Lecture 5+6 – Hemorrhage & Shock
20
Hemorrhage
Haemorrhage or bleeding is the loss of blood from the
circulatory system. It must be recognized & managed
aggressively to avoid multiple organ failure & death. It
must be treated first by arresting it, then other measures
like fluid resuscitation & blood transfusion.
Pathophysiology
Haemorrhage may lead to hypovolaemic shock
(hypoperfusion), the following events may occur:
Cellular anaerobic metabolism with lactic acidosis
(this acidosis causes coagulopathy & further
haemorrhage).
Ischaemic endothelial cells activate anti-coagulant
pathways & further haemorrhage.
Underperfused muscles are unable to generate heat so
hypothermia results which affects coagulation &
results in further haemorrhage.
These events result in a vicious cycle leading to
physiological exhaustion & death.
Medical therapy has a tendency to worsen the conditio
Intravenous fluids & blood are cold, so causes
hypothermia.
Many crystalloid fluids are acidic (normal saline has a
PH of 6.7).
Surgery causes heat loss (by opening body cavities) &
causes further haemorrhage.
Types of haemorrhage
1) Revealed & concealed haemorrhage :
Revealed haemorrhage: Obvious external haemorrhage.
eg. bleeding from open arterial wound, haematemesis
from DU.
Concealed haemorrhage: It is contained within body
cavity. It must be diagnosed & treated early, eg.
Abdominal (peritoneal & retroperitoneal), thoracic, &
pelvic bleeding due to trauma. Non-traumatic cause eg.
ruptured aortic aneurysm, occult GI bleeding.
2) Primary, reactionary, & secondary haemorrhage:
Primary hemorrhage: Occurring immediately as a result
of injury or surgery.
Reactionary (Delayed) haemorrhage : Occurring within
24 hours. Usually caused by dislodgement of clot (by
resuscitation, vasodilatation, normalization of BP) or due
to a slippage of a ligature.
Secondary haemorrhage: It usually occurs within 7 – 14
days after injury. It is precipitated by infection, pressure
necrosis (such as from a drain), or malignancy.
3) Surgical & non-surgical haemorrhage
Surgical haemorrhage: Result from direct injury; it is
amenable to surgical control.
Non-surgical haemorrhage: Result from oozing from
raw surfaces due to coagulopathy. It requires correction of
coagulation abnormalities or packing.
Hemorrhag is broken down into 4 classes by the
American College of Surgeons' Advanced Trauma Life
Support
1) Class I Hemorrhage involves up to 15% of blood
volume. There is typically no change in vital signs and
fluid resuscitation is not usually necessary.
2) Class II Hemorrhage involves 15-30% of total blood
volume. A patient is often tachycardic (rapid heartbeat)
with a narrowing of the difference between the systolic
and diastolic blood pressures. The body attempts to
compensate with peripheral vasoconstriction. Skin may
start to look pale and be cool to the touch. Volume
resuscitation with crystalloids (Saline solution or Lactated
Ringer's solution) is all that is typically required. Blood
transfusion is not typically required.
3) Class III Hemorrhage involves loss of 30-40% of
circulating blood volume. The patient's blood pressure
drops, the heart rate increases, peripheral perfusion, such
as capillary refill worsens, and the mental status worsens.
Fluid resuscitation with crystalloid and blood transfusion
are usually necessary.
4) Class IV Hemorrhage involves loss of >40% of
circulating blood volume. The limit of the body's
compensation is reached and aggressive resuscitation is
required to prevent death
Lecture 5+6 – Hemorrhage & Shock
21
Management of haemorrhage
1) Identify haemorrhage: Revealed haemorrhage may be
obvious but the diagnosis of concealed haemorrhage may
be difficult. Any shock should be assumed to be
hypovolaemic until proved otherwise & the cause should
be assumed haemorrhage until this has been excluded.
2) Immediate resuscitation:
Direct pressure should be placed over the site of external
haemorrhage .
Airway & breathing should be assessed & controlled.
Large- bore intravenous access should be instituted &
blood drawn for cross- matching.
Intravenous fluids should be given, & when the blood is
available it should be given according to the degree of
haemorrhage.
3) Identify the site of haemorrhage:
This is important to define the next step in haemorrhage
control (operation, endoscopic control,
angioembolization).
• History: Previous episodes, known aneurysm, drugs
(steroidal & nonsteroidal anti-inflammatory).
• Physical examination: Nature of blood : fresh, melaena,
external signs of injury, abdominal tenderness.
• Investigations: Must be appropriate to the patients
physiological condition, & unnecessary investigations
must be avoided. Chest & pelvic radiography, abdominal
ultrasound, diagnostic peritoneal aspiration.
4) haemorrhage control:
Control must be achieved rapidly by moving the patient
rapidly to a place of haemorrhage control (theater,
angiography or endoscopy suites). Patient needs
lifesaving procedure so surgery may need to be limited to
the minimum necessary to stop bleeding & control sepsis.
More definitive repairs can be delayed until the patient is
physiologically capable of sustaining the procedure
(Damage control surgery).
Shock
Shock is the most important cause of death among
surgical patients.
Definition: It is a systemic state of low tissue perfusion,
which is inadequate for normal cellular respiration.
Pathophysiology
1) Cellular
Tissue perfusion is reduced,
cells are deprived of oxygen
anaerobic metabolism occurs
Liberation of lactic acid (instead of carbon dioxide)
causes systemic metabolic acidosis .
As glucose within the cells exhausted anaerobic
respiration ceases
failure of sodium potassium pump in the cell membrane
& intracellular organelles.
Intracellular lysosomes release autodigestive enzymes &
cell lysis ensues.
Intracellular contents including potassium are released
into the blood stream causing hyperkalaemia.
2) Microvascular
Tissue ischemia activate immune & coagulation
systems.
Hypoxia & acidosis activate complement & prime
neutrophils resulting in the generation of oxygen free
radicals & cytokine release.
These lead to injury to capillary endothelial cells &
further activation of the immune & coagulation
systems.
The damaged endothelium becomes leaky, so fluid
leaks & tissue oedema ensues, exacerbating cellular
hypoxia.
3) Systemic
a) Cardiovascular: Decreased preload & afterload cause
compensatory baroreceptor response which leads to
increased sympathetic activity & release of
catecholamines into the circulation which results in
tachycardia & systemic vasoconstriction (except in sepsis)

Lecture 5+6 – Hemorrhage & Shock
22
b) Respiratory: The metabolic acidosis & increased
sympathetic activity result in an increased respiratory rate
& minute ventilation to increase the excretion of carbon
dioxide & this produces compensatory respiratory
alkalosis.
c) Renal: Decreased perfusion pressure in the kidney leads
to reduced filtration at the glomerulus & a decreased urine
output.
The renin-angiotensin-aldosterone axis is stimulated
resulting in further vasoconstriction & increased sodium
& water reabsorption by the kidney.
d) Endocrine: Antidiuretic hormon (vasopressin) is released
from hypothalamus & results in vasoconstriction & water
reabsorption in the renal collecting system.
Cortisol is also released from the adrenal cortex causes
sodium & water reabsorption & sensitising the cells to
catecholamines.
4) Ischemia-perfusion syndrome
Systemic hypo-perfusion causes tissue hypoxia which
activates complement, neutrophils, & microvascular
thrombi which cause further endothelial damage to
organs such as the lungs & kidneys.
The acid & potassium load cause myocardial
depression, vascular dilatation & further hypotension.
These events cause multiple organ failure.
Classification of shock
1) Hypovolemic shock:
It is the most common form of shock, caused by reduced
circulating volume due to
a) haemorrhagic causes
b) Non-haemorrhagic causes: poor fluid intake, excessive
fluid loss because of vomiting, diarrhea, urinary loss
(as in diabetes), evaporation & third- spacing (fluid is
lost into GIT & interstitial spaces as in bowel
obstruction or pancreatitis.
2) Cardigenic shock
It is due to primary failure of the heart to pump blood to
the tissues.
It occurs in:
a) myocardial infarction
b) dysrhythmias
c) valvular heart disease
d) blunt myocardial injury
e) cardiomyopathy
f) Myocardial depression: results from endogenous
factors released in sepsis & pancreatitis or exogenous
factors such as drugs.
3) Obstructive shock
Mechanical obstruction of cardiac filling causes reduction
of preload & fall in cardiac output.
It occurs in :
a) cardiac tamponade
b) tension pneumothorax
c) massive pulmonary embolism
d) Air embolism.
4) Distributive shock
There is abnormally high cardiac output with
vasodilatation & hypotension. There is maldistribution of
blood flow at a microvascular level with arteriovenous
shunting & dysfunction of the cellular utilization of
oxygen. The peripheries are worm & capillary refill is
brisk despite profound shock.
It occurs in
a) Septic shock: caused by release of endotoxins &
acivation of cellular & humoral components of the
immune system.
b) Anaphylaxis: vasodilatation is caused by histamine
release.
c) Spinal cord injury (neurogenic shock): caused by
failure of sympathetic outflow & adequate vascular
tone.
5)
Endocrine shock
: It occurs in:
a) hypo- & hyperthyroidism
b) Adrenal insufficiency.
In hypothyroidism there is disordered vascular & cardiac
responsiveness to circulating catecholamines so cardiac
output falls & there may be associated cardiomyopathy.
Hyperthyroidism may cause a high- output cardiac failure.
In adrenal insufficiency there is hypovolaemia & poor
response to circulating & exogenous catecholamines, it
occurs in Addisons disease, & systemic sepsis.
Severity of shock:
1) Compensated shock: There is a compensatory
cardiovascular & endocrine response to maintain adequate
blood flow to the most vital organs (brain, heart, lungs, &
kidneys) & reducing perfusion to the skin, muscles, &
Lecture 5+6 – Hemorrhage & Shock
23
GIT. Apart from tachycardia & cool peripheries
(vasoconstriction) there may be no other clinical signs of
hypovolaemia. Loss of 15% of the circulating blood
volume is within normal compensatory mechanism.
Blood pressure is only falls after 30-40% of circulating
volume has been lost.
2) Decompensation: Further loss of circulating volume
causes progressive cardiovascular, respiratory, & renal
decompensation.
3) Mild shock: Initially there is tachycardia, tachypnoea &
mild reduction in urine output with mild anxiety. Blood
pressure is maintained although there is a decrease in
pulse pressure. The peripheries are cold & sweaty with
prolonged capillary refill times (except in septic
distributive shock).
4) Moderate shock: As shock progresses, renal
compensatory mechanisms fail, renal perfusion falls &
urine output decreases below 0.5 ml/kg/h. There is further
tachycardia & blood pressure starts to fall. Patients
become drowsy & mildly confused.
5) Severe shock: There is profound tachycardia &
hypotension. Urine output falls to zero & patients are
unconscious with labored respiration.
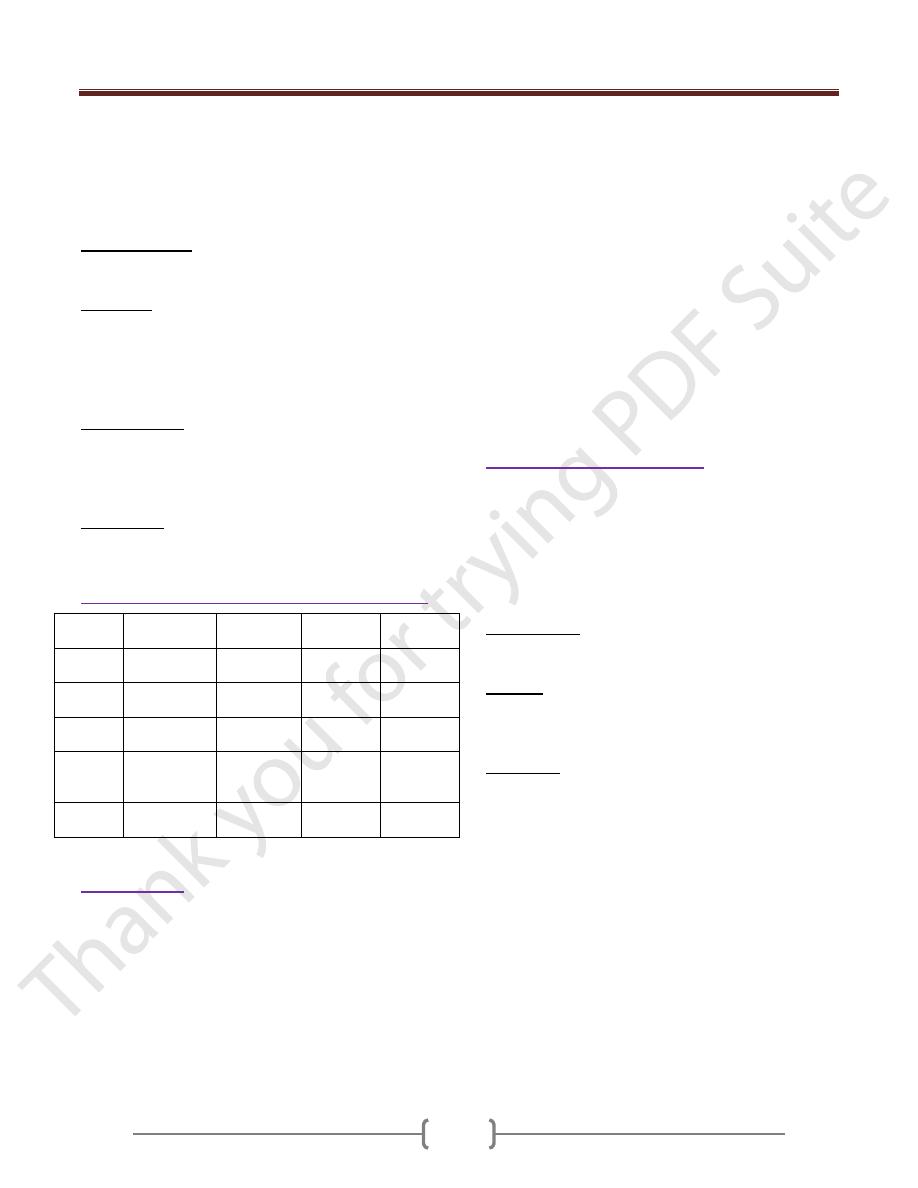
Cardiovascular and metabolic characteristics of shock
Hypovolaemia
Cardiogenic
Obstructive
Distributive
Cardiac
output
Low
Low
Low
High
Vascular
resistance
High
High
High
Low
Venous
pressure
Low
High
High
Low
Mixed
venous
saturation
Low
Low
Low
High
Base
deficit
High
High
High
High
Resuscitation
Should be rapid.
If there is doubt about the cause of shock it is safer to
assume the cause is hypovolaemia & begins with fluid
resuscitation followed by an assessment of the response.
If the general condition of the patient permits, rapid
clinical examination is performed.
In patients who are actively bleeding the resuscitation
should proceed parallel with surgery.
1) Ensure a patent airway & adequate oxygenation &
ventilation.
2) Intravenous access (with short wide- bore catheter) &
blood sample aspirated for cross-matching & blood
should be requested.
3) Intravenous administration of the available fluids
(crystalloid or colloid) while waiting blood Blood
transfusion should be done as early as possible.
4) Vasopressor agents (phenylephrine, noradrenaline) are
used in distributive shock in which there is peripheral
vasodilatation with hypotension despite high cardiac
output.
In cardiogenic shock or when myocardial depression
complicates a shock state inotropic therapy may be
needed to increase cardiac output & therefore oxygen
delivery. The inodilator dobutamine is the drug of choice.
Management of septic shock
1) Admission to intensive care unit of hospital.
2) Care of airway and breathing. Giving oxygen, and may
need mechanical ventilation.
3) Intravenous fluid (Crystalloid or colloid).
4) Antibiotic.
5) Taking history when the condition of patient permits.
6) Control of diabetes.
7) Investigations: Hb, WBC count, RBS, S. electrolytes, B.
urea, S. creatinin. Blood, urine and pus culture may be
needed. Chest X-ray.
8) Surgery: Drainage of pus, gangrene of limb may need
amputation.
9) Care of intravenous line (canula), intercostal tube and
Foley catheter if present.
10) Monitoring
a) Pulse rate, blood pressure, respiratory rate and
temperature
b) Oxygen saturation monitoring
c) Hourly urine output measurement. The best measures
of organ perfusion & the best monitor of the adequacy
of shock therapy remain the urine output.
d) CVP monitoring
e) Electrocardiogram
f) Cardiac output monitoring
g) Level of consciousness (is an important marker of
cerebral perfusion although it is a poor marker of
adequacy of resuscitation).
h) Measures of S. electrolytes and acid base balance.
