
652
CHAPTER 11
The Head and Neck
B
hard palate
tongue
entrance into larynx
laryngoscope
examiner's
eye
examiner's
eye
tongue
entrance into larynx
vestibular fold
rima glottidis
cuneiform
cartilage
corniculate
cartilage
epiglottis
vocal fold (cord)
orientation of laryngeal inlet
A
FIGURE 11.103
Inspection of the vocal folds (cords) indirectly through a laryngeal mirror
Note the orientation of the structures forming the laryngeal inlet.
and through a laryngoscope
(A)
(B).
A
B
M
T
P
M
T
P
FIGURE 11.104
Anatomic axes for endotracheal intubation.
the optic chiasma (Fig. 11.108).
The diaphragma sellae separates the anterior lobe from
aperture that allows the passage of the infundibulum.
The diaphragma sellae, which has a central
Superiorly:
the pons
The dorsum sellae, the basilar artery, and
Posteriorly:
The sphenoid sinus (Fig. 11.13)
Anteriorly:
eral surfaces of the pituitary stalk.
extends up along the anterior and lat
pars tuberalis,
an embryonic pouch. A projection from the pars anterior,
which may be separated by a cleft that is a remnant of
pars interme
pars distalis
(sometimes called the
pars anterior
The anterior lobe is subdivided into the
ysis.
neurohypoph
or
posterior lobe,
adenohypophysis,
or
anterior lobe,
The pituitary gland is divided into an
reason, it is vital to life.
is often referred to as the master endocrine gland. For this
ties of many other endocrine glands, the hypophysis cerebri
the hormones produced by the gland influence the activi
location in the sella turcica of the sphenoid bone. Because
and 11.108). The gland is well protected by virtue of its
(Figs. 11.13
infundibulum
undersurface of the brain by the
The pituitary gland is a small, oval structure attached to the
Location and Description
Pituitary Gland (Hypophysis Cerebri)
and pharynx are brought in line with the axis of the mouth.
flexing the cervical vertebral column, the axes of the trachea
If the back of the head is raised off the table with a pillow, thus
atlanto-occipital joints, the axis of the mouth is correctly placed.
If the head is extended at the
not aligned with one another.
the axis of the trachea (T), and the axis of the pharynx (P) are
With the head in the neutral position, the axis of the mouth (M),
A.
B.
Endocrine Glands in the Head
and Neck
-
and a
-
) and the
-
dia,
the
-
Relations
■
■
■
■
■
■
Basic Anatomy
653
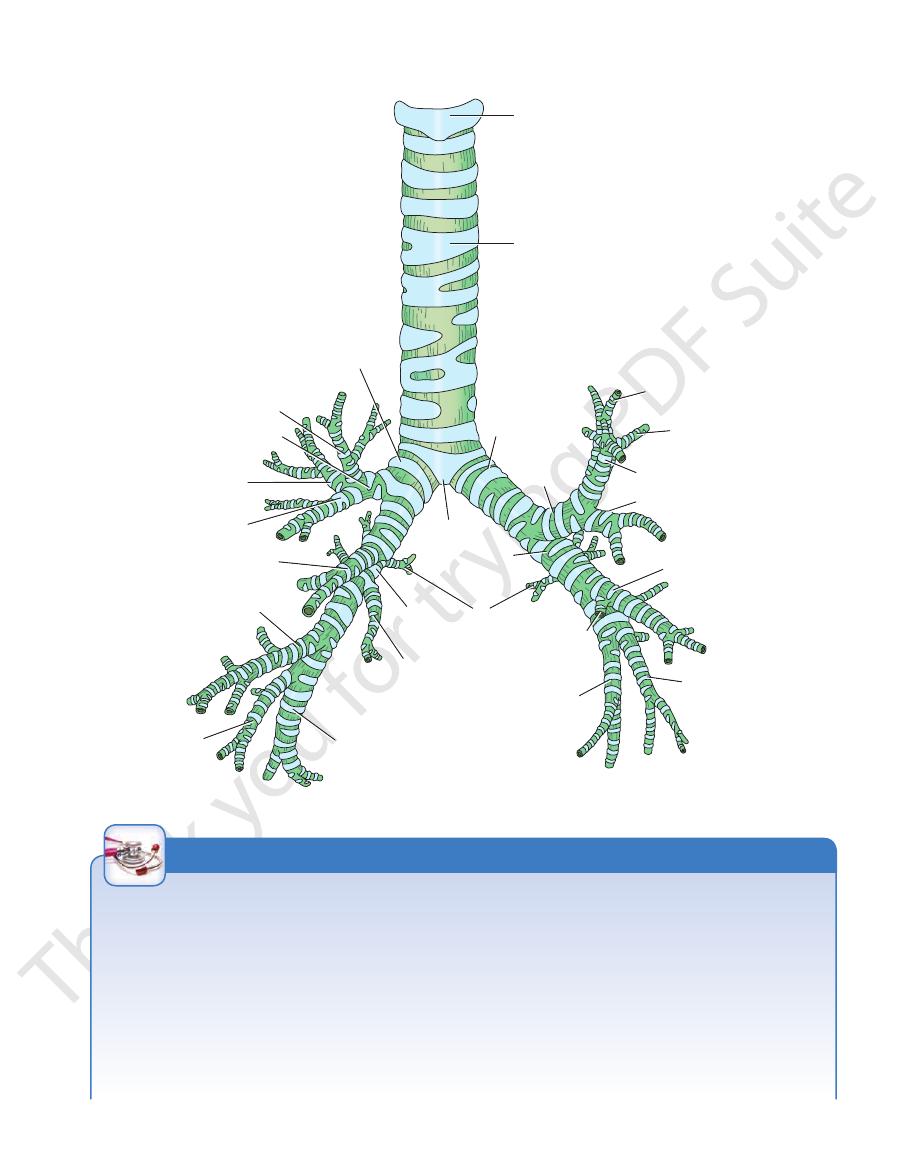
cricoid cartilage
trachea
right principal
bronchus
apical bronchus of
superior lobe
superior lobar bronchus
posterior segmental
bronchus
anterior segmental
bronchus
anterior basal
segmental bronchus
anterior basal
segmental bronchus
lateral basal
segmental
bronchus
lateral basal
segmental bronchus
posterior basal
segmental bronchus
medial basal
segmental
bronchus
apical segmental
bronchus of
superior lobe
posterior segmental
bronchus
anterior segmental
bronchus
lingular bronchus
superior apical
bronchus of
inferior lobe
medial
basal
segmental
bronchus
posterior basal
segmental bronchus
middle lobar bronchus
inferior
lobar
bronchus
inferior
lobar bronchus
superior
lobar
bronchus
carina
left principal
bronchus
FIGURE 11.105
The trachea and the bronchi.
Midline Structures in the Neck
the enlargement of adjacent organs or the presence of tumors.
The trachea is a mobile elastic tube and is easily displaced by
from the surface at the suprasternal notch. Remember that in
The midline structures in the neck should be readily recognized
as one passes an examining finger down the neck from the chin
to the suprasternal notch (for details, see page 676). The physi-
cian commonly forgets that an enlarged submental lymph node
may be caused by a pathologic condition anywhere between the
tip of the tongue and the point of the chin.
Palpation of the Trachea
The trachea can be readily felt below the larynx. As it descends,
it becomes deeply placed and may lie as much as 1.5 in. (4 cm)
the adult it may measure as much as 1 in. (2.5 cm) in diameter,
but in a 3-year-old child it may measure only 0.5 in. in diameter.
Remember also that lateral displacement of the cervical part of
the trachea may be caused by a pathologic lesion in the thorax.
Compromised Airway
No medical emergency quite produces the urgency and anxiety
of the compromised airway. The physician has to institute almost
C L I N I C A L N O T E S
(continued)
654
CHAPTER 11
The Head and Neck
immediate treatment. All techniques of airway management
Tracheostomy is rarely performed and is limited to patients with
tery that occasionally cross the front of the cricothyroid mem
the cricoid cartilage and the thyroid cartilage. The trachea and
require a detailed knowledge of anatomy.
Cricothyroidotomy
In cricothyroidotomy, a tube is inserted in the interval between
larynx are steadied by extending the neck over a sandbag.
A vertical or transverse incision is made in the skin in the
interval between the cartilages (Fig. 11.106). The incision is made
through the following structures: the skin, the superficial fascia
(beware of the anterior jugular veins, which lie close together on
either side of the midline), the investing layer of deep cervical
fascia, the pretracheal fascia (separate the sternohyoid mus-
cles and incise the fascia), and the larynx. The larynx is incised
through a horizontal incision through the cricothyroid ligament
and the tube inserted.
Complications
■
■
Esophageal perforation: Because the lower end of the phar-
ynx and the beginning of the esophagus lie directly behind
the cricoid cartilage, it is imperative that the scalpel incision
through the cricothyroid membrane not be carried too far
posteriorly. This is particularly important in young children, in
whom the cross diameter of the larynx is so small.
■
■
Hemorrhage: The small branches of the superior thyroid ar-
-
brane to anastomose with one another should be avoided.
Tracheostomy
extensive laryngeal damage and infants with severe airway
obstruction. Because of the presence of major vascular struc-
tures (carotid arteries and internal jugular vein), the thyroid
gland, nerves (recurrent laryngeal branch of vagus and vagus
nerve), the pleural cavities, and the esophagus, meticulous
attention to anatomic detail has to be observed (Fig. 11.107).
The procedure is as follows:
1.
The thyroid and cricoid cartilages are identified and the neck
is extended to bring the trachea forward.
2.
A vertical midline skin incision is made from the region of the cri-
cothyroid membrane inferiorly toward the suprasternal notch.
3.
The incision is carried through the superficial fascia and the
fibers of the platysma muscle. The anterior jugular veins in
the superficial fascia are avoided by maintaining a midline
position.
4.
The investing layer of deep cervical fascia is incised.
5. The pretracheal muscles embedded in the pretracheal fascia
are split in the midline two fingerbreadths superior to the
sternal notch.
6.
The tracheal rings are then palpable in the midline or the isth
the lower border of the cricoid cartilage and traction is ap
mus of the thyroid gland is visible. If a hook is placed under
-
-
plied upward, the slack is taken out of the elastic trachea;
this stops it from slipping from side to side.
7.
A decision is then made as to whether to enter the trachea
the pretracheal fascia contains the inferior thyroid veins and
lower tracheal rings below the thyroid isthmus. At the latter
through the second ring above the isthmus of the thyroid
gland; through the third, fourth, or fifth ring by first dividing
the vascular isthmus of the thyroid gland; or through the
site, the trachea is receding from the surface of the neck, and
possibly the thyroidea ima artery.
8.
The preferred site is through the second ring of the trachea
perficial fascia close to the midline should be avoided. If the
in the midline, with the thyroid isthmus retracted inferiorly. A
vertical tracheal incision is made, and the tracheostomy tube
is inserted.
Complications
Most complications result from not adequately palpating and
recognizing the thyroid, cricoid, and tracheal cartilages and not
confining the incision strictly to the midline.
■
■
Hemorrhage: The anterior jugular veins located in the su-
isthmus of the thyroid gland is transected, secure the anasto-
mosing branches of the superior and inferior thyroid arteries
that cross the midline on the isthmus.
■
■
Nerve paralysis: The recurrent laryngeal nerves may be
damaged as they ascend the neck in the groove between the
trachea and the esophagus.
The cavernous sinus and its contents
Laterally:
air sinuses
The body of the sphenoid, with its sphenoid
Inferiorly:
commonly in infants; it follows penetration of the small-
cated immediately posterior to the trachea, occurs most
Esophageal injury: Damage to the esophagus, which is lo
■
■
Pneumothorax: The cervical dome of the pleura may be
pierced. This is especially common in children because of the
high level of the pleura in the neck.
■
■
-
diameter trachea by the point of the scalpel blade.
Some Important Airway Distances
Table 11.13 shows some important distances between the inci-
sor teeth or nostrils to anatomic landmarks in the airway in the
adult. These approximate figures are helpful in determining the
correct placement of an endotracheal tube.
■
■
■
■
(Fig. 11.108)
ing electrolytes and hormones.
tral nervous system and by the plasma levels of the circulat
nervous afferent pathways from different parts of the cen
mus are modified by information received along numerous
by the hypothalamus and the activities of the hypothala
endocrine glands. The pituitary gland is itself controlled
The pituitary gland influences the activities of many other
Functions of the Pituitary Gland
artery. The veins drain into the intercavernous sinuses.
branches of the internal carotid
hypophyseal arteries,
inferior
The arteries are derived from the superior and
Blood Supply
-
-
-

Basic Anatomy
655
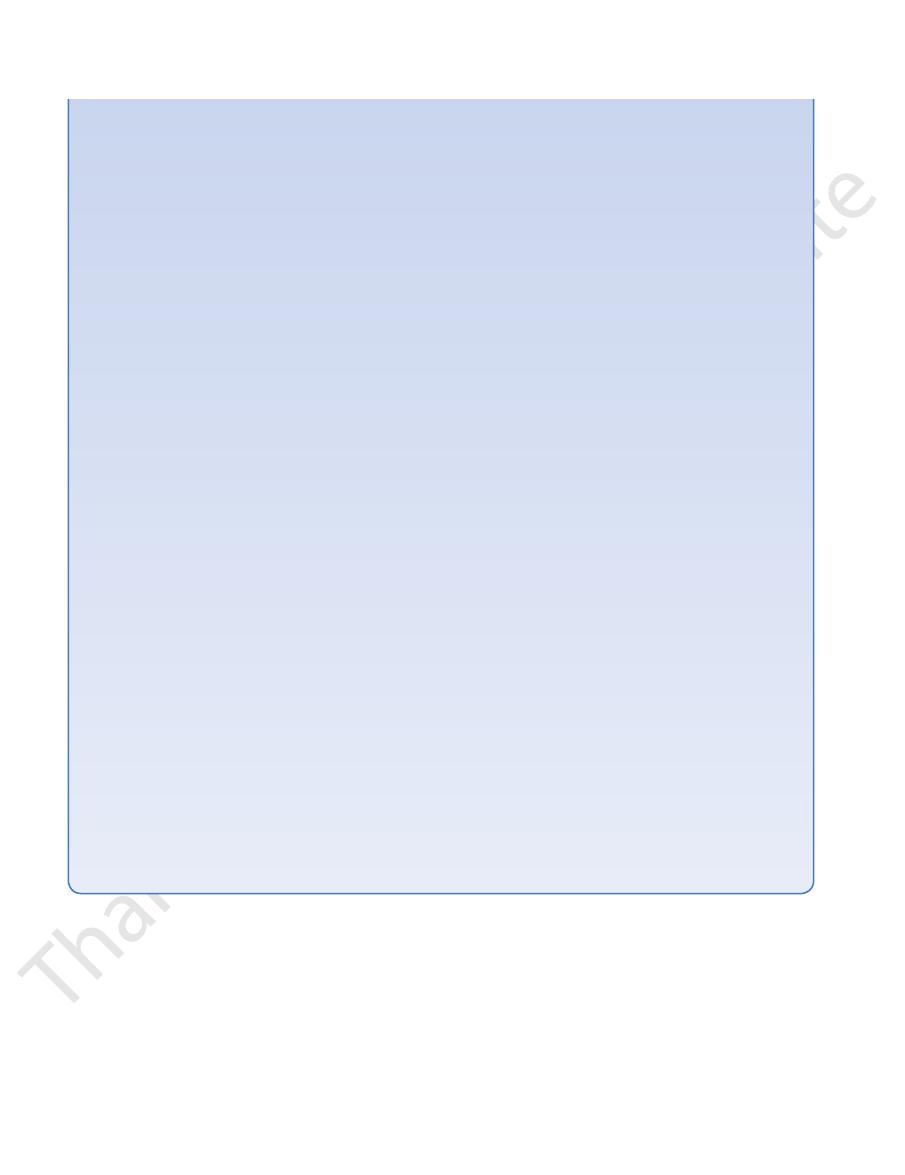
thyrohyoid
membrane
(ligament)
sternohyoid
muscle
superior belly of
omohyoid muscle
cricothyroid membrane
(ligament)
cricothyroid
muscle
anterior jugular
vein
isthmus
of thyroid
gland
first tracheal ring
cricoid
cartilage
site of skin
incision
thyroid cartilage
body of hyoid
bone
fascia
thyroid cartilage
small
cricothyroid
artery
skin
edge
cricothyroid
membrane
(ligament)
cricoid
cartilage
cricothyroid
membrane
(ligament)
thyroid
cartilage
A
B
C
FIGURE 11.106
The anatomy of cricothyroidotomy.
Insertion of the tube.
The cricothyroid membrane (ligament) is incised through a horizontal incision close to the upper border of
cervical fasciae.
A vertical incision is made through the skin and superficial and deep
A.
B.
the cricoid cartilage. C.
pretracheal
layer of deep
cervical fascia
omohyoid muscle
sternothyroid muscle
sternocleidomastoid muscle
investing layer of
deep cervical fascia
platysma muscle
sternohyoid
muscle
isthmus
of thyroid
gland
anterior jugular vein
branch of superior
thyroid artery
thyroid gland
common
carotid
artery
internal
jugular
vein
deep cervical
lymph node
vagus nerve
sympathetic
trunk
esophagus
prevertebral
layer of
deep cervical
fascia
carotid sheath
C7
skin
FIGURE 11.107
heal ring. A vertical incision is made through the ring,
Cross section of the neck at the level of the second trac
and the tracheostomy tube is inserted.

656
CHAPTER 11
The Head and Neck
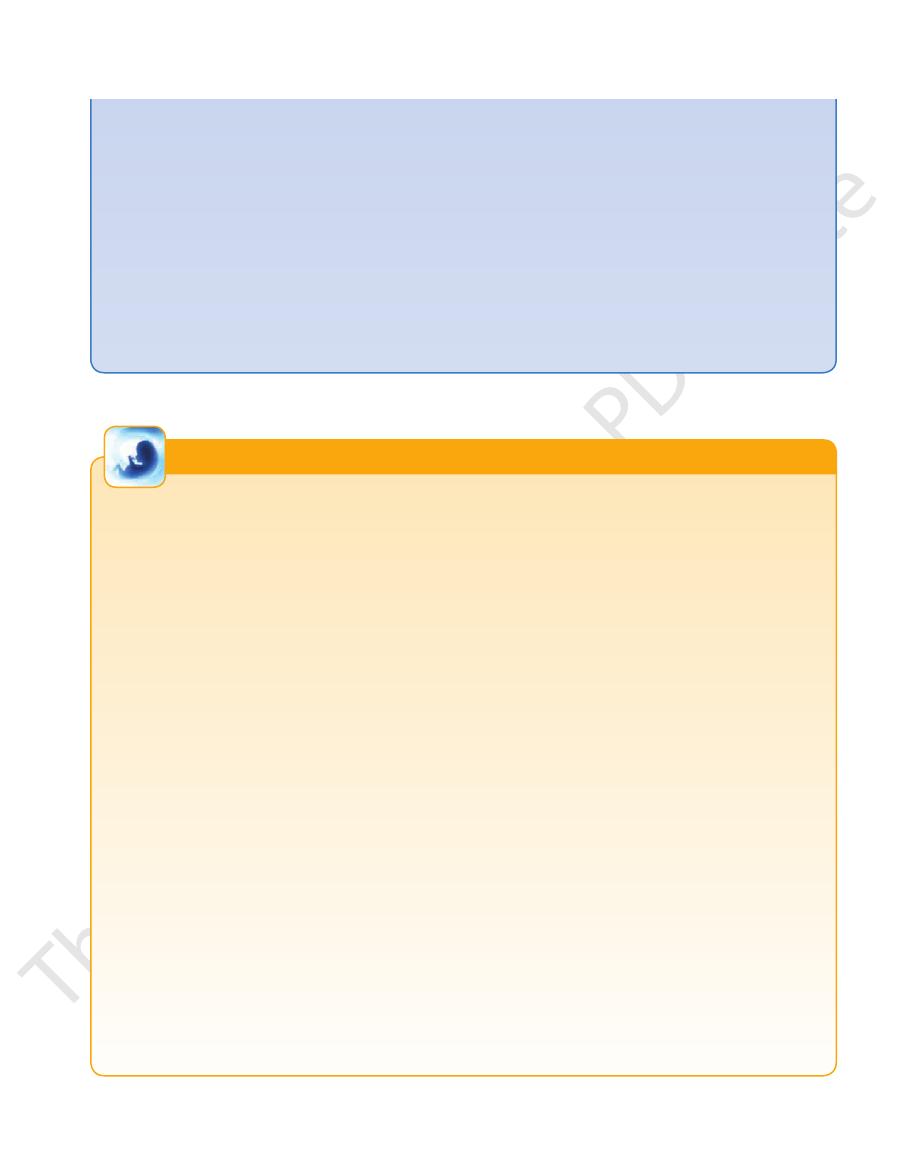
Development of the Pituitary Gland
rows, and finally disappears (Fig. 11.109). Rathke’s pouch now is
During the second month of development, Rathke’s pouch
), which grows inferiorly from the floor of the dien
The pituitary gland develops from two sources: a small ectoder-
mal diverticulum (Rathke’s pouch), which grows superiorly from
the roof of the stomodeum immediately anterior to the bucco-
pharyngeal membrane; and a small ectodermal diverticulum (the
infundibulum
-
cephalon of the brain (Fig. 11.109).
comes into contact with the anterior surface of the infundibu-
lum, and its connection with the oral epithelium elongates, nar-
a vesicle that flattens itself around the anterior and lateral sur
completely. Meanwhile, the infundibulum has differentiated into
the vesicle is reduced to a narrow cleft, which may disappear
cells later migrate anteriorly into the pars anterior. The cavity of
Some of the
The cells of the posterior wall of the vesicle never
superiorly and around the stalk of the infundibulum, forming the
the vesicle’s upper part, there is a cellular extension that grows
of the pituitary; from
faces of the infundibulum. The cells of the anterior wall of the
-
vesicle proliferate and form the pars anterior
pars tuberalis.
develop extensively; they form the pars intermedia.
the stalk and pars nervosa of the pituitary gland (Fig. 11.109).
E M B R Y O L O G I C N O T E S
posterior lobe of hypophysis cerebri
anterior lobe of
hypophysis
cerebri
pia mater
arachnoid mater
meningeal layer
of dura mater
endosteal layer
of dura mater
carotid sympathetic
nerve plexus
sphenoidal
air sinuses
maxillary division of
trigeminal nerve
internal carotid
artery
abducent
nerve
mandibular division
of trigeminal nerve
foramen
ovale
ophthalmic
division of
trigeminal
nerve
trochlear
nerve
oculomotor
nerve
temporal lobe of
cerebral
hemisphere
posterior
communicating
artery
middle
cerebral artery
anterior cerebral artery
optic
tract
third ventricle
infundibulum
diaphragma sellae
perforating arteries
cavernous sinus
subarachnoid space
FIGURE 11.108
y gland and the cavernous
Coronal section through the body of the sphenoid bone, showing the pituitar
tary gland, the islets of Langerhans of the pancreas, the
The pineal gland can influence the activities of the pitui
Functions of the Pineal Gland
by postganglionic sympathetic nerve fibers.
cells. The gland has a rich blood supply and is innervated
supported by glial
pinealocytes,
tially of groups of cells, the
ventricle of the brain (Fig. 11.13). The pineal consists essen
posteriorly from the posterior end of the roof of the third
The pineal gland is a small cone-shaped body that projects
Location and Description
sinuses. Note the position of the internal carotid artery and the cranial nerves.
Pineal Gland
-
-
Important Airway Distances
(Adult)
a
T A B L E 1 1 . 1 3
Average figures given ± 1 to 2 cm.
Airway
Distances
Incisor teeth to the vocal cords
5.9 in. (15 cm)
Incisor teeth to the carina
7.9 in. (20 cm)
External nares to the carina
11.8 in. (30 cm)
a

Basic Anatomy
657
buccopharyngeal membrane
stomodeum
infundibulum
Rathke's pouch
diencephalon
infundibulum
buccopharyngeal membrane
pharynx
mouth cavity
vesicle derived from
Rathke's pouch
infundibulum
buccopharyngeal
membrane
mouth cavity
pharynx
pars tuberalis
stalk
pars anterior
pars intermedia
pars nervosa
1
2
3
4
5
FIGURE 11.109
The different stages in the development of the pituitary gland shown in sagittal sections.
parathyroids, the adrenals, and the gonads. The pineal
gus and the trachea is the recurrent laryngeal nerve
laryngeal nerve. In the groove between the esopha
cricothyroid muscle and its nerve supply, the external
the esophagus. Associated with these structures are the
The larynx, the trachea, the pharynx, and
Medially:
nerve (Fig. 11.49)
carotid artery, the internal jugular vein, and the vagus
The carotid sheath with the common
Posterolaterally:
of the sternocleidomastoid (Fig. 11.49)
the omohyoid, the sternohyoid, and the anterior border
The sternothyroid, the superior belly of
Anterolaterally:
(Fig. 11.110).
levator glandulae thyroideae
dal lobe to the hyoid bone; if it is muscular, it is referred to
fibrous or muscular band frequently connects the pyrami
from the isthmus, usually to the left of the midline. A
is often present, and it projects upward
pyramidal lobe
second, third, and fourth tracheal rings (Fig. 11.110). A
extends across the midline in front of the
isthmus
The
fifth tracheal ring.
roid cartilage; its base lies below at the level of the fourth or
upward as far as the oblique line on the lamina of the thy
Each lobe is pear shaped, with its apex being directed
and the trachea.
of deep fascia. The sheath attaches the gland to the larynx
surrounded by a sheath derived from the pretracheal layer
by a narrow isthmus (Fig. 11.110). It is a vascular organ
The thyroid gland consists of right and left lobes connected
Location and Description
Thyroid Gland
the secretion of releasing factors by the hypothalamus.
inhibit the production of hormones or indirectly inhibit
fluid. Their actions are mainly inhibitory and either directly
organs via the bloodstream or through the cerebrospinal
secretions, produced by the pinealocytes, reach their target
-
-
as the
Relations of the Lobes
■
■
■
■
■
■
-
(Fig. 11.49).
(Fig. 11.110).
external laryngeal nerve
accompanied by the
carotid artery, descends to the upper pole of each lobe,
a branch of the external
superior thyroid artery,
The
another over the surface of the gland.
roidea ima. The arteries anastomose profusely with one
artery, the inferior thyroid artery, and sometimes the thy
to the thyroid gland are the superior thyroid
arteries
The
anastomose along its upper border.
The terminal branches of the superior thyroid arteries
trachea
The second, third, and fourth rings of the
Posteriorly:
jugular veins, fascia, and skin
The sternothyroids, sternohyoids, anterior
Anteriorly:
inferior thyroid arteries.
11.110) and the anastomosis between the superior and
riorly to the superior and inferior parathyroid glands (Fig.
The rounded posterior border of each lobe is related poste-
Relations of the Isthmus
■
■
■
■
Blood Supply
-
658
CHAPTER 11
The Head and Neck
anterior view
inferior thyroid vein
left brachiocephalic vein
trachea
esophagus
thyroidea ima artery
middle thyroid vein
lobe of
thyroid gland
isthmus of thyroid gland
common carotid
artery
superior thyroid vein
superior thyroid artery
internal jugular vein
pyramidal lobe
levator glandulae thyroideae
thyroid cartilage
lateral view of right lobe
apex
capsule of
pretracheal
fascia
capsule of
thyroid gland
lobe of
thyroid gland
isthmus of
thyroid gland
base
inferior
parathyroid
gland
superior
parathyroid
gland
cricothyroid
muscle
cricoid
cartilage
FIGURE 11.110
The blood supply and venous drainage of the thyroid gland.
descend to the paratracheal nodes.
into the deep cervical lymph nodes. A few lymph vessels
The lymph from the thyroid gland drains mainly laterally
Lymph Drainage
phalic vein in the thorax.
They drain into the left brachioce
front of the trachea.
the two sides anastomose with one another as they descend
inferior thyroid (Fig. 11.110). The inferior thyroid veins of
thyroid, which drains into the internal jugular vein; and the
roid, which drains into the internal jugular vein; the middle
from the thyroid gland are the superior thy
veins
The
front of the trachea to the isthmus (Fig. 11.110).
chiocephalic artery or the arch of the aorta. It ascends in
if present, may arise from the bra
thyroidea ima,
The
artery, or it may pass between its branches.
crosses either in front of or behind the
laryngeal nerve
recurrent
to reach the posterior border of the gland. The
cricoid cartilage. It then turns medially and downward
vical trunk, ascends behind the gland to the level of the
a branch of the thyrocer
inferior thyroid artery,
The
-
-
-
in
-
Nerve Supply
Superior, middle, and inferior cervical sympathetic
tonin, which lowers the level of blood calcium.
The parafollicular cells produce the hormone thyrocalci
increase the metabolic activity of most cells in the body.
The thyroid hormones, thyroxine and triiodothyronine,
Functions of the Thyroid Gland
ganglia
-
Swellings of the Thyroid Gland and Movement on
The attachment of the sternothyroid muscles to the thyroid
any pathologic neck swelling that is part of the thyroid gland will
the larynx in swallowing. This information is important because
cheal fascia. This tethers the gland to the larynx and the trachea
The thyroid gland is invested in a sheath derived from the pretra
Swallowing
-
and explains why the thyroid gland follows the movements of
move upward when the patient is asked to swallow.
The Thyroid Gland and the Airway
The close relationship between the trachea and the lobes of the
thyroid gland commonly results in pressure on the trachea in
patients with pathologic enlargement of the thyroid.
Retrosternal Goiter
cartilage effectively binds down the thyroid gland to the lar-
C L I N I C A L N O T E S
(continued)
Basic Anatomy
659
ynx and limits upward expansion of the gland. There being
no limitation to downward expansion, it is not uncommon
can be damaged during thyroidectomy operations. The superior
and cause dangerous dyspnea; it can also cause severe
enlargement of the thyroid gland) can compress the trachea
ward behind the sternum. A retrosternal goiter (any abnormal
for a pathologically enlarged thyroid gland to extend down-
venous compression.
Thyroid Arteries and Important Nerves
It should be remembered that the two main arteries supplying
the thyroid gland are closely related to important nerves that
thyroid artery on each side is related to the external laryngeal
nerve, which supplies the cricothyroid muscle. The terminal
branches of the inferior thyroid artery on each side are related to
the recurrent laryngeal nerve. Damage to the external laryngeal
superior mediastinum because they have been pulled down into
mon for the surgeon to find the inferior parathyroid glands in the
left undisturbed so that the parathyroid glands are not damaged.
closely related to the posterior surface of the thyroid gland. In
The parathyroid glands are usually four in number and are
nerve results in an inability to tense the vocal folds and in
hoarseness. For the results of damage to the recurrent laryngeal
nerve, see page 650.
Thyroidectomy and the Parathyroid Glands
partial thyroidectomy, the posterior part of the thyroid gland is
The development of the inferior parathyroid glands is closely
associated with the thymus. For this reason, it is not uncom-
the thorax by the thymus.
Development of the Thyroid Gland
of the hyoid bone, this may have to be excised also to prevent
surgically. Since remnants of the duct often traverse the body
enlarges, it is prone to infection and so it should be removed
of epithelium that continues to secrete mucus. As the cyst
line and develops as a result of persistence of a small amount
(Figs. 11.112 and 11.114). They occur most commonly in the
Cysts may occur at any point along the thyroglossal tract
assumed that this thyroid tissue arises from entodermal cells
relation to the trachea or bronchi or even the esophagus. It is
the base of the tongue and the trachea (Fig. 11.112).
which
parafollicular cells,
thyroid gland, where they form the
and neural crest cells are believed to be incorporated into the
cular mesenchymal tissue, the mass becomes broken up into
mass of cells. Later, as a result of invasion by surrounding vas
In the earliest stages, the thyroid gland consists of a solid
and disappears. The site of origin of the thyroglossal duct on the
of cells, and as a result of epithelial proliferation, the bilobed ter
Later, this thickening becomes a diverticulum that grows inferi
The thyroid gland begins to develop during the third week as
an entodermal thickening in the midline of the floor of the phar-
ynx between the tuberculum impar and the copula (Fig. 11.111).
-
orly into the underlying mesenchyme and is called the thyroglos-
sal duct. As development continues, the duct elongates, and its
distal end becomes bilobed. Soon, the duct becomes a solid cord
-
minal swellings expand to form the thyroid gland.
The thyroid gland now migrates inferiorly in the neck and
passes either anterior to, posterior to, or through the developing
body of the hyoid bone. By the seventh week, it reaches its final
position in relation to the larynx and trachea. Meanwhile, the
solid cord connecting the thyroid gland to the tongue fragments
tongue remains as a pit called the foramen cecum. The thyroid
gland may now be divided into a small median isthmus and two
large lateral lobes (Fig. 11.111).
-
plates and cords and finally into small clusters of cells. By the
third month, colloid starts to accumulate in the center of each
cluster so that follicles are formed. The fibrous capsule and con-
nective tissue develop from the surrounding mesenchyme.
The ultimobranchial bodies (from the fifth pharyngeal pouch)
produce calcitonin.
Agenesis of the Thyroid
Failure of development of the thyroid gland may occur and is the
commonest cause of cretinism.
Incomplete Descent of the Thyroid
The descent of the thyroid may be arrested at any point between
Lingual thy-
roid is the most common form of incomplete descent (Fig. 11.113).
The mass of tissue found just beneath the foramen cecum may
be sufficiently large to obstruct swallowing in the infant.
Ectopic Thyroid Tissue
Ectopic thyroid tissue is occasionally found in the thorax in
displaced during the formation of the laryngotracheal tube or
from entodermal cells of the developing esophagus
Persistent Thyroglossal Duct
Conditions related to a persistence of the thyroglossal duct usu-
ally appear in childhood, in adolescence, or in young adults.
Thyroglossal Cyst
region below the hyoid bone. Such a cyst occupies the mid-
recurrence.
Thyroglossal Sinus (Fistula)
Occasionally, a thyroglossal cyst ruptures spontaneously, pro-
ducing a sinus (Fig. 11.112). Usually, this is a result of an infec-
tion of a cyst. All remnants of the thyroglossal duct should be
removed surgically.
E M B R Y O L O G I C N O T E S
660
CHAPTER 11
The Head and Neck
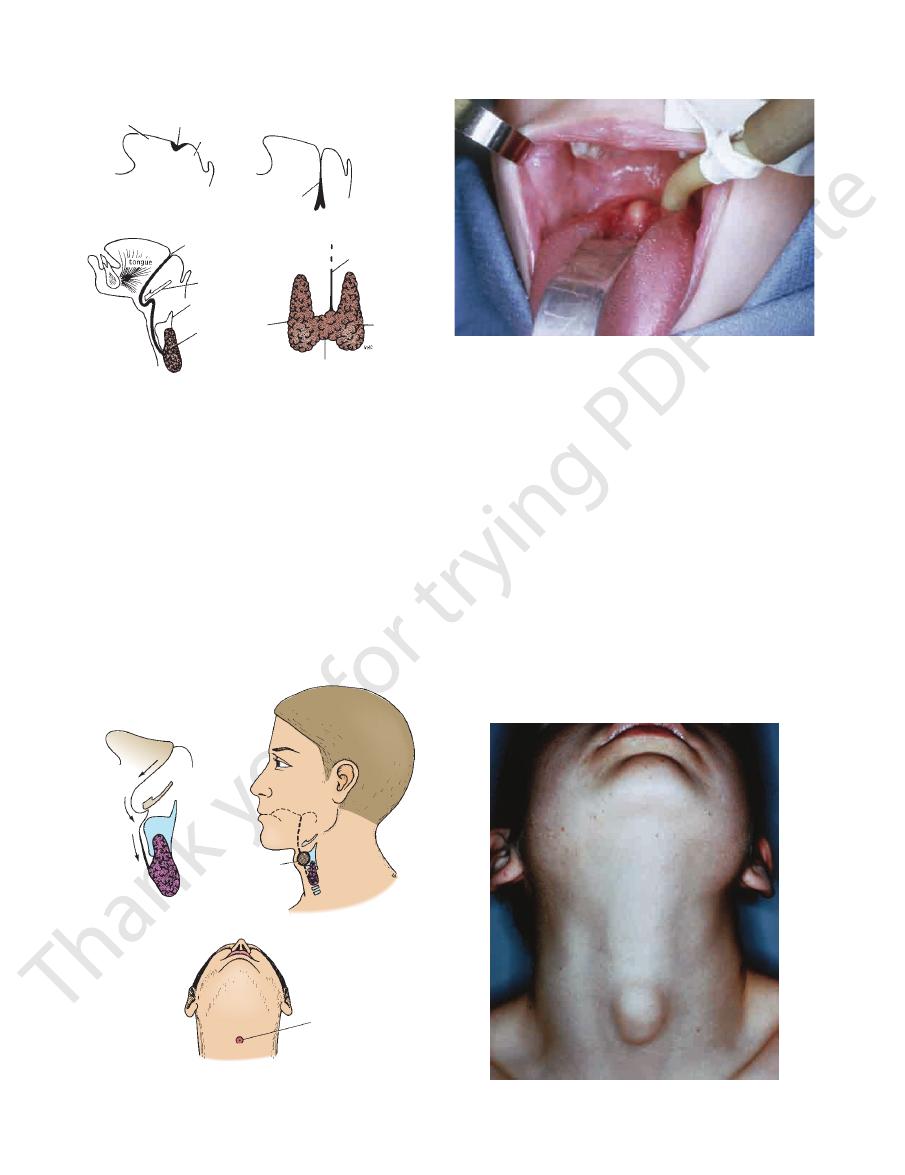
tuberculum
impar entodermal thickening
copula
tongue
tongue
thyroglossal duct
foramen cecum
hyoid bone
thyroid cartilage
remains of
thyroglossal
duct
lateral
lobe
isthmus
A
B
C
D
tongue
thyroid gland
FIGURE 11.111
The different stages in the development of
thyroglossal duct above the isthmus.
thyroid gland as seen from in front. Note the remains of the
The fully developed
thyroid gland as it migrates inferiorly.
tion of the tongue and neck showing the path taken by the
Sagittal sec
the development of the thyroglossal duct.
Sagittal section of the tongue showing
an entodermal thickening between the tuberculum impar
Sagittal section of the tongue showing
the thyroid gland. A.
and the copula. B.
C.
-
D.
thyroglossal
as it descends in the neck
thyroid gland
path taken
thyroglossal cyst
anterior
tongue
by
fistula
FIGURE 11.112
A thyroglossal cyst in the midline in the neck
and a thyroglossal fistula.
FIGURE 11.113
Lingual thyroid. (Courtesy of J. Randolph.)
FIGURE 11.114
A thyroglossal cyst. (Courtesy of L. Thompson.)
is into the superior, middle, and inferior thyroid veins.
superior and inferior thyroid arteries. The venous drainage
The arterial supply to the parathyroid glands is from the
rior mediastinum in the thorax.
inferior thyroid veins, or they may even reside in the supe
distance caudal to the thyroid gland, in association with the
outside the fascial sheath. Sometimes, they are found some
the fascial sheath, embedded in the thyroid substance, or
the inferior poles of the thyroid gland. They may lie within
usually lie close to
two inferior parathyroid glands
The
posterior border of the thyroid gland.
stant in position and lie at the level of the middle of the
are the more con
two superior parathyroid glands
The
thyroid gland, lying within its fascial capsule (Fig. 11.110).
ber and are closely related to the posterior border of the
6 mm long in their greatest diameter. They are four in num
The parathyroid glands are ovoid bodies measuring about
Location and Description
Parathyroid Glands
-
-
-
Blood Supply
Basic Anatomy
661
Development of the Parathyroid Glands
pulled inferiorly into the lower part of the neck or thoracic cavity.
has been demonstrated in individuals with idiopathic hypopara
rior aspect of the lateral lobe of the thyroid gland on each side, at
the pharyngeal wall and take up their final position on the poste
develop as a proliferation of entodermal cells in the fourth pha
develop as the result of proliferation of entodermal cells in the
The pair of inferior parathyroid glands, known as parathyroid III,
third pharyngeal pouch on each side. As the thymic diverticu-
lum on each side grows inferiorly in the neck, it pulls the inferior
parathyroid with it, so that it finally comes to rest on the posterior
surface of the lateral lobe of the thyroid gland near its lower pole
and becomes completely separate from the thymus (Fig. 11.115).
The pair of superior parathyroid glands, parathyroid IV,
-
ryngeal pouch on each side. These loosen their connection with
-
about the level of the isthmus (Fig. 11.115).
In the earliest stages, each gland consists of a solid mass of
clear cells, the chief cells. In late childhood, acidophilic cells,
the oxyphil cells, appear. The connective tissue and vascu-
lar supply are derived from the surrounding mesenchyme. It is
believed that the parathyroid hormone is secreted early in fetal
life by the chief cells to regulate calcium metabolism. The oxyphil
cells are thought to be nonfunctioning chief cells.
Absence and Hypoplasia of the Parathyroid Glands
Agenesis or incomplete development of the parathyroid glands
-
thyroidism.
Ectopic Parathyroid Glands
The close relationship between the parathyroid III and the devel-
oping thymus explains the frequent finding of parathyroid tis-
sue in the superior mediastinum of the thorax (Fig. 11.115). If the
parathyroid glands remain attached to the thymus, they may be
Moreover, this also explains the variable position of the inferior
parathyroid glands in relation to the lower poles of the lateral
lobes of the thyroid gland.
E M B R Y O L O G I C N O T E S
Lymph Drainage
the transverse processes of the next five cervical vertebrae
and extends from the transverse process of the atlas and
The scalenus medius lies behind the scalenus anterior
Scalenus Medius
neck, its relations should be understood. See page 592.
Because the muscle is an important landmark in the
almost vertically from the vertebral column to the 1st rib.
fully described on page 592. It is deeply placed and descends
to the understanding of the root of the neck and has been
The scalenus anterior muscle (Fig. 11.57) is a key muscle
Scalenus Anterior
Muscles of the Root of the Neck
immediately above the inlet into the thorax (Fig. 11.16).
The root of the neck can be defined as the area of the neck
controlled by the calcium levels in the blood.
of the kidney. The secretion of the parathyroid hormone is
sorption of phosphate in the proximal convoluted tubules
tubules of the kidney. It also strongly diminishes the reab
the reabsorption of calcium in the proximal convoluted
absorption of dietary calcium from the small intestine and
the blood. The parathyroid hormone also stimulates the
ing the bone calcium and increasing the calcium levels in
stimulates osteoclastic activity in bones, thus mobiliz
which
parathyroid hormone,
The chief cells produce the
Functions of the Parathyroid Glands
Superior or middle cervical sympathetic ganglia.
Deep cervical and paratracheal lymph nodes.
Nerve Supply
-
-
The Root of the Neck
(Fig.
nward and laterally to be inserted into the
11.57) dow
scalenus anterior muscle, and at the outer border of the 1st
It passes upward and laterally as a gentle curve behind the
artery, behind the right sternoclavicular joint (Fig. 11.57).
The right subclavian artery arises from the brachiocephalic
Subclavian Artery
ply, and their action, see Table 11.5.
For a summary of muscles of the neck, their nerve sup
chial plexus and the subclavian artery.
clavian artery. The muscle lies behind the roots of the bra
upper surface of the 1st rib behind the groove for the sub-
-
-
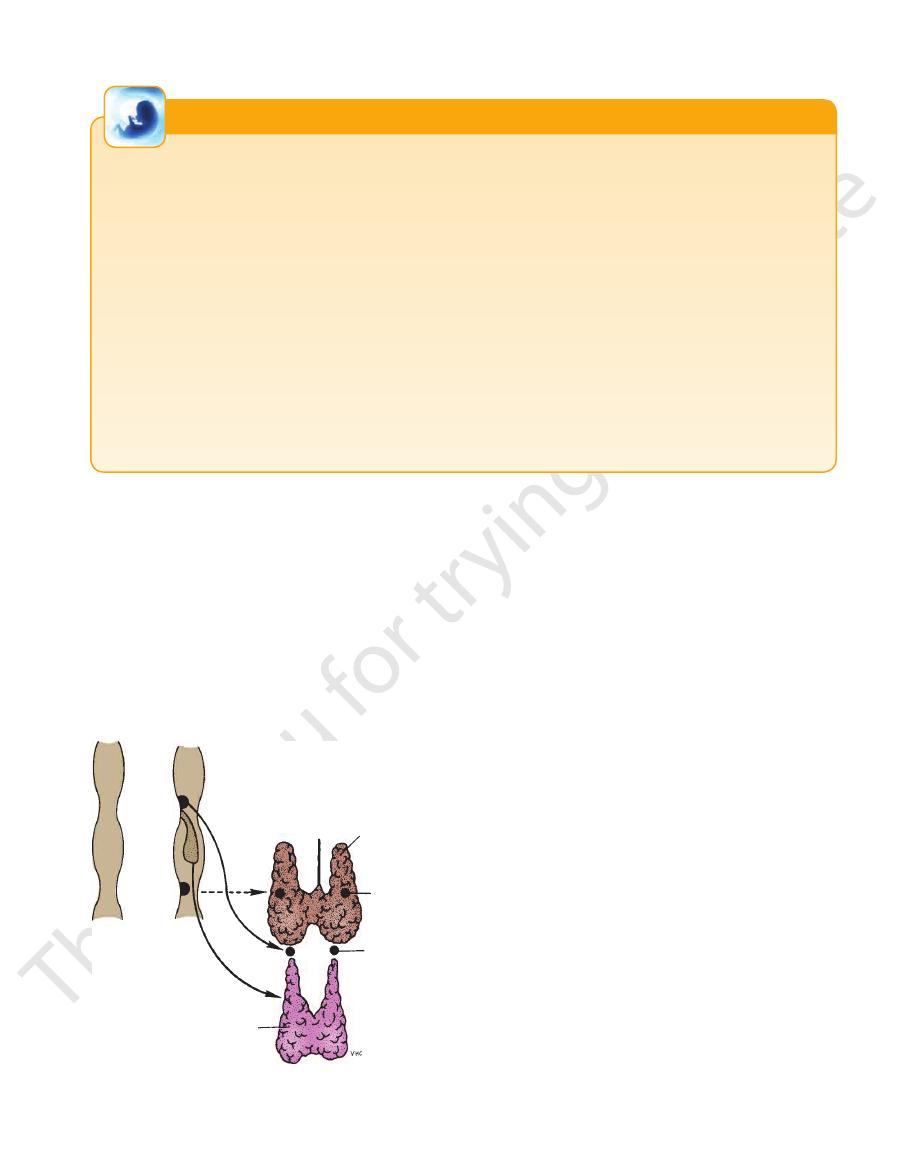
pharynx
III
IV
thyroid gland
parathyroid IV
parathyroid III
thymus
FIGURE 11.115
Parathyroid glands taking up their final posi
tions in the neck.
-
662
CHAPTER 11
The Head and Neck
of the subclavian or internal jugular veins.
chiocephalic vein. It may, however, end in the terminal part
downward and drains into the beginning of the left bra
reaching the medial border of the scalenus anterior, it turns
bends laterally behind the carotid sheath (Fig. 11.57). On
transverse process of the seventh cervical vertebra. Here, it
margin of the esophagus until it reaches the level of the
the root of the neck, it continues to ascend along the left
passing upward along the left margin of the esophagus. At
the left. On reaching the superior mediastinum, it is found
through the posterior mediastinum, inclining gradually to
through the aortic opening in the diaphragm and ascends
of the cisterna chyli (see page XXX). It enters the thorax
The thoracic duct begins in the abdomen at the upper end
jugular vein to form the brachiocephalic vein.
medial border of the scalenus anterior, it joins the internal
rib as a continuation of the axillary vein (Fig. 11.57). At the
The subclavian vein begins at the outer border of the first
Subclavian Vein
been described on page 599.
The relations and branches of the subclavian arteries have
similar to that of the right subclavian artery (Fig. 11.57).
the root of the neck and then arches laterally in a manner
arises from the arch of the aorta in the thorax. It ascends to
rib it becomes the axillary artery. The left subclavian artery
The Thoracic Duct
-
extend up into the root of the neck on each side. Covered by
Pleura and Lung Injuries in the Root of the Neck
The cervical dome of the pleura and the apex of the lung
the suprapleural membrane, they lie behind the subclavian
artery. A penetrating wound above the medial end of the clav-
icle may involve the apex of the lung.
C L I N I C A L N O T E S
natomy
aphic
adiog
R
R
a
Radiographic Appearance of the
the choroid plexuses also become calcified frequently.
normal adults. It lies in the midline. The falx cerebri and
dition. The pineal gland, for example, is calcified in 50% of
structures may indirectly give evidence of a pathologic con
become calcified in the adult, and the displacement of such
mass. However, a few normal structures within the skull
muscles, tendons, and nerves blend into a homogeneous
centrates mainly on the bony structures because the brain,
Routine radiologic examination of the head and neck con
Head and Neck
-
-
scan (Figs. 11.125, 11.126, and 11.127).
matter in the brain, its use can be more revealing than a CT
it provides better differentiation between gray and white
lesions. MRI is absolutely safe to the patient, and because
MRI is also commonly used for detection of intracranial
ples of CT scans of the head can be seen in Figure 11.124.
lesions. It is safe and provides accurate information. Exam
CT is commonly used for the detection of intracranial
Computed Tomography Scans
be seen in Figures 11.120, 11.121, 11.122, and 11.123.
clots, or abscesses. Examples of cerebral arteriograms can
tion of space-occupying lesions such as tumors, blood
detect abnormalities of the cerebral arteries and localiza
The technique of cerebral arteriography can be used to
studied in Figures 11.116, 11.117, 11.118, and 11.119.
straight posteroanterior views and lateral views can be
The radiographic appearances of the skull as seen on
ods of studying the intracranial contents.
scans has provided physicians with safe and accurate meth
The introduction of CT and MRI
(cerebral arteriogram).
contrast media into the arterial system leading to the brain
The brain can be studied indirectly by the injection of
-
Radiographic Appearance of the
Skull
Cerebral Arteriography
-
-
Magnetic Resonance Imaging
natomy
face
s
uR
a
Surface Landmarks of the Head
right and left cerebral hemispheres.
which separates the
longitudinal cerebral fissure,
superior sagittal sinus,
falx cerebri,
of the underlying
the superior aspect of the head would indicate the position
ing the nasion to the external occipital protuberance over
the spinous processes of the cervical vertebrae. A line join
runs down the back of the neck, connecting the skull to
to the ligamentum nuchae, which is a large ligament that
at the junction of the head and neck and gives attachment
part of the occipital bone (Fig. 11.128). It lies in the midline
This is a bony prominence in the middle of the squamous
the nose (Fig. 11.128).
The nasion is the depression in the midline at the root of
Nasion
External Occipital Protuberance
-
the
and the
