30 mEq/day to a high level of 300 mEq/day. Within 2 to 3 days after raising the
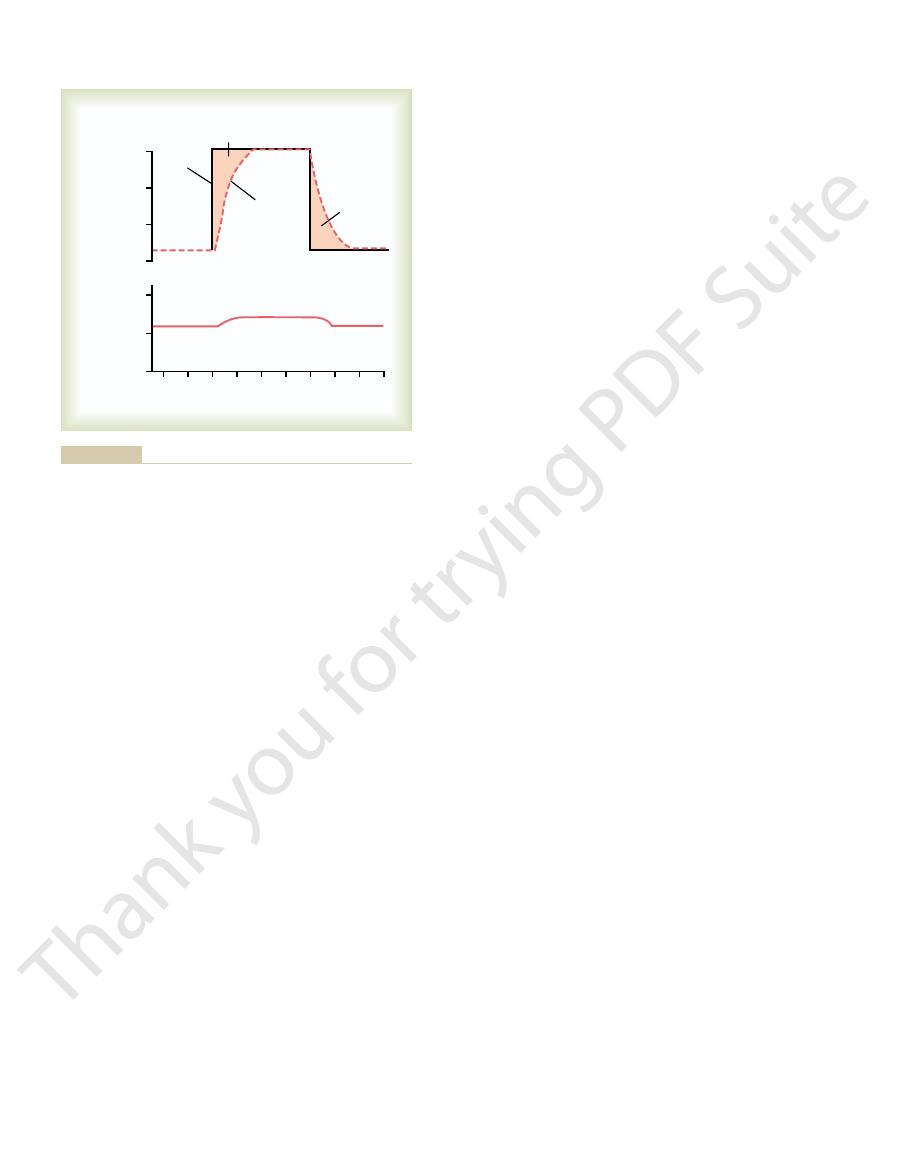
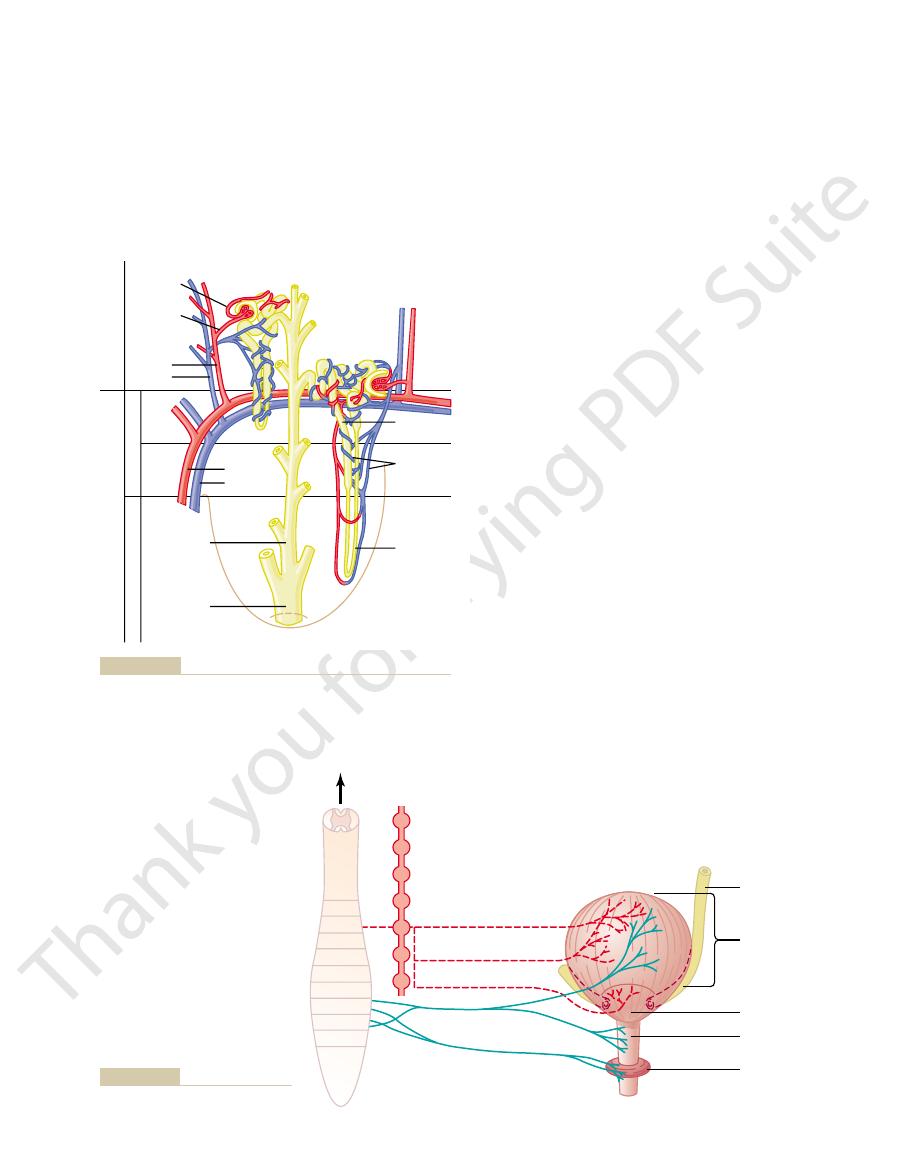
match the intake of various substances. Figure 26–1 shows the response of the
and drinking habits, requiring the kidneys to adjust their excretion rates to
Intake of water and many electrolytes is governed mainly by a person’s eating
less than excretion, the amount of that substance in the body will decrease.
excretion, the amount of that substance in the body will increase. If intake is
tion of water and electrolytes must precisely match intake. If intake exceeds
For maintenance of homeostasis, excre-
Regulation of Water and Electrolyte Balances.
the body or ingested, such as pesticides, drugs, and food additives.
eliminated from the body as rapidly as they are produced. The kidneys also
These waste products must be
metabolites of various hormones.
bilirubin), and
end products of hemoglobin breakdown
metabolism that are no longer needed by the body. These products include
The kidneys are the primary means for eliminating waste products of
Excretion of Metabolic Waste Products, Foreign Chemicals, Drugs, and Hormone Metabo-
Secretion, metabolism, and excretion of hormones
functions, including the following:
of renal excretion, it is important to recognize that the kidneys serve multiple
needs of the body. Ultimately, the kidneys “clear” unwanted substances from
and removing substances from the filtrate at variable rates, depending on the
The kidneys perform their most important functions by filtering the plasma
cells necessary for them to perform their various activities.
This regulatory function of the kidneys maintains the stable environment of the
excretion or metabolic consumption) is maintained in large part by the kidneys.
the body fluids. For water and virtually all electrolytes in the body, the balance
metabolism. A second function that is especially
Blood Flow, and Their Control
I. Glomerular Filtration, Renal
Urine Formation by the Kidneys:
C
H
A
P
T
E
R
2
6
307
Multiple Functions of the
Kidneys in Homeostasis
Most people are familiar with one important func-
tion of the kidneys—to rid the body of waste mate-
rials that are either ingested or produced by
critical is to control the volume and composition of
between intake (due to ingestion or metabolic production) and output (due to
the filtrate (and therefore from the blood) by excreting them in the urine while
returning substances that are needed back to the blood.
Although this chapter and the next few chapters focus mainly on the control
∑ Excretion of metabolic waste products and foreign chemicals
∑ Regulation of water and electrolyte balances
∑ Regulation of body fluid osmolality and electrolyte concentrations
∑ Regulation of arterial pressure
∑ Regulation of acid-base balance
∑
∑ Gluconeogenesis
lites.
urea
(from the metabolism of amino acids), creatinine (from muscle creatine), uric
acid (from nucleic acids),
(such as
eliminate most toxins and other foreign substances that are either produced by
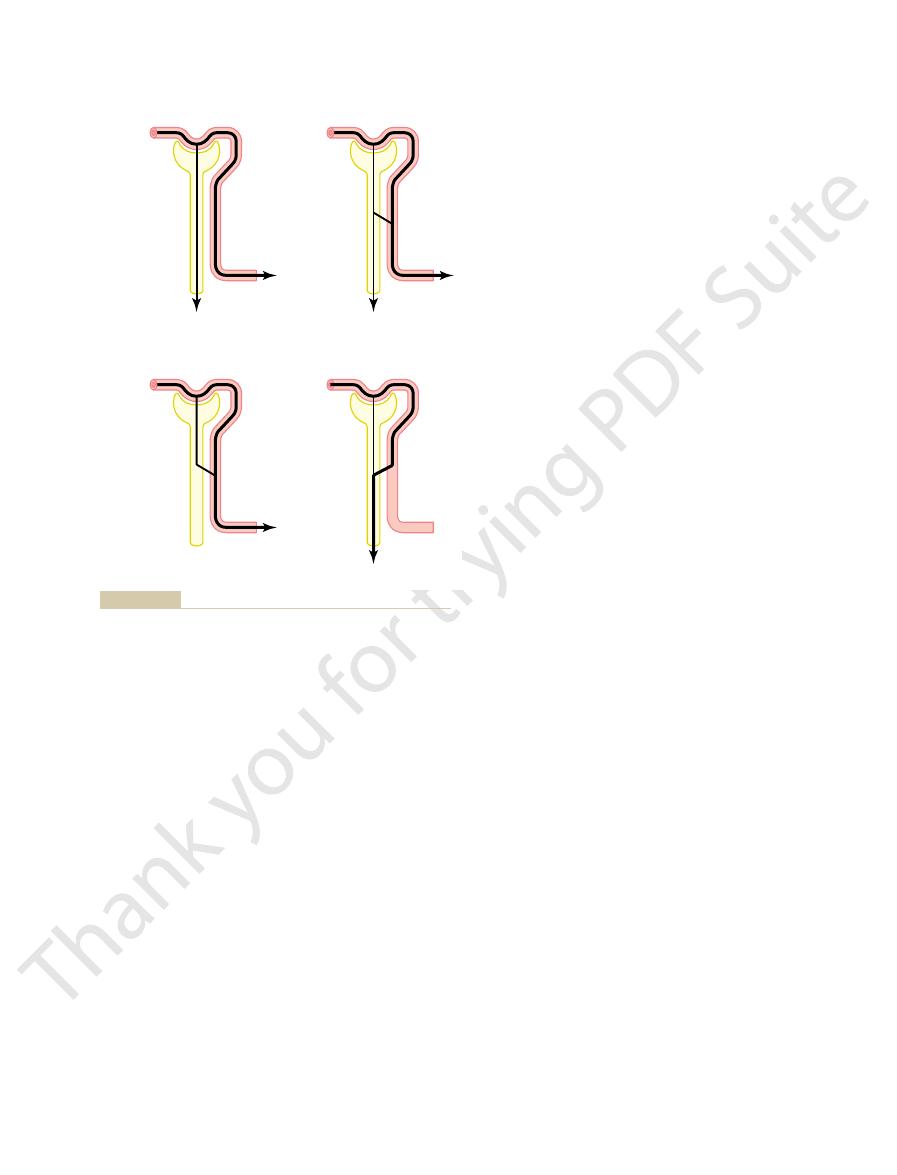
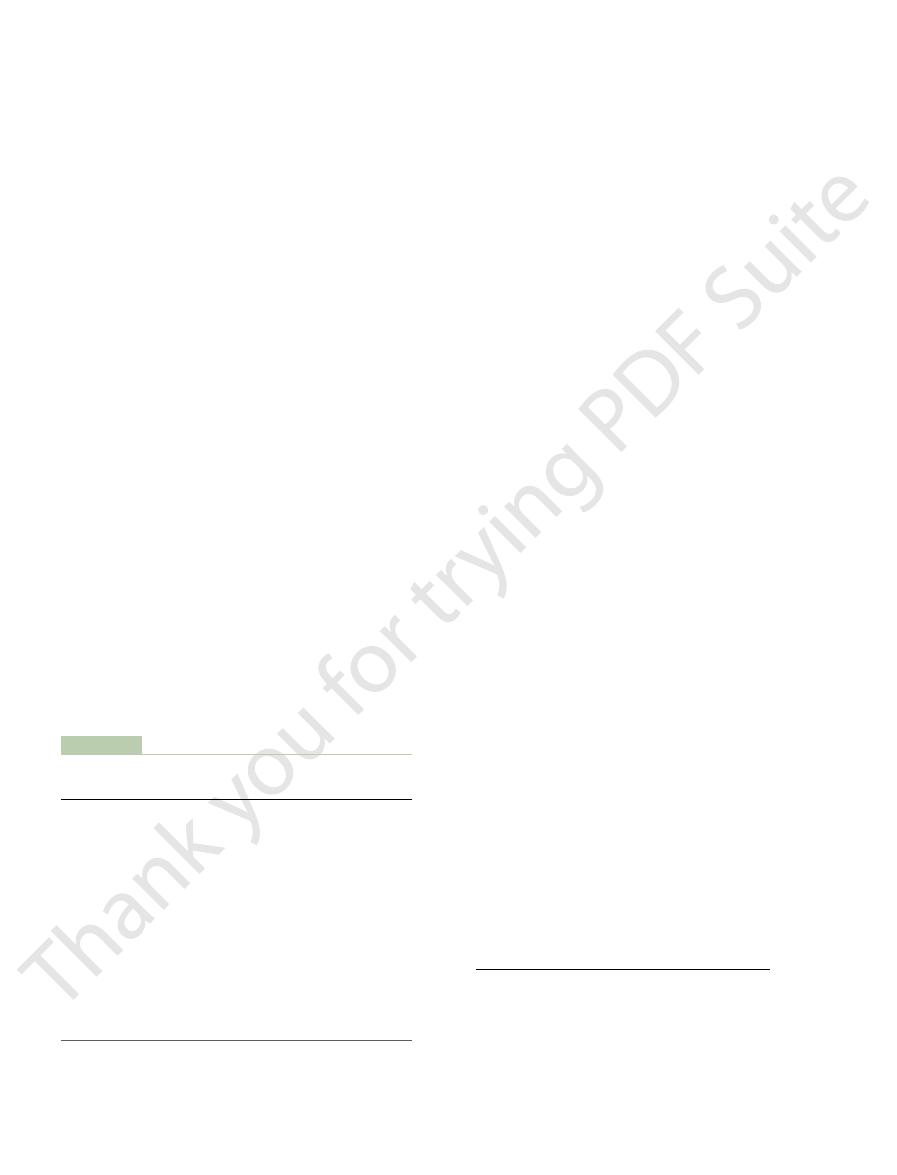
kidneys to a sudden 10-fold increase in sodium intake from a low level of
delicate inner structures.
rounded by a tough, fibrous
where it is stored until emptied. The kidney is sur-
carries the final urine from the kidney to the bladder,
and vein, lymphatics, nerve supply, and ureter, which
grams and is about the size of a clenched fist. The
abdomen, outside the peritoneal cavity (Figure 26–2).
The two kidneys lie on the posterior wall of the
and Urinary Tract
the body fluid and electrolyte balances.
hemodialysis are initiated to restore, at least partially,
a few days, unless clinical interventions such as
failure, enough potassium, acids, fluid, and other sub-
composition rapidly occur. With complete renal
kidneys, these homeostatic functions are disrupted,
With chronic kidney disease or acute failure of the
prolonged periods of fasting rivals that of the liver.
The
gluconeogenesis.
fasting, a process referred to as
The kidneys synthesize glucose from
in Chapter 79, calcitriol plays an important role in
reabsorption by the gastrointestinal tract. As discussed
vitamin at the “number 1” position. Calcitriol is essen-
), by hydroxylating this
kidneys produce the active form of vitamin D, 1,25-
The
hemodialysis, severe anemia develops as a result of
people with severe kidney disease or who have had
the erythropoietin secreted into the circulation. In
The kidneys normally account for almost all
hypoxia.
blood cells, as discussed in Chapter 32. One important
The kidneys secrete
Regulation of Erythrocyte Production.
erated by the metabolism of proteins.
acids, such as sulfuric acid and phosphoric acid, gen-
body fluid buffer stores. The kidneys are the only
fluid buffers, by excreting acids and by regulating the
to acid-base regulation, along with the lungs and body
The kidneys contribute
ucts (e.g., angiotensin II).
secreting vasoactive factors or substances, such as
amounts of sodium and water. The kidneys also con-
19, the kidneys play a dominant role in long-term reg-
these amazing feats of homeostasis.
phate ions. In the next few chapters, we discuss the spe-
potassium, calcium, hydrogen, magnesium, and phos-
water and for most other electrolytes, such as chloride,
plasma sodium concentration. This is also true for
people, sodium intake can be increased to 1500 mEq/
mous. Experimental studies have shown that in many
The capacity of the kidneys to alter sodium excre-
days of renal adaptation to the high sodium intake,
output is re-established. However, during the 2 to 3
300 mEq/day, so that a balance between intake and
sodium intake, renal excretion also increases to about
308
Unit V
The Body Fluids and Kidneys
there is a modest accumulation of sodium that raises
extracellular fluid volume slightly and triggers hor-
monal changes and other compensatory responses
that signal the kidneys to increase their sodium
excretion.
tion in response to changes in sodium intake is enor-
day (more than 10 times normal) or decreased to
10 mEq/day (less than one tenth normal) with rela-
tively small changes in extracellular fluid volume or
cific mechanisms that permit the kidneys to perform
Regulation of Arterial Pressure.
As discussed in Chapter
ulation of arterial pressure by excreting variable
tribute to short-term arterial pressure regulation by
renin, that lead to the formation of vasoactive prod-
Regulation of Acid-Base Balance.
means of eliminating from the body certain types of
erythropoietin, which stimulates the production of red
stimulus for erythropoietin secretion by the kidneys is
their kidneys removed and have been placed on
decreased erythropoietin production.
Regulation of 1,25–Dihydroxyvitamin D
3
Production.
dihydroxyvitamin D
3
(calcitriol
tial for normal calcium deposition in bone and calcium
calcium and phosphate regulation.
Glucose Synthesis.
amino acids and other precursors during prolonged
kidneys’ capacity to add glucose to the blood during
and severe abnormalities of body fluid volumes and
stances accumulate in the body to cause death within
Physiologic Anatomy
of the Kidneys
General Organization of the Kidneys
Each kidney of the adult human weighs about 150
medial side of each kidney contains an indented region
called the hilum through which pass the renal artery
capsule that protects its
Time (days)
Time (days)
2
0
2
4
6
8
10 12
14
Sodium intake and
excretion
(mEq/day)
Extracellular
fluid volume
(Liters)
-
4
-
300
Sodium
retention
Intake
Excretion
Sodium
loss
200
100
0
15
10
5
intake and sodium excretion.
sodium loss, determined from the difference between sodium
The shaded areas represent the net sodium retention or the net
day) on urinary sodium excretion and extracellular fluid volume.
Effect of increasing sodium intake 10-fold (from 30 to 300 mEq/
Figure 26–1
peritubular capillaries, thereby changing the rate of
and efferent arterioles, the kidneys can regulate the
sorption. By adjusting the resistance of the afferent
60 mm Hg) causes rapid fluid filtration, whereas a
pressure in both sets of capillaries. High hydro-
efferent arterioles, which help regulate the hydrostatic
which are arranged in series and separated by the
illary beds, the glomerular and peritubular capillaries,
The renal circulation is unique in that it has two cap-
renal tubules.
peritubular capillaries,
network, the
efferent arteriole,
begin urine formation (Figure 26–3). The distal ends of
glomerular capillaries,
afferent arterioles,
arcuate arteries, interlobular arteries
interlobar arteries,
cent of the cardiac output, or 1100 ml/min. The renal
later in this chapter.
bladder,
calyces, pelvis, and ureter contain contractile elements
The walls of the
minor calyces,
ureter. The outer border of the pelvis is divided into
renal pelvis,
The base of
renal pyramids.
The medulla is divided into multiple cone-shaped
If the kidney is bisected from top to bottom, the two
Urine Formation by the Kidneys: I. Glomerular Filtration, Renal Blood Flow, and Their Control
Chapter 26
309
major regions that can be visualized are the outer
cortex and the inner region referred to as the medulla.
masses of tissue called
each pyramid originates at the border between the
cortex and medulla and terminates in the papilla,
which projects into the space of the
a
funnel-shaped continuation of the upper end of the
open-ended pouches called major calyces that extend
downward and divide into
which collect
urine from the tubules of each papilla.
that propel the urine toward the
where urine
is stored until it is emptied by micturition, discussed in
Renal Blood Supply
Blood flow to the two kidneys is normally about 22 per
artery enters the kidney through the hilum and then
branches progressively to form the
(also called radial
arteries) and
which lead to the
where large amounts of fluid
and solutes (except the plasma proteins) are filtered to
the capillaries of each glomerulus coalesce to form the
which leads to a second capillary
that surrounds the
static pressure in the glomerular capillaries (about
much lower hydrostatic pressure in the peritubular
capillaries (about 13 mm Hg) permits rapid fluid reab-
hydrostatic pressure in both the glomerular and the
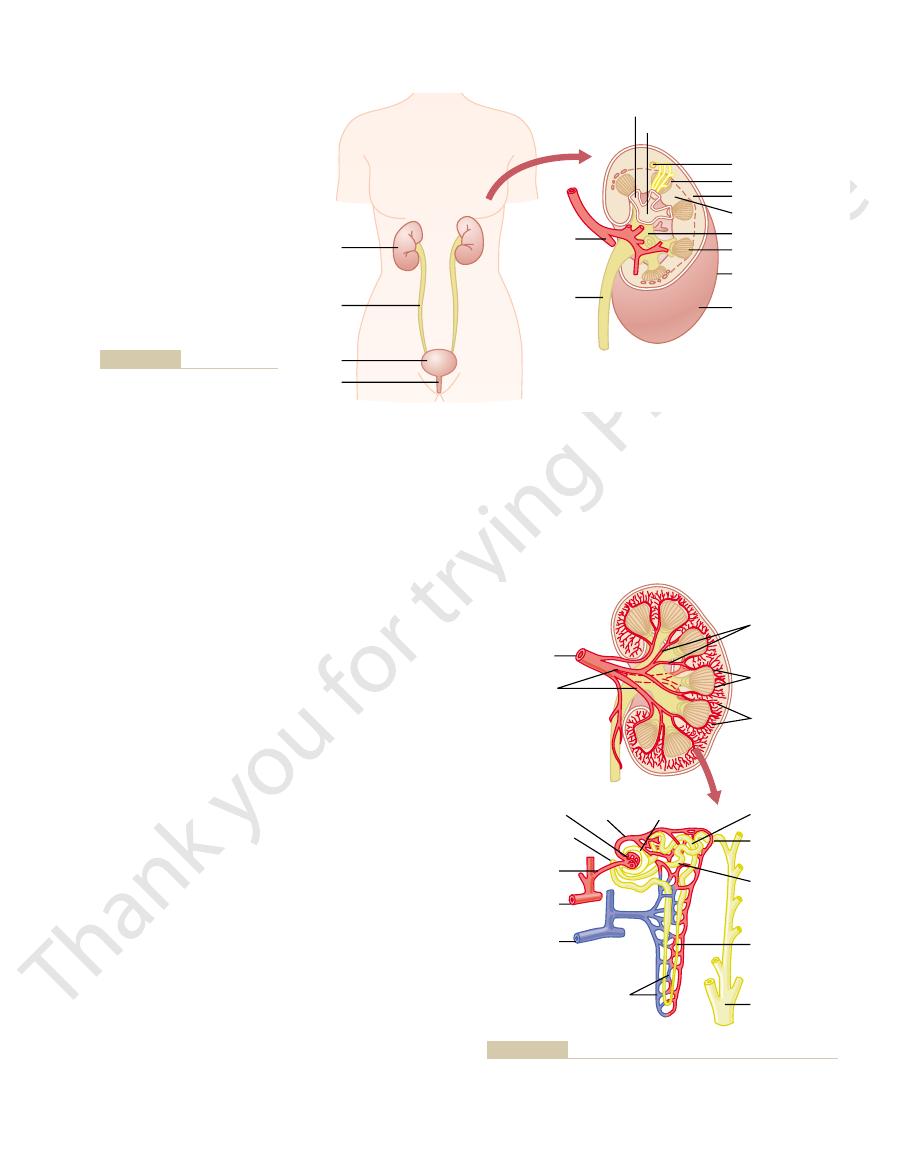
Nephron (enlarged)
Minor calyx
Major calyx
Papilla
Renal cortex
Renal medulla
Renal pelvis
Renal pyramid
Capsule
Kidney
Bladder
Urethra
Ureter
Kidney
Ureter
Renal
artery
kidneys and the urinary system.
General organization of the
Figure 26–2
Renal artery
Juxtaglomerular
apparatus
Efferent
arteriole
Bowman's
capsule
Glomerulus
Interlobar
arteries
Arcuate arteries
Cortical
collecting tubule
Collecting duct
Loop of
Henle
Proximal tubule
Interlobular
arterioles
Segmental
arteries
Afferent
arteriole
Arcuate
artery
Distal tubule
Arcuate
vein
Peritubular
capillaries
circulation of each nephron.
supply the blood flow to the kidney and schematic of the micro-
Figure 26–3
Section of the human kidney showing the major vessels that
urine.
the cortex and empty into the cortical veins. This
Like the loops of Henle, the vasa recta return toward
medulla, lying side by side with the loops of Henle.
tamedullary nephrons, long efferent arterioles extend
network of peritubular capillaries. For the jux-
the cortical nephrons. For the cortical nephrons, the
The vascular structures supplying the jux-
the tips of the renal papillae.
deeply into the medulla, in some cases all the way to
These nephrons have long loops of Henle that dip
juxtamedullary nephrons.
(Figure 26–5).
within the kidney mass. Those nephrons that have
ferences, depending on how deep the nephron lies
the components described earlier, there are some dif-
Juxtamedullary Nephrons.
collects urine from about 4000 nephrons.
250 of the very large collecting ducts, each of which
In each kidney, there are about
renal papillae.
The collecting
The initial parts of 8 to 10 cortical
cortical collecting tubule,
renal cortex. This is followed by the
which, like the proximal tubule, lies in the
distal tubule,
function. Beyond the macula densa, fluid enters the
As we discuss later, the macula
segment, which is actually a plaque in its wall, known
thick segment of the ascending limb.
cortex, its wall becomes much thicker, and it is referred
thin segment of the loop of Henle.
The
ascending limb.
which dips into the renal medulla. Each loop
of Henle,
From the proximal tubule, fluid flows into the
which lies in the cortex of the kidney (Figure 26–4).
proximal tubule,
Bowman’s capsule and then into the
Bowman’s capsule.
ies are covered by epithelial cells, and the total
pressure (about 60 mm Hg). The glomerular capillar-
pared with other capillaries, have high hydrostatic
and anastomosing glomerular capillaries that, com-
The glomerulus contains a network of branching
urine on its way to the pelvis of the kidney (see Figure
amounts of fluid are filtered from the blood, and (2) a
glomerulus,
electrolytes, and waste products, as discussed in
them to excrete the proper amounts of water,
did at age 40. This loss is not life threatening because
per cent every 10 years; thus, at age 80, many people
decrease in nephron number. After age 40, the number
injury, disease, or normal aging, there is a gradual
cannot regenerate new nephrons. Therefore, with renal
each capable of forming urine. The kidney
nephrons,
The Nephron Is the Functional Unit
leaves the kidney beside the renal artery and ureter.
arcuate vein, interlobar vein,
the venous system, which run parallel to the arteriolar
The peritubular capillaries empty into the vessels of
response to body homeostatic demands.
glomerular filtration, tubular reabsorption, or both in
310
Unit V
The Body Fluids and Kidneys
vessels and progressively form the interlobular vein,
and renal vein, which
of the Kidney
Each kidney in the human contains about 1 million
of functioning nephrons usually decreases about 10
have 40 per cent fewer functioning nephrons than they
adaptive changes in the remaining nephrons allow
Chapter 31.
Each nephron contains (1) a tuft of glomerular cap-
illaries called the
through which large
long tubule in which the filtered fluid is converted into
26–3).
glomerulus is encased in
Fluid
filtered from the glomerular capillaries flows into
loop
consists of a descending and an
walls of the descending limb and the lower end of the
ascending limb are very thin and therefore are called
the
After the ascend-
ing limb of the loop has returned partway back to the
to as the
At the end of the thick ascending limb is a short
as the macula densa.
densa plays an important role in controlling nephron
connecting tubule
and the
which lead to the cor-
tical collecting duct.
collecting ducts join to form a single larger collecting
duct that runs downward into the medulla and
becomes the medullary collecting duct.
ducts merge to form progressively larger ducts that
eventually empty into the renal pelvis through the tips
of the
Regional Differences in Nephron Structure: Cortical and
Although each nephron has all
glomeruli located in the outer cortex are called corti-
cal nephrons; they have short loops of Henle that
penetrate only a short distance into the medulla
About 20 to 30 per cent of the nephrons have
glomeruli that lie deep in the renal cortex near the
medulla and are called
tamedullary nephrons also differ from those supplying
entire tubular system is surrounded by an extensive
from the glomeruli down into the outer medulla and
then divide into specialized peritubular capillaries
called vasa recta that extend downward into the
specialized network of capillaries in the medulla plays
an essential role in the formation of a concentrated
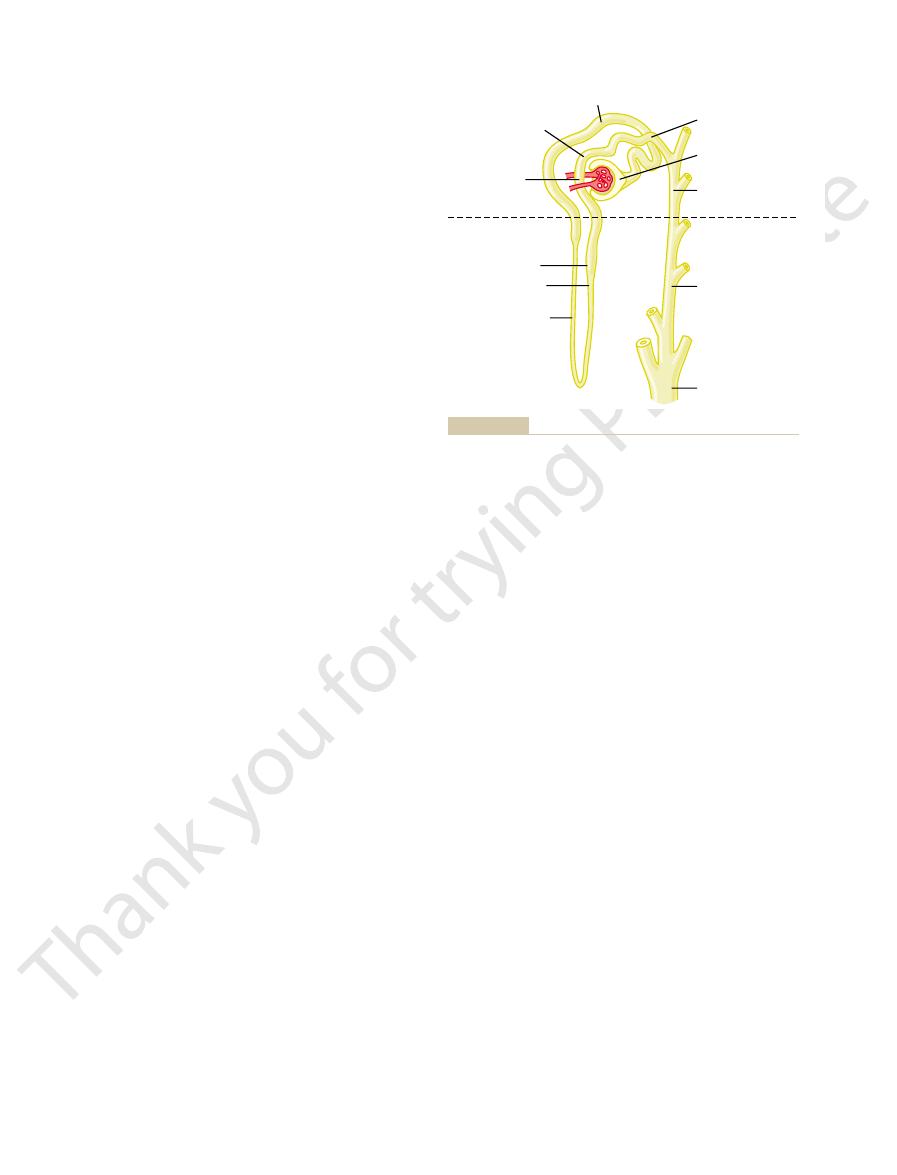
Cortical
collecting tubule
Macula densa
Loop of Henle:
Thick segment of
ascending limb
Thin segment of
ascending limb
Descending limb
Distal tubule
Proximal tubule
Collecting duct
Medullary
collecting tubule
Medulla
Cortex
Cortical
collecting tubule
Bowman's capsule
Connecting tubule
different tubular segments are not drawn to scale.
Basic tubular segments of the nephron. The relative lengths of the
Figure 26–4
bladder.
the bladder, courses obliquely through the detrusor
Each ureter, as it enters
rugae.
is smooth, in contrast to the remaining bladder mucosa,
the inner lining of the bladder,
angles of the trigone. The trigone can be identified by
At the lowermost apex of the trigone,
trigone.
ately above the bladder neck, is a small triangular area
On the posterior wall of the bladder, lying immedi-
traction of the entire bladder at once.
muscle, from one muscle cell to the next, to cause con-
exist from one muscle cell to the other. Therefore, an
bladder to 40 to 60 mm Hg. Thus,
when contracted, can increase the pressure in the
sor muscle.
The smooth muscle of the bladder is called the
urethra. The lower part of the bladder neck is also called
extension of the body, passing inferiorly and anteriorly
neck,
urine collects, and (2) the
body,
muscle chamber composed of two main parts: (1) the
The urinary bladder, shown in Figure 26–6, is a smooth
Nervous Connections
cord reflex, it can also be inhibited or facilitated by
fails, at least causes a conscious desire to urinate.
that empties the bladder or, if this
elicits the second step, which is a nervous reflex called
tension in its walls rises above a threshold level; this
steps: First, the bladder fills progressively until the
empties when it becomes filled. This involves two main
Urine Formation by the Kidneys: I. Glomerular Filtration, Renal Blood Flow, and Their Control
Chapter 26
311
Micturition
Micturition is the process by which the urinary bladder
the micturition reflex
Although the micturition reflex is an autonomic spinal
centers in the cerebral cortex or brain stem.
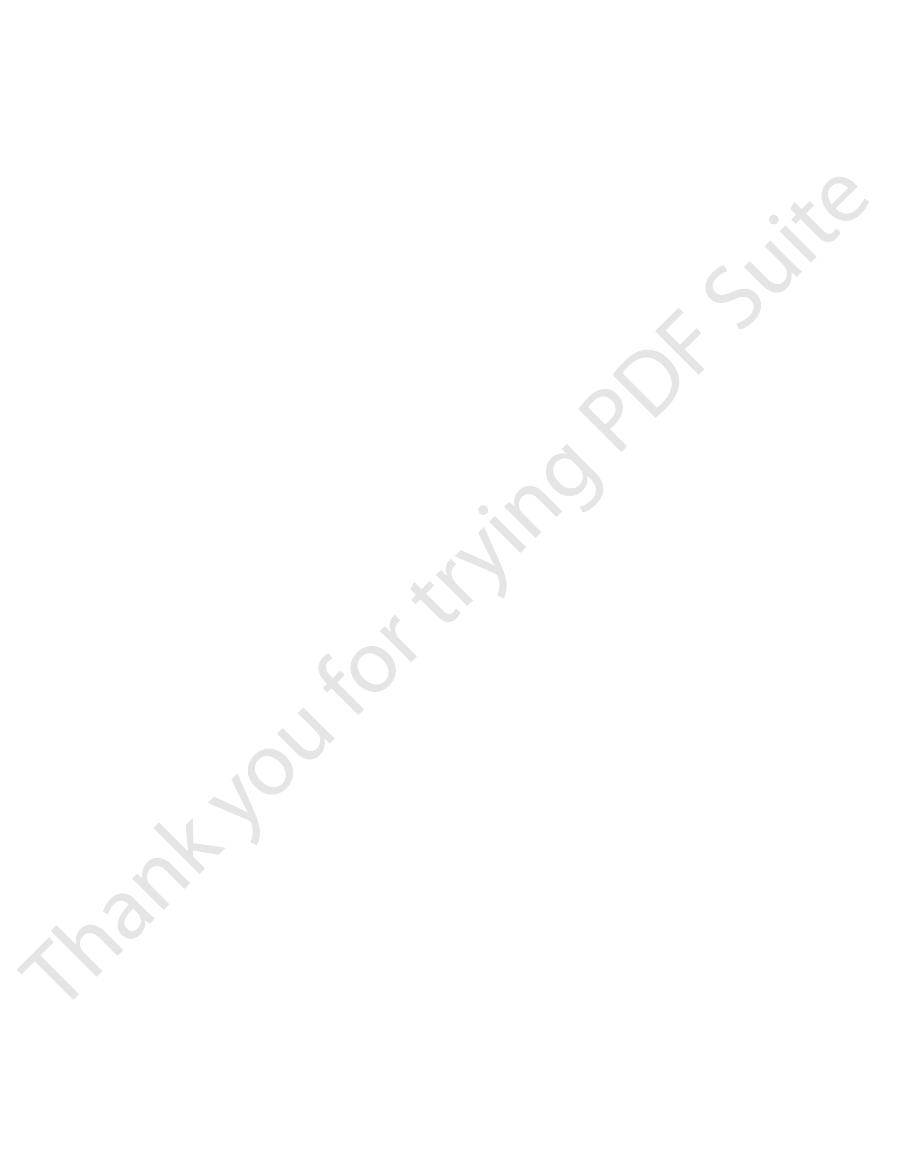
Physiologic Anatomy and
of the Bladder
which is the major part of the bladder in which
which is a funnel-shaped
into the urogenital triangle and connecting with the
the posterior urethra because of its relation to the
urethra.
detru-
Its muscle fibers extend in all directions and,
contraction of the
detrusor muscle is a major step in emptying the bladder.
Smooth muscle cells of the detrusor muscle fuse with
one another so that low-resistance electrical pathways
action potential can spread throughout the detrusor
called the
the bladder neck opens into the posterior urethra, and
the two ureters enter the bladder at the uppermost
the fact that its mucosa,
which is folded to form
muscle and then passes another 1 to 2 centimeters
beneath the bladder mucosa before emptying into the
Cortex
Medulla
Outer zone
Inner zone
Efferent
arteriole
Afferent
arteriole
Collecting
duct
Interlobar
artery
vein
Interlobar
artery
vein
Thick loop
of Henle
Juxtamedullary
nephron
Cortical
nephron
Duct of
Bellini
Vasa
recta
Thin loop
of Henle
nephrons.
tures and differences between cortical and juxtamedullary
Schematic of relations between blood vessels and tubular struc-
Figure 26–5
L1
L2
L3
L4
L5
S1
S2
S3
S4
Ureter
Body
Pudendal
Sympathetics
Parasympathetics
Trigone
Bladder neck
(posterior urethra)
External sphincter
Urinary bladder and its innervation.
Figure 26–6
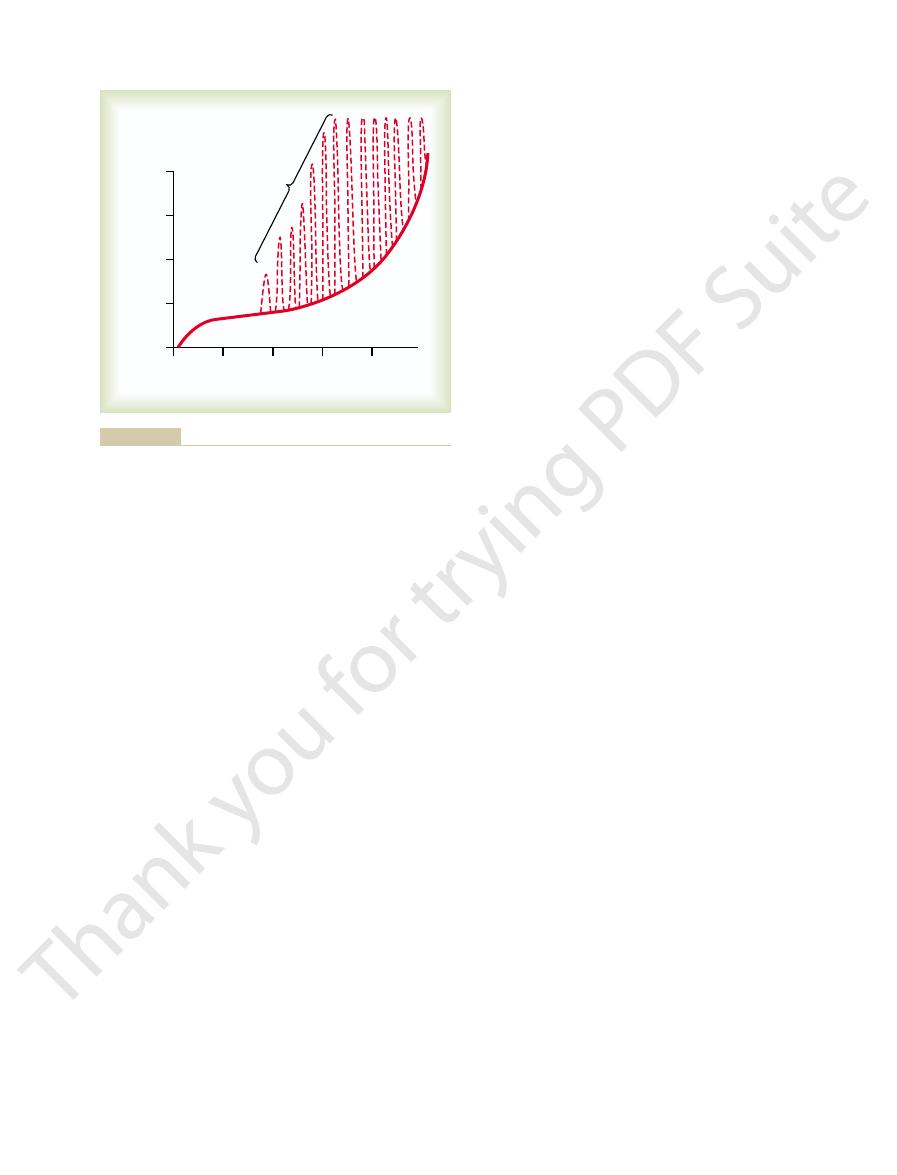
minute. The pressure peaks may rise only a few cen-
causes the pressure to rise rapidly.
400 milliliters, collection of more urine in the bladder
intrinsic tone of the bladder wall itself. Beyond 300 to
pressure; this constant level of pressure is caused by
timeters of water. Additional urine—200 to 300 milli-
urine has collected, the pressure rises to 5 to 10 cen-
sure is about 0, but by the time 30 to 50 milliliters of
there is no urine in the bladder, the intravesicular pres-
vesicular pressure as the bladder fills with urine. When
Figure 26–7 shows the approximate changes in intra-
the Cystometrogram
and Bladder Wall Tone;
the pelvis of a kidney with a blocked ureter.
kidney. This effect is called the
arterioles, thereby decreasing urine output from the
with severe pain. Also, the pain impulses cause a sym-
stone), intense reflex constriction occurs, associated
When a ureter becomes blocked (e.g., by a ureteral
The ureters are well supplied with pain nerve fibers.
medulla, causing damage to these regions.
of the ureters and, if severe, can increase the pressure
backward into the ureter, a condition called
result, some of the urine in the bladder is propelled
always lead to complete occlusion of the ureter. As a
through the bladder wall is less than normal, so that
In some people, the distance that the ureter courses
allows urine to flow into the bladder.
compression. Each peristaltic wave along the ureter
tends to compress the ureter, thereby preventing back-
for several centimeters through the bladder wall. The
in Figure 26–6. Normally, the ureters course obliquely
in the trigone region of the bladder, as shown
The ureters enter the bladder through the
by sympathetic stimulation.
enhanced by parasympathetic stimulation and inhibited
smooth muscle,
the entire length of the ureters. As with other visceral
bladder. The walls of the ureters contain smooth
and then downward along the length of the ureter,
inherent pacemaker activity, which in turn initiates
calyces and ureters to the bladder.
lecting ducts; there are no significant changes in the
Kidney Through the Ureters
Transport of Urine from the
sensation of fullness and, in some instances, pain.
traction. Some sensory nerve fibers also pass by way of
spinal cord. These sympathetic fibers stimulate mainly
nerves,
ter. Also, the bladder receives
sphincter. These are
innervation are important in bladder function. Most
In addition to the pelvic nerves, two other types of
glionic nerves then innervate the detrusor muscle.
cells located in the wall of the bladder. Short postgan-
These terminate on ganglion
parasympathetic fibers.
The motor nerves transmitted in the pelvic nerves are
emptying.
the bladder wall. Stretch signals from the posterior
The sensory fibers detect the degree of stretch in
fibers.
segments S-2 and S-3. Coursing through the pelvic
sacral plexus,
pelvic nerves,
The principal nerve supply of the bladder is by way of
Innervation of the Bladder
ing to empty the bladder.
neck, which is entirely smooth muscle. The external
bladder. This muscle is a voluntary skeletal muscle, in
Beyond the posterior urethra, the urethra passes
posterior urethra empty of urine and, therefore, pre-
internal sphincter.
The muscle in this area is called the
muscle interlaced with a large amount of elastic tissue.
timeters long, and its wall is composed of detrusor
The bladder neck (posterior urethra) is 2 to 3 cen-
312
Unit V
The Body Fluids and Kidneys
Its natural tone normally keeps the bladder neck and
vents emptying of the bladder until the pressure in the
main part of the bladder rises above a critical threshold.
through the urogenital diaphragm, which contains a
layer of muscle called the external sphincter of the
contrast to the muscle of the bladder body and bladder
sphincter muscle is under voluntary control of the
nervous system and can be used to consciously prevent
urination even when involuntary controls are attempt-
the
which connect with the spinal cord
through the
mainly connecting with cord
nerves are both sensory nerve fibers and motor nerve
urethra are especially strong and are mainly re-
sponsible for initiating the reflexes that cause bladder
important are the skeletal motor fibers transmitted
through the pudendal nerve to the external bladder
somatic nerve fibers that innervate
and control the voluntary skeletal muscle of the sphinc-
sympathetic innervation
from the sympathetic chain through the hypogastric
connecting mainly with the L-2 segment of the
the blood vessels and have little to do with bladder con-
the sympathetic nerves and may be important in the
and into the Bladder
Urine that is expelled from the bladder has essentially
the same composition as fluid flowing out of the col-
composition of urine as it flows through the renal
Urine flowing from the collecting ducts into the
renal calyces stretches the calyces and increases their
peristaltic contractions that spread to the renal pelvis
thereby forcing urine from the renal pelvis toward the
muscle and are innervated by both sympathetic and
parasympathetic nerves as well as by an intramural
plexus of neurons and nerve fibers that extends along
peristaltic contractions in the ureter are
detrusor
muscle
normal tone of the detrusor muscle in the bladder wall
flow of urine from the bladder when pressure builds
up in the bladder during micturition or bladder
increases the pressure within the ureter so that the
region passing through the bladder wall opens and
contraction of the bladder during micturition does not
vesi-
coureteral reflux. Such reflux can lead to enlargement
in the renal calyces and structures of the renal
Pain Sensation in the Ureters, and the Ureterorenal Reflex
.
pathetic reflex back to the kidney to constrict the renal
ureterorenal reflex and
is important for preventing excessive flow of fluid into
Filling of the Bladder
liters—can collect with only a small additional rise in
Superimposed on the tonic pressure changes during
filling of the bladder are periodic acute increases in
pressure that last from a few seconds to more than a
timeters of water or may rise to more than 100
Atonic Bladder Caused by Destruction of Sensory Nerve Fibers.
Abnormalities of Micturition
more than 5 to 10 milliliters left in the bladder.
Ordinarily, all the urine will be emptied, with rarely
simultaneously inhibits the external urethral sphincter.
receptors, which excites the micturition reflex and
thus stretching their walls. This stimulates the stretch
bladder neck and posterior urethra under pressure,
her abdominal muscles, which increases the pressure
lowing way: First, a person voluntarily contracts his or
Voluntary urination
urination can occur.
3. When it is time to urinate, the cortical centers can
a convenient time presents itself.
if the micturition reflex occurs, by continual tonic
2. The higher centers can prevent micturition, even
partially inhibited, except when micturition is
1. The higher centers keep the micturition reflex
tion, but the higher centers normally exert final control
The micturition reflex is the basic cause of micturi-
but can become excitatory.
stem, located mainly in the pons,
by centers in the brain. These centers include (1)
spinal cord reflex, but it can be inhibited or facilitated
The micturition reflex is a completely autonomic
urination will occur. If not, urination will not occur
voluntary constrictor signals to the external sphincter,
it. If this inhibition is more potent in the brain than the
enough, it causes another reflex, which passes through
and more and more powerfully.
filled, micturition reflexes occur more and more often
reflex occurs. As the bladder becomes more and more
emptying the bladder, the nervous elements of this
pressure to the basal tone of the bladder. Once a mic-
period of sustained pressure, and (3) return of the
of (1) progressive and rapid increase of pressure, (2) a
Thus, the micturition reflex is a single complete cycle
reflex ceases, permitting the bladder to relax.
to fatigue and the regenerative cycle of the micturition
more than a minute, the self-regenerative reflex begins
degree of contraction. Then, after a few seconds to
traction of the bladder; thus, the cycle is repeated again
urethra, which causes a further increase in reflex con-
ative.” That is, initial contraction of the bladder acti-
Once a micturition reflex begins, it is “self-regener-
of the detrusor muscle.
bladder continues to fill, the micturition reflexes
tracting, and pressure falls back to the baseline. As the
a fraction of a minute, the detrusor muscles stop con-
When the bladder is only partially filled, these mic-
by way of these same nerves.
sures. Sensory signals from the bladder stretch recep-
in the bladder wall, especially
sensory stretch receptors
They are the result of a stretch reflex initiated by
begin to appear, as shown by the dashed spikes.
bladder fills, many superimposed
Referring again to Figure 26–7, one can see that as the
in the cystometrogram and are caused
centimeters of water. These pressure peaks are called
Urine Formation by the Kidneys: I. Glomerular Filtration, Renal Blood Flow, and Their Control
Chapter 26
313
micturition waves
by the micturition reflex.
Micturition Reflex
micturition contrac-
tions
by the receptors in the posterior urethra when this
area begins to fill with urine at the higher bladder pres-
tors are conducted to the sacral segments of the cord
through the pelvic nerves and then reflexively back
again to the bladder through the parasympathetic
nerve fibers
turition contractions usually relax spontaneously after
become more frequent and cause greater contractions
vates the stretch receptors to cause a greater increase
in sensory impulses to the bladder and posterior
and again until the bladder has reached a strong
turition reflex has occurred but has not succeeded in
reflex usually remain in an inhibited state for a few
minutes to 1 hour or more before another micturition
Once the micturition reflex becomes powerful
the pudendal nerves to the external sphincter to inhibit
until the bladder fills still further and the micturition
reflex becomes more powerful.
Facilitation or Inhibition of Micturition
by the Brain
strong facilitative and inhibitory centers in the brain
and (2) several centers
located in the cerebral cortex that are mainly inhibitory
of micturition as follows:
desired.
contraction of the external bladder sphincter until
facilitate the sacral micturition centers to help
initiate a micturition reflex and at the same time
inhibit the external urinary sphincter so that
is usually initiated in the fol-
in the bladder and allows extra urine to enter the
Micturition reflex contraction cannot occur if the
sensory nerve fibers from the bladder to the spinal cord
0
100
200
300
400
Volume (milliliters)
Micturition
contractions
Basal cystom
etrogram
Intravesical pressure
(centimeters of water)
40
30
20
10
0
) caused by micturition reflexes.
Normal cystometrogram, showing also acute pressure waves
Figure 26–7
(dashed spikes
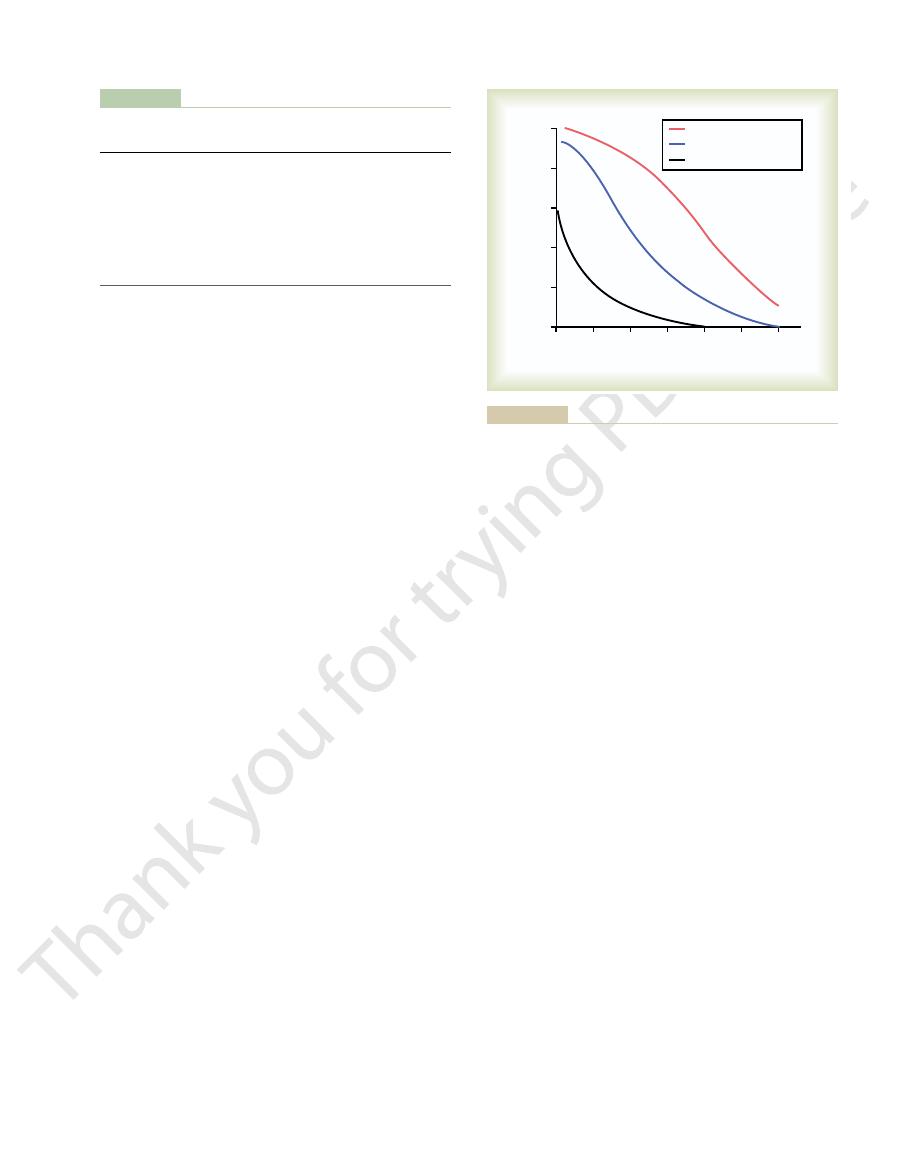
In panel C, the substance is freely filtered at the
for many of the electrolytes of the body.
tration rate minus the reabsorption rate. This is typical
In this case, the excretion rate is calculated as the fil-
than the rate of filtration at the glomerular capillaries.
blood. Therefore, the rate of urinary excretion is less
In panel B, the substance is freely filtered but is also
are handled by the kidneys in this manner, allowing
Certain waste products in the body, such as creatinine,
neither reabsorbed nor secreted. Therefore, its excre-
thetical substances. The substance shown in panel A is
Figure 26–9 shows the renal handling of four hypo-
peritubular capillaries into the tubules.
and passes through the tubules, it is modified by reab-
the plasma. As filtered fluid leaves Bowman’s capsule
filtrate in Bowman’s capsule is almost the same as in
filtered, so that their concentration in the glomerular
substances in the plasma, except for proteins, are freely
glomerular capillaries into Bowman’s capsule. Most
Filtration rate
mathematically,
from the blood into the renal tubules. Expressed
into the blood, and (3) secretion of substances
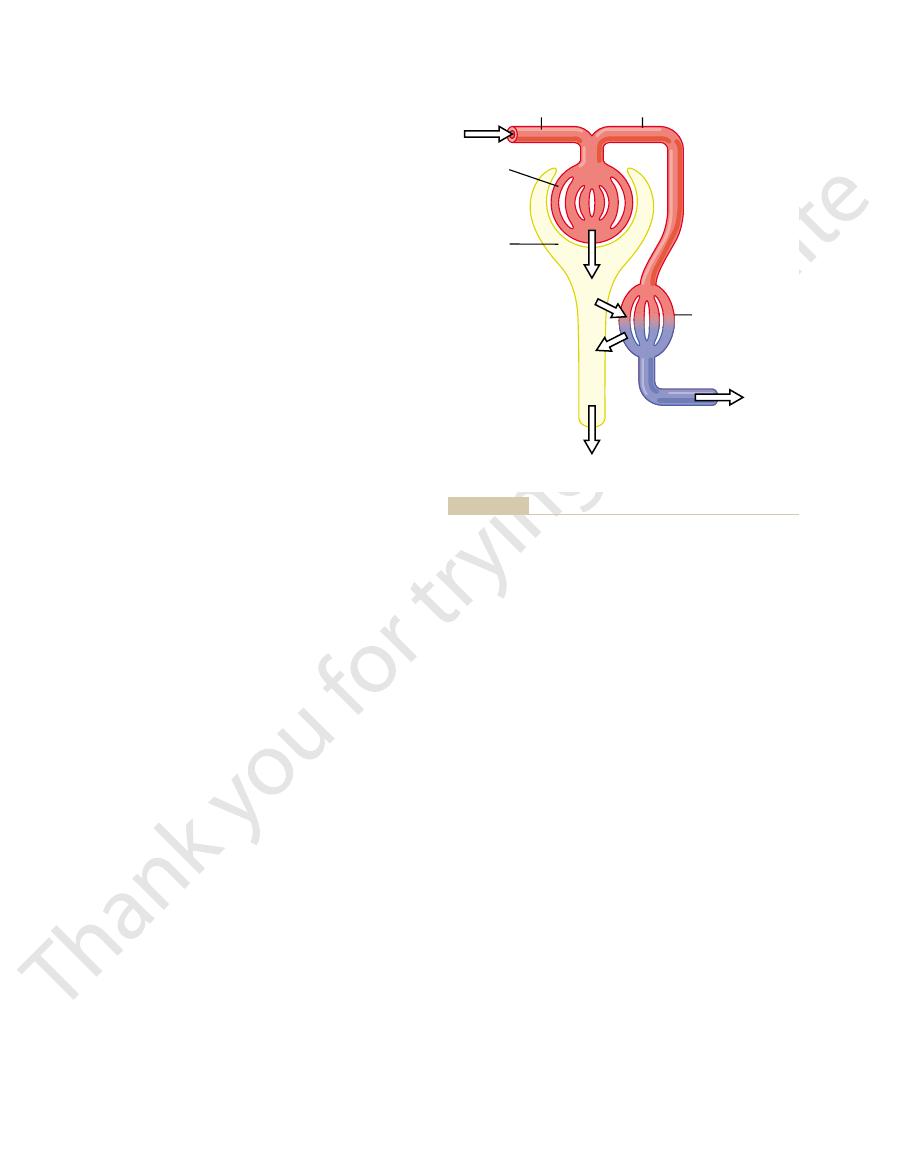
cesses, shown in Figure 26–8: (1) glomerular filtration,
The rates at which different substances are excreted
Tubular Secretion
Tubular Reabsorption, and
from Glomerular Filtration,
Urine Formation Results
elicits an uncontrollable micturition reflex, thereby pro-
of the inhibitory signals. Therefore, facilitative impulses
micturition. This condition derives from partial damage
tion is the so-called uninhibited neurogenic bladder,
Uninhibited Neurogenic Bladder Caused by Lack of Inhibitory
the genital region, which sometimes elicits a micturition
nounced) bladder emptying occurs.
micturition reflexes return; then, periodic (but unan-
caused by overstretching of the bladder, the excitability
stem and cerebrum. However, if the bladder is emptied
pressed because of the state of “spinal shock” caused by
cord has occurred, the micturition reflexes are sup-
they are no longer controlled by the brain. During the
typical micturition reflexes can still occur. However,
bladder.
tabes dorsalis,
destroying them. This condition is called
constrictive fibrosis around the dorsal root nerve fibers,
enter the spinal cord. For example, syphilis can cause
the sacral region of the spinal cord. Certain diseases can
overflow incontinence.
overflows a few drops at a time through the urethra.This
emptying periodically, the bladder fills to capacity and
neurogenic connections within the brain. Instead of
person loses bladder control, despite intact efferent
stretch signals from the bladder. When this happens, a
are destroyed, thereby preventing transmission of
314
Unit V
The Body Fluids and Kidneys
fibers from the cord to the bladder and despite intact
is called
A common cause of atonic bladder is crush injury to
also cause damage to the dorsal root nerve fibers that
and the resulting bladder condition is called tabetic
Automatic Bladder Caused by Spinal Cord Damage Above the
Sacral Region.
If the spinal cord is damaged above the
sacral region but the sacral cord segments are still intact,
first few days to several weeks after the damage to the
the sudden loss of facilitative impulses from the brain
periodically by catheterization to prevent bladder injury
of the micturition reflex gradually increases until typical
Some patients can still control urination in this con-
dition by stimulating the skin (scratching or tickling) in
reflex.
Signals from the Brain.
Another abnormality of micturi-
which results in frequent and relatively uncontrolled
in the spinal cord or the brain stem that interrupts most
passing continually down the cord keep the sacral
centers so excitable that even a small quantity of urine
moting frequent urination.
in the urine represent the sum of three renal pro-
(2) reabsorption of substances from the renal tubules
Urinary excretion rate
=
- Reabsorption rate + Secretion rate
Urine formation begins when a large amount of
fluid that is virtually free of protein is filtered from the
sorption of water and specific solutes back into the
blood or by secretion of other substances from the
freely filtered by the glomerular capillaries but is
tion rate is equal to the rate at which it was filtered.
excretion of essentially all that is filtered.
partly reabsorbed from the tubules back into the
glomerular capillaries but is not excreted into the
1. Filtration
2. Reabsorption
3. Secretion
4. Excretion
Peritubular
capillaries
1
2
3
4
Renal
vein
Urinary excretion
Excretion = Filtration – Reabsorption + Secretion
Glomerular
capillaries
Bowman's
capsule
Afferent
arteriole
Efferent
arteriole
rate at which it is secreted from the peritubular capillary blood into
which the substance is filtered minus its reabsorption rate plus the
urine. Urinary excretion rate of a substance is equal to the rate at
Basic kidney processes that determine the composition of the
Figure 26–8
the tubules.
volume and composition of the body fluids.
and processed about 60 times each day. This high GFR
is about 180 L/day, the entire plasma can be filtered
plasma volume is only about 3 liters, whereas the GFR
kidney many times each day. Because the entire
for effective removal from the body.
by the tubules and, therefore, depend on a high GFR
excretion. Most waste products are poorly reabsorbed
and then reabsorbing most of these substances. One
constant. In reality, changes in glomerular filtration
renal excretion. For example, an increase in glomeru-
excretion. Therefore, subtle adjustments of filtration or
For most substances, the rates of filtration and reab-
tion of the filtered sodium is reabsorbed, resulting in
when there is excess sodium in the body, the rate at
lated according to the needs of the body. For example,
tubular reabsorption, and tubular secretion—is regu-
capillaries.
amino acids and glucose, are completely reabsorbed
in the urine. Certain nutritional substances, such as
highly reabsorbed, so that only small amounts appear
as sodium ions, chloride ions, and bicarbonate ions, are
excretion rates are high. Conversely, electrolytes, such
secreted from the blood into the tubules, so that their
drugs are also poorly reabsorbed but, in addition, are
amounts in the urine. Certain foreign substances and
reabsorbed and are therefore excreted in large
as urea, creatinine, uric acid, and urates, are poorly
blood, especially the end products of metabolism such
urine. Most substances that must be cleared from the
urine, but secretion plays an important role in deter-
In general, tubular reabsorption is quantitatively more
Secretion of Different Substances
Filtration, Reabsorption, and
basic renal processes.
occurs. The rate at which the substance is excreted in
bination of filtration, reabsorption, and secretion
For each substance in the plasma, a particular com-
tubular secretion rate.
and excreted in large amounts in the urine. The excre-
This pattern often occurs for organic acids and bases,
the peritubular capillary blood into the renal tubules.
glomerular capillaries and is not reabsorbed, but addi-
The substance in panel D is freely filtered at the
to be conserved in the body fluids.
blood, such as amino acids and glucose, allowing them
from the tubules back into the blood. This pattern
Urine Formation by the Kidneys: I. Glomerular Filtration, Renal Blood Flow, and Their Control
Chapter 26
315
urine because all the filtered substance is reabsorbed
occurs for some of the nutritional substances in the
tional quantities of this substance are secreted from
permitting them to be rapidly cleared from the blood
tion rate in this case is calculated as filtration rate plus
the urine depends on the relative rates of these three
important than tubular secretion in the formation of
mining the amounts of potassium and hydrogen ions
and a few other substances that are excreted in the
from the tubules and do not appear in the urine even
though large amounts are filtered by the glomerular
Each of the processes—glomerular filtration,
which sodium is filtered increases and a smaller frac-
increased urinary excretion of sodium.
sorption are extremely large relative to the rates of
reabsorption can lead to relatively large changes in
lar filtration rate (GFR) of only 10 per cent (from 180
to 198 L/day) would raise urine volume 13-fold (from
1.5 to 19.5 L/day) if tubular reabsorption remained
and tubular reabsorption usually act in a coordinated
manner to produce the necessary changes in renal
excretion.
Why Are Large Amounts of Solutes Filtered and Then Reab-
sorbed by the Kidneys?
One might question the wisdom
of filtering such large amounts of water and solutes
advantage of a high GFR is that it allows the kidneys
to rapidly remove waste products from the body that
depend primarily on glomerular filtration for their
A second advantage of a high GFR is that it allows
all the body fluids to be filtered and processed by the
allows the kidneys to precisely and rapidly control the
Substance A
Urine
A.
Filtration only
Substance B
Urine
B.
Filtration, partial
reabsorption
Substance C
Urine
C.
Filtration, complete
reabsorption
Substance D
Urine
D.
Filtration, secretion
renal tubules.
sorbed but is secreted from the peritubular capillary blood into the
The substance is freely filtered and is not reab-
because all the filtered substance is reabsorbed from the tubules
The substance is freely filtered but is not excreted in the urine
tered, but part of the filtered load is reabsorbed back in the blood.
The substance is freely fil-
is freely filtered but not reabsorbed.
Figure 26–9
Renal handling of four hypothetical substances. A, The substance
B,
C,
into the blood. D,

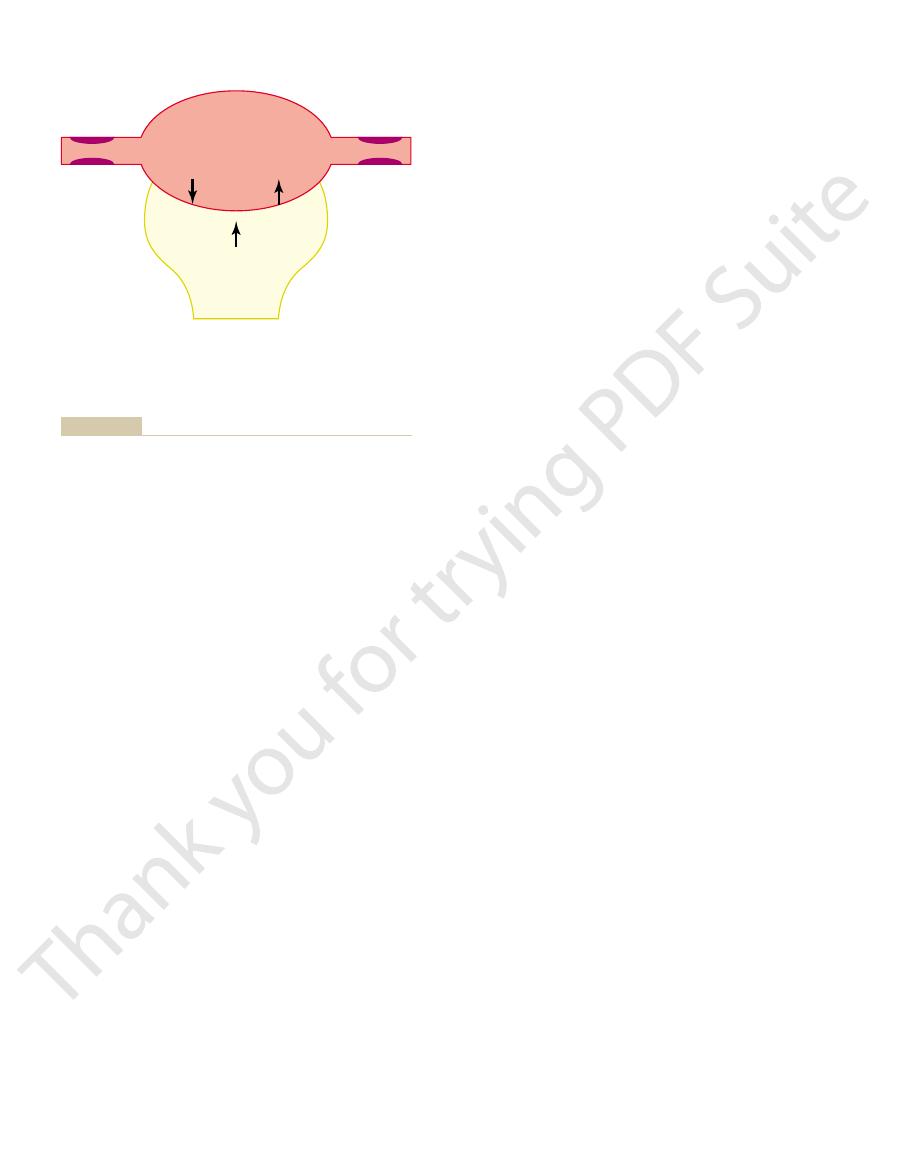
proteins.
proteins. Thus, all layers of the glomerular capillary
The epithelial cells, which also have negative charges,
through which the glomerular filtrate moves.
The foot processes are separated by gaps called
outer surface of the capillaries (see Figure 26–10).
long footlike processes (podocytes) that encircle the
glomerulus. These cells are not continuous but have
The final part of the glomerular membrane is a layer
proteoglycans.
filtration of plasma proteins, in part because of
filter. The basement membrane effectively prevents
brane,
the passage of plasma proteins.
fenestrations are relatively large, endothelial cells are
fenestrated capillaries found in the liver. Although the
fenestrae,
teristics. The capillary
The high filtration rate across the glomerular capil-
vents filtration of plasma proteins.
tion, the glomerular capillary membrane normally pre-
capillary membrane. Even with this high rate of filtra-
barrier, which, despite the three layers, filters several
26–10). Together, these layers make up the filtration
surface of the capillary basement membrane (Figure
basement membrane,
the capillary, (2) a
of the usual two) major layers: (1) the
of other capillaries, except that it has three (instead
The glomerular capillary membrane is similar to that
Filtration fraction
capillaries. The filtration fraction is calculated as
filtered (the filtration fraction) averages about 0.2; this
180 L/day. The fraction of the renal plasma flow that is
average adult human, the GFR is about 125 ml/min, or
. In the
The glomerular capillaries have a much higher rate of
meability and filtering surface area of the capillaries.
), the product of the per-
As in other capillaries, the GFR is determined by (1)
GFR Is About 20 Per Cent of the
are not filtered through the glomerular capillaries.
acids are bound to proteins, and these bound portions
partially bound to the plasma proteins. Almost one
fatty acids, that are not freely filtered because they are
low-molecular-weight substances, such as calcium and
plasma. Exceptions to this generalization include a few
molecules, are similar to the concentrations in the
glomerular filtrate, including most salts and organic
The concentrations of other constituents of the
cellular elements, including red blood cells.
proteins, so that the filtered fluid (called the glomeru-
into Bowman’s capsule. Like most capillaries, the
Composition of the Glomerular
First Step in Urine Formation
316
Unit V
The Body Fluids and Kidneys
Glomerular Filtration—The
Filtrate
Urine formation begins with filtration of large
amounts of fluid through the glomerular capillaries
glomerular capillaries are relatively impermeable to
lar filtrate) is essentially protein-free and devoid of
half of the plasma calcium and most of the plasma fatty
Renal Plasma Flow
the balance of hydrostatic and colloid osmotic forces
acting across the capillary membrane and (2) the cap-
illary filtration coefficient (K
f
filtration than most other capillaries because of a high
glomerular hydrostatic pressure and a large K
f
means that about 20 per cent of the plasma flowing
through the kidney is filtered through the glomerular
follows:
= GFR/Renal plasma flow
Glomerular Capillary Membrane
endothelium of
and (3) a layer
of epithelial cells (podocytes) surrounding the outer
hundred times as much water and solutes as the usual
lary membrane is due partly to its special charac-
endothelium is perforated by
thousands of small holes called
similar to the
richly endowed with fixed negative charges that hinder
Surrounding the endothelium is the basement mem-
which consists of a meshwork of collagen and
proteoglycan fibrillae that have large spaces through
which large amounts of water and small solutes can
strong negative electrical charges associated with the
of epithelial cells that line the outer surface of the
slit pores
provide additional restriction to filtration of plasma
wall provide a barrier to filtration of plasma
Efferent arteriole
Bowman's capsule
Bowman's space
Capillary loops
Afferent arteriole
Slit pores
Epithelium
Basement
membrane
Endothelium
Fenestrations
Proximal tubule
Podocytes
A
B
ponents: capillary endothelium, basement membrane, and epithe-
section of the glomerular capillary membrane and its major com-
Cross
Basic ultrastructure of the glomerular capillaries.
Figure 26–10
A,
B,
lium (podocytes).
The GFR can therefore be expressed as
is considered to be zero.)
colloid osmotic pressure of the Bowman’s capsule fluid
(Under normal conditions, the concentration of
), which promotes filtration.
Bowman’s capsule (
), which opposes filtration; and
outside the capillaries, which opposes filtration; (3) the
(2) the hydrostatic pressure in Bowman’s capsule (P
), which promotes filtration;
hydrostatic pressure, P
(Figure 26–12). These forces include (1) hydrostatic
The net filtration pressure represents the sum of the
. Expressed mathematically, the GFR equals the
net filtration pressure,
membrane, which gives the
The GFR is determined by (1) the sum of the hydro-
Determinants of the GFR
in the urine, a condition known as
proteins, especially albumin, are filtered and appear
membranes, some of the lower-molecular-weight
minimal change nephropathy.
noticeable changes in kidney histology, a condition
In certain kidney diseases, the negative charges on
including the plasma proteins.
for restricting large negatively charged molecules,
brane and the podocytes provide an important means
weight. The reason for these differences in filterability
more readily than negatively charged molecules.
radius, positively charged molecules are filtered much
positive charges. Note that for any given molecular
glomerulus. Dextrans are polysaccharides that can be
Figure 26–11 shows how electrical charge affects the
charges of the glomerular capillary wall proteoglycans.
from filtration, however, because of its negative charge
8 nanometers (80 angstroms). Albumin is restricted
is only about 6 nanometers, whereas the pores of
The molecular diameter of the plasma protein albumin
ing zero.
albumin, the filterability rapidly decreases, approach-
pounds such as glucose are freely filtered. As the
tered only 75 per cent as rapidly as water. Note that
terability of different molecules. A filterability of 1.0
Table 26–1 lists the effect of molecular size on fil-
based on their size and electrical charge.
is selective in determining which molecules will filter,
the high filtration rate, the glomerular filtration barrier
porous and therefore filters fluid at a high rate. Despite
than most other capillaries, but it is also much more
The glomerular capillary membrane is thicker
Filterability of Solutes Is Inversely Related to Their
Urine Formation by the Kidneys: I. Glomerular Filtration, Renal Blood Flow, and Their Control
Chapter 26
317
Size.
means that the substance is filtered as freely as water;
a filterability of 0.75 means that the substance is fil-
electrolytes such as sodium and small organic com-
molecular weight of the molecule approaches that of
Negatively Charged Large Molecules Are Filtered Less Easily
Than Positively Charged Molecules of Equal Molecular Size.
the glomerular membrane are thought to be about
and the electrostatic repulsion exerted by negative
filtration of different molecular weight dextrans by the
manufactured as neutral molecules or with negative or
Neutral dextrans are also filtered more readily than
negatively charged dextrans of equal molecular
is that the negative charges of the basement mem-
the basement membrane are lost even before there are
referred to as
As a result
of this loss of negative charges on the basement
proteinuria or
albuminuria.
static and colloid osmotic forces across the glomerular
and
(2) the glomerular capillary filtration coefficient,
K
f
product of K
f
and the net filtration pressure:
GFR
= K
f
¥ Net filtration pressure
hydrostatic and colloid osmotic forces that either favor
or oppose filtration across the glomerular capillaries
pressure inside the glomerular capillaries (glomerular
G
B
)
colloid osmotic pressure of the glomerular capillary
plasma proteins (
p
G
(4) the colloid osmotic pressure of the proteins in
p
B
protein in the glomerular filtrate is so low that the
GFR
= K
f
¥ (P
G
– P
B
–
p
G
+ p
B
)
Table 26–1
Filterability of Substances by Glomerular Capillaries Based
Myoglobin
17,000
0.75
Inulin
5,500
1.0
Glucose
180
1.0
Sodium
23
1.0
Water
18
1.0
Substance
Molecular Weight
Filterability
on Molecular Weight
Albumin
69,000
0.005
34
38
42
18
22
26
30
Effective molecular radius (A)
Effective molecular radius (A)
Relative filterability
1.0
0.8
0.6
0.4
0.2
0
Polycationic dextran
Polyanionic dextran
Neutral dextran
charges and with varying molecular weights.
manufactured as neutral molecules or with negative or positive
that it is not filtered. Dextrans are polysaccharides that can be
stance is filtered as freely as water, whereas a value of 0 indicates
Effect of size and electrical charge of dextran on its filterability by
Figure 26–11
the glomerular capillaries. A value of 1.0 indicates that the sub-
28 mm Hg, this value usually rises to about 36 mm Hg
Bowman’s capsule,
thereby concentrating the
20 per cent (Figure 26–13). The reason for this is that
the glomerular capillaries to the efferent arterioles,
capsule pressure. This reduces GFR and eventually
outflow of the urinary tract and raising Bowman’s
urinary tract, often in the ureter, thereby obstructing
of uric acid may lead to “stones” that lodge in the
tion of GFR. For example, precipitation of calcium or
pressure can increase markedly, causing serious reduc-
obstruction of the urinary tract, Bowman’s capsule
However, changes in Bowman’s capsule pressure nor-
GFR, whereas decreasing this pressure raises GFR.
the hydrostatic pressure in Bowman’s capsule reduces
about 18 mm Hg under normal conditions. Increasing
estimate for Bowman’s capsule pressure in humans is
static pressure in Bowman’s capsule and at different
Direct measurements, using micropipettes, of hydro-
Increased Bowman’s Capsule
basement membrane and, eventually, by damaging the
ductivity. For example, chronic, uncontrolled hyper-
lation of GFR. Some diseases, however, lower K
reduces GFR, changes in K
about 0.01 ml/min/mm Hg per 100 grams. This high K
of most other capillary systems of the body; the
4.2 ml/min/mm Hg, a value about 400 times as high as
100 grams of kidney weight, it averages about
is expressed per
Hg of filtration pressure. When K
min and the net filtration pressure is 10 mm Hg, the
cannot be measured directly, but it is
laries. The K
The K
altered mainly in disease states, as discussed later.
different physiologic conditions, whereas others are
Glomerular capillary colloid osmotic pressure
32
Bowman’s capsule hydrostatic pressure
18
Bowman’s capsule colloid osmotic pressure
0
Glomerular hydrostatic pressure
60
Figure 26–12):
Based on the results in animals, the approximate
have been estimated in animals such as dogs and rats.
GFR have not been measured directly in humans, they
318
Unit V
The Body Fluids and Kidneys
Although the normal values for the determinants of
normal forces favoring and opposing glomerular fil-
tration in humans are believed to be as follows (see
Forces Favoring Filtration (mm Hg)
Forces Opposing Filtration (mm Hg)
Net filtration pressure
= 60 – 18 – 32 = +10 mm Hg
Some of these values can change markedly under
Increased Glomerular Capillary
Filtration Coefficient Increases GFR
f
is a measure of the product of the hydraulic
conductivity and surface area of the glomerular capil-
f
estimated experimentally by dividing the rate of
glomerular filtration by net filtration pressure:
K
f
= GFR/Net filtration pressure
Because total GFR for both kidneys is about 125 ml/
normal K
f
is calculated to be about 12.5 ml/min/mm
f
the K
f
average K
f
of many other tissues in the body is only
f
for the glomerular capillaries contributes tremen-
dously to their rapid rate of fluid filtration.
Although increased K
f
raises GFR and decreased K
f
f
probably do not provide
a primary mechanism for the normal day-to-day regu-
f
by
reducing the number of functional glomerular capil-
laries (thereby reducing the surface area for filtration)
or by increasing the thickness of the glomerular
capillary membrane and reducing its hydraulic con-
tension and diabetes mellitus gradually reduce K
f
by
increasing the thickness of the glomerular capillary
capillaries so severely that there is loss of capillary
function.
Hydrostatic Pressure Decreases GFR
points in the proximal tubule suggest that a reasonable
mally do not serve as a primary means for regulating
GFR.
In certain pathological states associated with
can damage or even destroy the kidney unless the
obstruction is relieved.
Increased Glomerular Capillary
Colloid Osmotic Pressure
Decreases GFR
As blood passes from the afferent arteriole through
the plasma protein concentration increases about
about one fifth of the fluid in the capillaries filters into
glomerular plasma proteins that are not filtered.
Assuming that the normal colloid osmotic pressure
of plasma entering the glomerular capillaries is
Glomerular
hydrostatic
pressure
(60 mm Hg)
Net filtration
pressure
(10 mm Hg)
=
–
–
Glomerular
oncotic
pressure
(32 mm Hg)
Bowman's
capsule
pressure
(18 mm Hg)
Afferent
arteriole
Efferent
arteriole
Bowman's
capsule
pressure
(18 mm Hg)
Bowman's
capsule
pressure
(18 mm Hg)
Glomerular
hydrostatic
pressure
(60 mm Hg)
Glomerular
hydrostatic
pressure
(60 mm Hg)
Glomerular
colloid osmotic
pressure
(32 mm Hg)
Glomerular
colloid osmotic
pressure
(32 mm Hg)
The values shown are estimates for healthy humans.
Summary of forces causing filtration by the glomerular capillaries.
Figure 26–12
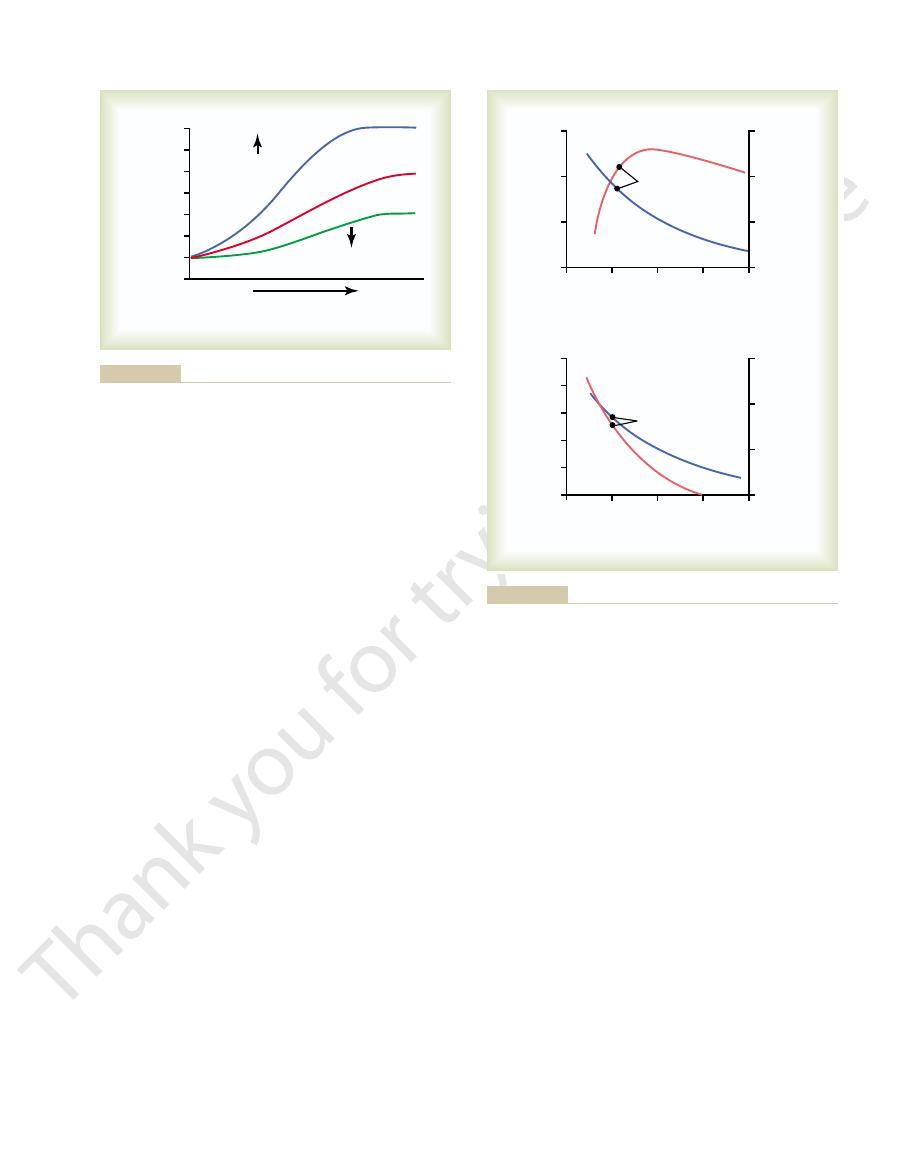
(Figure 26–14).
Conversely, dilation of the afferent arterioles increases
pressure fluctuates.)
GFR. (However, as discussed later, this effect is
lar hydrostatic pressure and, therefore, to increase
efferent arteriolar resistance.
resistance,
arterial pressure,
control: (1)
three variables, each of which is under physiologic
pressure raise GFR, whereas decreases in glomerular
lation of GFR. Increases in glomerular hydrostatic
conditions. Changes in glomerular hydrostatic pres-
The glomerular capillary hydrostatic pressure has
lower rate of blood flow into the glomerulus tends to
flow into the glomerulus tends to increase GFR, and a
glomerular hydrostatic pressure, a greater rate of blood
Consequently, even with a constant
capillaries, causing a slower rise in the glomerular
With increasing renal blood flow, a lower fraction of
pressure.
reason, changes in renal blood flow can influence GFR
osmotic pressure and tend to reduce GFR. For this
GFR or by reducing renal plasma flow. For example, a
tration fraction is defined as GFR/renal plasma flow,
(see Figure 26–13). Because the fil-
colloid osmotic pressure, which in turn decreases
tion fraction). Increasing the arterial plasma colloid
Thus, two factors that influence the glomerular cap-
32 mm Hg.
is midway between 28 and 36 mm Hg, or about
capillaries. Therefore, the average colloid osmotic
Urine Formation by the Kidneys: I. Glomerular Filtration, Renal Blood Flow, and Their Control
Chapter 26
319
by the time the blood reaches the efferent end of the
pressure of the glomerular capillary plasma proteins
illary colloid osmotic pressure are (1) the arterial
plasma colloid osmotic pressure and (2) the fraction
of plasma filtered by the glomerular capillaries (filtra-
osmotic pressure raises the glomerular capillary
GFR.
Increasing the filtration fraction also concentrates the
plasma proteins and raises the glomerular colloid
osmotic pressure
the filtration fraction can be increased either by raising
reduction in renal plasma flow with no initial change
in GFR would tend to increase the filtration fraction,
which would raise the glomerular capillary colloid
independently of changes in glomerular hydrostatic
the plasma is initially filtered out of the glomerular
capillary colloid osmotic pressure and less inhibitory
effect on GFR.
decrease GFR.
Increased Glomerular Capillary
Hydrostatic Pressure Increases GFR
been estimated to be about 60 mm Hg under normal
sure serve as the primary means for physiologic regu-
hydrostatic pressure reduce GFR.
Glomerular hydrostatic pressure is determined by
(2) afferent arteriolar
and (3)
Increased arterial pressure tends to raise glomeru-
buffered by autoregulatory mechanisms that maintain
a relatively constant glomerular pressure as blood
Increased resistance of afferent arterioles reduces
glomerular hydrostatic pressure and decreases GFR.
both glomerular hydrostatic pressure and GFR
Efferent
Afferent
Distance along
glomerular capillary
Distance along
glomerular capillary
Glomerular colloid
osmotic pressure
(mm Hg)
40
38
36
34
32
30
28
end
end
Filtration
fraction
Filtration
fraction
Normal
fraction have the opposite effect.
rises along the glomerular capillary; decreases in the filtration
increase the rate at which the plasma colloid osmotic pressure
the filtration fraction (glomerular filtration rate/renal plasma flow)
centrating the plasma proteins that are not filtered. Increases in
glomerular capillaries filters into Bowman’s capsule, thereby con-
glomerular capillary. Normally, about one fifth of the fluid in the
Increase in colloid osmotic pressure in plasma flowing through the
Figure 26–13
Efferent arteriolar resistance
(X normal)
Efferent arteriolar resistance
(X normal)
Glomerular filtration
rate (ml/min)
150
100
60
0
Renal blood flow
(ml/min)
2000
1400
800
200
0
1
Normal
Renal blood
flow
Glomerular
filtration
rate
2
3
4
Afferent arteriolar resistance
(X normal)
Afferent arteriolar resistance
(X normal)
Glomerular filtration
rate (ml/min)
250
100
150
100
50
0
Renal blood flow
(ml/min)
2000
1400
800
200
0
1
Normal
Renal blood
flow
Glomerular
filtration
rate
2
3
4
olar resistance on glomerular filtration rate and renal blood flow.
Effect of change in afferent arteriolar resistance or efferent arteri-
Figure 26–14
arteries, arterioles, capillaries, and veins (Table 26–3).
the individual vasculature segments, including the
vascular beds, the total vascular resistance through the
about 3 to 4 mm Hg under most conditions. As in other
arterial pressure, and renal vein pressure averages
sures), divided by the total renal vascular resistance:
Determinants of Renal Blood Flow
reflects the basic metabolic needs of the renal cells.
fourth normal. This residual oxygen consumption
pletely ceases, renal sodium reabsorption also ceases,
filtered (Figure 26–15). If glomerular filtration com-
portion to renal tubular sodium reabsorption, which in
Therefore, renal oxygen consumption varies in pro-
and GFR are reduced and less sodium is filtered, less
reabsorption by the renal tubules. If renal blood flow
other tissues.
metabolic needs, and the arterial-venous extraction of
almost seven times the blood flow of the brain. Thus,
On a per gram weight basis, the kidneys normally
Renal Blood Flow and Oxygen
and the excretory functions of the kidneys.
might be expected, the mechanisms that regulate renal
of body fluid volumes and solute concentrations. As
this need. The purpose of this additional flow is to
However, the high flow to the kidneys greatly exceeds
kidneys with nutrients and removes waste products.
As with other tissues, blood flow supplies the
pared with other organs.
per cent of the total body weight, one can readily see
about 22 per cent of the cardiac output. Considering
flow through both kidneys is about 1100 ml/min, or
In an average 70-kilogram man, the combined blood
Table 26–2 summarizes the factors that can decrease
striction; modest efferent constriction raises GFR, but
reduces GFR. However, the effect of efferent arterio-
To summarize, constriction of afferent arterioles
plasma proteins, which also exert an osmotic effect, as
tion, the more rapidly the colloid osmotic pressure
the Donnan effect; the higher the protein concentra-
protein concentration increases, there is a rapid, non-
striction, there is a decrease in GFR. The primary
there is a slight increase in GFR, but with severe con-
effect on GFR. At moderate levels of constriction,
Thus, efferent arteriolar constriction has a biphasic
for filtration actually decreases, causing a
efferent arteriolar constriction. When this occurs, the
increase in efferent arteriolar resistance), the rise in
increases. Therefore, if the constriction of efferent
arteriolar constriction also reduces renal blood flow,
slightly (see Figure 26–14). However, because efferent
reduce renal blood flow too much, GFR increases
This raises the glomerular hydrostatic pressure, and as
resistance to outflow from the glomerular capillaries.
320
Unit V
The Body Fluids and Kidneys
Constriction of the efferent arterioles increases the
long as the increase in efferent resistance does not
the filtration fraction and glomerular colloid osmotic
pressure increase as efferent arteriolar resistance
arterioles is severe (more than about a threefold
colloid osmotic pressure exceeds the increase in
glomerular capillary hydrostatic pressure caused by
net force
reduction in GFR.
cause of the eventual decrease in GFR is as follows:
As efferent constriction becomes severe and as plasma
linear increase in colloid osmotic pressure caused by
rises because of the interaction of ions bound to the
discussed in Chapter 16.
lar constriction depends on the severity of the con-
severe efferent constriction (more than a threefold
increase in resistance) tends to reduce GFR.
GFR.
Renal Blood Flow
the fact that the two kidneys constitute only about 0.4
that they receive an extremely high blood flow com-
supply enough plasma for the high rates of glomeru-
lar filtration that are necessary for precise regulation
blood flow are closely linked to the control of GFR
Consumption
consume oxygen at twice the rate of the brain but have
the oxygen delivered to the kidneys far exceeds their
oxygen is relatively low compared with that of most
A large fraction of the oxygen consumed by the
kidneys is related to the high rate of active sodium
sodium is reabsorbed and less oxygen is consumed.
turn is closely related to GFR and the rate of sodium
and oxygen consumption decreases to about one
Renal blood flow is determined by the pressure gradi-
ent across the renal vasculature (the difference
between renal artery and renal vein hydrostatic pres-
Renal artery pressure is about equal to systemic
kidneys is determined by the sum of the resistances in
Renal artery pressure Renal vein pressure)
Total renal vascular resistance
-
(
Table 26–2
Factors That Can Decrease the Glomerular Filtration Rate
hormones (e.g., norepinephrine,
Sympathetic activity, vasoconstrictor
ow, increased plasma
GFR
Urinary tract obstruction (e.g., kidney
GFR
Renal disease, diabetes mellitus,
Physical Determinants*
Physiologic/Pathophysiologic Causes
(GFR)
Ø K
f
Æ Ø
hypertension
≠ P
B
Æ Ø
stones)
≠ p
G
Æ Ø GFR
Ø Renal blood fl
proteins
Ø P
G
Æ Ø GFR
Ø A
P
Æ Ø P
G
Ø Arterial pressure (has only small effect
due to autoregulation)
Ø R
E
Æ Ø P
G
Ø Angiotensin II (drugs that block
angiotensin II formation)
≠ R
A
Æ Ø P
G
≠
endothelin)
, afferent arteriolar resistance.
resistance; R
, efferent arteriolar
, systemic arterial pressure; R
lary hydrostatic pressure; A
, glomerular capil-
, glomerular capillary colloid osmotic pressure; P
, Bowman
cient; P
, glomerular
* Opposite changes in the determinants usually increase GFR.
K
f
filtration coeffi
B
’s capsule hydrostatic pres-
sure;
p
G
G
P
E
A
bers. Strong activa-
ing the afferent and the efferent arterioles, are richly
Essentially all the blood vessels of the kidneys, includ-
feedback controls that are intrinsic to the kidneys.
released in the kidneys and act locally), and other
uenced by the sympathetic nervous system, hor-
colloid osmotic pressure. These variables, in turn, are
The determinants of GFR that are most variable and
Physiologic Control of
concentrated urine.
system. As discussed in Chapter 28, the vasa recta play
These vessels descend into
ow. Flow to the renal medulla is supplied
ow. Blood
The outer part of the kidney, the renal cortex, receives
with Flow in the Renal Cortex
Renal Medulla Is Very Low Compared
Blood Flow in the Vasa Recta of the
the kidneys, as discussed later in this chapter.
This capacity for autoregulation occurs
range between 80 and 170 mm Hg, a process called
ow, the kidneys have effec-
ow, whereas
mechanisms, as discussed later. An increase in the
various hormones, and local internal renal control
oles, and efferent arterioles. Resistance of these vessels
major segments: interlobular arteries, afferent arteri-
Urine Formation by the Kidneys: I. Glomerular Filtration, Renal Blood Flow, and Their Control
Chapter 26
321
Most of the renal vascular resistance resides in three
is controlled by the sympathetic nervous system,
resistance of any of the vascular segments of the
kidneys tends to reduce the renal blood fl
a decrease in vascular resistance increases renal blood
flow if renal artery and renal vein pressures remain
constant.
Although changes in arterial pressure have some
influence on renal blood fl
tive mechanisms for maintaining renal blood flow and
GFR relatively constant over an arterial pressure
autoregulation.
through mechanisms that are completely intrinsic to
most of the kidney’s blood fl
flow in the renal
medulla accounts for only 1 to 2 per cent of the total
renal blood fl
by a specialized portion of the peritubular capillary
system called the vasa recta.
the medulla in parallel with the loops of Henle and
then loop back along with the loops of Henle and
return to the cortex before emptying into the venous
an important role in allowing the kidneys to form a
Glomerular Filtration and
Renal Blood Flow
subject to physiologic control include the glomerular
hydrostatic pressure and the glomerular capillary
infl
mones and autacoids (vasoactive substances that are
Sympathetic Nervous System
Activation Decreases GFR
innervated by sympathetic nerve fi
tion of the renal sympathetic nerves can constrict the
renal arterioles and decrease renal blood flow and
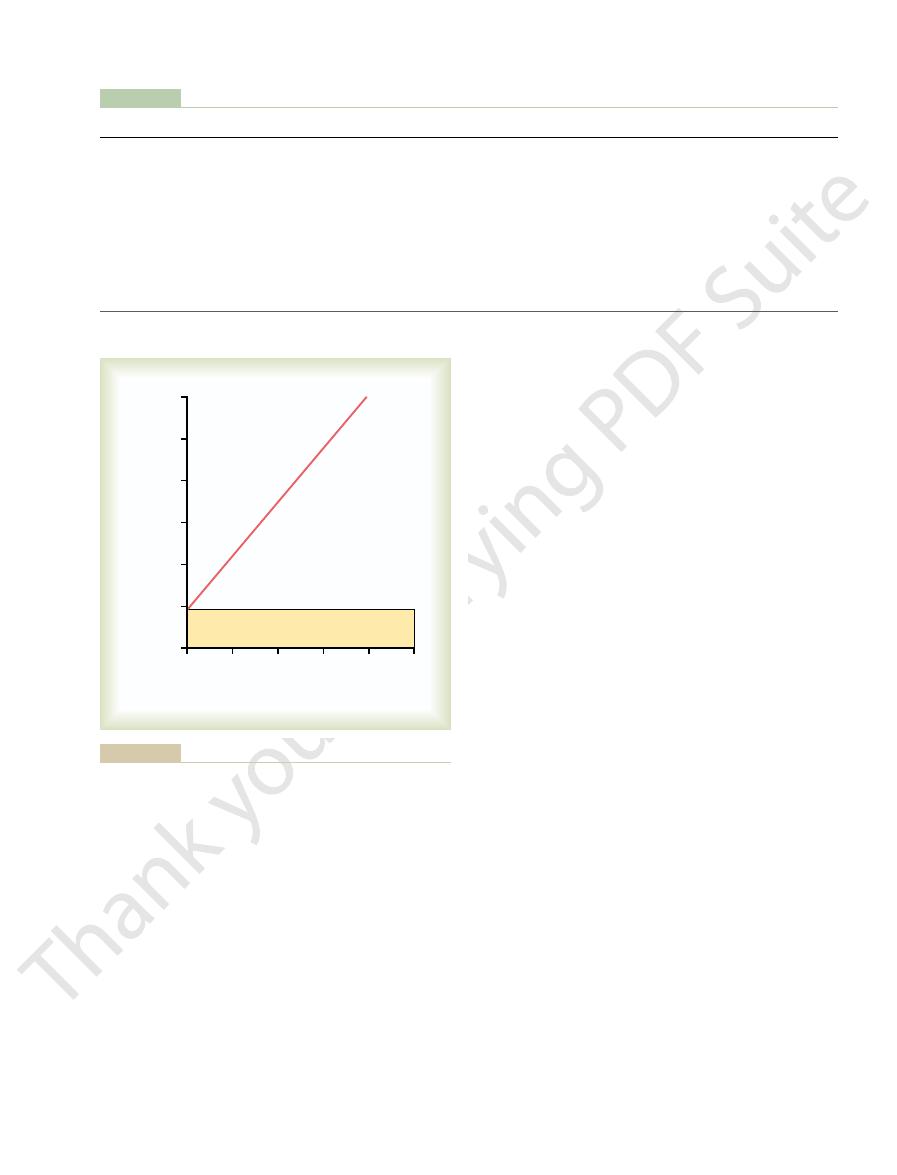
15
20
0
5
10
Oxygen consumption
(ml/min/100 gm kidney weight)
3.0
2.5
2.0
1.5
0.5
1.0
0
Sodium reabsorption
(mEq/min per 100 g kidney weight)
Sodium reabsorption
(mEq/min per 100 g kidney weight)
Basal oxygen consumption
during variations of blood pressure. Pflugers Arch Physiol
sorption in dog kidneys. (Kramer K, Deetjen P: Relation of renal
Relationship between oxygen consumption and sodium reab-
Figure 26–15
oxygen consumption to blood supply and glomerular filtration
271:782, 1960.)
Table 26–3
Interlobar, interlobular, and arcuate veins
8
4
Peritubular capillaries
18
8
Efferent arteriole
59
18
Glomerular capillaries
60
59
Afferent arteriole
85
60
100
85
Interlobar, arcuate, and interlobular arteries
Renal artery
100
100
Per Cent of Total Renal Vascular Resistance
Beginning
End
Vessel
Pressure in Vessel (mm Hg)
Approximate Pressures and Vascular Resistances in the Circulation of a Normal Kidney
~0
~
~16
~26
~1
~43
~10
~4
Renal vein
4
~4
~0
ow. Under stressful
By opposing vasoconstriction of afferent arterioles,
afferent arterioles.
angiotensin II, especially their effects to constrict the
GFR in normal conditions, they may dampen the renal
These substances are discussed in Chapter 17.
Prostaglandins and Bradykinin Tend to Increase GFR.
constriction and increased blood pressure.
some hypertensive patients, impaired nitric oxide pro-
excretion, eventually causing high blood pressure. In
fore, administration of drugs that inhibit this normal
excrete normal amounts of sodium and water. There-
vasodilation of the kidneys. This allows the kidneys to
lial-derived nitric oxide.
creases renal vascular resistance and is released by the
Endothelial-Derived Nitric Oxide Decreases Renal Vascular
detail later in this chapter.
and blood pressure. This effect of angiotensin II in
sodium and water, which helps restore blood volume
the same time, the angiotensin II
ltration for their excretion; at
Thus, increased angiotensin II levels that occur with
water, as discussed in Chapter 27.
ow through the peritubular capillaries,
same time, though, the reduction in renal blood
in glomerular hydrostatic pressure and GFR; at the
constricting efferent arterioles, helps
cumstances, the increased level of angiotensin II, by
depletion, which tend to decrease GFR. In these cir-
ow.
oles, increased angiotensin II levels raise glomerular
as well as in the systemic circulation. Because
renal vasoconstrictor,
conditions.
of pregnancy, acute renal failure, and chronic uremia,
states associated with vascular injury, such as toxemia
and releases this powerful vasoconstrictor. Plasma
vessel is severed, which damages the endothelium
understood. However, endothelin may contribute to
cells of the kidneys as well as by other tissues. The
Another vasoconstrictor,
such as severe hemorrhage.
renal hemodynamics except under extreme conditions,
activity of the sympathetic nervous system; thus, nor-
general, blood levels of these hormones parallel the
released from the adrenal medulla. In
ow, include
afferent and efferent arterioles, causing reductions in
Blood Vessels and Decrease GFR.
Table 26
ow, as summarized in
There are several hormones and autacoids that can
of Renal Circulation
Hormonal and Autacoid Control
ow.
person, sympathetic tone appears to have little in
ischemia, or severe hemorrhage. In the healthy resting
such as those elicited by the defense reaction, brain
turbances lasting for a few minutes to a few hours,
important in reducing GFR during severe, acute dis-
The renal sympathetic nerves seem to be most
example, re
ow and GFR. For
little in
GFR. Moderate or mild sympathetic stimulation has
322
Unit V
The Body Fluids and Kidneys
fluence on renal blood fl
flex activation of the sympathetic nervous
system resulting from moderate decreases in pressure
at the carotid sinus baroreceptors or cardiopulmonary
receptors has little influence on renal blood flow or
GFR.
flu-
ence on renal blood fl
influence GFR and renal blood fl
–4.
Norepinephrine, Epinephrine, and Endothelin Constrict Renal
Hormones that constrict
GFR and renal blood fl
norepinephrine and
epinephrine
epinephrine and epinephrine have little influence on
endothelin, is a peptide
that can be released by damaged vascular endothelial
physiologic role of this autacoid is not completely
hemostasis (minimizing blood loss) when a blood
endothelin levels also are increased in certain disease
and may contribute to renal vasoconstriction and
decreased GFR in some of these pathophysiologic
Angiotensin II Constricts Efferent Arterioles.
A powerful
angiotensin II, can be consid-
ered a circulating hormone as well as a locally pro-
duced autacoid because it is formed in the kidneys
angiotensin II preferentially constricts efferent arteri-
hydrostatic pressure while reducing renal blood fl
It should be kept in mind that increased angiotensin
II formation usually occurs in circumstances associ-
ated with decreased arterial pressure or volume
prevent decreases
flow
caused by efferent arteriolar constriction contributes
to decreased fl
which in turn increases reabsorption of sodium and
a low-sodium diet or volume depletion help preserve
GFR and maintain normal excretion of metabolic
waste products such as urea and creatinine that
depend on glomerular fi
–induced constriction
of efferent arterioles increases tubular reabsorption of
helping to “autoregulate” GFR is discussed in more
Resistance and Increases GFR.
An autacoid that de-
vascular endothelium throughout the body is endothe-
A basal level of nitric oxide
production appears to be important for maintaining
formation of nitric oxide increases renal vascular
resistance and decreases GFR and urinary sodium
duction could be the cause of increased renal vaso-
Hor-
mones and autacoids that cause vasodilation and
increased renal blood flow and GFR include the
prostaglandins (PGE
2
and PGI
2
) and bradykinin.
Although these vasodilators do not appear to be of
major importance in regulating renal blood flow or
vasoconstrictor effects of the sympathetic nerves or
the prostaglandins may help prevent excessive reduc-
tions in GFR and renal blood fl
Hormones and Autacoids That Influence Glomerular
Table 26–4
Hormone or Autacoid
Effect on GFR
Filtration Rate (GFR)
Norepinephrine
Ø
Epinephrine
Ø
Endothelin
Ø
Angiotensin II
¨Æ (prevents Ø)
Endothelial-derived nitric oxide
≠
Prostaglandins
≠
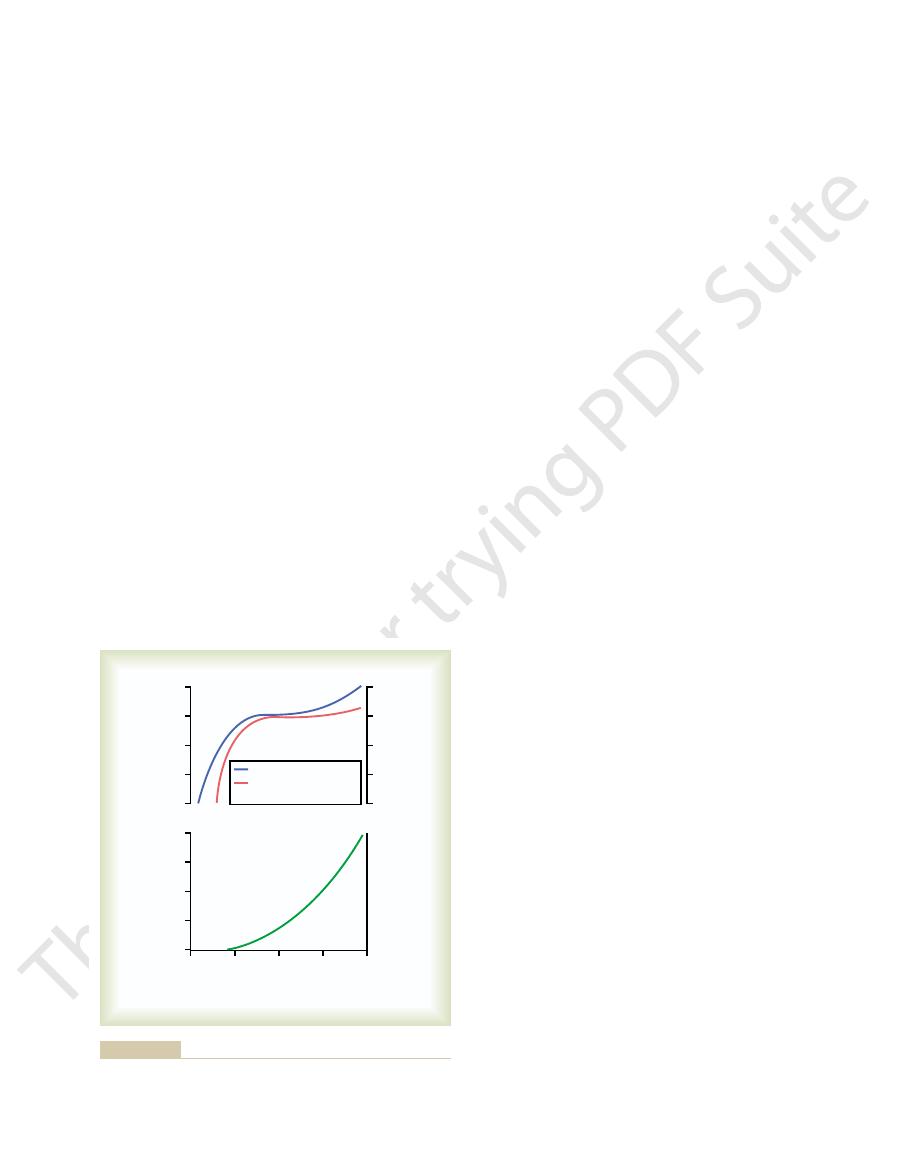
otherwise occur. In many circumstances, this feedback
with the control of renal arteriolar resistance. This
To perform the function of autoregulation, the kidneys
in Autoregulation of GFR
Role of Tubuloglomerular Feedback
arterial pressure, as discussed in Chapters 19 and 29.
pressure natriuresis,
renal excretion of water and sodium; this is referred to
Even with these special control mechanisms, changes
rate when GFR rises, a phenomenon referred to as
changes in GFR that would otherwise occur, and (2)
two reasons: (1) renal autoregulation prevents large
But in reality, such a change in arterial pressure
volume.
Because the total plasma volume is only about 3 liters,
ow to 46.5 L/day
day, this would increase the urine
increase in GFR (from about 180 to 225 L/day). If
to 125 mm Hg) would cause a similar 25 per cent
excreted in the urine. In the absence of autoregulation,
sorption is 178.5 L/day, leaving 1.5 L/day of
Normally, GFR is about 180 L/day and tubular reab-
mechanisms.
sorption, and renal excretion and the changes in renal
ltration, tubular reab-
blood pressure. One can understand the quantitative
100 per cent perfect, but they do prevent potentially
The autoregulatory mechanisms of the kidney are not
Importance of GFR Autoregulation
ciently autoregulated under certain conditions.
regulated in parallel with GFR, but GFR is more ef
percentage points. In general, renal blood
s usual activities. For instance, a decrease in
remains relatively constant), despite considerable
The GFR normally remains autoregulated (that is,
renal excretion of water and solutes.
required for these functions. The major function of
despite changes in the arterial pressure. In the kidneys,
The primary function of blood
(Figure 26
constancy of GFR and renal blood
uences. This relative
body, independent of systemic in
pressure. These mechanisms still function in blood-
constant, despite marked changes in arterial blood
Feedback mechanisms intrinsic to the kidneys nor-
Autoregulation of GFR and
agents, such as aspirin, that inhibit prostaglandin syn-
conditions, such as volume depletion or after surgery,
Urine Formation by the Kidneys: I. Glomerular Filtration, Renal Blood Flow, and Their Control
Chapter 26
323
the administration of nonsteroidal anti-inflammatory
thesis may cause significant reductions in GFR.
Renal Blood Flow
mally keep the renal blood flow and GFR relatively
perfused kidneys that have been removed from the
fl
flow is referred to
as autoregulation
–16).
flow autoregulation
in most tissues other than the kidneys is to maintain
the delivery of oxygen and nutrients at a normal level
and to remove the waste products of metabolism,
the normal blood flow is much higher than that
autoregulation in the kidneys is to maintain a rela-
tively constant GFR and to allow precise control of
arterial pressure fluctuations that occur during a
person’
arterial pressure to as low as 75 mm Hg or an increase
to as high as 160 mm Hg changes GFR only a few
flow is auto-
fi-
in Preventing Extreme Changes in
Renal Excretion
large changes in GFR and renal excretion of water and
solutes that would otherwise occur with changes in
importance of autoregulation by considering the rela-
tive magnitudes of glomerular fi
excretion that would occur without autoregulatory
fluid to be
a relatively small increase in blood pressure (from 100
tubular reabsorption remained constant at 178.5 L/
fl
(the difference between GFR and tubular reabsorp-
tion)—a total increase in urine of more than 30-fold.
such a change would quickly deplete the blood
exerts much less of an effect on urine volume for
there are additional adaptive mechanisms in the renal
tubules that allow them to increase their reabsorption
glomerulotubular balance (discussed in Chapter 27).
in arterial pressure still have significant effects on
as pressure diuresis or
and it is
crucial in the regulation of body fluid volumes and
have a feedback mechanism that links changes in
sodium chloride concentration at the macula densa
feedback helps ensure a relatively constant delivery of
sodium chloride to the distal tubule and helps prevent
spurious fluctuations in renal excretion that would
50
100
150
Renal blood flow
(ml/min)
1600
1200
800
400
Renal blood flow
Glomerular filtration
rate
0
Glomerular filtration
rate (ml/min)
160
120
80
40
0
Arterial pressure
(mm Hg)
Arterial pressure
(mm Hg)
200
Urine output
(ml/min)
8
6
4
2
0
rial pressure.
lack of autoregulation of urine flow during changes in renal arte-
Autoregulation of renal blood flow and glomerular filtration rate but
Figure 26–16
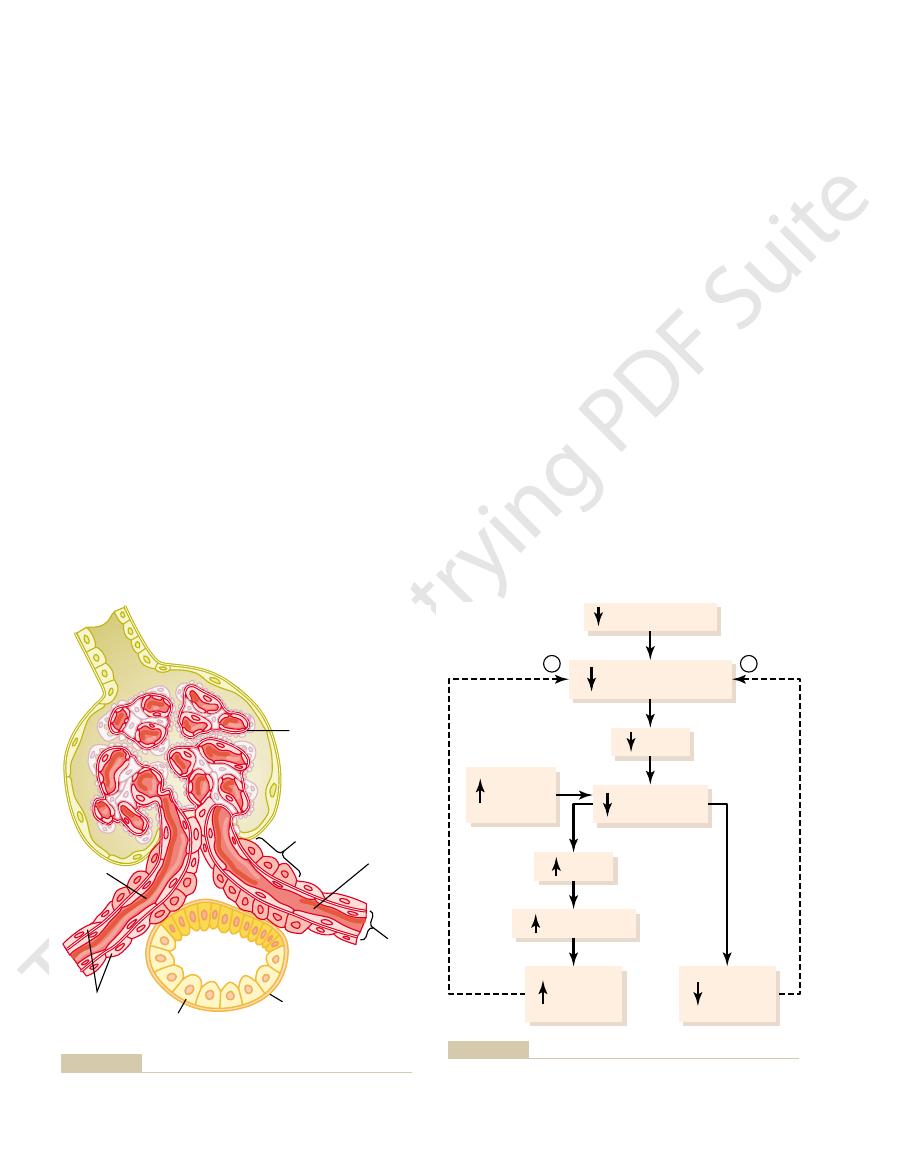
between the limits of 75 and 160 mm Hg.
points, even with large
together, the GFR changes only a few percentage
When both of these mechanisms are functioning
lation of GFR during changes in arterial pressure.
apparatus, provide feedback signals to both the affer-
feedback mechanism, operating together by way of the
These two components of the tubuloglomerular
rioles, thereby increasing glomerular hydrostatic pres-
Finally, the angiotensin II constricts the efferent arte-
angiotensin I, which is converted to angiotensin II.
sites for renin. Renin released from these cells then
and efferent arterioles, which are the major storage
return GFR toward normal, and (2) it increases renin
ow in the afferent arterioles,
18): (1) it decreases
that has two effects (Figure 26
macula densa cells. This decrease in sodium chloride
chloride ions in the ascending loop of Henle, thereby
Henle, causing increased reabsorption of sodium and
pletely understood. Experimental studies suggest that
The
be secreting a substance toward the arterioles.
toward the arterioles, suggesting that these cells may
oles. The macula densa cells contain Golgi apparatus,
efferent arterioles. The macula densa is a specialized
The juxtaglomerular complex consists of
(Figure
an efferent arteriolar feedback mechanism. These
The tubuloglomerular feedback mechanism has
ow, as discussed later.
the distal tubule, there are instances when GFR is
However, because this mechanism is speci
324
Unit V
The Body Fluids and Kidneys
autoregulates renal blood flow and GFR in parallel.
fically
directed toward stabilizing sodium chloride delivery to
autoregulated at the expense of changes in renal blood
fl
two components that act together to control GFR:
(1) an afferent arteriolar feedback mechanism and (2)
feedback mechanisms depend on special anatomical
arrangements of the juxtaglomerular complex
26–17).
macula
densa cells in the initial portion of the distal tubule and
juxtaglomerular cells in the walls of the afferent and
group of epithelial cells in the distal tubules that comes
in close contact with the afferent and efferent arteri-
which are intracellular secretory organelles directed
Decreased Macula Densa Sodium Chloride Causes Dilation of
Afferent Arterioles and Increased Renin Release.
macula densa cells sense changes in volume delivery
to the distal tubule by way of signals that are not com-
decreased GFR slows the flow rate in the loop of
reducing the concentration of sodium chloride at the
concentration initiates a signal from the macula densa
–
resistance to blood fl
which raises glomerular hydrostatic pressure and helps
release from the juxtaglomerular cells of the afferent
functions as an enzyme to increase the formation of
sure and returning GFR toward normal.
special anatomical structure of the juxtaglomerular
ent and the efferent arterioles for efficient autoregu-
fluctuations in arterial pressure
Juxtaglomerular
cells
Afferent
arteriole
Internal
elastic
lamina
Efferent
arteriole
Smooth
muscle
fiber
Distal
tubule
Glomerular
epithelium
Basement
membrane
Macula densa
sible feedback role in the control of nephron function.
Structure of the juxtaglomerular apparatus, demonstrating its pos-
Figure 26–17
Glomerular hydrostatic
pressure
-
-
GFR
Renin
Angiotensin II
Proximal
NaCl
reabsorption
Macula densa
NaCl
Efferent
arteriolar
resistance
Afferent
arteriolar
resistance
Arterial pressure
(GFR) during decreased renal arterial pressure.
glomerular hydrostatic pressure and glomerular filtration rate
Macula densa feedback mechanism for autoregulation of
Figure 26–18
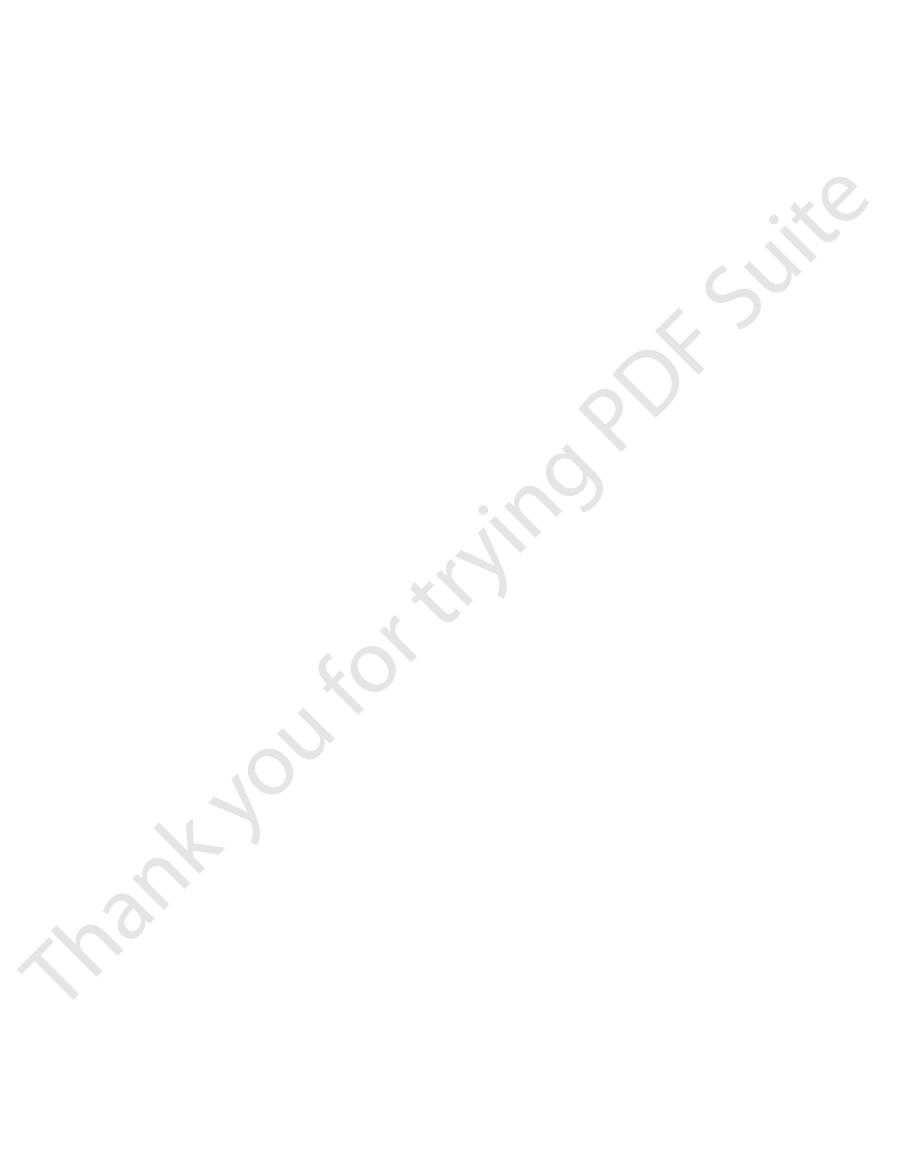
naling. Annu Rev Physiol 65:481, 2003.
Bell PD, Lapointe JY, Peti-Peterdi J: Macula densa cell sig-
Annu Rev Physiol 42:531, 1980.
Beeuwkes R III: The vascular organization of the kidney.
in the urine.
uid solutes, and tubular
the proper rate of delivery of sodium chloride, other
the macula densa in these circumstances. These exam-
depletion.
One of the important compensatory
compensations, would quickly cause excessive volume
delivered to the distal tubule and, without appropriate
consequence, large amounts of sodium chloride are
ability to reabsorb sodium chloride is decreased. As a
or large doses of drugs, such as tetracyclines), their
a result of poisoning by heavy metals, such as mercury,
mal tubular reabsorption is reduced. For example, when
tion can be maintained (see Figure 26
ow and GFR, which
nal processing of the urine takes place. Thus, distur-
delivery of sodium chloride to the distal tubule, where
by the tubuloglomerular feedback mechanism. The
These examples demonstrate that renal blood
chloride to the macula densa, activating a tubu-
with glucose. This, in turn, decreases delivery of sodium
the proximal tubule, increased glucose delivery to the
amino acids, is also reabsorbed along with sodium in
Because glucose, like some of the
diabetes mellitus.
increases in renal blood flow and GFR that occur with
A similar mechanism may also explain the marked
products of protein metabolism, such as urea.
ow and GFR. This increased GFR
earlier. The decreased afferent arteriolar resistance then
in resistance of the afferent arterioles, as discussed
decreases sodium delivery to the macula densa, which
lates sodium reabsorption in the proximal tubules. This
tubules, increased amino acid reabsorption also stimu-
sorbed in the proximal tubule. Because amino acids
release of amino acids into the blood, which are reab-
tion is the following: A high-protein meal increases the
not completely understood, but one possible explana-
The exact mechanisms by which this occurs are still
growth of the kidneys. However, GFR and renal blood
such as one that contains large amounts of meat, the
With a chronic high-protein diet,
blood flow and GFR.
a high protein intake is known to increase both renal
cantly. For example,
stable under most conditions, there are circumstances in
Blood Flow and GFR: High Protein
ow or GFR per se.
ates in most arterioles throughout the body, its impor-
increases.
vascular resistance, helps prevent excessive increases
tention of the vessel and at the same time, by raising
cussed in Chapter 8. This contraction prevents overdis-
uid into the cells,
contraction of the vascular smooth muscle. Stretch
myogenic mechanism.
resist stretching during increased arterial pressure, a
Myogenic Autoregulation of Renal
not occur.
heart failure, and other conditions, as long as they are
agents in many patients with hypertension, congestive
some cases, cause acute renal failure. Nevertheless,
artery) is a severe decrease in GFR that can, in
Therefore, an important complication of using these
pressure falls below normal. The administration of
As discussed earlier, a preferential
Urine Formation by the Kidneys: I. Glomerular Filtration, Renal Blood Flow, and Their Control
Chapter 26
325
Blockade of Angiotensin II Formation Further Reduces GFR During
Renal Hypoperfusion.
constrictor action of angiotensin II on efferent arteri-
oles helps prevent serious reductions in glomerular
hydrostatic pressure and GFR when renal perfusion
drugs that block the formation of angiotensin II
(angiotensin-converting enzyme inhibitors) or that
block the action of angiotensin II (angiotensin II antag-
onists) causes greater reductions in GFR than usual
when the renal arterial pressure falls below normal.
drugs to treat patients who have hypertension because
of renal artery stenosis (partial blockage of the renal
angiotensin II–blocking drugs can be useful therapeutic
monitored to ensure that severe decreases in GFR do
Blood Flow and GFR
Another mechanism that contributes to the main-
tenance of a relatively constant renal blood flow
and GFR is the ability of individual blood vessels to
phenomenon referred to as the
Studies of individual blood vessels (especially small
arterioles) throughout the body have shown that they
respond to increased wall tension or wall stretch by
of the vascular wall allows increased movement of
calcium ions from the extracellular fl
causing them to contract through the mechanisms dis-
in renal blood flow and GFR when arterial pressure
Although the myogenic mechanism probably oper-
tance in renal blood flow and GFR autoregulation has
been questioned by some physiologists because this
pressure-sensitive mechanism has no means of directly
detecting changes in renal blood fl
Other Factors That Increase Renal
Intake and Increased Blood Glucose
Although renal blood flow and GFR are relatively
which these variables change signifi
increases in GFR and renal blood flow are due partly to
flow increase 20 to 30 per cent within 1 or 2 hours after
a person eats a high-protein meal.
and sodium are reabsorbed together by the proximal
elicits a tubuloglomerular feedback–mediated decrease
raises renal blood fl
allows sodium excretion to be maintained at a nearly
normal level while increasing the excretion of the waste
large increases in blood glucose levels in uncontrolled
tubules causes them to reabsorb excess sodium along
loglomerular feedback–mediated dilation of the affer-
ent arterioles and subsequent increases in renal blood
flow and GFR.
flow
and GFR per se are not the primary variables controlled
main purpose of this feedback is to ensure a constant
fi
bances that tend to increase reabsorption of sodium
chloride at tubular sites before the macula densa tend
to elicit increased renal blood fl
helps return distal sodium chloride delivery toward
normal so that normal rates of sodium and water excre-
–18).
An opposite sequence of events occurs when proxi-
the proximal tubules are damaged (which can occur as
responses appears to be a tubuloglomerular feed-
back–mediated renal vasoconstriction that occurs in
response to the increased sodium chloride delivery to
ples again demonstrate the importance of this feedback
mechanism in ensuring that the distal tubule receives
tubular fl
fluid volume so that
appropriate amounts of these substances are excreted
References
c inhibitors. Am J Med 110 (Suppl 3A):33S,
ammatory drugs versus cyclooxyge-
Whelton A: Renal aspects of treatment with conventional
Annu Rev Physiol 65:501, 2003.
loglomerular feedback: adenosine, ATP, and nitric oxide.
Schnermann J, Levine DZ: Paracrine factors in tubu-
control of cardiovascular function. Physiol Rev 82:131,
Roman RJ: P-450 metabolites of arachidonic acid in the
284:F253, 2003.
medullary microcirculation. Am J Physiol Renal Physiol
Pallone TL, Zhang Z, Rhinehart K: Physiology of the renal
5:135, 2003.
angiotensin II and hypertension. Curr Hypertens Rep
Navar LG, Kobori H, Prieto-Carrasquero M: Intrarenal
York: Raven Press, 2000, pp 587-654.
Physiology and Pathophysiology, 3rd ed. New
malian kidney. In Seldin DW, Giebisch G (eds): The
Kriz W, Kaissling B: Structural organization of the mam-
glomerular barrier. News Physiol Sci 19:7, 2004.
uria? An update of our current understanding of the
rensson J: Why do we not all have protein-
Haraldsson B, S
2000, pp 1009-1046.
and Pathophysiology, 3rd ed. New York: Raven Press,
Seldin DW, Giebisch G (eds): The Kidney
system: renal mechanisms and circulatory homeostasis. In
Hall JE, Brands MW: The renin-angiotensin-aldosterone
Nephrol 10 (Suppl 12):s258, 1999.
ulation: the overriding dominance of the kidney. J Am Soc
Hall JE: Angiotensin II and long-term arterial pressure reg-
future. Hypertension 41:621, 2003.
DiBona GF: Neural control of the kidney: past, present, and
281:F579, 2001.
of glomerular permeability. Am J Physiol Renal Physiol
Deen WM, Lazzara MJ, Myers BD: Structural determinants
the vascular myogenic response. Physiol Rev 79:387,
Davis MJ, Hill MA: Signaling mechanisms underlying
ow.
Cowley AW Jr, Mori T, Mattson D, Zou AP: Role of renal
Kidney Int 61:782, 2002.
Blantz RC, Deng A, Lortie M, et al: The complex role of
326
Unit V
The Body Fluids and Kidneys
nitric oxide in the regulation of glomerular ultrafiltration.
NO production in the regulation of medullary blood fl
Am J Physiol Regul Integr Comp Physiol 284:R1355,
2003.
1999.
—Physiology
ö
Kidney—
2002.
nonsteroidal anti-infl
nase-2-specifi
2001.
