
Basic Anatomy
269
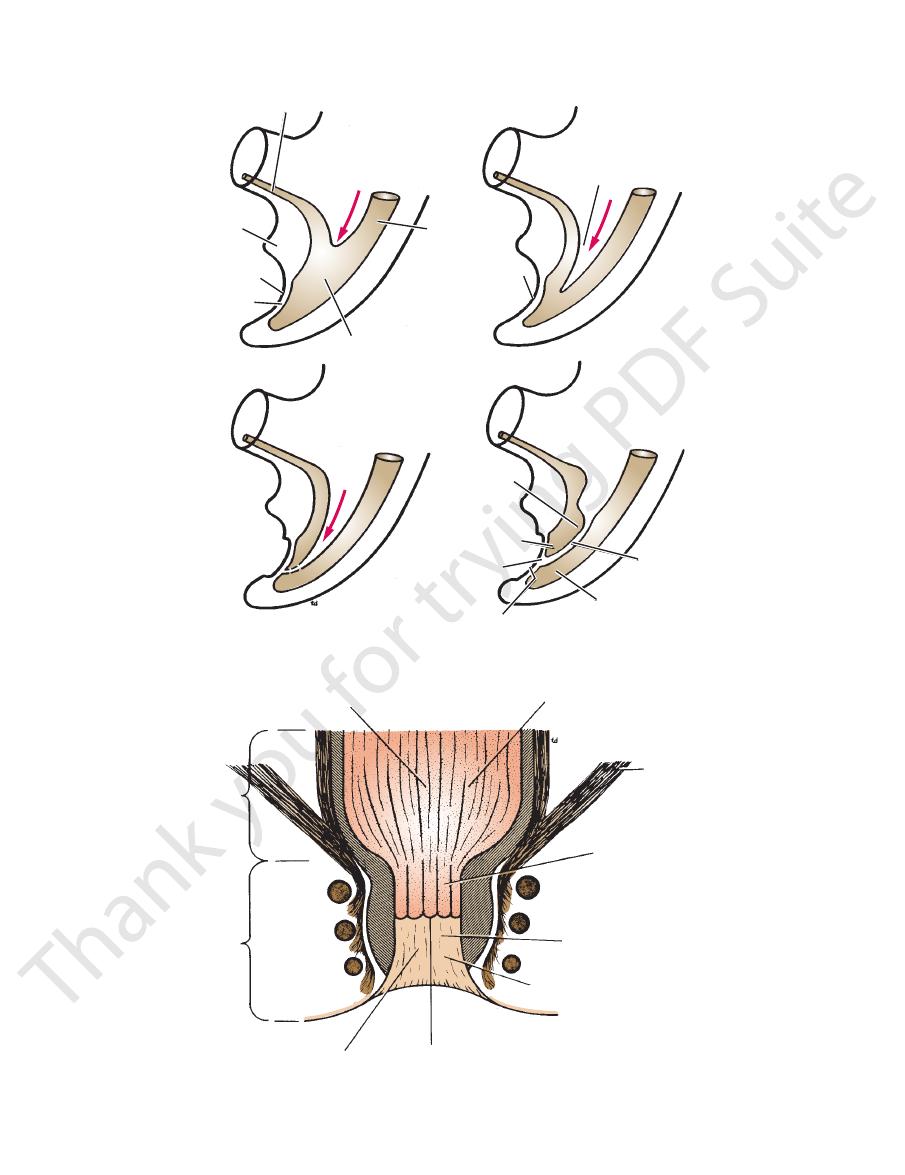
prolapse
of mucous
membrane
anus
external anal
sphincter
internal anal
sphincter
levator ani
peritoneum
mucous membrane
rectum
peritoneum
complete
prolapse
of rectal wall
internal anal
sphincter
external anal
sphincter
rectum
A
B
FIGURE 7.7
Coronal section of the rectum and anal canal.
is described on page 209.
to the posterior surface of the bladder. Its abdominal course
Each ureter is a muscular tube that extends from the kidney
vic cavity in the male are described in the following sections.
described above. The contents of the anterior part of the pel
occupy the posterior part of the pelvic cavity in both sexes, as
The rectum, sigmoid colon, and terminal coils of ileum
Pelvic Viscera in the Male
Complete rectal prolapse.
Incomplete rectal (mucosal) prolapse.
A.
B.
-
Ureters
to form the
treatment is operative excision of the aganglionic segment of
ment of the parasympathetic ganglion cells in this region. The
histologic examination reveals a complete failure of develop
stricted segment of the bowel that causes the obstruction, and
rectum and anal canal are constricted (Fig. 7.10). It is the con
sigmoid colon is greatly distended and hypertrophied, while the
nium, and the abdomen becomes enormously distended. The
during the first few days after birth. The child fails to pass meco
common in males than in females. Symptoms usually appear
Hirschsprung disease shows a familial tendency and is more
It starts to accumulate at
green in color and is called
gland secretions, bile, and amniotic fluid. This substance is dark
The lining of the inferior half of the anal canal is
anal canal.
Fig. 7.8). The fates of the primitive bladder and the urogenital
(see
On reaching the cloacal membrane, the urorectal
urogenital
the anterior part of
and divides the cloaca into anterior and posterior parts. The
of the mesenchyme, a septum is formed that grows inferiorly
chyme invaginates the entoderm. With continued proliferation
(see Fig. 7.8). In the interval
entodermal cloaca
between the allantois and the hindgut, a wedge of mesen-
septum is called the urorectal septum,
the cloaca becomes the primitive bladder and the
sinus, and the posterior part of the cloaca forms the anorec-
tal canal.
septum fuses with it and forms the future perineal body
sinus in both sexes are considered in detail on page 280.
The anorectal canal forms the rectum and the superior half of
the
formed from the ectoderm of the proctodeum (Fig. 7.9). The pos-
terior part of the cloacal membrane breaks down so that the gut
opens onto the surface of the embryo.
Hindgut Artery
The hindgut, which extends from the left colic flexure to half-
way down the anal canal, is supplied by the inferior mesenteric
artery (see Fig. 5.46). Here, a number of ventral branches of the
aorta fuse to form a single artery.
Meconium
At full term, the large intestine is filled with a mixture of intestinal
meconium.
4 months and reaches the rectum at the fifth month.
Primary Megacolon (Hirschsprung Disease)
-
-
-
the bowel.
270
CHAPTER 7
The Pelvis: Part II—The Pelvic Cavity
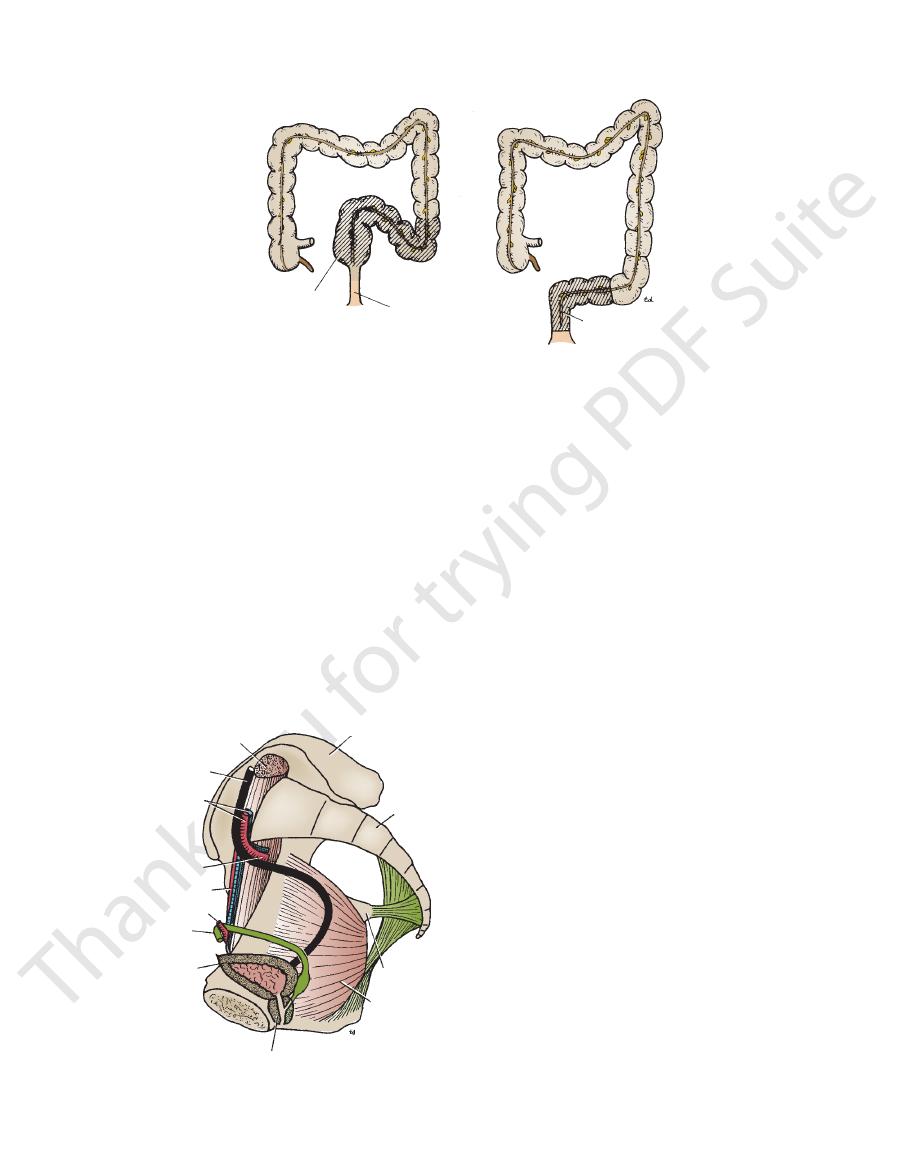
allantois
genital tubercle
proctodeum
cloacal membrane
hindgut
entodermal cloaca
direction of growth
of mesenchymal wedge
urorectal septum
proctodeum
primitive
bladder
urogenital sinus
perineal body
cloacal membrane
urorectal septum
anorectal canal
1
2
3
4
FIGURE 7.8
Progressive stages (
(the primitive bladder and the urogenital sinus) and a posterior part (the anorectal canal).
) in the formation of the urorectal septum, which divides the cloaca into an anterior part
1–4
columnar epithelium hindgut entoderm
rectum
anal canal
stratified squamous epithelium
proctodeum ectoderm
sensitive to distention
(autonomic nerves)
levator ani muscle
blood supply from
superior rectal vessels
(inferior mesenteric)
blood supply from
inferior rectal vessels
(internal iliac)
sensitive to all general sensations
(spinal nerves)
dentate line site of anal valves
embryologic site of cloacal membrane
FIGURE 7.9
Structure of the anal canal and its embryologic origin.
Basic Anatomy
271
distended and hypertrophied
sigmoid colon
constricted rectum
and anal canal
commonest area to find absence
of parasympathetic
ganglion cells
FIGURE 7.10
Main characteristics of primary megacolon (Hirschsprung disease).
tact with the anterior abdominal wall.
abdominal wall so that the bladder comes into direct con
toneal covering is peeled off the lower part of the anterior
surface bulges upward into the abdominal cavity. The peri
As the bladder fills, it becomes ovoid, and the superior
peritoneum passes to the lateral pelvic walls.
(see Fig. 7.4). Along the lateral margins of this surface, the
itoneum and is related to coils of ileum or sigmoid colon
of the bladder is covered with per
superior surface
The
vesicles, and the rectovesical fascia (see Fig. 7.4).
rated from the rectum by the vasa deferentia, the seminal
cal pouch. The lower part of the posterior surface is sepa
peritoneum, which forms the anterior wall of the rectovesi
part of the posterior surface of the bladder is covered by
seminal vesicles from each other (see Fig. 7.13). The upper
side on the posterior surface of the bladder and separate the
urethra (see Fig. 7.13). The two vasa deferentia lie side by
joined by the ureters, and the inferior angle gives rise to the
posteriorly and is triangular. The superolateral angles are
of the bladder, faces
posterior surface
or
The
(remains of urachus).
umbilical ligament
median
and 7.12). It is connected to the umbilicus by the
the upper margin of the symphysis pubis (see Figs. 7.4
of the bladder points anteriorly and lies behind
apex
The
it also has a neck.
apex, a base, and a superior and two inferolateral surfaces;
The empty bladder is pyramidal (Fig. 7.13), having an
to take up the adult position.
the pelvic cavity enlarges, the bladder sinks into the pelvis
empty bladder projects above the pelvic inlet; later, when
the hypogastric region (Fig. 7.12). In the young child, the
the pelvis; as the bladder fills, its superior wall rises up into
tains. The empty bladder in the adult lies entirely within
tions vary according to the amount of urine that it con
The bladder has a strong muscular wall. Its shape and rela
and in the adult has a maximum capacity of about 500 mL.
pubic bones (see Fig. 7.4) within the pelvis. It stores urine
The urinary bladder is situated immediately behind the
Location and Description
the ureter are described on page 211.
The blood supply, lymph drainage, and nerve supply of
pierces the bladder wall.
as it crosses the pelvic brim to enter the pelvis, and where it
pelvis joins the ureter in the abdomen, where it is kinked
The ureter possesses three constrictions: where the renal
Constrictions
into the bladder.
of the bladder for about 0.75 in. (1.9 cm) before opening
vas deferens. The ureter passes obliquely through the wall
bladder (Fig. 7.11). Near its termination, it is crossed by the
spine and turns forward to enter the lateral angle of the
front of the internal iliac artery to the region of the ischial
Each ureter then runs down the lateral wall of the pelvis in
of the common iliac artery in front of the sacroiliac joint.
The ureter enters the pelvis by crossing the bifurcation
Urinary Bladder
-
-
base,
-
-
-
-
-
psoas
ilium
sacrum
ischial spine
obturator
internus
prostate
bladder
vas deferens
inferior epigastric artery
external iliac artery
internal iliac artery
common iliac
vessels
ureter
FIGURE 7.11
Right half of the pelvis showing relations of
the ureter and vas deferens.

272
CHAPTER 7
The Pelvis: Part II—The Pelvic Cavity
peritoneum
body of
pubis
ureter
urethra
apex of bladder
interureteric crest
left ureter
left ureteric
orifice
trigone
urethral orifice
uvula vesicae
right ureter
cut bladder
wall
A
B
superior wall
of bladder
FIGURE 7.12
bladder is peeled off from the anterior abdominal wall as the
that the peritoneum covering the superior surface of the
superior wall rises as the viscus fills with urine. Note also
Lateral view of the bladder. Note that the
A.
bladder fills. B. Interior of the bladder in the male as seen
from in front.
superior surface
of bladder
left ureter
prostate
membranous
part of urethra
neck of bladder
apex of bladder
left ureter
superior
surface of bladder
right ureter
right
vas deferens
ampulla of
vas deferens
right
seminal vesicle
posterior surface of
prostate
membranous part of
urethra
left
seminal vesicle
left
vas deferens
A
B
left
seminal vesicle
left
vas deferens
FIGURE 7.13
is composed of
muscular coat of the bladder
The
lobe of the prostate.
thral orifice, which is produced by the underlying median
is a small elevation situated immediately behind the ure
uvula vesicae
The
interureteric ridge.
and is known as the
runs from the opening of one ureter to that of the other
The trigone is limited above by a muscular ridge, which
as the bladder fills.
which prevents a reverse flow of urine toward the kidneys
bladder wall obliquely, and this provides a valvelike action,
nal urethral orifice (see Fig. 7.12). The ureters pierce the
openings of the ureters, and the inferior angle to the inter
The superior angles of the trigone correspond to the
brane is firmly adherent to the underlying muscular coat.
viscus is empty (see Fig. 7.12), because the mucous mem
the mucous membrane is always smooth, even when the
Here,
trigone.
surface of the base of the bladder is called the
is full. The area of mucous membrane covering the internal
bladder is thrown into folds that disappear when the bladder
of the greater part of the empty
mucous membrane
The
vious paragraphs.
rior surface rises into the abdomen, as described in the pre
remain more or less unchanged in position, but the supe
When the bladder fills, the posterior surface and neck
ligaments are thickenings of the pelvic fascia.
in the female. These
pubovesical ligaments
are called the
in the male; these
puboprostatic ligaments
position by the
with those of the prostate. The neck of the bladder is held in
smooth muscle fibers of the bladder wall are continuous
upper surface of the prostate (see Fig. 7.13). Here, the
of the bladder lies inferiorly and rests on the
neck
The
above and the levator ani muscle below.
orly, they lie in contact with the obturator internus muscle
and the pubic bones. More posteri
retropubic pad of fat
are related in front to the
inferolateral surfaces
The
tate, vasa deferentia, and seminal vesicles.
Posterior view of the bladder, pros
left seminal vesicle.
Lateral view of the bladder, prostate, and
A.
B.
-
-
-
-
-
-
-
smooth muscle and is arranged as three layers of interlacing
Internal and external iliac nodes.
Lymph Drainage
the internal iliac vein.
that drains into
vesical venous plexus
The veins form the
Veins
internal iliac arteries.
The superior and inferior vesical arteries, branches of the
Arteries
sphincter vesicae.
ened to form the
bladder, the circular component of the muscle coat is thick
At the neck of the
detrusor muscle.
bundles known as the
-
Blood Supply
Basic Anatomy
the first and second lumbar segments of the spinal cord.
sympathetic nerves via the hypogastric plexuses and enter
vic splanchnic nerves. Some afferent fibers travel with the
in the bladder reach the central nervous system via the pel
postganglionic neurons. Most afferent sensory fibers arising
plexuses to reach the bladder wall, where they synapse with
sacral nerves; they pass through the inferior hypogastric
pelvic splanchnic nerves from the second, third, and fourth
uses. The parasympathetic preganglionic fibers arise as the
ganglia and descend to the bladder via the hypogastric plex
ganglionic fibers originate in the 1st and 2nd lumbar
The inferior hypogastric plexuses. The sympathetic post
Nerve Supply
273
-
-
-
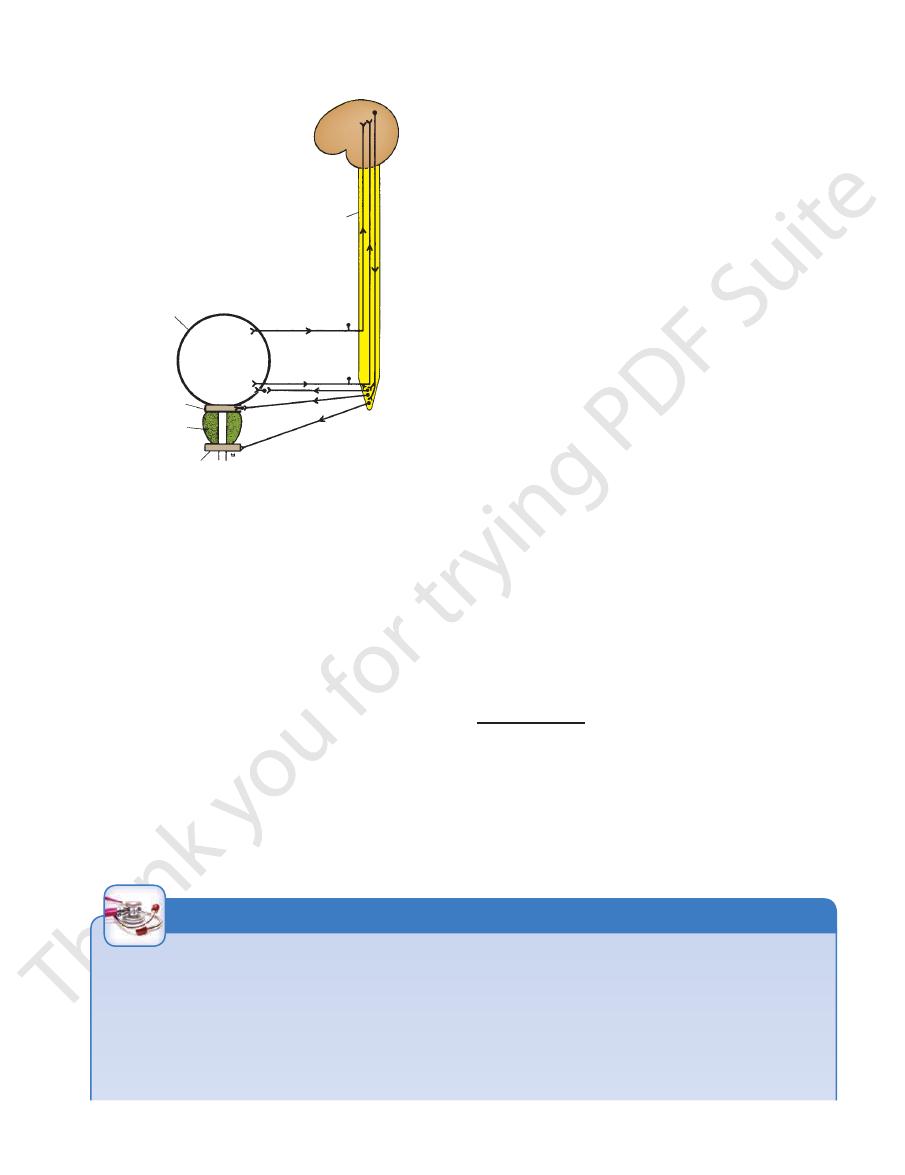
bladder wall
spinal cord
L1 and 2
S2, 3, and 4
sphincter urethrae
prostate
sphincter vesicae
FIGURE 7.14
Nervous control of the bladder. Sympathetic
rusor muscle of the bladder wall and stimulate closure of
The sympathetic nerves* inhibit contraction of the det
fibers have been omitted for simplification.
-
the sphincter vesicae. The parasympathetic nerves stimulate
the second, third, and fourth sacral segments and pass
Efferent parasympathetic impulses leave the cord from
second lumbar segments of the spinal cord.
nerves via the hypogastric plexuses and enter the first and
7.14). Some afferent impulses travel with the sympathetic
the 2nd, 3rd, and 4th sacral segments of the spinal cord (Fig.
ent impulses pass up the pelvic splanchnic nerves and enter
individual has a conscious desire to micturate. Most affer
transmit impulses to the central nervous system, and the
stretch receptors in the bladder wall are stimulated and
is initiated when the volume of urine reaches about 300 mL;
vidual, is controlled by higher centers in the brain. The reflex
Micturition is a reflex action that, in the toilet-trained indi
Micturition
inhibit the action of the sphincter vesicae.
contraction of the detrusor muscle of the bladder wall and
-
-
via the parasympathetic preganglionic nerve fibers through
adult, this simple stretch reflex is inhibited by the activity
takes place whenever the bladder becomes distended. In the
In young children, micturition is a simple reflex act and
pelvic pressures and exert external pressure on the bladder.
the abdominal muscles to raise the intra-abdominal and
reflex action. Micturition can be assisted by contraction of
pass to the spinal cord from the urethra and reinforce the
Once urine enters the urethra, additional afferent impulses
pudendal nerve (S2, 3, and 4), and this undergoes relaxation.
Efferent impulses also pass to the urethral sphincter via the
made to contract, and the sphincter vesicae is made to relax.
smooth muscle of the bladder wall (the detrusor muscle) is
ganglionic neurons. By means of this nervous pathway, the
plexuses to the bladder wall, where they synapse with post
the pelvic splanchnic nerves and the inferior hypogastric
-
* The sympathetic nerves to the detrusor muscle are now thought to
entering the bladder.
about by sympathetic action), thus preventing seminal fluid from
active contraction of the bladder neck during ejaculation (brought
ever, in males, the sympathetic innervation of the sphincter causes
contraction of the sphincter in maintaining urinary continence. How
the sphincter vesicae are thought to play only a minor role in causing
are distributed mainly to the blood vessels. The sympathetic nerves to
have little or no action on the smooth muscle of the bladder wall and
-
Ureteric Calculi
der. In the male, one hand is placed on the anterior abdominal
of the empty bladder with or without a
Bimanual palpation
The full bladder in the adult projects up into the abdomen and
Ureteric calculi are discussed on page 212. The ureter is nar-
rowed anatomically where it bends down into the pelvis at the
pelvic brim and where it passes through the bladder wall. It is at
these sites that urinary stones may be arrested.
When a calculus enters the lower pelvic part of the ureter,
the pain is often referred to the testis and the tip of the penis in
the male and the labium majus in the female.
Palpation of the Urinary Bladder
may be palpated through the anterior abdominal wall above the
symphysis pubis.
general anesthetic is an important method of examining the blad-
wall above the symphysis pubis, and the gloved index finger of
C L I N I C A L N O T E S
(continued)
Basic Anatomy
without interruption from one organ to the other. The
the neck of the bladder, the smooth muscle passing
The base of the prostate is continuous with
Superiorly:
Relations
margins of the prostatic utricle (see Fig. 7.16).
the prostate to open into the prostatic urethra at the lateral
tory ducts pierce the upper part of the posterior surface of
against the urogenital diaphragm below. The two ejacula
which lies
apex,
lies against the bladder neck above, and an
which
Fig. 7.16). The somewhat conical prostate has a
The prostate is surrounded by a fibrous capsule (see
above and the urogenital diaphragm below (see Fig. 7.16).
1.25 in. (3 cm) long and lies between the neck of the bladder
rounds the prostatic urethra (see Figs. 7.4 and 7.16). It is about
The prostate is a fibromuscular glandular organ that sur
Location and Description
the prostatic urethra.
tatic utricle; their function is to drain the seminal fluid into
static part of the urethra, close to the margins of the pros
the posterior surface of the prostate and open into the pro
the seminal vesicle (Fig. 7.16). The ejaculatory ducts pierce
are formed by the union of the vas deferens and the duct of
The two ejaculatory ducts are each <1 in. (2.5 cm) long and
thus washing the spermatozoa out of the urethra.
contract and expel their contents into the ejaculatory ducts,
the spermatozoa. During ejaculation, the seminal vesicles
that is added to the seminal fluid. The secretions nourish
The function of the seminal vesicles is to produce a secretion
Function
The internal iliac nodes.
Lymph Drainage
The veins drain into the internal iliac veins.
Veins
The inferior vesicle and middle rectal arteries.
Arteries
embedded in connective tissue.
Each seminal vesicle consists of a much-coiled tube
ejaculatory duct.
the same side to form the
each seminal vesicle narrows and joins the vas deferens of
vesicles are related to the rectum (see Fig. 7.4). Inferiorly,
terminal part of the vas deferens. Posteriorly, the seminal
(see Fig. 7.13). On the medial side of each vesicle lies the
(5 cm) long lying on the posterior surface of the bladder
The seminal vesicles are two lobulated organs about 2 in.
Seminal Vesicles
ejaculatory duct.
the duct of the seminal vesicle to form the
The inferior end of the ampulla narrows down and joins
ampulla of the vas deferens.
deferens is dilated to form the
of the bladder (see Fig. 7.11). The terminal part of the vas
275
Blood Supply
Ejaculatory Ducts
-
-
Prostate
-
base,
-
■
■
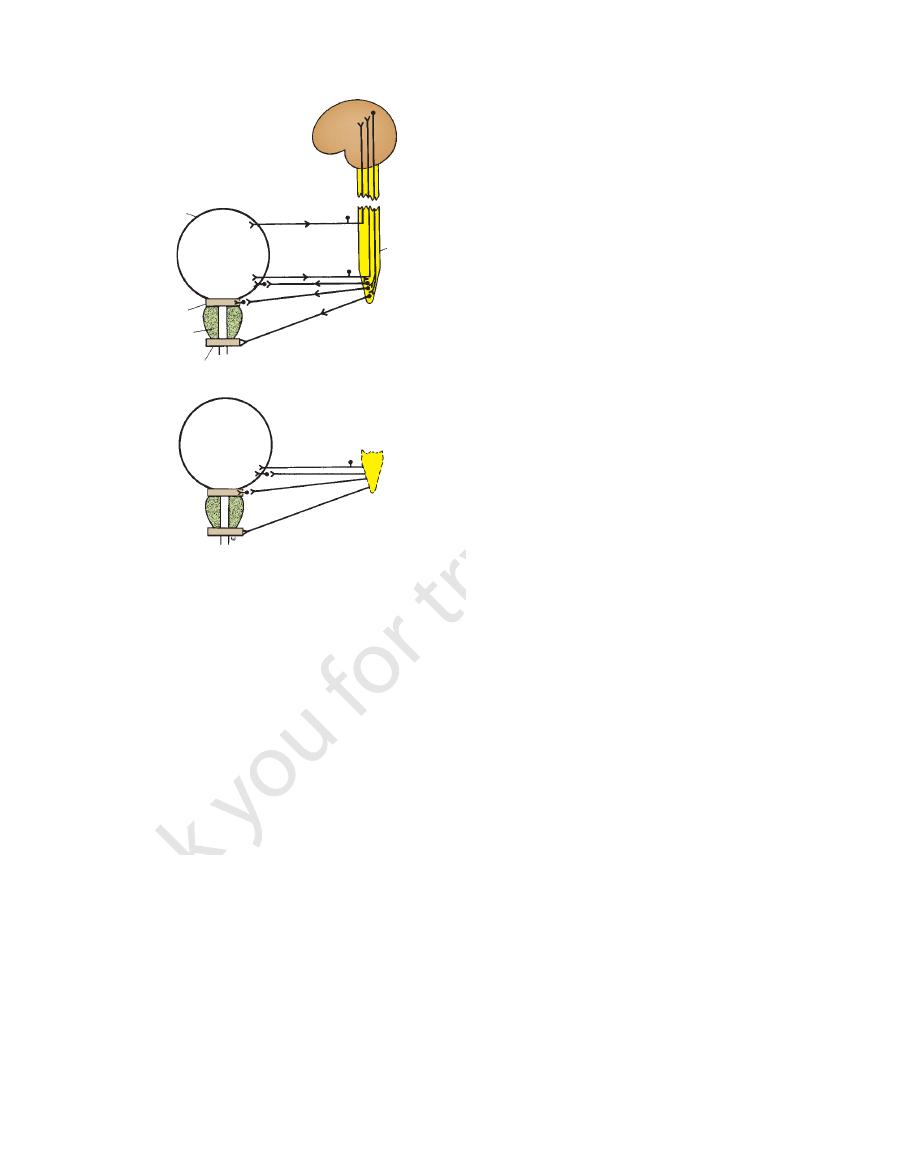
bladder wall
sphincter vesicae
prostate
sphincter urethrae
spinal cord
A
B
FIGURE 7.15
then runs medially and downward on the posterior surface
the ureter in the region of the ischial spine. The vas deferens
and backward on the lateral wall of the pelvis and crosses
epigastric artery (see Fig. 7.11). It then passes downward
nal ring and passes around the lateral margin of the inferior
through the inguinal canal. It emerges from the deep ingui
from the lower end or tail of the epididymis and passes
epididymis to the ejaculatory duct and the urethra. It arises
(45 cm) long that conveys mature sperm from the
The vas deferens is a thick-walled tube about 18 in.
Vas Deferens
are described on page 131.
epididymides
testes
The
during the second or third year of life.
Voluntary control of micturition is normally developed
which compresses the bladder neck.
closes the urethra; this is assisted by the sphincter vesicae,
accomplished by contracting the sphincter urethrae, which
segments of the cord. Voluntary control of micturition is
with the corticospinal tracts to the 2nd, 3rd, and 4th sacral
rition are favorable. The inhibitory fibers pass downward
of the cerebral cortex until the time and place for mictu
omitted for clarity.
to the bladder are shown; the sympathetic fibers have been
ous system and the parasympathetic efferent fibers passing
sensory fibers from the bladder entering the central nerv
The afferent
of the spinal cord in the upper thoracic region. Destruction
Nervous control of the bladder after section
A.
of the sacral segments of the spinal cord. B.
-
-
Male Genital Organs
and
-
