cause automatic rhythmical discharge and contraction. This is especially true of
sinus nodal fibers connect directly with the atrial muscle fibers, so that any
10 to 15 micrometers for the surrounding atrial muscle fibers. However, the
and are each only 3 to 5 micrometers in diameter, in contrast to a diameter of
vena cava. The fibers of this node have almost no contractile muscle filaments
1 millimeter thick. It is located in the superior posterolateral wall of the right
of specialized cardiac muscle about 3 millimeters wide, 15 millimeters long, and
) is a small, flattened, ellipsoid strip
The
the ventricles.
branches of Purkinje fibers,
the impulse from the atria into the ventricles; and the
A-V bundle,
is delayed before passing into the ventricles; the
A-V node,
atrioventricular (A-V) node; the
internodal pathways
), in which the normal rhythmical impulse is generated;
that controls cardiac contractions. The figure shows the
Figure 10–1 shows the specialized excitatory and conductive system of the heart
of the Heart
Specialized Excitatory and Conductive System
of the heart often is affected severely, even to the extent of causing death.
sequence of contraction of the heart chambers, and the pumping effectiveness
coronary blood flow. The result is often a bizarre heart rhythm or abnormal
by heart disease, especially by ischemia of the heart tissues resulting from poor
This rhythmical and conductive system of the heart is susceptible to damage
chambers.
that it allows all portions of the ventricles to contract almost simultaneously,
lungs and peripheral circulation. Another special importance of the system is
tricular contraction, which allows filling of the ven-
heart. When this system functions normally, the atria
The heart is endowed with a special system for (1)
C
H
A
P
T
E
R
1
0
116
Rhythmical Excitation
of the Heart
generating rhythmical electrical impulses to cause
rhythmical contraction of the heart muscle and (2)
conducting these impulses rapidly through the
contract about one sixth of a second ahead of ven-
tricles before they pump the blood through the
which is essential for most effective pressure generation in the ventricular
sinus node (also called
sinoatrial or S-A node
the
that conduct the impulse from the sinus node to the
in which the impulse from the atria
which conducts
left and right bundle
which conduct the cardiac impulse to all parts of
Sinus (Sinoatrial) Node
sinus node (also called sinoatrial node
atrium immediately below and slightly lateral to the opening of the superior
action potential that begins in the sinus node spreads immediately into the atrial
muscle wall.
Automatic Electrical Rhythmicity of the Sinus Fibers
Some cardiac fibers have the capability of self-excitation, a process that can
When the potential reaches a
potential gradually rises between each two heartbeats.
direction. Thus, as shown in Figure 10–2, the “resting”
leak to the inside. Therefore, between heartbeats,
number of already open sodium channels, positive
the nodal fiber, as well as a moderate
Self-Excitation of Sinus Nodal Fibers.
ventricular fiber.
after the action potential does occur, return of the
the action potential of the ventricular muscle. Also,
thereby cause the action potential. As a result, the
channels can open (i.e., can become “activated”) and
remain so. Therefore, only the slow sodium-calcium
millivolts for more than a few milliseconds, the inacti-
blocked. The cause of this is that any time the mem-
“inactivated,” which means that they have become
55 millivolts,
tricular muscle fiber. At this level of
because the “resting”
lasts for about 0.3 second. Finally, opening of potas-
opening of the slow sodium-calcium channels, which
interior of the fiber. Then the “plateau” of the ven-
muscle,
potassium channels.
calcium channels,
slow sodium-
fast sodium channels,
They are (1)
sinus nodal fibers, first recall from the discussions of
ions neutralize much of the intracellular negativity.
are naturally leaky to sodium and calcium ions, and
for the ventricular muscle fiber. The cause of this lesser
60 millivolts, in comparison with
“resting membrane potential” of the sinus nodal fiber
ventricular muscle fiber action potential. Note that the
fiber for three heartbeats and, by comparison, a single
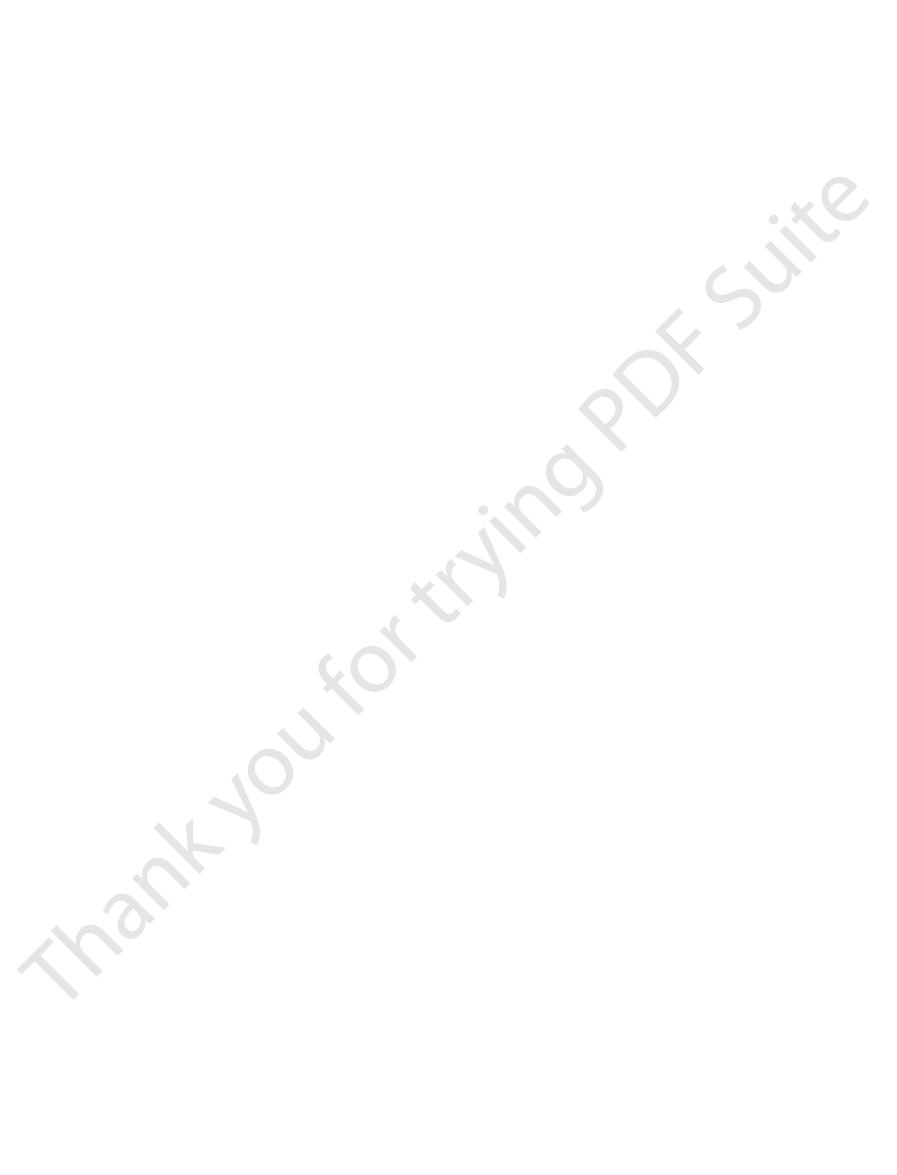
Figure 10–2 shows
Mechanism of Sinus Nodal Rhythmicity.
rhythmicity.
this chapter. First, let us describe this automatic
of the entire heart, as discussed in detail later in
including the fibers of the sinus node. For this reason,
the fibers of the heart’s specialized conducting system,
Chapter 10
Rhythmical Excitation of the Heart
117
the sinus node ordinarily controls the rate of beat
action potentials recorded from inside a sinus nodal
between discharges has a negativity of about
-55 to
-
-85 to -90 millivolts
negativity is that the cell membranes of the sinus fibers
positive charges of the entering sodium and calcium
Before attempting to explain the rhythmicity of the
Chapters 5 and 9 that cardiac muscle has three types
of membrane ion channels that play important roles in
causing the voltage changes of the action potential.
(2)
and (3)
Opening
of the fast sodium channels for a few 10,000ths of a
second is responsible for the rapid upstroke spike of
the action potential observed in ventricular
because of rapid influx of positive sodium ions to the
tricular action potential is caused primarily by slower
sium channels allows diffusion of large amounts of
positive potassium ions in the outward direction
through the fiber membrane and returns the mem-
brane potential to its resting level.
But there is a difference in the function of these
channels in the sinus nodal fiber
potential is much less negative—only
-55 millivolts in
the nodal fiber instead of the
-90 millivolts in the ven-
-
the fast sodium channels mainly have already become
brane potential remains less negative than about
-55
vation gates on the inside of the cell membrane that
close the fast sodium channels become closed and
atrial nodal action potential is slower to develop than
potential to its negative state occurs slowly as well,
rather than the abrupt return that occurs for the
Because of the
high sodium ion concentration in the extracellular
fluid outside
sodium ions from outside the fibers normally tend to
influx of positively charged sodium ions causes a slow
rise in the resting membrane potential in the positive
threshold voltage of
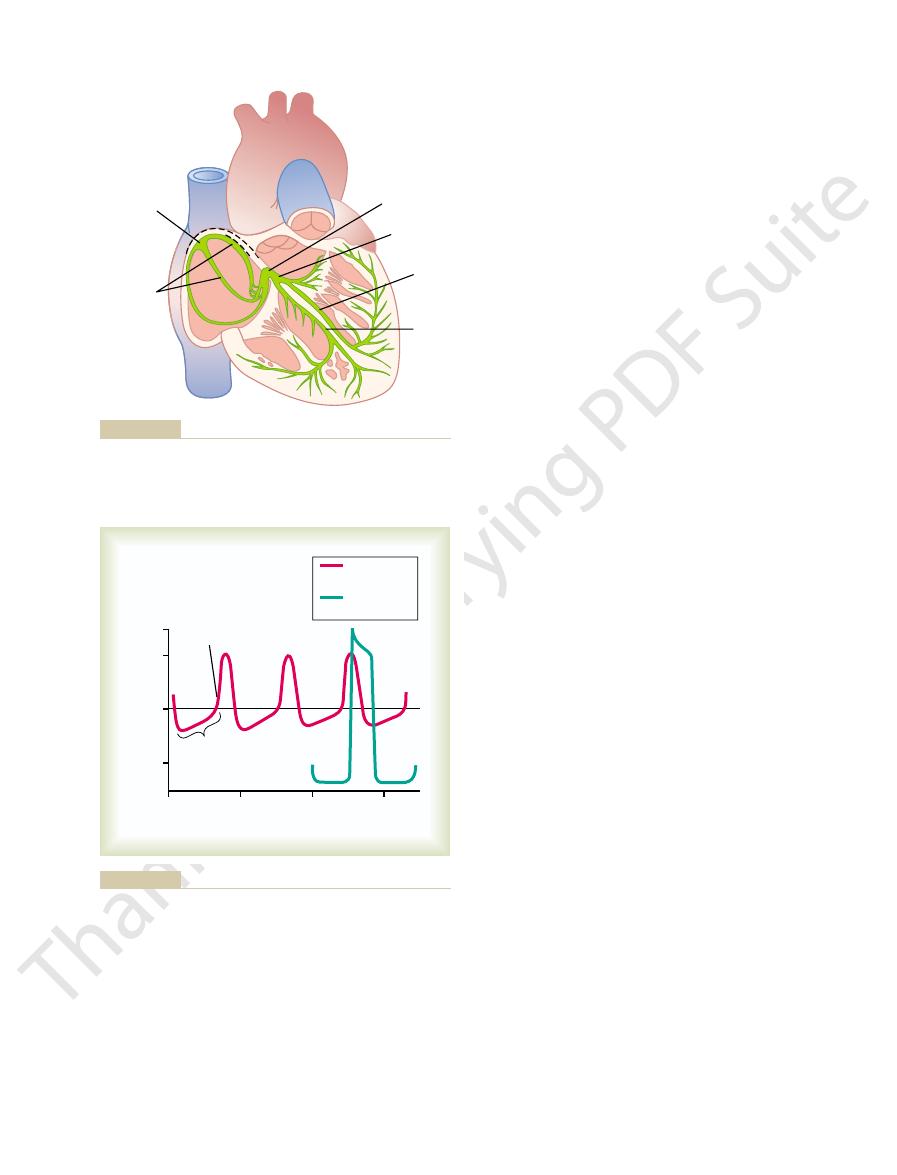
Internodal
A-V node
A-V bundle
Right
bundle
branch
Left
bundle
branch
Sinus
node
pathways
the A-V node, atrial internodal pathways, and ventricular bundle
Sinus node, and the Purkinje system of the heart, showing also
Figure 10–1
branches.
+20
0
1
2
3
Sinus
nodal fiber
Ventricular
muscle fiber
Threshold for
discharge
“Resting
potential”
Millivolts
Seconds
0
– 40
– 80
action potential is compared with that of a ventricular muscle fiber.
sinus nodal fiber.
Figure 10–2
Rhythmical discharge of a
Also, the sinus nodal

. The figure
pathway fibers
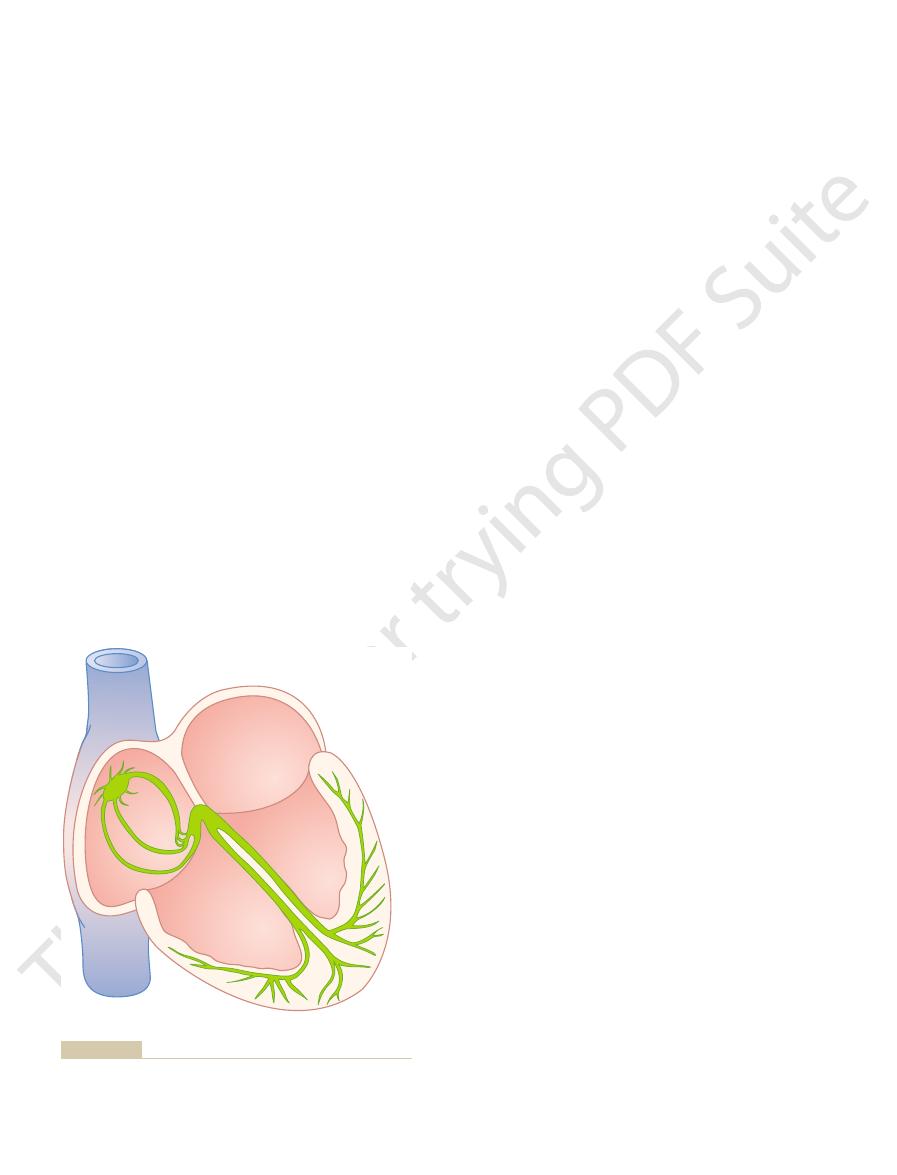
grammatically the different parts of this node, plus
as shown in Figure 10–1. And Figure 10–3 shows dia-
right atrium immediately behind the tricuspid valve,
The A-V node is located in the posterior wall of the
transmission into the ventricles.
ventricular contraction begins. It is primarily the
the ventricles too rapidly; this delay allows time for the
The atrial conductive system is organized so that the
to the Ventricles
of Impulse Conduction from the Atria
tricles, which will be discussed.
more rapidly conducting “Purkinje fibers” of the ven-
ized conduction fibers. These fibers are similar to even
The cause of more rapid velocity of
nodal pathways.
anterior, middle,
respectively, the
node; shown in Figures 10–1 and 10–3, these are called,
and posterior atrial walls and terminate in the A-V
other small bands curve through the anterior, lateral,
walls of the atria to the left atrium. In addition, three
small bands of atrial fibers. One of these, called the
conduction is more rapid, about 1 m/sec, in several
duction in most atrial muscle is about 0.3 m/sec, but
and, eventually, to the A-V node. The velocity of con-
into these atrial muscle fibers. In this way, the action
surrounding atrial muscle fibers. Therefore, action
The ends of the sinus nodal fibers connect directly with
Through the Atria
Transmission of the Cardiac Impulse
person’s life.
cycle. This process continues indefinitely throughout a
to threshold, and finally re-excitation to elicit another
action potential is over, drift of the “resting” potential
from the action potential, hyperpolarization after the
self-excitation to cause the action potential, recovery
40 millivolts. Then the entire process begins again:
potential to drift upward once more, finally reaching
flux of potassium ions, and this causes the “resting”
potassium channels close. The inward-leaking sodium
action potential is over, progressively more and more
polarization is not maintained forever. The reason is
Last, we must explain why this new state of hyper-
ization state initially carries the “resting” membrane
The hyperpolar-
fiber; this is called
of the cell, with resultant
remain open for another few tenths of a second, tem-
action potential. Furthermore, the potassium channels
of the fiber. Both of these
ions through the sodium-calcium channels ceases,
open. Therefore, influx of positive calcium and sodium
time, greatly increased numbers of potassium channels
liseconds after opening, and second, at about the same
tivated (i.e., they close) within about 100 to 150 mil-
this. First, the sodium-calcium channels become inac-
all the time? The answer is that two events occur
Why does this leakiness to sodium and calcium ions
Therefore, basically, the inherent leakiness of the sinus
become “activated,” thus causing the action potential.
40 millivolts, the sodium-calcium channels
118
Unit III
The Heart
about
-
nodal fibers to sodium and calcium ions causes their
self-excitation.
not cause the sinus nodal fibers to remain depolarized
during the course of the action potential to prevent
while at the same time large quantities of positive
potassium ions diffuse out
effects reduce the intracellular potential back to its
negative resting level and therefore terminate the
porarily continuing movement of positive charges out
excess negativity inside the
hyperpolarization.
potential down to about
-55 to -60 millivolts at the
termination of the action potential.
that during the next few tenths of a second after the
and calcium ions once again overbalance the outward
the threshold level for discharge at a potential of about
-
Internodal Pathways and
potentials originating in the sinus node travel outward
potential spreads through the entire atrial muscle mass
anterior interatrial band, passes through the anterior
and posterior inter-
conduction in these bands is the presence of special-
Atrioventricular Node, and Delay
cardiac impulse does not travel from the atria into
atria to empty their blood into the ventricles before
A-V
node and its adjacent conductive fibers that delay this
its connections with the entering atrial internodal
and the exiting A-V bundle
also shows the approximate intervals of time in
Internodal
Atrioventricular
fibrous tissue
Transitional fibers
A-V node
(0.12)
(0.03)
pathways
Ventricular
septum
(0.16)
Penetrating portion
of A-V bundle
Distal portion of
A-V bundle
Left bundle branch
Right bundle branch
of time from the origin of the impulse in the sinus node. The values
Organization of the A-V node. The numbers represent the interval
Figure 10–3
have been extrapolated to human beings.
0.03 second, approximately equal to the time required
the directions of the spirals. Because of this, transmis-
layers; therefore, the cardiac impulse does not neces-
double spiral, with fibrous septa between the spiraling
The cardiac muscle wraps around the heart in a
that in the Purkinje fibers.
velocity of transmission is now only 0.3 to 0.5 m/sec,
mass by the ventricular muscle fibers themselves. The
fibers, it is transmitted through the ventricular muscle
in the Ventricular Muscle
Transmission of the Cardiac Impulse
entire ventricular muscle mass.
ductive system, it spreads almost immediately to the
time averages only 0.03 second. Therefore, once the
terminations of the Purkinje fibers, the total elapsed
From the time the cardiac impulse enters the bundle
become continuous with the cardiac muscle fibers.
heart. The ends of the Purkinje fibers penetrate about
These branches in turn course sidewise around each
tricle, progressively dividing into smaller branches.
respective sides of the ventricular septum. Each
branches
10–3. Then the bundle divides into
the apex of the heart, as shown in Figures 10–1 and
distal portion of the A-V bundle passes downward in
tissue between the atrial and ventricular muscle, the
Distribution of the Purkinje Fibers in the Ventricles—The Left
at the A-V bundle. Under such conditions, the cardiac
itself. (In rare instances, an abnormal muscle bridge
besides forward conduction through the A-V bundle
10–3. This barrier normally acts as an insulator to
fibrous barrier, a portion of which is shown in Figure
except at the A-V bundle, the atrial muscle is sepa-
Furthermore, it should be recalled that everywhere,
tion from the atria to the ventricles.
ventricles to the atria, allowing only forward conduc-
. This prevents
ward from the ventricles to the atria
of action potentials to travel back-
in abnormal states,
inability,
characteristic of the A-V bundle is the
One-Way Conduction Through the A-V Bundle.
myofibrils, which means that they contract little or not
of transmission. The Purkinje fibers also have very few
from one cell to the next, thus enhancing the velocity
Purkinje fibers. Therefore, ions are transmitted easily
The rapid transmission of action potentials by Purk-
entire remainder of the ventricular muscle.
A-V nodal fibers. This allows almost instantaneous
4.0 m/sec, a velocity about 6 times that in the usual
larger than the normal ventricular muscle fibers, and
A-V nodal fibers. They are very large fibers, even
the A-V fibrous barrier, they have functional charac-
through the A-V bundle into the ventricles. Except for
lead from the A-V node
Rapid Transmission in the Ventricular
Therefore, it is easy to see why each succeeding cell is
ways, so that there is great resistance to conduction of
transitional, nodal, and penetrating A-V bundle fibers
The slow conduction in the
contracting muscle of the ventricles.
sinus node to the A-V node, makes a total delay of 0.16
bundle system is about 0.13 second. This, in addition to
Thus, the total delay in the A-V nodal and A-V
the atria from the ventricles.
ing A-V bundle, which is composed of multiple small
where it passes into the ventricles.A final delay
bundle,
penetrating portion of the A-V
another 0.09 second in the A-V node itself before the
origin in the sinus node. Then there is a delay of
ways, reaches the A-V node about 0.03 second after its
impulse, after traveling through the internodal path-
appearance in the A-V nodal system. Note that the
Chapter 10
Rhythmical Excitation of the Heart
119
fractions of a second between initial onset of the
cardiac impulse in the sinus node and its subsequent
impulse enters the
of another 0.04 second occurs mainly in this penetrat-
fascicles passing through the fibrous tissue separating
the initial conduction delay of 0.03 second from the
second before the excitatory signal finally reaches the
Cause of the Slow Conduction.
is caused mainly by diminished numbers of gap junc-
tions between successive cells in the conducting path-
excitatory ions from one conducting fiber to the next.
slow to be excited.
Purkinje System
Special Purkinje fibers
the initial portion of these fibers where they penetrate
teristics that are quite the opposite of those of the
they transmit action potentials at a velocity of 1.5 to
ventricular muscle and 150 times that in some of the
transmission of the cardiac impulse throughout the
inje fibers is believed to be caused by a very high level
of permeability of the gap junctions at the intercalated
discs between the successive cells that make up the
at all during the course of impulse transmission.
A special
except
re-entry of cardiac impulses by this route from the
rated from the ventricular muscle by a continuous
prevent passage of the cardiac impulse between atrial
and ventricular muscle through any other route
does penetrate the fibrous barrier elsewhere besides
impulse can re-enter the atria from the ventricles and
cause a serious cardiac arrhythmia.)
and Right Bundle Branches.
After penetrating the fibrous
the ventricular septum for 5 to 15 millimeters toward
left and right bundle
that lie beneath the endocardium on the two
branch spreads downward toward the apex of the ven-
ventricular chamber and back toward the base of the
one third the way into the muscle mass and finally
branches in the ventricular septum until it reaches the
cardiac impulse enters the ventricular Purkinje con-
Once the impulse reaches the ends of the Purkinje
one sixth
sarily travel directly outward toward the surface of the
heart but instead angulates toward the surface along
sion from the endocardial surface to the epicardial
surface of the ventricle requires as much as another
for transmission through the entire ventricular portion
maker then occurs most frequently at the A-V node or
node to the other parts of the heart. The new pace-
debility of heart pumping.
“ectopic” pacemaker.
ops excessive excitability and becomes the pacemaker.
tions, a place in the atrial or ventricular muscle devel-
or to the excited Purkinje fibers. Under rarer condi-
the heart shifts from the sinus node to the A-V node
becomes abnormal. In either case, the pacemaker of
node. For instance, this sometimes occurs in the A-V
Abnormal Pacemakers—“Ectopic” Pacemaker.
that of any other part of the heart. Therefore, the sinus
Thus, the sinus node controls the beat of the heart
either of these.
from the sinus node discharges both the A-V node and
olds for self-excitation. Therefore, the new impulse
the sinus node discharges again before either the A-V
fibers, also discharging their excitable membranes. But
is conducted into both the A-V node and the Purkinje
fibers. Each time the sinus node discharges, its impulse
discharge rate of either the A-V node or the Purkinje
control the heart’s rhythmicity? The answer derives
node rather than the A-V node or the Purkinje fibers
The question we must ask is: Why does the sinus
per minute.
15 and 40 times per minute. These rates are in contrast
mical rate of 40 to 60 times per minute, and the Purk-
some outside source, discharge at an intrinsic rhyth-
The A-V nodal fibers, when not stimulated from
nodal and Purkinje fibers.
nodal fibers do; this is particularly true of the A-V
node. In some abnormal conditions, this is not the case.
sion of the cardiac impulse through the heart, we have
Conduction in the Heart
Control of Excitation and
understanding of electrocardiography, to be discussed
separate part of the heart, because a thorough quanti-
ventricular muscle to the epicardial surfaces.
endocardial surfaces of the ventricles. Then the impulse
A-V bundle. Once it has entered this bundle, it spreads
atria but is delayed more than 0.1 second in the A-V
ance at each respective point in the heart. Note that
in fractions of a second, that lapse between the origin
numbers on the figure represent the intervals of time,
of the cardiac impulse through the human heart. The
Figure 10–4 shows in summary form the transmission
of the Purkinje system. Thus, the total time for trans-
120
Unit III
The Heart
mission of the cardiac impulse from the initial bundle
branches to the last of the ventricular muscle fibers in
the normal heart is about 0.06 second.
Summary of the Spread of the Cardiac
Impulse Through the Heart
of the cardiac impulse in the sinus node and its appear-
the impulse spreads at moderate velocity through the
nodal region before appearing in the ventricular septal
very rapidly through the Purkinje fibers to the entire
once again spreads slightly less rapidly through the
It is extremely important that the student learn in
detail the course of the cardiac impulse through the
heart and the precise times of its appearance in each
tative knowledge of this process is essential to the
in Chapters 11 through 13.
The Sinus Node as the Pacemaker
of the Heart
In the discussion thus far of the genesis and transmis-
noted that the impulse normally arises in the sinus
A few other parts of the heart can exhibit intrinsic
rhythmical excitation in the same way that the sinus
inje fibers discharge at a rate somewhere between
to the normal rate of the sinus node of 70 to 80 times
from the fact that the discharge rate of the sinus node
is considerably faster than the natural self-excitatory
node or the Purkinje fibers can reach their own thresh-
the Purkinje fibers before self-excitation can occur in
because its rate of rhythmical discharge is faster than
node is virtually always the pacemaker of the normal
heart.
Occasionally
some other part of the heart develops a rhythmical dis-
charge rate that is more rapid than that of the sinus
node or in the Purkinje fibers when one of these
A pacemaker elsewhere than the sinus node is
called an
An ectopic pacemaker
causes an abnormal sequence of contraction of the
different parts of the heart and can cause significant
Another cause of shift of the pacemaker is blockage
of transmission of the cardiac impulse from the sinus
.04
.03
.07
.07
.07
.05
.03
.00
A-V
S-A
.09
.06
.16
.19
.19
.22
.21
.21
.20
.18
.18
.17
.17
appearance at the sinoatrial node) in different parts of the heart.
Transmission of the cardiac impulse through the heart, showing
Figure 10–4
the time of appearance (in fractions of a second after initial
sinus nodal discharge. Second, it increases the rate
stimulation, as follows: First, it increases the rate of
conduction entirely.
duction of the impulse, but a large decrease blocks
decreases. A moderate decrease simply delays con-
the transitional fibers into the A-V nodal fibers
tricity to excite the nodal fibers. Therefore, the
In the A-V node, a state of hyperpolarization caused
mical self-excitation of this node.
strong enough, it is possible to stop entirely the rhyth-
ity of these nodal fibers. If the vagal stimulation is
for excitation. This greatly slows the rate of rhythmic-
60 millivolts. Therefore,
tive than usual, to
decreases the “resting” membrane potential of the
In the sinus node, the state of hyperpolarization
as explained in Chapter 5.
which makes this excitable tissue much less excitable,
inside the fibers, an effect called
the conductive fibers. This causes increased negativity
ions, which allows rapid leakage of potassium out of
released at the vagal nerve endings greatly increases
The acetylcholine
Mechanism of the Vagal Effects.
ventricular escape.
15 to 40 beats per minute. This phenomenon is called
portion of the A-V bundle, develops a rhythm of its
Purkinje fibers, usually in the ventricular septal
beating for 5 to 20 seconds, but then some point in the
transmitted into the ventricles. The ventricles stop
either case, rhythmical excitatory signals are no longer
the atria into the ventricles through the A-V mode. In
of heart pumping, often to as little as one half normal.
Weak to moderate vagal stimulation slows the rate
ventricles.
the atrial musculature and the A-V node, thereby
the excitability of the A-V junctional fibers between
of rhythm of the sinus node, and second, it decreases
major effects on the heart. First, it decreases the rate
released at the vagal endings. This hormone has two
acetylcholine
Cardiac Rhythm and Conduction—“Ventricular Escape.”
Parasympathetic (Vagal) Stimulation Can Slow or Even Block
lar muscle as well as to all the other areas.
the heart, with strong representation to the ventricu-
thetic nerves, conversely, are distributed to all parts of
little directly to the ventricular muscle. The sympa-
lesser extent to the muscle of the two atria, and very
distributed mainly to the S-A and A-V nodes, to a
Chapter 9. The parasympathetic nerves (the vagi) are
parasympathetic nerves, as shown in Figure 9-10 of
The heart is supplied with both sympathetic and
Impulse Conduction by the Cardiac
Control of Heart Rhythmicity and
mission does occur, and the pumping effectiveness of
which are discussed in Chapters 12 and 13, slow trans-
Indeed, in some types of cardiac debilities, several of
before contraction of the remainder, in which case the
slowly, much of the ventricular mass would contract
requires this synchronous type of contraction. If the
muscle fiber. This causes all portions of the ventricular
portions of the ventricles within a narrow span of time,
of the Ventricular Muscle
the delay period is too long, it can lead to death.
Stokes-Adams syndrome.
of lack of blood flow to the brain. This delayed pickup
5 to 20 seconds, the ventricles fail to pump blood, and
consequently, are in a suppressed state. During these
been “overdriven” by the rapid sinus impulses and,
because, before the blockage, the Purkinje fibers had
block, the Purkinje system does not begin to emit its
15 and 40 beats per minute. After sudden A-V bundle
sinus node, while a new pacemaker usually develops
through the A-V nodal and bundle system—the atria
When A-V block occurs—that is, when the cardiac
way to the ventricles.
in the penetrating portion of the A-V bundle on the
Chapter 10
Rhythmical Excitation of the Heart
121
impulse fails to pass from the atria into the ventricles
continue to beat at the normal rate of rhythm of the
in the Purkinje system of the ventricles and drives the
ventricular muscle at a new rate somewhere between
intrinsic rhythmical impulses until 5 to 20 seconds later
the person faints after the first 4 to 5 seconds because
of the heartbeat is called
If
Role of the Purkinje System
in Causing Synchronous Contraction
It is clear from our description of the Purkinje system
that normally the cardiac impulse arrives at almost all
exciting the first ventricular muscle fiber only 0.03 to
0.06 second ahead of excitation of the last ventricular
muscle in both ventricles to begin contracting at
almost the same time and then to continue contract-
ing for about another 0.3 second.
Effective pumping by the two ventricular chambers
cardiac impulse should travel through the ventricles
overall pumping effect would be greatly depressed.
the ventricles is decreased as much as 20 to 30 per cent.
Nerves: The Sympathetic and
Parasympathetic Nerves
Stimulation of the parasympathetic nerves to the heart
(the vagi) causes the hormone
to be
slowing transmission of the cardiac impulse into the
And strong stimulation of the vagi can stop completely
the rhythmical excitation by the sinus node or block
completely transmission of the cardiac impulse from
own and causes ventricular contraction at a rate of
the permeability of the fiber membranes to potassium
hyperpolarization,
sinus nodal fibers to a level considerably more nega-
-65 to -75 millivolts rather than
the normal level of
-55 to -
the initial rise of the sinus nodal membrane potential
caused by inward sodium and calcium leakage
requires much longer to reach the threshold potential
by vagal stimulation makes it difficult for the small
atrial fibers entering the node to generate enough elec-
safety
factor for transmission of the cardiac impulse through
Effect of Sympathetic Stimulation on Cardiac Rhythm and Con-
duction.
Sympathetic stimulation causes essentially the
opposite effects on the heart to those caused by vagal
of conduction as well as the level of excitability in all
125:683, 2004.
Yasuma F, Hayano J: Respiratory sinus arrhythmia: why does
Electrophysiol 14(12 Suppl):S267, 2003.
Waldo AL: Mechanisms of atrial fibrillation. J Cardiovasc
Arrhythmias. Baltimore: Williams & Wilkins, 1995.
Surawicz B: Electrophysiologic Basis of ECG and Cardiac
90:939, 2002.
regional specialization in electrical function. Circ Res
Schram G, Pourrier M, Melnyk P, Nattel S: Differential dis-
Cardiac ion channels. Annu Rev Physiol 64:431, 2002.
Roden DM, Balser JR, George AL Jr, Anderson ME:
plexity beyond monogenic disorders. Circ Res 94:140,
Priori SG: Inherited arrhythmogenic diseases: the com-
34:885, 2002.
nomic nervous system regulation. J Mol Cell Cardiol
cycling, historic overview and perspectives: role for auto-
Petrashevskaya NN, Koch SE, Bodi I, Schwartz A: Calcium
York: Oxford University Press, 2002.
sec 2: The Cardiovascular System, vol 1: The Heart. New
Page E, Fozzard HA, Solaro JR: Handbook of Physiology,
for atrioventricular conduction. Circulation 103:2660,
Mazgalev TN,
Ho SY,
Anderson RH:
Anatomic-
state of the art. Circulation 109:296, 2004.
Leclercq C, Hare JM: Ventricular resynchronization: current
84:431, 2004.
propagation and associated arrhythmias. Physiol Rev
Kléber AG, Rudy Y: Basic mechanisms of cardiac impulse
channels. Annu Rev Physiol 63:235, 2001.
Kaupp UB, Seifert R: Molecular diversity of pacemaker ion
Prog Cardiovasc Dis 45:327, 2003.
and His bundle of the human heart: part II—function.
James TN: Structure and function of the sinus node, AV node
Cardiovasc Dis 45:235, 2002.
and His bundle of the human heart: part I—structure. Prog
James TN: Structure and function of the sinus node, AV node
heart. Physiol Rev 80:31, 2000.
Hume JR, Duan D, Collier ML, et al: Anion transport in
to cardiac arrhythmias. N Engl J Med 345:1473, 2001.
Huikuri HV, Castellanos A, Myerburg RJ: Sudden death due
review. Chest 125:297, 2004.
incompetence in a young adult: case report and literature
Gentlesk PJ, Markwood TT, Atwood JE: Chronotropic
traction.Am J Physiol Heart Circ Physiol 280:H1928, 2001.
pling: role of membrane potential in regulation of con-
Ferrier GR, Howlett SE: Cardiac excitation-contraction cou-
and alternans in atrial myocytes. J Physiol 546:19, 2003.
Blatter LA, Kockskamper J, Sheehan KA, et al: Local
the myofibrils.
of sympathetic stimulation, because calcium ions play
The increase in permeability to calcium ions is at
conduction time from the atria to the ventricles.
the conducting fiber bundles, thereby decreasing the
In the A-V node and A-V bundles, increased
therefore, increasing the heart rate.
excitation, thus accelerating self-excitation and,
brane to sodium and calcium ions. In the sinus node,
muscle fibers is somewhat unclear, but the belief is
at the sympathetic nerve endings. The precise
Mechanism of the Sympathetic Effect.
can almost triple the frequency of heartbeat and can
overall activity of the heart. Maximal stimulation
In short, sympathetic stimulation increases the
both atrial and ventricular, as discussed in Chapter 9.
force of contraction of all the cardiac musculature,
portions of the heart. Third, it increases greatly the
122
Unit III
The Heart
increase the strength of heart contraction as much as
twofold.
Stimulation of
the sympathetic nerves releases the hormone norepi-
nephrine
mechanism by which this hormone acts on cardiac
that it increases the permeability of the fiber mem-
an increase of sodium-calcium permeability causes
a more positive resting potential and also causes
increased rate of upward drift of the diastolic mem-
brane potential toward the threshold level for self-
sodium-calcium permeability makes it easier for the
action potential to excite each succeeding portion of
least partially responsible for the increase in contrac-
tile strength of the cardiac muscle under the influence
a powerful role in exciting the contractile process of
References
calcium gradients during excitation-contraction coupling
electrophysiological correlations concerning the pathways
2001.
2004.
tribution of cardiac ion channel expression as a basis for
the heartbeat synchronize with respiratory rhythm? Chest
