
50
process of the sternum and the body of the sternum
is the joint between the xiphoid
xiphisternal joint
The
these cases, it may be easier to count up from the 12th rib.
tal spaces are often obscured by large pectoral muscles. In
Occasionally in a very muscular male, the ribs and intercos
then the 2nd rib. All ribs may be counted from this point.
to the left will pass directly onto the 2nd costal cartilage and
seen as a transverse ridge. The finger moved to the right or
position of the sternal angle can easily be felt and is often
between the 4th and 5th thoracic vertebrae (see Fig. 2.2). The
Figs. 2.19 and 2.20). It lies opposite the intervertebral disc
between the manubrium and the body of the sternum (see
is the angle made
sternal angle (angle of Louis)
The
The Thorax: Part I—The Thoracic Wall
-
(Fig. 2.21). It lies opposite the body of the ninth thoracic
cess of the scapula.
It articulates at its lateral extremity with the acromion pro
length and can be easily palpated (see Figs. 2.19 and 2.20).
is subcutaneous throughout its entire
clavicle
The
lumbar vertebra.
is formed by the 10th rib and lies at the level of the third
Figs. 2.19 and 2.20). The lowest part of the costal margin
10th ribs and the ends of the 11th and 12th cartilages (see
and is formed by the cartilages of the 7th, 8th, 9th, and
is the lower boundary of the thorax
costal margin
The
cartilages (see Fig. 2.21).
sternum, between the sternal attachments of the 7th costal
is situated at the inferior end of the
subcostal angle
The
vertebra (see Fig. 2.2).
-
■
■
■
■
■
■
as the result of calcification and even ossification of the
■
■
Anatomic and Physiologic Changes in the Thorax
with Aging
Certain anatomic and physiologic changes take place in the
thorax with advancing years:
The rib cage becomes more rigid and loses its elasticity
costal cartilages; this also alters their usual radiographic
appearance.
The stooped posture (kyphosis), so often seen in the
old because of degeneration of the intervertebral discs,
decreases the chest capacity.
Disuse atrophy of the thoracic and abdominal muscles can
result in poor respiratory movements.
Degeneration of the elastic tissue in the lungs and bronchi
results in impairment of the movement of expiration.
These changes, when severe, diminish the efficiency of respi-
ratory movements and impair the ability of the individual to
withstand respiratory disease.
C L I N I C A L N O T E S
Ribs
pressing the fingers upward into the axilla and drawing
The lateral surfaces of the remaining ribs can be felt by
The 1st rib lies deep to the clavicle and cannot be palpated.
them downward over the lateral surface of the chest wall.
esophagus
diaphragm
stomach
stomach
A
B
peritoneum
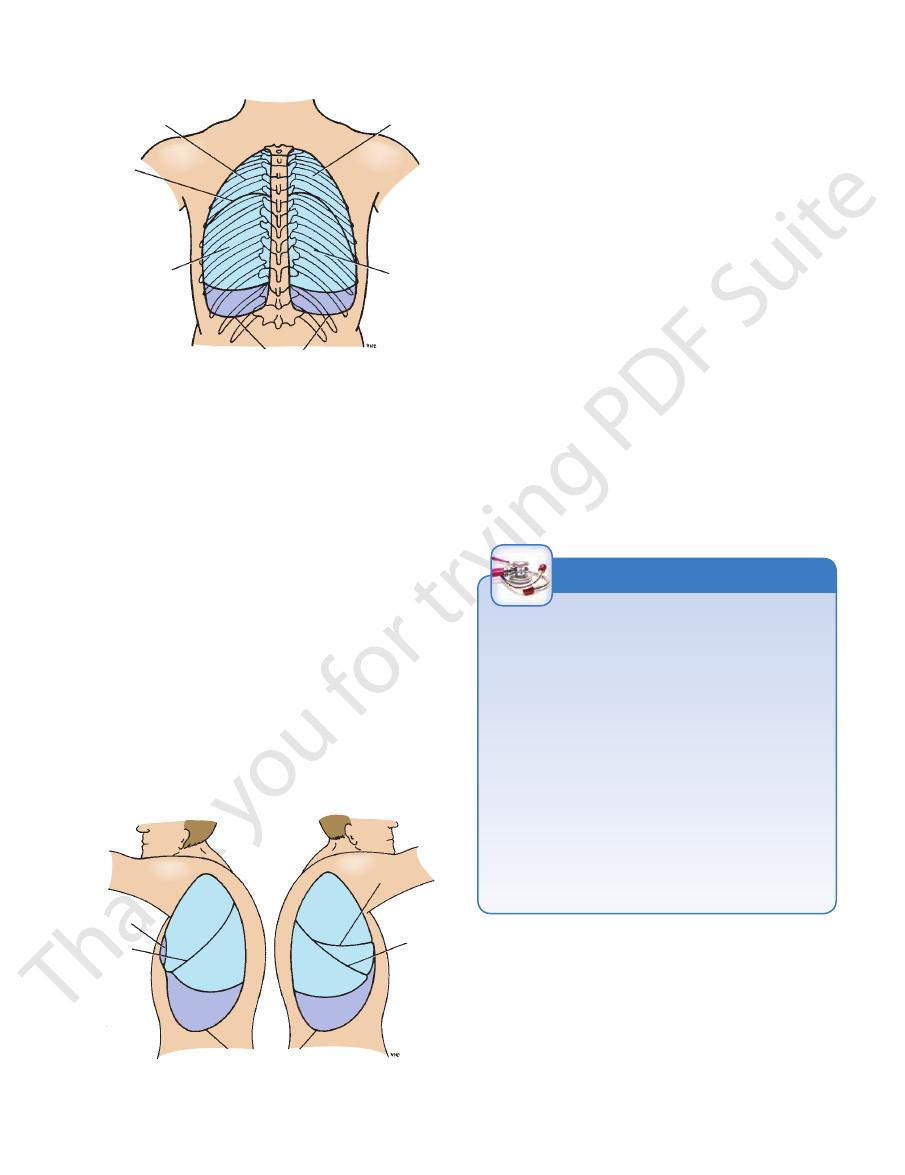
FIGURE 2.17
Paraesopha
A. Sliding esophageal hernia. B.
-
geal hernia.
natomy
aphic
adiog
R
R
a
This is fully described on page 102.
the internal thoracic artery, and posteriorly to the posterior
posterior chest wall passes to the posterior axillary nodes
of the skin of the anterior chest wall
lymph drainage
ing one of the internal thoracic arteries and joining its distal
the myocardium can be revascularized by surgically mobiliz
inserting a graft. The graft most commonly used is the great
sclerosis, the diseased arterial segment can be bypassed by
Internal Thoracic Artery in the Treatment
of Coronary Artery Disease
In patients with occlusive coronary disease caused by athero-
saphenous vein of the leg (see page 453). In some patients,
-
cut end to a coronary artery.
Lymph Drainage of the Thoracic Wall
The
passes to the anterior axillary lymph nodes; that from the
(Fig. 2.18). The lymph drainage of the intercostal spaces
passes forward to the internal thoracic nodes, situated along
intercostal nodes and the para-aortic nodes in the poste-
rior mediastinum. The lymphatic drainage of the breast is
described on page 337.
C L I N I C A L N O T E S
natomy
face
s
uR
a
Anterior Chest Wall
2nd thoracic vertebra (see Fig. 2.2).
2.20). It lies opposite the lower border of the body of the
medial ends of the clavicles in the midline (Figs. 2.19 and
manubrium sterni and is easily felt between the prominent
is the superior margin of the
suprasternal notch
The
Surface Anatomy
51
trapezius
tendon of
sternocleidomastoid
suprasternal notch
manubrium sterni
body of sternum
anterior axillary fold
xiphoid process
costal margin
linea semilunaris
cubital fossa
site of apex
beat of heart
areola
nipple
pectoralis major
deltoid
sternal angle
(angle of Louis)
acromion process
clavicle
supraclavicular
fossa
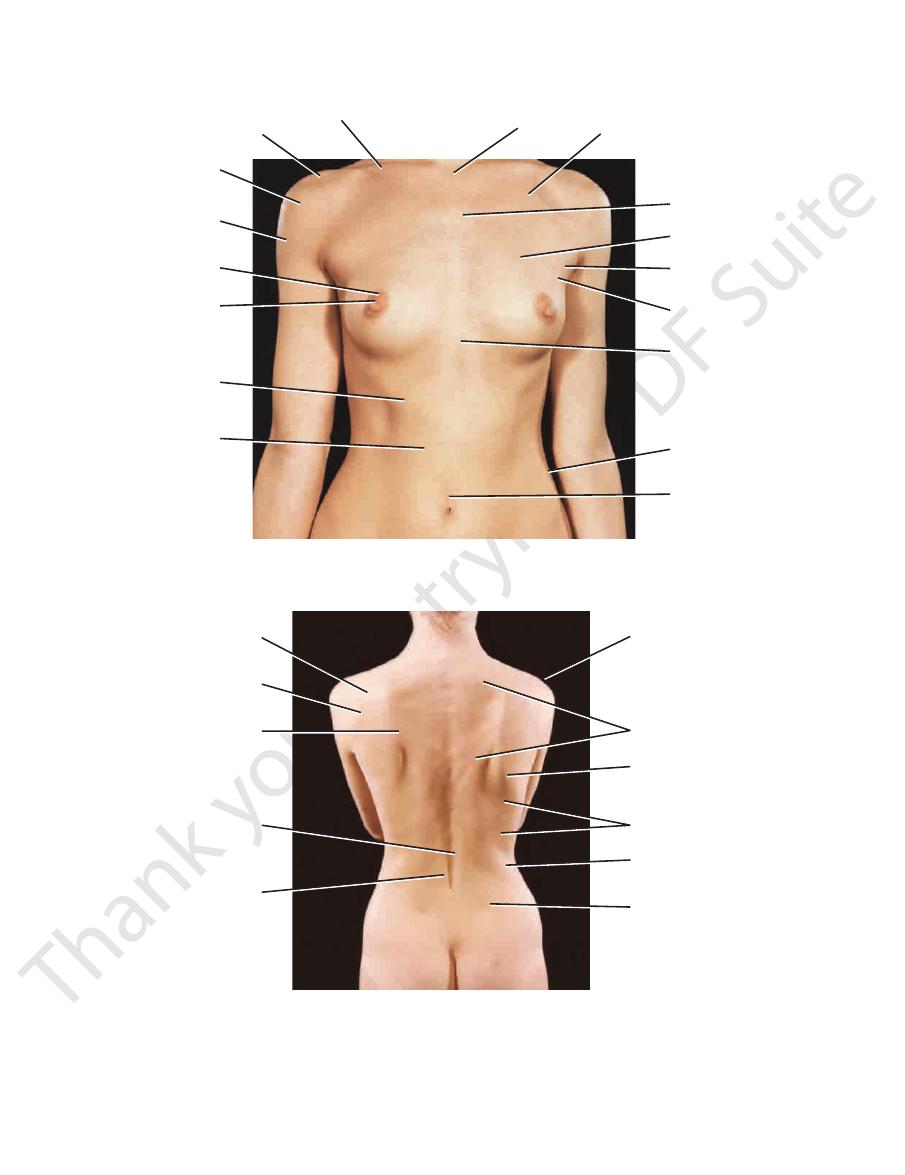
FIGURE 2.19
Anterior view of the thorax of a 27-year-old man.
anterior
axillary
nodes
watershed
superficial
inguinal
lymph
nodes
posterior
axillary
lymph
nodes
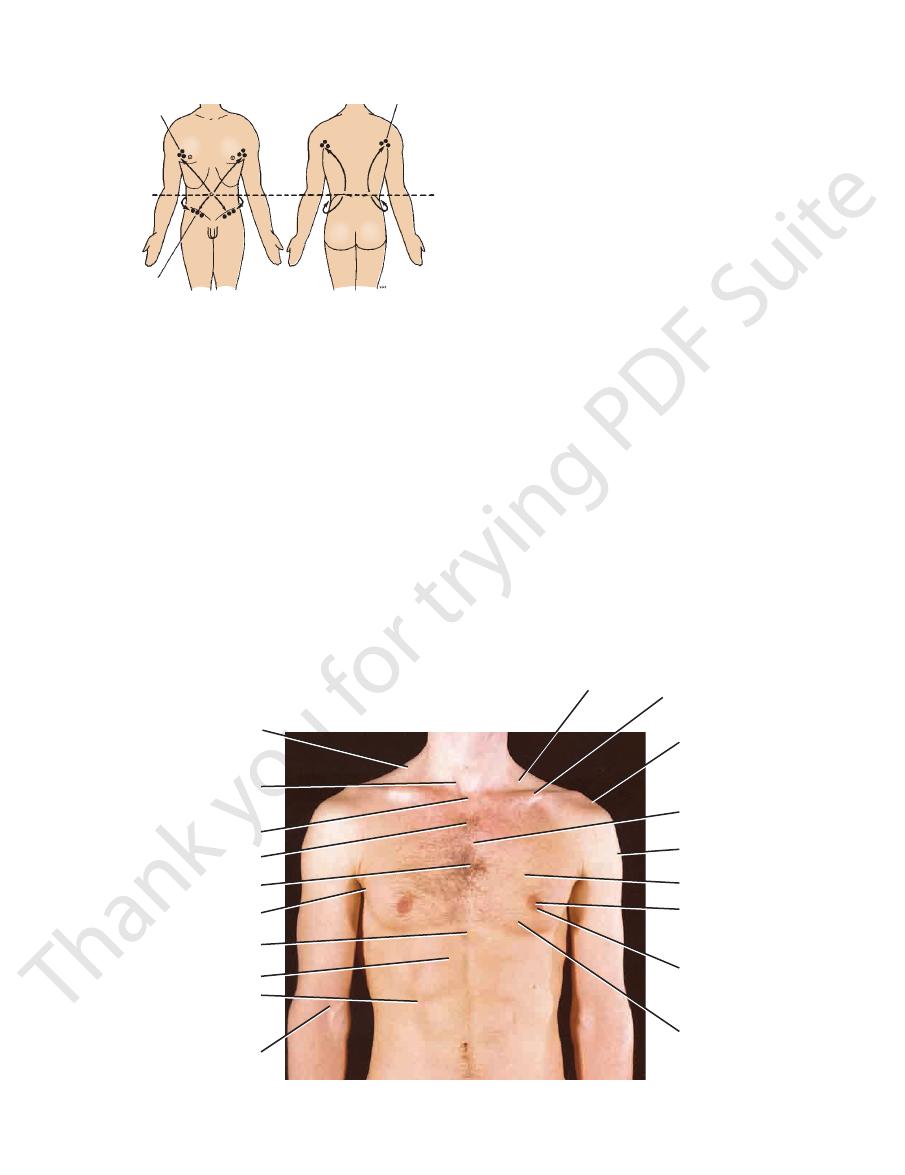
FIGURE 2.18
Lymph drainage of the skin of the thorax and
below as the intercostal spaces are palpated.
ing fingers should gently raise the left breast from
In a female with pendulous breasts, the examin
have the patient lean forward in the sitting position.
Should you have difficulty in finding the apex beat,
left intercostal space 3.5 in. (9 cm) from the midline.
is found. The apex beat is normally found in the fifth
moving them until the point of maximum pulsation
placing two fingers over the intercostal spaces and
determined, the apex beat is accurately localized by
the heart. After the area of cardiac pulsation has been
by placing the flat of the hand on the chest wall over
the heart forward.) The apex beat can usually be felt
the curved aorta to straighten slightly, thus pushing
aorta; the force of the blood in the aorta tends to cause
the ejection of blood from the left ventricle into the
forward with each ventricular contraction because of
racic wall as the heart contracts. (The heart is thrust
apex of the heart being thrust forward against the tho
of the left ventricle. The apex beat is caused by the
The apex of the heart is formed by the lower portion
line. In the female, its position is not constant.
intercostal space about 4 in. (10 cm) from the mid
In the male, the nipple usually lies in the fourth
border of the 5th rib.
line, but the left dome only reaches as far as the lower
as far as the upper border of the 5th rib in the midclavicular
summit of the right dome of the diaphragm arches upward
the xiphisternal joint. In the midrespiratory position, the
The central tendon of the diaphragm lies directly behind
palpating the sternal angle and the second costal cartilage.
an alternative method may be used to identify ribs by first
12th rib is very short and difficult to feel. For this reason,
counting from below. However, in some individuals, the
The 12th rib can be used to identify a particular rib by
lymph flow.
iliac crests posteriorly may be regarded as watersheds for
abdomen. Note that levels of the umbilicus anteriorly and
Diaphragm
Nipple
-
Apex Beat of the Heart
-
-
52
The Thorax: Part I—The Thoracic Wall
clavicle
acromion
greater tuberosity
of humerus
deltoid
areola
nipple
costal margin
rectus abdominis
umbilicus
iliac crest
xiphoid process
axillary tail of
mammary gland
anterior
axillary fold
pectoralis major
sternal angle
(angle of Louis)
deltopectoral triangle
suprasternal
notch
spine of scapula
posterior fibers
of deltoid
medial border
of scapula
skin furrow over
spinous processes
of lumbar vertebrae
erector spinae
skin dimple
overlying posterior
superior iliac spine
iliac crest
latissimus dorsi
inferior angle
of scapula
trapezius
acromion
A
B
FIGURE 2.20
old woman.
Posterior view of the thorax of a 29-year-
Anterior view of the thorax and abdomen of a 29-year-old woman.
A.
B.
Surface Anatomy
vertebra (see Figs. 2.20 and 2.22).
lies on a level with the spine of the seventh thoracic
angle
inferior
thoracic vertebra (see Figs. 2.21 and 2.22). The
root of the spine lies on a level with the spine of the third
is subcutaneous, and the
spine of the scapula
2.22). The
spine of the second thoracic vertebra (see Figs. 2.20 and
lies opposite the
superior angle
surface of the thorax. The
shape and is located on the upper part of the posterior
(shoulder blade) is flat and triangular in
The
below.
vertebra lies posterior to the body of the next vertebra
be noted that the tip of a spinous process of a thoracic
by a large ligament, the ligamentum nuchae. It should
vertebrae. The spines of C1 to 6 vertebrae are covered
Below this level are the overlapping spines of the thoracic
(vertebra prominens).
of the seventh cervical vertebrae
nuchal groove. The first spinous process to be felt is that
posterior surface of the neck and drawn downward in the
finger should be placed on the skin in the midline on the
palpated in the midline posteriorly (Fig. 2.22). The index
can be
thoracic vertebrae
of the
spinous processes
The
Posterior Chest Wall
the lower border of the teres major muscle.
tendon of the latissimus dorsi muscle as it passes around
is formed by the
posterior fold
hard against the hip. The
made to stand out by asking the patient to press a hand
toralis major muscle (see Figs. 2.19 and 2.20). This can be
is formed by the lower border of the pec
anterior fold
The
53
Axillary Folds
-
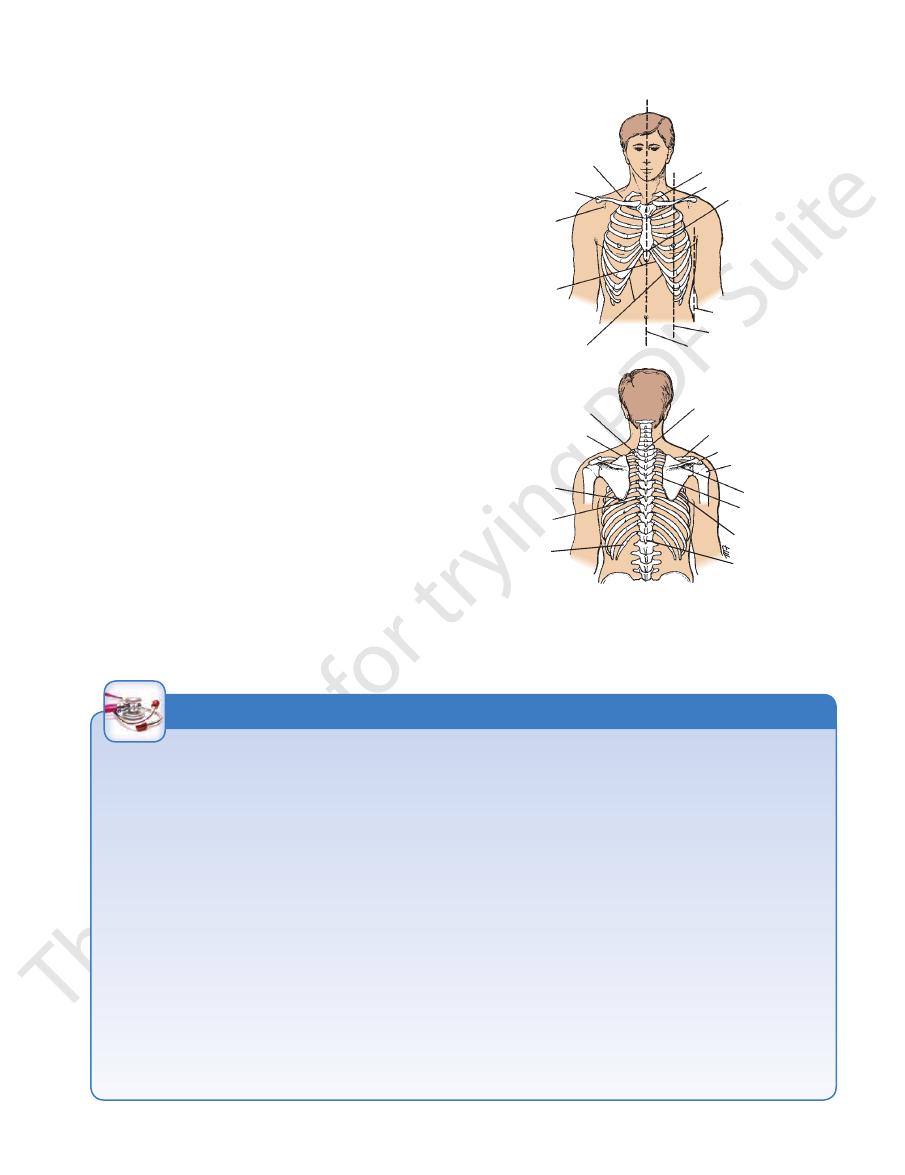
scapula
supraclavicular fossa
clavicle
infraclavicular
fossa
subcostal
angle
costal margin
midsternal line
midclavicular line
anterior axillary line
xiphisternal joint
sternal angle
suprasternal notch
first rib
superior angle
of scapula
inferior angle
of scapula
thoracic
spine seven
12th rib
cervical spine seven
clavicle
acromion
greater tuberosity
of humerus
spine of scapula
medial border
of scapula
lateral border
of scapula
thoracic
spine 12
A
B
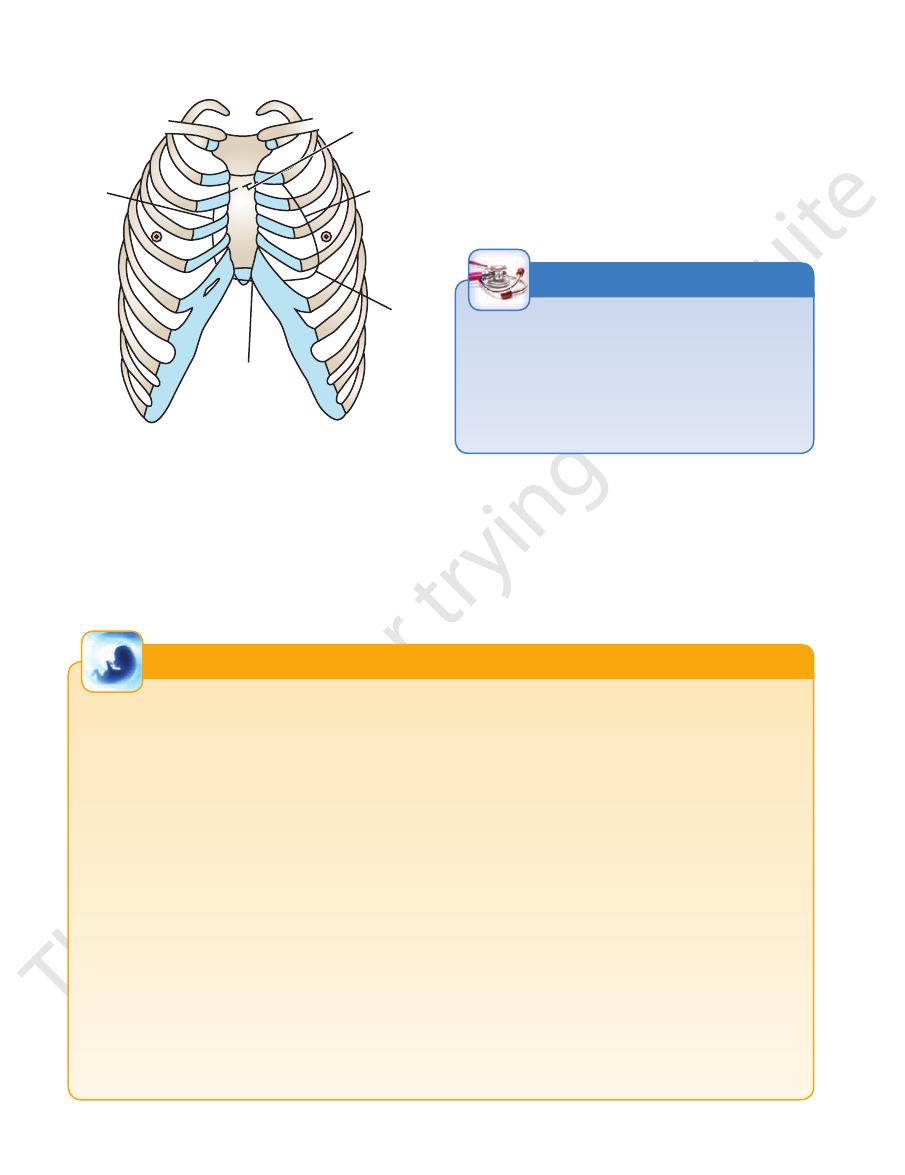
FIGURE 2.21
Surface landmarks of anterior
thoracic walls.
(A) and posterior
(B)
Clinical Examination of the Chest
ments of respiration, many bony landmarks change their levels
identifiable bony landmarks so that he or she can accurately
detect friction sounds produced by the rubbing together of dis
of the heart can be confirmed by auscultation, and the various
sounds as the air enters and leaves the respiratory passages.
produces a dull note. With practice, it is possible to distinguish
the chest wall is noted. Abnormal pulsations are felt and tender
the chest wall. Abnormal protuberances or recession of part of
As medical personnel, you will be examining the chest to detect
evidence of disease. Your examination consists of inspection,
palpation, percussion, and auscultation.
Inspection shows the configuration of the chest, the range of
respiratory movement, and any inequalities on the two sides. The
type and rate of respiration are also noted.
Palpation enables the physician to confirm the impressions
gained by inspection, especially of the respiratory movements of
areas detected.
Percussion is a sharp tapping of the chest wall with the
fingers. This produces vibrations that extend through the tissues
of the thorax. Air-containing organs such as the lungs produce a
resonant note; conversely, a more solid viscus such as the heart
the lungs from the heart or liver by percussion.
Auscultation enables the physician to listen to the breath
Should the alveoli or bronchi be diseased and filled with fluid, the
nature of the breath sounds will be altered. The rate and rhythm
sounds produced by the heart and its valves during the different
phases of the cardiac cycle can be heard. It may be possible to
-
eased layers of pleura or pericardium.
To make these examinations, the physician must be familiar
with the normal structure of the thorax and must have a mental
image of the normal position of the lungs and heart in relation to
identifiable surface landmarks. Furthermore, it is essential that
the physician be able to relate any abnormal findings to easily
record and communicate them to colleagues.
Since the thoracic wall actively participates in the move-
with each phase of respiration. In practice, to simplify matters,
the levels given are those usually found at about midway
between full inspiration and full expiration.
C L I N I C A L N O T E S
54
the inferior angle of the scapula (arms at the sides)
rior wall of the thorax (see Fig. 2.22), passing through
Runs vertically downward on the poste
Scapular line:
rior axillary folds
point situated midway between the anterior and poste
Runs vertically downward from a
Midaxillary line:
the posterior axillary fold
Runs vertically downward from
Posterior axillary line:
the anterior axillary fold (see Fig. 2.21)
Runs vertically downward from
Anterior axillary line:
midpoint of the clavicle (see Fig. 2.21)
Runs vertically downward from the
Midclavicular line:
num (see Fig. 2.21)
Lies in the median plane over the ster
Midsternal line:
face locations on the anterior and posterior chest walls.
Several imaginary lines are sometimes used to describe sur
The Thorax: Part I—The Thoracic Wall
Lines of Orientation
-
■
■
-
■
■
■
■
■
■
■
■
-
■
■
-
be counted from this point. The 12th rib can usually be felt from
second costal cartilage and then the 2nd rib. All other ribs can
When one is examining the chest from in front, the
Rib and Costal Cartilage Identification
sternal
angle is an important landmark. Its position can easily be felt
and often be seen by the presence of a transverse ridge. The
finger moved to the right or to the left passes directly onto the
behind, but in some obese persons this may prove difficult.
C L I N I C A L N O T E S
Trachea
surface by a line drawn from the root of the spine of the
of the lung can be indicated on the
oblique fissure
The
(4 cm) from the midline (Fig. 2.24).
the level of the 10th thoracic vertebra and lies about 1.5 in.
from the spinous process of the 7th cervical vertebra to
extends downward
posterior border of the lung
The
ing inspiration and expiration.
that the level of the inferior border of the lung changes dur
(Figs. 2.23, 2.24, and 2.25). It is important to understand
the 10th rib adjacent to the vertebral column posteriorly
lar line and the 8th rib in the midaxillary line, and reaches
a curving line, which crosses the 6th rib in the midclavicu
in midinspiration follows
lower border of the lung
The
sharply downward to the level of the xiphisternal joint.
placing the lung to the left. The anterior border then turns
(see Fig. 2.23). This notch is produced by the heart dis
cardiac notch
lateral margin of the sternum to form the
ates laterally and extends for a variable distance beyond the
course, but at the level of the fourth costal cartilage it devi
anterior border of the left lung
2.23). The
downward until it reaches the xiphisternal joint (see Fig.
ing the midline behind the sternal angle. It then continues
sternoclavicular joint and runs downward, almost reach
begins behind the
anterior border of the right lung
The
Fig. 2.23).
of the medial and intermediate thirds of the clavicle (see
vicular joint to a point 1 in. (2.5 cm) above the junction
drawing a curved line, convex upward, from the sternocla
mapped out on the anterior surface of the body by
projects into the neck. It can be
apex of the lung
The
palpated in the midline in the suprasternal notch.
left principal bronchi. At the root of the neck, it may be
the right of the midline by dividing into the right and the
(Fig. 2.23). It commences in the midline and ends just to
in the neck to the level of the sternal angle in the thorax
cartilage (opposite the body of the 6th cervical vertebra)
The trachea extends from the lower border of the cricoid
Lungs
-
-
has a similar
-
-
-
-
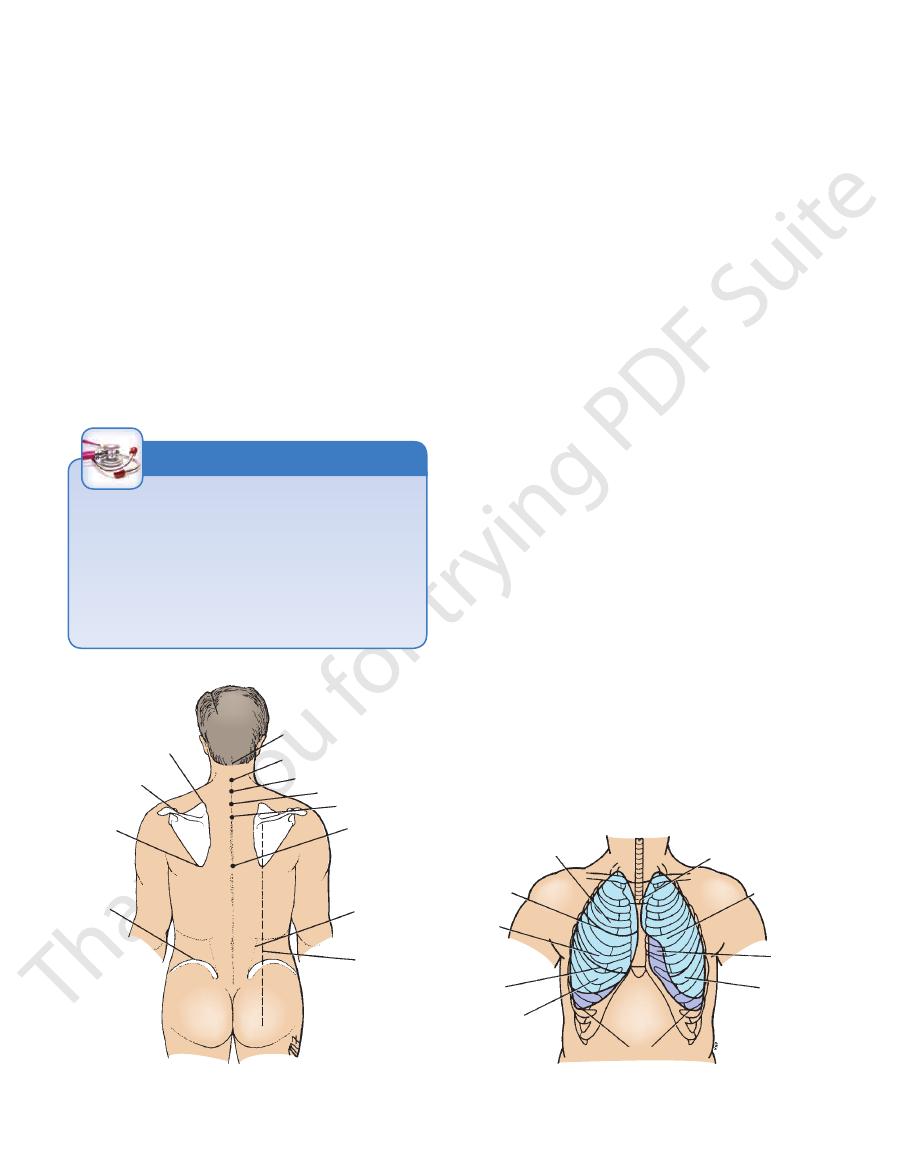
superior angle
of scapula
spine of
scapula
inferior
angle of
scapula
iliac
crest
nuchal groove
cervical spine seven
thoracic spine one
thoracic spine two
thoracic spine
three
thoracic spine
seven
lateral border
of erector
spinae
muscle
scapular line
FIGURE 2.22
Surface landmarks of the posterior thoracic
wall.
upper lobe
horizontal
fissure
middle
lobe
oblique
fissure
lower
lobe
lower border of pleura
sternal
angle
upper
lobe
cardiac
notch
lower
lobe
FIGURE 2.23
Surface markings of the lungs and parietal
pleura on the anterior thoracic wall.
Surface Anatomy
(see page 62).
diaphragmatic recess
costo
distance between the two borders corresponds to the
same points, the 8th, 10th, and 12th ribs, respectively. The
respectively; the lower margins of the pleura cross, at the
the midaxillary lines, and the sides of the vertebral column,
cross the 6th, 8th, and 10th ribs at the midclavicular lines,
2.24, and 2.25). Note that the lower margins of the lungs
lateral border of the erector spinae muscle (see Figs. 2.23,
12th rib adjacent to the vertebral column—that is, at the
line and the 10th rib in the midaxillary line, and reaches the
curved line, which crosses the 8th rib in the midclavicular
on both sides follows a
lower border of the pleura
The
to the xiphisternal joint (see Fig. 2.23).
cardiac notch of the lung.) It then turns sharply downward
(Note that the pleural cardiac notch is not as large as the
the lateral margin of the sternum to form the cardiac notch.
fourth costal cartilage it deviates laterally and extends to
has a similar course, but at the level of the
of the left pleura
anterior border
until it reaches the xiphisternal joint. The
line behind the sternal angle. It then continues downward
behind the sternoclavicular joint, almost reaching the mid
runs down
anterior border of the right pleura
The
clavicle (see Fig. 2.23).
the junction of the medial and intermediate thirds of the
the sternoclavicular joint to a point 1 in. (2.5 cm) above
lung. A curved line may be drawn, convex upward, from
has a surface marking identical to that of the apex of the
bulges upward into the neck and
cervical pleura
The
lines of pleural reflection.
surface, are referred to as the
limits of the parietal pleura where it lies close to the body
on the surface of the body. The lines, which indicate the
The boundaries of the pleural sac can be marked out as lines
fissure lies the lower lobe.
it lies the middle lobe; below and posterior to the oblique
Above the horizontal fissure lies the upper lobe and below
fissure in the midaxillary line (see Figs. 2.23 and 2.25).
tally along the fourth costal cartilage to meet the oblique
which may be represented by a line drawn horizon
fissure,
horizontal
In the right lung is an additional fissure, the
to it (see Figs. 2.23 and 2.24).
anterior to this line; the lower lobe lies below and posterior
junction. In the left lung, the upper lobe lies above and
lowing the course of the 6th rib to the sixth costochondral
scapula obliquely downward, laterally and anteriorly, fol
55
-
-
Pleura
-
-
tomy. The pleura crosses the 12th rib and may be damaged
ratory tract, it should be possible to have a mental image of
of the lungs. When listening to the breath sounds of the respi
the surface markings of the pleural reflections and the lobes
Pleural Reflections
It is hardly necessary to emphasize the importance of knowing
-
the structures that lie beneath the stethoscope.
The cervical dome of the pleura and the apex of the lungs
extend up into the neck so that at their highest point they lie
about 1 in. (2.5 cm) above the clavicle (see Figs. 2.6, 2.13, and
2.23). Consequently, they are vulnerable to stab wounds in the
root of the neck or to damage by an anesthetist’s needle when
a nerve block of the lower trunk of the brachial plexus is being
performed.
Remember also that the lower limit of the pleural reflection,
as seen from the back, may be damaged during a nephrec-
during removal of the kidney through an incision in the loin.
C L I N I C A L N O T E S
Heart
costal cartilage (remember sternal angle) 0.5 in. (1.3 cm)
great blood vessels, extends from a point on the second left
formed by the roots of the
superior border,
The
3.5 in. (9 cm) from the midline (Fig. 2.26).
the apex beat and is found in the fifth left intercostal space
formed by the left ventricle, corresponds to
apex,
The
both an apex and four borders.
For practical purposes, the heart may be considered to have
upper lobe
oblique
fissure
lower lobe
lower border of pleura
lower lobe
upper lobe
FIGURE 2.24
Surface markings of the lungs and parietal
pleura on the posterior thoracic wall.
cardiac
notch
oblique
fissure
lower border of pleura
oblique
fissure
horizontal
fissure
FIGURE 2.25
Surface markings of the lungs and parietal
pleura on the lateral thoracic walls.
56
of the sternum (see Fig. 2.26).
the 6th right costal cartilage 0.5 in. (1.3 cm) from the edge
cm) from the edge of the sternum downward to a point on
from a point on the third right costal cartilage 0.5 in. (1.3
formed by the right atrium, extends
right border,
The
num (see Fig. 2.26).
costal cartilage 0.5 in. (1.3 cm) from the edge of the ster
from the edge of the sternum to a point on the third right
The Thorax: Part I—The Thoracic Wall
-
right
border
superior
border
left
border
apex
inferior
border
FIGURE 2.26
Surface markings of the heart.
Development of the Diaphragm
weak musculature around the esophageal opening in the dia
between the xiphoid and costal origins of the diaphragm, and (c)
peritoneal membranes from the body wall. The herniae occur at
peritoneum from the pleuroperitoneal membranes are derived
nerves. This is understandable, since the peripheral pleura and
lower surfaces of the diaphragm is from the lower six thoracic
peritoneum covering the peripheral areas of the upper and
sensory innervation of the peripheral parts of the pleura and
explains their sensory innervation from the phrenic nerve. The
surface are also formed from the septum transversum, which
surface of the diaphragm and the peritoneum on the lower
phragm is the phrenic nerve. The central pleura on the upper
tery posterior to the esophagus. During the process of fusion,
and 5th cervical segments. With the descent of the heart from
which are largely
pleuroperitoneal membranes,
don; (b) the two
The diaphragm is formed from the following structures: (a) the
septum transversum, which forms the muscle and central ten-
responsible for the peripheral areas of the diaphragmatic pleura
and peritoneum that cover its upper and lower surfaces, respec-
tively; and (c) the dorsal mesentery of the esophagus, in which
the crura develop.
The septum transversum is a mass of mesoderm that is
formed in the neck by the fusion of the myotomes of the 3rd, 4th
the neck to the thorax, the septum is pushed caudally, pulling its
nerve supply with it; thus, its motor nerve supply is derived from
the 3rd, 4th and 5th cervical nerves, which are contained within
the phrenic nerve.
The pleuroperitoneal membranes grow medially from the
body wall on each side until they fuse with the septum trans-
versum anterior to the esophagus and with the dorsal mesen-
the mesoderm of the septum transversum extends into the other
parts, forming all the muscles of the diaphragm.
The motor nerve supply to the entire muscle of the dia-
from the body wall.
Diaphragmatic Herniae
Congenital herniae occur as the result of incomplete fusion of
the septum transversum, the dorsal mesentery, and the pleuro-
the following sites: (a) the pleuroperitoneal canal (more common
on the left side; caused by failure of fusion of the septum trans-
versum with the pleuroperitoneal membrane), (b) the opening
the esophageal hiatus.
Acquired herniae may occur in middle-aged people with
-
phragm. These herniae may be either sliding or paraesophageal
(Fig. 2.17).
E M B R Y O L O G I C N O T E S
The
the apex beat (see Fig. 2.26).
right costal cartilage 0.5 in. (1.3 cm) from the sternum to
the apical part of the left ventricle, extends from the sixth
formed by the right ventricle and
inferior border,
The
(see Fig. 2.26).
from the edge of the sternum to the apex beat of the heart
from a point on the 2nd left costal cartilage 0.5 in. (1.3 cm)
formed by the left ventricle, extends
left border,
beat may enable a physician to determine whether the heart
Position and Enlargement of the Heart
The surface markings of the heart and the position of the apex
has shifted its position in relation to the chest wall or whether
the heart is enlarged by disease. The apex beat can often be
seen and almost always can be felt. The position of the mar-
gins of the heart can be determined by percussion.
C L I N I C A L N O T E S
Thoracic Blood Vessels
manubrium sterni.
also lie behind the
left brachiocephalic veins
right
and the terminal parts of the
superior vena cava
The
brium sterni (Fig. 2.2).
lie behind the manu
left common carotid arteries
brachiocephalic
and the roots of the
arch of the aorta
The
and
-
and

Surface Anatomy
and the overlying skin is wrinkled.
hemispherical shape lost; the breasts then become smaller,
sue of the breast may become reduced in amount and the
dulous. In older women past menopause, the adipose tis
multiparous women, the breasts may be large and pen
the pectoralis major and enters the axilla. In middle-aged
Its upper lateral edge extends around the lower border of
the lateral margin of the sternum to the midaxillary line.
2nd to 6th ribs and their costal cartilages and extends from
spherical shape. In the young adult female, it overlies the
the female after puberty, it enlarges and assumes its hemi
(Fig. 2.20). In the child and in men, it is rudimentary. In
in the superficial fascia covering the anterior chest wall
Chapter 9. To summarize briefly, the mammary gland lies
nodes, it will be fully described with the Upper Limb in
and its main lymph drainage is into the axillary lymph
ture. Because it is closely related to the pectoral muscles
The mammary gland is clinically a very important struc
immediately below their corresponding ribs (see Fig. 2.8).
VAN—is the order from above downward) are situated
The intercostal vessels and nerve (“vein, artery, nerve”—
sixth intercostal space.
the edge of the sternum (see Figs. 2.9 and 2.10), as far as the
posterior to the costal cartilages, 0.5 in. (1.3 cm) lateral to
run vertically downward,
internal thoracic vessels
The
57
Mammary Gland
-
-
-
-
www.thePoint.lww.com/Snell9e.
Clinical Cases
and
Review Questions
are available online at
