2
Lec. 1+2+3 General Digestion
Digestion & Absorption
• Overview of the GIT functions
• Dig. & abs. Of carbohydrate.
• Dig. & abs. Of protein
• Dig. & abs. Of lipid
• GIT diseases
• Abnormal digestion and absorption.
Objectives
• Describe the processes of digestion and absorption.
• Name the organs in the digestive system and describe their functions.
• Name the enzymes or juices secreted by each organ and gland in the digestive system.
• Discussing factors controlling digestion and absorption.
• Discussing disordered digestion and absorption.
For good health and growth
We should have
1) Good and complete sources of food.
2) Good gastrointestinal tract.
3) We should not eat more or less than required.
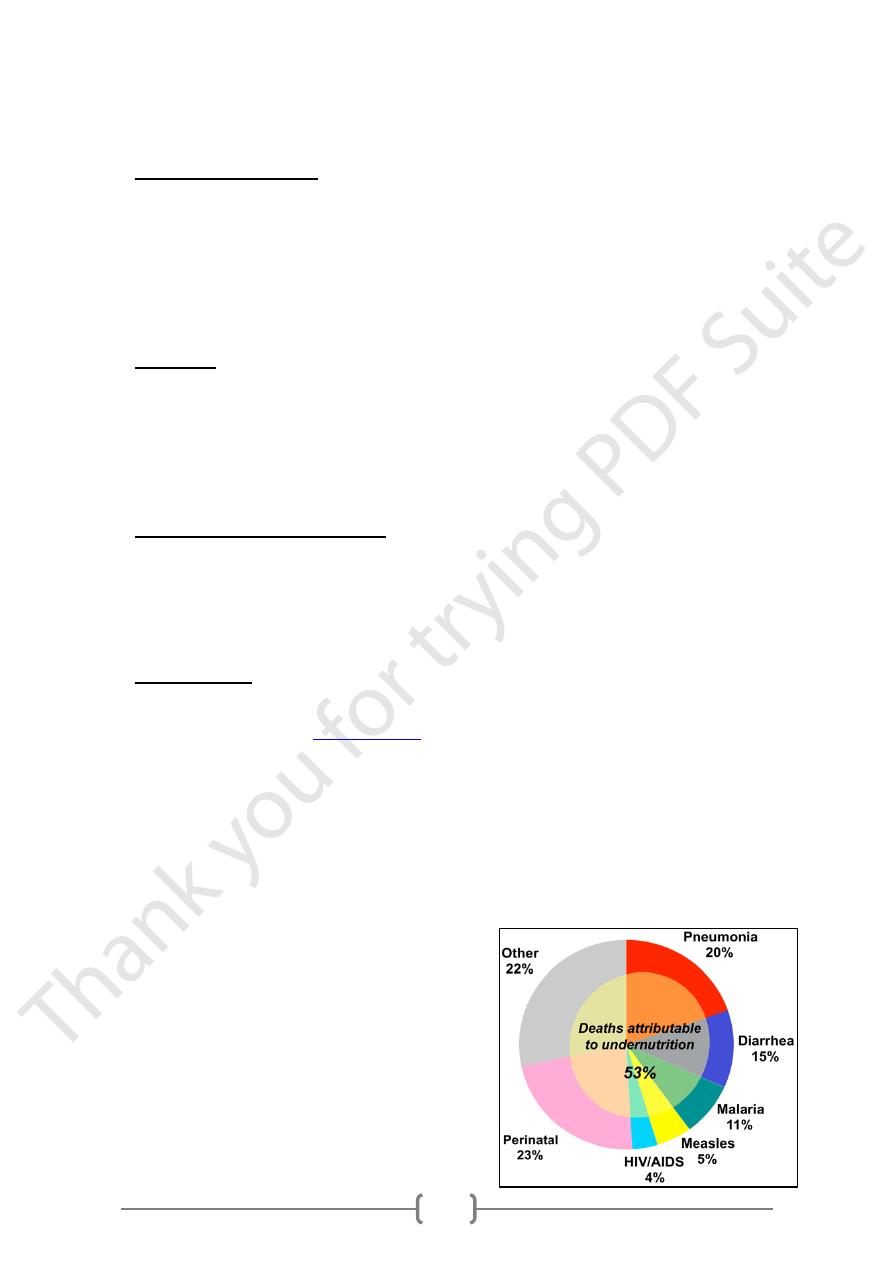
Malnutrition
• Starvation (body digest itself) and OBESITY
• Anorexia nervosa is an
eating disorder
Characterized by food restriction and fear of gaining weight. It typically involves
excessive weight loss.
Anorexia nervosa usually develops during adolescence and early adulthood , due to
the fear of gaining weight, people with this disorder restrict the amount of food they
consume. This restriction of food intake causes metabolic and hormonal disorders.
• Marasmus: protein & carbohydrates malnutrition
• Kwashiorkor: protein malnutrition characterized by protruded abdomen &
edematous face.
• Rickets: vitamin D deficiency.
• Anemia: reduced RBC number.
• Athlete: overweight but not obese.
3
(BMI)
ndex
I
ass
M
ody
B
• The weight of the person in kilograms divided by the square of the height in meters
• Used as an indicator of whether or not person is over or under weight
• Example: a person with 1.7 m height and 65 kg wt. has a BMI of 65/2.89 =22.5
• Values of (BMI)
o Underweight === less than 20
o Normal WEIGHT === Between 20 -24.9
o Overweight === Between 25-30
o Obesity === over 30
Digestion
• The breakdown of food in the GIT in the preparation for absorption.
• Mechanical digestion: food is broken up by teeth and moved along GI tract by
peristalsis.
• Chemical digestion: carbohydrates, proteins, and fats are broken down into nutrients
tissues can absorb and use.
• Chemical changes occur through hydrolysis (the addition of water and breaking down
of food molecules).
• Enzymes act on food substances, causing them to break down into simple compounds.
• An enzyme can act as a catalyst, which speeds up the chemical reactions without itself
being changed in the process.
Absorption
• The passage of nutrients into the blood or lymphatic system.
• Nutrients must be in their simplest form
Carbohydrates: simple sugars
Proteins: amino acids
Fats: fatty acids and glycerol
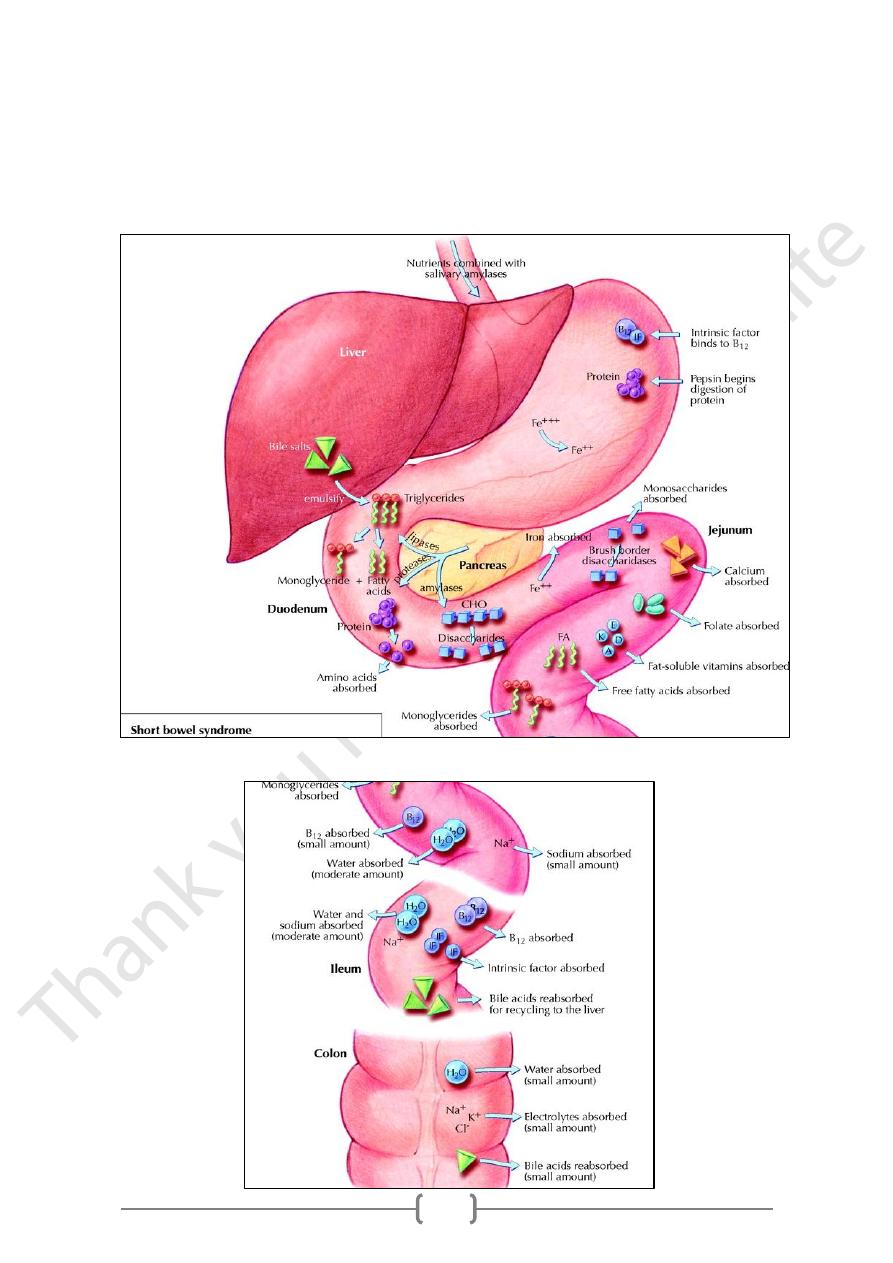
• Most absorption occurs in: The small intestine, Some occurs in the stomach and large
intestine.
• Water: is absorbed in the stomach, small intestine, and large intestine.
4
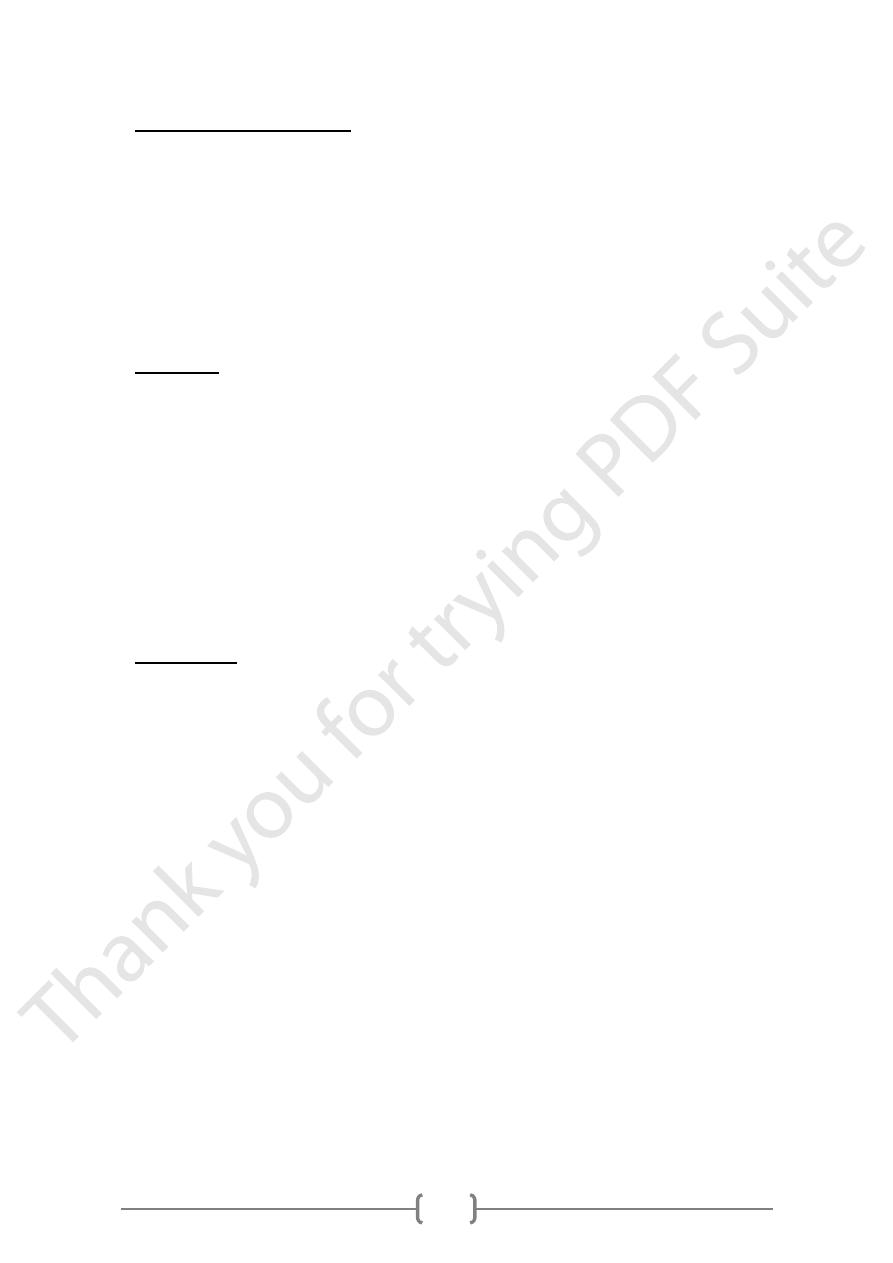
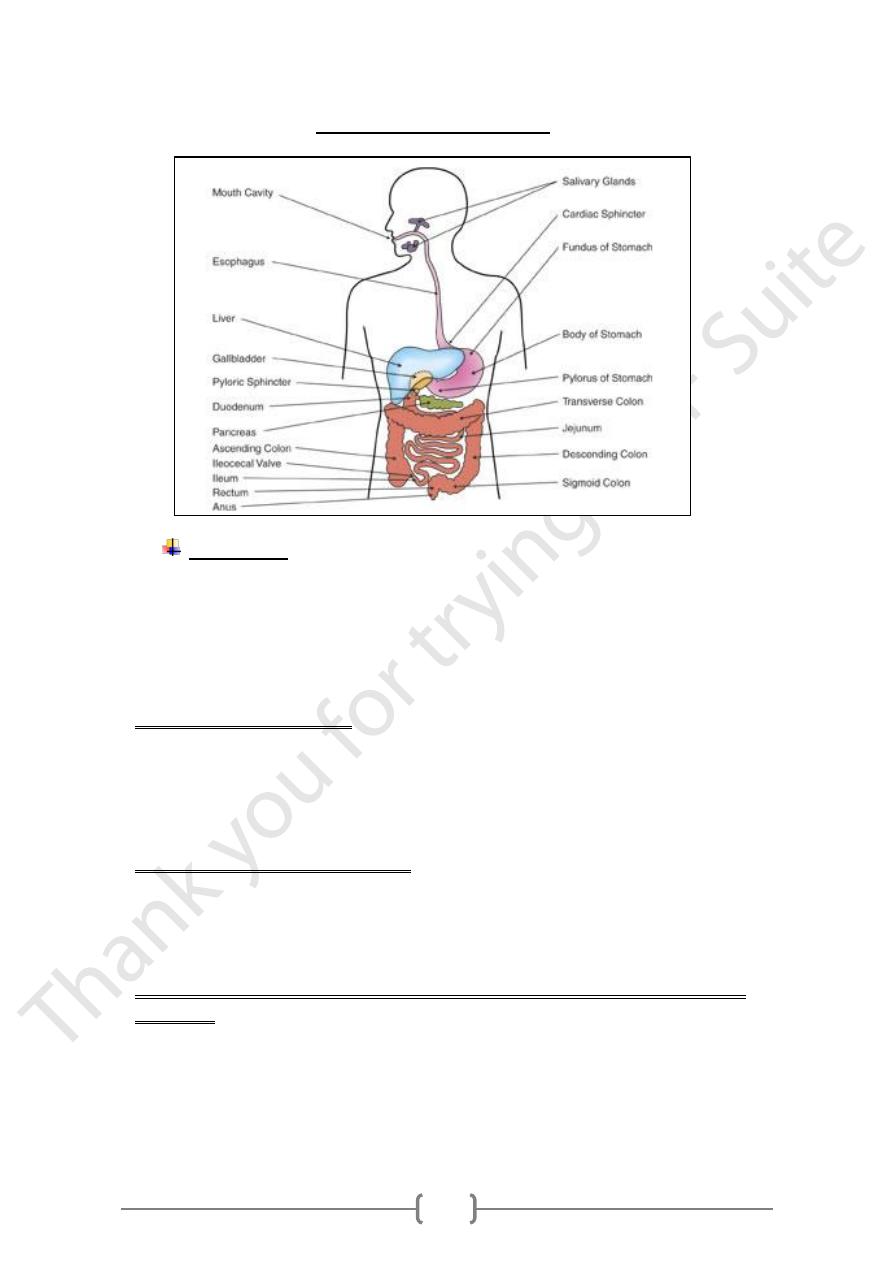
The Digestive System
The mouth
• Digestion begins here
• Enzyme (salivary amylase) acts on starch which is a complex carbohydrate.
• Teeth break up food; food mixes with saliva and “Bolus” formed
• Length of time food in mouth is brief
• Small amounts of carbohydrates changed
Salivary glands and saliva
• Saliva: is secreted mainly by three pairs of glands: Parotid and submaxillary and
sublingual.
• Parotid saliva: is non-viscous (serous). (more water)
• Saliva from the other glands is viscous. (more mucin)
:
Flow of saliva is stimulated by
Stimulation of salivary secretion:
1) Mechanical factors: presence of food in the mouth.
2) Conditional reflexes: sight or smell.
3) No hormonal stimulation is required for salivary secretions.
The composition but not the secretion of saliva is controlled by hormonal
activities:
• Adrenocorticotrophic hormone (Steroids) and Aldosteron
• Affect the contents of Electrolytes especially: Na, K, H.
• Composition of saliva, PH and volume are variable:
o usually from 1 or 2 liters of:
o hypotonic mixed secretion daily.
5
Composition of saliva
1) Mucin: is the chief organic constituent.
2) Water and electrolytes: Na, K, Ca, Cl.
3) CHO, Glucose, urea, lactate, phenol, vitamins.
4) PH= (6.4 – 7.4).
5) Enzymes: amylase, lipase, Phosphatase, and carbonic unhydrase.
The Oesophaqus
• Food travels through this muscular tube
• Connects mouth to stomach.
• Peristalsis and gravity act to move bolus.
• Cardiac sphincter opens at lower end of esophagus to allow passage of bolus into
stomach.
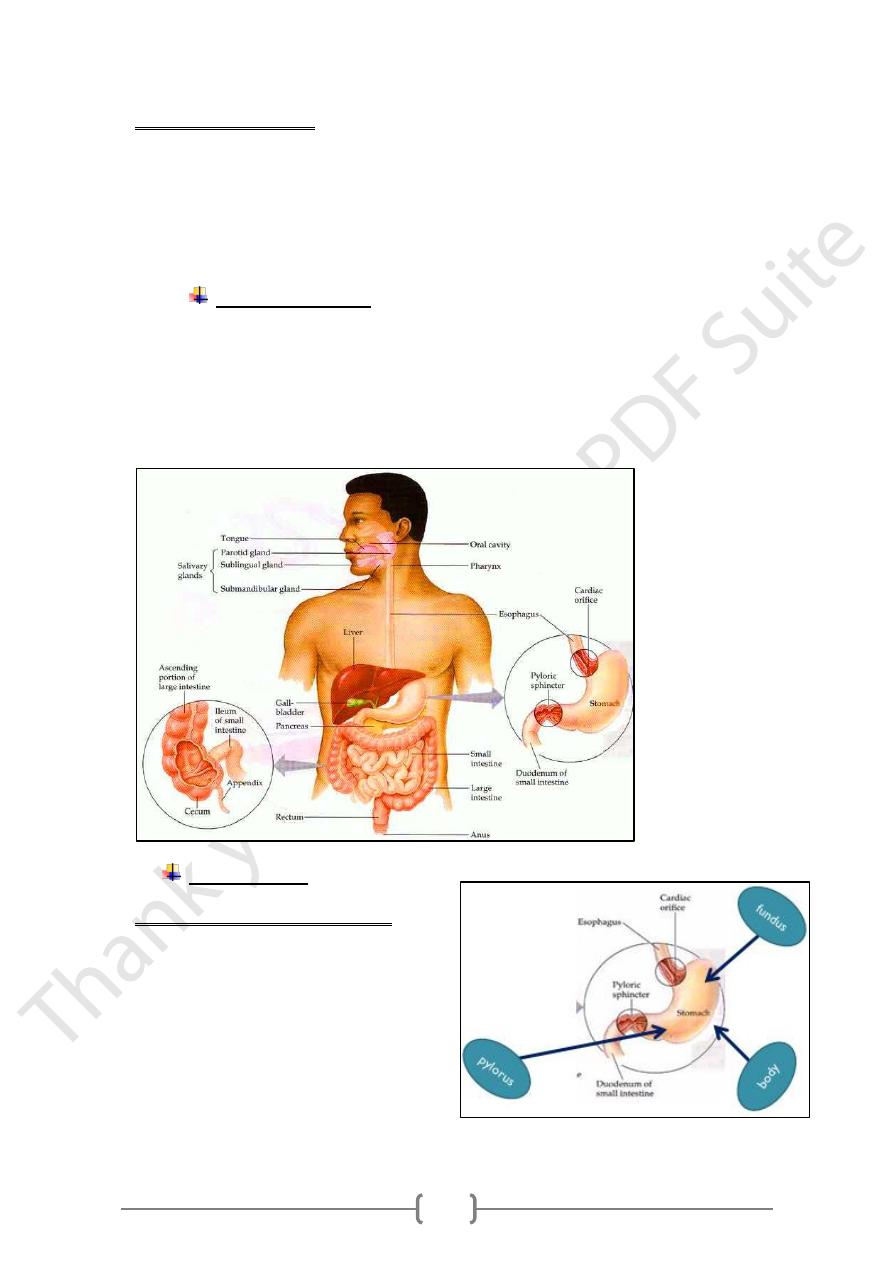
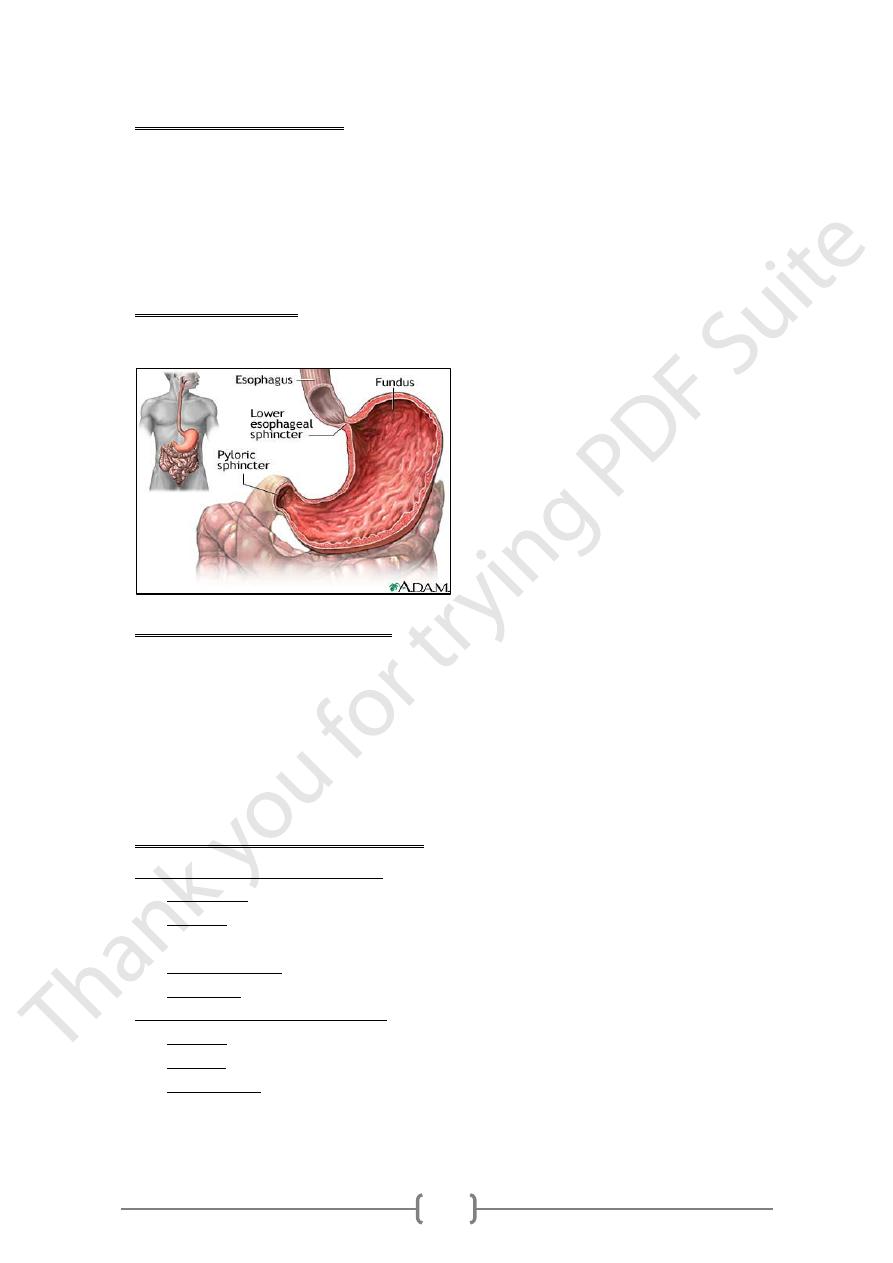
The Stomach
Anatomic Parts of the stomach
1) Fundus: upper portion of the stomach
2) Body of the stomach: middle area
3) Pylorus: end of stomach near small
intestines
6
Functions of the stomach
1) Temporary storage of food.
2) Mixing of food with gastric juices.
3) Regulation of a slow controlled emptying of food into the intestine.
4) Secretion of gastric juices.
5) Secretion of the intrinsic factor for vit.B
12.
6) Destruction of most bacteria accidentally consumed.
Stomach Secretions
Hydrochloric acid, Pepsin, Rennin, Lipase, Intrinsic factor & Mucous.
Functions of Gastric secretions
1) HCl: activates the proenzyme pepsinogen to pepsin, and performs a bactericidal
function.
2) Pepsin: begins the process of protein digestion.
3) Rennin: In children, breaks down milk proteins.
4) Intrinsic factor: helps in the absorption of vit.B12 in the ileum.
5) Mucous: acts as lubricant and protects the gastric lining.
6) Lipase: acts on emulsified fats.
Factors affecting gastric secretions
A. initiating and Regulating Factors:
1) Food stuffs: Peptides and amino acids.
2) Gastrins : a grope of hormones secreted from the pyloric mucosa by direct action
of food.
3) Nervous system: Direct stimulation of the nervous system (vagus nerve).
4) Histamine: Stimulating factor from the gastric mucosa.
B. Gastrins production is inhibited by
1) Low PH.
2) Secretin: a hormone produced by duodenal mucosa.
3) Somatostatin: a hormone produced by the hypothalamus and pancreatic cells.
7
:
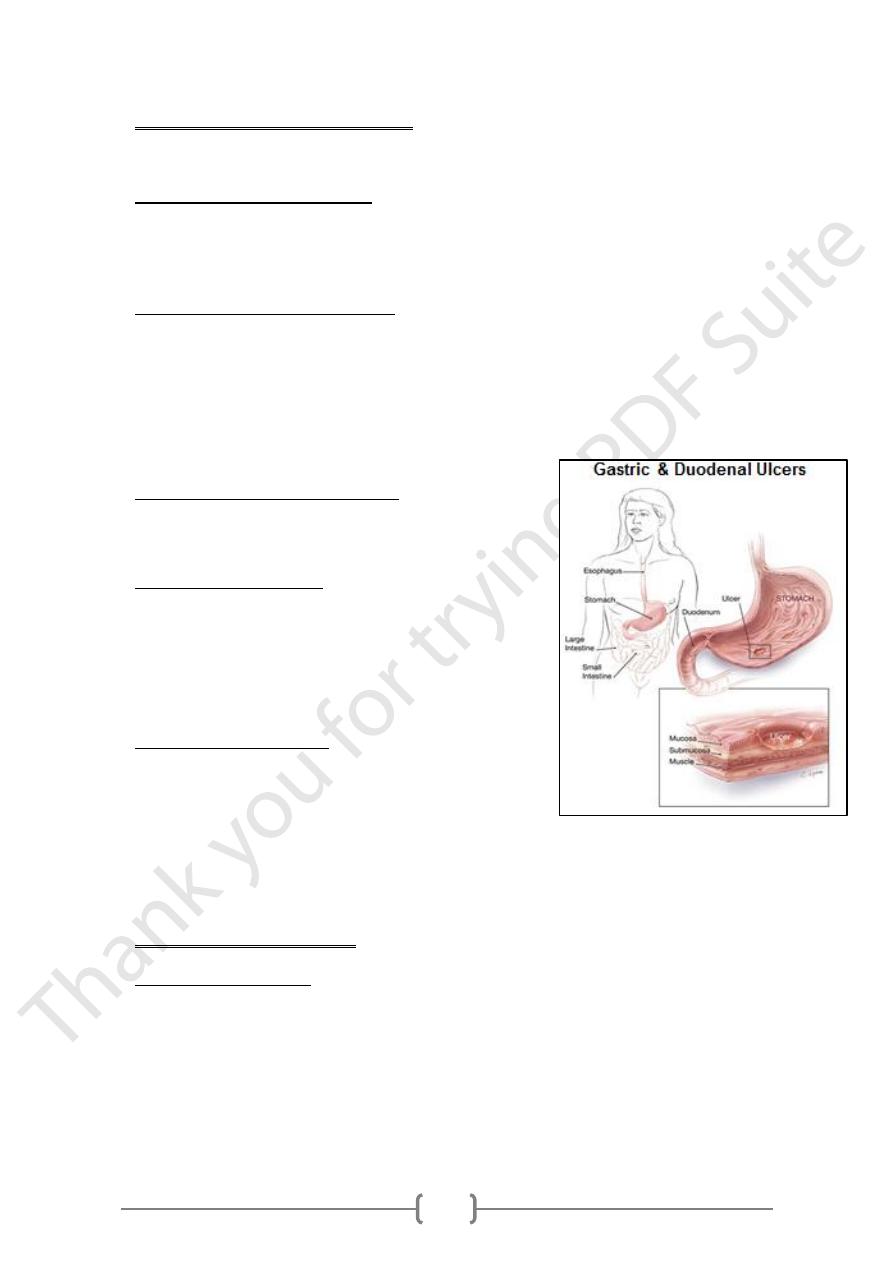
Abnormal gastric juice secretion
Hypersecretion & Hyposecretion of gastric acide
Hypersecretion of gastric acides
• Leads to Stomach and duodenal ulcers (peptic ulceration) which result from the
digestion of gastric or duodenal mucosa by the actions of pepsin and HCL.
• There are three types of peptic ulcers: Acute, chronic and recurrent.
The main cause of peptic ulcers are:
1) Increased HCl and pepsin secretions.
2) Drugs: aspirin and corticosteroids.
3) Psychological factors.
4) Genetic and familial predisposing factors.
5) Zollenger-Elson syndrome: due to excessive gastrin production.
6) Bacterial infection: helicobacter pylori.
Signs and symptoms of peptic ulcers
1) Epigastric pain, acidity, and decreased apatite.
2) Anemia and decreased body weight.
Diagnosis of peptic ulcers
1) Signs and symptoms.
2) Stool examination for blood. (occult blood).
3) Estimation of gastric secretions. (HCl and pepsin).
4) X-ray for stomach and duodenum (Barium meal).
5) Gastroscopy.
Treatment of peptic ulcers
1) Medical: is by diet and drugs that reduce the
secretions of HCl and pepsin: Milk, Antacids,
Antihistamines, Antibiotics.
2) Surgical:
Removal of the ulcered area from the stomach
Vagotomy (cutting the vagus nerve).
Hyposecretion of gastric juice
Causes of hyposecretion
1) Pernicious anemia, due to formation of antibodies to the parietal cells of gastric mucosa.
2) Carcinoma of stomach.
3) Chronic gastritis.
8
The Pancreas
Pancreatic secretion
• Pancreatic juice is secreted into the small intestine and contains:
1) Pancreatic bicarbonate neutralize acids.
2) Pancreatic proteases: (trypsin, chymotrypsin, carboxypeptidases): split proteins.
3) Pancreatic amylase: converts starches. (polysaccharides) to simple sugars.
4) Pancreatic lipase: reduces fats to fatty acids and glycerol.
• Pancreatic secretion
o An aqueous secretion: rich in bicarbonate.
o An enzyme component: rich in enzymes and proenzymes.
proteolytic, glycosidic and lipoltic enzymes.
are:
Pancreatic enzymes
Trypsinogen, Chymotrypsinogen, Protease, amylase, Lipase and Phoshpolipase.
• The daily volume of pancreatic secretion is about 500-800 ml/day
"PH" of 7.4 to 8.3 contain Na+, K+, Ca++, Cl-, HCO3- and HPO4-.
Control of Pancreatic Secretion
1) Hormonal control:
• (secretin) the Acid in the upper part of the duodenum librates a hormone called
secretin in the circulation which stimulates the flow of pancreatic juice, bile and
intestinal secretion.
• Cholecystokinin: a second duodenal hormone stimulates enzymatic secretion of
the pancreas.
2) Neural control: Vagal stimulation results in marked increase in enzyme activity. But
not enhance the volume of the pancreatic secretion.
Pancreatic disease
• Inflammation of the pancreas is called pancreatitis
• There are three types of pancreatitis: Acute, relapsing and chronic pancreatitis.
• Main causes of pancreatitis are: Gall stones and chronic alcoholism.
• Signs and symptoms: sever pain in the upper abdomen and back with shock.
• Diagnosis:
o History and examination.
o Signs and symptoms.
o Investigations: serum amylase is high.
o X-ray may show gall stones or calcified pancreas.
• Complications: malabsorption and diabetes.
• Treatment:
o No oral fluid or food.
o Bed rest.
o Removal of gall stones.
o Anticholinergic drugs.
9
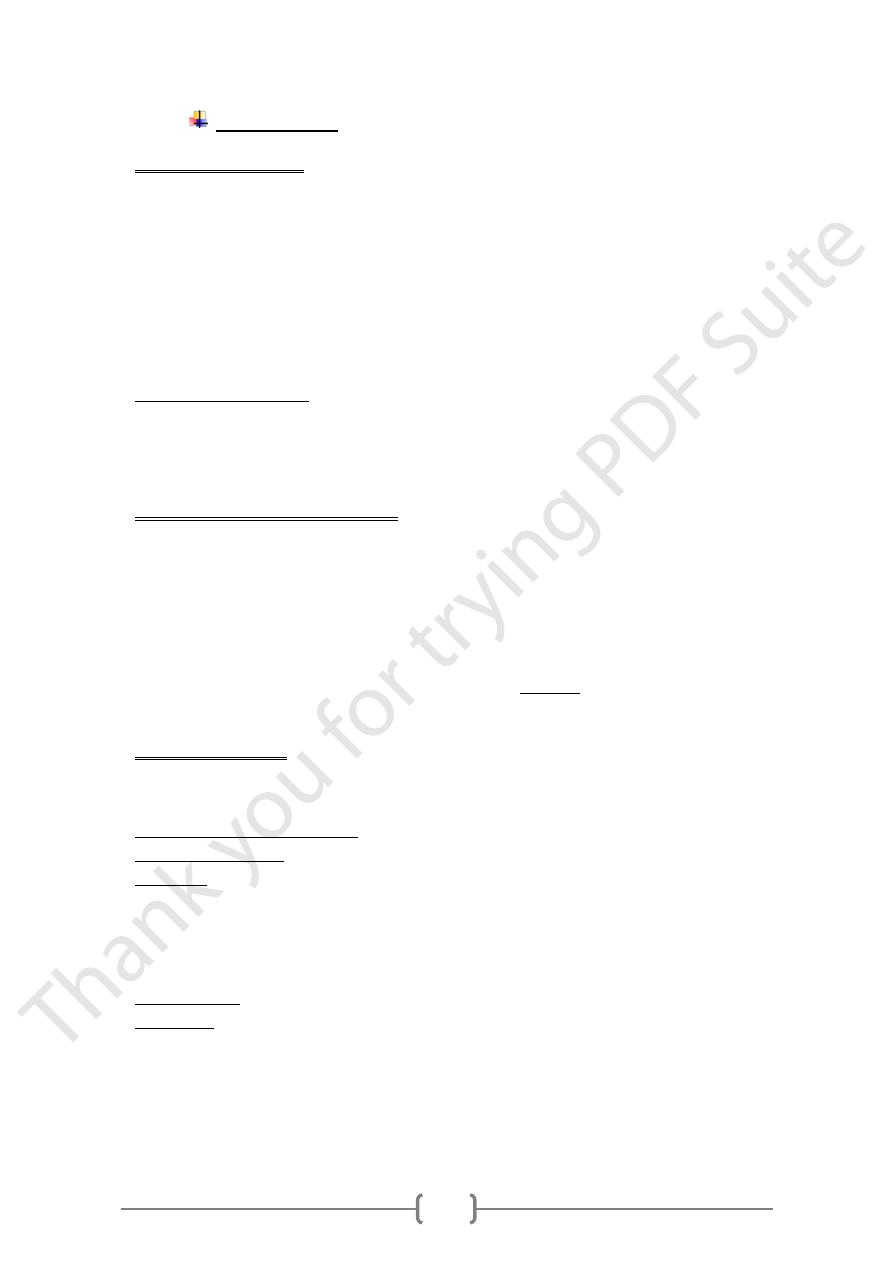
Gall bladder and Bile
• Gall bladder is a storage sac.
• Concentrate bile by absorption of water and
electrolytes
• Secretes of mucin.
• Bile contains: Cholesterol, Bile acids and Bile
pigments, and Electrolytes.
• The resulting solution of bile secretion may be
neutral or slightly acidic. The capacity of gallbladder
is so to 60 ml in adults.
Gallbladder Secretion Contains
1) Primary bile acids: cholic acid and chenic acid. They help in emulsification ,
hydrolysis and absorption of lipids.
2) Bile pigments: ( bilirubin) is derived from the metabolism of hemoglobin.
3) A number of enzymes have been found in bile of which alkaline phosphatase.
Cholecystits and gall stones
• Cholecystitis: is acute or chronic inflammation of the gall bladder.
It is caused by bacterial infection.
• Gallstones: Because of the high concentration of bile salts and there limited solubility.
Gallstones usually occur in the gallbladder and bile ducts leading to obstruction
of bile flow.
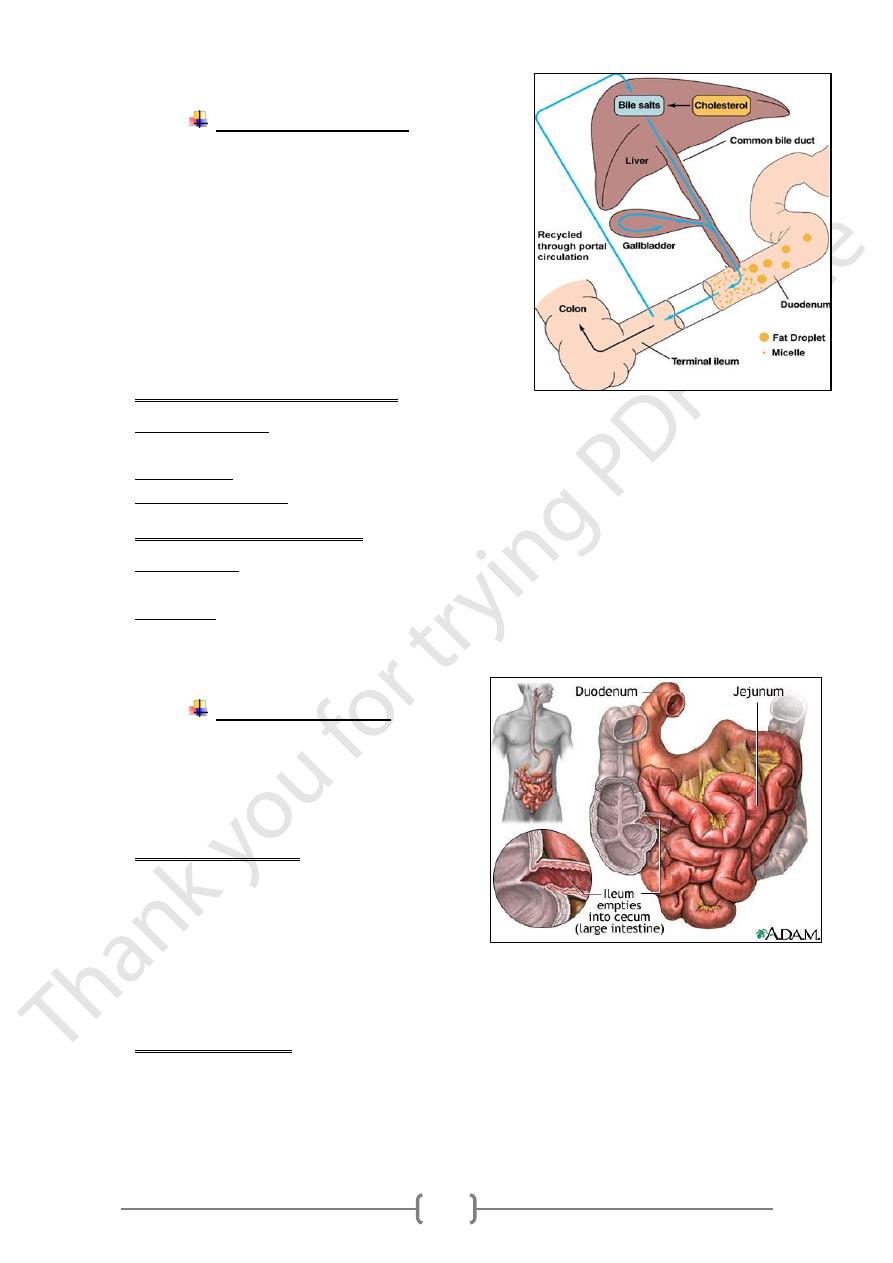
The Small Intestine
Is divided into three sections:
1) The duodenum is the first section.
2) The jejunum is the middle section.
3) The ileum is the last section.
Hormones Released
• Secretin: causes pancreas to release
bicarbonate to neutralize acidity of chyme.
• Cholecystokinin: triggers gallbladder to
release bile
• Bile: Emulsifies fat after it is secreted into small intestine. Produced in liver; stored in
gallbladder.
Produces Enzymes
• Prepares foods for absorption
Lactase, maltase, sucrase convert lactose, maltose, sucrose :to simple sugars.
Peptidases convert proteins to amino acids
11
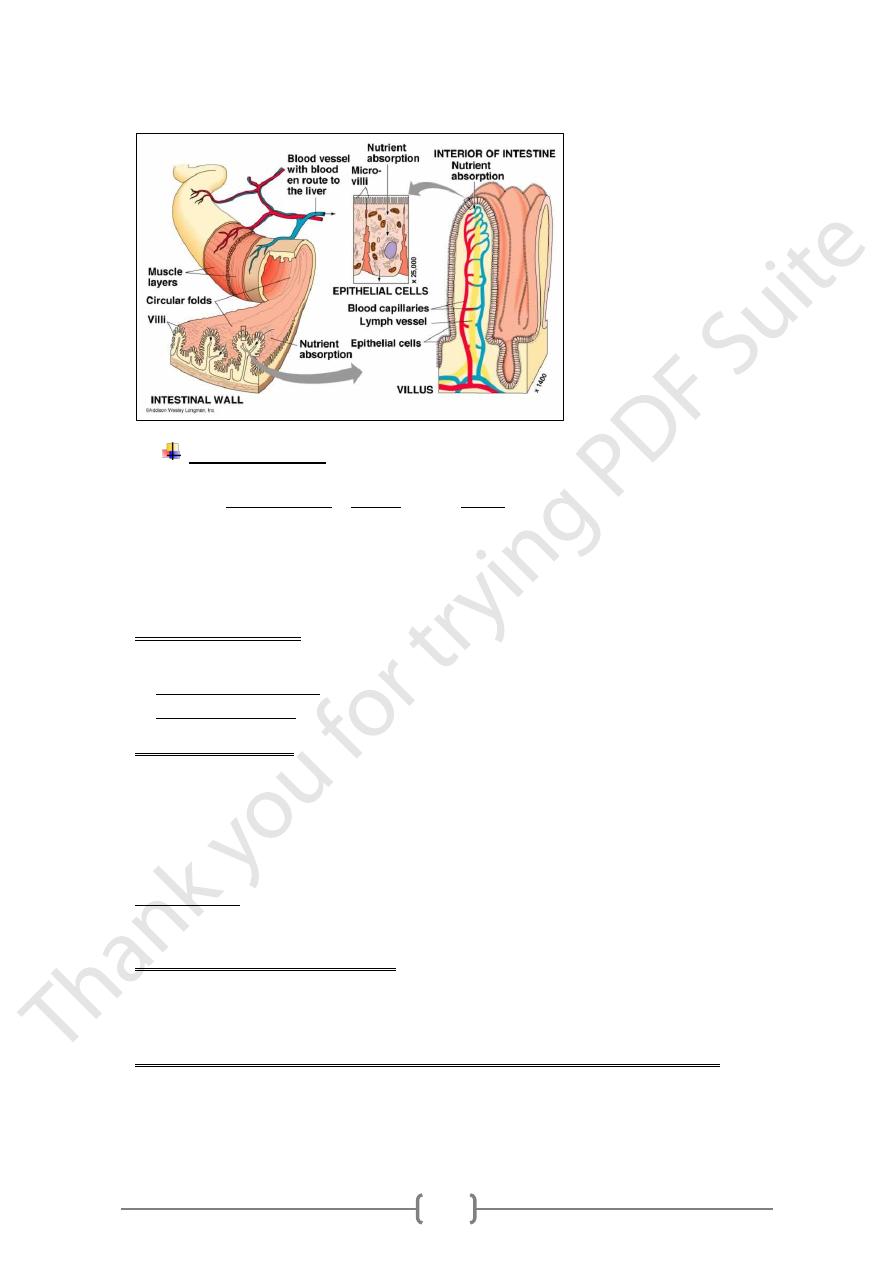
• Villi: are hair like projections, increase surface area for maximum absorption.
Large Intestine
• Colon walls secrete mucus to protect against acidic digestive juices in chyme.
• Major tasks of the large intestine:
o Absorb water
o Synthesize some B vitamins and vitamin K
o Collect food residue
Intestinal secretions
Two types of intestinal glands
1) Cryptus of Lieberkuhn: the secreting cells are found in mucosal glands.
2) Glands of Brunner: A second type of glands is found only in the duodenum.
Intestinal Enzymes
1) Enteropeptidase. Aminopeptidase. Dipeptiase.
2) Nuclease. Nucleotidase. Nucleosidase.
3) Maltase. Sucrase. Lactase.
4) Lipase. Alkaline Phosphatase.
Only Enteropeptidase and Alkaline phosphatase are actually secreted by the
h
other enzymes are in fact either an integral part of the brus
The
.
intestinal cells
border or found within the epithelial cell cytoplasm.
Functions of intestinal enzymes
These enzymes complete the digestion of different food stuff during its passage through
the gut either in the lumen or inside the cytoplasm of the intestinal epithelial cells.
the stomach and other digestive organs do not digest themselves?
Why
1) The digestive enzymes are isolated within the cells in "secretary vacuoles".
2) All the major proteases are stored as inactive enzymes, such as: pepsinogen,
trypsinogen, chymotrypsinogen.
11
3) These enzymes and hormones cannot enter into the mucosal cells after secretion.
4) The gastric mucous provides a protective coating for the mucosal cells.
5) There are other protective elements such as cell surface glycoproteins that cover the
cell membrane.
