
Basic Anatomy
605
Clinical Significance of the Cervical Lymph Nodes
the pharynx, the cervical part of the esophagus, and the external
ined, including the face, scalp, tongue, mouth, tonsil, and
cally the various areas known to drain into a node to discover
or the tongue. An infected tooth of the upper or lower jaw may
pathologic condition in the scalp, the face, the maxillary sinus,
example, an enlarged submandibular node can be caused by a
of the body that drains its lymph into a particular node. For
determine the cause and be knowledgeable about the area
an enlarged lymph node. It is the physician’s responsibility to
great clinical importance. Examination of a patient may reveal
Knowledge of the lymph drainage of an organ or region is of
be responsible. Often, a physician has to search systemati-
the cause.
Examination of the Deep Cervical Lymph Nodes
Lymph nodes in the neck should be examined from behind the
patient. The examination is made easier by asking the patient to
flex the neck slightly to reduce the tension of the muscles. The
groups of nodes should be examined in a definite order to avoid
omitting any.
After the identification of enlarged lymph nodes, pos-
sible sites of infection or neoplastic growth should be exam-
pharynx.
Carcinoma Metastases in the Deep Cervical Lymph
Node
In the head and neck, all the lymph ultimately drains into the
deep cervical group of nodes. Secondary carcinomatous depos-
its in these nodes are common. The primary growth may be easy
to find. On the other hand, at certain anatomic sites, the primary
growth may be small and overlooked, for example, in the larynx,
auditory meatus. The bronchi, breast, and stomach are some-
times the site of the primary tumor. In these cases, the second-
ary growth has spread far beyond the local lymph nodes.
When cervical metastases occur, the surgeon usually
decides to perform a block dissection of the cervical nodes. This
procedure involves the removal en bloc of the internal jugular
vein, the fascia, the lymph nodes, and the submandibular sali-
vary gland. The aim of the operation is removal of all the lymph
tissues on the affected side of the neck. The carotid arteries
and the vagus nerve are carefully preserved. It is often neces-
sary to sacrifice the hypoglossal and vagus nerves, which may
be involved in the cancerous deposits. In patients with bilateral
spread, a bilateral block dissection may be necessary. An inter-
val of 3 to 4 weeks is necessary before removing the second
internal jugular vein.
C L I N I C A L N O T E S
Cranial Nerves
The cranial nerves are named as follows:
Organization of the Cranial Nerves
I. Olfactory
II. Optic
III. Oculomotor
IV. Trochlear
V. Trigeminal
VI. Abducent
VII. Facial
VIII. Vestibulocochlear
IX.
yngeal
Glossophar
X. Vagus
XI. Accessory
XII. Hypoglossal
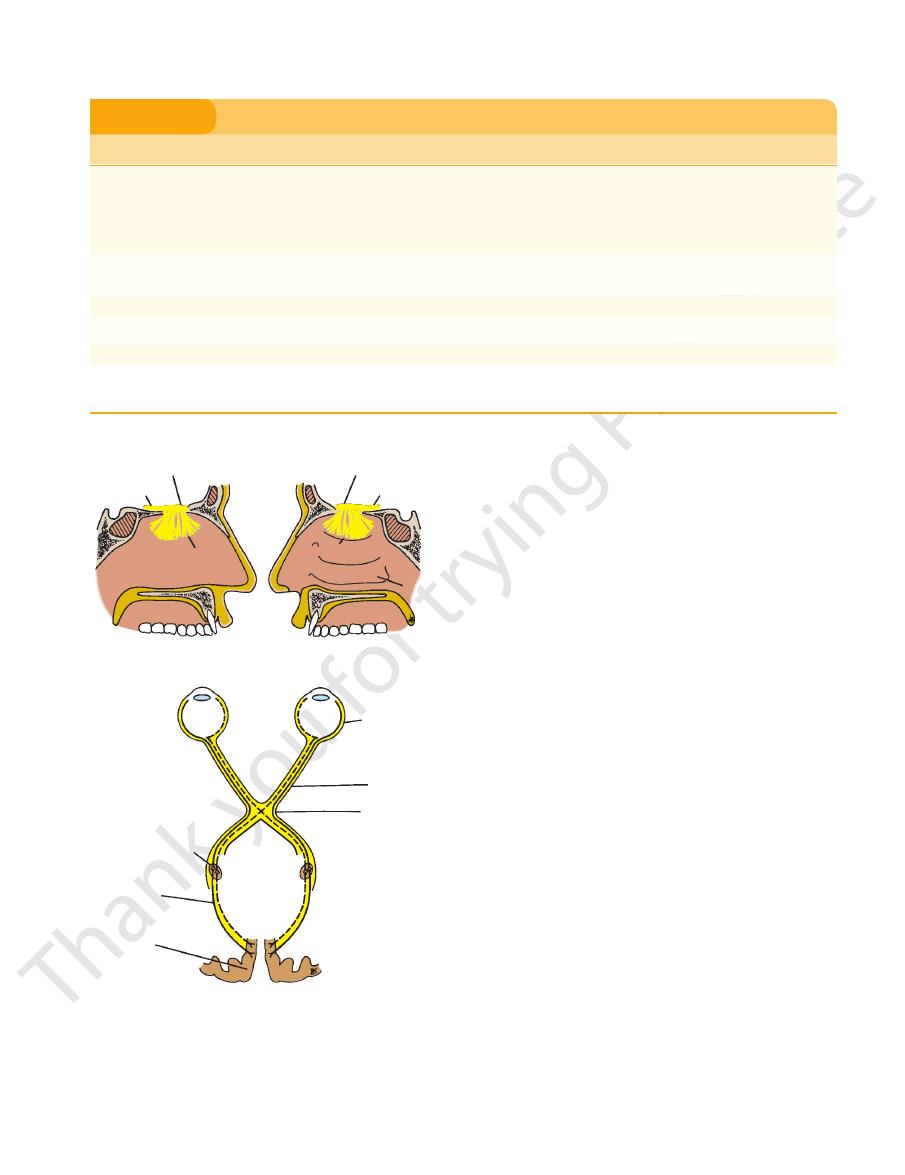
olfactory bulb
enter the
openings of the cribriform plate of the ethmoid bone to
Bundles of these olfactory nerve fibers pass through the
cavity above the level of the superior concha (Fig. 11.63).
mucous membrane is situated in the upper part of the nasal
in the olfactory mucous membrane. The olfactory
cells
olfactory receptor nerve
The olfactory nerves arise from
Olfactory Nerves
are summarized in Table 11.6.
the skull through which the nerves leave the cranial cavity
of the cranial nerves, their functions, and the openings in
the remaining nerves are mixed. The different components
accessory, and hypoglossal nerves are entirely motor; and
entirely sensory; the oculomotor, trochlear, abducent,
The olfactory, optic, and vestibulocochlear nerves are
in the cranial cavity. The
ry
olfacto
bulb is connected to the olfactory area of the cerebral
ex
cort
the back of the eyeball and leaves the orbital cavity through
of the retina. The optic nerve emerges from
ganglionic layer
The optic nerve is composed of the axons of the cells of the
Optic Nerve
olfactory tract
by the
.
the optic canal to enter the cranial cavity (Fig. 11.11). The
the midbrain (Fig. 11.64). It passes forward between the pos
The oculomotor nerve emerges on the anterior surface of
Oculomotor Nerve
of the cerebral hemisphere (Fig. 11.63).
visual cortex
and terminate
optic radiation
body pass posteriorly as the
The axons of the nerve cells of the lateral geniculate
superior colliculus and are concerned with light reflexes.
11.63). A few fibers pass to the pretectal nucleus and the
(Fig.
lateral geniculate body
apsing with nerve cells in the
side. Most of the fibers of the optic tract terminate by syn
each retina pass posteriorly in the optic tract of the same
opposite side, whereas the fibers from the lateral half of
of the
optic tract
retina cross the midline and enter the
In the chiasma, the fibers from the medial half of each
side to form the optic chiasma (Fig. 11.63).
optic nerve then unites with the optic nerve of the opposite
-
in the
-
terior cerebral and superior cerebellar arteries (Fig. 11.11).
It then continues into the middle cranial fossa in the lateral
wall of the cavernous sinus. Here, it divides into a superior
606
CHAPTER 11
The Head and Neck
Cranial Nerves
T A B L E 1 1 . 6
V. Trigeminal
IV. Trochlear
Vision
Nerve
Components
Function
Opening in Skull
I. Olfactory
Sensory
Smell
Openings in cribriform plate of
ethmoid
II. Optic
Sensory
Optic canal
III. Oculomotor
Motor
Lifts upper eyelid, turns eyeball upward,
downward, and medially; constricts pupil;
accommodates eye
Superior orbital fissure
Motor
Assists in turning eyeball downward and
laterally
Superior orbital fissure
Ophthalmic division
Sensory
Cornea, skin of forehead, scalp, eyelids, and
nose; also mucous membrane of paranasal
sinuses and nasal cavity
Superior orbital
fissure
Maxillary
division
Sensory
Skin of face over maxilla and the upper lip;
teeth of upper jaw; mucous membrane of
nose, the maxillary air sinus, and palate
Foramen rotundum
Mandibular
division
VIII. Vestibulocochlear
Taste from anterior two thirds of tongue, floor
Motor
Muscles of mastication, mylohyoid, anterior
belly of digastric, tensor veli palatini, and
tensor tympani
Foramen ovale
Sensory
Skin of cheek, skin over mandible, lower lip,
and side of head; teeth of lower jaw and
temporomandibular joint; mucous mem-
brane of mouth and anterior two thirds of
tongue
VI. Abducent
Motor
Lateral rectus muscle: turns eyeball laterally
Superior orbital fissure
VII. Facial
Motor
Muscles of face, cheek, and scalp; stapedius
muscle of middle ear; stylohyoid; and poste-
rior belly of digastric
Internal acoustic meatus, facial
canal, stylomastoid foramen
Sensory
of mouth, and palate
Secretomotor
parasympathetic
Submandibular and sublingual salivary glands,
lacrimal gland, and glands of nose and
palate
Vestibular
Sensory
Position and movement of head
Internal acoustic meatus
Cochlear
Sensory
Hearing
IX. Glossopharyngeal
Motor
Stylopharyngeus muscle: assists swallowing
Secretomotor
parasympathetic
Parotid salivary gland
Jugular foramen
Sensory
General sensation and taste from posterior
third of tongue and pharynx; carotid sinus
and carotid body
Basic Anatomy
607
Cranial Nerves (continued )
T A B L E 1 1 . 6
olfactory bulb
olfactory tract
olfactory nerves
nasal septum
olfactory bulb
olfactory tract
olfactory nerves
inferior
concha
right eyeball
and retina
optic nerve
optic chiasma
visual
cortex
optic
radiation
lateral geniculate
body
A
B
FIGURE 11.63
A.
which enter the orbital cavity
inferior ramus,
nerve and its connections.
The optic
nasal septum and the lateral wall of the nose.
Distribution of the olfactory nerves on the
B.
and an
through the superior orbital fissure (Fig. 11.18).
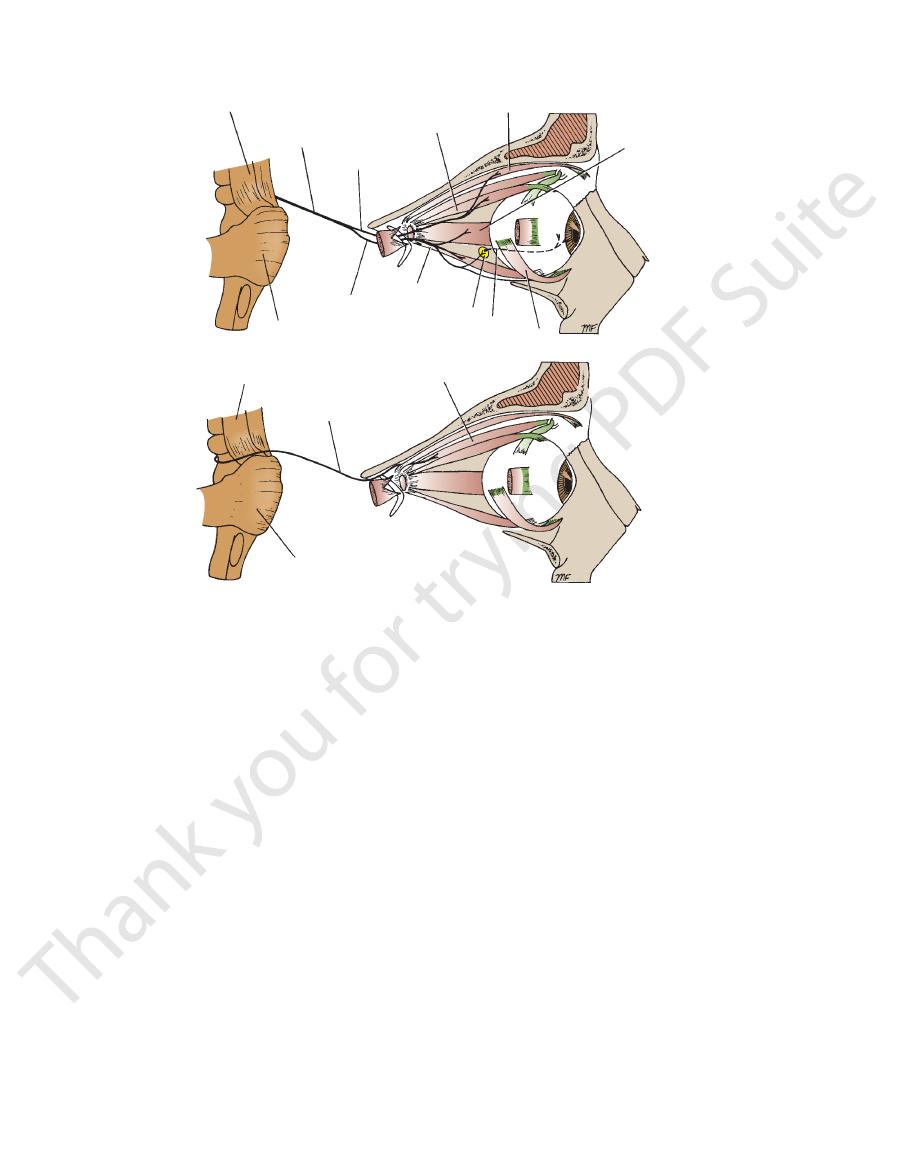
The superior oblique muscle of the eyeball (extrinsic
The trochlear nerve supplies:
through the superior orbital fissure (Figs. 11.11 and 11.18).
the lateral wall of the cavernous sinus and enters the orbit
It then passes forward through the middle cranial fossa in
leaves the posterior surface of the midbrain (Fig. 11.64).
nerves. Having crossed the nerve of the opposite side, it
The trochlear nerve is the most slender of the cranial
Trochlear Nerve
and accommodation of the eye.
upward, downward, and medially; constricting the pupil;
responsible for lifting the upper eyelid; turning the eye
The oculomotor nerve, therefore, is entirely motor. It is
(Fig. 11.19).
short ciliary nerves
the eyeball in the
and reach
ciliary ganglion
These fibers synapse in the
parasympathetic component of the oculomotor nerve.
lae of the iris and the ciliary muscles are supplied by the
The constrictor pupil
The intrinsic muscles of the eye:
tus, and inferior oblique (Fig. 11.64; see also Figs. 11.18
superioris, superior rectus, medial rectus, inferior rec
the levator palpebrae
The extrinsic muscles of the eye:
The oculomotor nerve supplies the following:
■
■
-
and 11.19)
■
■
-
muscle) (Fig. 11.20)
Trigeminal Nerve
the eye downward and laterally.
The trochlear nerve is entirely motor and assists in turning
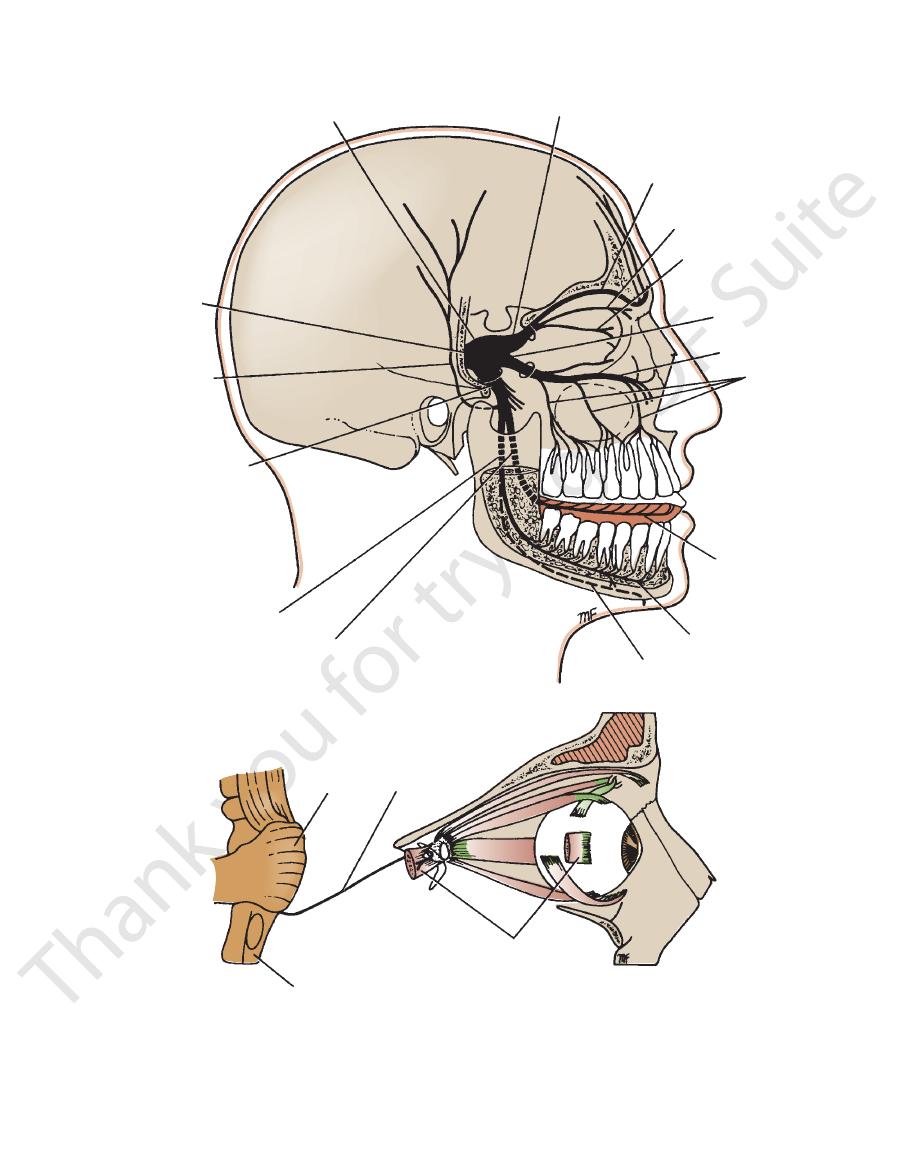
The trigeminal nerve is the largest cranial nerve (Fig. 11.65).
trigeminal
the large sensory root expands to form the
part of the temporal bone in the middle cranial fossa. Here,
the posterior cranial fossa, to reach the apex of the petrous
and it passes forward, out of
sensory root,
and a large
root
motor
It leaves the anterior aspect of the pons as a small
Taste from epiglottis and vallecula and afferent
X. Vagus
Nerve
Components
Function
Opening in Skull
Motor
Constrictor muscles of pharynx and intrinsic
muscles of larynx; involuntary muscle of
trachea and bronchi, heart, alimentary tract
from pharynx to splenic flexure of colon;
liver and pancreas
Jugular foramen
Sensory
fibers from structures named above
XI. Accessory
Cranial root
Motor
Muscles of soft palate, pharynx, and larynx
Jugular foramen
Spinal root
Motor
Sternocleidomastoid and trapezius muscles
XII. Hypoglossal
Motor
Muscles of tongue controlling its shape and
movement (except palatoglossus )
Hypoglossal canal
608
CHAPTER 11
The Head and Neck
midbrain
oculomotor nerve
superior ramus
superior rectus
levator palpebrae superioris
medial rectus
inferior oblique
short ciliary nerve
ciliary ganglion
inferior rectus
inferior ramus
pons
midbrain
trochlear nerve
superior oblique
pons
A
B
FIGURE 11.64
A.
Origin and distribution of the trochlear nerve.
Origin and distribution of the oculomotor nerve. B.
ganglion
of the face and the side of the nose.
the infraorbital foramen. It gives sensory fibers to the skin
the infraorbital groove, and it emerges on the face through
(Fig. 11.19). It then continues as the infraorbital nerve in
fossa to enter the orbit through the inferior orbital fissure
men rotundum (Fig. 11.11) and crosses the pterygopalatine
of the cavernous sinus and leaves the skull through the fora
the middle cranial fossa. It passes forward in the lateral wall
The maxillary nerve arises from the trigeminal ganglion in
Maxillary Nerve (V2)
ethmoid and sphenoid sinuses
that is sensory to the
Posterior ethmoidal nerve
that supplies the skin of the eyelids
Infratrochlear nerve
nea (Fig. 11.20)
the dilator pupillae muscle and sensory fibers to the cor
that contain sympathetic fibers to
Long ciliary nerves
to the ciliary ganglion (Fig. 11.20)
Sensory fibers
the following:
Its branches include
external nasal nerve.
the nose with the
and it then supplies the skin of the tip of
nasal branches
internal
crista galli to enter the nasal cavity. It gives off two
nial cavity. It then descends through a slit at the side of the
through the anterior ethmoidal foramen to enter the cra
anterior ethmoid nerve
(Fig. 11.20), and continues as the
forward on the upper border of the medial rectus muscle
crosses the optic nerve, runs
nasociliary nerve
The
air sinus and the skin of the forehead and the scalp.
These nerves leave the orbital cavity and supply the frontal
(Fig. 11.20).
supratrochlear nerves
and
supraorbital
the levator palpebrae superioris muscle and divides into
runs forward on the upper surface of
frontal nerve
The
the upper eyelid.
gland and gives branches to the conjunctiva and the skin of
lacrimal gland. The lacrimal nerve then enters the lacrimal
contains the parasympathetic secretomotor fibers to the
zygomaticotemporal branch of the maxillary nerve, which
the lateral rectus muscle (Fig. 11.18). It is joined by the
runs forward on the upper border of
lacrimal nerve
The
Branches
enter the orbital cavity through the superior orbital fissure.
branches, the lacrimal, frontal, and nasociliary nerves, which
ous sinus in the middle cranial fossa and divides into three
11.50). It runs forward in the lateral wall of the cavern
The ophthalmic nerve is purely sensory (Figs. 11.65 and
Ophthalmic Nerve (V1)
(Figs. 11.11 and 11.65).
(V3) nerves arise from the anterior border of the ganglion
it. The ophthalmic (V1), maxillary (V2), and mandibular
below the sensory ganglion and is completely separate from
The motor root of the trigeminal nerve is situated
cave.
trigeminal
lies within a pouch of dura mater called the
(Figs. 11.11 and 11.65). The trigeminal ganglion
-
the
-
■
■
■
■
-
■
■
■
■
-
Basic Anatomy
609
medulla oblongata
trigeminal ner
auriculotemporal
mandibular
inferior alveolar
inferior alveolar
alveolar
superior
lacrimal ner
trigeminal ganglion
ophthalmic division
frontal nerve
ve
nasociliary nerve
maxillary nerve
infraorbital nerve
nerves
lingual nerve
nerve
mylohyoid nerve
lingual nerve
nerve
division
nerve
ve
pons
abducent nerve
lateral rectus (cut)
A
B
FIGURE 11.65
Origin and distribution of the abducent nerve.
Distribution of the trigeminal nerve.
A.
B.
610
CHAPTER 11
to the temporalis muscle
Deep temporal nerves
to the masseter muscle (Fig. 11.36)
Masseteric nerve
Branches from the Anterior Division of the
palatini muscle.
not only the medial pterygoid, but also the tensor veli
which supplies
Nerve to the medial pterygoid muscle,
Meningeal branch
Branches from the Main Trunk of the Mandibular
rior and a large posterior division (Fig. 11.66).
the mandibular nerve, and then divides into a small ante
men ovale and joins the sensory root to form the trunk of
the trigeminal nerve also leaves the skull through the fora
ovale to enter the infratemporal fossa. The motor root of
ganglion and passes out of the skull through the foramen
11.11 and 11.65). The sensory root leaves the trigeminal
The mandibular nerve is both motor and sensory (Figs.
Mandibular Nerve (V3)
nasopharynx
which supplies the roof of the
Pharyngeal branch,
supply the palate, the tonsil, and the nasal cavity
(Fig. 11.19), which
Greater and lesser palatine nerves
inferior orbital fissure
which enter the orbit through the
Orbital branches,
Branches
lacrimal and nasal glands (see page 551).
pterygopalatine fossa (Fig. 11.19). It is secretomotor to the
glion, which is suspended from the maxillary nerve in the
The pterygopalatine ganglion is a parasympathetic gan
Pterygopalatine Ganglion
and the incisor teeth
supplies the maxillary sinus as well as the upper canine
(Fig. 11.19), which
Anterior superior alveolar nerve
teeth, the gums, and the cheek
plies the maxillary sinus as well as the upper premolar
(Fig. 11.19), which sup
Middle superior alveolar nerve
teeth and adjoining parts of the gum and the cheek
supplies the maxillary sinus as well as the upper molar
(Fig. 11.19), which
Posterior superior alveolar nerve
rimal gland.
glionic parasympathetic fibers that are going to the lac
the palate, and the pharynx. They also contain postgan
that have passed through the ganglion from the nose,
palatine fossa (Fig. 11.19). They contain sensory fibers
suspend the pterygopalatine ganglion in the pterygo
which are two short nerves that
Ganglionic branches,
the lacrimal gland via the lacrimal nerve.
ral branch gives parasympathetic secretomotor fibers to
that supply the skin of the face. The zygomaticotempo
zygomaticotemporal and the zygomaticofacial nerves
(Fig. 11.19), which divides into the
Zygomatic branch
Meningeal branches
Branches
The Head and Neck
■
■
■
■
-
■
■
-
-
-
■
■
■
■
-
■
■
-
■
■
■
■
■
■
-
-
Nerve
■
■
■
■
Mandibular Nerve
■
■
■
■
(Fig. 11.36)
nerve are sensory (except the nerve to the mylohyoid muscle).
The branches of the posterior division of the mandibular
the inferior alveolar nerve to the lingual nerve
which frequently runs from
Communicating branch,
muscle.
hyoid muscle and the anterior belly of the digastric
(Fig. 11.36), which supplies the mylo
hyoid nerve
mylo
11.50). Before entering the canal, it gives off the
(mental nerve) to supply the skin of the chin (Fig.
lower jaw and emerges through the mental foramen
enters the mandibular canal to supply the teeth of the
(Figs. 11.36 and 11.66), which
Inferior alveolar nerve
to the submandibular ganglion.
secretomotor fibers
preganglionic parasympathetic
mouth. It also gives off
anterior two thirds of the tongue and the floor of the
11.66), and it supplies the mucous membrane of the
(Figs. 11.36 and
chorda tympani nerve
joined by the
and crosses the submandibular duct. In its course, it is
11.66). It then runs forward on the side of the tongue
alveolar nerve and enters the mouth (Figs. 11.36 and
which descends in front of the inferior
Lingual nerve,
gland.
tor fibers from the otic ganglion to the parotid salivary
conveys postganglionic parasympathetic secretomo
temporomandibular joint, and the scalp. This nerve also
auricle (Fig. 11.66), the external auditory meatus, the
which supplies the skin of the
Auriculotemporal nerve,
Branches from the Posterior Division of the
division of the mandibular nerve.
of the anterior
only sensory branch
nerve), and it is the
(which is supplied by the facial
the buccinator muscle
does not supply
the cheek (Fig. 11.36). The buccal nerve
to the skin and the mucous membrane of
Buccal nerve
Nerve to the lateral pterygoid muscle
■
■
■
■
Mandibular Nerve
■
■
-
■
■
■
■
-
-
■
■
to the posterior border of the mylohyoid line on the mandible.
region from the infratemporal fossa by running beneath the
Injury to the Lingual Nerve
The lingual nerve passes forward into the submandibular
origin of the superior constrictor muscle, which is attached
Here, it is closely related to the last molar tooth and is liable
to be damaged in cases of clumsy extraction of an impacted
third molar.
C L I N I C A L N O T E S
Otic Ganglion
auriculotemporal nerve.
secretomotor fibers reach the parotid salivary gland via the
lesser petrosal nerve (see page 614). The postganglionic
sopharyngeal nerve, and they reach the ganglion via the
goid muscle. The preganglionic fibers originate in the glos
skull, and it is adherent to the nerve to the medial ptery
located medial to the mandibular nerve just below the
The otic ganglion is a parasympathetic ganglion that is
-
-
Basic Anatomy
611
mandibular nerve
middle meningeal artery
auriculotemporal nerve
styloid process
inferior alveolar nerve
stylopharyngeus
glossopharyngeal nerve
superior constrictor
middle constrictor
styloglossus
inferior alveolar nerve
nerve to mylohyoid
stylohyoid ligament
deep part of submandibular gland
submandibular ganglion
lingual nerve
hypoglossal nerve
sublingual gland
genioglossus
opening of
submandibular duct
mylohyoid
anterior belly
of digastric
geniohyoid
hypoglossus
buccinator
medial pterygoid
chorda tympani
lingual nerve
nerve to
medial pterygoid
tensor veli palatini
FIGURE 11.66
Infratemporal and submandibular regions. Parts of the zygomatic arch, the ramus, and the body of the mandi
(Figs. 11.11 and 11.65). It passes forward with the internal
hindbrain between the pons and the medulla oblongata
This small nerve emerges from the anterior surface of the
Abducent Nerve
tenses the soft palate and the tympanic membrane.
the head and innervates the muscles of mastication. It also
The trigeminal nerve is thus the main sensory nerve of
salivary glands.
motor fibers pass to the submandibular and the sublingual
tympani and the lingual nerves. Postganglionic secreto
reach the ganglion from the facial nerve via the chorda
11.36 and 11.66). Preganglionic parasympathetic fibers
and is attached to the lingual nerve by small nerves (Figs.
glion that lies deep to the submandibular salivary gland
The submandibular ganglion is a parasympathetic gan
outline of the sublingual gland is shown as a solid black wavy line.
ble have been removed. Mylohyoid and lateral pterygoid muscles have also been removed to display deeper structures. The
-
Submandibular Ganglion
-
-
carotid artery through the cavernous sinus in the middle
612
CHAPTER 11
stylomastoid foramen. The facial nerve now passes forward
mid and it emerges from the temporal bone through the
pages 567 and 568). The nerve descends behind the pyra
on the medial side of the aditus of the mastoid antrum (see
tory and, at the posterior wall of the middle ear, bends down
The nerve then bends sharply backward above the promon
(Fig. 11.67; see also Figs. 11.29 and 11.30).
late ganglion
genicu
panic cavity), the nerve swells to form the sensory
ear. On reaching the medial wall of the middle ear (tym
enters the facial canal that runs laterally through the inner
bone (Fig. 11.28). At the bottom of the meatus, the nerve
internal acoustic meatus in the petrous part of the temporal
cranial fossa with the vestibulocochlear nerve and enter the
medulla oblongata. The roots pass laterally in the posterior
anterior surface of the hindbrain between the pons and the
(Fig. 11.67). The nerve emerges on the
vus intermedius)
(ner
The facial nerve has a motor root and a sensory root
Facial Nerve
ble for turning the eye laterally.
lateral rectus muscle (Fig. 11.65) and is therefore responsi
orbital fissure (Fig. 11.18). The abducent nerve supplies the
cranial fossa and enters the orbit through the superior
The Head and Neck
-
-
-
-
-
-
through the parotid gland to its
tion (Fig.
distribu
11.67).
temporal branch
facial nerve
zygomatic branch
upper buccal branch
lower buccal branch
marginal mandibular branch
cervical branch
to platysma
nerve to posterior
belly of digastric
nerve to stylohyoid
posterior
auricular
branch
motor root
sensory root
geniculate
ganglion
greater
petrosal
nerve
nerve of
pterygoid canal
deep petrosal
nerve
sympathetic
plexus around
internal
carotid artery
nerve to medial
pterygoid muscle
lingual nerve
tympanic branch
glossopharyngeal
nerve
chorda tympani
facial canal
facial nerve
tympanic plexus
nerve to
stapedius
lesser
petrosal nerve
sympathetic nerve
otic
ganglion
A
B
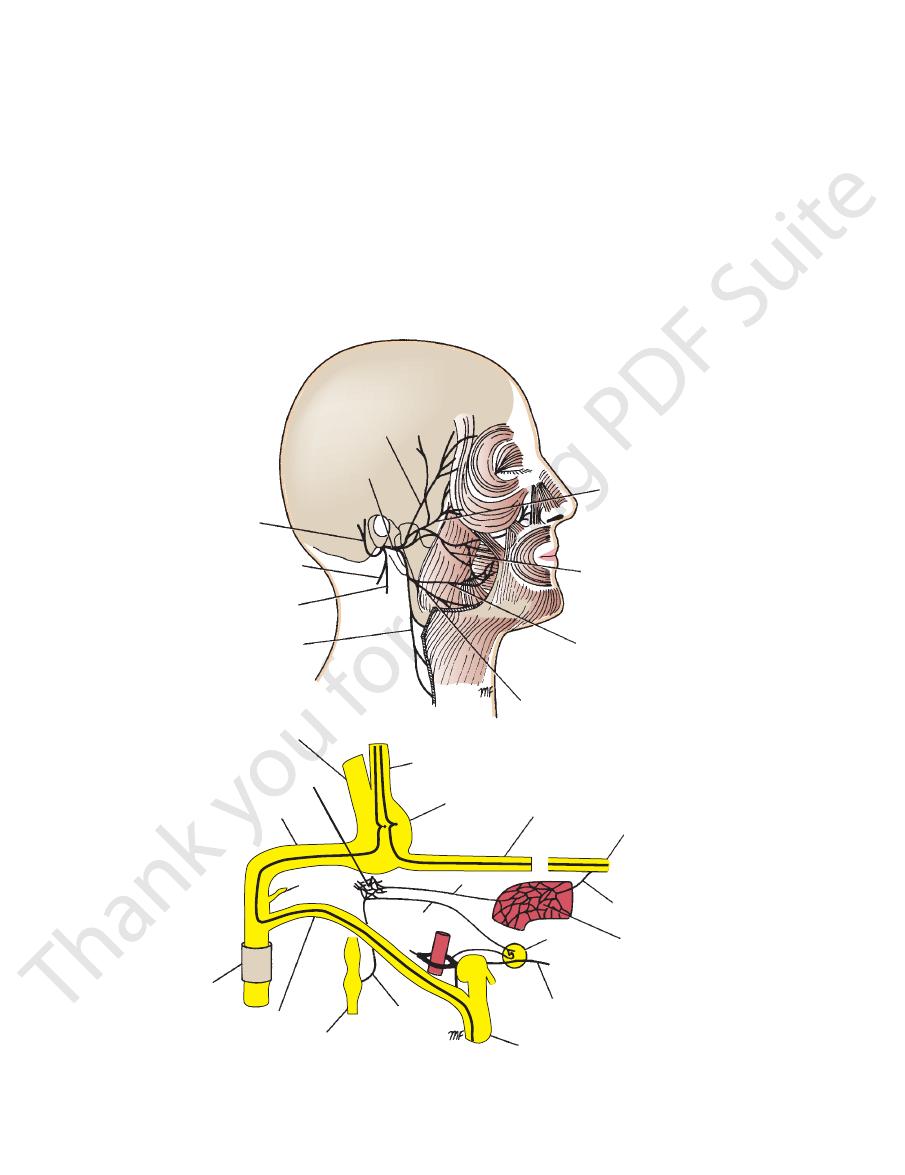
FIGURE 11.67
A.
the taste fibers are shown in black. The glossopharyngeal nerve is also shown.
Branches of the facial nerve within the petrous part of the temporal bone;
Distribution of the facial nerve. B.

Basic Anatomy
from the stylomastoid foramen.
lar branches given off by the facial nerve as it emerges
muscu
tric, and the stylohyoid nerves (Fig. 11.67) are
the posterior belly of the digas
Posterior auricular,
floor of the mouth.
fibers from the anterior two thirds of the tongue and
and the sublingual salivary glands. It also contains taste
sympathetic secretomotor fibers to the submandibular
nerve. The chorda tympani contains preganglionic para
entering the infratemporal fossa and joining the lingual
thus
petrotympanic fissure,
middle ear through the
of the tympanic membrane (Fig. 11.29) and leaves the
It runs forward over the medial surface of the upper part
canal in the posterior wall of the middle ear (Fig. 11.67).
arises from the facial nerve in the facial
Chorda tympani
middle ear (Fig. 11.67).
supplies the stapedius muscle in the
Nerve to stapedius
tains taste fibers from the palate.
nose and the palate. The greater petrosal nerve also con
secretomotor to the lacrimal gland and the glands of the
gopalatine ganglion. The postganglionic fibers are
onic parasympathetic fibers that synapse in the ptery
geniculate ganglion (Fig. 11.67). It contains pregangli
arises from the nerve at the
Greater petrosal nerve
Important Branches of the Facial Nerve
613
■
■
-
-
-
■
■
■
■
-
■
■
-
-
■
■
Five terminal branches to the muscles of facial expression.
the facial nerve (Fig. 11.28).
cranial fossa and enter the internal acoustic meatus with
medulla oblongata (Fig. 11.68). They cross the posterior
the anterior surface of the brain between the pons and the
They leave
cochlear.
vestibular
of two sets of fibers:
The vestibulocochlear nerve is a sensory nerve that consists
Vestibulocochlear Nerve
and from the palate.
from the anterior part of the tongue and floor of the mouth
tion, and lacrimation and is a pathway for taste sensation
The facial nerve thus controls facial expression, saliva
anguli oris muscles.
vical branch supplies the platysma and the depressor
cal branch supplies the buccinator muscle, and the cer
The buc
and pass to the muscles of the face and the scalp.
branches that emerge from the anterior border of the gland
the gland (see page 630). Here, it gives off the terminal
it is located between the superficial and the deep parts of
(Fig. 11.85B) after leaving the stylomastoid foramen, and
The facial nerve lies within the parotid salivary gland
(Fig. 11.67).
cervical branches
mandibular,
the
buccal,
zygomatic,
temporal,
These are the
the
the
and the
-
-
-
and
pons
cochlear nerve
vestibular ganglion
utricle
ampulla of superior
semicircular duct
ampulla of lateral semicircular duct
ampulla of posterior semicircular duct
cochlear duct
spiral ganglion
vestibular nerve
medulla oblongata of cochlea
tympanic plexus
lesser petrosal
nerve
rootlets of glossopharyngeal nerve
superior and inferior sensory ganglia
internal carotid artery
stylopharyngeus
soft palate
tonsillar branches
lingual branches to posterior third of tongue
pharyngeal branch
common carotid artery
carotid body
carotid sinus nerve
carotid sinus
otic
ganglion
parotid
salivary
gland
A
B
external carotid artery
tympanic
branch
FIGURE 11.68
A.
Distribution of the glossopharyngeal nerve.
Origin and distribution of the vestibulocochlear nerve. B.
614
CHAPTER 11
clavian artery
first part of the sub
side, the nerve hooks around the
(Fig. 11.69). On the right
Recurrent laryngeal nerve
the cricothyroid muscle.
is located close to the superior thyroid artery; it supplies
is motor and
external laryngeal nerve
vocal cords. The
of the piriform fossa and the larynx down as far as the
is sensory to the mucous membrane
laryngeal nerve
internal
internal and the external laryngeal nerves. The
(Fig. 11.69) divides into the
Superior laryngeal nerve
palate (except the tensor veli palatini).
pharynx (except the stylopharyngeus) and of the soft
pharyngeal plexus and supplies all the muscles of the
nial part of the accessory nerve. This branch joins the
contains nerve fibers from the cra
Pharyngeal branch
Meningeal and auricular branches
Important Branches of the Vagus Nerve in the Neck
opening in the diaphragm.
the lung, and enters the abdomen through the esophageal
num of the thorax (Fig. 11.69), passing behind the root of
carotid sheath (Fig. 11.49). It passes through the mediasti
the carotid arteries and internal jugular vein within the
The vagus nerve descends through the neck alongside
laryngeal branches.
and is distributed mainly in its pharyngeal and recurrent
joins the vagus nerve
cranial root of the accessory nerve
Below the inferior ganglion, the
inferior sensory ganglia.
superior and
jugular foramen. The vagus nerve has both
the posterior cranial fossa and leaves the skull through the
cerebellar peduncle. The nerve passes laterally through
the medulla oblongata between the olive and the inferior
ers (Fig. 11.69). It emerges from the anterior surface of
The vagus nerve is composed of motor and sensory fib
Vagus Nerve
from the carotid sinus and carotid body.
which influence the arterial blood pressure and respiration,
pharynx and the back of the tongue and carries impulses,
promotes salivation. It also conducts sensation from the
The glossopharyngeal nerve thus assists swallowing and
vallate papillae).
brane of the posterior third of the tongue (including the
(Fig. 11.68) passes to the mucous mem
Lingual branch
nerve and the sympathetic trunk.
and also receive branches from the vagus
geal plexus
pharyn
(Fig. 11.68) run to the
Pharyngeal branches
Nerve to the stylopharyngeus muscle
tion) (Fig. 11.68).
mechanism for the regulation of heart rate and respira
blood pressure and the carotid body and chemoreceptor
sinus (pressoreceptor mechanism for the regulation of
contains sensory fibers from the carotid
Carotid branch
ganglion.
and they synapse in the otic
lesser petrosal nerve,
fibers for the parotid salivary gland now leave the plexus
middle ear (Fig. 11.68). Preganglionic parasympathetic
passes to the tympanic plexus in the
Tympanic branch
Important Branches of the Glossopharyngeal
part of the neck to the back of the tongue (Fig. 11.68).
glossopharyngeal nerve then descends through the upper
located on the nerve as it passes through the foramen. The
are
inferior sensory ganglia
superior
foramen. The
fossa and leaves the skull by passing through the jugular
ebellar peduncle. It passes laterally in the posterior cranial
medulla oblongata between the olive and the inferior cer
(Fig. 11.68). It emerges from the anterior surface of the
The glossopharyngeal nerve is a motor and sensory nerve
Glossopharyngeal Nerve
are therefore concerned with hearing.
spiral organ of Corti
cochlear fibers originate in the
(Fig. 11.68). The
spiral ganglion of the cochlea
cells of the
The cochlear fibers are the central processes of the nerve
Cochlear Fibers
movement of the head.
they are concerned with the sense of position and with
from the vestibule and the semicircular canals; therefore,
acoustic meatus (Fig. 11.68). The vestibular fibers originate
cells of the vestibular ganglion situated in the internal
The vestibular fibers are the central processes of the nerve
Vestibular Fibers
The Head and Neck
and
-
and
Nerve
■
■
as the
■
■
-
■
■
■
■
-
■
■
-
-
-
■
■
■
■
-
■
■
■
■
-
men magnum. It then turns laterally to join the cranial root.
side the spinal cord and enters the skull through the fora
part of the spinal cord (Fig. 11.70). The nerve ascends along
column (horn) of the upper five segments of the cervical
The spinal root arises from nerve cells in the anterior gray
Spinal Root
posterior cranial fossa and joins the spinal root.
ebellar peduncle (Fig. 11.70). The nerve runs laterally in the
medulla oblongata between the olive and the inferior cer
The cranial root emerges from the anterior surface of the
Cranial Root
root (part) and a spinal root (part) (Fig. 11.70).
The accessory nerve is a motor nerve. It consists of a cranial
Accessory Nerve
structures with afferent and efferent fibers.
of all the cranial nerves and supplies the aforementioned
The vagus nerve has the most extensive distribution
pancreas.
associated with the alimentary tract, such as the liver and
to the splenic flexure of the colon. It also supplies glands
lungs; and much of the alimentary tract from the pharynx
sels within the thorax; the larynx, trachea, bronchi, and
The vagus nerve thus innervates the heart and great ves
(Fig. 11.69).
descend into the thorax, and end in the cardiac plexus
(two or three) arise in the neck,
Cardiac branches
of the upper part of the trachea.
ynx below the vocal cords, and the mucous membrane
cricothyroid muscle, the mucous membrane of the lar
and it supplies all the muscles of the larynx, except the
The nerve is closely related to the inferior thyroid artery,
into the neck between the trachea and the esophagus.
and then ascends
arch of the aorta
hooks around the
the trachea and the esophagus. On the left side, the nerve
and then ascends in the groove between
-
■
■
-
-
-
-
Basic Anatomy
615
superior laryngeal nerve
left vagus nerve
internal laryngeal nerve
external laryngeal nerve
left recurrent
laryngeal nerve
left recurrent laryngeal nerve
cardiac branches
cardiac branches
cardiac plexus
left vagus nerve
celiac plexus
aorta
liver
heart
right recurrent
laryngeal nerve
right vagus nerve (cut)
right lung
celiac branch of
right vagus nerve
spleen
kidney
anterior pulmonary
plexus
pharyngeal branch
superior and inferior
sensory ganglia of vagus
nerve
esophageal plexus
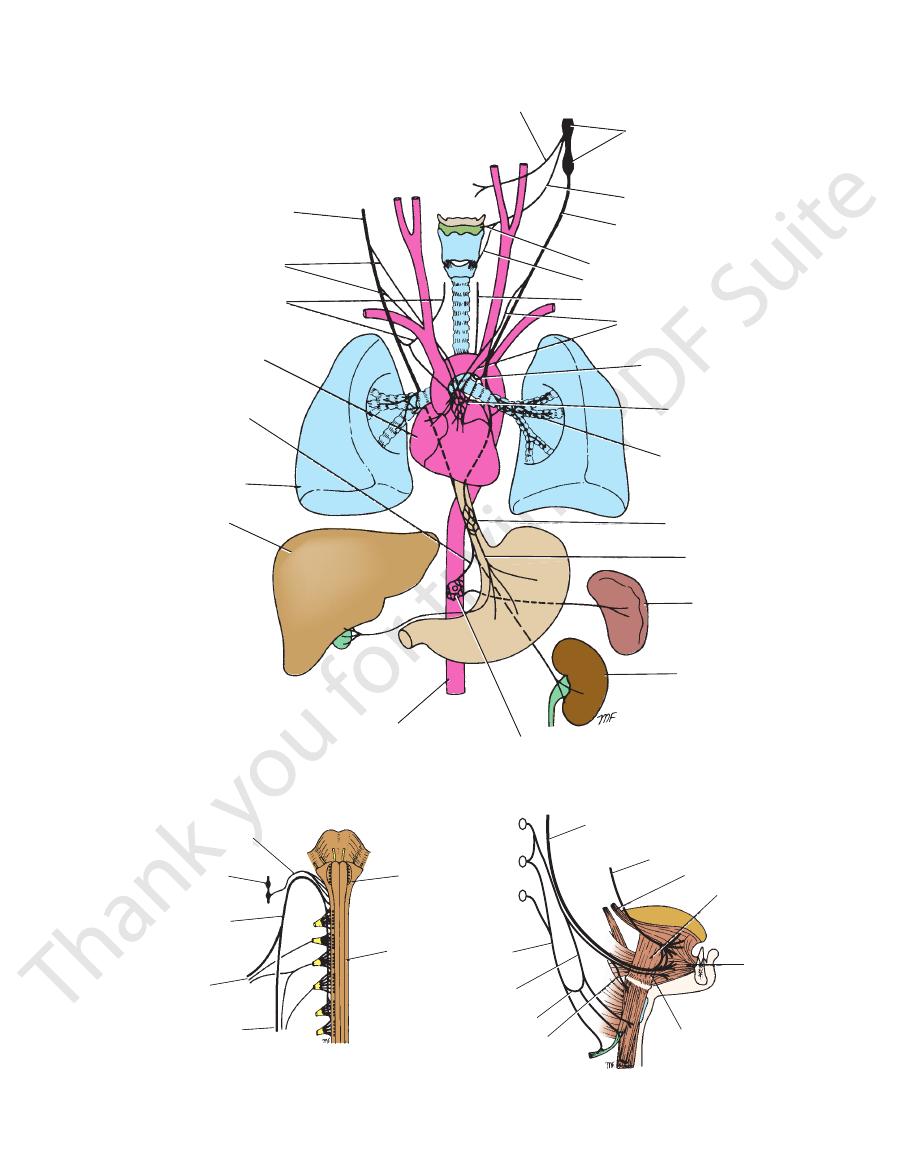
FIGURE 11.69
Distribution of the vagus nerve.
hypoglossal nerve
hypoglossus muscle
genioglossus
muscle
nerve to geniohyoid
muscle
lingual nerve
styloglossus muscle
descending
cervical
nerve
C1
C2
C3
nerve to thyrohyoid
muscle
ansa cervicalis
descending branch
of hypoglossal nerve
B
medulla
oblongata
spinal cord
c1
c2
c3
c4
c5
nerves to trapezius
muscle
nerves to
sternocleidomastoid
muscle
spinal root (part)
of accessory nerve
vagus nerve
cranial root of accessory nerve
A
FIGURE 11.70
A.
Distribution of the hypoglossal nerve.
Origin and distribution of the accessory nerve. B.
616
CHAPTER 11
two large muscles in the neck.
ments of the sternocleidomastoid and trapezius muscles,
the soft palate, pharynx, and larynx and controls the move
The accessory nerve thus brings about movements of
cle (Fig. 11.55).
posterior triangle of the neck to supply the trapezius mus
mastoid muscle, which it supplies, and then crosses the
laterally and enters the deep surface of the sternocleido
cricothyroid muscle). The spinal root runs downward and
yngeal plexus) and to the muscles of the larynx (except the
the muscles of the soft palate and pharynx (via the phar
joins the vagus nerves and is distributed in its branches to
jugular foramen. The roots then separate: The cranial root
The two roots unite and leave the skull through the
The Head and Neck
-
-
-
-
into action. Then, the patient is asked to shrug the shoulders,
causing the sternocleidomastoid of the opposite side to come
will drop. The patient will experience difficulty in elevating the
is paralyzed, the muscle will show wasting, and the shoulder
triangle in a relatively superficial position. It can be injured at
Injury to the Spinal Part of the Accessory Nerve
The spinal part of the accessory nerve crosses the posterior
operation or from penetrating wounds. The trapezius muscle
arm above the head, having abducted it to a right angle by
using the deltoid muscle.
Clinical examination of this nerve involves asking the
patient to rotate the head to one side against resistance,
causing the trapezius muscles to come into action.
C L I N I C A L N O T E S
Hypoglossal Nerve
the omohyoid, the sternohyoid, and the sternothyroid
Branches from this loop supply
ansa cervicalis.
(C2 and 3) to form
descending cervical nerve
joins the
(C1 fibers) passes downward and
Descending branch
Meningeal branch
Important Branches of the Hypoglossal Nerve
joined by C1 fibers from the cervical plexus.
the tongue (Fig. 11.70). In the upper part of its course, it is
crosses the internal and external carotid arteries to reach
nerve then passes downward and forward in the neck and
and leaves the skull through the hypoglossal canal. The
pyramid and the olive, crosses the posterior cranial fossa,
anterior surface of the medulla oblongata between the
The hypoglossal nerve is a motor nerve. It emerges on the
■
■
■
■
the
muscles.
of the levator scapulae and the scalenus medius muscles
branches, which form loops that lie in front of the origins
first four cervical nerves. The rami are joined by connecting
The cervical plexus is formed by the anterior rami of the
movements of the tongue.
the palatoglossus) and therefore controls the shape and
nerve thus innervates the muscles of the tongue (except
The hypoglossal
Nerve to the geniohyoid muscle (C1).
except the palatoglossus (pharyngeal plexus)
Muscular branches to all the muscles of the tongue
Nerve to the thyrohyoid muscle (C1)
■
■
■
■
■
■
Main Nerves of the Neck
Cervical Plexus
(Fig.
xus is covered in front by the pre
11.57). The ple
internal jugular vein within the carotid sheath. The cervical
vertebral layer of deep cervical fascia and is related to the
-
Clinical Testing of the Cranial Nerves
retinal veins, edema of the retina, and bulging of the optic disc
vein as it crosses the space, resulting in congestion of the
arachnoid space will compress the thin walls of the retinal
arachnoid space of the nerve sheath a short distance behind
forward around the optic nerve to the back of the eyeball. The
remembered that the intracranial subarachnoid space extends
ophthalmoscope. When examining the optic disc, it should be
The retinas and optic discs should then be examined with an
is then tested by using charts with lines of print of varying size.
any changes in eyesight have been noted. The acuity of vision
The optic nerve is evaluated by first asking the patient whether
tumors of the frontal lobes may produce lesions of the olfactory
that food flavors depend on the sense of smell and not on the
part of the examination of every neurologic patient. It may reveal
Systematic examination of the 12 cranial nerves is an important
a lesion of a cranial nerve nucleus or its central connections, or
it may show an interruption of the lower motor neurons.
Testing the Integrity of the Olfactory Nerve
The olfactory nerve can be tested by applying substances with
different odors to each nostril in turn. It should be remembered
sense of taste. Fractures of the anterior cranial fossa or cerebral
nerves, with consequent loss of the sense of smell (anosmia).
Testing the Integrity of the Optic Nerve
retinal artery and vein run in the optic nerve and cross the sub-
the eyeball. A rise in cerebrospinal fluid pressure in the sub-
(papilledema).
The visual fields should then be tested. The patient is asked
to gaze straight ahead at a fixed object with the eye under test,
the opposite eye being covered. A small object is then moved in
an arc around the periphery of the field of vision, and the patient
is asked whether he or she can see the object. It is important not
C L I N I C A L N O T E S
(continued)
618
CHAPTER 11
The Head and Neck
All the muscles of the larynx are supplied by the recurrent
plexus and their distribution.
Table 11.7 summarizes the branches of the cervical
central part of the diaphragm.
peritoneum covering the upper and lower surfaces of the
dium, the mediastinal parietal pleura, and the pleura and
diaphragm. It also sends sensory branches to the pericar
The phrenic nerve is the only motor nerve supply to the
described on page 99.
of the subclavian artery. Its further course in the thorax is
cle (Fig. 11.57) and enters the thorax by passing in front
downward across the front of the scalenus anterior mus
5th cervical nerves of the cervical plexus. It runs vertically
The phrenic nerve arises in the neck from the 3rd, 4th, and
Phrenic Nerve
Phrenic nerve
Muscular branch to the diaphragm.
the nerve to the thyrohyoid and geniohyoid.
Other C1 fibers within the hypoglossal nerve leave it as
the omohyoid, sternohyoid, and sternothyroid muscles.
cervical nerve fibers within the ansa cervicalis supply
(Fig. 11.60). The first, second, and third
ansa cervicalis
(C2 and 3), to form the
descending cervical nerve
hypoglossal as the descending branch, which unites with
glossal nerve. Some of these C1 fibers later leave the
ceptive, C3 and 4). A branch from C1 joins the hypo
3), levator scapulae (C3 and 4), and trapezius (proprio
muscles, sternocleidomastoid (proprioceptive, C2 and
Prevertebral
Muscular branches to the neck muscles.
from the phrenic nerve (gallbladder disease).
clinically, because pain may be referred along them
over the shoulder region. These nerves are important
intermediate, and lateral branches supply the skin
(C3 and 4). The medial, and
supraclavicular nerves
The
plies the skin over the front of the neck
(C2 and 3), which sup
transverse cervical nerve
The
the skin over the angle of the mandible
(C2 and 3), which supplies
greater auricular nerve
The
of the scalp and the auricle
(C2), which supplies the back
lesser occipital nerve
The
Cutaneous branches
Branches
neck, and the shoulders.
plexus supplies the skin and the muscles of the head, the
the muscles on the affected side are wasted, and the tongue
the paralyzed side. In patients with long-standing paralysis,
tionary. The result is the tip of the tongue’s deviation toward
tongue forward, leaving the paralyzed side of the tongue sta
normal genioglossus muscle pulls the unaffected side of the
tongue forward, is paralyzed on the affected side. The other,
as follows. One of the genioglossus muscles, which pull the
toward the paralyzed side (Fig. 11.78). This can be explained
the nerve is present, it will be noted that the tongue deviates
The patient is asked to put out the tongue, and if a lesion of
The hypoglossal nerve supplies the muscles of the tongue.
action. Then, the patient should be asked to shrug the shoulders,
laryngeal branch of the vagus, except the cricothyroid muscle,
which is supplied by the external laryngeal branch of the supe-
rior laryngeal branch of the vagus. Hoarseness or absence of the
voice may occur. Laryngoscopic examination may reveal abduc-
tor paralysis (see page 650).
Testing the Integrity of the Accessory Nerve
The accessory nerve supplies the sternocleidomastoid and the
trapezius muscles by means of its spinal part. The patient should
be asked to rotate the head to one side against resistance, caus-
ing the sternocleidomastoid of the opposite side to come into
causing the trapezius muscles to come into action.
Testing the Integrity of the Hypoglossal Nerve
-
is wrinkled on that side.
■
■
-
■
■
-
-
the
■
■
-
-
abdominal pressure. Consequently, the lower lobe of the lung
Phrenic Nerve Injury and Paralysis of the
Diaphragm
The phrenic nerve, which arises from the anterior rami of
the third, fourth, and fifth cervical nerves, is of considerable
clinical importance because it is the sole nerve supply to the
muscle of the diaphragm. Each phrenic nerve supplies the
corresponding half of the diaphragm.
The phrenic nerve can be injured by penetrating wounds
in the neck. If that occurs, the paralyzed half of the diaphragm
relaxes and is pushed up into the thorax by the positive
on that side may collapse.
About one third of persons have an accessory phrenic
nerve. The root from the fifth cervical nerve may be incor-
porated in the nerve to the subclavius and may join the main
phrenic nerve trunk in the thorax.
C L I N I C A L N O T E S
Brachial Plexus
become arranged around the axillary artery in the axilla
cross the posterior triangle of the neck, and the cords
medius muscles (Fig. 11.57). The trunks and divisions
neck between the scalenus anterior and the scalenus
The roots of the brachial plexus enter the base of the
terior cord.
pos
posterior divisions of all three trunks join to form the
medial cord,
of the lower trunk continues as the
the anterior division
lateral cord,
trunks unite to form the
The anterior divisions of the upper and middle
divisions.
posterior
anterior
Each trunk then divides into
trunk.
lower
and the roots of C8 and T1 unite to form the
trunk,
middle
the root of C7 continues as the
upper trunk,
The roots of C5 and 6 unite to form
cords.
divisions,
roots, trunks,
(Fig. 11.71). This plexus is divided into
7th, and 8th cervical and the first thoracic spinal nerves
the neck by the union of the anterior rami of the 5th, 6th,
The brachial plexus is formed in the posterior triangle of
and
the
and
and the
-
Basic Anatomy
619
Summary of the Branches
of the Cervical Plexus
and Their Distribution
T A B L E 1 1 . 7
Branches
Distribution
Cutaneous
Lesser occipital
Skin of scalp behind ear
Greater auricular
Skin over parotid salivary gland,
auricle, and angle of jaw
Transverse
cutaneous
Skin over side and front of neck
Supraclavicular
Skin over upper part of chest and
shoulder
Muscular
Segmental
Prevertebral muscles, levator scapulae
Ansa cervicalis
(C1, 2, 3)
Omohyoid, sternohyoid, sternothyroid
C1 fibers via
hypoglossal nerve
Thyrohyoid, geniohyoid
Phrenic nerve
(C3, 4, 5)
Diaphragm (most important muscle of
respiration)
Sensory
Phrenic nerve
(C3, 4, 5)
are summarized in Table 9.4.
The branches of the brachial plexus and their distribution
Branches
axillary sheath.
artery and vein are enclosed in the
(see Fig. 9.20). Here, the brachial plexus and the axillary
Pericardium, mediastinal parietal
pleura, and pleura and peritoneum
covering central diaphragm
Injury to the Brachial Plexus
ing a local anesthetic. The anesthetic solution is massaged
The roots and trunks of the brachial plexus occupy the antero-
inferior angle of the posterior triangle of the neck. Incomplete
lesions can result from stab or bullet wounds, traction, or
pressure injuries. The clinical findings in Erb-Duchenne and
Klumpke’s lesions are fully described on page 429.
Brachial Plexus Nerve Block
It will be remembered that the axillary sheath, formed from the
prevertebral layer of deep cervical fascia, encloses the bra-
chial plexus and the axillary artery. A brachial plexus nerve
block can easily be obtained by closing the distal part of the
sheath in the axilla with finger pressure, inserting a syringe
needle into the proximal part of the sheath, and then inject-
along the sheath, producing a nerve block. The syringe needle
C L I N I C A L N O T E S
(continued)
may be inserted into the axillary sheath in the lower part of the
posterior triangle of the neck or in the axilla.
page 89)
neck and ends in the cardiac plexus in the thorax (see
which descends in the
superior cardiac branch,
The
form the pharyngeal plexus
branches of the glossopharyngeal and vagus nerves to
which unite with the pharyngeal
Pharyngeal branches,
12th cranial nerves
which join the 9th, 10th, and
Cranial nerve branches,
carotid artery.
ies and are distributed along the branches of the external
arteries. These branches form a plexus around the arter
to the common and external carotid
Arterial branches
rami of the cervical nerves
to the upper four anterior
Gray rami communicantes
plexus.
branches around the artery to form the internal carotid
the carotid canal in the temporal bone. It divides into
onic fibers, accompanies the internal carotid artery into
consisting of postgangli
internal carotid nerve,
The
Branches
skull (Fig. 11.60).
The superior cervical ganglion lies immediately below the
rior, middle, and inferior cervical ganglia.
The sympathetic trunk possesses three ganglia: the supe
the prevertebral layer of deep fascia (Fig. 11.49).
embedded in deep fascia between the carotid sheath and
common carotid arteries (i.e., medial to the vagus) and is
sympathetic trunk. It lies directly behind the internal and
where it becomes continuous with the thoracic part of the
to the base of the skull and below to the neck of the 1st rib,
The cervical part of the sympathetic trunk extends upward
Cervical Part of the Sympathetic Trunk
exercise. Rarely, pressure on the first thoracic nerve causes
At the root of the neck, the brachial plexus and the subclavian
Compression of the Brachial Plexus and the
Subclavian Artery
artery enter the posterior triangle through a narrow muscu-
lar–bony triangle. The boundaries of the narrow triangle are
formed in front by the scalenus anterior, behind by the sca-
lenus medius, and below by the 1st rib. In the presence of a
cervical rib (see page XXX), the 1st thoracic nerve and the
subclavian artery are raised and angulated as they pass over
the rib. Partial or complete occlusion of the artery causes
ischemic muscle pain in the arm, which is worsened by
symptoms of pain in the forearm and hand and wasting of the
small muscles of the hand.
The Autonomic Nervous System in
the Head and Neck
Sympathetic Part
-
Superior Cervical Ganglion
■
■
-
■
■
■
■
-
■
■
■
■
■
■
