Basic Anatomy
The
ductus venosus close and become fibrous cords.
joins the inferior vena cava. At birth, the umbilical vein and
liver in the ductus venosus (ligamentum venosum) and
teres). The greater proportion of the blood bypasses the
is brought to the liver in the umbilical vein (ligamentum
cava (Figs. 5.8 and 5.22). In the fetus, oxygenated blood
face of the liver to be attached above to the inferior vena
portal vein and ascends in a fissure on the visceral sur
is attached to the left branch of the
ductus venosus,
of the
a fibrous band that is the remains
ligamentum venosum,
portal vein in the porta hepatis (Figs. 5.9 and 5.22). The
ceral surface of the liver and joins the left branch of the
passes into a fissure on the vis
ligamentum teres
The
(Fig. 5.8).
bare area of the liver
of liver devoid of peritoneum. Such an area is referred to as
the coronary ligament are widely separated, leaving an area
liver. It should be noted that the peritoneal layers forming
of the
right triangular ligament
ligament is known as the
(Fig. 5.8). The right extremity of the coronary
lar ligament
left triangu
the left layer forms the upper layer of the
ment;
coronary liga
The right layer forms the upper layer of the
superior surfaces of the liver and then splits into two layers.
falciform ligament passes on to the anterior and then the
the ligamentum teres, the remains of the umbilical vein. The
(Fig. 5.8). It has a sickle-shaped free margin that contains
the peritoneum, ascends from the umbilicus to the liver
which is a two-layered fold of
falciform ligament,
The
Peritoneal Ligaments of the Liver
and esophagus and fundus of the stomach
of the colon, duodenum, gallbladder, inferior vena cava,
Diaphragm, right kidney, hepatic flexure
Posteriorly:
costal angle
xiphoid process, and anterior abdominal wall in the sub
right and left pleura and lower margins of both lungs,
Diaphragm, right and left costal margins,
Anteriorly:
Important Relations
into the central vein.
and drains
sinusoids
between the liver cells by means of
duct (portal triad). The arterial and venous blood passes
of the hepatic artery, portal vein, and a tributary of a bile
which contain branches
portal canals,
the lobules are the
is a tributary of the hepatic veins. In the spaces between
of each lobule
central vein
The
liver lobules.
made up of
sule but only partially covered by peritoneum. The liver is
The liver is completely surrounded by a fibrous cap
lymph nodes.
and gallbladder and send their efferent vessels to the celiac
A few hepatic lymph nodes lie here; they drain the liver
sympathetic and parasympathetic nerve fibers (Fig. 5.47).
and left branches of the hepatic artery, the portal vein, and
margins. In it lie the right and left hepatic ducts, the right
of the free edge of the lesser omentum is attached to its
and quadrate lobes (Figs. 5.8 and 5.9). The upper part
the posteroinferior surface and lies between the caudate
or hilum of the liver, is found on
porta hepatis,
The
two sides overlap very little.
quadrate plus caudate lobes), respectively. Apparently, the
ducts, are distributed to the right lobe and the left lobe (plus
hepatic artery and portal vein, and the right and left hepatic
lobe of the liver. Thus, the right and left branches of the
quadrate and caudate lobes are a functional part of the left
tum venosum. Experiments have shown that, in fact, the
teres, the inferior vena cava, and the fissure for the ligamen
presence of the gallbladder, the fissure for the ligamentum
by the
caudate lobe
and a
quadrate lobe
divided into a
the falciform ligament (Fig. 5.8). The right lobe is further
by the attachment of the peritoneum of
left lobe
a small
right lobe
The liver may be divided into a large
nal gland, and the gallbladder.
num, the right colic flexure, the right kidney and suprare
abdominal part of the esophagus, the stomach, the duode
is therefore irregular in shape; it lies in contact with the
is molded to adjacent viscera and
visceral surface,
or
rior,
posteroinfe
surface of the domes of the diaphragm. The
convex upper surface of the liver is molded to the under
197
-
-
-
-
and
-
-
■
■
-
■
■
-
-
a
-
-
hepatis.
into right and left terminal branches that enter the porta
The hepatic artery, a branch of the celiac artery, divides
Arteries
passes down to the lesser curvature of the stomach (Fig. 5.10).
hepatis and the fissure for the ligamentum venosum and
arises from the edges of the porta
lesser omentum
Blood Supply
plicae circulares
jejunum
small intestine
ileum
colon
Peyer's patch
smooth mucous membrane
teniae coli
appendices
epiploicae
teniae coli
large intestine
sacculations
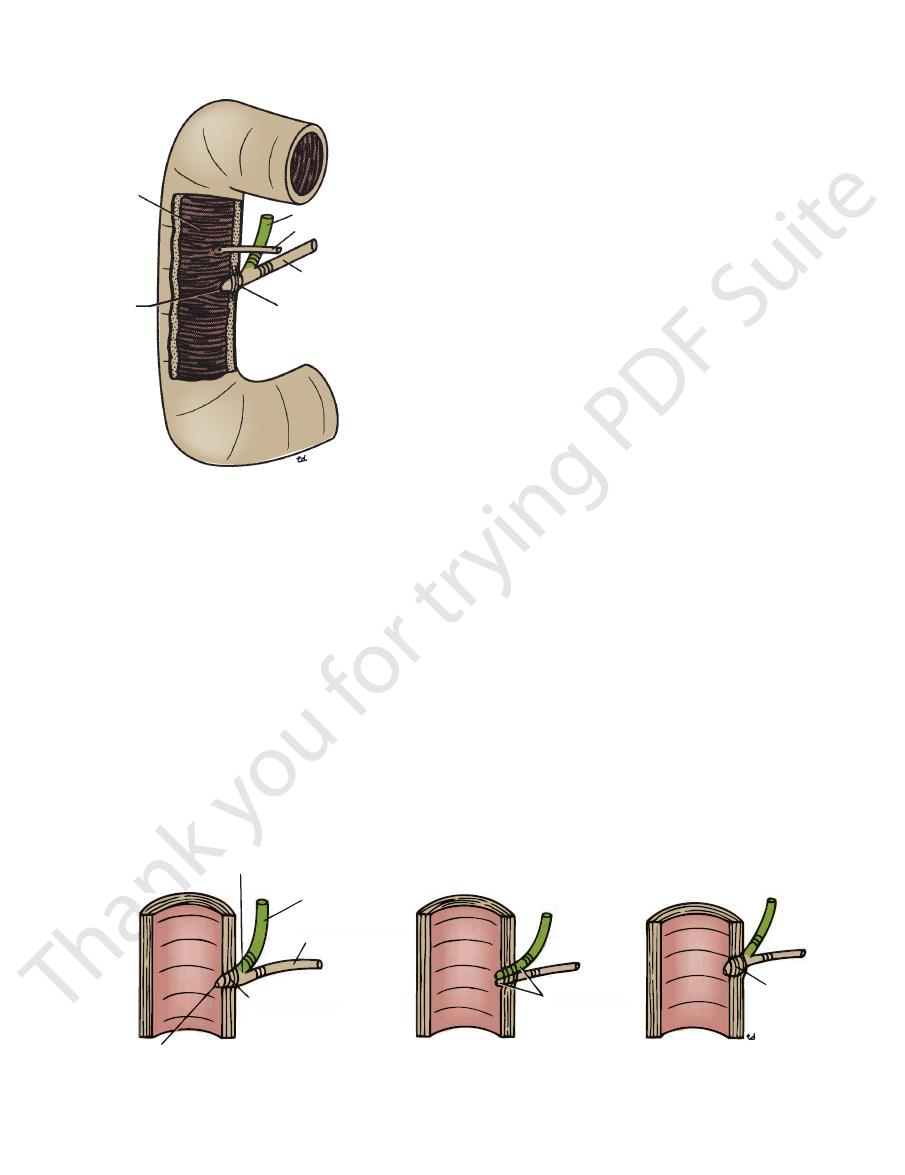
FIGURE 5.50
Some external and internal differences
between the small and large intestine.
198
CHAPTER 5
it lies in a groove on the posterior surface of the head of the
troduodenal artery (Fig. 5.4). In the third part of its course,
first part of the duodenum (Fig. 5.7) to the right of the gas
In the second part of its course, it is situated behind the
portal vein and on the right of the hepatic artery (Fig. 5.11).
the lesser sac. Here, it lies in front of the right margin of the
margin of the lesser omentum in front of the opening into
long. In the first part of its course, it lies in the right free
The bile duct (common bile duct) is about 3 in. (8 cm)
gallbladder to form the bile duct (Fig. 5.29).
tum. It is joined on the right side by the cystic duct from the
and descends within the free margin of the lesser omen
is about 1.5 in. (4 cm) long
common hepatic duct
The
hepatic duct (Fig. 5.29).
short course, the hepatic ducts unite to form the common
left lobes of the liver in the porta hepatis (Fig. 5.47). After a
The right and left hepatic ducts emerge from the right and
lobe.
left duct drains the left lobe, caudate lobe, and quadrate
right hepatic duct drains the right lobe of the liver and the
porta hepatis, form the right and left hepatic ducts. The
to form progressively larger ducts and, eventually, at the
the bile canaliculi. The interlobular ducts join one another
are situated in the portal canals of the liver; they receive
The smallest interlobular tributaries of the bile ducts
cystic duct.
and the
gallbladder,
bile duct,
mon hepatic duct,
com
the
left hepatic ducts,
and
right
liver consist of the
it is delivered to the duodenum. The bile ducts of the
bile is stored and concentrated in the gallbladder; later,
40 mL per hour. When digestion is not taking place, the
Bile is secreted by the liver cells at a constant rate of about
branch, which passes directly to the liver.
plexus. The anterior vagal trunk gives rise to a large hepatic
Sympathetic and parasympathetic nerves form the celiac
Nerve Supply
to the posterior mediastinal lymph nodes.
pass from the bare area of the liver through the diaphragm
The efferent vessels pass to the celiac nodes. A few vessels
the liver and enter several lymph nodes in the porta hepatis.
third to one half of all body lymph. The lymph vessels leave
The liver produces a large amount of lymph—about one
Lymph Drainage
directly into the inferior vena cava.
and these leave the posterior surface of the liver and open
The central veins drain into the right and left hepatic veins,
the central vein of each liver lobule by the liver sinusoids.
tinal tract. The arterial and venous blood is conducted to
digestion, which have been absorbed from the gastrointes
the portal vein brings venous blood rich in the products of
hepatic artery brings oxygenated blood to the liver, and
are the hepatic artery (30%) and portal vein (70%). The
The blood vessels (Fig. 5.47) conveying blood to the liver
Blood Circulation through the Liver
the liver and drain into the inferior vena cava.
(three or more) emerge from the posterior surface of
veins
hepatic
that enter the porta hepatis behind the arteries. The
The portal vein divides into right and left terminal branches
Veins
The Abdomen: Part II—The Abdominal Cavity
-
Bile Ducts of the Liver
-
the
the
Hepatic Ducts
-
Bile Duct
-
Liver Supports and Surgery
nied by a loss of liver dullness caused by the accumulation of gas
dull on percussion. Perforation of a gastric ulcer is often accompa
the peritoneal surfaces. The anterior surface of the liver is normally
abnormal accumulation of gas or fluid is necessary for separation of
potential spaces only, and the peritoneal surfaces are in contact. An
are described on page 163. Under normal conditions, these are
The important subphrenic spaces and their relationship to the liver
hepatic arteries, and portal vein are distributed in a segmental
or upper abdomen are common causes of liver injury. Blunt trau
surgically because even if the peritoneal ligaments are cut, the
cava. The peritoneal ligaments and the tone of the abdominal
cavity by the attachment of the hepatic veins to the inferior vena
The liver is held in position in the upper part of the abdominal
muscles play a minor role in its support. This fact is important
liver can be only slightly rotated.
Liver Trauma
The liver is a soft, friable structure enclosed in a fibrous cap-
sule. Its close relationship to the lower ribs must be emphasized.
Fractures of the lower ribs or penetrating wounds of the thorax
-
matic injuries from automobile accidents are also common, and
severe hemorrhage accompanies tears of this organ.
Because anatomic research has shown that the bile ducts,
manner, appropriate ligation of these structures allows the sur-
geon to remove large portions of the liver in patients with severe
traumatic lacerations of the liver or with a liver tumor. (Even
large, localized carcinomatous metastatic tumors have been
successfully removed.)
Liver Biopsy
Liver biopsy is a common diagnostic procedure. With the patient
holding his or her breath in full expiration—to reduce the size of
the costodiaphragmatic recess and the likelihood of damage to
the lung—a needle is inserted through the right 8th or 9th inter-
costal space in the midaxillary line. The needle passes through
the diaphragm into the liver, and a small specimen of liver tissue
is removed for microscopic examination.
Subphrenic Spaces
-
over the anterior surface of the liver and in the subphrenic spaces.
C L I N I C A L N O T E S
Basic Anatomy
cle around the distal end of the bile duct and the ampulla is
gallbladder to contract. At the same time, the smooth mus
denum; the hormone then enters the blood, causing the
from the mucous membrane of the duo
cholecystokinin
the duodenum. The fat causes release of the hormone
mechanism is initiated by the entrance of fatty foods into
traction and partial emptying of the gallbladder. This
Bile is delivered to the duodenum as the result of con
microvilli on their free surface.
ance. The columnar cells lining the surface have numerous
each other, giving the surface a honeycombed appear
membrane is thrown into permanent folds that unite with
and secretes mucus. To aid in these functions, the mucous
absorbs bile salts, keeping the bile acid; excretes cholesterol;
The gallbladder concentrates bile; stores bile; selectively
remains closed and bile accumulates in the gallbladder.
When digestion is not taking place, the sphincter of Oddi
Function of the Gallbladder
ond parts of the duodenum (Fig. 5.29)
The transverse colon and the first and sec
Posteriorly:
rior surface of the liver (Fig. 5.2)
The anterior abdominal wall and the infe
Anteriorly:
Relations
face of the liver.
gallbladder and binds the body and neck to the visceral sur
The peritoneum completely surrounds the fundus of the
(Fig. 5.29).
to join the common hepatic duct, to form the bile duct
with the cystic duct, which turns into the lesser omentum
becomes continuous
neck
backward, and to the left. The
with the visceral surface of the liver and is directed upward,
lies in contact
body
tip of the 9th right costal cartilage. The
contact with the anterior abdominal wall at the level of the
below the inferior margin of the liver, where it comes in
is rounded and projects
fundus
dus, body, and neck. The
absorbing water. The gallbladder is divided into the fun
of 30 to 50 mL and stores bile, which it concentrates by
face of the liver (Figs. 5.8, 5.9, and 5.29). It has a capacity
The gallbladder is a pear-shaped sac lying on the undersur
Location and Description
Figure 5.52.
common variations of this arrangement are shown in
pancreatic ducts open separately into the duodenum. The
(Fig. 5.51). Occasionally, the bile and
(sphincter of Oddi)
sphincter of the hepatopancreatic ampulla
known as the
ducts and the ampulla are surrounded by circular muscle,
(Fig. 5.51). The terminal parts of both
duodenal papilla
major
of the duodenum by means of a small papilla, the
The ampulla opens into the lumen
(ampulla of Vater).
hepatopancreatic ampulla
the duodenal wall, called the
atic duct, and together they open into a small ampulla in
length (Fig. 5.51). It is usually joined by the main pancre
the second part of the duodenum about halfway down its
The bile duct ends below by piercing the medial wall of
with the main pancreatic duct.
pancreas (Fig. 5.29). Here, the bile duct comes into contact
199
-
Gallbladder
-
-
-
■
■
-
■
■
-
-
-
-
-
plicae
circulares
major
duodenal
papilla
sphincter of Oddi
(sphincter of the
hepatopancreatic ampulla)
bile duct
accessory pancreatic duct
main pancreatic duct
FIGURE 5.51
Terminal parts of the bile and pancreatic ducts
as they enter the second part of the duodenum. Note the
sphincter of Oddi and the smooth muscle around the ends
of the bile duct and the main pancreatic duct.
combined ducts
bile duct
main pancreatic duct
sphincter of Oddi
major duodenal papilla
separate ducts
ampulla of
Vater
bile duct
main pancreatic duct
sphincter of Oddi
separate ducts
ampulla
Vater
FIGURE 5.52
Three common variations of terminations of the bile and main pancreatic ducts as they enter the second part of
the duodenum.
200
CHAPTER 5
form a spiral fold that is continuous with a similar fold in
The mucous membrane of the cystic duct is raised to
free margin of the lesser omentum.
S-shaped and descends for a variable distance in the right
to form the bile duct (Fig. 5.29). It usually is somewhat
the neck of the gallbladder to the common hepatic duct
is about 1.5 in. (3.8 cm) long and connects
cystic duct
The
food from the stomach.
mucous membrane of the duodenum on the arrival of fatty
the hormone cholecystokinin, which is produced by the
celiac plexus. The gallbladder contracts in response to
Sympathetic and parasympathetic vagal fibers form the
artery and then to the celiac nodes.
pass to the hepatic nodes along the course of the hepatic
the neck of the gallbladder. From here, the lymph vessels
situated near
cystic lymph node
The lymph drains into a
Lymph Drainage
veins also run between the liver and gallbladder.
directly into the portal vein. Several very small arteries and
drains
cystic vein
(Fig. 5.47), supplies the gallbladder. The
a branch of the right hepatic artery
cystic artery,
The
digestion and absorption.
emulsifying the fat in the intestine and in assisting with its
the duodenum. The bile salts in the bile are important in
relaxed, thus allowing the passage of concentrated bile into
The Abdomen: Part II—The Abdominal Cavity
Blood Supply
Nerve Supply
Cystic Duct
Gallstones
Sonograms can now be used to demonstrate the gallbladder
bladder rarely becomes gangrenous. In addition to the cystic
rise to referred pain over the shoulder, because the skin in this
irritation of the subdiaphragmatic parietal peritoneum, which is
pancreatic duct is subject to considerable variation. The type of
arrangement of the terminal part of the bile duct and the main
greater splanchnic nerves to the thoracic segments of the spinal
Gallstones are usually asymptomatic; however, they can give
rise to gallstone colic or produce acute cholecystitis.
Biliary Colic
Biliary colic is usually caused by spasm of the smooth muscle
of the wall of the gallbladder in an attempt to expel a gallstone.
Afferent nerve fibers ascend through the celiac plexus and the
cord. Referred pain is felt in the right upper quadrant or the epi-
gastrium (T7, 8, and 9 dermatomes).
Obstruction of the biliary ducts with a gallstone or by com-
pression by a tumor of the pancreas results in backup of bile in
the ducts and development of jaundice. The impaction of a stone
in the ampulla of Vater may result in the passage of infected bile
into the pancreatic duct, producing pancreatitis. The anatomic
duct system present determines whether infected bile is likely to
enter the pancreatic duct.
Gallstones have been known to ulcerate through the gallblad-
der wall into the transverse colon or the duodenum. In the former
case, they are passed naturally per the rectum, but in the latter
case, they may be held up at the ileocecal junction, producing
intestinal obstruction.
Acute Cholecystitis
Acute cholecystitis produces discomfort in the right upper quad-
rant or epigastrium. Inflammation of the gallbladder may cause
supplied in part by the phrenic nerve (C3, 4, and 5). This may give
area is supplied by the supraclavicular nerves (C3 and 4).
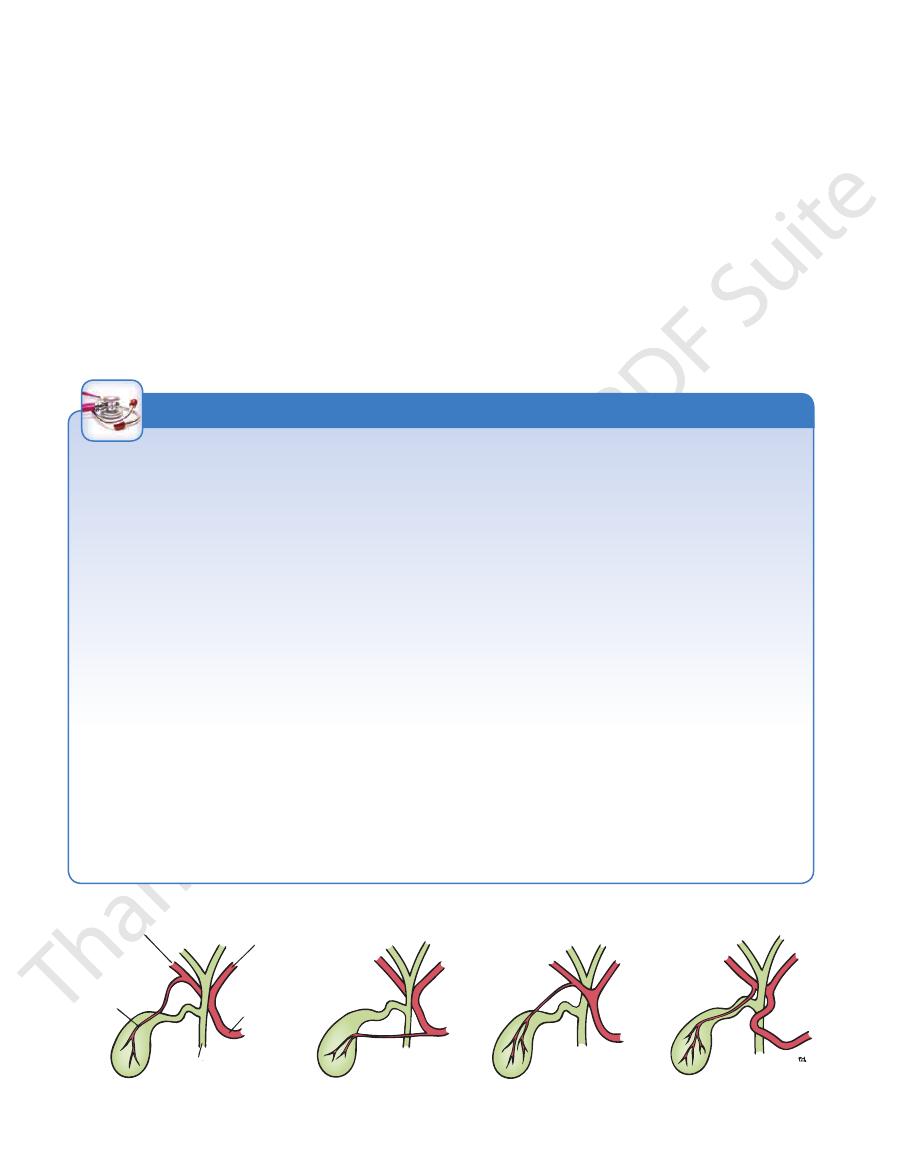
Cholecystectomy and the Arterial Supply
to the Gallbladder
Before attempting a cholecystectomy operation, the surgeon
must be aware of the many variations in the arterial supply to
the gallbladder and the relationship of the vessels to the bile
ducts (Fig. 5.53). Unfortunately, there have been several reported
cases in which the common hepatic duct or the main bile duct
have been included in the arterial ligature with disastrous con-
sequences.
Gangrene of the Gallbladder
Unlike the appendix, which has a single arterial supply, the gall-
artery, the gallbladder also receives small vessels from the vis-
ceral surface of the liver.
(Fig. 5.54).
C L I N I C A L N O T E S
right hepatic artery
cystic artery
left hepatic artery
hepatic artery
bile duct
FIGURE 5.53
Some common variations of blood supply to the gallbladder.
