the wall of the gut, the arteries branch
celiac artery, which provides a similar blood supply to
arching arterial system. Not shown in the figure is the
blood supply to the gut, including the superior mesen-
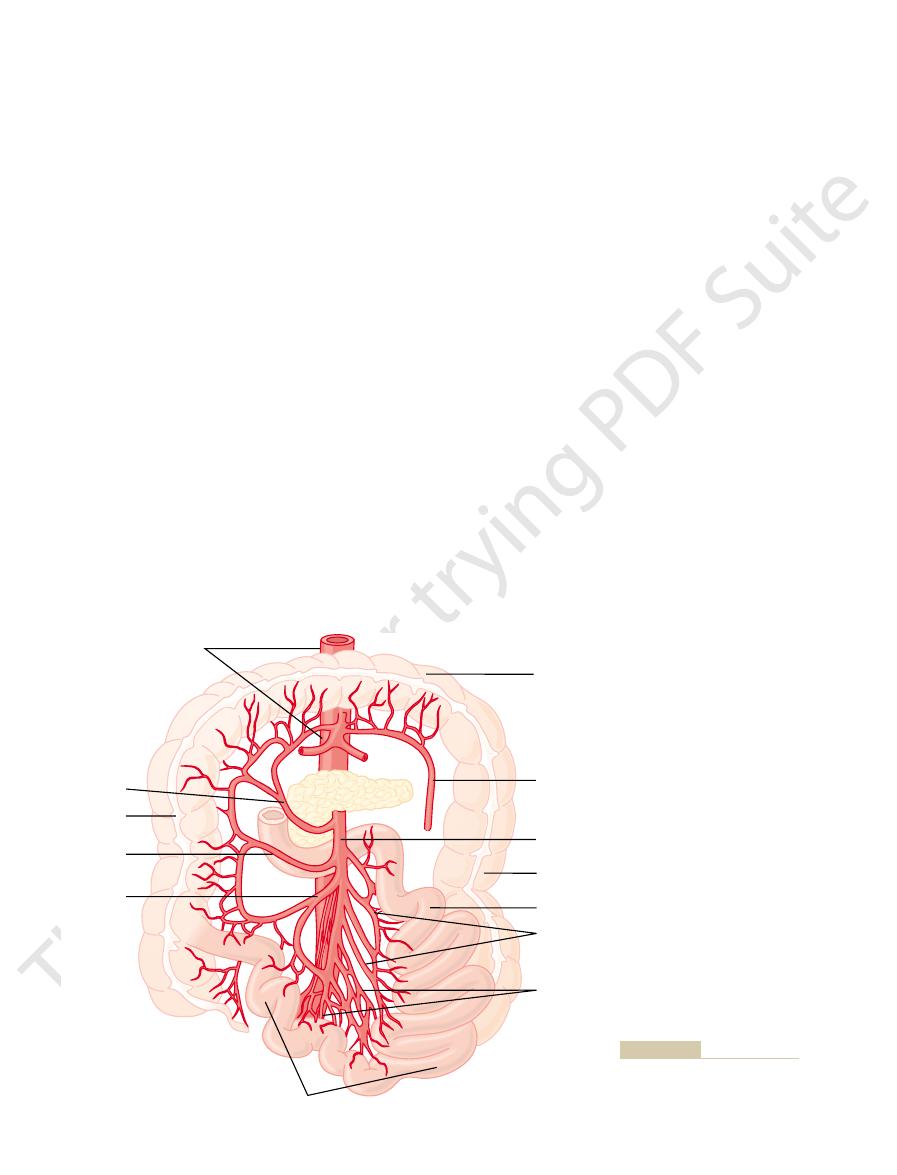
Figure 62–7 shows the general plan of the arterial
Anatomy of the Gastrointestinal
bypassing the liver.
the liver in Chapters 67 through 71. Almost all of the
the liver cells. We discuss these nutritional functions of
three quarters of the nutrients. Also, much chemical
, absorb and store temporarily from one half to
the principal parenchymal cells of the liver, the
sinusoids. Here, both the reticuloendothelial cells and
water-soluble nutrients
The
remainder of the body.
from the gastrointestinal tract, thus preventing direct
778
Unit XII
Gastrointestinal Physiology
other particulate matter that might enter the blood
transport of potentially harmful agents into the
nonfat,
absorbed from
the gut (such as carbohydrates and proteins) are trans-
ported in the portal venous blood to the same liver
hepatic
cells
intermediary processing of these nutrients occurs in
fats absorbed from the intestinal tract are not carried
in the portal blood but instead are absorbed into the
intestinal lymphatics and then conducted to the sys-
temic circulating blood by way of the thoracic duct,
Blood Supply
teric and inferior mesenteric arteries supplying the
walls of the small and large intestines by way of an
the stomach.
and send smaller arteries circling in both directions
on the side of the gut wall opposite the mesenteric
smaller arteries penetrate into the intestinal wall and
epithelium to serve the secretory and absorptive func-
tions of the gut.
small arteriole and venule that interconnect with a
arterioles are highly muscular and are highly active in
Factors on Gastrointestinal
Blood Flow
blood flow in the muscle layers of the intestinal wall
Transverse
colon
Descending
colon
Jejunum
Jejunal
Ileal
Ileum
Branch of
inferior
mesenteric
Superior
mesenteric
Right colic
Ascending
colon
Middle colic
Aorta
Ileocolic
tines through the mesenteric
Arterial blood supply to the intes-
Figure 62–7
web.
glands and muscle.
therefore, redilate the arterioles, thus causing return of
tory escape.” That is, the local metabolic vasodilator
normal by means of a mechanism called “autoregula-
this vasoconstriction, the flow often returns almost to
greatly decreased blood flow. After a few minutes of
Sympathetic stimulation, by contrast, has a direct
This increased flow probably results secondarily from
lower colon
stomach
Nervous Control of Gastrointestinal
absorptive capacity.
blunted, leading to greatly diminished intestinal
Therefore, for this reason and others, in many gas-
villus suffers ischemic death and can disintegrate.
tory shock, the oxygen deficit in the tips of the villi can
the gut becomes greatly curtailed, such as in circula-
villi, but in disease conditions in which blood flow to
Under normal conditions, this shunting of oxygen
nism in the vasa recta of the kidney medulla, discussed
local metabolic functions of the villi. The reader will
ment, much of the blood oxygen diffuses out of the
tion to each other. Because of this vascular arrange-
to each other, and that the vessels lie in close apposi-
Note in Figure
Thus, the increased blood flow during increased gas-
of the increased flow.
, a well-
vasodilation. The decrease in oxygen can also lead to
100 per cent; therefore, the increased mucosal and gut
decreased oxygen concentration
Third,
secretions into the lumen. These kinins are powerful
, at the same time that they secrete their
release into the gut wall two kinins,
Second, some of the gastrointestinal glands also
will see in Chapters 63 and 64.
specific motor and secretory activities of the gut, as we
. These same hormones control
, and
cholecystokinin
digestive process. Most of these are peptide hormones,
First, several vasodilator substances are released
testinal activity are still unclear, some facts are known.
testinal Activity.
back to the resting level over another 2 to 4 hours.
activity, and absorptive activity all increase; likewise,
General Principles of Gastrointestinal Function—Motility, Nervous Control, and Blood Circulation
Chapter 62
779
the blood flow increases greatly but then decreases
Possible Causes of the Increased Blood Flow During Gastroin-
Although the precise cause or causes
of the increased blood flow during increased gastroin-
from the mucosa of the intestinal tract during the
including
, vasoactive intestinal peptide,
gastrin
secretin
kallidin and
bradykinin
vasodilators that are believed to cause much of the
increased mucosal vasodilation that occurs along with
secretion.
in the gut
wall can increase intestinal blood flow at least 50 to
wall metabolic rate during gut activity probably lowers
the oxygen concentration enough to cause much of the
as much as a fourfold increase of adenosine
known vasodilator that could be responsible for much
trointestinal activity is probably a combination of
many of the aforementioned factors plus still others
yet undiscovered.
“Countercurrent” Blood Flow in the Villi.
62–8 that the arterial flow into the villus and the
venous flow out of the villus are in directions opposite
arterioles directly into the adjacent venules without
ever being carried in the blood to the tips of the villi.
As much as 80 per cent of the oxygen may take this
short-circuit route and therefore not be available for
recognize that this type of countercurrent mechanism
in the villi is analogous to the countercurrent mecha-
in detail in Chapter 28.
from the arterioles to the venules is not harmful to the
become so great that the villus tip or even the whole
trointestinal diseases the villi become seriously
Blood Flow
Stimulation of the parasympathetic nerves going to the
and
increases local blood flow at
the same time that it increases glandular secretion.
the increased glandular activity and not as a direct
effect of the nervous stimulation.
effect on essentially all the gastrointestinal tract to
cause intense vasoconstriction of the arterioles with
mechanisms that are elicited by ischemia become pre-
potent over the sympathetic vasoconstriction and,
necessary nutrient blood flow to the gastrointestinal
Central lacteal
Vein
Artery
Blood capillaries
ment of blood flow in the arterioles and venules.
Microvasculature of the villus, showing a countercurrent arrange-
Figure 62–8

Physiol Gastrointest Liver Physiol 286:G7, 2004
gastrointestinal signals that influence food intake. Am J
Woods SC: Gastrointestinal satiety signals I. An overview of
of normal and neoplastic tissues. Endocr Rev 24:571,
BM: Role of gastrointestinal hormones in the proliferation
Thomas RP, Hellmich MR, Townsend CM Jr, Evers
University Press, 1998.
Smith GP: Satiation: From Gut to Brain. New York: Oxford
Physiol Gastrointest Liver Physiol 282:G747, 2002.
orders caused by loss of interstitial cells of Cajal. Am J
bedside. IV. Genetic and animal models of GI motility dis-
physiology of the interstitial cells of Cajal: from bench to
Sanders KM, Ordog T, Ward SM: Physiology and patho-
Physiol Rev 78:1087, 1998.
Rehfeld JF: The new biology of gastrointestinal hormones.
tract. Am J Physiol Gastrointest Liver Physiol 283:G1217,
in our understanding of vago-vagal reflexes? I. Morphol-
Powley TL, Phillips RJ: Musings on the wanderer: what’s new
286:G183, 2004.
Cholecystokinin. Am J Physiol Gastrointest Liver Physiol
Moran TH, Kinzig KP: Gastrointestinal satiety signals II.
News Physiol Sci 16:138, 2001.
Lammers WJ, Slack JR: Of slow waves and spike patches.
Mosby, 2001.
Johnson LR: Gastrointestinal Physiology, 6th ed. St. Louis:
endocrine organ. FASEB J 18:439, 2004.
gastric motility: the emerging role of the stomach as an
Inui A, Asakawa A, Bowers CY, et al: Ghrelin, appetite, and
281:G1129, 2001.
innervation. Am J Physiol Gastrointest Liver Physiol
motility: lessons from mutant mice on slow waves and
stitial cell of Cajal: from bench to bedside. II. Gastric
Huizinga JD: Physiology and pathophysiology of the inter-
gene regulation. Ann N Y Acad Sci 1014:97, 2004.
Hocker M: Molecular mechanisms of gastrin-dependent
Sci 18:109, 2003.
human visceral pain in health and disease. News Physiol
Hobson AR, Aziz Q: Central nervous system processing of
functions. Pharmacol Toxicol 92:249-57, 2003.
Hansen MB: The enteric nervous system II: gastrointestinal
Prog Neurobiol 72:143, 2004.
afferent neurons and nerve circuits within the intestine.
Furness JB, Jones C, Nurgali K, Clerc N: Intrinsic primary
281:G1329, 2001.
assessment. Am J Physiol Gastrointest Liver Physiol
interstitial cells of Cajal with neuromediators: an interim
tial cell of Cajal: from bench to bedside. III. Interaction of
Daniel EE: Physiology and pathophysiology of the intersti-
Physiol Sci 19:27, 2004.
sonomicrometry and gastrointestinal motility. News
Adelson DW, Million M: Tracking the moveable feast:
states of low blood volume, this mechanism can
parts of the circulation. In hemorrhagic shock or other
. This decreases the volume of these veins,
teric veins
splanchnic blood flow to very little for many hours.
when all the body’s vital tissues are in danger of cel-
skeletal muscle and heart. Also, in circulatory shock,
heavy exercise, when increased flow is needed by the
Flow When Other Parts of the Body Need Extra Blood Flow.
Importance of Nervous Depression of Gastrointestinal Blood
780
Unit XII
Gastrointestinal Physiology
A
major value of sympathetic vasoconstriction in the gut
is that it allows shut-off of gastrointestinal and other
splanchnic blood flow for short periods of time during
lular death for lack of blood flow—especially the brain
and the heart—sympathetic stimulation can decrease
Sympathetic stimulation also causes strong vaso-
constriction of the large-volume intestinal and mesen-
thereby displacing large amounts of blood into other
provide as much as 200 to 400 milliliters of extra blood
to sustain the general circulation.
References
ogy and topography of vagal afferents innervating the GI
2002.
2003.
