278
CHAPTER 7
lateral to the lateral fornix of the vagina, to enter the bladder.
artery (Figs. 7.18 and 7.19). The ureter then runs forward,
of the broad ligament, where it is crossed by the uterine
spine. It then turns forward and medially beneath the base
behind the ovary until it reaches the region of the ischial
ward and backward in front of the internal iliac artery and
cation of the common iliac artery (Fig. 7.18). It runs down
The ureter crosses over the pelvic inlet in front of the bifur
sections.
the pelvic cavity in the female are described in the following
as described previously. The contents of the anterior part of
occupy the posterior part of the pelvic cavity (see Fig. 7.5),
The rectum, sigmoid colon, and terminal coils of ileum
Pelvic Viscera in the Female
directly in contact with the abdominal wall.
the anterior abdominal wall so that the bladder becomes
up into the abdomen and peels off the peritoneum from
to remember that as the bladder fills, the superior wall rises
not cover the lateral surfaces of the bladder. It is important
bladder passes laterally to the lateral pelvic walls and does
The peritoneum covering the superior surface of the
the erect position, is the rectovesical pouch (see Fig. 7.4).
abdominopelvic peritoneal cavity, when the patient is in
abdominal wall. It is thus seen that the lowest part of the
continuous with the parietal peritoneum on the posterior
surfaces of the upper third of the rectum. It then becomes
the middle third of the rectum and the front and lateral
The peritoneum then passes up on the front of
pouch.
rectovesical
aspect of the rectum, forming the shallow
nal vesicles. Here, it sweeps backward to reach the anterior
a short distance until it reaches the upper ends of the semi
then runs down on the posterior surface of the bladder for
nal wall onto the upper surface of the urinary bladder. It
The peritoneum passes down from the anterior abdomi
pelvis in a sagittal plane (see Fig. 7.4).
The peritoneum is best understood by tracing it around the
covers and supports the pelvic viscera (see Fig.7.16).
The visceral pelvic fascia is a layer of connective tissue that
Visceral Pelvic Fascia
openings of the two ejaculatory ducts (see Fig. 7.16).
in females. On the edge of the mouth of the utricle are the
which is an analog of the uterus and vagina
static utricle,
pro
the summit of the urethral crest is a depression, the
the prostatic glands open into these grooves. On
sinus;
prostatic
On each side of this ridge is a groove called the
(see Fig. 7.16).
urethral crest
longitudinal ridge called the
On the posterior wall is a
portion of the entire urethra.
prostatic urethra is the widest and most dilatable
The
with the membranous part of the urethra (see Fig. 7.16).
tate from the base to the apex, where it becomes continuous
begins at the neck of the bladder. It passes through the pros
The prostatic urethra is about 1.25 in. (3 cm) long and
The Pelvis: Part II—The Pelvic Cavity
Prostatic Urethra
-
-
Peritoneum
-
-
Ureters
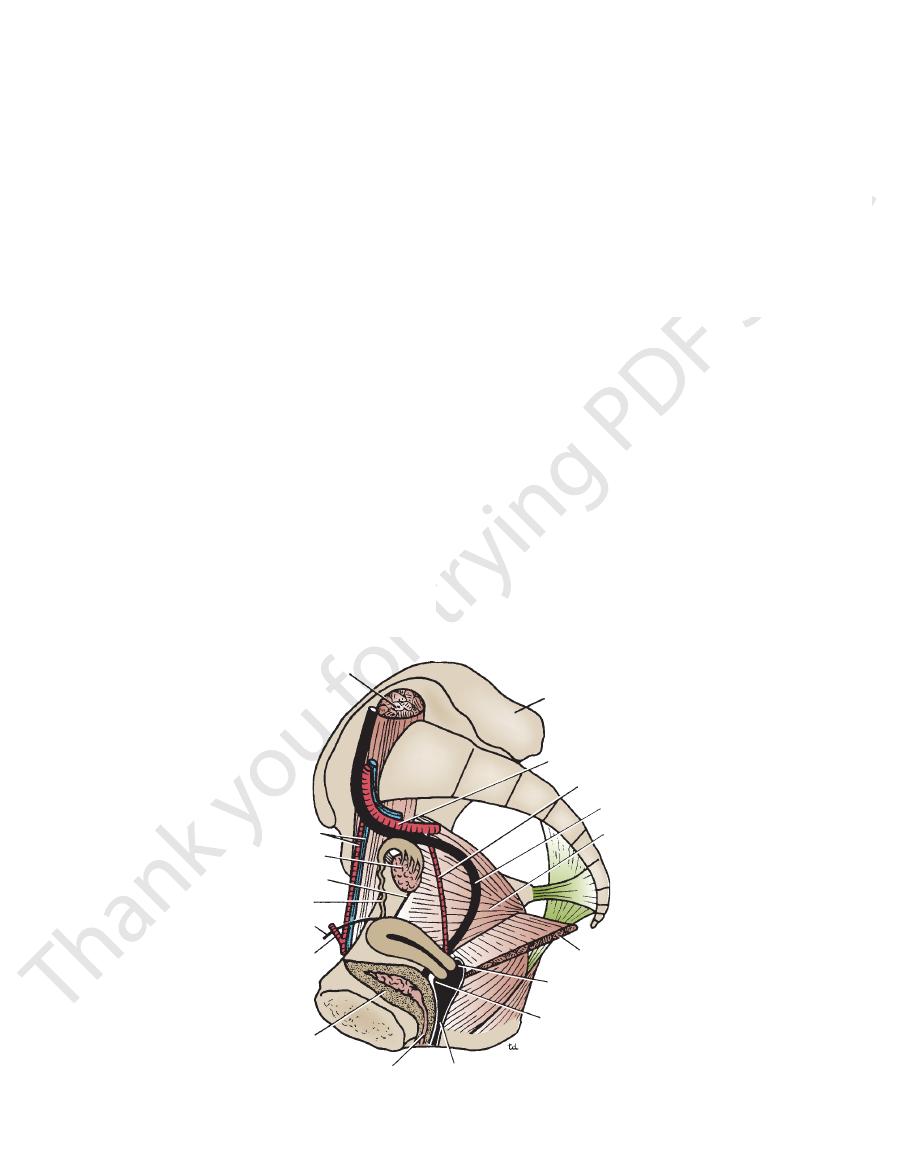
-
-
psoas
ilium
internal iliac artery
uterine artery
ureter
obturator internus
levator ani
posterior fornix
anterior fornix
vagina
bladder
inferior epigastric artery
round ligament of uterus
uterine tube
round ligament of ovary
ovary
external iliac vessels
urethra
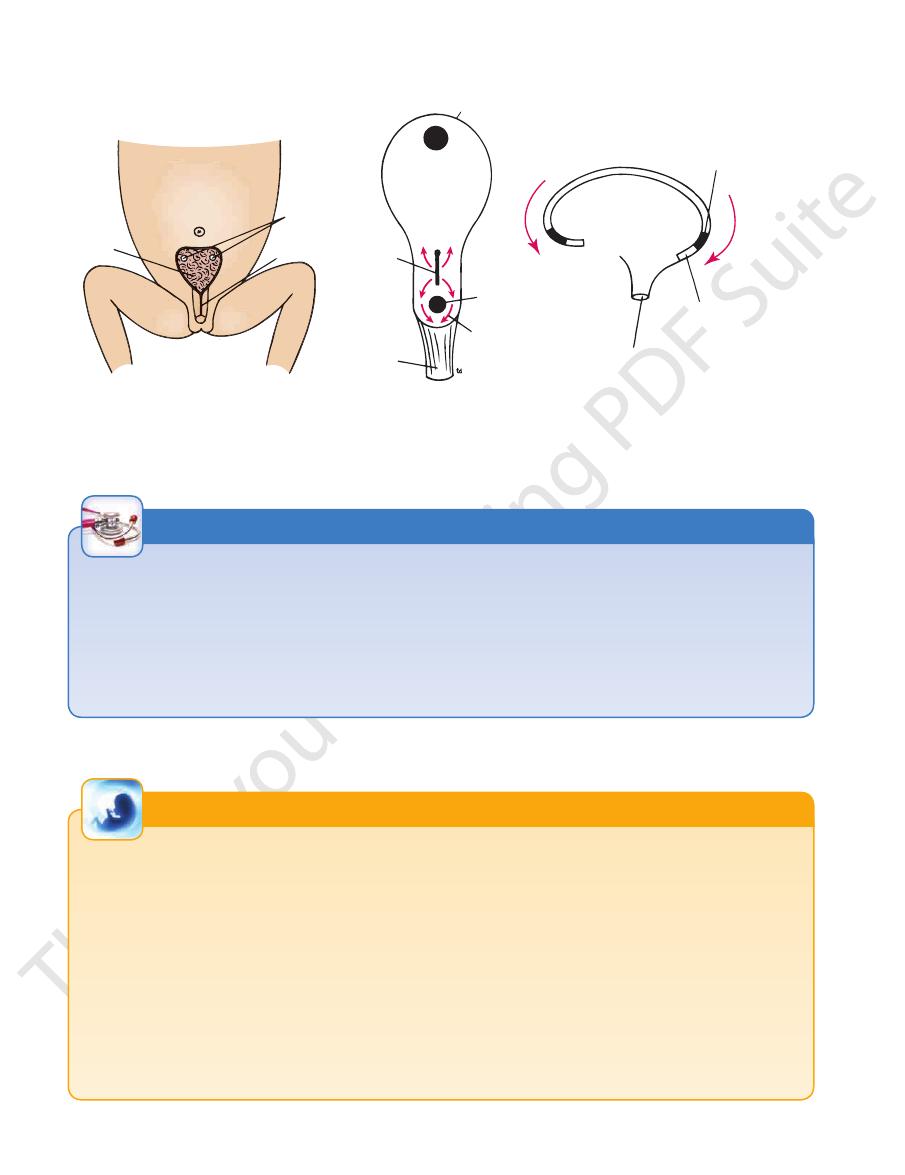
FIGURE 7.18
y, the uterine tube, and the vagina.
Right half of the pelvis showing the ovar
Basic Anatomy
279
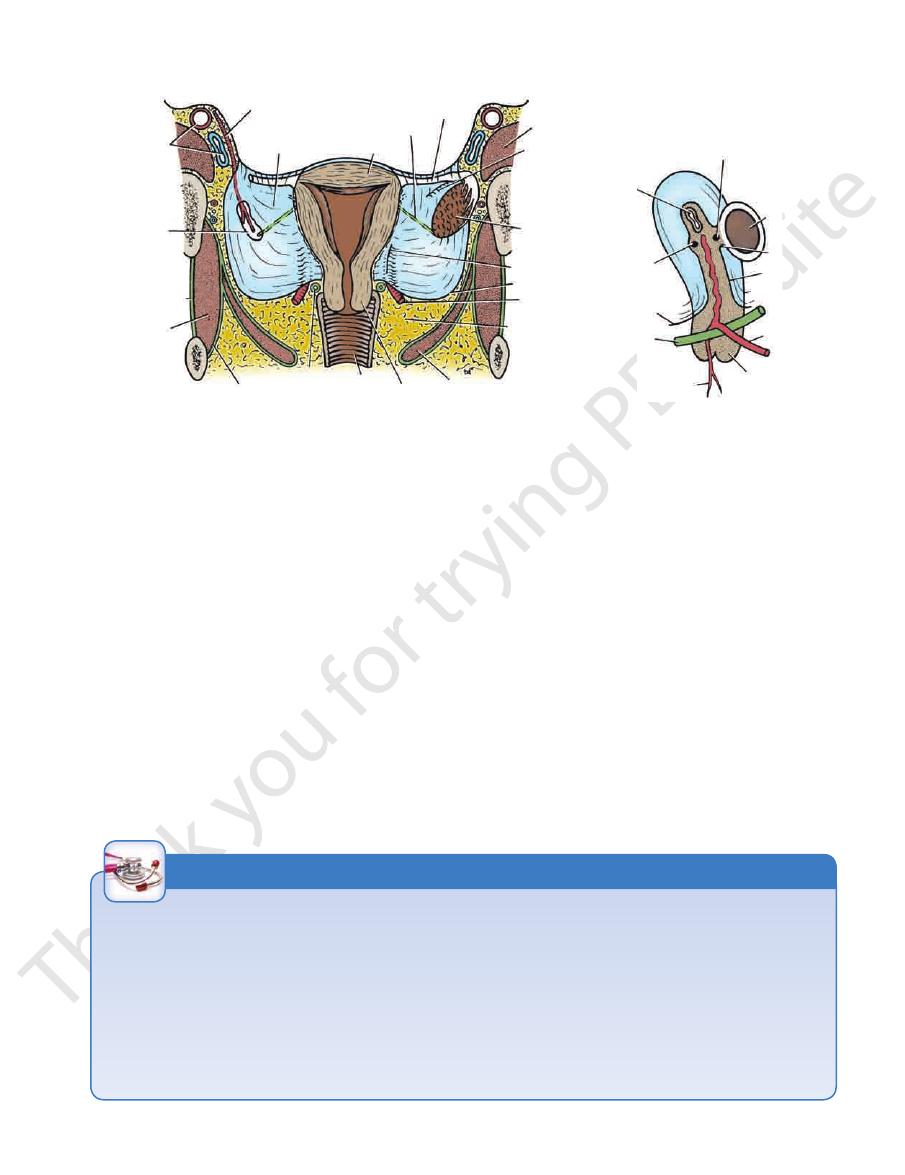
ovarian artery
external iliac
vessels
attachment of
mesovarium
obturator
membrane
obturator
internus
obturator internus fascia
ureter
vagina
levator ani
cervix
pelvic fascia
uterine artery
peritoneum
paroophoron
ovary
epoophoron
psoas
uterine tube
round ligament of ovary
fundus
broad
ligament
round ligament of ovary
uterine tube
round
ligament
of uterus
peritoneum
ureter
vaginal branch
cervix
uterine artery
broad ligament
mesovarium
ovary
A
B
FIGURE 7.19
Location and Description
of micturition are identical to those in the male.
supply, lymph drainage, and nerve supply; and the process
The general shape and structure of the bladder; its blood
urogenital diaphragm.
of the bladder rests on the upper surface of the
neck
The
internus muscle above and the levator ani muscle below.
More posteriorly, they lie in contact with the obturator
and the pubic bones.
retropubic pad of fat
in front to the
are related
inferolateral surfaces
body of the uterus. The
related to the uterovesical pouch of peritoneum and to the
superior surface
by the vagina from the rectum. The
is separated
posterior surface,
or
(see Fig. 7.5). The
of the bladder lies behind the symphysis pubis
apex
The
clinical importance (see Fig. 7.5).
the bladder to the uterus and the vagina is of considerable
surface of the urogenital diaphragm. The close relation of
in the male pelvis, and the neck rests directly on the upper
absence of the prostate, the bladder lies at a lower level than
ately behind the pubic bones (see Fig. 7.5). Because of the
As in the male, the urinary bladder is situated immedi
within the broad ligament. Note that the uterus has been retroverted into the plane of the vaginal lumen in both diagrams.
Uterus on lateral view. Note the structures that lie
ovary and part of the left uterine tube have been removed for clarity.
Coronal section of the pelvis showing the uterus, broad ligaments, and right ovary on posterior view. The left
A.
B.
Urinary Bladder
-
base,
is
Female Genital Organs
Ovary
Each ovary is oval shaped, measuring 1.5 × 0.75 in. (4 × 2 cm),
lateral margin of the uterus to the ovary (see Figs. 7.18 and 7.19).
remains of the upper part of the gubernaculum, connects the
which represents the
round ligament of the ovary,
The
(see Fig. 7.19).
suspensory ligament of the ovary
is called the
attachment of the mesovarium and the lateral wall of the pelvis
That part of the broad ligament extending between the
(see Fig. 7.19).
mesovarium
and is attached to the back of the broad ligament by the
Stress Incontinence
ing the urethra and the bladder neck surgically by sutures or
into the vagina that raises the upper end of the urethra. A
plished with some success by the introduction of a pessary
of the bladder and the urethra is restored. This may be accom
is directed to supporting the urethra so that the normal angle
nence than lean women. The treatment of stress incontinence
of partial urinary incontinence occurring when the patient
der is lost. This injury causes stress incontinence, a condition
stretches the supports of the bladder neck, and the normal
labor, especially one in which forceps is used, excessively
tone of the levatores ani muscles. In the female, a difficult
However, the most important support for the bladder is the
cia, which in certain areas is condensed to form ligaments.
The bladder is normally supported by the visceral pelvic fas-
angle between the urethra and the posterior wall of the blad-
coughs or strains or laughs excessively. It has been deter-
mined that obese women have twice the incidence of inconti-
-
more satisfactory permanent result may be achieved by rais-
by a fascial sling or artificial tape.
C L I N I C A L N O T E S
280
CHAPTER 7
The Pelvis: Part II—The Pelvic Cavity
Development of the Bladder in Both Sexes
absorbed into the lower part of the bladder so that the ure
The caudal ends of the mesonephric ducts now become
primitive
the anterior part of the cloaca on each side permits one, for
The entrance of the distal ends of the mesonephric ducts into
(Fig. 7.20).
is described on page
The division of the cloaca into anterior and posterior parts by
the development of the urorectal septum
268. The posterior portion forms the anorectal canal
purposes of description, to divide the anterior part of the clo-
aca into an area above the duct entrances called the
bladder and another area below called the urogenital sinus.
-
ters and ducts have individual openings in the dorsal wall (see
Fig. 7.20). With differential growth of the dorsal bladder wall, the
umbilicus (Fig. 7.22). The condition is caused by a failure of the
The primitive bladder may now be divided into an upper
the urethra. That part of the dorsal bladder wall marked off by
ureters come to open through the lateral angles of the bladder,
and the mesonephric ducts open close together in what will be
the openings of these four ducts forms the trigone of the blad-
der (Fig. 7.21). Thus, it is seen that in the earliest stages the lin-
ing of the bladder over the trigone is mesodermal in origin; later,
this mesodermal tissue is thought to be replaced by epithelium
of entodermal origin. The smooth muscle of the bladder wall is
derived from the splanchnopleuric mesoderm.
dilated portion, the bladder, and a lower narrow portion, the
urethra (see Fig. 7.20). The apex of the bladder is continuous
with the allantois, which now becomes obliterated and forms a
fibrous core, the urachus. The urachus persists throughout life
as a ligament that runs from the apex of the bladder to the umbi-
licus and is called the median umbilical ligament.
Congenital Anomalies of the Bladder
Exstrophy of the Bladder (Ectopia Vesicae)
Exstrophy of the bladder occurs three times more commonly
in males than in females. The posterior bladder wall protrudes
through a defect in the anterior abdominal wall below the
embryonic mesenchyme to invade the embryonic disc caudal to
of the prostatic urethra is formed from the urogenital sinus (see
(see page 212). Its inferior end is absorbed
In both sexes, the mesonephric (or Wolffian) duct gives origin on
mesenchyme between the ectoderm and entoderm produces an
the cloacal membrane (see Fig. 7.22). The absence of intervening
unstable state, which is followed by breakdown of this area.
Because of the urinary incontinence and almost certain
occurrence of ascending urinary infection, surgical reconstruc-
tion of the bladder is attempted.
Fate of the Mesonephric Duct in Both Sexes
each side to the ureteric bud, which forms the ureter, the pelvis
of the ureter, the major and minor calyces, and the collecting
tubules of the kidney
into the developing bladder and forms the trigone and part of the
urethra.
In the male, its upper or cranial end is joined to the develop-
ing testis by the efferent ductules of the testis, and so it becomes
the duct of the epididymis, the vas deferens, and the ejaculatory
duct. From the latter, a small diverticulum arises that forms the
seminal vesicle (see Fig. 4.26).
In the female, the mesonephric duct largely disappears. Only
small remnants persist—as the duct of the epoophoron and the
duct of the paroöphoron. The caudal end may persist and extend
from the epoophoron to the hymen as Gartner’s duct.
Development of the Urethra
In the male, the prostatic urethra is formed from two sources.
The proximal part, as far as the openings of the ejaculatory
ducts, is derived from the mesonephric ducts. The distal part
Fig. 7.21). The
In the female, the upper two thirds of the urethra are derived
membranous urethra and the greater part of the
penile urethra also are formed from the urogenital sinus. The
distal end of the penile urethra is derived from an ingrowth of
ectodermal cells on the glans penis.
from the mesonephric ducts. The lower end of the urethra is
formed from the urogenital sinus (see Fig. 7.21).
E M B R Y O L O G I C N O T E S
The ovary usually lies against the lateral wall of the pelvis
germinal
by a modified area of peritoneum called the
This capsule is covered externally
tunica albuginea.
The ovaries are surrounded by a thin fibrous capsule,
is lax, the ovary takes up a variable position in the pelvis.
abdominal cavity. After childbirth, when the broad ligament
nancy, the enlarging uterus pulls the ovary up into the
the rectouterine pouch (pouch of Douglas). During preg
extremely variable, and it is often found hanging down in
behind (see Fig. 7.18). The position of the ovary is, however,
external iliac vessels above and by the internal iliac vessels
bounded by the
ovarian fossa,
in a depression called the
-
the
epithelium.
the ovary becomes progressively scarred as successive
Before puberty, the ovary is smooth, but after puberty,
before birth from primordial germ cells.
because the layer does not give rise to ova. Oogonia develop
is a misnomer
germinal epithelium
The term
corpora lutea degenerate. After menopause, the ovary
right side and into the left renal vein on the left side.
The ovarian vein drains into the inferior vena cava on the
Veins
level of the 1st lumbar vertebra.
arises from the abdominal aorta at the
ovarian artery
The
Arteries
female.
in the sexually mature
progesterone,
estrogen
mones,
and the female sex hor
ova,
of the female germ cells, the
The ovaries are the organs responsible for the production
Function
becomes shrunken and its surface is pitted with scars.
-
and
Blood Supply
Basic Anatomy
281
mesonephric duct
anorectal canal
ureteric bud
allantois
allantois
bladder
urethra
ureter
remains of mesonephric duct
area of bladder and urethra formed
from mesonephric duct
urethra
bladder
ureter
Male
Female
urogenital sinus
primitive bladder
mesonephric duct
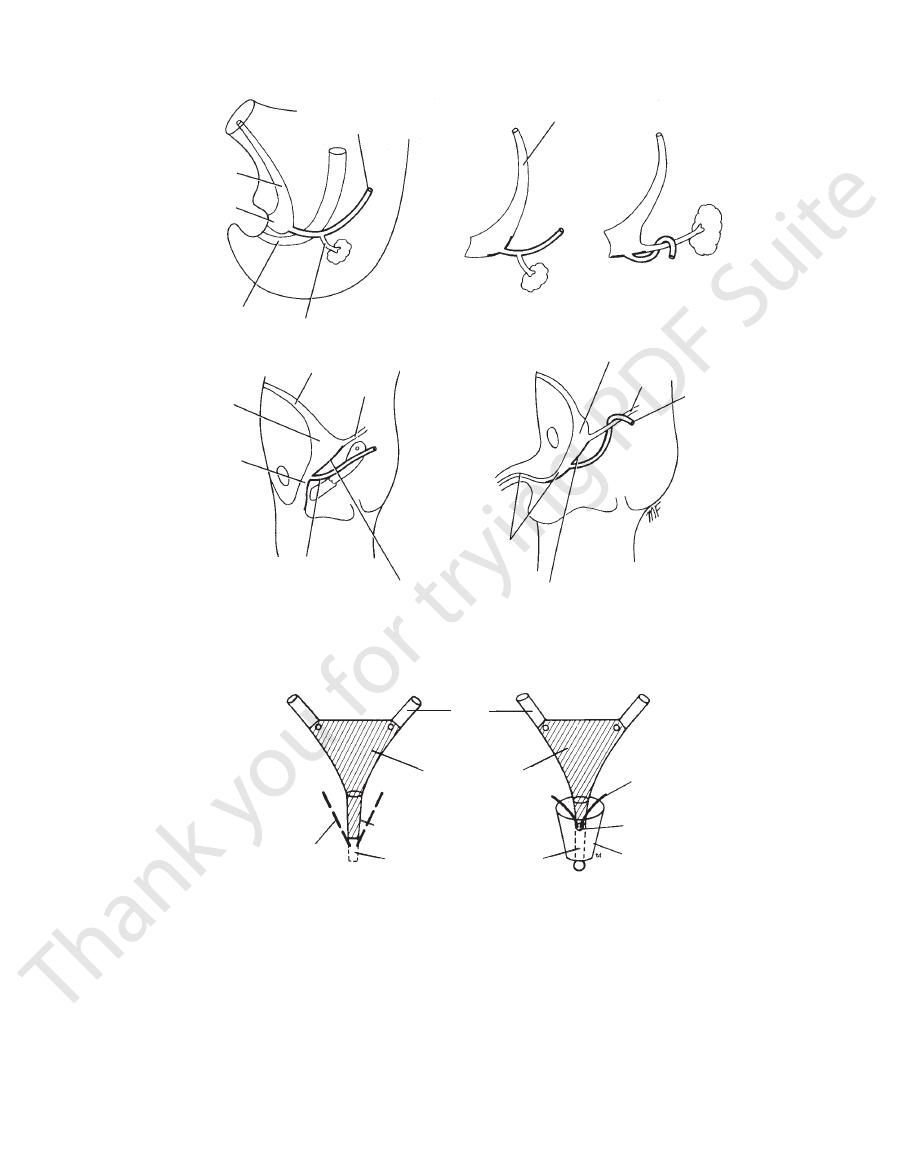
FIGURE 7.20
Formation of the urinary bladder from the anterior part of the cloaca and the terminal parts of the mesonephric
ducts in both sexes. The mesonephric ducts and the ureteric buds are drawn into the developing bladder.
ureter
trigone of bladder
urethra
derived from urogenital sinus
remains of mesonephric duct
forming Gartner's duct
mesonephric duct forming
ejaculatory duct
prostatic utricle
prostate gland
Female
Male
FIGURE 7.21
Parts of the bladder and urethra derived from the mesonephric ducts in both sexes (
drainage of the ovary with those of the testis.)
mesovarium. (Compare the blood supply and the lymph
sels and nerves finally enter the hilum of the ovary via the
known as the suspensory ligament of the ovary. The ves
ing through the lateral end of the broad ligament, the part
iliac vessels (see Fig. 7.19). They reach the ovary by pass
the ovary pass over the pelvic inlet and cross the external
The blood supply, lymph drainage, and nerve supply of
plexus and accompanies the ovarian artery.
The nerve supply to the ovary is derived from the aortic
Nerve Supply
lumbar vertebra.
and drain into the para-aortic nodes at the level of the 1st
The lymph vessels of the ovary follow the ovarian artery
Lymph Drainage
end of the urethra in the female and the lower part of the prostatic urethra in the male are formed from the urogenital sinus.
). The lower
hatch marks
-
-
282
CHAPTER 7
The Pelvis: Part II—The Pelvic Cavity
trigone of
bladder
ureteric
orfifices
epispadias
embryonic disc
primitive
streak
body stalk
cloacal
membrane
normal path
taken by
embryonic
mesenchyme
cloacal membrane
tail fold
absence of mesenchyme here
is responsible for exstrophy
of the bladder
umbilical cord
A
B
C
FIGURE 7.22
oped, but the mesenchyme has failed to enter the ventral body wall between the cloaca and the umbilical cord.
Fetus as seen from the side. The head and tail folds have devel
onic mesenchyme in the region of the cloaca is shown.
Dorsal view of the embryonic disc. The normal path taken by the growing embry
Exstrophy of the bladder.
A.
B.
-
C.
-
Position of the Ovary
ovarium. After pregnancy, the broad ligament is lax, and the
The ovary is kept in position by the broad ligament and the mes-
ovaries may prolapse into the rectouterine pouch (pouch of
Douglas). In these circumstances, the ovary may be tender and
cause discomfort on sexual intercourse (dyspareunia). An ovary
situated in the rectouterine pouch may be palpated through the
posterior fornix of the vagina.
Cysts of the Ovary
Follicular cysts are common and originate in unruptured graafian
follicles; they rarely exceed 0.6 in. (1.5 cm) in diameter. Luteal
cysts are formed in the corpus luteum. Fluid is retained, and
the corpus luteum cannot become fibrosed. Luteal cysts rarely
exceed 1.2 in. (3 cm) in diameter.
C L I N I C A L N O T E S
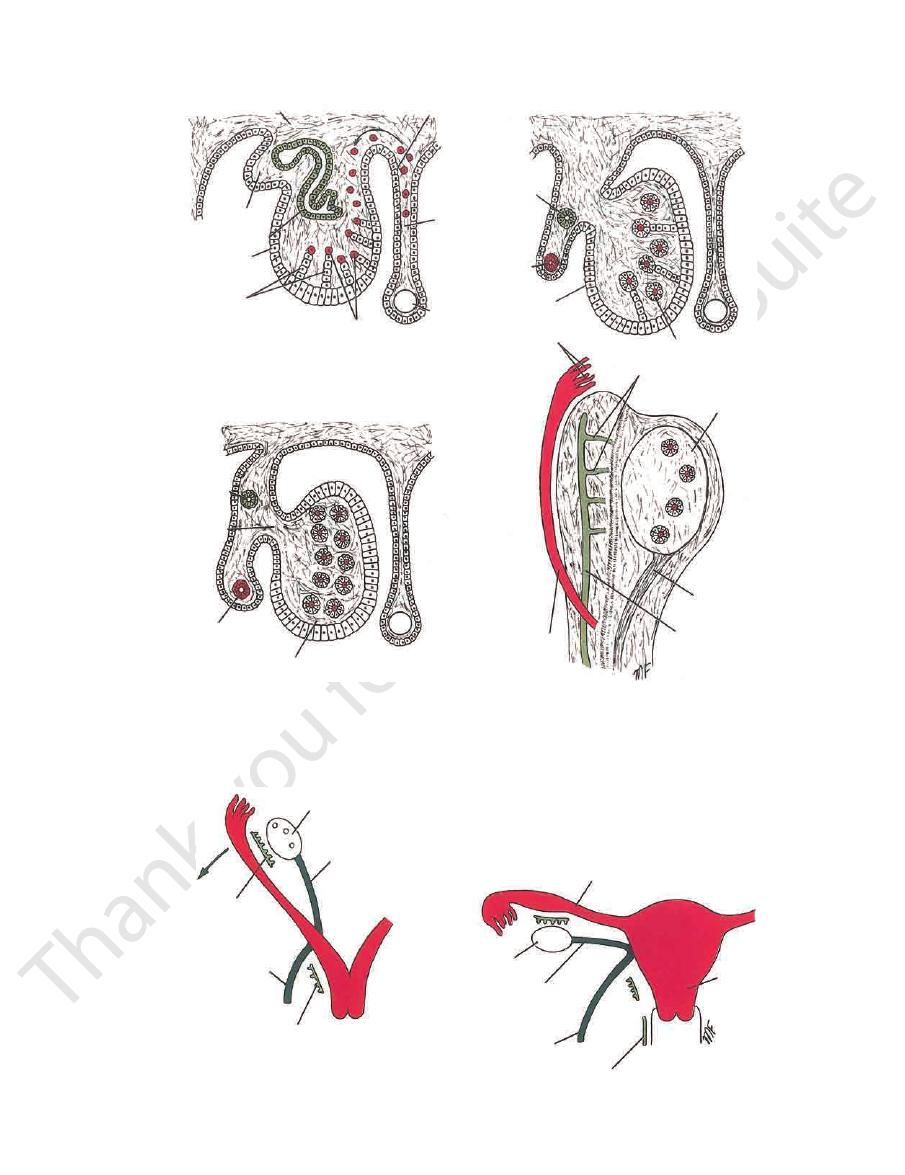
Development of the Ovary
posterior abdominal wall to secrete estrogens. The presence of
The female sex chromosome causes the genital ridge on the
estrogen and the absence of testosterone induce the develop-
ment of the ovary and the other female genital organs.
The sex cords contained within the genital ridges con-
tain groups of primordial germ cells. These become broken up
into irregular cell clusters by the proliferating mesenchyme
(Fig. 7.23). The germ cells differentiate into
primary oocytes become surrounded by a single layer of cells
oogonia, and by the
third month, they start to undergo a number of mitotic divisions
within the cortex of the ovary to form primary oocytes. These
derived from the sex cords, called the granulosa cells. Thus, pri-
mordial follicles
have been formed, but later, many degenerate.
The mesenchyme that surrounds the follicles provides the
ovarian stroma. The relationship of the ovary to the developing
The ovary may fail to descend into the pelvis or very rarely may
syndrome. The classic features of this syndrome are webbed
uterine tube is shown in Figure 7.24.
Ovarian Dysgenesis
Complete failure of both ovaries to develop is found in Turner’s
neck, short stocky build, increased carrying angle of the elbows,
lack of secondary sex characteristics, and amenorrhea.
Imperfect Descent of the Ovary
be drawn downward with the round ligament of the uterus into
the inguinal canal or even into the labium majus.
E M B R Y O L O G I C N O T E S
Basic Anatomy
283
posterior abdominal wall
mesonephros
mesonephric tubule
genital ridge
sex cords
gut
primordial sex cells
coelomic epithelium
dorsal mesentery
mesonephric duct
genital ridge
primordial follicle
mesonephric
duct
mesovarium
paramesonephric
duct
developing ovary
fimbria
mesonephric tubules
developing
ovary
gubernaculum
mesonephric duct
paramesonephric duct
A
B
C
D
papamesonephric
duct
FIGURE 7.23
Formation of the ovary and its relationship to the mesonephric and paramesonephric ducts.
ovary
round ligament
of the ovary
epoophoron
round ligament
of the uterus
paroophoron
uterine tube
ovary
round ligament
of the ovary
round ligament
of the uterus
Gartner's duct
uterus
A
B
FIGURE 7.24
The descent of the ovary and its relationship to the developing uterine tube and uterus.

284
CHAPTER 7
The Pelvis: Part II—The Pelvic Cavity
infundibulum
ampulla
isthmus
intramural part
fundus
uterine tube
cavity of uterus
body
internal os
supravaginal cervix
cervical canal
vaginal cervix
external os
vagina
lateral fornix
ureter
uterine artery
ovarian artery
fimbriae
90˚
170˚
A
B
C
D
FIGURE 7.25
is divided into four parts:
of the ovary with the cavity of the uterus. The uterine tube
and 7.19). Each connects the peritoneal cavity in the region
lie in the upper border of the broad ligament (see Figs. 7.18
The two uterine tubes are each about 4 in. (10 cm) long and
Location and Description
Uterine Tube
Anteverted and anteflexed position of the uterus.
Anteverted position of the uterus.
External os of the cervix:
Different parts of the uterine tube and the uterus.
A.
B.
(above) nulliparous; (below)
parous. C.
D.
1.
The
ovary (see Figs. 7.19 and 7.25).
which are draped over the
fimbriae,
processes, known as
ovary. The free edge of the funnel has several fingerlike
projects beyond the broad ligament and overlies the
is the funnel-shaped lateral end that
infundibulum
2.
The
is the widest part of the tube (see Fig. 7.25).
ampulla
3.
The
just lateral to the uterus (see Fig. 7.25).
is the narrowest part of the tube and lies
isthmus
4.
The
cular walls. In the young nulliparous adult, it measures 3 in.
The uterus is a hollow, pear-shaped organ with thick mus
Location and Description
hypogastric plexuses.
Sympathetic and parasympathetic nerves from the inferior
Nerve Supply
The internal iliac and para-aortic nodes.
Lymph Drainage
The veins correspond to the arteries.
Veins
ovarian artery from the abdominal aorta (see Fig. 7.25).
The uterine artery from the internal iliac artery and the
Arteries
travel to reach the ovum.
The tube serves as a conduit along which the spermatozoa
fertilized ovum and transports it to the cavity of the uterus.
(usually in the ampulla). It provides nourishment for the
vides a site where fertilization of the ovum can take place
The uterine tube receives the ovum from the ovary and pro
Function
uterine wall (see Fig. 7.25).
is the segment that pierces the
intramural part
-
Blood Supply
Uterus
-
