
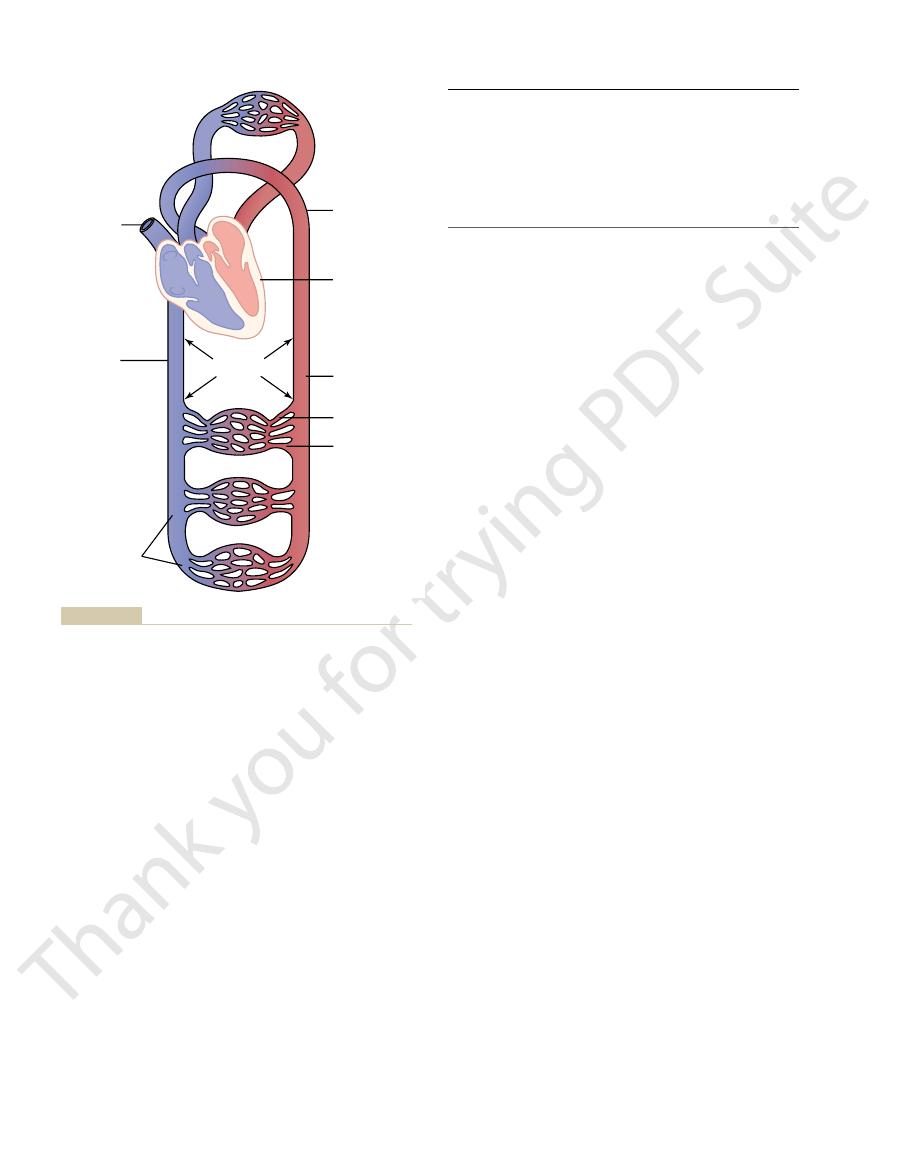
Figure 14–1 gives an
Volumes of Blood in the Different Parts of the Circulation.
controllable reservoir for the extra blood, either a small or a large amount,
Even so, they are muscular enough to contract or expand and thereby act as a
Because the pressure in the venous system is very low, the venous walls are thin.
to the heart; equally important, they serve as a major reservoir of extra blood.
The
into progressively larger veins.
collect blood from the capillaries, and they gradually coalesce
The
permeable to water and other small molecular substances.
To serve this role, the capillary walls are very thin and have numerous minute
hormones, and other substances between the blood and the interstitial fluid.
is to exchange fluid, nutrients, electrolytes,
The function of the
blood flow in each tissue bed in response to the need of the tissue.
by relaxing, dilate it severalfold, thus having the capability of vastly altering
through which blood is released into the capillaries. The arte-
are the last small branches of the arterial system; they act as
The
at a high velocity in the arteries.
tissues. For this reason, the arteries have strong vascular walls, and blood flows
The function of the
tion, it is important to understand the role of each part of the circulation.
flow to all the tissues of the body except the lungs, it is also called the
The circulation, shown in Figure 14–1, is divided into the
Physical Characteristics of the Circulation
functions of the circulation? These are some of the topics and questions that we
trolling blood volume and blood flow, and how does this relate to all the other
sure to cause the needed tissue blood flow. What are the mechanisms for con-
controlled in response to tissue need for nutrients. The heart and circulation in
The rate of blood flow through most tissues is
optimal survival and function of the cells.
another, and, in general, to maintain an appropriate
the body tissues, to transport waste products away,
The function of the circulation is to service the
Flow, and Resistance
Medical Physics of Pressure,
C
H
A
P
T
E
R
1
4
161
Overview of the Circulation;
needs of the body tissues—to transport nutrients to
to conduct hormones from one part of the body to
environment in all the tissue fluids of the body for
turn are controlled to provide the necessary cardiac output and arterial pres-
discuss in this section on the circulation.
systemic circulation
and the pulmonary circulation. Because the systemic circulation supplies blood
greater
circulation or peripheral circulation.
Functional Parts of the Circulation.
Before discussing the details of circulatory func-
arteries is to transport blood under high pressure to the
arterioles
control conduits
riole has a strong muscular wall that can close the arteriole completely or can,
capillaries
capillary pores
venules
veins function as conduits for transport of blood from the venules back
depending on the needs of the circulation.
overview of the circulation and lists the percentage of the total blood volume
are in accord with the needs of the lungs, because
culation. The low pressures of the pulmonary system
7 mm Hg. Yet the total blood flow through the lungs
The mean pulmonary capillary pressure averages only
a mean pulmonary arterial pressure of only 16 mm Hg.
8 mm Hg, with
about 25 mm Hg and
pulmonary artery systolic pressure
pulsatile, just as in the aorta, but the pressure level is
In the pulmonary arteries, the pressure is
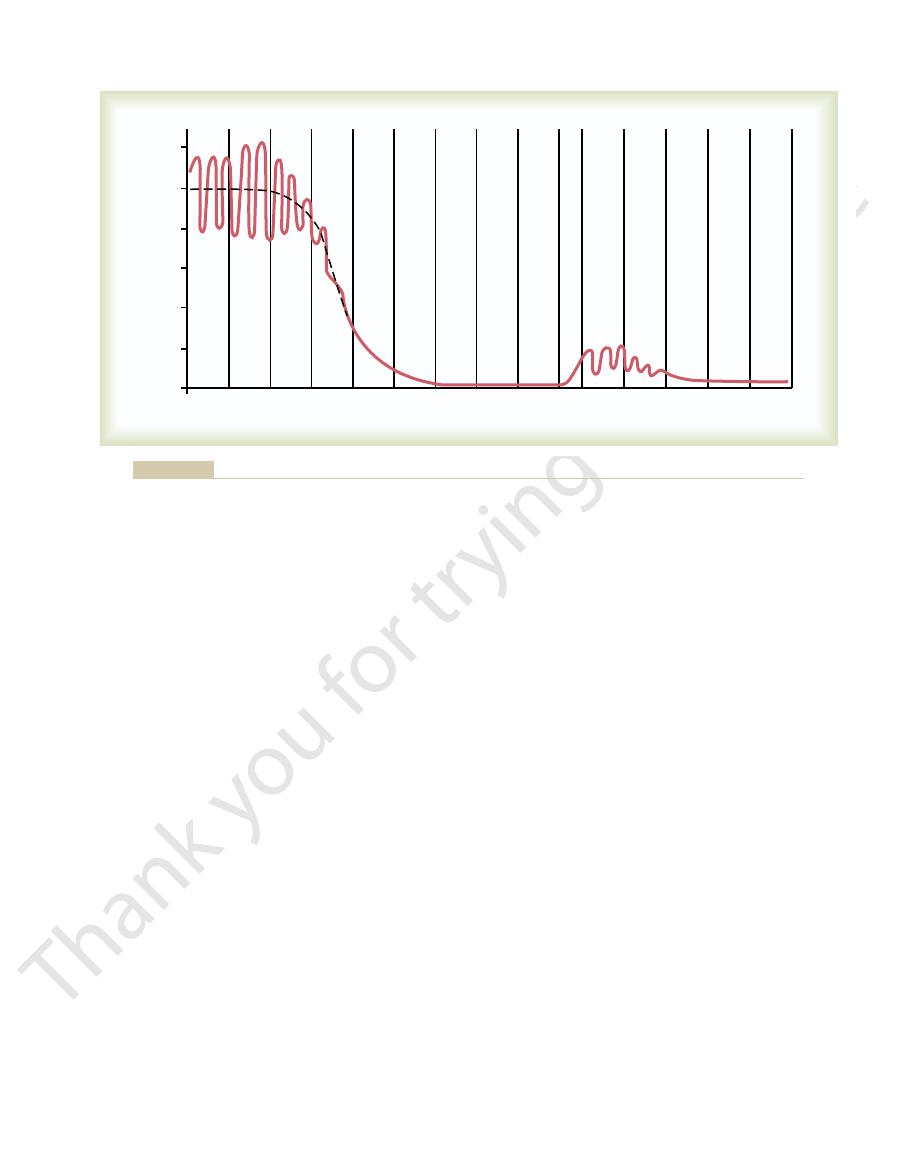
Note at the far right side of Figure 14–2 the respec-
these same pores to the outlying tissue cells.
walls, even though nutrients can
17 mm Hg, a pressure low enough that little of the
“functional” pressure in most vascular beds is about
as 10 mm Hg near the venous ends, but their average
as high as 35 mm Hg near the arteriolar ends to as low
The pressure in the systemic capillaries varies from
its mean pressure falls progressively to about 0 mm Hg
of 80 mm Hg, as shown on the left side of Figure 14–2.
of 120 mm Hg and a
100 mm Hg. Also, because heart pumping is pulsatile,
the mean pressure in the aorta is high, averaging about
Pressures in the Various Portions of the Circulation.
ingly short time.
remains in the capillaries for only 1 to 3 seconds. This
typical length of only 0.3 to 1 millimeter, the blood
0.3 mm/sec. However, because the capillaries have a
aorta but only 1/1000 as rapidly in the capillaries, about
ditions, the velocity averages about 33 cm/sec in the
vascular cross-sectional area. Thus, under resting con-
through each segment of the circulation each minute,
four times those of the corresponding arteries. This
areas of the veins than of the arteries, averaging about
of each type were put side by side,
Cross-Sectional Areas and Velocities of Blood Flow.
tissues. This function is discussed in detail in Chapter
function of the circulation occurs, diffusion of sub-
illaries. It is here, however, that the most important
and the pulmonary vessels, 9 per cent.
capillaries. The heart contains 7 per cent of the blood,
arteries, and 7 per cent in the systemic arterioles and
culation, 64 per cent is in the veins, 13 per cent in the
heart and lungs. Of the 84 per cent in the systemic cir-
body is in the systemic circulation, and 16 per cent in
in major segments of the circulation. For instance,
162
Unit IV
The Circulation
about 84 per cent of the entire blood volume of the
Most surprising is the low blood volume in the cap-
stances back and forth between the blood and the
16.
If all the
systemic vessels
their approximate total cross-sectional areas for the
average human being would be as follows:
Note particularly the much larger cross-sectional
explains the large storage of blood in the venous
system in comparison with the arterial system.
Because the same volume of blood must flow
the velocity of blood flow is inversely proportional to
short time is surprising because all diffusion of
nutrient food substances and electrolytes that occurs
through the capillary walls must do so in this exceed-
Because
the heart pumps blood continually into the aorta,
the arterial pressure alternates between a systolic pres-
sure level
diastolic pressure level
As the blood flows through the systemic circulation,
by the time it reaches the termination of the venae
cavae where they empty into the right atrium of the
heart.
plasma leaks through the minute pores of the capillary
diffuse easily through
tive pressures in the different parts of the pulmonary
circulation.
far less:
averages
diastolic pressure
each minute is the same as through the systemic cir-
all that is required is to expose the blood in the
Systemic
vessels
Veins, venules,
Arteries–13%
Arterioles
and
capillaries–7%
Heart–7%
Aorta
Pulmonary circulation–9%
and venous
sinuses–64%
Inferior
vena cava
Superior
vena cava
parts of the circulatory system.
Distribution of blood (in percentage of total blood) in the different
Figure 14–1
Small veins
80
Venules
250
Capillaries
2500
Arterioles
40
Small arteries
20
Aorta
2.5
Vessel
Cross-Sectional Area (cm
2
)
Venae cavae
8
control of cardiac output and arterial pressure.
remainder of this chapter, we begin to discuss the basic
are served specifically by the circulation. In the
Thus, in summary, the needs of the individual tissues
and by regulating the blood volume.
prolonged periods, hours and days, the kidneys
increase the arterial pressure. Then, over more
heart, and (c) cause generalized constriction of
heart pumping, (b) cause contraction of the large
raise the pressure back toward normal. The
100 mm Hg, within seconds a barrage of nervous
For instance, if at any time the pressure falls
controlling the arterial blood pressure.
The circulatory
independently of either local blood flow control
3. In general the arterial pressure is controlled
pump the required amounts of blood flow.
the tissues. The heart, however, often needs help
as an automaton, responding to the demands of
whence it had originally come. Thus, the heart acts
the veins to the heart. The heart responds
through a tissue, it immediately returns by way of
When blood flows
sum of all the local tissue flows.
2. The cardiac output is controlled mainly by the
flow.
activity. Also, nervous control of the circulation
constricting them, to control local blood flow
act directly on the local blood vessels, dilating or
and other tissue waste products, and these in turn
of each tissue continuously monitor tissue needs,
demands increased flow. Instead, the microvessels
seven times greater than resting levels. Therefore,
the resting level. Yet the heart normally cannot
When tissues are active, they need
is almost always precisely controlled in relation to
1. The rate of blood flow to each tissue of the body
complex, there are three basic principles that underlie
Basic Theory of Circulatory
Overview of the Circulation; Medical Physics of Pressure, Flow, and Resistance
Chapter 14
163
pulmonary capillaries to oxygen and other gases in the
pulmonary alveoli.
Function
Although the details of circulatory function are
all functions of the system.
the tissue need.
greatly increased supply of nutrients and
therefore much more blood flow than when at
rest—occasionally as much as 20 to 30 times
increase its cardiac output more than four to
it is not possible simply to increase blood flow
everywhere in the body when a particular tissue
such as the availability of oxygen and other
nutrients and the accumulation of carbon dioxide
precisely to that level required for the tissue
from the central nervous system provides
additional help in controlling tissue blood
automatically to this increased inflow of blood by
pumping it immediately into the arteries from
in the form of special nerve signals to make it
or cardiac output control.
system is provided with an extensive system for
significantly below the normal level of about
reflexes elicits a series of circulatory changes to
nervous signals especially (a) increase the force of
venous reservoirs to provide more blood to the
most of the arterioles throughout the body so that
more blood accumulates in the large arteries to
play an additional major role in pressure control
both by secreting pressure-controlling hormones
details of the management of tissue blood flow and
Systemic
Pulmonary
Pressure (mm Hg)
0
60
80
100
120
40
20
0
Aorta
Large arteries
Small arteries
Arterioles
Capillaries
Venules
Small veins
Large veins
Venae cavae
Pulmonary arteries
Arterioles
Capillaries
Venules
Pulmonary veins
Normal blood pressures in the different portions of the circulatory system when a person is lying in the horizontal position.
Figure 14–2
tance of this formula, the reader should also become
ics of the circulation. Because of the extreme impor-
Ohm’s law, illustrated in Equation 1, expresses the
pressure.
will be no flow despite the presence of 100 mm Hg
yet no difference exists between the two ends, there
the pressure at both ends of a vessel is 100 mm Hg and
vessel, that determines rate of flow. For example, if
two ends of the vessel, not the absolute pressure in the
ference but inversely proportional to the resistance.
the resistance. This formula states, in effect, that the
) between the two ends of the vessel, and R is
in which F is blood flow,
Ohm’s law
culated by the following formula, which is called
the vessel. The flow through the vessel can be cal-
. Resistance occurs
at the other end, the pressure is P
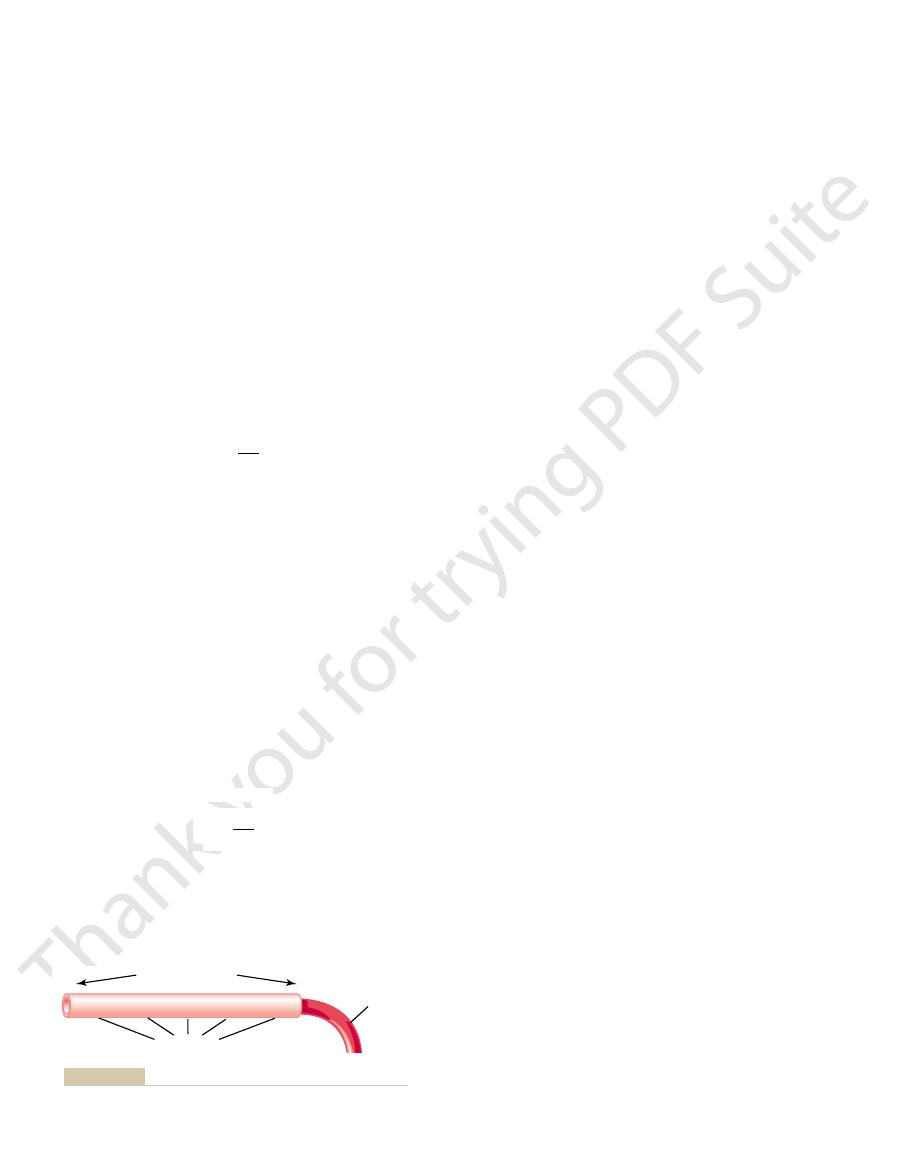
these relationships, showing a blood vessel segment
Figure 14–3 demonstrates
vascular resistance.
impediment to blood flow through the vessel, which is
that pushes the blood through the vessel, and (2) the
“pressure gradient” along the vessel, which is the force
tween the two ends of the vessel, also sometimes called
two factors: (1)
Pressure, Flow, and
Interrelationships Among
164
Unit IV
The Circulation
Resistance
Blood flow through a blood vessel is determined by
pressure difference of the blood be-
called
located anywhere in the circulatory system.
P
1
represents the pressure at the origin of the vessel;
2
as a result of friction between the flowing blood and
the intravascular endothelium all along the inside of
:
DP is the pressure difference
(P
1
- P
2
blood flow is directly proportional to the pressure dif-
Note that it is the difference in pressure between the
most important of all the relations that the reader
needs to understand to comprehend the hemodynam-
familiar with its other algebraic forms:
Blood Flow
Blood flow means simply the quantity of blood that
passes a given point in the circulation in a given period
R
P
F
=
D
P
F
R
D =
¥
F
P
R
=
D
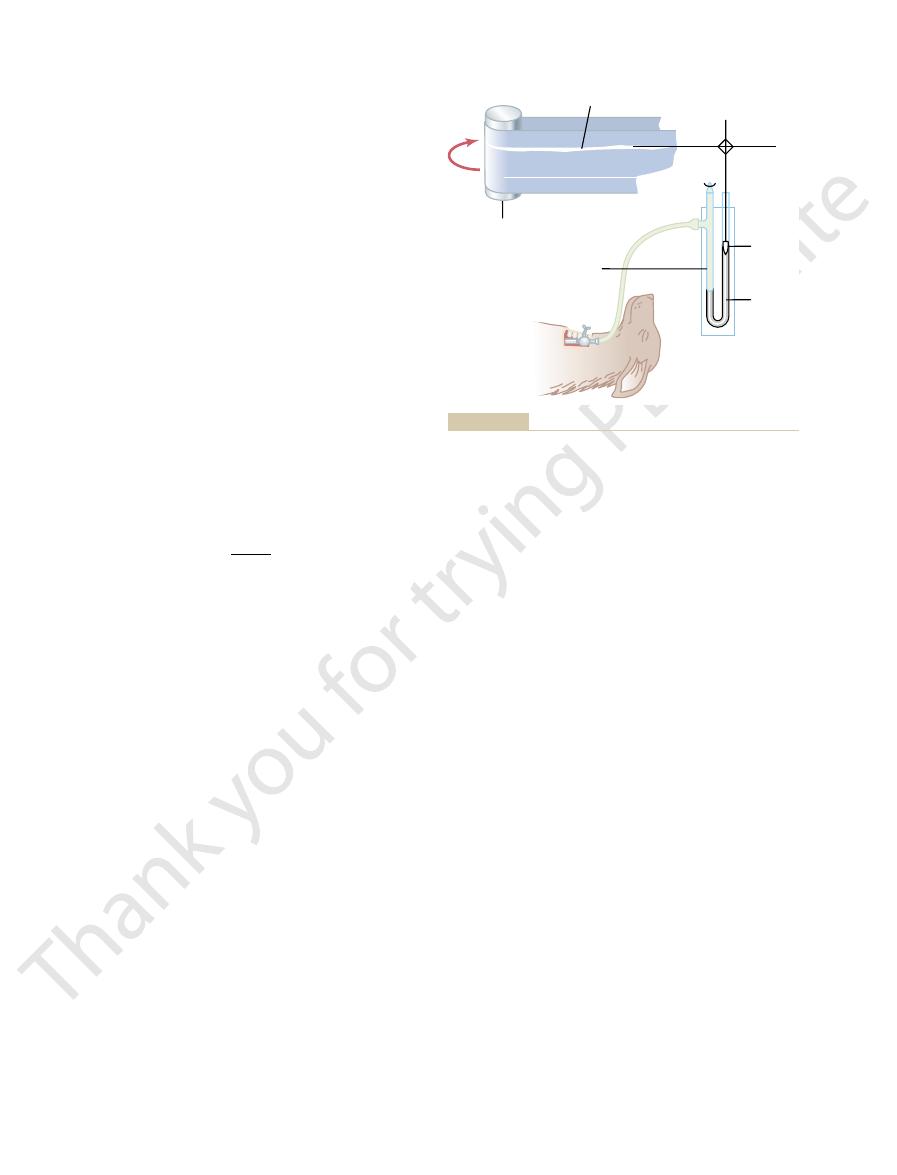
ed greatly by the electronic apparatus. Another
frequency ultrasound wave is intermittently cut off, and
5, the high-
owmeter shown in Figure 14
For the
approaching.)
by the person, the pitch of the sound from the whistle
while blowing its whistle. Once the whistle has passed
is called the Doppler effect. (It is the same effect that
cells are moving away from the transmitter crystal. This
frequency than the transmitted wave because the red
ected waves have a lower
toward the crystal. These re
owing blood. The re
owing blood. A portion of the sound is re
dred thousand cycles per second downstream along the
transmits ultrasound at a frequency of several hun-
energized with an appropriate electronic apparatus,
at one end in the wall of the device. This crystal, when
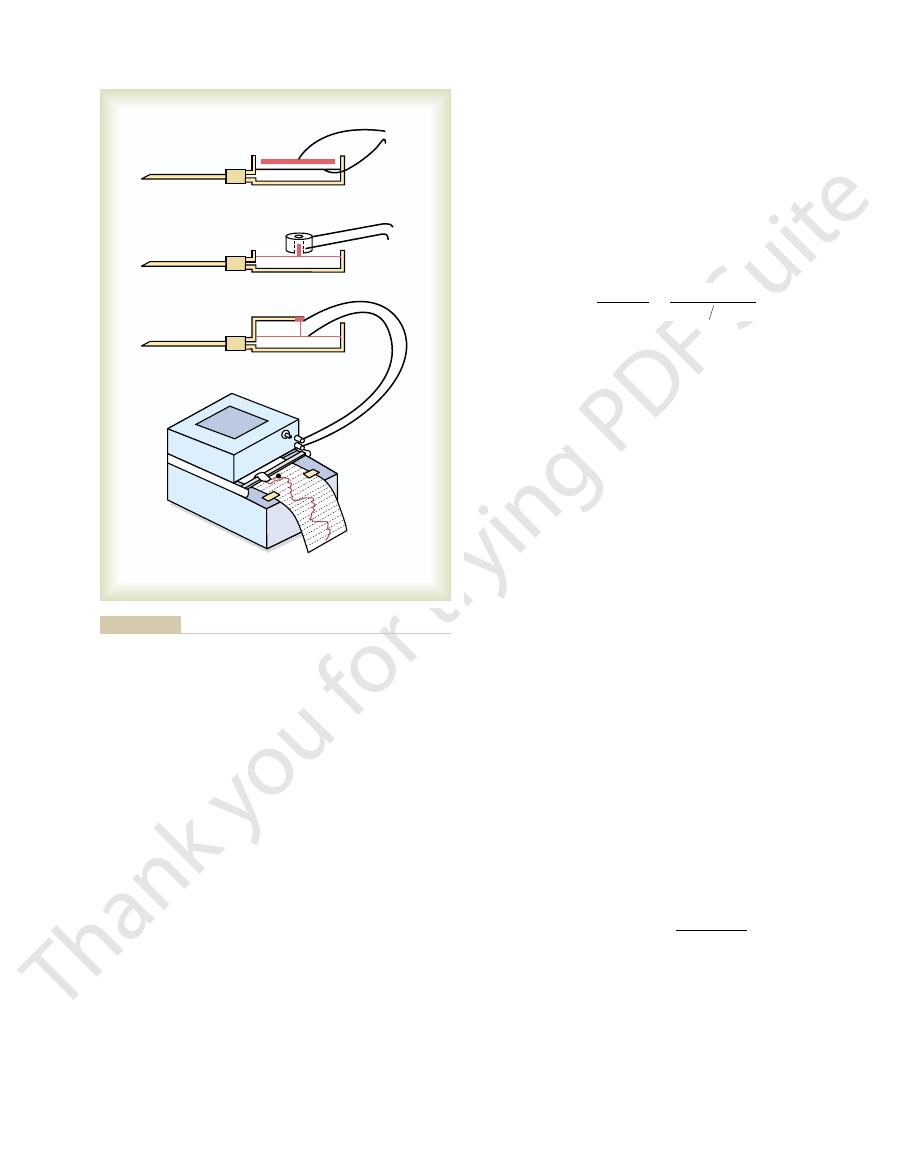
5. A minute piezoelectric crystal is mounted
Figure 14
ultrasonic Doppler flowmeter,
Ultrasonic Doppler Flowmeter.
ow.
of a second, allowing accurate recording of pulsatile
magnet and the electrodes.
ow. The probe contains both the strong
recording apparatus. Figure 14
ow is generated between the two electrodes, and this
lines of force. When blood
of a strong magnet, and electrodes are placed on the
this case, a blood vessel is placed between the poles
eld. In
electric generator. Figure 14
eld. This is the well-
4. Figure 14
of which are illustrated in Figure 14
owmeter, the principles
Electromagnetic Flowmeter.
flowmeters.
ow. They are called
a blood vessel or, in some instances, applied to the
Methods for Measuring Blood Flow.
pumped into the aorta by the heart each minute.
cardiac output
adult person at rest is about 5000 ml/min. This is called
The overall blood
ow.
liters per minute,
ow is expressed in
of time. Ordinarily, blood fl
milliliters
per minute or
but it can be expressed
in milliliters per second or in any other unit of fl
flow in the total circulation of an
the
because it is the amount of blood
Many mechanical and
mechanoelectrical devices can be inserted in series with
outside of the vessel to measure fl
One of the most important
devices for measuring blood flow without opening the
vessel is the electromagnetic fl
–
–4A
shows the generation of electromotive force (electrical
voltage) in a wire that is moved rapidly in a cross-wise
direction through a magnetic fi
known principle for production of electricity by the
–4B shows that the same
principle applies for generation of electromotive force
in blood that is moving through a magnetic fi
two sides of the vessel perpendicular to the magnetic
flows through the vessel,
an electrical voltage proportional to the rate of blood
fl
is recorded using an appropriate voltmeter or electronic
–4C shows an actual
“probe” that is placed on a large blood vessel to record
its blood fl
A special advantage of the electromagnetic flowme-
ter is that it can record changes in flow in less than 1/100
changes in flow as well as steady fl
Another type of flowmeter
that can be applied to the outside of the vessel and that
has many of the same advantages as the electromagnetic
flowmeter is the
shown in
–
fl
flected by the
red blood cells in the fl
flected ultra-
sound waves then travel backward from the blood cells
fl
one experiences when a train approaches and passes by
suddenly becomes much lower than when the train is
fl
–
the reflected wave is received back onto the crystal and
amplifi
portion of the electronic apparatus determines the
Pressure gradient
P
1
P
2
Resistance
Blood flow
Interrelationships among pressure, resistance, and blood flow.
Figure 14–3

le is the following:The
The cause of the parabolic pro
ow.
long distance. This effect is called the
slightly away from the wall has moved a small distance,
cent to the vessel wall has hardly moved, the portion
; the portion of
1 second later in Figure 14
a parabolic interface develops between them, as shown
ow,
ow in the vessel. When the
uid, but there is
uids, the one at the left colored by
6. In Figure 14
This is demonstrated in Figure 14
vessel is far greater than that toward the outer edges.
ow occurs, the velocity of
When laminar
Parabolic Velocity Profile During Laminar Flow.
subsequently.
continually mixing within the vessel, as discussed
, which
turbulent flow
, and it is the opposite of
line flow
laminar flow
vessel. This type of
same distance from the vessel wall. Also, the central
, with each layer of blood remaining the
steady rate through a long, smooth blood vessel, it
When blood
Laminar Flow of Blood in Vessels.
ow.
owmeter is capable of recording rapid, pul-
owmeter, the ultrasonic
ow.
ected wave, thus determining the velocity of
frequency difference between the transmitted wave and
Overview of the Circulation; Medical Physics of Pressure, Flow, and Resistance
Chapter 14
165
the refl
blood fl
Like the electromagnetic fl
Doppler fl
satile changes in flow as well as steady fl
flows at a
flows
in streamlines
most portion of the blood stays in the center of the
flow is called
or stream-
is blood flowing in all directions in the vessel and
fl
flow in the center of the
–
–6A, a
vessel contains two fl
a dye and the one at the right a clear fl
no fl
fluids are made to fl
–6B
fluid adja-
and the portion in the center of the vessel has moved a
“parabolic profile
for velocity of blood fl
”
fi
fluid molecules touching the wall barely move because
–
+
0
–
+
0
N
S
+
+
–
–
A
B
N
S
C
for chronic implantation around
electromagnetic flowmeter probe
); and a modern
field and blood flows through
is placed in a strong magnetic
electrical voltage in electrodes on
passes through an electromag-
electrical voltage in a wire as it
Flowmeter of the electromagnetic
Figure 14–4
type, showing generation of an
netic field (A); generation of an
a blood vessel when the vessel
the vessel (B
blood vessels (C).
Crystal
Reflected
wave
Transmitted
wave
Ultrasonic Doppler flowmeter.
Figure 14–5
A
B
C
lent flow, with elements of the fluid moving in a disorderly pattern.
, Two fluids (one dyed red, and the other clear) before flow
Figure 14–6
A
begins; B, the same fluids 1 second after flow begins; C, turbu-
because the mercury manometer (shown in Figure
is measured in millimeters of mercury (mm Hg)
turbulence.
number is almost never high enough to cause
(4) large vessel diameter. However, in small vessels,
ow, (3) sudden change in vessel diameter, and
ow, (2) pulsatile nature of
ejection by the ventricles; this causes considerable tur-
number
of the aorta and pulmonary artery, Reynolds
the branches of these vessels. In the proximal portions
even normally rises to 200 to 400 in large arteries; as a
number for
straight, smooth vessel.
imately 2000, turbulence will usually occur even in a
number rises above approx-
However, when Reynolds
will die out along the smooth portions of the vessels.
number rises above 200 to 400,
than 1. When Reynolds
about 1/30 poise, and the density is only slightly greater
cosity (in poise). The viscosity of blood is normally
is density, and
, r
ow (in centimeters/second), d is the vessel
tendency for turbulence to occur,
inversely proportional to the viscosity of the blood, in
the blood vessel, and the density of the blood, and is
ow, the diameter of
The tendency for turbulent
When eddy currents are present, the blood
. These are similar to the whirlpools that one
). Turbulent
(see Figure 14
, or disorderly, rather than streamline
when it passes over a rough surface, the
obstruction in a vessel, when it makes a sharp turn, or
ow becomes too great, when it passes by an
When the rate
Turbulent Flow of Blood Under Some Conditions.
more rapidly than the outer layers.
thus, each layer toward the center
the fourth layer over the third, and so forth. Therefore,
ecules slips over these, the third layer over the second,
of adherence to the vessel wall. The next layer of mol-
166
Unit IV
The Circulation
the fluid in the middle of the vessel can move rapidly
because many layers of slipping molecules exist
between the middle of the vessel and the vessel wall;
flows progressively
of blood fl
flow may then
become turbulent
–6C
flow means that the blood
flows crosswise in the vessel as well as along the vessel,
usually forming whorls in the blood called eddy cur-
rents
frequently sees in a rapidly flowing river at a point of
obstruction.
flows with
much greater resistance than when the flow is stream-
line because eddies add tremendously to the overall
friction of flow in the vessel.
flow increases in direct
proportion to the velocity of blood fl
accordance with the following equation:
where Re is Reynolds’ number and is the measure of the
n is the mean velocity
of blood fl
diameter (in centimeters)
h is the vis-
’
turbulent flow will occur at some branches of vessels but
’
Reynolds’
flow in the vascular system
result there is almost always some turbulence of flow at
’
can rise to several thousand during the rapid phase of
bulence in the proximal aorta and pulmonary artery
where many conditions are appropriate for turbulence:
(1) high velocity of blood fl
the fl
Reynolds’
Blood Pressure
Standard Units of Pressure.
Blood pressure almost always
14–7) has been used since antiquity as the standard
Re
=
◊ ◊
n
r
h
d
is low, it returns toward its resting position.
sure is high, the membrane bulges slightly, and when it
in which the pressure is to be measured. When the pres-
uid chamber. The
cal recorder. Each of these transducers uses a very thin,
recorder is needed. Figure 14
changing pressures, some other type of pressure
3 seconds. Whenever it is desired to record rapidly
that occur more rapidly than about one cycle every 2 to
steady pressures, cannot respond to pressure changes
mercury manometer, although excellent for recording
that it cannot rise and fall rapidly. For this reason, the
The
1 millimeter.
that of water, and 1 centimeter is 10 times as great as
gravity to a height of 10 centimeters.
. A pressure of 10 cm H
Occasionally, pressure is measured in
up to 100 millimeters.
sure is 100 mm Hg, it will push the column of mercury
against gravity up to a level 50 mm high. If the pres-
pressure in a vessel is 50 mm Hg, one means that the
. When one says that the
force exerted by the blood against any
reference for measuring pressure. Actually, blood pres-
sure means the
unit area of the vessel wall
force exerted is sufficient to push a column of mercury
centimeters of
water (cm H
2
O)
2
O means a
pressure sufficient to raise a column of water against
One millimeter of
mercury pressure equals 1.36 cm water pressure
because the specific gravity of mercury is 13.6 times
High-Fidelity Methods for Measuring Blood Pressure.
mercury in the mercury manometer has so much inertia
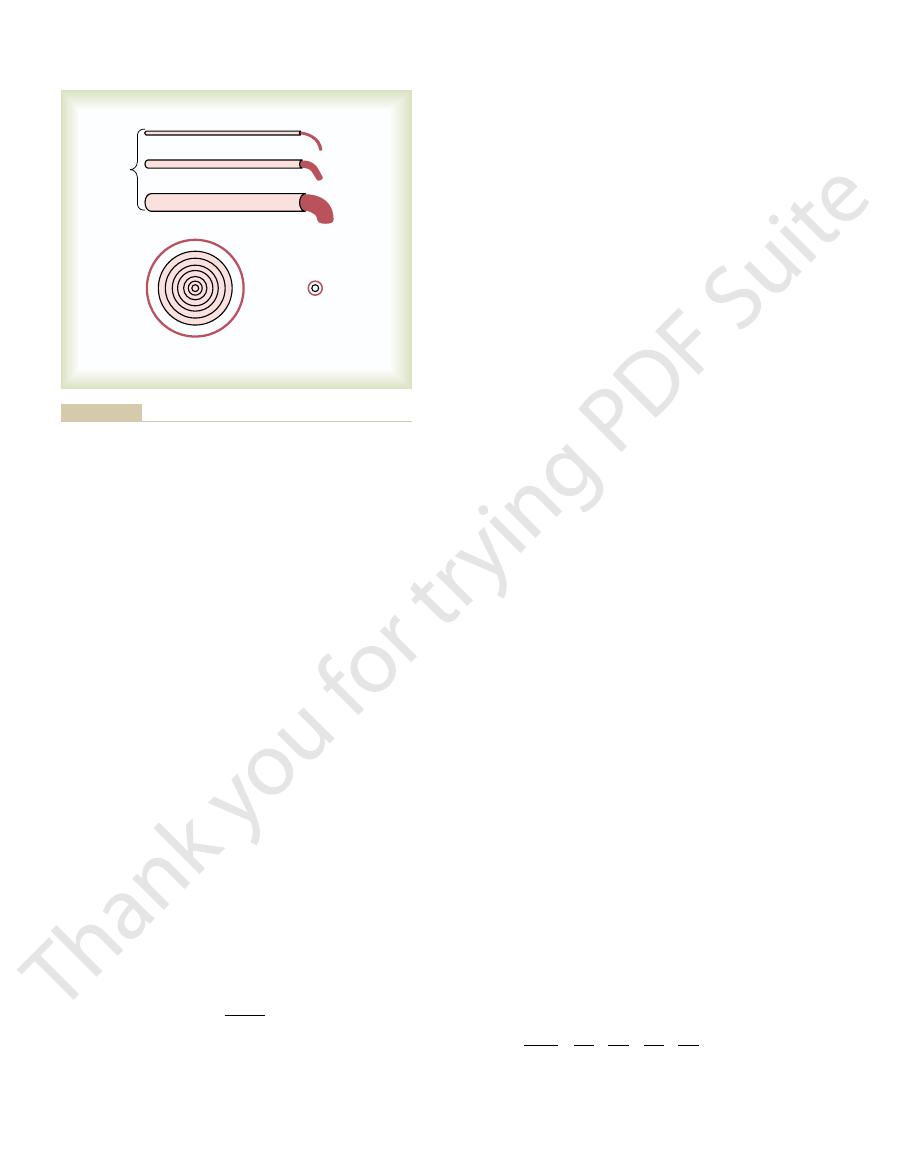
–8 demonstrates the basic
principles of three electronic pressure transducers com-
monly used for converting blood pressure and/or rapid
changes in pressure into electrical signals and then
recording the electrical signals on a high-speed electri-
highly stretched metal membrane that forms one wall
of the fl
fluid chamber in turn is con-
nected through a needle or catheter to the blood vessel
Anticoagulant
solution
Float
0 pressure
Mercury
Mercury
manometer
Moving sooted
paper
100 mm Hg pressure
throughout the history of physiology.
that has been used in the manner shown for recording pressure
Recording arterial pressure with a mercury manometer, a method
Figure 14–7
of the vessels. Although the diameters of these vessels
sure difference of 100 mm Hg between the two ends
relative diameters of 1, 2, and 4 but with the same pres-
trated in Figure 14
lined. This is demonstrated by the experiment illus-
Conductance Tremendously!
Very Slight Changes in Diameter of a Vessel Can Change Its
pressure.
per millimeter of mercury pressure, but it can also be
through a vessel for a given pressure difference. This
“Conductance” of Blood in a Vessel and Its Relation to Resis-
0.14 PRU (about one seventh that in the systemic
output is normal at about 100 ml/sec, the
sure difference of 14 mm. Therefore, when the cardiac
atrial pressure averages 2 mm Hg, giving a net pres-
rial pressure averages 16 mm Hg and the mean left
In the pulmonary system, the mean pulmonary arte-
dilated, the resistance can fall to as little as 0.2 PRU.
PRU. Conversely, when the vessels become greatly
out the body become strongly constricted, the total
100/100, or 1 PRU.
total peripheral resistance,
lation, called the
Therefore, the resistance of the entire systemic circu-
arteries to the systemic veins is about 100 mm Hg.
100 ml/sec. The pressure difference from the systemic
output. In the adult human being, this is approximately
that is, it is equal to the cardiac
The rate of blood
Total Peripheral Vascular Resistance and Total Pulmonary Vas-
. Resistance in these units can
seconds) unit is used to express resistance. This unit is
basic physical unit called the CGS (centimeters, grams,
Occasionally, a
PRU
, usually abbreviated
ow is 1 ml/sec, the resistance is said to be 1
pressure difference between two points is 1 mm Hg
difference between two points in the vessel. If the
any direct means. Instead, resistance must be calcu-
ow in a vessel, but it cannot be measured by
Resistance to Blood Flow
manner shown on the recording paper in Figure 14
occur as rapidly as 20 to 100 cycles per second, in the
have been recorded accurately. In common use are
systems, pressure cycles up to 500 cycles per second
With some of these high-
too, can be recorded by an electronic system.
stretched less, its resistance decreases. These changes,
is stretched greatly, its resistance increases; when it is
ance wire is connected to the membrane. When this wire
a very thin, stretched resist-
Finally, in Figure 14
and this, too, can be recorded electronically.
space inside an electrical wire coil. Movement of the
brane, and this can be displaced upward into a center
In Figure 14
between these two, and this change in capacitance can
the plate, which increases the
the membrane bulges, the membrane comes closer to
hundredths of a centimeter above the membrane. When
In Figure 14
Overview of the Circulation; Medical Physics of Pressure, Flow, and Resistance
Chapter 14
167
–8A, a simple metal plate is placed a few
electrical capacitance
be recorded using an appropriate electronic system.
–8B, a small iron slug rests on the mem-
iron into the coil increases the inductance of the coil,
–8C,
fidelity types of recording
recorders capable of registering pressure changes that
–8C.
Units of Resistance.
Resistance is the impediment to
blood fl
lated from measurements of blood flow and pressure
and the fl
peripheral resistance unit
.
Expression of Resistance in CGS Units.
dyne seconds/centimeters
5
be calculated by the following formula:
cular Resistance.
flow through the
entire circulatory system is equal to the rate of blood
pumping by the heart—
is about
In conditions in which all the blood vessels through-
peripheral resistance occasionally rises to as high as 4
total
pulmonary vascular resistance calculates to be about
circulation).
tance.
Conductance is a measure of the blood flow
is generally expressed in terms of milliliters per second
expressed in terms of liters per second per millimeter
of mercury or in any other units of blood flow and
It is evident that conductance is the exact reciprocal
of resistance in accord with the following equation:
Slight changes in the diame-
ter of a vessel cause tremendous changes in the vessel’s
ability to conduct blood when the blood flow is stream-
–9A, which shows three vessels with
Conductance
Resistance
=
1
ml sec
mm Hg
R in
dyne
cm
sec
5
1333
Ê
Ë
ˆ
¯ =
¥
A
B
C
rapidly changing blood pressures (explained in the text).
Principles of three types of electronic transducers for recording
Figure 14–8
of the vessel, l is length of the vessel, and
difference between the ends of the vessel, r is the radius
ow,
derive the following formula, known as Poiseuille
multiplying them by the areas of the rings, one can
stream of blood simply does not exist. By integrating the
wall, so that the extremely rapidly
In the small vessel, essentially all the blood is near the
ows extremely rapidly.
ows extremely slowly, whereas that in the
velocities. Thus, the blood that is near the wall of the
fth, and
ows more rapidly. The third, fourth,
therefore,
the vascular endothelium. The next ring of blood toward
That is, the blood in the ring touching the wall of the
ow, which was discussed earlier in the chapter.
of a large and a small vessel. The concentric rings inside
by referring to Figure 14
The cause of this great increase in con-
Poiseuille’s Law.
fourth power of the diameter,
Thus, the conductance of the vessel increases in pro-
ow.
and 256 ml/mm, which is a 256-fold increase in
ows are 1, 16,
increase only fourfold, the respective
168
Unit IV
The Circulation
fl
fl
portion to the
in accor-
dance with the following formula:
ductance when the diameter increases can be explained
–9B, which shows cross sections
the vessels indicate that the velocity of flow in each ring
is different from that in the adjacent rings because of
laminar fl
vessel is barely flowing because of its adherence to
the center of the vessel slips past the first ring and,
fl
fi
sixth rings likewise flow at progressively increasing
vessel fl
middle of the vessel fl
flowing central
velocities of all the concentric rings of flowing blood and
’s law:
in which F is the rate of blood fl
DP is the pressure
h is viscosity
of the blood.
F
l
=
p
h
D Pr
4
8
Conductance
Diameter
µ
4
ow is expressed
), the total resistance to blood
For blood vessels arranged in parallel (Figure
ow to other tissues.
extent, independently of
ow, to a great
tissues of the body. This parallel arrangement permits
, the total vascular resistance
shown in Figure 14
oles, capillaries, venules, and veins. In the example
equal to the sum of resistances of the arteries, arteri-
The total peripheral vascular resistance is therefore
vessels are arranged in series,
veins are collectively arranged in series. When blood
lel. The arteries, arterioles, capillaries, venules, and
the low pressure side (i.e., vena cava) through many
pressure part of the systemic circulation (i.e., aorta) to
Resistance to Blood Flow in Series and Parallel Vascular Cir-
ow. Indeed, ranges of blood
signals, either to turn off almost completely the blood
the arterioles, responding with only small changes in
Thus, this fourth power law makes it possible for
the vessel, one can see that a fourfold increase in vessel
often as much as fourfold. From the fourth power law
allow the internal diameters to change tremendously,
25 micrometers. However, their strong vascular walls
arterioles. The internal diameters of the arterioles
tion, about two thirds of the total systemic resistance
Importance of the Vessel Diameter “Fourth Power Law” in
of the vessel, which demonstrates once
fourth power
Note particularly in this equation that the rate of
blood flow is directly proportional to the
of the radius
again that the diameter of a blood vessel (which is equal
to twice the radius) plays by far the greatest role of all
factors in determining the rate of blood flow through a
vessel.
Determining Arteriolar Resistance.
In the systemic circula-
to blood flow is arteriolar resistance in the small
range from as little as 4 micrometers to as great as
discussed above that relates blood flow to diameter of
diameter can increase the flow as much as 256-fold.
diameter to nervous signals or local tissue chemical
flow to the tissue or at the other extreme to cause a
vast increase in fl
flow of
more than 100-fold in separate tissue areas have been
recorded between the limits of maximum arteriolar
constriction and maximum arteriolar dilatation.
cuits.
Blood pumped by the heart flows from the high
miles of blood vessels arranged in series and in paral-
flow through each blood
vessel is the same and the total resistance to blood flow
(R
total
) is equal to the sum of the resistances of each
vessel:
–10A
is equal to the sum of R
1
and R
2
.
Blood vessels branch extensively to form parallel
circuits that supply blood to the many organs and
each tissue to regulate its own blood fl
fl
14–10B
fl
as:
It is obvious that for a given pressure gradient,
far greater amounts of blood will flow through this
=
+
+
+
R
R
R
R
R
1
1
1
1
1
1
2
3
4
total
. . .
=
+
+
+
R
R
R
R
R . . .
total
1
2
3
4
P =
100 mm
Hg
d = 1
d = 2
d = 4
1 ml/min
16 ml/min
256 ml/min
Large vessel
Small vessel
A
B
farther away from the vessel wall, the faster the flow.
, Concentric rings of blood flowing at different velocities; the
, Demonstration of the effect of vessel diameter on blood flow.
Figure 14–9
A
B

the viscosity of water.
if all other factors are constant. Furthermore,
ow in a vessel
The greater the viscosity, the less the
in Poiseuille
Viscosity on Vascular Resistance and
Effect of Blood Hematocrit and Blood
increasing total peripheral vascular resistance.
ow (i.e., cardiac output) while
well as the pressure gradient. Therefore, amputation of
ow in the tissue, as
tance of the systemic circulation. Blood
lel, and each tissue contributes to the overall conduc-
skin, and coronary circulations are arranged in paral-
For example, brain, kidney, muscle, gastrointestinal,
ow. The total conductance (C
, for blood
each parallel vessel provides another pathway, or
ance. Many parallel blood vessels, however, make it
resistance.
blood vessels. However, increasing the resistance of
resistance, not the resistance of the other parallel
through each of the parallel vessels in Figure 14
than the resistance of any single blood vessel. Flow
blood vessels. Therefore, the total resistance is far less
Overview of the Circulation; Medical Physics of Pressure, Flow, and Resistance
Chapter 14
169
parallel system than through any of the individual
–10B
is determined by the pressure gradient and its own
any of the blood vessels increases the total vascular
It may seem paradoxical that adding more blood
vessels to a circuit reduces the total vascular resist-
easier for blood to flow through the circuit because
con-
ductance
fl
total
)
for blood flow is the sum of the conductance of each
parallel pathway:
flow through
each tissue is a fraction of the total blood flow (cardiac
output) and is determined by the resistance (the recip-
rocal of conductance) for blood fl
a limb or surgical removal of a kidney also removes a
parallel circuit and reduces the total vascular conduc-
tance and total blood fl
Blood Flow
Note especially that another of the important factors
’s equation is the viscosity of the blood.
fl
the vis-
cosity of normal blood is about three times as great as
But what makes the blood so viscous? It is mainly
the large numbers of suspended red cells in the blood,
=
+
+
+
C
C
C
C
C . . .
total
1
2
3
4
the plasma, but these effects are so much less than
as great as 10 times that of water, and its
, the blood viscosity can become
When the hematocrit rises to 60 or 70, which it often
at normal hematocrit is about 3; this means that three
12. The viscosity of whole blood
as shown in Figure 14
blood increases drastically as the hematocrit increases,
The viscosity of
Effect of Hematocrit on Blood Viscosity.
bration allows direct reading of the percentage of cells.
11. The cali-
a calibrated tube, as shown in Figure 14
the person resides. These changes in hematocrit are
degree of bodily activity, and on the altitude at which
depending on whether the person has anemia, on the
averages about 38. These values vary tremendously,
tocrit of men averages about 42, while that of women
volume is cells and the remainder is plasma.The hema-
ocrit of 40, this means that 40 per cent of the blood
Thus, if a person has a hemat-
The percentage of the blood that is cells is
each of which exerts frictional drag against adjacent
cells and against the wall of the blood vessel.
Hematocrit.
called the hematocrit.
discussed in relation to the red blood cells and their
oxygen transport function in Chapter 32.
Hematocrit is determined by centrifuging blood in
–
–
times as much pressure is required to force whole
blood as to force water through the same blood vessel.
does in polycythemia
flow through
blood vessels is greatly retarded.
Other factors that affect blood viscosity are the
plasma protein concentration and types of proteins in
the effect of hematocrit that they are not significant
A
B
R
1
R
1
R
2
R
2
R
3
R
4
Vascular resistances:
Figure 14–10
A, in series and B, in parallel.
Normal
Anemia
Polycythemia
0
10
20
30
40
50
60
70
80
90
100
0
10
20
30
40
50
60
70
80
90
100
0
10
20
30
40
50
60
70
80
90
100
Hematocrits in a healthy (normal) person and in patients with
Figure 14–11
anemia and polycythemia.
despite high arterial pressure.
more. Conversely, very strong sympathetic stimulation
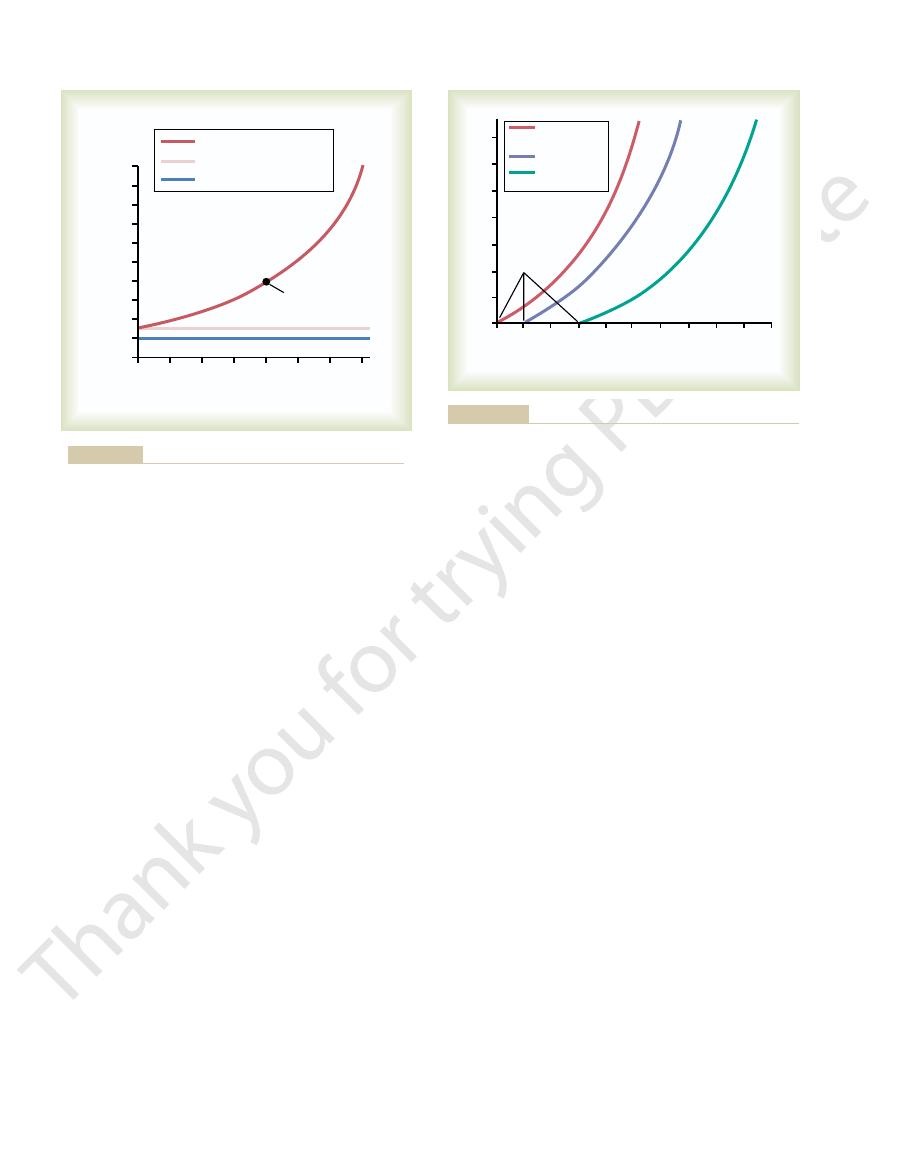
gure,
peripheral blood vessels. Thus, as shown in the
13 the large changes in
Note also in Figure 14
to increase vascular diameter.
ow at 50 mm Hg instead of two times as would
ow at 100 mm Hg
Therefore, for most tissues, blood
ow in both of these ways.
which decreases vascular resistance. Thus, greater
vessels but also distends the vessels at the same time,
13. The reason for
upward curving lines in Figure 14
ow is greater than one would expect, as shown by the
the body. However, the effect of pressure on blood
From the discussion thus far, one might expect an
Resistance and Tissue Blood Flow
Effects of Pressure on Vascular
cosity of blood plasma is about 1.5 times that of water.
considerations in most hemodynamic studies. The vis-
170
Unit IV
The Circulation
increase in arterial pressure to cause a proportionate
increase in blood flow through the various tissues of
fl
–
this is that an increase in arterial pressure not only
increases the force that pushes blood through the
pressure increases the fl
fl
arterial pressure is usually four to six times as great as
blood fl
be true if there were no effect of increasing pressure
–
blood flow that can be caused by either increased
or decreased sympathetic nerve stimulation of the
fi
inhibition of sympathetic activity greatly dilates the
vessels and can increase the blood flow twofold or
can constrict the vessels so much that blood flow occa-
sionally decreases to as low as zero for a few seconds
References
See references for Chapter 15.
0
10
20
30
40
50
60
70
Viscosity (water = 1)
0
9
10
8
7
6
5
4
3
2
1
Hematocrit
Viscosity of whole blood
Viscosity of plasma
Viscosity of water
Normal blood
Effect of hematocrit on blood viscosity. (Water viscosity
Figure 14–12
= 1.)
20
40
60
80 100 120 140 160 180 200
Blood flow (ml/min)
0
0
1
2
3
4
5
6
7
Arterial pressure (mm Hg)
Sympathetic
inhibition
Normal
Sympathetic
stimulation
Critical
closing
pressure
decreased sympathetic stimulation of the vessel.
different degrees of vascular tone caused by increased or
Effect of arterial pressure on blood flow through a blood vessel at
Figure 14–13
