Basic Anatomy
first lumbar vertebra (Fig. 12.7). In the young child, it is
inferiorly in the adult at the level of the lower border of the
ous with the medulla oblongata of the brain. It terminates
begins above at the foramen magnum, where it is continu
The spinal cord is a cylindrical, grayish white structure that
For dermatomes of the back, see Figure 1.25.
posterior ramus divides into a medial and a lateral branch.
causes diminished, but not total, loss of sensation. Each
skin areas supplied occurs so that section of a single nerve
foramen from which they emerge. Considerable overlap of
posterior median sulcus.
face a shallow furrow, the
and on the posterior sur
anterior median fissure,
sure, the
possesses in the midline anteriorly a deep longitudinal fis
back of the coccyx (Figs. 12.7, 12.11, and 12.15). The cord
descends to be attached to the
filum terminale,
mater, the
from the apex of which a prolongation of the pia
ullaris,
conus med
Inferiorly, the spinal cord tapers off into the
lumbar enlargements.
cervical
called
gin to the lumbosacral plexus, has fusiform enlargements
the lower thoracic and lumbar regions, where it gives ori
region, where it gives origin to the brachial plexus, and in
the third lumbar vertebra. The spinal cord in the cervical
relatively longer and ends inferiorly at the upper border of
697
-
and
-
-
-
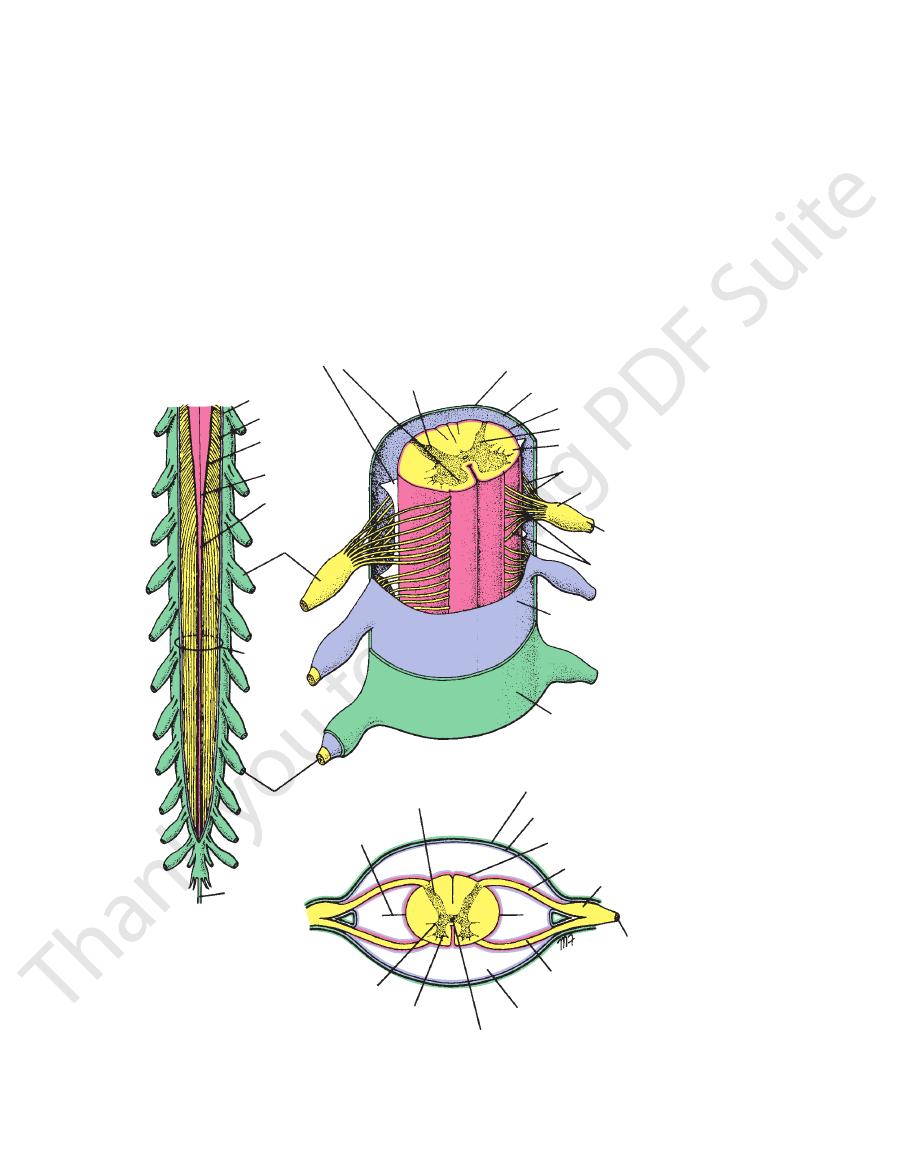
Spinal Cord
-
anterior gray column
posterior gray column
dura mater
arachnoid mater
pia mater
gray matter
white matter
posterior rootlets of spinal nerve
posterior root
ganglion
spinal nerve
anterior rootlets of spinal nerve
arachnoid mater
dura mater
spinal nerve
cauda
equina
posterior root ganglion
filum terminale
conus medullaris
pia mater
arachnoid mater
dura mater
filum terminale
ligamentum denticulatum
posterior gray column or horn
dura mater
arachnoid mater
pia mater
posterior root
posterior root ganglion
spinal nerve
anterior root
subarachnoid space filled with cerebrospinal fluid
central canal
anterior gray column or horn
lateral gray column or horn
A
B
C
ligamentum denticulatum
FIGURE 12.11
A.
showing the meninges and the position of the cerebrospinal fluid.
Transverse section through the spinal cord
showing the anterior and posterior roots of the spinal nerves and meninges.
Lower end of the spinal cord and the cauda equina. B. Section through the thoracic part of the spinal cord
C.
698
CHAPTER 12
Here,
spinal nerve.
foramina, where they unite to form a
cord segment to the level of their respective intervertebral
The spinal nerve roots pass laterally from each spinal
rise to peripheral and central nerve fibers.
possesses a posterior root ganglion, the cells of which give
responding segment of the cord. Each posterior nerve root
series of rootlets, which extend the whole length of the cor
12.14, and 12.15). Each root is attached to the cord by a
(Figs. 12.11, 12.13,
sensory, roots
or
posterior,
motor, roots
or
anterior,
31 pairs of spinal nerves by the
Along the whole length of the spinal cord are attached
(Figs. 12.11 and 12.15).
cauda equina
terminale. The inferior nerve roots together are called the
the adult) form a vertical leash of nerves around the filum
of the cord (lower border of the first lumbar vertebra in
and sacral nerves inferior to the level of the termination
and run almost horizontally, but the roots of the lumbar
the upper cervical region, the spinal nerve roots are short
sively from above downward (Figs. 12.12 and 12.15). In
the spinal cord, the length of the roots increases progres
vertebral column during development compared to that of
ers. Because of the disproportionate growth in length of the
nerve is made up of a mixture of motor and sensory fib
the motor and sensory fibers become mixed so that a spinal
The Back
-
-
Roots of the Spinal Nerves
and the
-
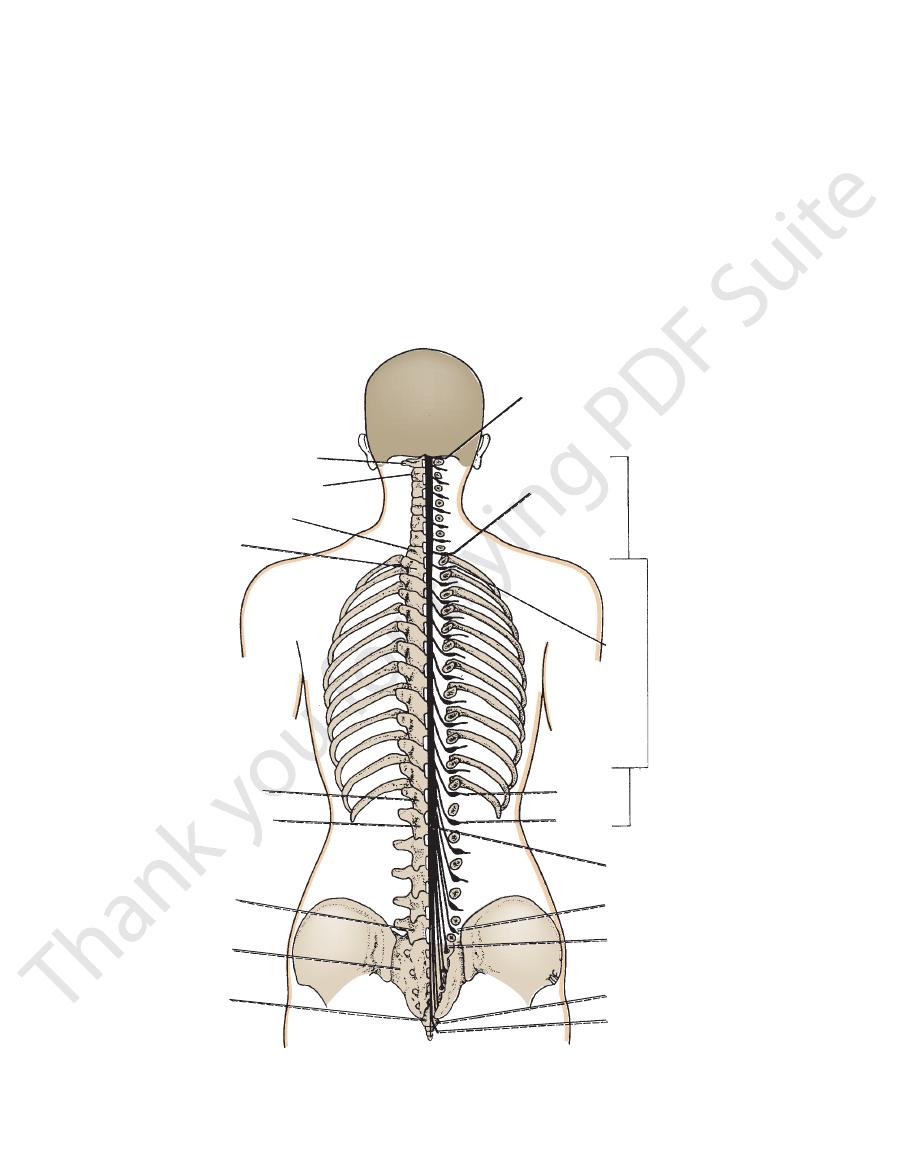
S5
atlas
axis
seventh cervical vertebra
first thoracic vertebra
first lumbar vertebra
twelfth thoracic vertebra
sacrum
coccyx
C1 spinal nerve
cervical
segments
of spinal
cord
coccygeal spinal nerve one
lower end of spinal cord
lumbar, sacral, and
coccygeal segments
of spinal cord
thoracic
segments
of spinal
cord
fifth lumbar vertebra
L1
L5
S1
C8
T1
T12
FIGURE 12.12
Posterior view of the spinal cord showing the origins of the roots of the spinal nerves and their relationship
nerve roots.
to the different vertebrae. On the right, the laminae have been removed to expose the right half of the spinal cord and the
Basic Anatomy
anterior spinal arteries,
The
close to the attachments of the posterior spinal nerve roots.
the vertebral arteries, run down the side of the spinal cord,
which arise either directly or indirectly from
nal arteries,
posterior spi
The
anterior spinal artery.
arteries and one
longitudinally running arteries: the two posterior spinal
The spinal cord receives its arterial supply from three small,
motor and sensory fibers.
which contain both
posterior ramus,
and a smaller
ramus
anterior
spinal nerve immediately divides into a large
After emergence from the intervertebral foramen, each
699
Blood Supply of the Spinal Cord
-
which arise from the
ebral
vert
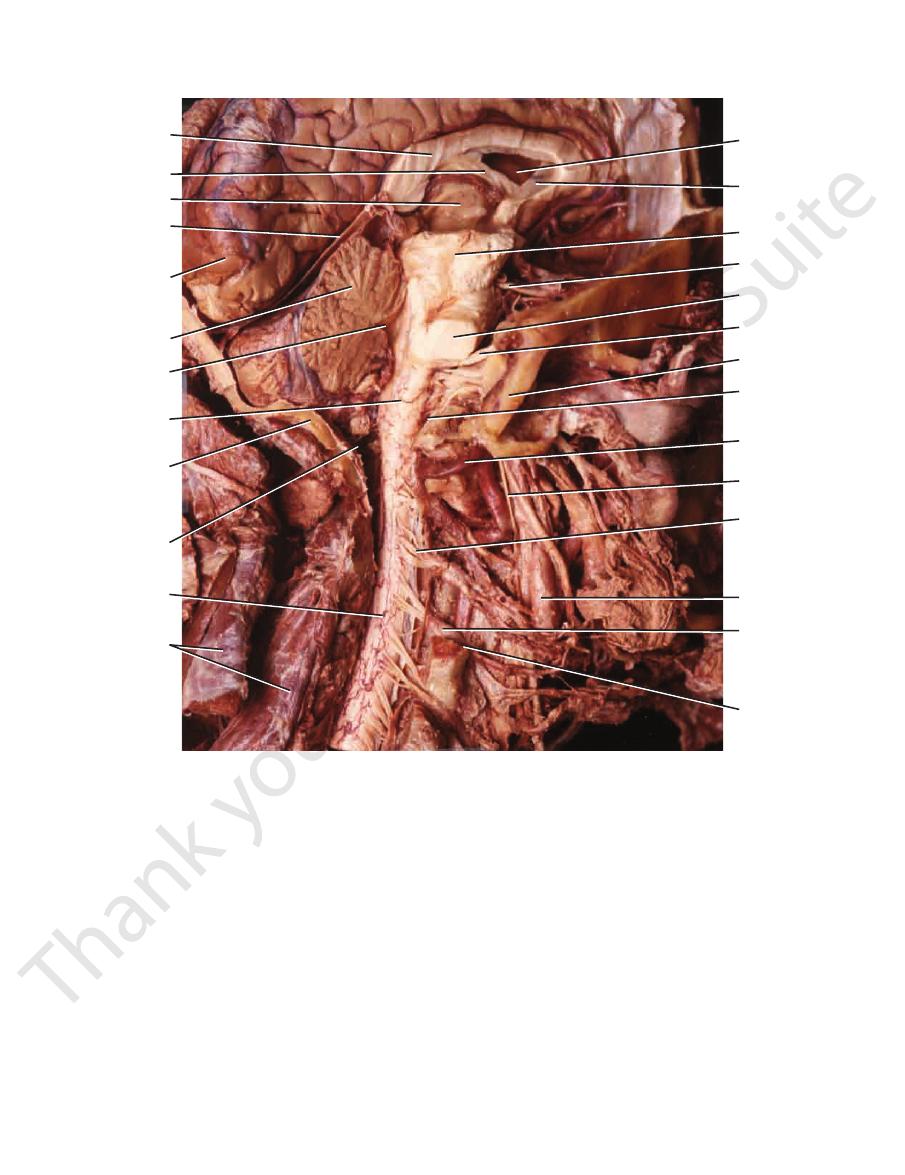
cavity of lateral
ventricle
septum
pellucidum
midbrain
III c. nerve
pons
V c. nerve
occipital bone
spinal root of
accessory nerve
vertebral artery
X c. nerve
rootlets of
posterior root
of third cervical
spinal n.
carotid artery
posterior root
ganglion of
fourth cervical
spinal n.
fourth cervical
spinal n.
corpus
callosum
POSTERIOR
ANTERIOR
fornix
thalamus
tentorium
cerebelli
occipital lobe
of cerebrum
cerebellum
fourth
ventricle
medulla
oblongata
occipital
bone
foramen
magnum
spinal
cord
post vertebral
muscles
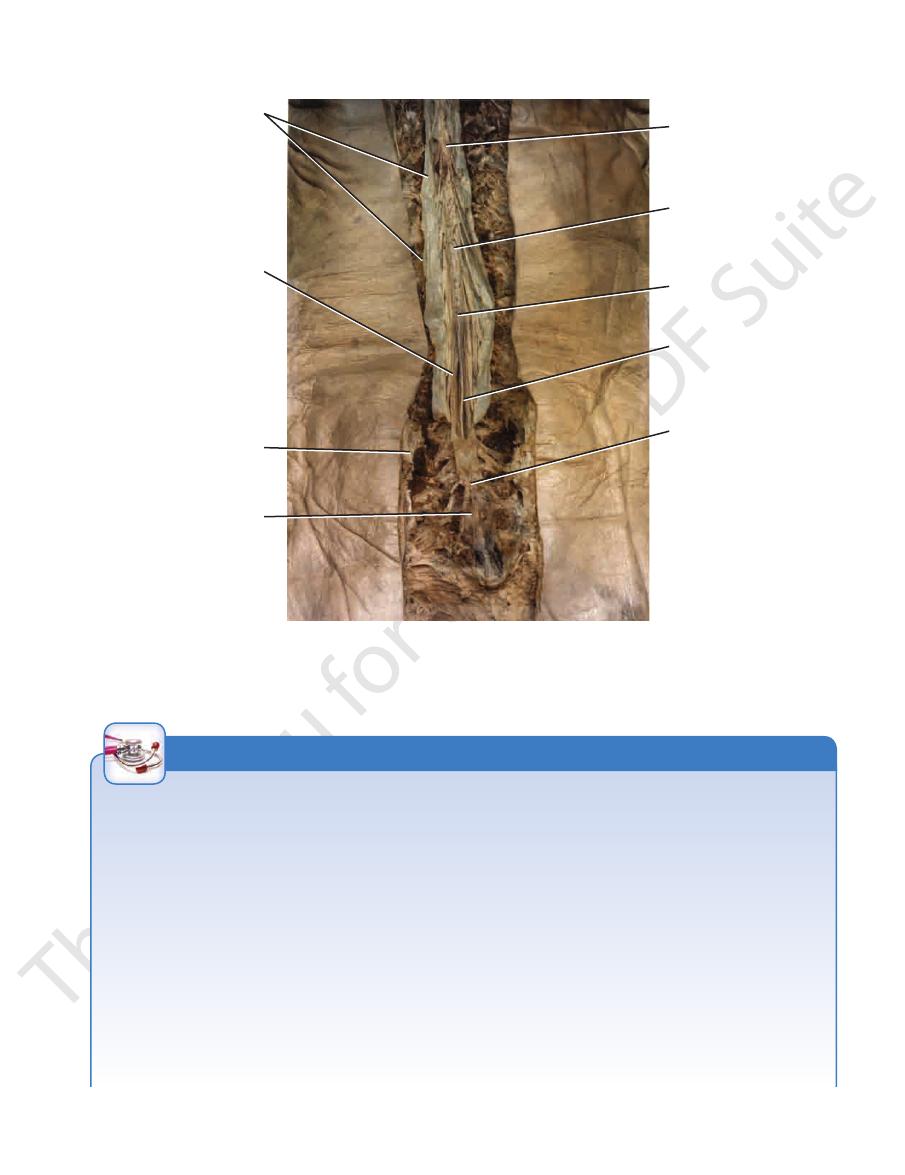
FIGURE 12.13
tal section
Dissection of the skull and the upper part of the cervical vertebral column showing the brain in sagit
of the spinal cord drain into the internal
veins
The
through the intervertebral foramina.
which enter the vertebral canal
radicular arteries,
by
The posterior and anterior spinal arteries are reinforced
within the anterior median fissure.
arteries, unite to form a single artery, which runs down
intervertebral foramina.
Note also the roots of the cervical spinal nerves and the trunks of the spinal nerves as they emerge through the dissected
and the intact spinal cord in situ. Note the continuity of the medulla oblongata and the spinal cord at the foramen magnum.
vertebral venous plexus.
mater (see Figs. 12.11, 12.14, and 12.15).
meninges: the dura mater, the arachnoid mater, and the pia
The spinal cord, like the brain, is surrounded by three
Meninges of the Spinal Cord
700
CHAPTER 12
The Back
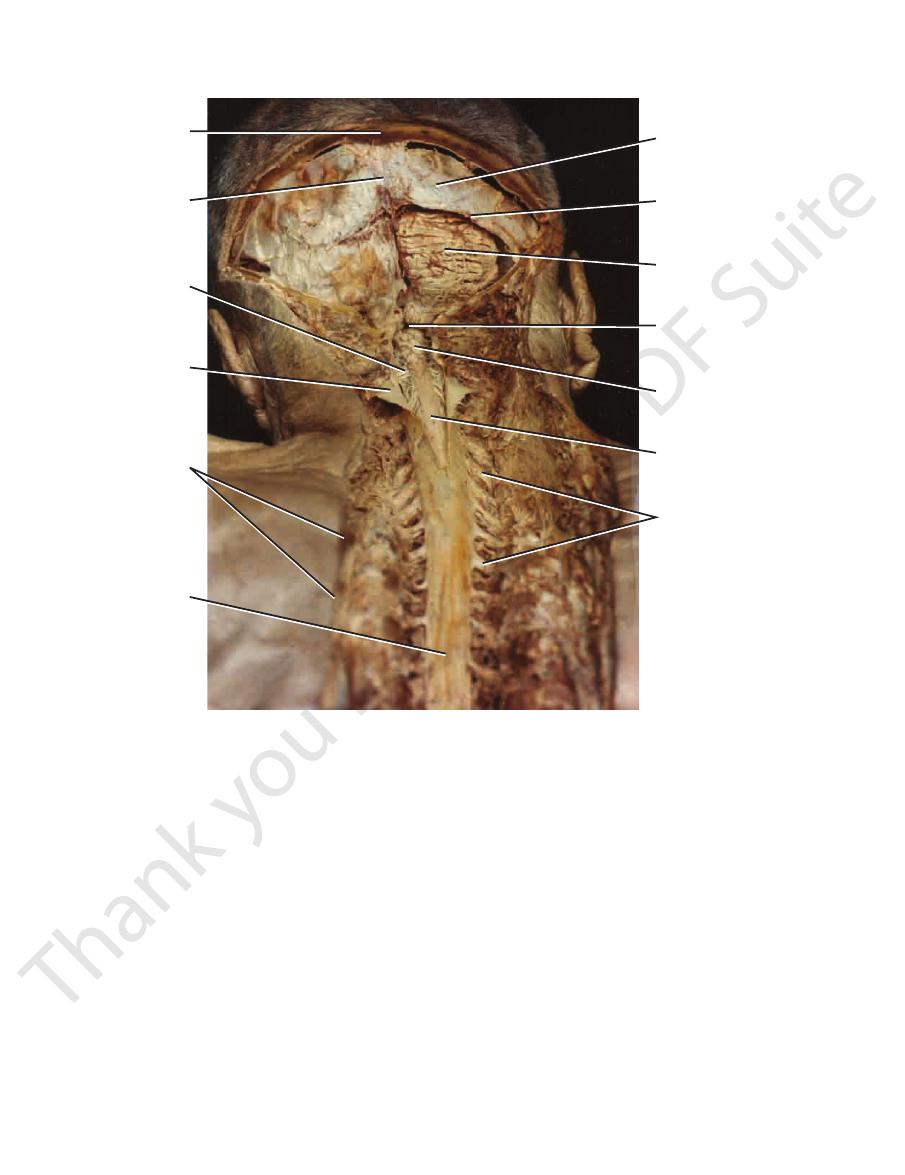
periosteal
layer of dura
cut edge of periosteal
layer of dura just below
transverse sinus
right cerebellar
hemisphere
foramen of
magendie
medulla
oblongata
spinal cord
posterior roots of
cervical spinal nerves
surrounded by
meningeal sheaths
cut edge of
skull bone
site of superior
sagittal sinus
reflected cut
flap of dura and
arachnoid
posterior root
of cervical spinal
nerve
cut edge
of skin
dural sheath
for spinal
cord
FIGURE 12.14
he greater part of the occipital bone has been removed expos
Dissection of the back of the head and neck. T
intervertebral foramen. The inner surface of the dura mater
(epineurium)
tissue surrounding each spinal nerve
each nerve root and becomes continuous with connective
vertebral venous plexus. The dura mater extends along
space). This contains loose areolar tissue and the internal
(epidural
extradural space
the walls of the canal by the
lies loosely in the vertebral canal and is separated from
of the second sacral vertebra (Fig. 12.7). The dural sheath
ends on the filum terminale at the level of the lower border
the meningeal layer of dura covering the brain. Inferiorly, it
continuous superiorly through the foramen magnum with
and cauda equina (Figs. 12.10, 12.11, 12.14, and 12.15). It is
dense, strong, fibrous sheet that encloses the spinal cord
The dura mater is the most external membrane and is a
Dura Mater
nerves leaving the vertebral canal enveloped in a meningeal sheath.
been incised in the midline to expose the spinal cord and rootlets of the cervical spinal nerves. Note the cervical spinal
to expose the cerebellum and the medulla oblongata in the posterior cranial fossa. In the neck the dura and arachnoid have
ing the periosteal layer of dura. On the right side a window has been made in the dura below the transverse venous sinus
-
at the
is separated from the arachnoid mater by the potential
border of the second sacral vertebra (Figs. 12.7 and 12.15).
orly, it ends on the filum terminale at the level of the lower
magnum with the arachnoid covering the brain. Inferi
The arachnoid is continuous above through the foramen
(Fig. 12.11).
cerebrospinal fluid
which is filled with
space,
subarachnoid
arated from the pia mater by a wide space, the
that contains a thin film of tissue fluid. The arachnoid is sep
12.11). It is separated from the dura by the subdural space
internally and the dura mater externally (Figs. 12.10 and
covering the spinal cord and lying between the pia mater
The arachnoid mater is a delicate impermeable membrane
Arachnoid Mater
subdural space.
-
-
Basic Anatomy
701
spinal cord
conus
medullaris
lower end of
spinal cord
filum
terminale
lower end of
subarachnoid
space
reflected cut
edge of dura
and arachnoid
anterior and
posterior nerve
roots of
cauda equina
cut lamina
of sacrum
filum
terminale
FIGURE 12.15
Dissection of the lower part of the back including a complete laminectomy of the lumbar and sacral regions of
roots of the lumbar and sacral spinal nerves forming the cauda equina.
lower end of the spinal cord, and the cauda equina. Note the filum terminale surrounded by the anterior and posterior nerve
the vertebral column. The meningeal sheath has been incised and reflected laterally exposing the subarachnoid space, the
Nerve Root Pain
is, the cervicothoracic junction and the lumbosacral junction. In
The discs most commonly affected are those in areas where
the disc is undergoing degenerative changes that result in her
sudden shocks, particularly if the vertebral column is flexed and
on their shoulders. Nevertheless, the discs are vulnerable to
umn is the growth of osteophytes, which commonly encroach on
cesses and joints (Fig. 12.5). In the lumbar region, the largest
disc and the vertebral body, and posteriorly by the articular pro
Spinal nerve roots exit from the vertebral canal through the
intervertebral foramina. Each foramen is bounded superiorly
and inferiorly by the pedicles, anteriorly by the intervertebral
-
foramen is between the first and second lumbar vertebrae and
the smallest is between the fifth lumbar and first sacral vertebra.
One of the complications of osteoarthritis of the vertebral col-
the intervertebral foramina, causing pain along the distribution
of the segmental nerve. The fifth lumbar spinal nerve is the larg-
est of the lumbar spinal nerves, and it exits from the vertebral
column through the smallest intervertebral foramen. For this rea-
son, it is the most vulnerable.
Osteoarthritis as a cause of root pain is suggested by the
patient’s age, its insidious onset, and a history of back pain of
long duration. A prolapsed disc usually occurs in a younger age
group and often has an acute onset.
Herniated Intervertebral Discs
The structure and function of the intervertebral disc are
described on pages 689 and 690. The resistance of these discs
to compression forces is substantial, as seen, for example, in cir-
cus acrobats who can support four or more of their colleagues
-
niation of the nucleus pulposus.
a mobile part of the column joins a relatively immobile part—that
these areas, the posterior part of the anulus fibrosus ruptures,
and the nucleus pulposus is forced posteriorly like toothpaste out
C L I N I C A L N O T E S
(continued)
Basic Anatomy
703
Summary of Important Features Found in Cervical and Lumbosacral Root Syndromes
T A B L E 1 2 . 1
Toe extension, ankle
Tibialis anterior, quadriceps
Triceps
Triceps and flexor carpi
Wrist extensors
Movement Weakness
Root Injury Dermatome Pain
Muscle Supplied
Reflex Involved
C5
Lower lateral aspect of upper arm
Deltoid and biceps
Shoulder abduction, elbow
flexion
Biceps
C6
Lateral aspect of forearm
Extensor carpi radialis longus
and brevis
Brachioradialis
C7
Middle finger
radialis
Extension of elbow and flexion
of wrist
C8
Medial aspect of forearm
Flexor digitorum superficialis
and profundus
Finger flexion
None
L1
Groin
Iliopsoas
Hip flexion
Cremaster
L2
Anterior aspect of thigh
Iliopsoas, sartorius, hip
adductors
Hip flexion, hip adduction
Cremaster
L3
Medial aspect of knee
Iliopsoas, sartorius,
quadriceps, hip adductors
Hip flexion, knee extension,
hip adduction
Patellar
L4
Medial aspect of calf
Foot inversion, knee extension
Patellar
L5
Lateral part of lower leg and
dorsum of foot
Extensor hallucis longus,
extensor digitorum longus
dorsiflexion
None
S1
Lateral edge of foot
Gastrocnemius, soleus
Ankle plantar flexion
Ankle jerk
S2
Posterior part of thigh
Flexor digitorum longus, flexor
hallucis longus
Ankle plantar flexion, toe
flexion
None
disc
occipital bone
atlas
nucleus
pulposus
anulus
fibrosus
C1
C2
C3
C4
C5
C6
C7
C8
T1
T1
1
2
3
4
5
6
7
L3
L5
S1
L5
S1
A
B
C
D
foramen magnum
L5—S1
S1
L5
3
5
4
E
S1
L4
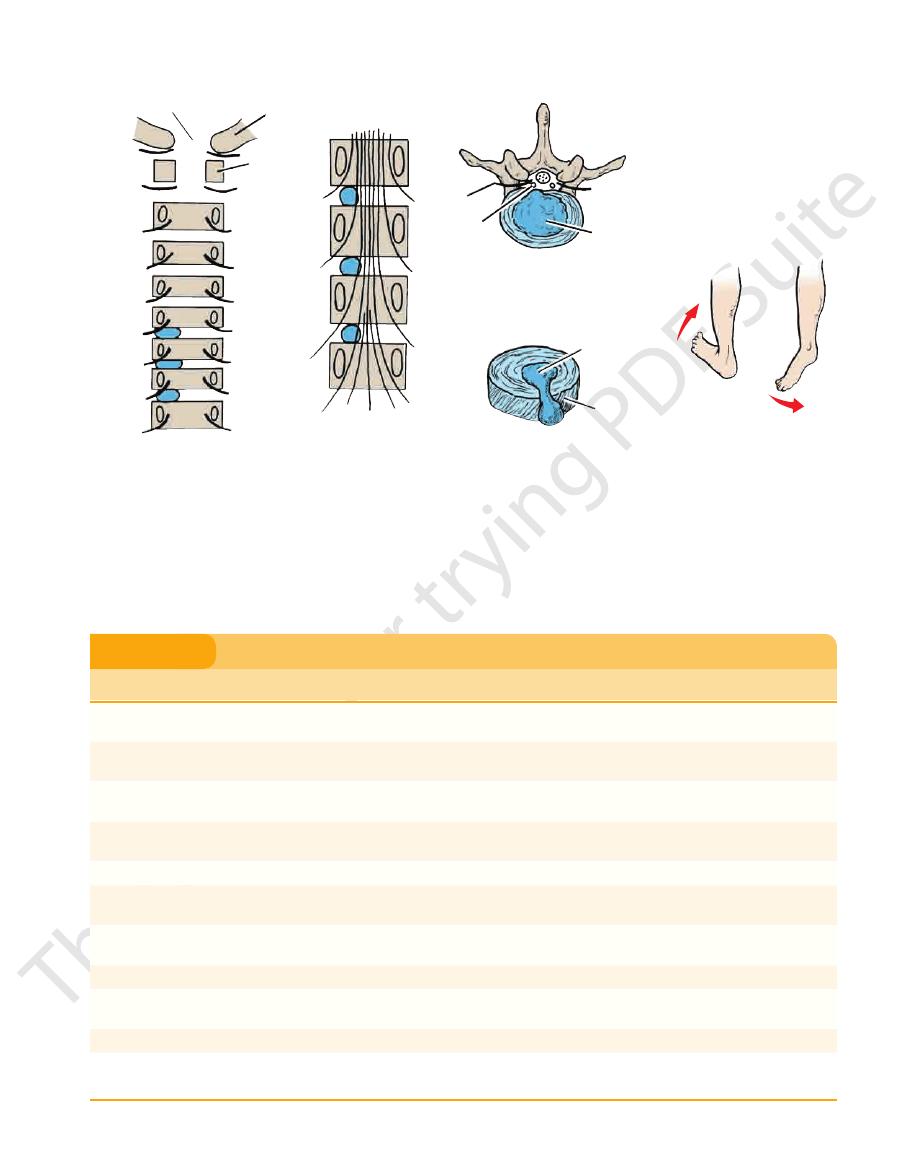
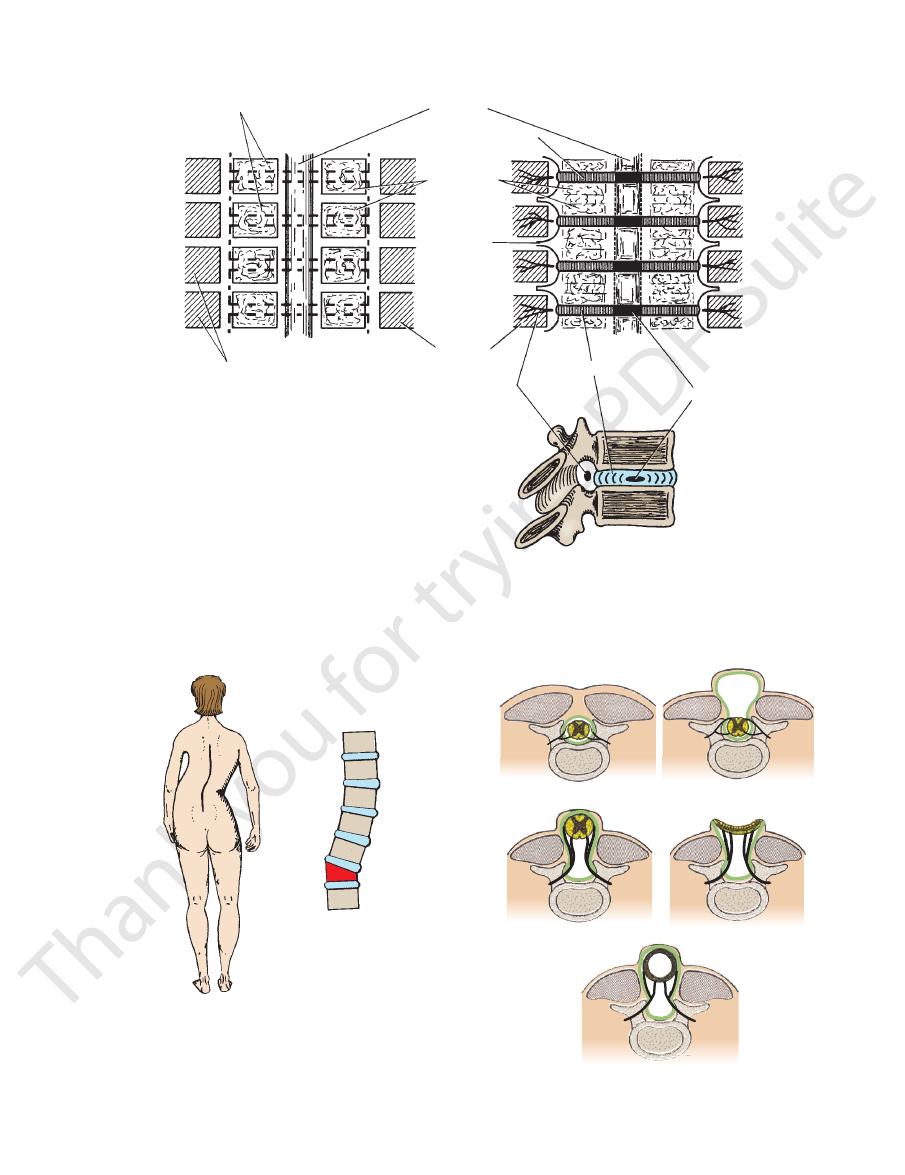
FIGURE 12.16
A, B.
the S1 motor nerve root produces weakness of plantar flexion of the ankle joint.
Pressure on the L5 motor nerve root produces weakness of dorsiflexion of the ankle; pressure on
pulposus posteriorly.
An intervertebral disc that has herniated its nucleus
and the first sacral vertebra showing pressure on the S1 nerve root.
Posterolateral herniation of the nucleus pulposus of the intervertebral disc between the fifth lumbar vertebra
vertebrae.
the pedicle of the fourth lumbar vertebra and are not related to the intervertebral disc between the fourth and fifth lumbar
but only seven cervical vertebrae. In the lumbar region, for example, the emerging L4 nerve roots pass out laterally close to
exist between the herniated nucleus pulposus and the spinal nerve roots. Note that there are eight cervical spinal nerves
Posterior views of vertebral bodies in the cervical and lumbar regions showing the relationship that might
C.
D.
E.
704
CHAPTER 12
(Fig. 12.11).
the connective tissue surrounding each spinal nerve
along each nerve root and becomes continuous with
in the middle of the dural sheath. The pia mater extends
dura. It is by this means that the spinal cord is suspended
which passes laterally to be attached to the
ticulatum,
ligamentum den
between the nerve roots to form the
terminale. The pia mater is thickened on either side
covering the brain; inferiorly, it fuses with the filum
superiorly through the foramen magnum with the pia
The Back
-
Spinal Cord Ischemia
gia in flexion and extension are beyond the scope of this book. For
of function of afferent and efferent nerve tracts below the level of
of function at the level of the lesion and partial or complete loss
Injury to the spinal cord can produce partial or complete loss
bar vertebra. Second, the large size of the vertebral foramen
only down as far as the level of the lower border of the first lum
facts aid the patient. First, the spinal cord in the adult extends
ing severe injury. However, when considerable displacement
of the vertebral canal often results in the spinal cord escap
running anterior and posterior spinal arteries are of small and
The blood supply to the spinal cord is surprisingly meager, con-
sidering the importance of this nervous tissue. The longitudinally
variable diameter, and the reinforcing segmental arteries vary in
number and in size. Ischemia of the spinal cord can easily follow
minor damage to the arterial supply as a result of regional anes-
thesia, pain block procedures, or aortic surgery.
Spinal Cord Injuries
The degree of spinal cord injury at different vertebral levels is
largely governed by anatomic factors. In the cervical region,
dislocation or fracture dislocation is common, but the large size
-
occurs, the cord is sectioned and death occurs immediately.
Respiration ceases if the lesion occurs above the segmental ori-
gin of the phrenic nerves (C3, 4, and 5).
In fracture dislocations of the thoracic region, displacement
is often considerable, and the small size of the vertebral canal
results in severe injury to the spinal cord.
In fracture dislocations of the lumbar region, two anatomic
-
in this region gives the roots of the cauda equina ample room.
Nerve injury may therefore be minimal in this region.
the lesion. The symptoms and signs of spinal shock and paraple-
further information, a textbook of neurology should be consulted.
Relationships of Spinal Cord Segments to Vertebral
Numbers
Because the spinal cord is shorter than the vertebral column,
the spinal cord segments do not correspond numerically with
the vertebrae that lie at the same level (Fig. 12.12). The following
list helps determine which spinal segment is contiguous with a
given vertebral body.
Vertebrae
Spinal Segment
Cervical
Add 1
Upper thoracic
Add 2
Lower thoracic (T7 to 9)
Add 3
Tenth thoracic
L1 and 2 cord segments
Eleventh thoracic
L3 and 4 cord segments
Twelfth thoracic
L5 cord segment
First lumbar
Sacral and coccygeal cord segments
C L I N I C A L N O T E S
Between the levels of the conus medullaris and the lower end
The pia mater is a vascular membrane that closely covers
Pia Mater
space.
roots, forming small lateral extensions of the subarachnoid
The arachnoid mater is continued along the spinal nerve
equina bathed in cerebrospinal fluid (Figs. 12.11 and 12.15).
of the subarachnoid space lie the nerve roots of the cauda
the spinal cord (Figs. 12.10 and 12.11). It is
uous
contin
Lumbar Puncture (Spinal Tap)
with a stylet, is passed into the vertebral canal above or below
region is opened to a maximum (Fig. 12.17). An imaginary line
this region usually pushes the nerve roots to one side without
bra. The lower lumbar part of the vertebral canal is thus occu
terminates inferiorly at the level of the lower border of the first
Lumbar puncture may be performed to withdraw a sample of
cerebrospinal fluid for examination. Fortunately, the spinal cord
lumbar vertebra in the adult. (In the infant, it may reach as low
as the third lumbar vertebra.) The subarachnoid space extends
inferiorly as far as the lower border of the second sacral verte-
-
pied by the subarachnoid space, which contains the cauda
equina—that is, the lumbar and sacral nerve roots and the filum
terminale. A needle introduced into the subarachnoid space in
causing damage.
With the patient lying on the side with the vertebral column
well flexed, the space between adjoining laminae in the lumbar
joining the highest points on the iliac crests passes over the
fourth lumbar spine (Fig. 12.35). With a careful aseptic technique
and under local anesthesia, the lumbar puncture needle, fitted
C L I N I C A L N O T E S
(continued)
706
CHAPTER 12
The Back
cauda equina (anterior and posterior nerve roots)
posterior longitudinal ligament
anterior longitudinal ligament
intervertebral disc
fourth lumbar spinal nerve
articular process
transverse process
cauda equina
arachnoid mater
dura mater
supraspinous ligament
ligamentum flavum
interspinous ligament
lumbar puncture needle
skin
internal vertebral veins
spine
L3
L4
L5
superficial fascia
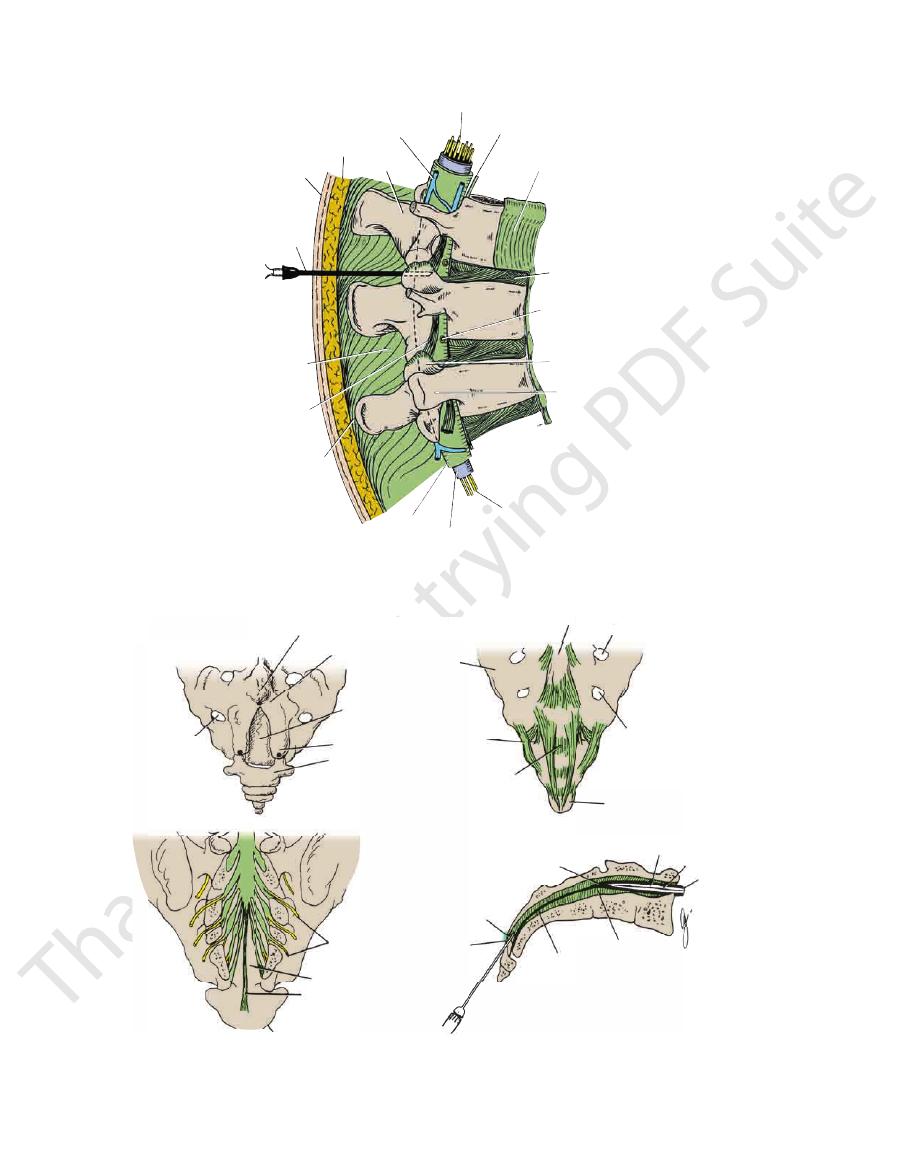
FIGURE 12.17
Sagittal section through the lumbar part of the vertebral column in flexion. Note that the spines and laminae
are well separated in this position, enabling one to introduce a lumbar puncture needle into the subarachnoid space.
fourth sacral
spinous process
sacral hiatus
coccyx
sacral cornu
A
B
D
lamina of fourth
sacral vertebra
lateral mass
of sacrum
sacrococcygeal
ligament
sacrococcygeal
membrane
fourth posterior
sacral foramen
dura and
arachnoid
coccyx
sacrococcygeal
membrane
coccyx
sacral
hiatus
sacral hiatus
filum terminale
lower limit of
subarachnoid space
posterior rami
of spinal nerves
filum terminale
extradural space
subarachnoid space filum
terminale
C
fourth posterior
sacral foramen
third sacral spinous process
third posterior sacral foramen
FIGURE 12.18
A.
Longitudinal section through the sacrum showing the anatomy of caudal anesthesia.
removed.
sheath (thecal sac) around the lower end of the spinal cord and spinal nerves in the sacral canal; the laminae have been
The dural
lower end of the sacrum and the coccyx showing the sacrococcygeal membrane covering the sacral hiatus.
Posterior surface of the
indicate the position of important bony landmarks.
Black dots
The sacral hiatus.
B.
C.
D.
Basic Anatomy
effectively protects the spinal cord from trauma.
with the bony and ligamentous walls of the vertebral canal,
medium that surrounds the spinal cord. This fluid, together
neuronal activity, the cerebrospinal fluid provides a fluid
In addition to removing waste products associated with
venous sinus.
superior sagittal
the dural venous sinuses, in particular the
into
arachnoid villi
bloodstream by passing through the
filum terminale (Fig. 12.7). Eventually, the fluid enters the
second sacral vertebra, where the arachnoid fuses with the
noid space extends down as far as the lower border of the
around the spinal cord. The spinal part of the subarach
over the surface of the cerebral hemispheres and downward
fourth ventricle (see page 548). It circulates both upward
noid space through the three foramina in the roof of the
through the ventricular system and enters the subarach
and fourth ventricles of the brain. The fluid circulates
within the lateral, third,
choroid plexuses,
mainly by the
The cerebrospinal fluid is a clear, colorless fluid formed
707
Cerebrospinal Fluid
-
-
cases with prolapse of an intervertebral disc (Fig. 12.16) (see
Relationship of the Vertebral Body to the Spinal
Nerve
Since the fully developed vertebral body is intersegmental in
position, each spinal nerve leaves the vertebral canal through
the intervertebral foramen and is closely related to the inter-
vertebral disc. This fact is of great clinical significance in
page 701).
C L I N I C A L N O T E S
Development of the Vertebral Column
only the neural arch for the atlas, which grows anteriorly and
neural arch (Fig. 12.19). The two centers for the centrum usually
At about the ninth week of development, primary ossification
pass between the myotomes to form the mesenchymal
nerves to fuse with their fellows of the opposite side and form
sclerotomic mesenchyme situated between adjacent vertebral
of the intervertebral disc is derived from
anulus fibrosus,
(Fig. 12.20). The surrounding fibrocartilage,
of the
pletely in the region of the vertebral body, but in the interver
(Figs. 12.19 and 12.20). Each vertebral body is thus
(Fig. 12.19). The caudal half of each
migrate medially during the fourth week of development and
The mesenchymal cells of the sclerotome rapidly divide and
Early in development, the embryonic mesoderm becomes differ-
entiated into three distinct regions: paraxial mesoderm, interme-
diate mesoderm, and lateral mesoderm. The paraxial mesoderm
is a column of tissue situated on either side of the midline of the
embryo, and at about the fourth week, it becomes divided into
blocks of tissue called somites. Each somite becomes differenti-
ated into a ventromedial part (the sclerotome) and a dorsolateral
part (the dermatomyotome). The dermatomyotome now further
differentiates into the myotome and the dermatome (Fig. 12.19).
surround the notochord
sclerotome now fuses with the cephalic half of the immedi-
ately succeeding sclerotome to form the mesenchymal verte-
bral body
an intersegmental structure. The notochord degenerates com-
-
tebral region, it enlarges to form the nucleus pulposus
intervertebral discs
the
bodies (Fig. 12.20).
Meanwhile, the mesenchymal vertebral body gives rise
to dorsal and lateral outgrowths on each side. The dorsal out-
growths grow around the neural tube between the segmental
the mesenchymal neural arch (Fig. 12.19). The lateral outgrowths
costal
processes, or primordia of the ribs.
Two centers of chondrification appear in the middle of each
mesenchymal vertebral body. These quickly fuse to form a car-
tilaginous centrum (Fig. 12.19). A chondrification center forms in
each half of the mesenchymal neural arch and spreads dorsally
to fuse behind the neural tube with its fellow of the opposite side.
These centers also extend anteriorly to fuse with the cartilagi-
nous centrum and laterally into the costal processes. The con-
densed mesenchymal or membranous vertebra has thus been
converted into a cartilaginous vertebra.
In the thoracic region, each costal process forms a carti-
laginous rib. The costal processes in the cervical region remain
short and form the lateral and anterior boundaries of the foramen
transversarium of each vertebra. In the lumbar region, the cos-
tal process forms part of the transverse process; in the sacral
region, the costal processes fuse together to form the lateral
mass of the sacrum.
centers appear: two for each centum and one for each half of the
unite quickly, but the complete union of all the primary centers
does not occur until several years after birth.
During adolescence, secondary centers appear in the car-
tilage covering the superior and inferior ends of the vertebral
body, and the epiphyseal plates are formed. A secondary center
also appears at the tip of each transverse process and at the tip
of the spinous process. By the 25th year, all the secondary cen-
ters have fused with the rest of the vertebra.
The atlas and axis develop somewhat differently. The cen-
trum of the atlas fuses with that of the axis and becomes the part
of the axis vertebra known as the odontoid process. This leaves
finally fuses in the midline to form the characteristic ring shape
of the atlas vertebra.
In the sacral region, the bodies of the individual vertebrae
are separated from each other in early life by intervertebral
discs. At about the 18th year, the bodies start to become united
E M B R Y O L O G I C N O T E S
(continued)

708
CHAPTER 12
The Back
neural tube
dermatome
myotome
sclerotome
notochord
mesenchymal neural arch
myotome
centers of chondrification
mesenchymal
costal process
mesenchymal
vertebral body
cartilaginous neural arch
primary centers
of ossification
cartilaginous
costal process
developing rib
fusion between
cartilage centers
notochord remains
cartilaginous
vertebral body
(centrum)
secondary centers
of ossification
site of neurocentral fusion
1
2
3
4
FIGURE 12.19
The stages in the formation of a thoracic vertebra.
by bone; this process starts caudally. Usually by the 13th
in the affected region. The types of spina bifida are shown in
tube and the surface ectoderm, to form the vertebral arches
ure of the mesenchyme, which grows in between the neural
this defect, the meninges and spinal cord may or may not be
in the lower thoracic, lumbar, and sacral regions. Beneath
vertebrae fail to develop. The condition occurs most frequently
In spina bifida, the spines and arches of one or more adjacent
The prevertebral and postvertebral muscles develop from the
develops. Toward the end of the first year, when the child stands
his or her head, the cervical curve, which is convex anteriorly,
uous anterior (ventral) concavity. When the child begins to raise
(ventral) concavity. Later, the sacrovertebral angle develops. At
The embryonic vertebral column shows one continuous anterior
year, all the sacral vertebrae are united. In the coccygeal region,
segmental fusion also takes place, and in later life the coccyx
often fuses with the sacrum.
Development of the Curves of the Vertebral Column
birth, the cervical, thoracic, and lumbar regions show one contin-
up, the lumbar curve, which is convex anteriorly, develops.
Development of the Muscles of the Vertebral Column
segmental myotomes.
Scoliosis
Scoliosis results from a congenital hemivertebra. A hemiverte-
bra is caused by a failure in development of one of the two ossi-
fication centers that appear in the centrum of the body of each
vertebra (Fig. 12.21).
Spina Bifida
involved in varying degrees. This condition is a result of fail-
Figures 12.22 and 12.23.
Basic Anatomy
709
sclerotomes
myotomes
notochord
intervertebral disc
sclerotomes
costal
process
myotomes
spinal nerves
anulus fibrosus
nucleus pulposus
FIGURE 12.20
The formation of each mesenchymal vertebral body by the fusion of the caudal half of each sclerotome with
spinal nerve and each intervertebral disc.
costal processes grow out between adjacent myotomes. Also shown is the close relationship that exists between each
the cephalic half of the immediately succeeding sclerotome. Each vertebral body is thus an intersegmental structure. The
FIGURE 12.21
Posterior view of a woman with scoliosis
resulting from a congenital hemivertebra in the lower
thoracic region.
spina bifida occulta
meningocele
meningomyelocele
myelocele
syringomyelocele
FIGURE 12.22
Different types of spina bifida.
