
hemoglobin in the cell fluid up to about 34 grams in each 100 milliliters of cells.
of red blood cells. This is discussed later.
300,000). Persons living at high altitudes have greater numbers
300,000); in normal women,
In normal men, the average number
would be the case with many other cells.
stretch the membrane greatly and, consequently, does not rupture the cell, as
of cell membrane for the quantity of material inside, deformation does not
into almost any shape. Furthermore, because the normal cell has a great excess
through capillaries. Actually, the red blood cell is a “bag” that can be deformed
The shapes of red blood cells can change remarkably as the cells squeeze
micrometers.
in the center. The average volume of the red blood cell is 90 to 95 cubic
Normal red blood cells, shown in Figure 32–3,
Shape and Size of Red Blood Cells.
(as is true of most proteins), so that the red
expelled into the atmosphere as a body waste product. The hemoglobin in the
) from the tissues to the lungs, where it is reconverted to CO
sandfold. The rapidity of this reaction makes it possible for the water of the
), increasing the rate of this reaction several thou-
carbonic anhydrase,
For instance, they contain a large quantity of
The red blood cells have other functions besides transport of hemoglobin.
globin to remain in the human blood stream, it must exist inside red blood cells.
filtrate each time the blood passes through the capillaries. Therefore, for hemo-
enclosed in red blood cells. When it is free in the plasma of the human being,
some lower animals, hemoglobin circulates as free protein in the plasma, not
which in turn carries oxygen from the lungs to the tissues. In
erythrocytes,
The major function of red blood cells, also known as
Red Blood Cells (Erythrocytes)
tissues.
cells, which are the most abundant cells of the blood
We first present the functions of red blood
With this chapter we begin discussing the
and Polycythemia
Red Blood Cells, Anemia,
C
H
A
P
T
E
R
3
2
419
blood cells
and cells of the macrophage system and lymphatic
system.
and are necessary for the delivery of oxygen to the
is to trans-
port hemoglobin,
about 3 per cent of it leaks through the capillary membrane into the tissue
spaces or through the glomerular membrane of the kidney into the glomerular
an enzyme
that catalyzes the reversible reaction between carbon dioxide (CO
2
) and water
to form carbonic acid (H
2
CO
3
blood to transport enormous quantities of CO
2
in the form of bicarbonate ion
(HCO
3
–
2
and
cells is an excellent acid-base buffer
blood cells are responsible for most of the acid-base buffering power of whole
blood.
are biconcave discs having a mean diameter of about 7.8 micrometers and
a thickness of 2.5 micrometers at the thickest point and 1 micrometer or less
Concentration of Red Blood Cells in the Blood.
of red blood cells per cubic millimeter is 5,200,000 (
±
it is 4,700,000 (
±
Quantity of Hemoglobin in the Cells.
Red blood cells have the ability to concentrate
the starting point in Figure 32–3. Under appropriate
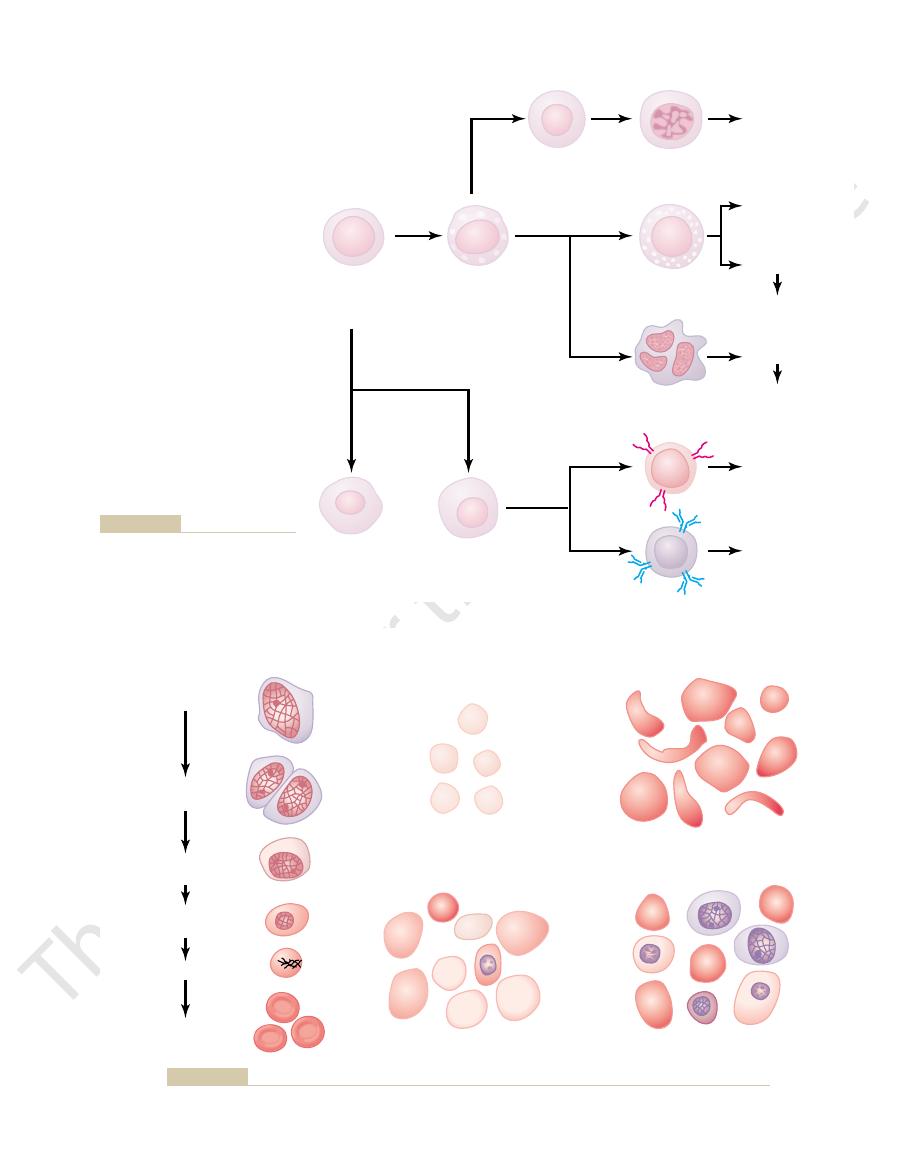
The first cell that can be identified as belonging to the
Stages of Differentiation of Red Blood Cells
diseases cause growth, differentiation, and eventual
case of some of the white blood cells, infectious
erythrocytes, as discussed later in the chapter. In the
ation, and production of greatly increased numbers of
for a long time results in growth induction, differenti-
(red blood cells), exposure of the blood to low oxygen
bone marrow. For instance, in the case of erythrocytes
Formation of the growth inducers and differentia-
differentiation inducers.
ferentiation of the cells. This is the function of another
The growth inducers promote growth but not dif-
specific types of cells.
stem cells, whereas the others induce growth of only
these,
described, each having different characteristics. One of
Four major growth inducers have been
inducers.
growth
CFU-GM, and so forth.
granulocytes and monocytes have the designation
of stem cell. Likewise, colony-forming units that form
colony-forming unit–erythrocyte,
cytes is called a
cells. A committed stem cell that produces erythro-
culture, will produce colonies of specific types of blood
The different committed stem cells, when grown in
committed stem cells.
stem cells, even though they have already become
shown to the right in Figure 32–2. The intermediate-
however, differentiate to form the other cell types
diminish with age. Most of the reproduced cells,
to maintain a supply of these, although their numbers
ing blood cells. As these cells reproduce, a small
derived. Figure 32–2 shows the successive divisions of
from which
The blood cells begin their lives
becomes less productive as age increases.
sternum, ribs, and ilia. Even in these bones, the marrow
of the membranous bones, such as the vertebrae,
blood cells after about age 20 years. Beyond this age,
tibiae, becomes quite fatty and produces no more red
a person is 5 years old. The marrow of the long bones,
As demonstrated in Figure 32–1, the bone marrow
marrow.
Then,
lymph nodes.
production of red blood cells, but reasonable numbers
trimester of gestation, the
yolk sac.
weeks of embryonic life, primitive, nucleated red blood
Production of Red Blood Cells
in a normal woman, 19 milliliters of oxygen can be
with hemoglobin in each 100 milliliters of blood, and
Therefore, in a normal man, a maximum of about 20
oxygen in Chapter 40, each gram of pure hemoglobin
it contains an average of 14 grams per 100 milliliters.
of hemoglobin per 100 milliliters of cells; for women,
of hemoglobin in each respective cell are normal, the
is cells—normally, 40 to 45 per cent) and the quantity
When the hematocrit (the percentage of blood that
value, and the volume of the red cell may also decrease
globin formation is deficient, the percentage of hemo-
near the maximum in each cell. However, when hemo-
people, the percentage of hemoglobin is almost always
globin-forming mechanism. Furthermore, in normal
because this is the metabolic limit of the cell’s hemo-
The concentration does not rise above this value,
Blood Cells, Immunity, and Blood Clotting
420
Unit VI
globin in the cells may fall considerably below this
because of diminished hemoglobin to fill the cell.
whole blood of men contains an average of 15 grams
As discussed in connection with blood transport of
is capable of combining with 1.34 milliliters of oxygen.
milliliters of oxygen can be carried in combination
carried.
Areas of the Body That Produce Red Blood Cells.
In the early
cells are produced in the
During the middle
liver is the main organ for
are also produced in the spleen and
during the last month or so of gestation and after birth,
red blood cells are produced exclusively in the bone
of essentially all bones produces red blood cells until
except for the proximal portions of the humeri and
most red cells continue to be produced in the marrow
Genesis of Blood Cells
Pluripotential Hematopoietic Stem Cells, Growth Inducers, and
Differentiation Inducers.
in the bone marrow from a single type of cell called
the pluripotential hematopoietic stem cell,
all the cells of the circulating blood are eventually
the pluripotential cells to form the different circulat-
portion of them remains exactly like the original
pluripotential cells and is retained in the bone marrow
stage cells are very much like the pluripotential
committed to a particular line of cells and are called
and
the abbreviation CFU-E is used to designate this type
Growth and reproduction of the different stem
cells are controlled by multiple proteins called
interleukin-3, promotes growth and reproduc-
tion of virtually all the different types of committed
set of proteins called
Each of
these causes one type of committed stem cell to dif-
ferentiate one or more steps toward a final adult blood
cell.
tion inducers is itself controlled by factors outside the
formation of specific types of white blood cells that are
needed to combat each infection.
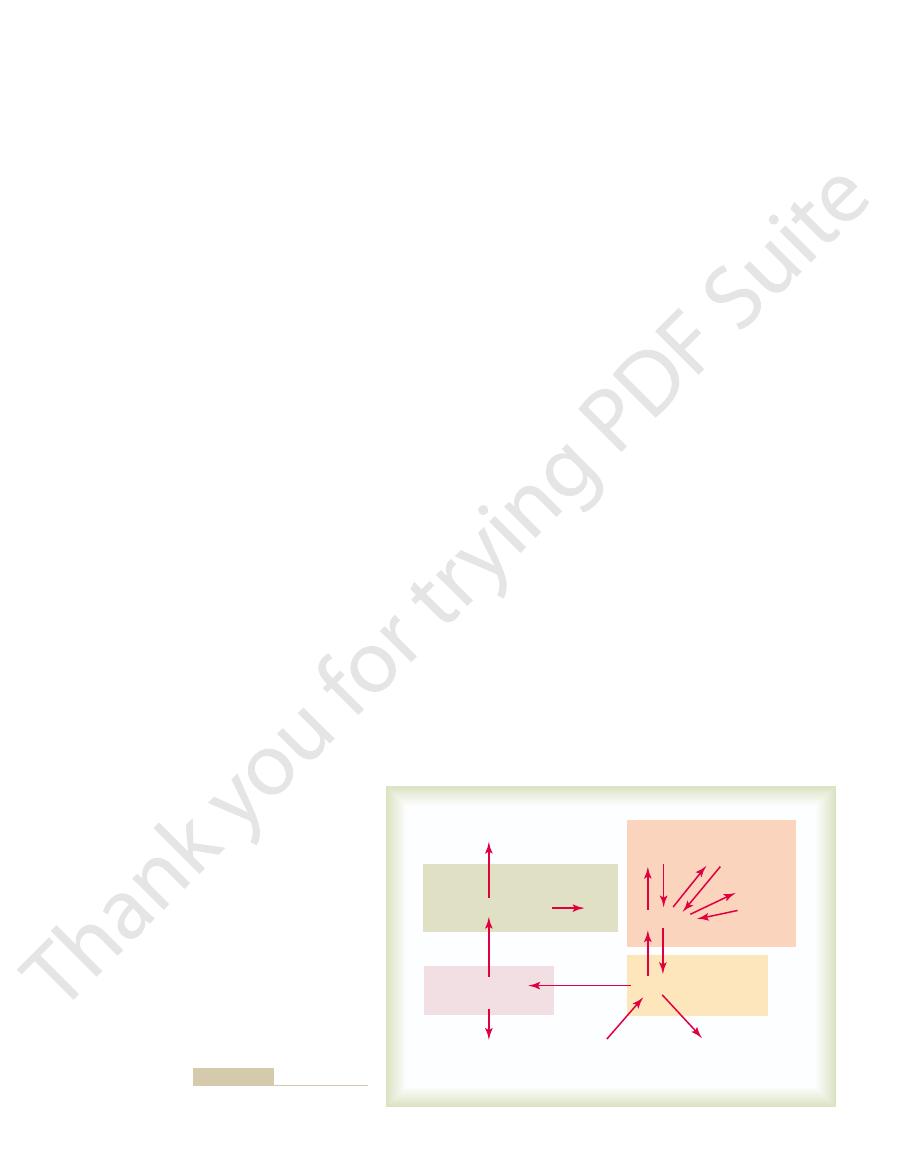
red blood cell series is the proerythroblast, shown at
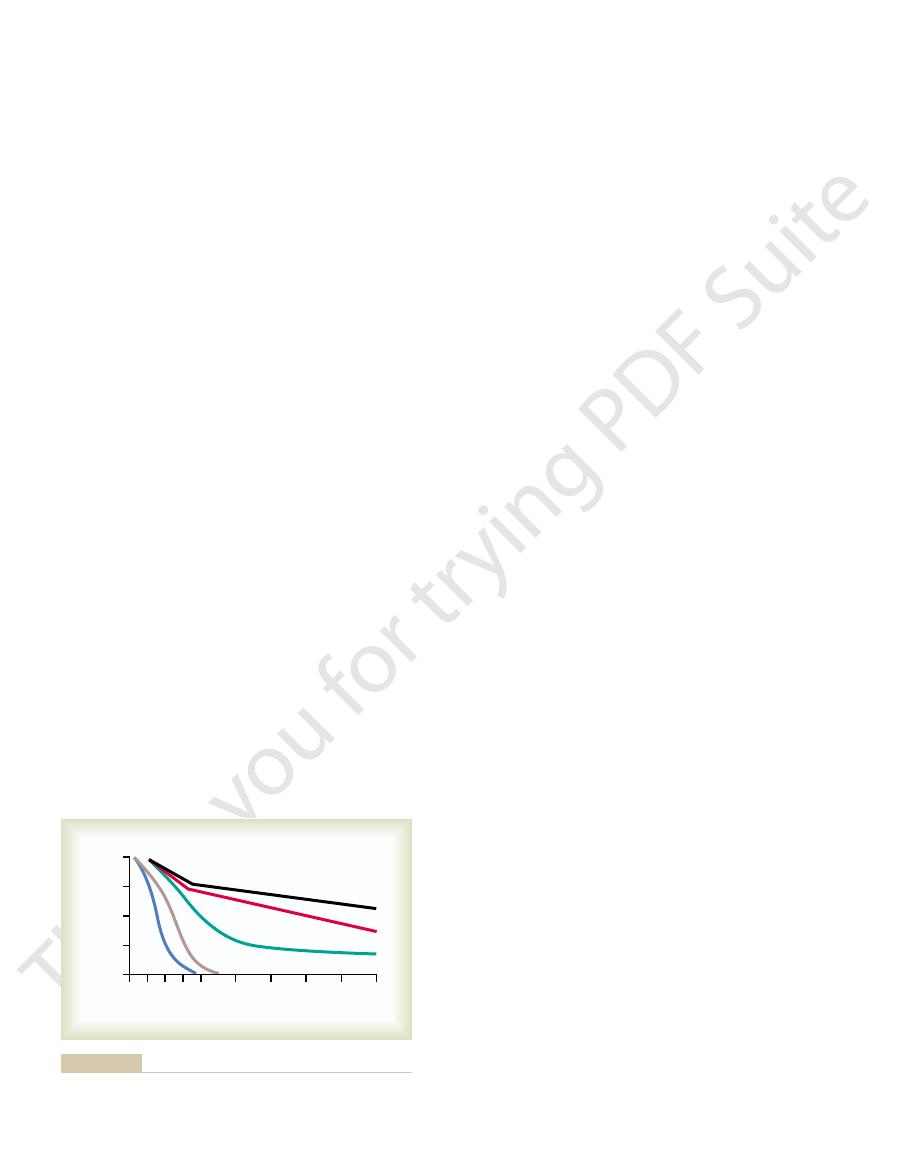
0 5 10 15 20
30
40
50
60
70
0
25
50
75
100
Cellularity (per cent)
Age (years)
Rib
T
ib
ia
(s
h
a
ft)
F
e
m
u
r
(s
haft)
Sternum
Vertebra
different bones at different ages.
Relative rates of red blood cell production in the bone marrow of
Figure 32–1
Red Blood Cells, Anemia, and Polycythemia
Chapter 32
421
PHSC
(Pluripotent
hematopoietic
stem cell)
PHSC
CFU-S
(Colony-forming
unit–spleen)
CFU-B
(Colony-forming
unit–blast)
CFU-E
(Colony-forming
unit–erythrocytes)
CFU-GM
(Colony-forming unit–
granulocytes, monocytes)
CFU-M
(Colony-forming unit–
megakaryocytes)
LSC
(Lymphoid stem cell)
B lymphocytes
T lymphocytes
Megakaryocytes
Macrocytes
Granulocytes
Erythrocytes
Monocytes
(Neutrophils)
(Eosinophils)
(Basophils)
Platelets
in the bone marrow.
blood cells from the original
Formation of the multiple different
Figure 32–2
pluripo-
tent hematopoietic stem cell (PHSC)
Megaloblastic anemia
Erythroblastosis fetalis
Proerythroblast
Basophil
erythroblast
Microcytic,
hypochromic anemia
Sickle cell anemia
Polychromatophil
erythroblast
Orthochromatic
erythroblast
Reticulocyte
Erythrocytes
GENESIS OF RBC
Genesis of normal red blood cells (RBCs) and characteristics of RBCs in different types of anemias.
Figure 32–3
tubular cells, thus stimulating erythropoietin pro-
lial cells secrete the erythropoietin, because anemic
formed mainly in the liver. It is not known exactly
poietin is formed in the kidneys; the remainder is
the normal person, about 90 per cent of all erythro-
Role of the Kidneys in Formation of Erythropoietin.
tion, and the erythropoietin in turn enhances red
when the erythropoietin system is functional, hypoxia
effect in stimulating red blood cell production. But
the absence of erythropoietin, hypoxia has little or no
coprotein with a molecular weight of about 34,000. In
The principal stim-
Erythropoietin Stimulates Red Cell Production, and Its Forma-
duction, with a resultant increase in hematocrit and
lung diseases,
cardiac failure
can also increase the rate of red cell production. This
absorption by the blood as it passes through the lungs,
decreased blood flow through the peripheral vessels,
Various diseases of the circulation that cause
greatly increased. In this case, it is not the concentra-
transported to the tissues, and red cell production is
in the air is greatly decreased, insufficient oxygen is
high altitudes,
the demand for red blood cells in the body.
remaining bone marrow, thereby attempting to supply
especially by x-ray therapy, causes hyperplasia of the
major portions of the bone marrow by any means,
large quantities of red blood cells. Also, destruction of
tion, the bone marrow immediately begins to produce
production. Thus, when a person becomes extremely
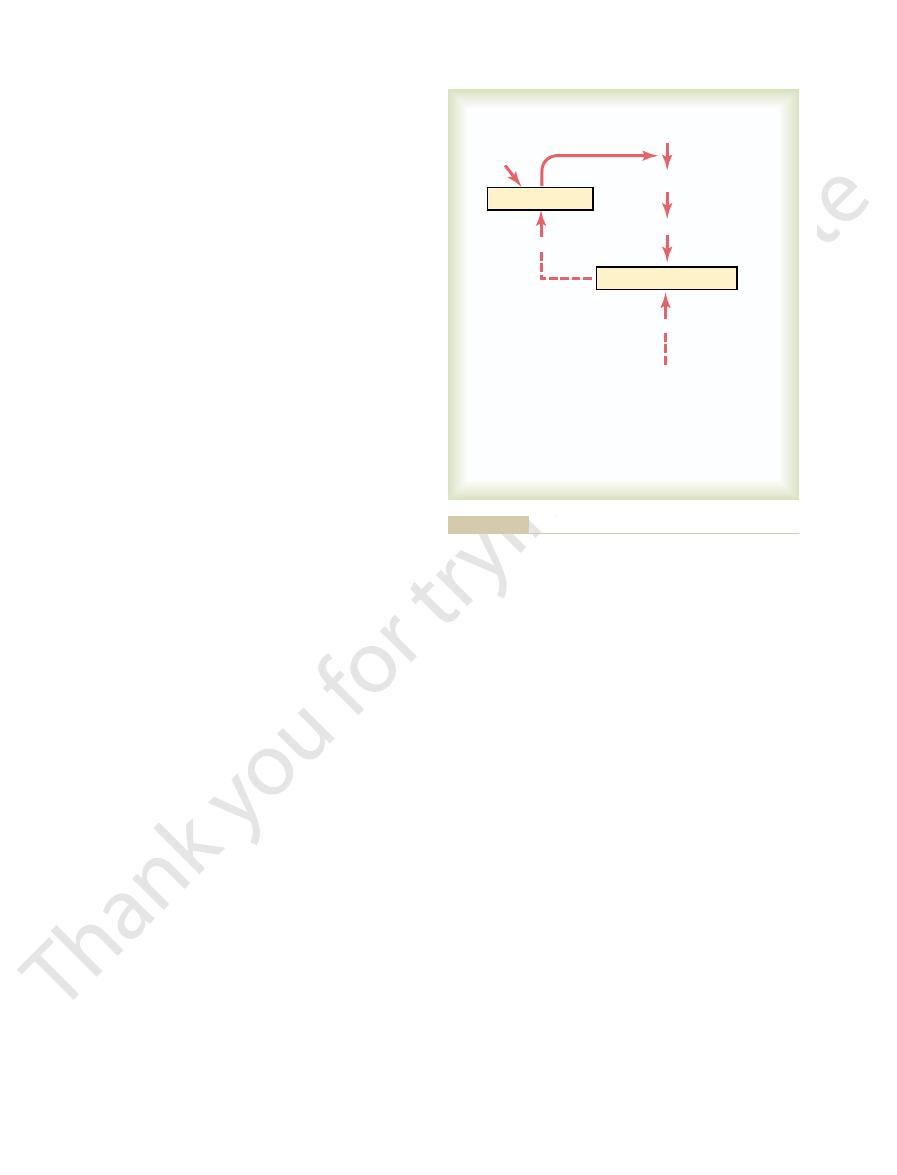
Tissue Oxygenation Is the Most Essential Regulator of Red
and is as follows.
this control mechanism is diagrammed in Figure 32–4
ous that they impede blood flow. What we know about
to the tissues, yet (2) the cells do not become so numer-
system is regulated within narrow limits, so that (1) an
The total mass of red blood cells in the circulatory
of Erythropoietin
Regulation of Red Blood Cell Production—Role
life of the reticulocytes, their concentration among all
mature erythrocyte.
cyte normally disappears within 1 to 2 days, and the
The remaining basophilic material in the reticulo-
organelles. During this reticulocyte stage, the cells pass
tus, mitochondria, and a few other cytoplasmic
material, consisting of remnants of the Golgi appara-
sorbed. The cell at this stage is called a
same time, the endoplasmic reticulum is also reab-
remnant is absorbed or extruded from the cell. At the
the nucleus condenses to a small size, and its final
shown in Figure 32–3, the cells become filled with
little hemoglobin. In the succeeding generations, as
basic dyes; the cell at this time has accumulated very
mature red blood cells. The first-generation cells are
divides multiple times, eventually forming many
Once the proerythroblast has been formed, it
from the CFU-E stem cells.
stimulation, large numbers of these cells are formed
Blood Cells, Immunity, and Blood Clotting
422
Unit VI
called basophil erythroblasts because they stain with
hemoglobin to a concentration of about 34 per cent,
reticulocyte
because it still contains a small amount of basophilic
from the bone marrow into the blood capillaries by
diapedesis (squeezing through the pores of the capil-
lary membrane).
cell is then a
Because of the short
the red cells of the blood is normally slightly less than
1 per cent.
adequate number of red cells is always available to
provide sufficient transport of oxygen from the lungs
Blood Cell Production.
Any condition that causes the
quantity of oxygen transported to the tissues to
decrease ordinarily increases the rate of red blood cell
anemic as a result of hemorrhage or any other condi-
At very
where the quantity of oxygen
tion of red blood cells in the blood that controls red
cell production but the amount of oxygen transported
to the tissues in relation to tissue demand for oxygen.
and particularly those that cause failure of oxygen
is especially apparent in prolonged
and
in many
because the tissue hypoxia
resulting from these conditions increases red cell pro-
usually total blood volume as well.
tion Increases in Response to Hypoxia.
ulus for red blood cell production in low oxygen states
is a circulating hormone called erythropoietin, a gly-
causes a marked increase in erythropoietin produc-
blood cell production until the hypoxia is relieved.
In
where in the kidneys the erythropoietin is formed.
One likely possibility is that the renal tubular epithe-
blood is unable to deliver enough oxygen from the
peritubular capillaries to the highly oxygen-consuming
duction.
Tissue Oxygenation
Red Blood Cells
Proerythroblasts
Hematopoietic Stem Cells
Decreases
Kidney
Decreases
Factors that decrease
oxygenation
1. Low blood volume
2. Anemia
3. Low hemoglobin
4. Poor blood flow
5. Pulmonary disease
Erythropoietin
of red blood cells when tissue oxygenation decreases.
Function of the erythropoietin mechanism to increase production
Figure 32–4

deficiency of intestinal absorption of both folic acid
in many instances of maturation failure, the cause is
. Therefore,
sprue,
malities, such as the frequently occurring small intes-
Also, people with gastrointestinal absorption abnor-
liver). However, it is easily destroyed during cooking.
of green vegetables, some fruits, and meats (especially
Folic acid is a normal constituent
amount.Therefore, 3 to 4 years of defective B
only 1 to 3 micrograms, and the normal storage in the
marrow. The minimum amount of vitamin B
the liver, then released slowly as needed by the bone
trointestinal tract, it is first stored in large quantities in
of intrinsic factor, therefore, causes diminished avail-
and the vitamin together through the membrane. Lack
by the process of pinocytosis, carrying intrinsic factor
mucosal cells in the ileum. (3) Then, vitamin B
Still in the bound state, intrinsic factor binds to specific
from digestion by the gastrointestinal secretions. (2)
. In this bound state, the B
following way: (1) Intrinsic factor binds tightly with
available for absorption by the gut. It does this in the
intrinsic factor,
secretions. The parietal cells of the gastric glands
tract. This often occurs in the disease
from the Gastrointestinal Tract—Pernicious Anemia.
in the process of erythropoiesis.
to one third normal. Therefore, it is said that deficiency
their fragility causes them to have a short life, one half
ing blood, are capable of carrying oxygen normally, but
These poorly formed cells, after entering the circulat-
large, and oval instead of the usual biconcave disc.
itself has a flimsy membrane and is often irregular,
macrocytes,
failing to proliferate rapidly, produce mainly larger
throblastic cells of the bone marrow, in addition to
maturation and cell division. Furthermore, the ery-
ished DNA and, consequently, failure of nuclear
building blocks of DNA. Therefore, lack of either
mation of thymidine triphosphate, one of the essential
Both of these are essential for the synthesis of DNA,
blood cells are two vitamins,
greatly by a person’s nutritional status.
in the entire body. Therefore, as would be expected,
cells, the erythropoietic cells of the bone marrow are
for Vitamin B
Maturation of Red Blood Cells—Requirement
powerful one.
times normal. Therefore, the erythropoietin mecha-
other required nutrients available, the rate of red
are formed available, and if there is plenty of iron and
extreme, when large quantities of erythropoietin
cells are formed by the bone marrow. At the other
In the absence of erythropoietin, few red blood
excess.
tissues despite the low oxygen; at this time, the rate of
new red blood cells. The rapid production of cells con-
normally do, further speeding up the production of
dition, once the proerythroblasts are formed, the
hematopoietic stem cells in the bone marrow. In ad-
From this fact, as well as other studies, it has been
appear in the circulating blood until about 5 days later.
within 24 hours. Yet almost no new red blood cells
minutes to hours, and it reaches maximum production
oxygen, erythropoietin begins to be formed within
When an
Effect of Erythropoietin in Erythrogenesis.
needed by the body.
when the kidneys are destroyed by renal disease, the
When both kidneys are removed from a person or
kidneys to produce this hormone. In particular, both
secretion, which suggests that there might be some
not in the kidneys, stimulates kidney erythropoietin
At times, hypoxia in other parts of the body, but
Red Blood Cells, Anemia, and Polycythemia
Chapter 32
423
nonrenal sensor that sends an additional signal to the
norepinephrine and epinephrine and several of the
prostaglandins stimulate erythropoietin production.
person invariably becomes very anemic because the 10
per cent of the normal erythropoietin formed in other
tissues (mainly in the liver) is sufficient to cause only
one third to one half the red blood cell formation
animal or a person is placed in an atmosphere of low
determined that the important effect of erythropoietin
is to stimulate the production of proerythroblasts from
erythropoietin causes these cells to pass more rapidly
through the different erythroblastic stages than they
tinues as long as the person remains in a low oxygen
state or until enough red blood cells have been pro-
duced to carry adequate amounts of oxygen to the
erythropoietin production decreases to a level that will
maintain the required number of red cells but not an
blood cell production can rise to perhaps 10 or more
nism for controlling red blood cell production is a
12
(Cyanocobalamin) and
Folic Acid
Because of the continuing need to replenish red blood
among the most rapidly growing and reproducing cells
their maturation and rate of production are affected
Especially important for final maturation of the red
vitamin B
12
and folic acid.
because each in a different way is required for the for-
vitamin B
12
or folic acid causes abnormal and dimin-
than normal red cells called
and the cell
of either vitamin B
12
or folic acid causes maturation
failure
Maturation Failure Caused by Poor Absorption of Vitamin
B
12
A
common cause of red blood cell maturation failure is
failure to absorb vitamin B
12
from the gastrointestinal
pernicious
anemia, in which the basic abnormality is an atrophic
gastric mucosa that fails to produce normal gastric
secrete a glycoprotein called
which
combines with vitamin B
12
in food and makes the B
12
the vitamin B
12
12
is protected
receptor sites on the brush border membranes of the
12
is
transported into the blood during the next few hours
ability of vitamin B
12
because of faulty absorption of
the vitamin.
Once vitamin B
12
has been absorbed from the gas-
12
required
each day to maintain normal red cell maturation is
liver and other body tissues is about 1000 times this
12
absorp-
tion are usually required to cause maturation failure
anemia.
Failure of Maturation Caused by Deficiency of Folic Acid
(Pteroylglutamic Acid).
tinal disease called
often have serious difficulty
absorbing both folic acid and vitamin B
12
and vitamin B
12
.
to combine loosely and reversibly with oxygen. This
The most impor-
likely to rupture the cell membranes, leading to sickle
small capillaries, and the spiked ends of the crystals are
sometimes 15 micrometers in length. These make it
type of hemoglobin is exposed to low oxygen, it forms
one point in each of the two beta chains. When this
sickle cell anemia,
molecule as well. For instance, in
globin for oxygen. Abnormalities of the chains can
The types of hemoglobin chains in the hemoglobin
ported by each hemoglobin molecule.
molecule of oxygen, making a total of four molecules
bin molecule; each of these can bind loosely with one
molecule, one finds four iron atoms in each hemoglo-
thetic group containing an atom of iron, and because
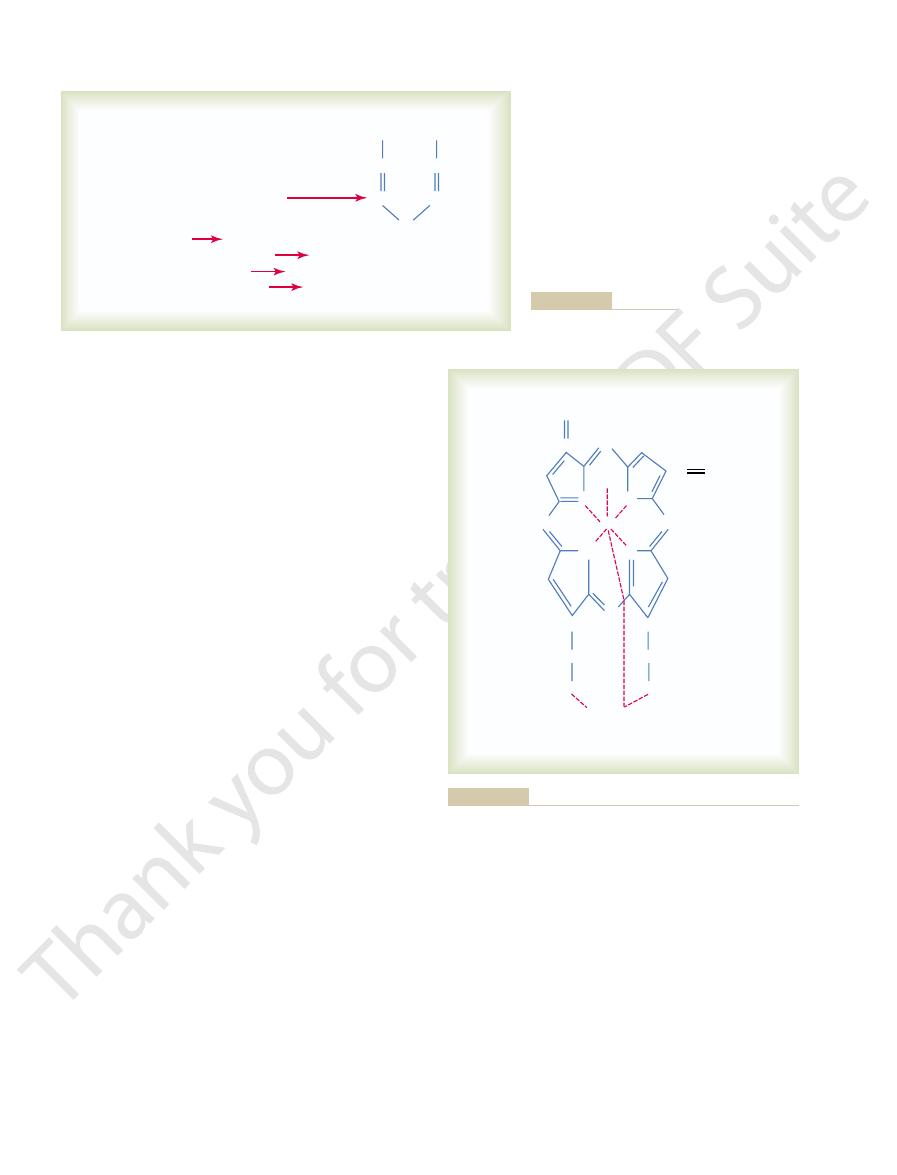
Hemoglobin A has a
two beta chains.
chains
being,
The most
delta chains.
chains, gamma chains,
alpha chains, beta
acid composition of the polypeptide portion. The dif-
subunit hemoglobin chains, depending on the amino
There are several slight variations in the different
molecule.
molecular weight of about 16,000; four of these in turn
(Figure 32–6). Each chain has a
hemoglobin chain
ribosomes, forming a subunit of hemoglobin called a
a long polypeptide chain, a
molecule. Finally, each heme molecule combines with
IX, which then combines with iron to form the
turn, four pyrroles combine to form protoporphyrin
67), binds with glycine to form a pyrrole molecule. In
in the Krebs metabolic cycle (as explained in Chapter
formation of hemoglobin. First, succinyl-CoA, formed
Figure 32–5 shows the basic chemical steps in the
cytes.
the bone marrow and pass into the blood stream, they
the red blood cells. Therefore, when reticulocytes leave
blasts and continues even into the reticulocyte stage of
Formation of Hemoglobin
Blood Cells, Immunity, and Blood Clotting
424
Unit VI
Synthesis of hemoglobin begins in the proerythro-
continue to form minute quantities of hemoglobin for
another day or so until they become mature erythro-
heme
globin synthesized by
bind together loosely to form the whole hemoglobin
ferent types of chains are designated
and
common form of hemoglobin in the adult human
hemoglobin A, is a combination of two alpha
and
molecular weight of 64,458.
Because each hemoglobin chain has a heme pros-
there are four hemoglobin chains in each hemoglobin
of oxygen (or eight oxygen atoms) that can be trans-
molecule determine the binding affinity of the hemo-
alter the physical characteristics of the hemoglobin
the
amino acid valine is substituted for glutamic acid at
elongated crystals inside the red blood cells that are
almost impossible for the cells to pass through many
cell anemia.
Combination of Hemoglobin with Oxygen.
tant feature of the hemoglobin molecule is its ability
ability is discussed in detail in Chapter 40 in relation
chains
hemoglobin A
heme + polypeptide
hemoglobin chain (
4 pyrrole
protoporphyrin IX
2 succinyl-CoA + 2 glycine
A
C
HC
P
C
N
H
(pyrrole)
CH
protoporphyrin IX + Fe
++
heme
a
or
b
)
2
a
chains + 2
b
I.
II.
III.
IV.
V.
Formation of hemoglobin.
Figure 32–5
COOH
COOH
Fe
CH
CH
CH
CH
2
CH
2
H
3
C
CH
3
H
C
A
B
N
(–)
N
O
2
CH
3
H
3
C
C
CH
2
CH
2
CH
2
CH
2
C
H
D
HC
N
(–)
N
Polypepitide
(hemoglobin chain–
a
or
b
)
four heme chains that bind together to form the hemoglobin
Basic structure of the hemoglobin molecule, showing one of the
Figure 32–6
molecule.
—that is, red cells that contain
hypochromic anemia
of transferrin in their blood, failure to transport iron
sized. In people who do not have adequate quantities
directly to the mitochondria, where heme is synthe-
endocytosis. There the transferrin delivers the iron
its bound iron, it is ingested into the erythroblasts by
of erythroblasts in the bone marrow. Then, along with
plasma to the areas of the body where it is needed. A
When the quantity of iron in the plasma falls low,
microscope.
be seen in the cell cytoplasm only with the electron
scopically as large particles. In contrast, ferritin parti-
can accommodate. Hemosiderin collects in cells in the
This is especially true when the total quantity of iron
large amount. This iron stored as ferritin is called
iron radicals with this large molecule; therefore,
has a molecular weight of about 460,000, and
In the cell cytoplasm, iron combines mainly with
cells of the bone marrow.
liver hepatocytes and less in the reticuloendothelial
released to any tissue cell at any point in the body.
bound in the transferrin and, consequently, can be
then transported in the plasma. The iron is loosely
iron is absorbed from the small intestine, it immedi-
Figure 32–7 and can be explained as follows: When
Transport, storage, and
Transport and Storage of Iron.
parenchymal cells, principally in the form of ferritin.
use, mainly in the reticuloendothelial system and liver
blood plasma, and 15 to 30 per cent is stored for later
compounds that promote intracellular oxidation, 0.1
globin, 1 per cent is in the form of the various heme
hemoglobin. About 4 per cent is in the form of myo-
grams, about 65 per cent of which is in the form of
The total quantity of iron in the body averages 4 to 5
stand the means by which iron is utilized in the body.
), it is important to under-
oxidase, peroxidase, catalase
myoglobin, cytochromes, cytochrome
the body (e.g.,
loose, readily reversible combination, it is released into
oxygen atoms) to the tissues, where, because of the
thermore, the oxygen does not become ionic oxygen
bond, so that the combination is easily reversible. Fur-
bonds of the iron atom. This is an extremely loose
bonds of the iron in the hemoglobin molecule. Instead,
of oxygen is much lower than in the lungs.
peripheral tissue capillaries, where the gaseous tension
to respiration, because the primary function of hemo-
Red Blood Cells, Anemia, and Polycythemia
Chapter 32
425
globin in the body is to combine with oxygen in the
lungs and then to release this oxygen readily in the
Oxygen does not combine with the two positive
it binds loosely with one of the so-called coordination
but is carried as molecular oxygen (composed of two
the tissue fluids still in the form of molecular oxygen
rather than ionic oxygen.
Iron Metabolism
Because iron is important for the formation not only
of hemoglobin but also of other essential elements in
per cent is combined with the protein transferrin in the
metabolism of iron in the body are diagrammed in
ately combines in the blood plasma with a beta
globulin, apotransferrin, to form transferrin, which is
Excess iron in the blood is deposited especially in the
a protein, apoferritin, to form ferritin. Apoferritin
varying quantities of iron can combine in clusters of
ferritin may contain only a small amount of iron or a
storage iron.
Smaller quantities of the iron in the storage pool are
in an extremely insoluble form called hemosiderin.
in the body is more than the apoferritin storage pool
form of large clusters that can be observed micro-
cles are so small and dispersed that they usually can
some of the iron in the ferritin storage pool is removed
easily and transported in the form of transferrin in the
unique characteristic of the transferrin molecule is that
it binds strongly with receptors in the cell membranes
to the erythroblasts in this manner can cause severe
much less hemoglobin than normal.
Hemoglobin
Transferrin
Ferritin
Hemosiderin
Macrophages
Degrading hemoglobin
Free
iron
Tissues
Bilirubin (excreted)
–Fe
Red Cells
Blood loss – 0.7 mg Fe
daily in menses
Fe
++
absorbed
(small intestine)
Fe excreted–0.6 mg daily
Plasma
Free iron
Heme
Enzymes
Iron transport and metabolism.
Figure 32–7

chemicals, and even drugs to which the person might
Likewise, excessive x-ray treatment, certain industrial
marrow, followed in a few weeks by lethal anemia.
functioning bone marrow. For instance, a person
Bone marrow aplasia
which is shown in Figure 32–3.
hypochromic anemia,
microcytic,
little hemoglobin inside them, giving rise to
globin as rapidly as it is lost. Red cells are then pro-
In chronic blood loss, a person frequently cannot
to 6 weeks.
If a second hemorrhage does not occur, the red blood
but this leaves a low concentration of red blood cells.
replaces the fluid portion of the plasma in 1 to 3 days,
After rapid hemorrhage, the body
anemia and their physiologic causes are the following.
or too little hemoglobin in the cells. Some types of
Anemia means deficiency of hemoglobin in the blood,
liver into the bile; this is discussed in relation to liver
macrophages, through a series of stages, into the bile
storage in the form of ferritin. The porphyrin portion
pass it back into the blood, to be carried by transfer-
bone marrow. During the next few hours to days, the
many parts of the body, but especially by the Kupffer
phagocytized almost immediately by macrophages in
and release their hemoglobin, the hemoglobin is
When red blood cells burst
considerably.
cell. When the spleen is removed, the number of old
cells must pass, are only 3 micrometers wide, in com-
trabeculae of the red pulp, through which most of the
of the spleen. There, the spaces between the structural
in the spleen, where they squeeze through the red pulp
of the circulation. Many of the red cells self-destruct
Once the red cell membrane becomes fragile, the
and more fragile, presumably because their life
progressively less active, and the cells become more
Even so, the metabolic systems of old red cells become
(4) prevent oxidation of the proteins in the red cells.
globin in the ferrous form rather than ferric form, and
transport of ions, (3) keep the iron of the cells’ hemo-
ity of the cell membrane, (2) maintain membrane
triphosphate. These enzymes also (1) maintain pliabil-
cytoplasmic enzymes that are capable of metabolizing
mitochondria, or endoplasmic reticulum, they do have
Even though mature red cells do not have a nucleus,
culate an average of 120 days before being destroyed.
marrow into the circulatory system, they normally cir-
When red blood cells are delivered from the bone
Life Span and Destruction of Red
ate probably five or more times normal. Thus, total
become depleted, the rate of absorption can acceler-
decreased. Conversely, when the iron stores have
already combined with iron, the rate of additional iron
When the body has become saturated with iron so that
Regulation of Total Body Iron by Controlling Rate of Absorption.
of iron are present in the food, only small proportions
day. This means that even when tremendous quantities
slow, at a maximum rate of only a few milligrams per
carrying its iron store, is absorbed into the epithelial
cells. Then, by pinocytosis, the transferrin molecule,
It, in turn, is attracted to and binds with
sources of iron in the diet. This combination is called
myoglobin from meat, two of the most important
with certain iron compounds, such as hemoglobin and
Here, the apotransferrin binds with free iron and also
into the bile,
mostly by the following mechanism. The liver secretes
Iron is absorbed from all parts of the small intestine,
Absorption of Iron from the Intestinal Tract
term iron loss to an average of about 1.3 mg/day.
woman, additional menstrual loss of blood brings long-
quantities of iron are lost when bleeding occurs. For a
of iron each day, mainly into the feces. Additional
is ingested by monocyte-macrophage cells. There,
are destroyed, the hemoglobin released from the cells
When red blood cells have lived their life span and
Blood Cells, Immunity, and Blood Clotting
426
Unit VI
iron is liberated and is stored mainly in the ferritin
pool to be used as needed for the formation of new
hemoglobin.
Daily Loss of Iron.
A man excretes about 0.6 milligram
moderate amounts of apotransferrin
which flows through the bile duct into the duodenum.
transferrin.
receptors in the membranes of the intestinal epithelial
cells and later released into the blood capillaries
beneath these cells in the form of plasma transferrin.
Iron absorption from the intestines is extremely
can be absorbed.
essentially all apoferritin in the iron storage areas is
absorption from the intestinal tract becomes greatly
body iron is regulated mainly by altering the rate of
absorption.
Blood Cells
glucose and forming small amounts of adenosine
processes wear out.
cell ruptures during passage through some tight spot
parison with the 8-micrometer diameter of the red
abnormal red cells circulating in the blood increases
Destruction of Hemoglobin.
cells of the liver and macrophages of the spleen and
macrophages release iron from the hemoglobin and
rin either to the bone marrow for the production of
new red blood cells or to the liver and other tissues for
of the hemoglobin molecule is converted by the
pigment bilirubin, which is released into the blood and
later removed from the body by secretion through the
function in Chapter 70.
Anemias
which can be caused by either too few red blood cells
Blood Loss Anemia.
cell concentration usually returns to normal within 3
absorb enough iron from the intestines to form hemo-
duced that are much smaller than normal and have too
Aplastic Anemia.
means lack of
exposed to gamma ray radiation from a nuclear bomb
blast can sustain complete destruction of bone
be sensitive can cause the same effect.
; this allows these people to perform
pheric oxygen is very low. The blood count is generally
altitudes of 14,000 to 17,000 feet, where the atmos-
A common type of secondary polycythemia, called
produce large quantities of extra red blood cells. This
failure, the blood-forming organs automatically
oxygen delivery to the tissues, such as in cardiac
air, such as at high altitudes, or because of failure of
Whenever the tissues become
Secondary Polycythemia.
ensues.
acute cardiac failure
tissue hypoxia results, and
greatly increases tissue demand for oxygen, extreme
pumping.
Consequently,
during exercise,
which
begins to exercise, the heart is not capable of pumping
the tissues. However, when a person with anemia
blood carries only small quantities of oxygen, the rate
anemia, because even though each unit quantity of
The increased cardiac output in anemia partially
increased cardiac
sometimes three to four times normal. Thus, one of the
tissue blood vessels to dilate, allowing a further
Moreover, hypoxia resulting from diminished trans-
to the heart, thereby greatly increasing cardiac output.
eral blood vessels, so that far greater than normal
water rather than the normal value of about 3. This
centration of red blood cells. In severe anemia, the
Chapter 14, depends almost entirely on the blood con-
The viscosity of the blood, which was discussed in
Effects of Anemia on Function of the
of blood. The extremely rapid formation of new red
causing the child to be born with serious anemia. This
Rh-positive cells fragile, leading to rapid rupture and
an Rh-negative mother. These antibodies make the
erythroblastosis fetalis,
few hours and, often, death.
Once the process starts, it progresses rapidly, eventu-
red cells, which causes a further decrease in oxygen
in the tissues causes sickling, which leads to ruptured
sickle cell disease “crisis,” in which low oxygen tension
fragile, leading to serious anemia. Such patients fre-
the cell membrane, so that the cells become highly
cave disc. The precipitated hemoglobin also damages
the red blood cell. These crystals elongate the cell and
tions of oxygen, it precipitates into long crystals inside
When this hemoglobin is exposed to low concentra-
globin molecule, as explained earlier in the chapter.
globin S,
per cent of West African and American blacks, the cells
sickle cell anemia,
cular beds, they are easily ruptured by even slight
membrane structure of the biconcave discs. On passing
because they do not have the normal loose, baglike cell
These cells cannot withstand compression forces
rather than being biconcave discs.
hereditary spherocytosis,
following.
results. Some of these types of anemia are the
faster than they can be formed, and serious anemia
normal in some hemolytic diseases, the life span of the
formed may be normal, or even much greater than
spleen. Even though the number of red blood cells
they go through the capillaries, especially through the
make the cells fragile, so that they rupture easily as
blood cells, many of which are hereditarily acquired,
adequate number of red cells.
rupture easily, leaving the person in dire need of an
shapes, and have fragile membranes. These cells
that are formed are mostly oversized, have bizarre
form normal numbers of red blood cells, those red cells
develop megaloblastic anemia. Because in these states
vitamin B compounds are poorly absorbed, often
, and other
tinal sprue, in which folic acid, vitamin B
megaloblastic anemia. Also, patients who have intes-
Thus, atrophy of the stomach mucosa,
megaloblasts.
cells grow too large, with odd shapes, and are called
erythroblasts in the bone marrow. As a result, the red
stomach mucosa, one can readily understand that loss
, folic acid, and intrinsic factor from the
Red Blood Cells, Anemia, and Polycythemia
Chapter 32
427
Megaloblastic Anemia.
Based on the earlier discussions
of vitamin B
12
of any one of these can lead to slow reproduction of
as occurs in pernicious anemia, or loss of the entire
stomach after surgical total gastrectomy can lead to
12
the erythroblasts cannot proliferate rapidly enough to
Hemolytic Anemia.
Different abnormalities of the red
fragile red cell is so short that the cells are destroyed
In
the red cells are very
small and spherical
through the splenic pulp and some other tight vas-
compression.
In
which is present in 0.3 to 1.0
have an abnormal type of hemoglobin called hemo-
containing faulty beta chains in the hemo-
give it the appearance of a sickle rather than a bicon-
quently experience a vicious circle of events called a
tension and still more sickling and red cell destruction.
ating in a serious decrease in red blood cells within a
In
Rh-positive red blood
cells in the fetus are attacked by antibodies from
is discussed in Chapter 35 in relation to the Rh factor
cells to make up for the destroyed cells in erythro-
blastosis fetalis causes a large number of early blast
forms of red cells to be released from the bone marrow
into the blood.
Circulatory System
blood viscosity may fall to as low as 1.5 times that of
decreases the resistance to blood flow in the periph-
quantities of blood flow through the tissues and return
port of oxygen by the blood causes the peripheral
increase in the return of blood to the heart and
increasing the cardiac output to a still higher level—
major effects of anemia is greatly
output, as well as increased pumping workload on the
heart.
offsets the reduced oxygen-carrying effect of the
of blood flow may be increased enough so that almost
normal quantities of oxygen are actually delivered to
much greater quantities of blood than it is already
Polycythemia
hypoxic because of too little oxygen in the breathed
condition is called secondary polycythemia, and the
red cell count commonly rises to 6 to 7 million/mm
3
,
about 30 per cent above normal.
physiologic polycythemia, occurs in natives who live at
6 to 7 million/mm
3
Suppl):1051, 2004.
Trigg ME: Hematopoietic stem cells. Pediatrics 113(4
2:237, 2003.
management of polycythemia vera. Curr Hematol Rep
Tefferi A: A contemporary approach to the diagnosis and
25:168, 2004.
Shah S, Vega R: Hereditary spherocytosis. Pediatr Rev
an old disease. N Engl J Med 350:2383, 2004.
Pietrangelo A: Hereditary hemochromatosis—a new look at
ders. Curr Opin Mol Ther 5:508, 2003.
Persons DA: Update on gene therapy for hemoglobin disor-
relevance to the kidney. J Am Soc Nephrol 14:2712, 2003.
Maxwell P: HIF-1: an oxygen response system with special
Oncologist 8(Suppl 1):15, 2003.
Lappin T: The cellular biology of erythropoietin receptors.
Cell 117:285, 2004.
acts: molecular control of mammalian iron metabolism.
Hentze MW, Muckenthaler MU, Andrews NC: Balancing
Rev Nutr 21:1, 2001.
Hallberg L: Perspectives on nutritional iron deficiency. Annu
Integr Comp Physiol 286:R977, 2004.
of erythropoietin gene expression. Am J Physiol Regul
Fandrey J: Oxygen-dependent and tissue-specific regulation
327:1151, 2003.
Claster S, Vichinsky EP: Managing sickle cell disease. BMJ
Hematol Rep 3:107, 2004.
new insights in iron transport and metabolism. Curr
Brissot P, Troadec MB, Loreal O: The clinical relevance of
bin? Nat Rev Drug Discov 3:152, 2004.
Alayash AI: Oxygen therapeutics: can we tame haemoglo-
ruddy complexion with a bluish (cyanotic) tint to the
fore, a person with polycythemia vera ordinarily has a
the red color of the oxygenated hemoglobin. There-
normal quantity of hemoglobin is deoxygenated. The
before entering the venous plexus, a larger than
this plexus is greatly increased. Further, because the
plexus. In polycythemia vera, the quantity of blood in
The color of the skin depends to a great extent on
regulations fail, and hypertension develops.
arterial pressure. Beyond certain limits, however, these
increase peripheral resistance and, thereby, increase
offset the tendency for increased blood viscosity to
them, the arterial pressure is elevated. This means that
with polycythemia, although in about one third of
The arterial pressure is also normal in most people
neutralize each other.
from normal, because these two factors more or less
Actually, the cardiac output in polycythemia is not far
cythemia, which tends to
versely, the blood volume is greatly increased in poly-
the rate of venous return to the heart. Con-
as discussed in Chapter 20, increasing blood viscosity
blood vessels is often very sluggish. In accordance with
in polycythemia, blood flow through the peripheral
Effect of Polycythemia on Function of
3 times the viscosity of water to 10 times that of water.
cythemia vera sometimes increases from the normal of
the viscous blood; the viscosity of the blood in poly-
addition, many blood capillaries become plugged by
entire vascular system becomes intensely engorged. In
some occasions to almost twice normal. As a result, the
increase, but the total blood volume also increases, on
In polycythemia vera, not only does the hematocrit
type of breast cell. It usually causes excess production
many cells are already present. This causes excess pro-
hemocytoblastic cells that produce the blood cells. The
cythemia vera is caused by a genetic aberration in the
cent instead of the normal 40 to 45 per cent. Poly-
people who have physiologic polycythemia, others
Polycythemia Vera (Erythremia).
rarefied atmosphere.
Blood Cells, Immunity, and Blood Clotting
428
Unit VI
reasonably high levels of continuous work even in a
In addition to those
have a pathological condition known as polycythemia
vera, in which the red blood cell count may be 7 to 8
million/mm
3
and the hematocrit may be 60 to 70 per
blast cells no longer stop producing red cells when too
duction of red blood cells in the same manner that a
breast tumor causes excess production of a specific
of white blood cells and platelets as well.
the Circulatory System
Because of the greatly increased viscosity of the blood
the factors that regulate return of blood to the heart,
decreases
increase venous return.
the blood pressure–regulating mechanisms can usually
the quantity of blood in the skin subpapillary venous
blood passes sluggishly through the skin capillaries
blue color of all this deoxygenated hemoglobin masks
skin.
References
