
and especially store large quantities of calcium ions; (3) mitochondria and
, that can cause the platelets to contract; (2) residuals of both the
to those found in muscle cells, and still another contractile protein,
, which are contractile proteins similar
they do not have nuclei and cannot reproduce. In their cytoplasm are such active
Platelets have many functional characteristics of whole cells, even though
per microliter.
after entering the blood, especially as they squeeze through capillaries. The
ocytes fragment into the minute platelets either in the bone marrow or soon
extremely large cells of the hematopoietic series in the marrow; the megakary-
, which are
eter. They are formed in the bone marrow from
we first discuss the nature of platelets themselves.
rather than by a blood clot. To understand this, it is important that
platelet plug,
If the cut in the blood vessel is very small—indeed, many very small vascular
Formation of the Platelet Plug
the processes of platelet plugging and blood coagulation can take place.
spasm. The spasm can last for many minutes or even hours, during which time
The more severely a vessel is traumatized, the greater the degree of vascular
thromboxane A
ing a vasoconstrictor substance,
vessels, the platelets are responsible for much of the vasoconstriction by releas-
vessels initiated by direct damage to the vascular wall. And, for the smaller
inate from the traumatized vessel or nearby tissues. However, even more vaso-
matized tissues and blood platelets, and (3) nervous reflexes. The nervous
results from (1) local myogenic spasm, (2) local autacoid factors from the trau-
taneously reduces the flow of blood from the ruptured vessel. The contraction
vessel wall itself causes the smooth muscle in the wall to contract; this instan-
Immediately after a blood vessel has been cut or ruptured, the trauma to the
Vascular Constriction
fibrous tissue into the blood clot to close the hole in the vessel permanently.
blood coagulation, and (4) eventual growth of
plug, (3) formation of a blood clot as a result of
vascular constriction, (2) formation of a platelet
hemostasis is achieved by several mechanisms: (1)
loss. Whenever a vessel is severed or ruptured,
The term
C
H
A
P
T
E
R
3
6
457
Hemostasis and Blood Coagulation
Events in Hemostasis
hemostasis means prevention of blood
reflexes are initiated by pain nerve impulses or other sensory impulses that orig-
constriction probably results from local myogenic contraction of the blood
2
.
holes do develop throughout the body each day—the cut is often sealed by a
Physical and Chemical Characteristics of Platelets
Platelets (also called thrombocytes) are minute discs 1 to 4 micrometers in diam-
megakaryocytes
normal concentration of platelets in the blood is between 150,000 and 300,000
factors as (1) actin and myosin molecules
throm-
bosthenin
endoplasmic reticulum and the Golgi apparatus that synthesize various enzymes

courses: (1) It can become invaded by
Once a blood clot has formed, it can follow one of two
Fibrous Organization or Dissolution
in this clot retraction, as is discussed later.
vessel still further. Platelets also play an important role
minutes to an hour, the clot retracts; this closes the
broken end of the vessel is filled with clot. After 20
vessel opening is not too large, the entire opening or
Within 3 to 6 minutes after rupture of a vessel, if the
important of the clotting factors.
shown in Figure 36–1, and Table 36–1 lists the most
clotting process. The physical events of this process are
cular wall, from platelets, and from blood proteins
minor. Activator substances from the traumatized vas-
severe, and in 1 to 2 minutes if the trauma has been
the blood clot. The clot begins to develop in 15 to 20
The third mechanism for hemostasis is formation of
Ruptured Vessel
Blood Coagulation in the
skin and throughout the internal tissues, but this does
form additional endothelial cell membrane. A person
daily. Indeed, multiple small holes through the
The platelet-plugging mechanism is extremely
Importance of the Platelet Mechanism for Closing Vascular
an unyielding plug.
These attach tightly to the platelets, thus constructing
cular opening is small. Then, during the subsequent
This is at first a loose plug, but
platelet plug.
selves attract more and more additional platelets, thus
vessel wall, the damaged vascular wall activates suc-
Therefore, at the site of any opening in a blood
activated platelets.
activate them as well, and the stickiness of these addi-
. The ADP
thromboxane A
from the plasma; they secrete large quantities of ADP;
von Wille-
factors; they become sticky so that they adhere to col-
swell; they assume irregular forms with numerous irra-
their own characteristics drastically. They begin to
wall, the platelets themselves immediately change
surface, especially with collagen fibers in the vascular
important functions of the platelet itself. When
trabeculae.
macrophage system. More than one half of the
weeks its functional processes run out. Then it is
life in the blood of 8 to 12 days, so that over several
Thus, the platelet is an active structure. It has a half-
in the blood-clotting process, as we discuss later.
addition, the platelet membrane contains large
exposed collagen from deep within the vessel wall. In
areas of the vessel wall, especially
The cell membrane of the platelets is also important.
eventually helps repair damaged vascular walls.
multiply and grow, thus causing cellular growth that
cells, vascular smooth muscle cells, and fibroblasts to
growth factor
we discuss later in relation to blood coagulation; and
, which
many vascular and other local tissue reactions; (5) an
, which are local hormones that cause
(ADP);
(4) enzyme systems that synthesize
(ATP) and
Blood Cells, Immunity, and Blood Clotting
458
Unit VI
enzyme systems that are capable of forming adenosine
triphosphate
adenosine diphosphate
prostaglandins
important protein called fibrin-stabilizing factor
(6) a
that causes vascular endothelial
On its surface is a coat of glycoproteins that repulses
adherence to normal endothelium and yet causes
adherence to injured
to injured endothelial cells and even more so to any
amounts of phospholipids that activate multiple stages
eliminated from the circulation mainly by the tissue
platelets are removed by macrophages in the spleen,
where the blood passes through a latticework of tight
Mechanism of the Platelet Plug
Platelet repair of vascular openings is based on several
platelets come in contact with a damaged vascular
diating pseudopods protruding from their surfaces;
their contractile proteins contract forcefully and cause
the release of granules that contain multiple active
lagen in the tissues and to a protein called
brand factor that leaks into the traumatized tissue
and their enzymes form
2
and thromboxane in turn act on nearby platelets to
tional platelets causes them to adhere to the original
cessively increasing numbers of platelets that them-
forming a
it is usually successful in blocking blood loss if the vas-
process of blood coagulation, fibrin threads form.
Holes.
important for closing minute ruptures in very small
blood vessels that occur many thousands of times
endothelial cells themselves are often closed by
platelets actually fusing with the endothelial cells to
who has few blood platelets develops each day liter-
ally thousands of small hemorrhagic areas under the
not occur in the normal person.
seconds if the trauma to the vascular wall has been
adhering to the traumatized vascular wall initiate the
of the Blood Clot
fibroblasts,
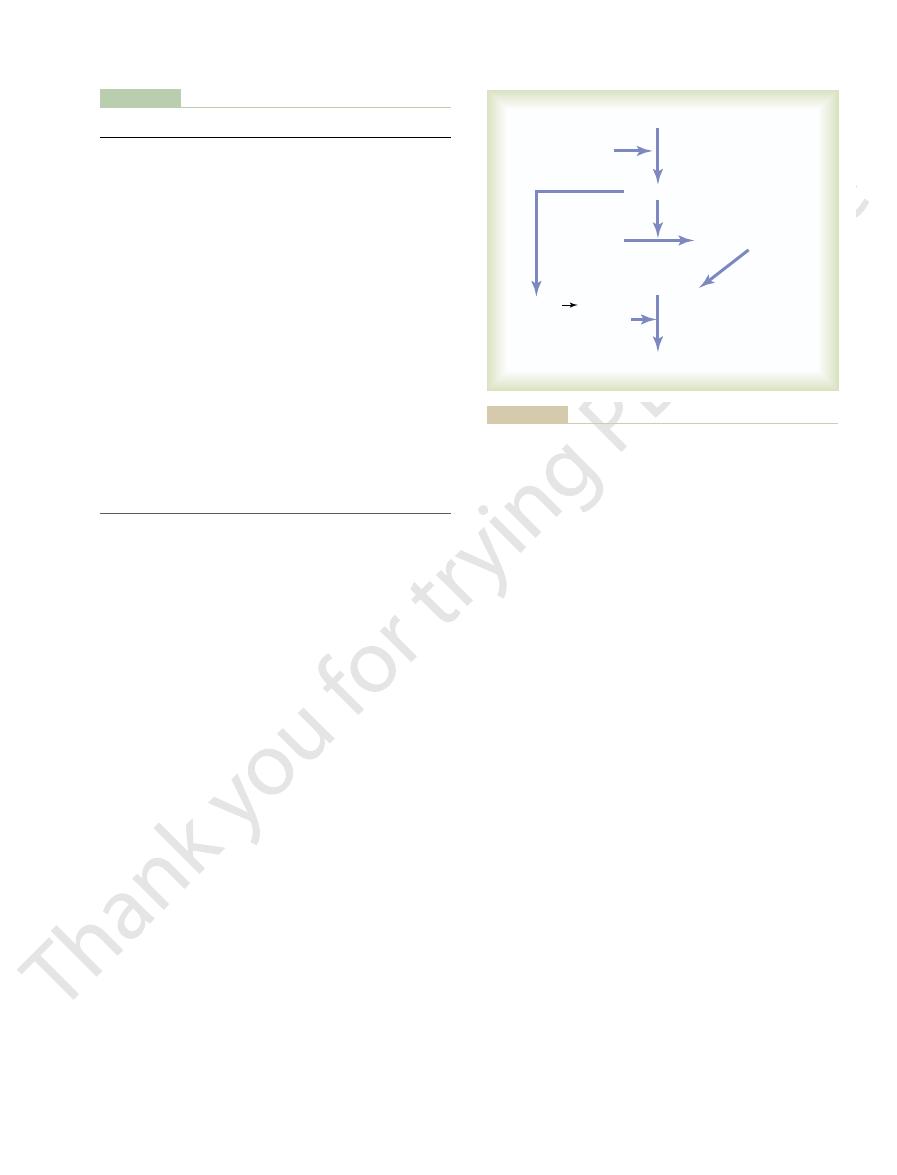
1. Severed vessel
2. Platelets agglutinate
3. Fibrin appears
5. Clot retraction occurs
4. Fibrin clot forms
Thomas, Publisher, Ltd., Springfield, IL.)
Seegers WH: Hemostatic Agents, 1948. Courtesy of Charles C
Clotting process in a traumatized blood vessel. (Modified from
Figure 36–1
form the clot itself.
fibrin fibers within another 10 to 15 seconds. Thus, the
thrombin to thrombin (Figure 36–2). Third, the throm-
, causes conversion of pro-
thrombin activator, in the presence of sufficient
to special substances in the blood. Second, the pro-
First, prothrombin activator is formed as a result of
Conversion of Prothrombin
of prothrombin to thrombin; then we will come back
blood clot itself is formed, beginning with conversion
enmesh platelets, blood cells, and plasma to form the
. (3) The thrombin acts as
The prothrombin activator catalyzes conversion of
. (2)
more than a dozen blood coagulation factors. The net
vessel or damage to the blood itself, a complex cascade
three essential steps: (1) In response to rupture of the
develop.
and override the anticoagulants, and then a clot does
from the area of tissue damage become “activated”
vessels. But when a vessel is ruptured, procoagulants
coagulants normally predominate, so that the blood
groups of substances. In the blood stream, the anti-
. Whether blood will
coagulation, called
procoagulants,
ulation, called
Basic Theory.
to dissolve the clot, as discussed later in the chapter.
usually become activated. These function as enzymes
not needed, special substances within the clot itself
Conversely, when excess blood has leaked into the
within about 1 to 2 weeks.
secreted by platelets). This continues
growth factor
sion by fibroblasts, beginning within a few hours after
the clot, or (2) it can dissolve. The usual course for a
Chapter 36
Hemostasis and Blood Coagulation
459
which subsequently form connective tissue all through
clot that forms in a small hole of a vessel wall is inva-
the clot is formed (which is promoted at least partially
by
to complete organization of the clot into fibrous tissue
tissues and tissue clots have occurred where they are
Mechanism of Blood
Coagulation
More than 50 important substances that
cause or affect blood coagulation have been found in
the blood and in the tissues—some that promote coag-
and others that inhibit
anticoagulants
coagulate depends on the balance between these two
does not coagulate while it is circulating in the blood
General Mechanism.
All research workers in the field of
blood coagulation agree that clotting takes place in
of chemical reactions occurs in the blood involving
result is formation of a complex of activated sub-
stances collectively called prothrombin activator
prothrombin into thrombin
an enzyme to convert fibrinogen into fibrin fibers that
clot.
Let us discuss first the mechanism by which the
to the initiating stages in the clotting process by which
prothrombin activator is formed.
to Thrombin
rupture of a blood vessel or as a result of damage
amounts of ionic Ca
++
bin causes polymerization of fibrinogen molecules into
rate-limiting factor in causing blood coagulation is
usually the formation of prothrombin activator and
not the subsequent reactions beyond that point,
because these terminal steps normally occur rapidly to
Platelets also play an important role in the con-
version of prothrombin to thrombin because much
of the prothrombin first attaches to prothrombin
Table 36–1
kininogen
(high-molecular-weight) kininogen
High-molecular-weight
Fitzgerald factor; HMWK
Prekallikrein
Fletcher factor
Factor XIII
Fibrin-stabilizing factor
Factor XII
Hageman factor
(PTA); antihemophilic factor C
Factor XI
Plasma thromboplastin antecedent
Factor X
Stuart factor; Stuart-Prower factor
(PTC); Christmas factor;
Factor IX
Plasma thromboplastin component
antihemophilic factor A
Factor VIII
Antihemophilic factor (AHF);
accelerator (SPCA); proconvertin;
Factor VII
Serum prothrombin conversion
Factor V
Proaccelerin; labile factor; Ac-globulin
Calcium
Factor IV
Tissue factor
Factor III; tissue thromboplastin
Prothrombin
Factor II
Fibrinogen
Factor I
Clotting Factor
Synonyms
Clotting Factors in Blood and Their Synonyms
(Ac-G)
stable factor
antihemophilic globulin (AHG);
antihemophilic factor B
Platelets
Thrombin
activated
Cross-linked fibrin fibers
Prothrombin
Thrombin
Fibrin fibers
Fibrinogen monomer
Fibrinogen
Prothrombin
activator
Ca
++
Ca
++
fibrin-stabilizing
factor
ization of fibrinogen to form fibrin fibers.
Schema for conversion of prothrombin to thrombin and polymer-
Figure 36–2
feedback) to promote more clotting. One of the most
That is, the clot itself initiates a vicious circle (positive
Once a blood clot has started to develop, it normally
Vicious Circle of Clot Formation
further to the ultimate state of hemostasis.
vessel are pulled together, thus contributing still
As the clot retracts, the edges of the broken blood
platelets.
endoplasmic reticulum, and Golgi apparatus of the
into a smaller mass. The contraction is activated and
fibrin. This also helps compress the fibrin meshwork
bosthenin, actin, and myosin molecules, which are all
addition, the platelets themselves contribute directly
cross-linking bonds between adjacent fibrin fibers. In
fibrin-stabilizing factor, which causes more and more
substances, one of the most important of which is
different fibers together. Furthermore, platelets
might be low. Electron micrographs of platelets in
Therefore, failure of clot retraction is an indication
Platelets are necessary for clot retraction to occur.
factors.
plasma. Serum cannot clot because it lacks these
have been removed; in this way, serum differs from
60 minutes. The fluid expressed is called
clot is formed, it begins to contract and usually
Within a few minutes after a
opening and thereby prevents further blood loss.
fore, the blood clot becomes adherent to any vascular
adhere to damaged surfaces of blood vessels; there-
blood cells, platelets, and plasma. The fibrin fibers also
The clot is composed of a meshwork of
linkages between adjacent fibrin fibers, thus adding
fibrin monomer molecules, as well as multiple cross-
covalent bonds
Then this activated substance operates as an enzyme
mation also activates the fibrin-stabilizing factor.
activated. The same thrombin that causes fibrin for-
can have an effect on the fibrin fibers, it must itself be
entrapped in the clot. Before fibrin-stabilizing factor
This involves a substance called
ease. But another process occurs during the next few
fibers are not cross-linked with one another; therefore,
covalent hydrogen bonding, and the newly forming
In the early stages of polymerization, the fibrin
Therefore,
It acts on fibrinogen to remove four low-molecular-
with weak proteolytic capabilities.
Thrombin
Action of Thrombin on Fibrinogen to Form Fibrin.
ordinarily do not coagulate. Yet, when the permeabil-
tial factors in the coagulation process, interstitial fluids
stitial fluids, and because fibrinogen is one of the essen-
Because of its large molecular size, little fibrinogen
tration of prothrombin, pointed out above.
tration of circulating fibrinogen, as it does the concen-
the liver, and liver disease can decrease the concen-
quantities of 100 to 700 mg/dl. Fibrinogen is formed in
Fibrinogen is a high-molecular-weight
Conversion of Fibrinogen to Fibrin—
results.
prothrombin level so low that a bleeding tendency
few other clotting factors. Therefore, either lack of
Vitamin K is required by the liver for normal for-
bin, in a day or so prothrombin concentration in
blood clotting. If the liver fails to produce prothrom-
Prothrombin is formed continually by the liver, and
, which has a molecular weight of 33,700,
can split easily into smaller compounds, one of which
tration of about 15 mg/dl. It is an unstable protein that
of 68,700. It is present in normal plasma in a concen-
protein, an alpha2-globulin, having a molecular weight
damaged tissue.
Blood Cells, Immunity, and Blood Clotting
460
Unit VI
receptors on the platelets already bound to the
Prothrombin and Thrombin.
Prothrombin is a plasma
is thrombin
almost exactly one half that of prothrombin.
it is continually being used throughout the body for
the plasma falls too low to provide normal blood
coagulation.
mation of prothrombin as well as for formation of a
vitamin K or the presence of liver disease that pre-
vents normal prothrombin formation can decrease the
Formation of the Clot
Fibrinogen.
protein (MW
= 340,000) that occurs in the plasma in
normally leaks from the blood vessels into the inter-
ity of the capillaries becomes pathologically increased,
fibrinogen does then leak into the tissue fluids in suf-
ficient quantities to allow clotting of these fluids in
much the same way that plasma and whole blood can
clot.
is a protein enzyme
weight peptides from each molecule of fibrinogen,
forming one molecule of fibrin monomer that has the
automatic capability to polymerize with other fibrin
monomer molecules to form fibrin fibers.
many fibrin monomer molecules polymerize within
seconds into long fibrin fibers that constitute the retic-
ulum of the blood clot.
monomer molecules are held together by weak non-
the resultant clot is weak and can be broken apart with
minutes that greatly strengthens the fibrin reticulum.
fibrin-stabilizing
factor that is present in small amounts in normal
plasma globulins but is also released from platelets
to cause
between more and more of the
tremendously to the three-dimensional strength of the
fibrin meshwork.
Blood Clot.
fibrin fibers running in all directions and entrapping
Clot Retraction—Serum.
expresses most of the fluid from the clot within 20 to
serum because
all its fibrinogen and most of the other clotting factors
that the number of platelets in the circulating blood
blood clots show that they become attached to the
fibrin fibers in such a way that they actually bond
entrapped in the clot continue to release procoagulant
to clot contraction by activating platelet throm-
contractile proteins in the platelets and cause strong
contraction of the platelet spicules attached to the
accelerated by thrombin as well as by calcium ions
released from calcium stores in the mitochondria,
extends within minutes into the surrounding blood.
from the
. This factor is
. Traumatized tissue
lowing steps, as shown in Figure 36–3:
come in contact with the blood. This leads to the fol-
The extrinsic pathway for initiating the formation of
to indicate the activated state of Factor VIII.
added after the Roman numeral, such as Factor VIIIa
the activated form of the factor, a small letter “a” is
36–1, are designated by Roman numerals. To indicate
Most of the clotting factors, which are listed in Table
cessive, cascading reactions of the clotting process.
the active forms, their enzymatic actions cause the suc-
forms of proteolytic enzymes. When converted to
play major roles. Most of these are
In both the extrinsic and the intrinsic pathways, a
that begins in the blood itself.
pathway
sic pathway
interact constantly with each other: (1) by the
formed in two ways, although, in reality, the two ways
steps.
, which then causes prothrombin
vessel. In each instance, this leads to the formation of
adjacent tissues, (2) trauma to the blood, or (3) contact
initiate clotting in the first place. These mechanisms
Now that we have discussed the clotting process itself,
of Prothrombin Activator
ceases.
and more and more thrombin to be formed; thus,
Once a critical amount of thrombin is formed, a vicious
VIII, IX, X, XI, and XII and aggregation of platelets.)
graphs, include acceleration of the actions of Factors
activator. (These effects, discussed in subsequent para-
more thrombin, and it acts on some of the blood-clot-
on prothrombin itself, tending to convert this into still
For instance, thrombin has a direct proteolytic effect
Chapter 36
Hemostasis and Blood Coagulation
461
important causes of this is the fact that the proteolytic
action of thrombin allows it to act on many of the
other blood-clotting factors in addition to fibrinogen.
ting factors responsible for formation of prothrombin
circle develops that causes still more blood clotting
the blood clot continues to grow until blood leakage
Initiation of Coagulation: Formation
we must turn to the more complex mechanisms that
are set into play by (1) trauma to the vascular wall and
of the blood with damaged endothelial cells or with
collagen and other tissue elements outside the blood
prothrombin activator
conversion to thrombin and all the subsequent clotting
Prothrombin activator is generally considered to be
extrin-
that begins with trauma to the vascular
wall and surrounding tissues and (2) by the intrinsic
series of different plasma proteins called blood-
clotting factors
inac-
tive
Extrinsic Pathway for Initiating Clotting
prothrombin activator begins with a traumatized vas-
cular wall or traumatized extravascular tissues that
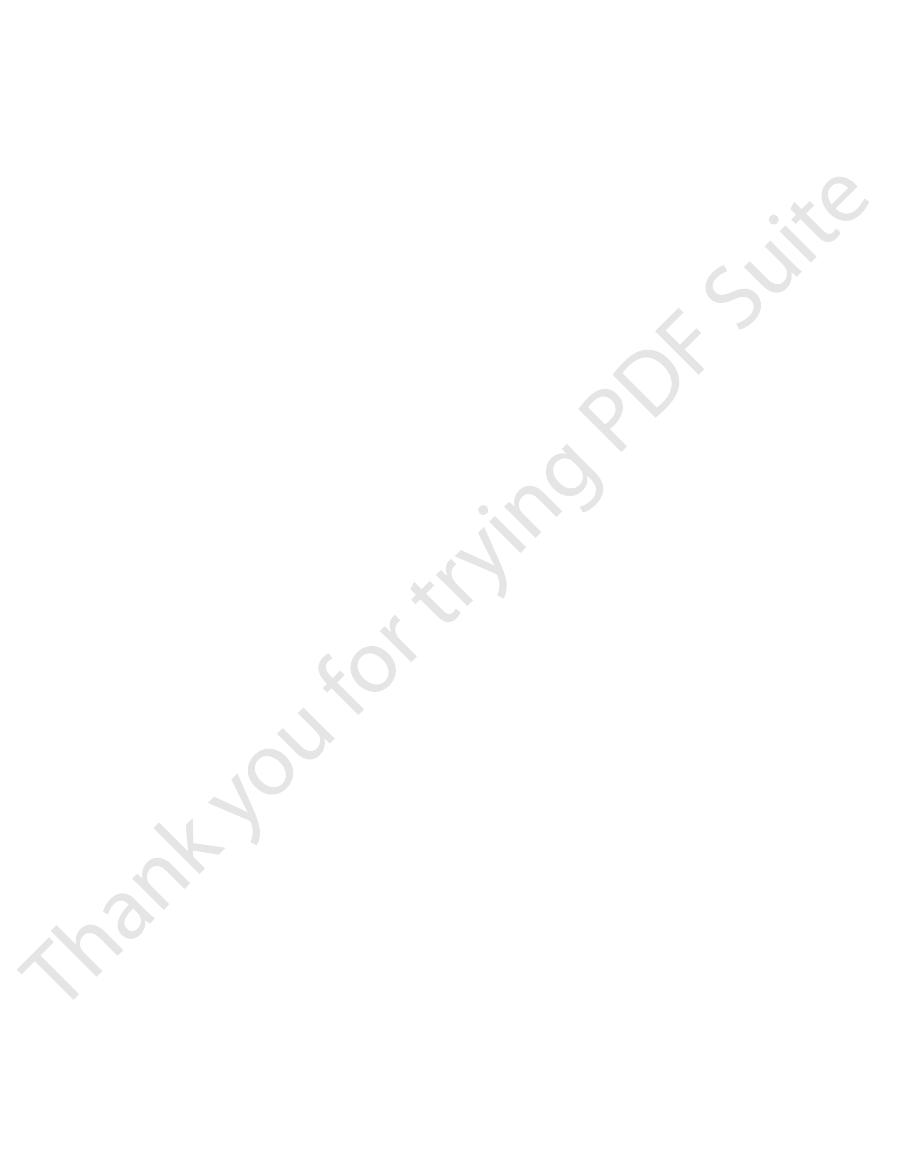
1. Release of tissue factor
releases a complex of several factors called tissue
factor or tissue thromboplastin
composed especially of phospholipids
membranes of the tissue plus a lipoprotein
complex that functions mainly as a proteolytic
enzyme.
Tissue trauma
Tissue factor
VIIa
Vll
Thrombin
Prothrombin
X
Activated X (Xa)
Ca
++
Ca
++
Ca
++
Prothrombin
Activator
Platelet
phospholipids
V
(1)
(2)
(3)
Figure 36–3
Extrinsic pathway for initiating blood clotting.
. Trauma
Blood trauma causes (1) activation of Factor XII
series of cascading reactions shown in Figure 36–4.
vessel wall. Then the process continues through the
ting,
thrombin activator, and therefore for initiating clot-
The second mechanism for initiating formation of pro-
process once it begins.
acting through Factor V, to accelerate the entire
positive feedback
a vehicle that further accelerates the process. Note
protease activity, and platelet phospholipids act as
activated Factor V greatly accelerates this
Factor X is the actual protease that causes
final prothrombin activator complex, activated
accelerator of prothrombin activation. Thus, in the
V. This then becomes an additional strong
the proteolytic action of thrombin activates Factor
prothrombin activator complex is inactive, but
explained. At first, the Factor V in the
), this splits prothrombin to form thrombin,
few seconds, in the presence of calcium ions
Within a
prothrombin activator.
platelets as well as with Factor V to form the
activated Factor X combines immediately with
. The
prothrombin activator—role of Factor V
Effect of activated Factor X (Xa) to form
Factor X
acts enzymatically on Factor X to form
Factor VII and, in the presence of calcium ions,
. The lipoprotein complex of tissue
Activation of Factor X—role of Factor VII and
Blood Cells, Immunity, and Blood Clotting
462
Unit VI
2.
tissue factor
factor further complexes with blood coagulation
activated
(Xa).
3.
tissue phospholipids that are part of tissue factor
or with additional phospholipids released from
complex called
(Ca
++
and the clotting process proceeds as already
once clotting begins and thrombin begins to form,
splitting of prothrombin to form thrombin;
especially the
effect of thrombin,
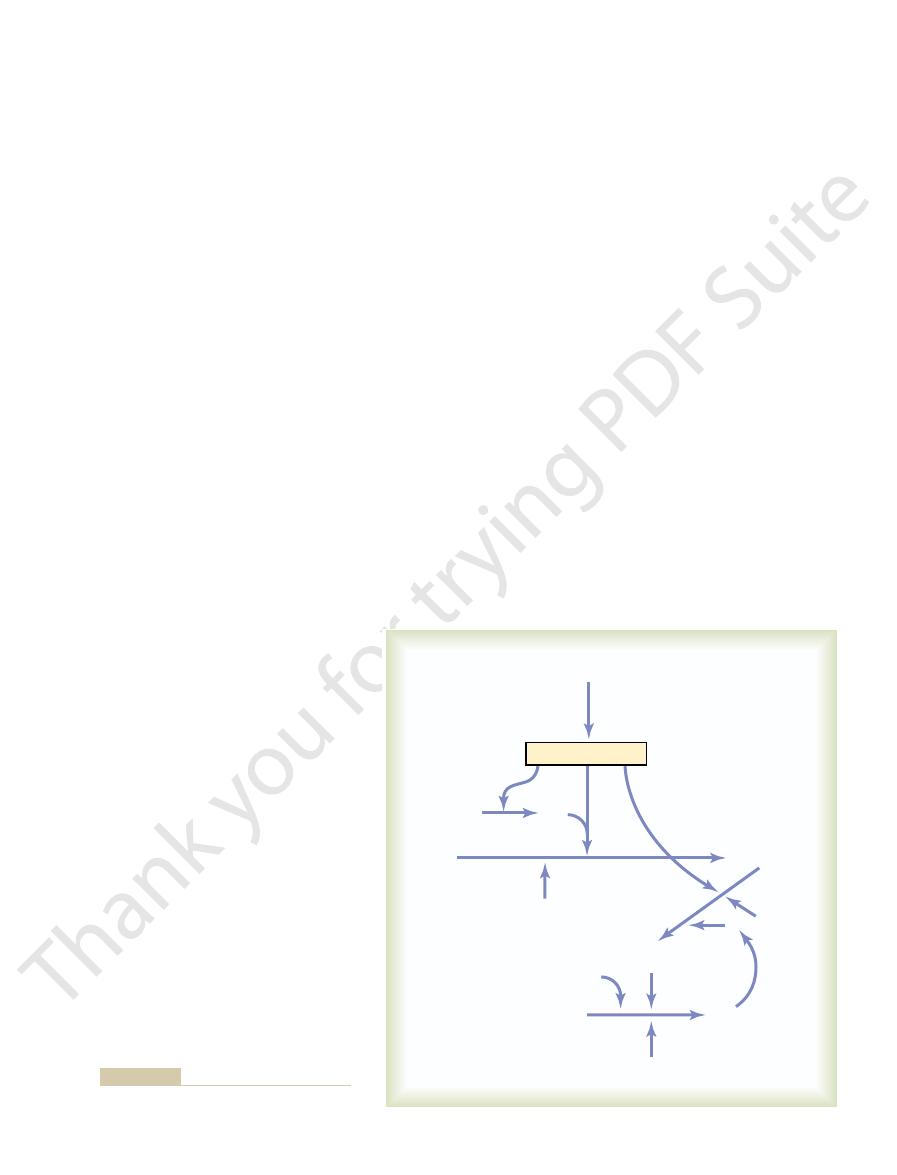
Intrinsic Pathway for Initiating Clotting
begins with trauma to the blood itself or exposure
of the blood to collagen from a traumatized blood
1.
and (2) release of platelet phospholipids
to the blood or exposure of the blood to vascular
X
Activated X (Xa)
XI
Activated XI (XIa)
XII
Activated XII (XIIa)
IX
(1)
(2)
(3)
(4)
(5)
Activated IX (IXa)
(HMW kininogen, prekallikrein)
Ca
++
Ca
++
Ca
++
Ca
++
VIII
Thrombin
VIIIa
Thrombin
Thrombin
Prothrombin
V
Prothrombin
Activator
Platelet
phospholipids
Blood trauma or
contact with collagen
Platelet
phospholipids
Figure 36–4
Intrinsic pathway for initiating
blood clotting.
blood and, therefore, prevents excessive spread of the
adsorbed to the fibrin fibers as they develop. This helps
While a clot is forming, about 85 to 90 per cent of
are those that remove thrombin from the blood. The
subendothelial collagen, the activation is even more
Factor XII and platelets come in contact with the
thus setting off the intrinsic pathway of clotting. If
which activates both Factor XII and the platelets,
When the endothelial wall is damaged, its smooth-
activated Factors V and VIII.
, that acts as an anticoagulant by
process by removing thrombin, but the thrombomod-
which binds thrombin. Not only does the binding of
with the endothelial membrane,
venting activation of clotting; and (3) a protein bound
which repels clotting factors and platelets, thereby pre-
sic clotting system; (2) a layer of
surface, which prevents contact activation of the intrin-
in the Normal Vascular System
Prevention of Blood Clotting
minutes to cause clotting.
is much slower to proceed, usually requiring 1 to 6
occur in as little as 15 seconds. The intrinsic pathway
in the blood. With severe tissue trauma, clotting can
tissues and by the quantities of Factors X, VII, and V
can be explosive; once initiated, its speed of
pathway
wall initiates the intrinsic pathway.
Factor XII and platelets with collagen in the vascular
initiates the extrinsic pathway, whereas contact of
occurs by both pathways simultaneously. Tissue factor
sic systems that after blood vessels rupture, clotting
and Intrinsic Pathways—Summary
oxalate ion
threshold level for clotting, either by deionizing the
from a person, it can be prevented from clotting by
kinetics of blood clotting. But, when blood is removed
In the living body, the calcium ion concentration
pathway does not occur.
the absence of calcium ions, blood clotting by either
tion of all the blood-clotting reactions. Therefore, in
Except for the first two steps in the intrinsic pathway,
earlier.
into motion the final clotting process, as described
prothrombin to form thrombin, thereby setting
. The prothrombin activator
combines with Factor V and platelet or tissue
the extrinsic pathway. That is, activated Factor X
. This step in the
activator—role of Factor V
Action of activated Factor X to form prothrombin
this step is deficient. Factor VIII is the factor that
either Factor VIII or platelets are in short supply,
platelets, activates Factor X. It is clear that when
activated Factor VIII and with the platelet
The activated Factor IX, acting in concert with
Activation of Factor X—role of Factor VIII
on Factor IX to activate this factor also.
The activated Factor XI then acts enzymatically
Activation of Factor IX by activated Factor XI
HMW (high-molecular-weight) kininogen
intrinsic pathway. This reaction also requires
factor as well, which is the second step in the
acts enzymatically on Factor XI to activate this
. The activated Factor XII
Activation of Factor XI
subsequent clotting reactions.
, which also plays a role in
in other ways), and this releases platelet
Simultaneously, the blood trauma also damages
enzyme called “activated Factor XII.”
such as glass, it takes on a new molecular
Factor XII is disturbed, such as by coming into
in the blood: Factor XII and the platelets. When
Chapter 36
Hemostasis and Blood Coagulation
463
wall collagen alters two important clotting factors
contact with collagen or with a wettable surface
configuration that converts it into a proteolytic
the platelets because of adherence to either
collagen or a wettable surface (or by damage
phospholipids that contain the lipoprotein called
platelet factor 3
2.
and is
accelerated by prekallikrein.
3.
.
4.
.
phospholipids and factor 3 from the traumatized
is missing in a person who has classic hemophilia,
for which reason it is called antihemophilic factor.
Platelets are the clotting factor that is lacking in
the bleeding disease called thrombocytopenia.
5.
intrinsic pathway is the same as the last step in
phospholipids to form the complex called
prothrombin activator
in turn initiates within seconds the cleavage of
Role of Calcium Ions in the Intrinsic and
Extrinsic Pathways
calcium ions are required for promotion or accelera-
seldom falls low enough to significantly affect the
reducing the calcium ion concentration below the
calcium by causing it to react with substances such as
citrate ion or by precipitating the calcium with sub-
stances such as
.
Interaction Between the Extrinsic
of Blood-Clotting Initiation
It is clear from the schemas of the intrinsic and extrin-
An especially important difference between the
extrinsic and intrinsic pathways is that the extrinsic
completion to the final clot is limited only by the
amount of tissue factor released from the traumatized
—
Intravascular Anticoagulants
Endothelial Surface Factors.
Probably the most important
factors for preventing clotting in the normal vascular
system are (1) the smoothness of the endothelial cell
glycocalyx on the
endothelium (glycocalyx is a mucopolysaccharide
adsorbed to the surfaces of the endothelial cells),
thrombomodulin,
thrombin with thrombomodulin slow the clotting
ulin-thrombin complex also activates a plasma protein,
protein C
inactivating
ness and its glycocalyx-thrombomodulin layer are lost,
powerful.
Antithrombin Action of Fibrin and Antithrombin III.
Among
the most important anticoagulants in the blood itself
most powerful of these are (1) the fibrin fibers that
themselves are formed during the process of clotting
and (2) an alpha-globulin called antithrombin III or
antithrombin-heparin cofactor.
the thrombin formed from the prothrombin becomes
prevent the spread of thrombin into the remaining
clot.
disease). Lack of bile prevents adequate fat digestion
ciency is failure of the liver to secrete bile into the gas-
the blood along with the fats.
fats from the gastrointestinal tract. The reason is that
ciency often occurs as a result of poor absorption of
However, in gastrointestinal disease, vitamin K defi-
tinal tract by bacteria, so that vitamin K deficiency
Vitamin K is continually synthesized in the intes-
dencies.
K, subsequent insufficiency of these coagulation
. In the absence of vitamin
, and
Factor X
Factor
Factor VII
factors by the liver is vitamin K deficiency. Vitamin K
greatly that the patient develops a severe tendency to
acute yellow
, and
factors are formed by the liver. Therefore, diseases of
With few exceptions, almost all the blood-clotting
by Vitamin K De
(3) thrombocytopenia (platelet deficiency).
caused by (1) vitamin K deficiency, (2) hemophilia, and
to the greatest extent are discussed here: bleeding
one of the many blood-clotting factors. Three particu-
Excessive bleeding can result from deficiency of any
nism. Thus, an especially important function of the
fact, many small blood vessels in which blood flow has
turn removes the remaining unnecessary blood clot. In
eventually converts plasminogen to plasmin, which in
days later, after the clot has stopped the bleeding,
(t-PA) that a few
until it is activated. The injured tissues and vascular
This will not become plasmin or cause lysis of the clot
is trapped in the clot along with other plasma proteins.
When a clot is formed, a large amount of plasminogen
Activation of Plasminogen to Form Plasmin: Then Lysis of Clots.
factors, thereby sometimes even causing hypocoagula-
Therefore, whenever plasmin is formed, it can cause
Factor V, Factor VIII, prothrombin, and Factor XII.
pancreatic secretion. Plasmin digests fibrin fibers and
) that, when activated,
The plasma proteins contain a euglobulin called
Lysis of Blood Clots
growth of the clots.
blood; sufficient formation of heparin prevents further
ies of the liver. It is easy to understand why large quan-
mast cells, release small quantities of heparin into
blood, which are functionally almost identical to the
into the circulatory system. The
nective tissue throughout the body. These cells contin-
body, but especially large quantities are formed by the
Factors XII, XI, X, and IX.
ness of anticoagulation. The others include activated
addition to thrombin, further enhancing the effective-
The complex of heparin and antithrombin III
antithrombin III is almost instantaneous.
Therefore, in the presence of excess heparin, removal
a thousandfold, and thus it acts as an anticoagulant.
antithrombin III, the effectiveness of antithrombin III
anticoagulant properties, but when it combines with
conjugated polysaccharide. By itself, it has little or no
The heparin molecule is a highly negatively charged
prevent intravascular clotting.
it have significant anticoagulant effects. However,
but its concentration in the blood is normally low, so
during the next 12 to 20 minutes.
fibers soon combines with antithrombin III, which
The thrombin that does not adsorb to the fibrin
Blood Cells, Immunity, and Blood Clotting
464
Unit VI
further blocks the effect of the thrombin on the fi-
brinogen and then also inactivates the thrombin itself
Heparin.
Heparin is another powerful anticoagulant,
that only under special physiologic conditions does
heparin is used widely as a pharmacological agent in
medical practice in much higher concentrations to
for removing thrombin increases by a hundredfold to
of free thrombin from the circulating blood by
removes several other activated coagulation factors in
Heparin is produced by many different cells of the
basophilic mast cells located in the pericapillary con-
ually secrete small quantities of heparin that diffuse
basophil cells of the
the plasma.
Mast cells are abundant in tissue surrounding the
capillaries of the lungs and to a lesser extent capillar-
tities of heparin might be needed in these areas
because the capillaries of the lungs and liver receive
many embolic clots formed in slowly flowing venous
—Plasmin
plasminogen (or profibrinolysin
becomes a substance called plasmin (or fibrinolysin).
Plasmin is a proteolytic enzyme that resembles trypsin,
the most important proteolytic digestive enzyme of
some other protein coagulants such as fibrinogen,
lysis of a clot by destroying many of the clotting
bility of the blood.
endothelium very slowly release a powerful activator
called tissue plasminogen activator
been blocked by clots are reopened by this mecha-
plasmin system is to remove minute clots from millions
of tiny peripheral vessels that eventually would
become occluded were there no way to clear them.
Conditions That Cause
Excessive Bleeding in
Human Beings
lar types of bleeding tendencies that have been studied
Decreased Prothrombin, Factor VII,
Factor IX, and Factor X Caused
ficiency
the liver such as hepatitis, cirrhosis
atrophy can sometimes depress the clotting system so
bleed.
Another cause of depressed formation of clotting
is necessary for liver formation of five of the impor-
tant clotting factors: prothrombin,
,
IX,
protein C
factors in the blood can lead to serious bleeding ten-
seldom occurs in the normal person as a result of
vitamin K absence from the diet (except in neonates
before they establish their intestinal bacterial flora).
vitamin K is fat-soluble and ordinarily is absorbed into
One of the most prevalent causes of vitamin K defi-
trointestinal tract (which occurs either as a result of
obstruction of the bile ducts or as a result of liver
blood vessels, where small quantities of thrombin and
when it flows very slowly
or trauma—is likely to initiate the clotting process. (2)
—as may be caused by arteriosclerosis, infection,
twofold: (1) Any
The causes of throm-
brain, kidneys, or elsewhere. Emboli that originate in
. Also, emboli that originate in
are known as
the clot to flow with the blood; such freely flowing clots
developed, continued flow of blood past the clot is
. Once a clot has
Thrombi and Emboli.
Thromboembolic Conditions
helpful, sometimes effecting almost complete cure
large numbers of platelets. Also,
effected in a patient with thrombocytopenia by
unknown reasons, specific antibodies have formed and
of these people, it has been discovered that for
means thrombocytopenia of unknown cause. In most
, which
Most people with thrombocytopenia have the
because, as pointed out earlier, clot retraction is nor-
thrombocytopenia if the person’s blood fails to retract,
blood, sometimes one can suspect the existence of
than the normal 150,000 to 300,000. Levels as low as
l, rather
Ordinarily, bleeding will not occur until the number
capillaries and other small vessels.
. As stated earlier, platelets are
purplish blotches, giving the disease the name
tissues. The skin of such a person displays many small,
from larger vessels as in hemophilia. As a result, small
from many small venules or capillaries, rather than
do hemophiliacs, except that the bleeding is usually
with thrombocytopenia have a tendency to bleed, as
numbers of platelets in the circulating blood. People
Thrombocytopenia means the presence of very low
human blood and only in extremely small quantities.
VIII. The cost of Factor VIII is high, and its availabil-
that is truly effective is injection of purified Factor
severe prolonged bleeding, almost the only therapy
When a person with classic hemophilia experiences
ferent characteristics, called von Willebrand’s disease,
philia. Another bleeding disease with somewhat dif-
of this part of Factor VIII that causes classic hemo-
the intrinsic pathway for clotting, and it is deficiency
230,000. The smaller component is most important in
Factor VIII has two active components, a large com-
For instance, bleeding can often last for days after
bleeding may be so mild that it is hardly noticeable.
except after trauma, but in some patients, the degree
genetic deficiency. Bleeding usually does not occur
degrees of severity, depending on the character of the
The bleeding trait in hemophilia can have various
half of her female offspring.
, transmitting the disease to half of
If one of her X chromosomes is deficient, she will be
two X chromosomes will have the appropriate genes.
female chromosome. Therefore, almost never will a
is caused by deficiency of Factor IX. Both of these
per cent of hemophilia patients, the bleeding tendency
United States has classic hemophilia. In the other 15
. About 1 of every 10,000 males in the
abnormality or deficiency of Factor VIII;
exclusively in males. In 85 per cent of cases, it is caused
are at least one-half normal in function, sufficient
before performing the surgical procedure. Ordinarily,
Because of this, vitamin K is injected into all surgical
absorption and because of the diseased liver cells.
absorption as well. Thus, liver disease often causes
and absorption and, therefore, depresses vitamin K
Chapter 36
Hemostasis and Blood Coagulation
465
decreased production of prothrombin and some other
clotting factors both because of poor vitamin K
patients with liver disease or with obstructed bile ducts
if vitamin K is given to a deficient patient 4 to 8 hours
before the operation and the liver parenchymal cells
clotting factors will be produced to prevent excessive
bleeding during the operation.
Hemophilia
Hemophilia is a bleeding disease that occurs almost
by an
this
type of hemophilia is called hemophilia A or classic
hemophilia
factors are transmitted genetically by way of the
woman have hemophilia because at least one of her
a hemophilia carrier
her male offspring and transmitting the carrier state to
of trauma required to cause severe and prolonged
extraction of a tooth.
ponent with a molecular weight in the millions and a
smaller component with a molecular weight of about
results from loss of the large component.
ity is limited because it can be gathered only from
Thrombocytopenia
punctate hemorrhages occur throughout all the body
throm-
bocytopenic purpura
especially important for repair of minute breaks in
of platelets in the blood falls below 50,000/
m
10,000/
ml are frequently lethal.
Even without making specific platelet counts in the
mally dependent on release of multiple coagulation
factors from the large numbers of platelets entrapped
in the fibrin mesh of the clot.
disease known as idiopathic thrombocytopenia
react against the platelets themselves to destroy them.
Relief from bleeding for 1 to 4 days can often be
giving fresh whole blood transfusions that contain
splenectomy is often
because the spleen normally removes large numbers
of platelets from the blood.
in the Human Being
An abnormal clot that develops in
a blood vessel is called a thrombus
likely to break it away from its attachment and cause
emboli
large arteries or in the left side of the heart can flow
peripherally and plug arteries or arterioles in the
the venous system or in the right side of the heart gen-
erally flow into the lungs to cause pulmonary arterial
embolism.
Cause of Thromboembolic Conditions.
boembolic conditions in the human being are usually
roughened endothelial surface of a
vessel
Blood often clots
through
other procoagulants are always being formed.
for 1 hour or more. The reason for this delay is that
siliconized containers
glass test tube normally clots in about 6 minutes, blood
Prevention of Blood Coagulation
coumarin therapy.
factors already present in the plasma. Normal coagu-
In other words, the coagulation process is not blocked
to about 20 per cent of normal by the end of 24 hours.
farin, the coagulant activity of the blood decreases to
of prothrombin and the other three clotting factors,
on liver formation of these compounds. Warfarin
VII, IX, and X, all formed by the liver, begin to fall,
patient, the plasma levels of prothrombin and Factors
When a coumarin, such as
Coumarins as Anticoagulants
The action of heparin lasts about 1.5 to 4 hours. The
time occurs instantaneously, thereby immediately pre-
more minutes. Furthermore, this change in clotting
1 mg/kg of body weight, causes the blood-clotting time
Injection of relatively small quantities, about 0.5 to
have been developed for this purpose. The ones most
delay the coagulation process. Various anticoagulants
In some thromboembolic conditions, it is desirable to
to bleed. The reason for this is that so many of the
85 per cent or more of patients.
septicemic shock
that leads to or exacerbates circulatory shock. It is
activate the clotting mechanisms. Plugging of
endotox-
with widespread septicemia, in which either circulat-
eral blood vessels. This occurs especially in patients
ous, and they plug a large share of the small periph-
the blood. Frequently, the clots are small but numer-
. This often results from the presence of
vated in widespread areas of the circulation, giving rise
a lifesaver.
the pulmonary vessels. But, again, t-PA therapy can be
pulmonary artery is blocked, death may not occur, or
the same time, immediate death ensues. If only one
. If the clot is large
cause massive blockage of the pulmonary arteries,
about 1 time out of every 10, a large part of the clot
the common iliac vein and inferior vena cava. Then,
moving venous blood, sometimes growing the entire
the clot grows, mainly in the direction of the slowly
one or more of the leg veins for hours at a time. Then
body, the immobility of patients confined to bed plus
Femoral Venous Thrombosis and
damage.
coronary artery, the heart is often spared serious
some intravascular clots. For instance, if used within
plasminogen to plasmin, which in turn can dissolve
area through a catheter, it is effective in activating
available. When delivered directly to a thrombosed
engineered t-PA (tissue plasminogen activator) is
Use of t-PA in Treating Intravascular Clots.
Blood Cells, Immunity, and Blood Clotting
466
Unit VI
Genetically
the first hour or so after thrombotic occlusion of a
Massive Pulmonary Embolism
Because clotting almost always occurs when blood
flow is blocked for many hours in any vessel of the
the practice of propping the knees with pillows often
causes intravascular clotting because of blood stasis in
length of the leg veins and occasionally even up into
disengages from its attachments to the vessel wall and
flows freely with the venous blood through the right
side of the heart and into the pulmonary arteries to
called massive pulmonary embolism
enough to occlude both of the pulmonary arteries at
the embolism may lead to death a few hours to several
days later because of further growth of the clot within
Disseminated Intravascular
Coagulation
Occasionally the clotting mechanism becomes acti-
to the condition called disseminated intravascular
coagulation
large amounts of traumatized or dying tissue in the
body that releases great quantities of tissue factor into
ing bacteria or bacterial toxins—especially
ins—
small peripheral vessels greatly diminishes delivery of
oxygen and other nutrients to the tissues—a situation
partly for this reason that
is lethal in
A peculiar effect of disseminated intravascular
coagulation is that the patient on occasion begins
clotting factors are removed by the widespread clot-
ting that too few procoagulants remain to allow
normal hemostasis of the remaining blood.
Anticoagulants for
Clinical Use
useful clinically are heparin and the coumarins.
Heparin as an Intravenous
Anticoagulant
Commercial heparin is extracted from several differ-
ent animal tissues and prepared in almost pure form.
to increase from a normal of about 6 minutes to 30 or
venting or slowing further development of a throm-
boembolic condition.
injected heparin is destroyed by an enzyme in the
blood known as heparinase.
warfarin, is given to a
indicating that warfarin has a potent depressant effect
causes this effect by competing with vitamin K for
reactive sites in the enzymatic processes for formation
thereby blocking the action of vitamin K.
After administration of an effective dose of war-
about 50 per cent of normal by the end of 12 hours and
immediately but must await the natural consumption
of the prothrombin and the other affected coagulation
lation usually returns 1 to 3 days after discontinuing
Outside the Body
Although blood removed from the body and held in a
collected in
often does not clot
preparing the surfaces of the containers with silicone
thrombin concentration to prothrombin time, such as
seconds. In each laboratory, a curve relating pro-
centration. The normal prothrombin time is about 12
of the time
. The
pathway. The time required for coagulation to take
The excess calcium nullifies the effect of the oxalate,
into thrombin. Then, a large excess of calcium ion and
thrombin time is the following.
thrombin time. The method for determining pro-
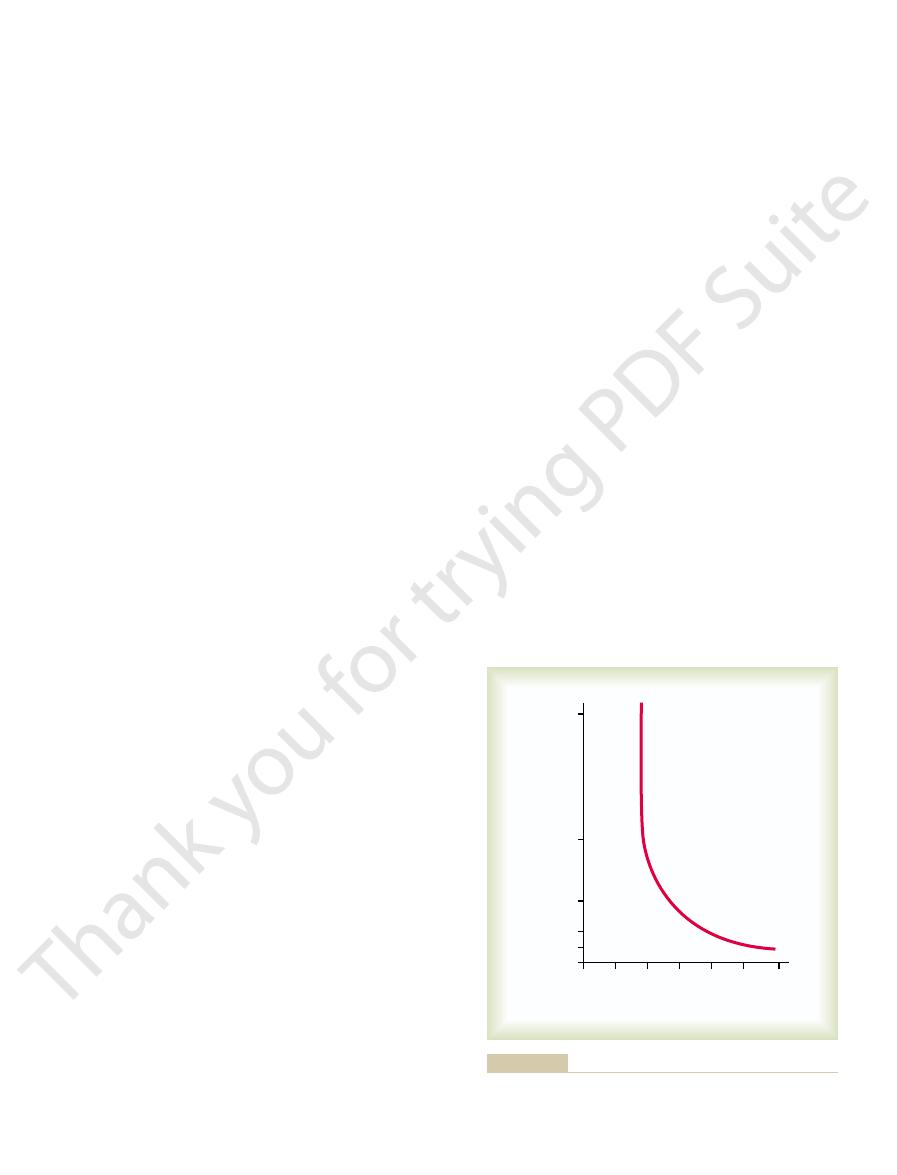
tration of prothrombin in the blood. Figure 36–5 shows
Prothrombin Time
using sophisticated chemical procedures.
ments of the clotting factors themselves are made,
is no longer used in many clinics. Instead, measure-
depending on the method used for measuring it, so it
Unfortunately, the clotting time varies widely,
determining clotting time more accurately.
the normal clotting time is 6 to 10 minutes. Procedures
seconds until the blood has clotted. By this method,
blood clotting times. The one most widely used is to
Clotting Time
of platelets.
the bleeding time, but it is especially prolonged by lack
the finger or ear lobe at the time of the test. Lack of
for 1 to 6 minutes. The time depends largely on the
of the finger or lobe of the ear, bleeding ordinarily lasts
When a sharp-pointed knife is used to pierce the tip
Bleeding Time
Blood Coagulation Tests
the level of calcium ion in the blood, which can result
the citrate can, under these conditions, greatly depress
citrate ion may not be removed quickly enough, and
given too rapidly (within fractions of a minute), the
without dire consequences. But if the liver is damaged
Consequently, 500 milliliters of blood that has been
into glucose or metabolized directly for energy.
injection, the citrate ion is removed from the blood
tities of citrate can be injected intravenously. After
oxalate is toxic to the body, whereas moderate quan-
coagulation. Citrate anticoagulants have an important
compound, and the lack of
. The citrate ion combines with
, or
is especially valuable for this purpose, mixed with
prevent coagulation. The negatively charged
oxalate
instance, a soluble
the body. For
Various substances that
blood outside the body as well as in the body. Heparin
XII, with rapid development of clots.
ers allow contact activation of the platelets and Factor
ting mechanism. Conversely, untreated glass contain-
prevents contact activation of platelets and Factor XII,
Chapter 36
Hemostasis and Blood Coagulation
467
the two principal factors that initiate the intrinsic clot-
Heparin can be used for preventing coagulation of
is especially used in surgical procedures in which the
blood must be passed through a heart-lung machine
or artificial kidney machine and then back into the
person.
decrease the concentration
of calcium ions in the blood can also be used for pre-
venting blood coagulation outside
compound mixed in a very
small quantity with a sample of blood causes precipi-
tation of calcium oxalate from the plasma and thereby
decreases the ionic calcium level so much that blood
coagulation is blocked.
Any substance that deionizes the blood calcium will
citrate ion
blood usually in the form of sodium, ammonium
potassium citrate
calcium in the blood to cause an un-ionized calcium
ionic calcium prevents
advantage over the oxalate anticoagulants because
within a few minutes by the liver and is polymerized
rendered incoagulable by citrate can ordinarily be
transfused into a recipient within a few minutes
or if large quantities of citrated blood or plasma are
in tetany and convulsive death.
depth of the wound and the degree of hyperemia in
any one of several of the clotting factors can prolong
Many methods have been devised for determining
collect blood in a chemically clean glass test tube and
then to tip the tube back and forth about every 30
using multiple test tubes have also been devised for
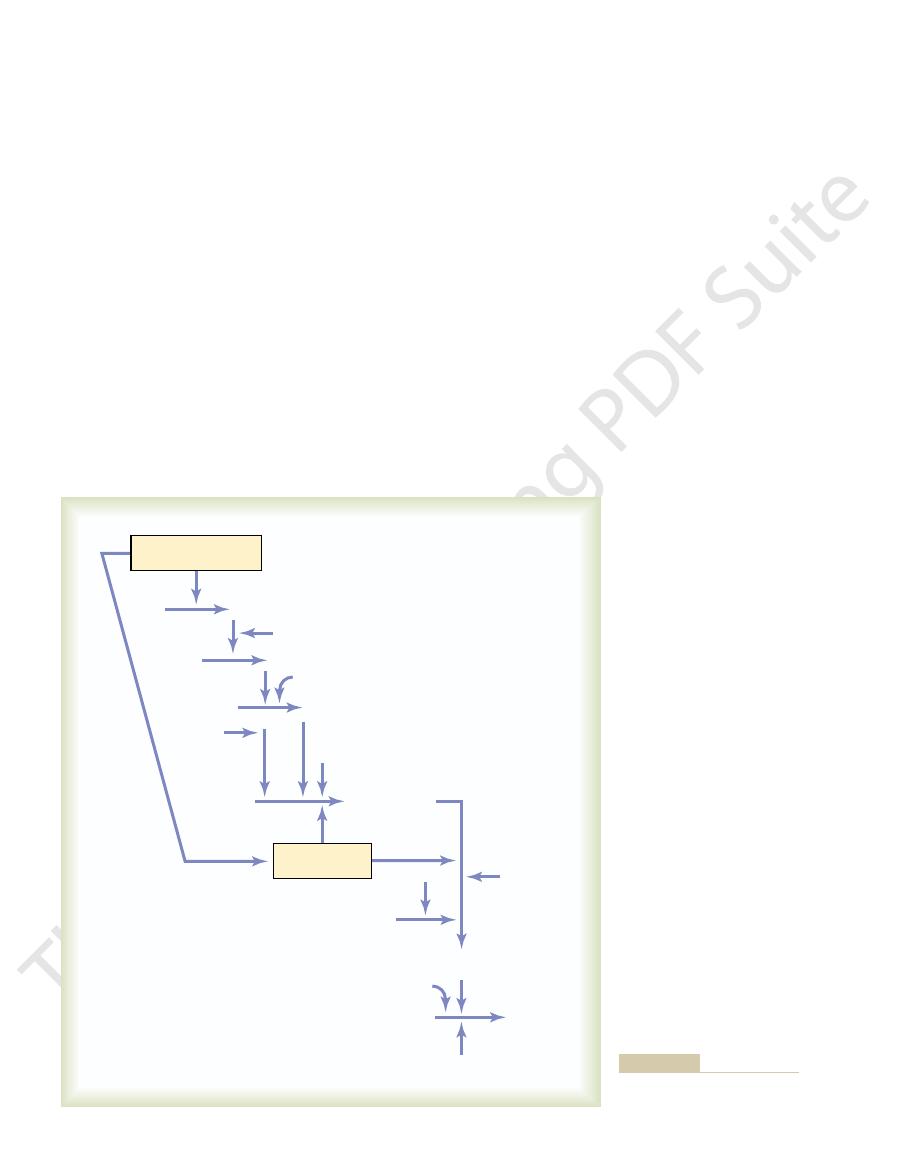
Prothrombin time gives an indication of the concen-
the relation of prothrombin concentration to pro-
Blood removed from the patient is immediately
oxalated so that none of the prothrombin can change
tissue factor is quickly mixed with the oxalated blood.
and the tissue factor activates the prothrombin-to-
thrombin reaction by means of the extrinsic clotting
place is known as the prothrombin time
shortness
is determined mainly by prothrombin con-
0
10
20
30
40
50
60
0
6.25
12.5
25.0
50.0
Concentration (per cent of normal)
100
Prothrombin time
(seconds)
Relation of prothrombin concentration in the blood to “prothrom-
Figure 36–5
bin time.”
they all the same? Br J Haematol 121:12, 2003.
White RH, Ginsberg JS: Low-molecular-weight heparins: are
Intern Med 140:112, 2004.
purpura following splenectomy: a systematic review. Ann
patients with persistent idiopathic thrombocytopenic
Vesely SK, Perdue JJ, Rizvi MA, et al: Management of adult
the hemophilias. J Thromb Haemost 1:1550, 2003.
VandenDriessche T, Collen D, Chuah MK: Gene therapy for
Biol 23:388, 2003.
thrombocytopenic purpura. Arterioscler Thromb Vasc
platelet plug: deficiency of ADAMTS13 causes thrombotic
Tsai HM: Platelet activation and the formation of the
Nephrol 14:1072, 2003.
ment of thrombotic thrombocytopenic purpura. J Am Soc
Tsai HM: Advances in the pathogenesis, diagnosis, and treat-
old disease, new hope. BMJ 327:974, 2003.
Toh CH, Dennis M: Disseminated intravascular coagulation:
Biol 19:2841, 1999.
leading to clinical disorders. Arterioscler Thromb Vasc
Solum NO: Procoagulant expression in platelets and defects
1:922, 2003.
recombinant coagulation factors. J Thromb Haemost
Saenko EL, Ananyeva NM, Shima M, et al: The future of
100:722, 2004.
of hemostasis: implications for therapy. Anesthesiology
Roberts HR, Monroe DM, Escobar MA: Current concepts
347:589, 2002.
Moake JL: Thrombotic microangiopathies. N Engl J Med
Opin Neurol 16:73, 2003.
Lindsberg PJ, Kaste M: Thrombolysis for acute stroke. Curr
lar coagulation. Br J Haematol 124:567, 2004.
Levi M: Current understanding of disseminated intravascu-
bleeding severity: a critical review. Transfusion 44:605,
Koreth R, Weinert C, Weisdorf DJ, Key NS: Measurement of
Intern Med 164:17, 2004.
thrombosis and the postthrombotic syndrome. Arch
Kahn SR, Ginsberg JS: Relationship between deep venous
production. Curr Opin Pediatr 16:15, 2004.
Geddis AE, Kaushansky K: Inherited thrombocytopenias:
stroke: new therapies on trial. Stroke 34:359, 2003.
Fisher M, Brott TG: Emerging therapies for acute ischemic
tor in platelet activation. J Clin Invest 113:340, 2004.
Dorsam RT, Kunapuli SP: Central role of the P2Y12 recep-
bolism. Circulation 109(12 Suppl 1):I4, 2004.
Caprini JA, Glase CJ, Anderson CB, Hathaway K: Labora-
Suppl):18S, 2003.
Brass LF: Thrombin and platelet activation. Chest 124(3
tate the concentration of the factor.
prolonged. The time itself can then be used to quanti-
factor being tested is deficient, the coagulation time is
in the same manner as for prothrombin time. If the
Then the time required for coagulation is determined
are added to oxalated blood all at once.
clotting factors. In each of these tests, excesses of
Tests similar to that for prothrombin time have been
that shown in Figure 36–5, is drawn for the method
Blood Cells, Immunity, and Blood Clotting
468
Unit VI
used so that the prothrombin in the blood can be quan-
tified.
devised to determine the quantities of other blood
calcium ions and all the other factors besides the one
being tested
References
tory markers in the diagnosis of venous thromboem-
toward a molecular understanding of disorders of platelet
2004.
